The Metabolic Impact of Nonalcoholic Fatty Liver Disease on Cognitive Dysfunction: A Comprehensive Clinical and Pathophysiological Review
Abstract
1. Introduction
2. Clinical Evidence
2.1. Evidence in Support of Correlation between NAFLD and Cognitive Impairment
2.2. Evidence in Support of Correlation between NAFLD and Alzheimer’s Disease
2.3. Evidence in Support of Correlation between NAFLD and Vascular Dementia
2.4. Evidence against Correlation between NAFLD and Cognitive Impairment/Dementia
| Authors | Location |
Study Type and
Patient Sample | Test Used | Findings Summary |
|---|---|---|---|---|
| Cognitive Impairment | ||||
| Liu et al. [30] | China | Longitudinal Study. 1651 middle-aged and elderly participants (>40 years) without cognitive impairment | MMSE | 48.2% with NAFLD had higher 4-year incidence of cognitive impairment and 1.45-fold risk for cognitive impairment with NAFLD. |
| Weinstein et al. [26] | United States | Longitudinal Study. 1102 individuals identified from 19,931 NHANES participants. Of those eligible, 49.6% did not have NAFLD or T2DM, 21.7% had NAFLD only, 12.9% had T2DM only, and 15.8% had both NAFLD and T2DM. | MMSE AFT DSST | Individuals with both NAFLD and T2DM scored significantly lower on cognitive assessments than those with neither condition. For the AFT, those with T2DM only and those with both NAFLD and T2DM scored lower than those with neither condition (NAFLD only: 18.57 ± 0.31; T2DM only: 15.91 ± 0.54; both: 16.84 ± 0.45). For the DSST, similar results were found with lower scores for those with T2DM only and those with both NAFLD and T2DM compared to those with neither (NAFLD only: 55.99 ± 1.05; T2DM only: 45.08 ± 1.98; both: 47.12 ± 1.65). |
| Seo et al. [31] | United States | Cross-Sectional Study. 4472 adults aged 20–59 years who participated in NHANES III, with 874 fulfilling the ultrasound definition of NAFLD | SRTT, SDST, SDLT | NAFLD was independently associated with lower cognitive performance. Participants with NAFLD showed lower performance on the SDLT after controlling for demographic factors, cardiovascular disease, and cardiovascular risk factors. The associations with SRTT and SDST did not reach statistical significance after adjusting for such comorbidities. |
| Filipović et al. [32] | Serbia | Cross-Sectional Study. 89 first diagnosed therapy-naive patients with high levels of aminotransferases were involved, out of which 40 (22 men and 18 women) aged 34–57 years satisfied the recruiting criteria. | MoCA | Patients with NAFLD had lower cognitive statuses according to the MoCA index compared to controls. Specifically, 26 patients in the NAFLD group had lower MoCA scores than the cutoff value of 26 points, versus 6 control members. Patients with NAFLD had a significantly increased risk of cognitive impairment, with an odds ratio of 0.096 and a relative risk (RR) of 3.9 for cognitive impairment. Additionally, NAFLD significantly influenced cognitive deficits, correlating with white and grey-matter volume reduction, and patients with NAFLD were about four times more likely to have cognitive impairment. |
| Celikbilek et al. [33] | Turkey | Cross-Sectional Study. 70 participants with NAFLD and 73 age-matched and sex-matched healthy participants ranging from 18 to 70 years old. | MoCA | The MoCA scores were significantly lower in participants with NAFLD than in the healthy group. More NAFLD participants presented with deficits in the visuospatial and executive function domains. Education level and area of residence were independently associated with cognitive dysfunction in both the NAFLD and healthy groups. |
| Tuttolomondo et al. [42] | Italy | Cross-Sectional Study. 80 consecutive patients with biopsy-proven NAFLD and 83 controls without fatty liver disease. | MMSE | AFLD patients had a lower mean MMSE score compared to patients without NAFLD. NAFLD subjects in comparison to controls had (1) lower mean values of Reactive Hyperemia Index (RHI); (2) higher mean values of pulse wave velocity (PWV) and augmentation index (Aix); (3) lower MMSE scores; (4) a significant relationship at multivariate analysis between RHI and MMSE with NAFLD; (5) a significant negative relationship between ballooning grade and MMSE grade only in NASH subjects; and (6) a significant positive relationship between steatosis and augmentation index only in NASH subjects |
