Laser Resonance Frequency Analysis: A Novel Measurement Approach to Evaluate Acetabular Cup Stability During Surgery
Abstract
1. Introduction
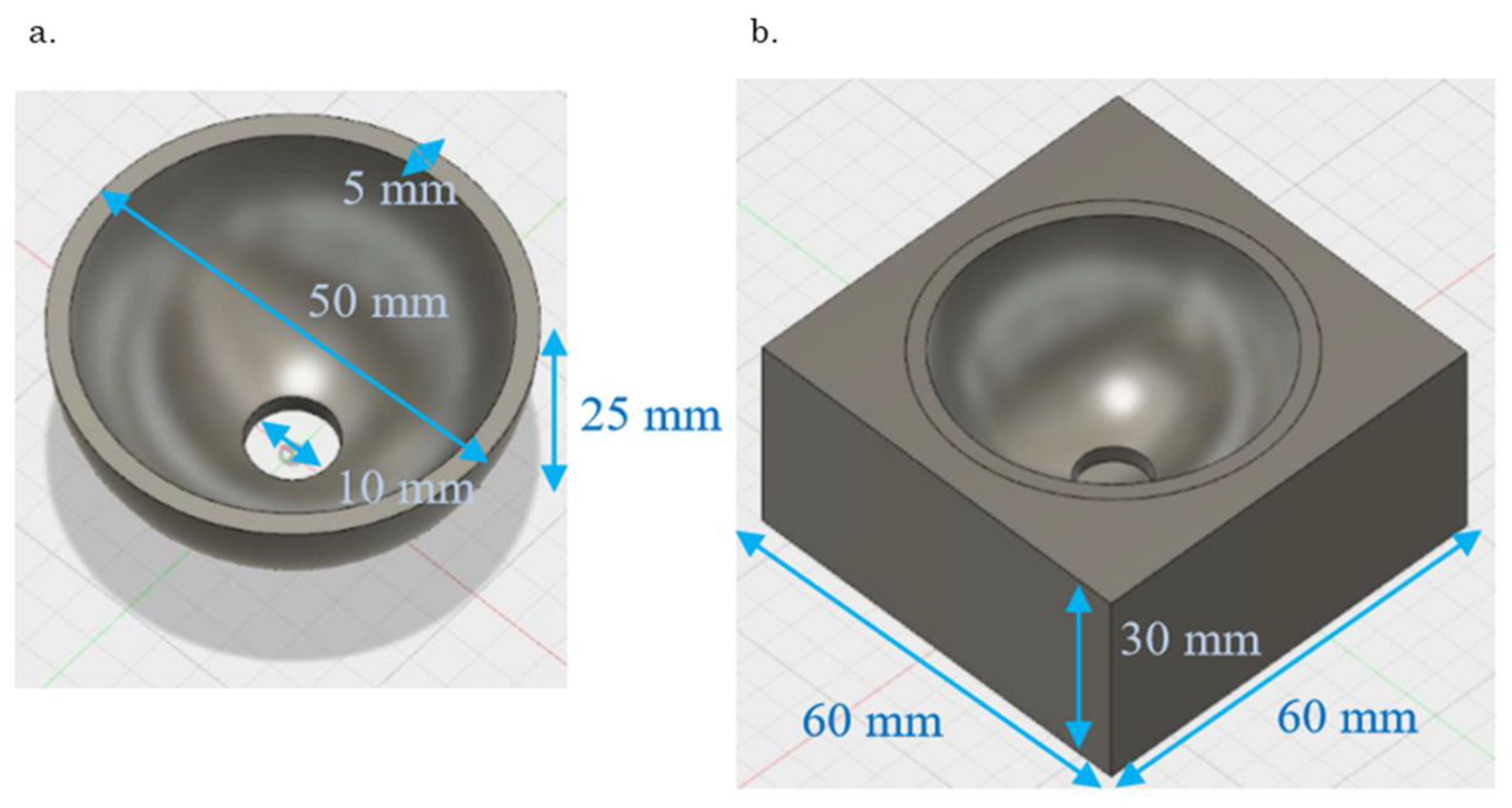
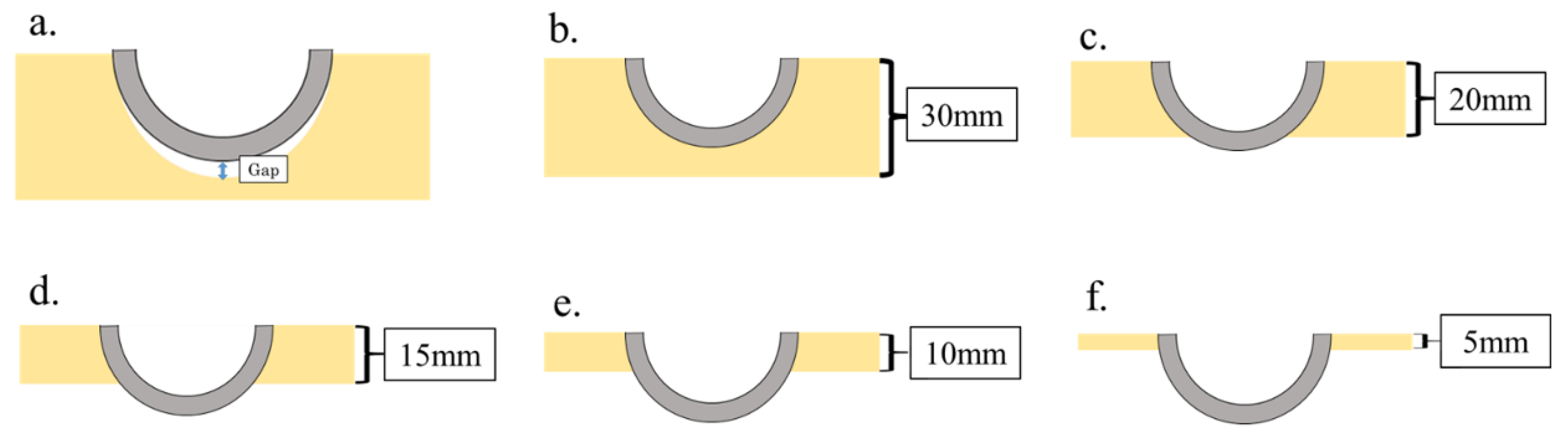
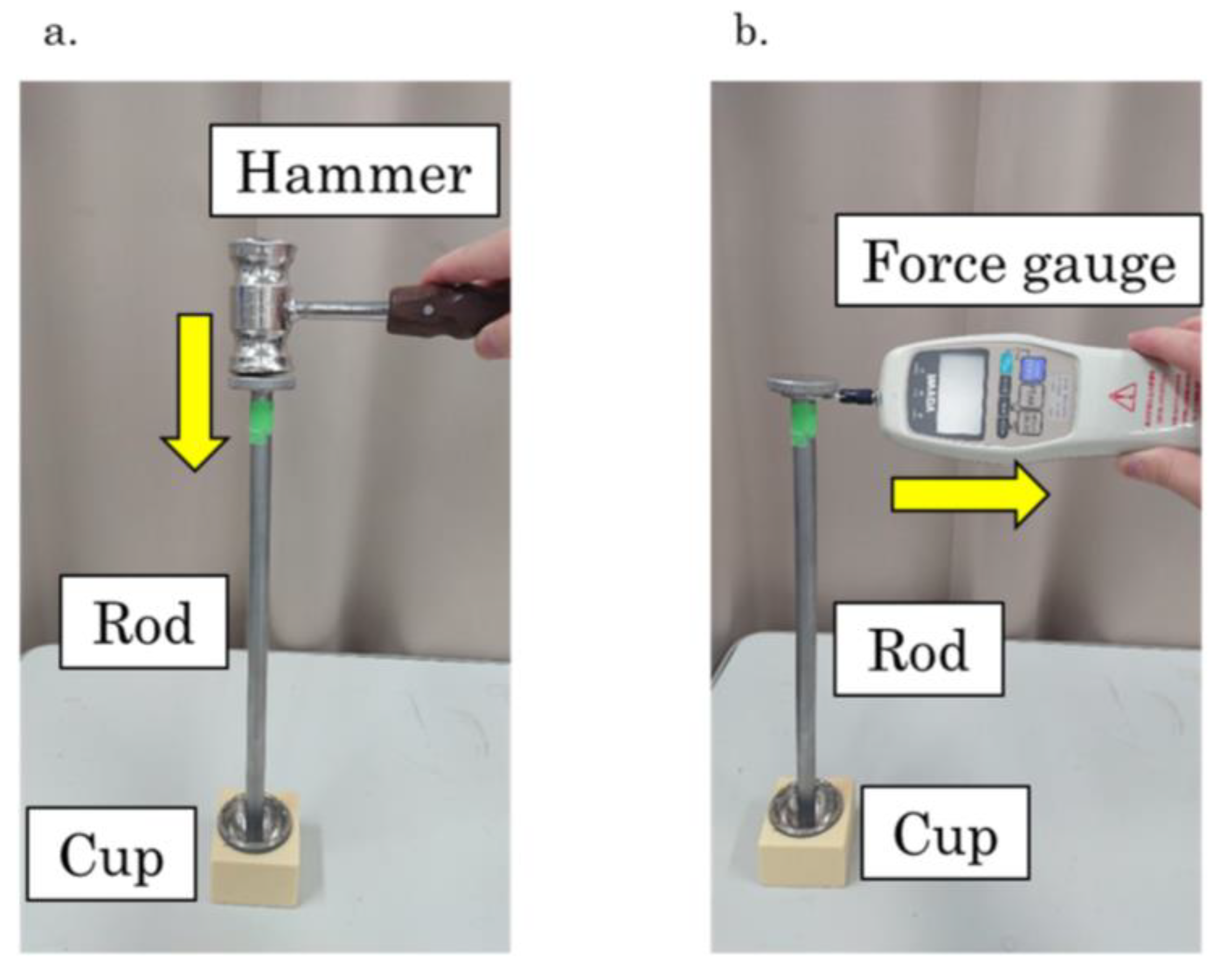
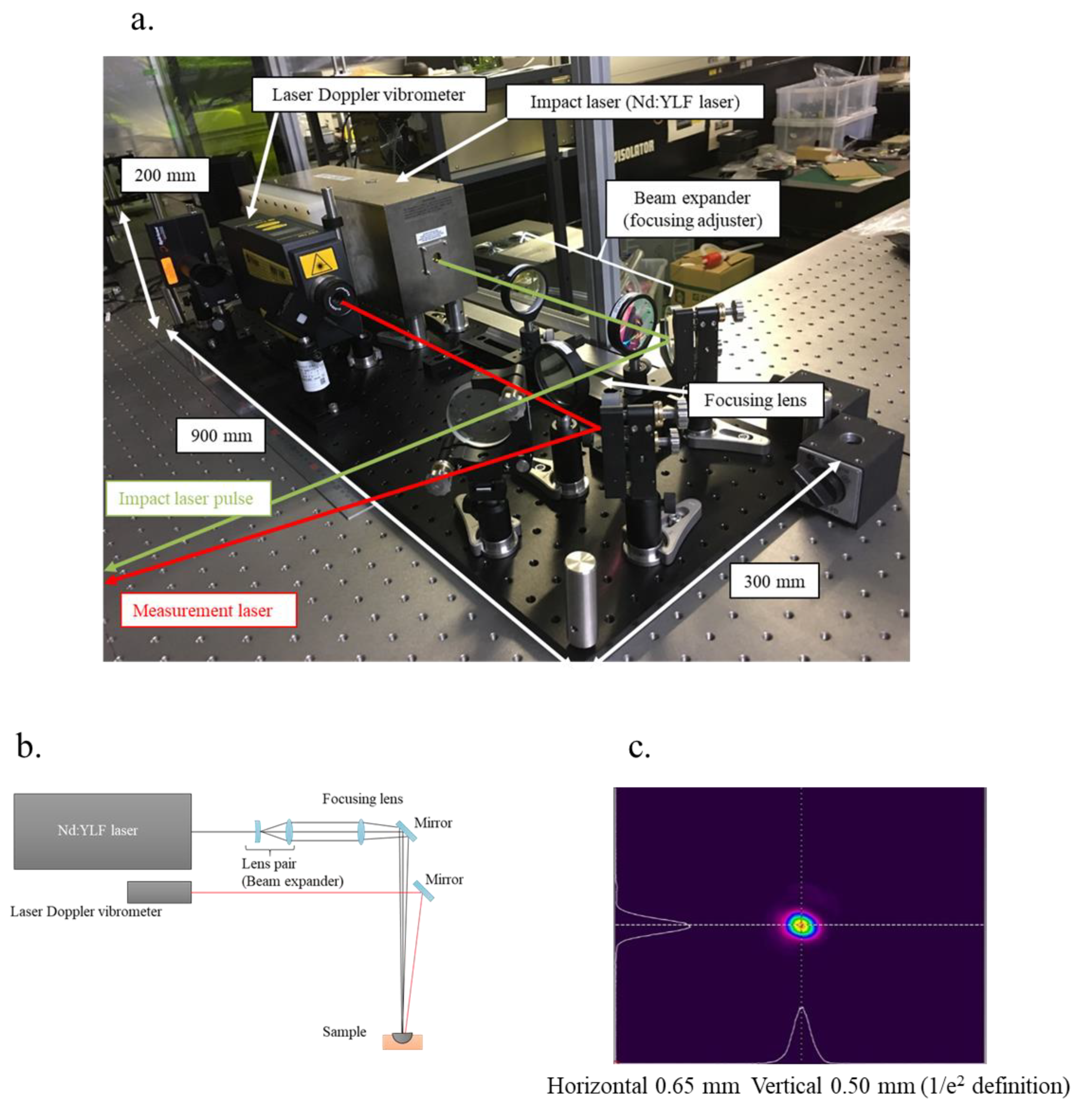
2. Materials and Methods
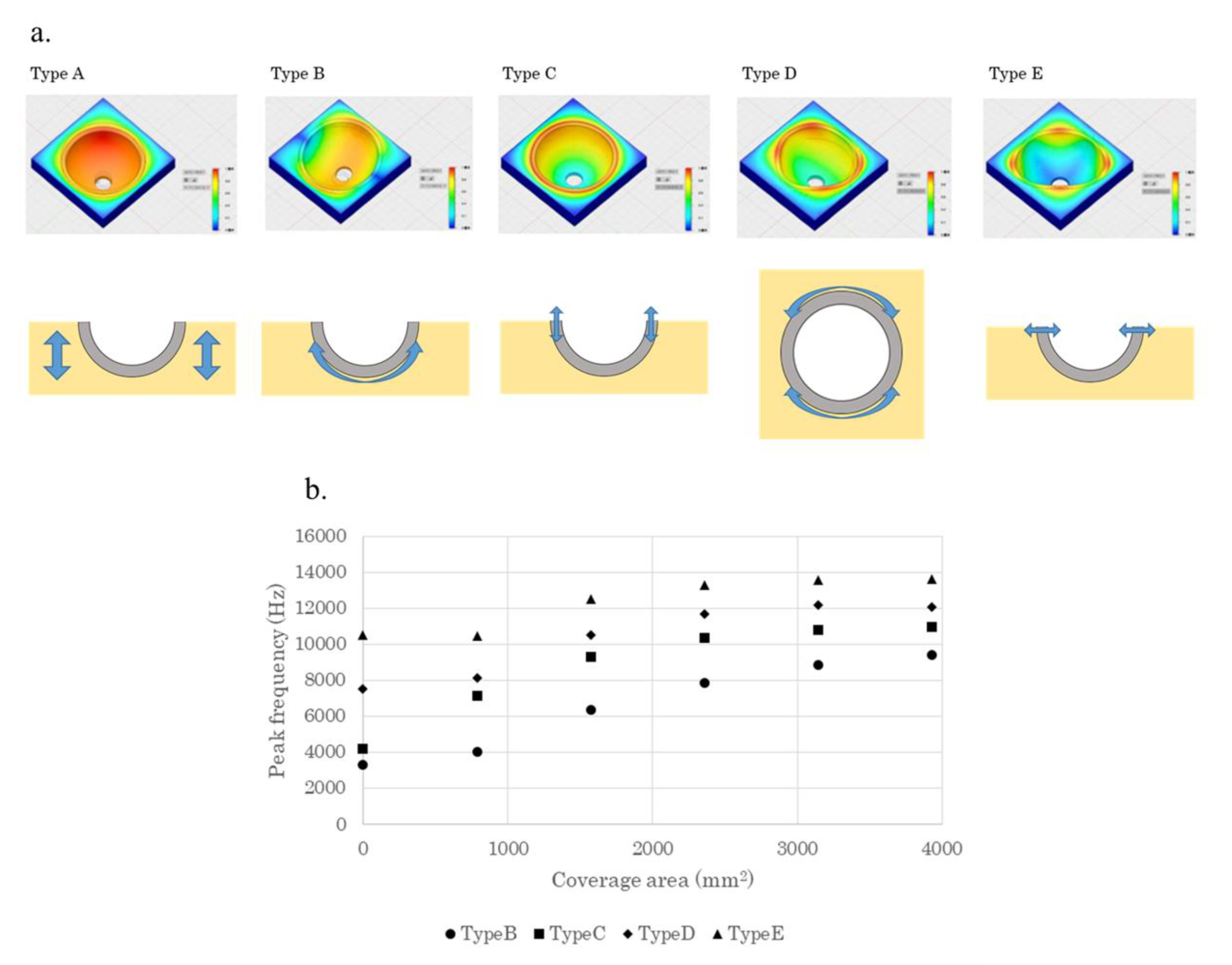
2.1. Finite Element Method to Analyse the Vibration Mode
2.2. Material
2.3. Measurement
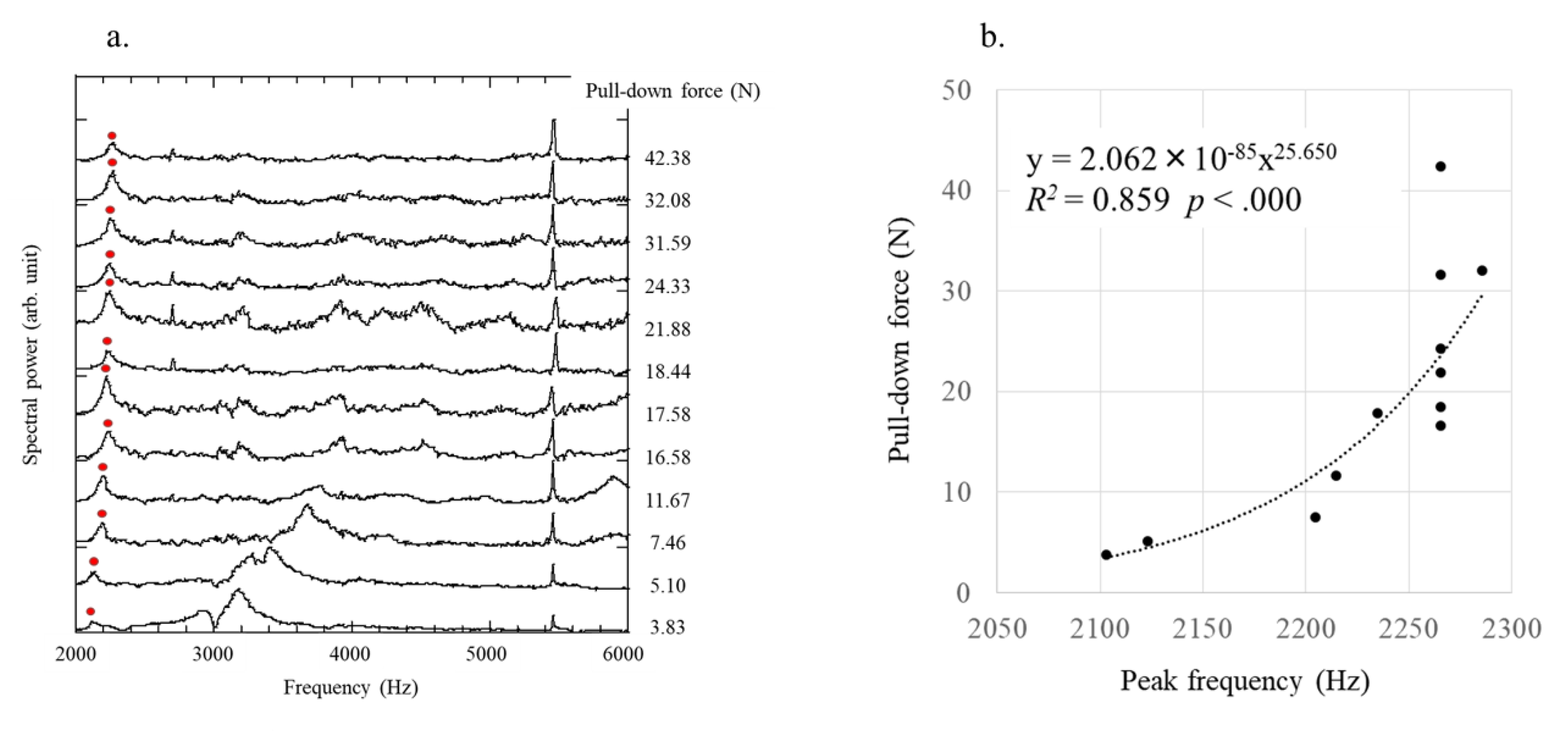
2.4. Laser Resonance Frequency Analysis
2.5. Statistical Analysis
3. Results
3.1. Analysis of the Vibration Pattern Using Finite Element Method
3.2. Laser Resonance Frequency Analysis
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Human Trabecular Bone | Polyurethane Foam | |
|---|---|---|
| Tension strength (MPa) | 14.88 ± 0.18 | 12.0 |
| Compressive strength (MPa) | 20.64 ± 0.59 | 18.0 |
| Shear strength (MPa) | 4.47 ± 0.12 | 7.60 |
References
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg. 2007, 89, 780–785. [Google Scholar]
- Akiyama, H.; Hoshino, A.; Iida, H.; Shindo, H.; Takakura, Y.; Miura, H.; Yamamoto, K.; Yoshiya, S.; Hasegawa, Y.; Shimamura, T.; et al. A pilot project for the Japan arthroplasty register. J. Orthop. Sci. 2012, 17, 358–369. [Google Scholar] [CrossRef] [PubMed]
- Kyriakopoulos, G.; Poultsides, L.; Christofilopoulos, P. Total hip arthroplasty through an anterior approach: The pros and cons. EFORT Open Rev. 2018, 3, 574–583. [Google Scholar] [CrossRef] [PubMed]
- Kwong, L.M.; O’Connor, D.O.; Sedlacek, R.C.; Krushell, R.J.; Maloney, W.J.; Harris, W.H. A quantitative in vitro assessment of fit and screw fixation on the stability of a cementless hemispherical acetabular component. J. Arthroplast. 1994, 9, 163–170. [Google Scholar] [CrossRef]
- Hamilton, W.G.; Calendine, C.L.; Beykirch, S.E.; Hopper, R.H., Jr.; Engh, C.A. Acetabular fixation options: First-generation modular cup curtain calls and caveats. J. Arthroplast. 2007, 22, 75–81. [Google Scholar] [CrossRef]
- Miettinen, S.S.; Makinen, T.J.; Laaksonen, I.; Makela, K.; Huhtala, H.; Kettunen, J.; Remes, V. Early aseptic loosening of cementless monoblock acetabular components. Int. Orthop. 2017, 41, 715–722. [Google Scholar] [CrossRef]
- Kim, Y.S.; Brown, T.D.; Pedersen, D.R.; Callaghan, J.J. Reamed surface topography and component seating in press-fit cementless acetabular fixation. J. Arthroplast. 1995, 10, S14–S21. [Google Scholar] [CrossRef]
- Henys, P.; Capek, L.; Fencl, J.; Prochazka, E. Evaluation of acetabular cup initial fixation by using resonance frequency principle. Proc. Inst. Mech. Eng. H 2015, 229, 3–8. [Google Scholar] [CrossRef]
- Michel, A.; Bosc, R.; Sailhan, F.; Vayron, R.; Haiat, G. Ex vivo estimation of cementless acetabular cup stability using an impact hammer. Med. Eng. Phys. 2016, 38, 80–86. [Google Scholar] [CrossRef]