| Elliott et al. [23] | United Kingdom | Longitudinal Cohort Study. The study included consecutive patients attending the Newcastle Tertiary Liver Clinic with a histological diagnosis of NAFLD. In total, 224 NAFLD patients and 107 alcoholic liver disease (ALD) patients returned the assessment tools for analysis. | The study utilized validated functional, cognitive, autonomic, and fatigue symptom assessment tools completed by the patients. | Both NAFLD and ALD patients demonstrated significant functional difficulties that were worse than those of the control group. The functional impairment affected activities of daily living and persisted over the 3-year follow-up period. No significant difference in functional difficulty was observed between precirrhotic and cirrhotic participants. |
| Takahashi et al. [43] | Japan | Cross-Sectional Study. 24 female NAFLD patients without psychiatric disorders, including depression, and 15 age-adjusted healthy females | NIRS | NAFLD subjects had lower mean oxygenated-Hb concentration at baseline and during the fluency task, especially in the frontal lobes, and decreased brain activity reflected by poor cerebral oxygen reactivity and reduced word production. |
| Kang et al. [36] | South Korea | Cross-Sectional Study. The study included 4400 participants, of which 1415 (32.2%) had NAFLD based on the Fatty Liver Index (FLI) ≥ 30. | MMSE | Among the patients with NAFL, 666 (15.1%) participants had Mini-Mental Status Examination (MMSE) scores of <24, which was defined as cognitive impairment. Significant correlation between NAFLD (detected with Fatty Liver Index) and cognitive impairment after adjusting for socio-demographics, lifestyle factors, and comorbidities (OR = 1.26; 95% CI = 1.04–1.52) and in sensitivity analysis. |
| Yu et al. [35] | USA | Cross-Sectional Study. 4973 participants aged 20–59 from NHANES. | SDLT, SRTT, SDST | Subjects with NAFLD and metabolic dysfunctions (MD), but not NAFLD subjects without MD, were significantly predisposed to develop cognitive impairment, particularly in visual–motor speed tasks and response time. MAFLD independently associated with cognitive function, highlighting NAFLD’s systemic impact on lipid metabolism and chronic low-grade inflammation. |
| Cushman et al. [34] | USA | Nested Case-Control Study. 17,630 participants; 495 cases, 587 controls. | Six-item screener, animal fluency, word list learning, and recall | Significant association between cognitive impairment and NAFLD, suggesting NAFLD is a key risk factor for cognitive dysfunction. |
| Weinstein et al. [46] | United States | Cross-Sectional Study. 5660 NAFLD subjects with brain MRI. | Brain MRI | Detected lower total brain and grey-matter volumes in NAFLD subjects, significant even after demographic and clinical factors correction. Supporting the possible association between liver disease and brain aging. |
| Miao et al. [45] | China | Cross-Sectional Study. 225 participants, 70 with fMRI. | fMRI, cognitive tests | Significant correlation between NAFLD and poor memory performance, hippocampal volume loss, and functional brain-imaging alterations in NAFLD subjects. |
| Xu et al. [47] | China | Cross-Sectional Study. 44 NAFLD subjects, 20 healthy controls. | MoCA, DST, TMT-A, resting-state fMRI | NAFLD subjects had inferior cognitive performance, and nonobese NAFLD patients had abnormal functional connectivity in various brain regions. |
| An et al. [48] | USA | Cross-sectional cohort of 23 NAFLD patients | RBANS (Repeatable Battery for the Assessment of Neuropsychological Status, exploring immediate and delayed memory, attention, language, and visuospatial memory) | Association between high levels of CTRP13 (tumor necrosis factor-related proteins involved in metabolic regulations and obesity) and poor cognitive performance, especially in visuospatial memory, in NAFLD subjects. |