- Tijou, A.; Rosi, G.; Hernigou, P.; Flouzat-Lachaniette, C.H.; Haiat, G. Ex Vivo Evaluation of Cementless Acetabular Cup Stability Using Impact Analyses with a Hammer Instrumented with Strain Sensors. Sensors 2017, 18, 62. [Google Scholar] [CrossRef]
- Tabata, T.; Kaku, N.; Hara, K.; Tsumura, H. Initial stability of cementless acetabular cups: Press-fit and screw fixation interaction—An in vitro biomechanical study. Eur. J. Orthop. Surg. Traumatol. 2015, 25, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, A.; Scheller, G.; Schwarz, M. Primary stability of cement-free press-fit acetabulum cups. In vitro displacement studies. Biomed. Tech. Biomed. Eng. 1999, 44, 356–359. [Google Scholar]
- Wetzel, R.; Simnacher, M.; Scheller, G. Initial stability of press-fit acetabular cups—An in-vitro study. Biomed. Tech. Biomed. Eng. 2005, 50, 400–403. [Google Scholar] [CrossRef] [PubMed]
- Kanda, A.; Kaneko, K.; Obayashi, O.; Mogami, A.; Iwase, H. Limitation of total hip arthroplasty of the acetabular roof by press-fit without screw fixation: Discussion of a biomechanical study. Eur. J. Orthop. Surg. Traumatol. 2013, 23, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Meredith, N.; Alleyne, D.; Cawley, P. Quantitative determination of the stability of the implant-tissue interface using resonance frequency analysis. Clin. Oral Implant. Res. 1996, 7, 261–267. [Google Scholar] [CrossRef]
- Meredith, N.; Book, K.; Friberg, B.; Jemt, T.; Sennerby, L. Resonance frequency measurements of implant stability in vivo. A cross-sectional and longitudinal study of resonance frequency measurements on implants in the edentulous and partially dentate maxilla. Clin. Oral Implant. Res. 1997, 8, 226–233. [Google Scholar] [CrossRef]
- Valderrama, P.; Oates, T.W.; Jones, A.A.; Simpson, J.; Schoolfield, J.D.; Cochran, D.L. Evaluation of two different resonance frequency devices to detect implant stability: A clinical trial. J. Periodontol. 2007, 78, 262–272. [Google Scholar] [CrossRef]
- Huwiler, M.A.; Pjetursson, B.E.; Bosshardt, D.D.; Salvi, G.E.; Lang, N.P. Resonance frequency analysis in relation to jawbone characteristics and during early healing of implant installation. Clin. Oral Implant. Res. 2007, 18, 275–280. [Google Scholar] [CrossRef]
- Nakashima, D.; Ishii, K.; Nishiwaki, Y.; Kawana, H.; Jinzaki, M.; Matsumoto, M.; Nakamura, M.; Nagura, T. Quantitative CT-based bone strength parameters for the prediction of novel spinal implant stability using resonance frequency analysis: A cadaveric study involving experimental micro-CT and clinical multislice CT. Eur. Radiol. Exp. 2019, 3, 1. [Google Scholar] [CrossRef]
- Nakashima, D.; Ishii, K.; Matsumoto, M.; Nakamura, M.; Nagura, T. A study on the use of the Osstell apparatus to evaluate pedicle screw stability: An in-vitro study using micro-CT. PLoS ONE 2018, 13, e0199362. [Google Scholar] [CrossRef]
- Michel, A.; Bosc, R.; Meningaud, J.P.; Hernigou, P.; Haiat, G. Assessing the Acetabular Cup Implant Primary Stability by Impact Analyses: A Cadaveric Study. PLoS ONE 2016, 11, e0166778. [Google Scholar] [CrossRef] [PubMed]
- Qi, G.; Paul Mouchon, W.; Tan, T.E. How much can a vibrational diagnostic tool reveal in total hip arthroplasty loosening? Clin. Biomech. 2003, 18, 444–458. [Google Scholar] [CrossRef]
- Goossens, Q.; Leuridan, S.; Henys, P.; Roosen, J.; Pastrav, L.; Mulier, M.; Desmet, W.; Denis, K.; Vander Sloten, J. Development of an acoustic measurement protocol to monitor acetabular implant fixation in cementless total hip Arthroplasty: A preliminary study. Med. Eng. Phys. 2017, 49, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Georgiou, A.P.; Cunningham, J.L. Accurate diagnosis of hip prosthesis loosening using a vibrational technique. Clin. Biomech. 2001, 16, 315–323. [Google Scholar] [CrossRef]
- Mikami, K.; Hasegawa, N.; Okada, H.; Kondo, S.; Nishikino, M.; Kawachi, T. Flash-lamp-pumped 4 J, 50 Hz Nd: YAG nanosecond laser system for mobile and transportable equipment. Jpn. J. Appl. Phys. 2017, 56, 082701. [Google Scholar] [CrossRef]
- Kurahashi, S.; Mikami, K.; Kitamura, T.; Hasegawa, N.; Okada, H.; Kondo, S.; Nishikino, M.; Kawachi, T.; Shimada, Y. Demonstration of 25-Hz-inspection-speed laser remote sensing for internal concrete defects. J. Appl. Remote Sens. 2018, 12, 015009. [Google Scholar] [CrossRef]
- Amirouche, F.; Solitro, G.; Broviak, S.; Gonzalez, M.; Goldstein, W.; Barmada, R. Factors influencing initial cup stability in total hip arthroplasty. Clin. Biomech. 2014, 29, 1177–1185. [Google Scholar] [CrossRef]
- Debruyne, S.; Grognard, N.; Verleye, G.; Van Massenhove, K.; Mavreas, D.; Vannet, B.V. ISQ calculation evaluation of in vitro laser scanning vibrometry-captured resonance frequency. Int. J. Implant Dent. 2017, 3, 44. [Google Scholar] [CrossRef]
- Henys, P.; Capek, L. Impact Force, Polar Gap and Modal Parameters Predict Acetabular Cup Fixation: A Study on a Composite Bone. Ann. Biomed. Eng. 2018, 46, 590–604. [Google Scholar] [CrossRef]
- Adler, E.; Stuchin, S.A.; Kummer, F.J. Stability of press-fit acetabular cups. J. Arthroplast. 1992, 7, 295–301. [Google Scholar] [CrossRef]
- Henys, P.; Leuridan, S.; Goossens, Q.; Mulier, M.; Pastrav, L.; Desmet, W.; Sloten, J.V.; Denis, K.; Capek, L. Modal frequency and shape curvature as a measure of implant fixation: A computer study on the acetabular cup. Med. Eng. Phys. 2018, 60, 30–38. [Google Scholar] [CrossRef] [PubMed]
- ASTM. F1839-01 Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopaedic Devices and Instruments; American Society for Testing and Materials: West Conshohocken, PA, USA, 2001. [Google Scholar]
- Pandit, H.; Glyn-Jones, S.; McLardy-Smith, P.; Gundle, R.; Whitwell, D.; Gibbons, C.L.; Ostlere, S.; Athanasou, N.; Gill, H.S.; Murray, D.W. Pseudotumours associated with metal-on-metal hip resurfacings. J. Bone Jt. Surg. 2008, 90, 847–851. [Google Scholar] [CrossRef] [PubMed]
- Daniel, J.; Holland, J.; Quigley, L.; Sprague, S.; Bhandari, M. Pseudotumors associated with total hip arthroplasty. J. Bone Jt. Surg. 2012, 94, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Willert, H.G.; Buchhorn, G.H.; Fayyazi, A.; Flury, R.; Windler, M.; Koster, G.; Lohmann, C.H. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J. Bone Jt. Surg. 2005, 87, 28–36. [Google Scholar] [CrossRef]
- Langton, D.J.; Jameson, S.S.; Joyce, T.J.; Hallab, N.J.; Natu, S.; Nargol, A.V. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: A consequence of excess wear. J. Bone Jt. Surg. 2010, 92, 38–46. [Google Scholar] [CrossRef]
- Campbell, P.; Ebramzadeh, E.; Nelson, S.; Takamura, K.; De Smet, K.; Amstutz, H.C. Histological features of pseudotumor-like tissues from metal-on-metal hips. Clin. Orthop. Relat. Res. 2010, 468, 2321–2327. [Google Scholar] [CrossRef]
| Acetabular Cup (Ti-6Al-4V) | Polyethylene Foam | |
|---|---|---|
| Thermal Conductivity (W/m·k) | 6.7 | 0.211 |
| Specific Heat (J/g·k) | 0.526 | 2.859 |
| Thermal Expansion Meter Rate (μm/m·k) | 8.600 | 150.00 |
| Young’s Modulus (GPa) | 113.770 | 0.911 |
| Poisson Ratio | 0.34 | 0.39 |
| Modulus of Shearing Elasticity (MPa) | 42,451.493 | 320.000 |
| Density (g/cm3) | 4.43 | 0.952 |
| Yield Strength (MPa) | 882.529 | 20.670 |
| Tensile Strength (MPa) | 951.477 | 13.780 |
| Protectability | Repeatability | Reproducibility | Contactability | |
|---|---|---|---|---|
| Pull-Down | × | × | × | × |
| Hammer Instrument | ○ | × | × | × |
| Dental RFA | ○ | ○ | ○ | × |
| Laser RFA | ○ | ○ | ○ | ○ |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kikuchi, S.; Mikami, K.; Nakashima, D.; Kitamura, T.; Hasegawa, N.; Nishikino, M.; Kanaji, A.; Nakamura, M.; Nagura, T. Laser Resonance Frequency Analysis: A Novel Measurement Approach to Evaluate Acetabular Cup Stability During Surgery. Sensors 2019, 19, 4876. https://doi.org/10.3390/s19224876
Kikuchi S, Mikami K, Nakashima D, Kitamura T, Hasegawa N, Nishikino M, Kanaji A, Nakamura M, Nagura T. Laser Resonance Frequency Analysis: A Novel Measurement Approach to Evaluate Acetabular Cup Stability During Surgery. Sensors. 2019; 19(22):4876. https://doi.org/10.3390/s19224876
Chicago/Turabian StyleKikuchi, Shunsuke, Katsuhiro Mikami, Daisuke Nakashima, Toshiyuki Kitamura, Noboru Hasegawa, Masaharu Nishikino, Arihiko Kanaji, Masaya Nakamura, and Takeo Nagura. 2019. "Laser Resonance Frequency Analysis: A Novel Measurement Approach to Evaluate Acetabular Cup Stability During Surgery" Sensors 19, no. 22: 4876. https://doi.org/10.3390/s19224876
APA StyleKikuchi, S., Mikami, K., Nakashima, D., Kitamura, T., Hasegawa, N., Nishikino, M., Kanaji, A., Nakamura, M., & Nagura, T. (2019). Laser Resonance Frequency Analysis: A Novel Measurement Approach to Evaluate Acetabular Cup Stability During Surgery. Sensors, 19(22), 4876. https://doi.org/10.3390/s19224876