| Weinstein et al. [28] | United States | Cross-Sectional (Framingham Heart Study). 1287 participants (mean age = 61 ± 12 years, 48% men), of whom 378 (29%) had nonalcoholic fatty liver disease (NAFLD). | Standardized neuropsychological test battery including the Wechsler Memory Scale, Trail-making Test, Similarities test (SIM), and the Hooper Visual Organization Test (HVOT) | The presence of NAFLD was not associated with cognitive function. However, NAFLD with high risk for advanced fibrosis was associated with poorer performance on the similarities test and trail-making test (specifically the difference in time between Trail-making B and A), indicating a potential link between liver fibrosis severity and reduced cognitive function in executive function and abstract reasoning. |
| Weinstein et al. [44] | United States | Cross-Sectional Study (Framingham Heart Study). 766 participants (53.5% women, mean age = 67 years), of whom 137 (17.9%) had nonalcoholic fatty liver disease (NAFLD). | Brain MRI measures include total cerebral brain volume, hippocampal and white matter hyperintensity volumes, and presence or absence of covert brain infarcts. | NAFLD was significantly associated with smaller total cerebral brain volume (β [SE] −0.26 [0.11]; p = 0.02), corresponding to an accelerated brain aging of 4.2 years in the general sample and up to 7.3 years in individuals younger than 60 years. No significant associations were found between NAFLD and other MRI measures like hippocampal volume, white matter hyperintensity volume, or covert brain infarcts. |
| Dementia | ||||
| Shang et al. [37] | Sweden | Longitudinal Cohort Study. 2898 patients with NAFLD aged 65 y or older; 28,357 controls. | Not Reported | Significant association between NAFLD and dementia, with an HR of 1.86 for developing dementia in NAFLD patients, which weakened after adjustment for comorbidities. Enhanced association if cardiovascular comorbidities. |
| Jeong et al. [38] | Korea | Longitudinal Study. 608,994 adults aged ≥60 years. | Not Reported | 8% developed dementia and 7.7% developed Alzheimer’s disease (AD), with a significant association between NAFLD and increased risk of incident dementia, particularly AD. |
| Weinstein et al. [52] | FHS | Cross-Sectional Study. Based on a subsample of 169 NAFLD subjects from the Framingham Heart Study. | β-amiloyd or tau deposition on PET | Prevalent NAFLD was not associated with β-amyloid or tau onPET. FIB-4 was significantly associated with increased rhinal tau (β = 1.03 ± 0.33, p = 0.002). FIB-4 was related to inferior temporal, parahippocampal gyrus, entorhinal, and rhinal tau and to β-amyloid deposition overall and in the inferior temporal and parahippocampal regions. |
| Solfrizzi et al. [39] | Italy | Longitudinal Study. 1061 older adults with NAFLD aged 65 to 84 years. The focus was on assessing the risk of dementia over an 8-year follow-up period. | Not Reported | Higher fibrosis score in NAFLD patients was associated with an increased overall risk of dementia, HR of 4.23. |
| Moretti et al. [40] | Italy | Cross-Sectional Study. 319 adult patients diagnosed with subcortical vascular dementia (sVaD). | Frontal Assessment Battery (FAB), Hamilton Anxiety Rating Scale (HAM-A), Apathy Evaluation Score (AES-C), Neuropsychiatric Inventory (NPI), and Quality of Life in Dementia Scale (QUALID). Additionally, clinical and biochemical parameters, including liver enzymes and ultrasound for NAFLD assessment, were utilized. | Patients with comorbid NAFLD and sVaD had worse neuropsychological outcomes, including higher scores in HAM-A (indicating anxiety), AES-C (indicating apathy), and NPI (indicating neuropsychiatric symptoms), and a lower FAB score (indicating poorer executive function). These patients also had a worse metabolic profile, characterized by higher levels of homocysteine and deficiencies in vitamins B12, D, and folate. |
| Wang et al. [41] | China | Population-based cross-sectional study including 5129 participants (aged ≥60 years; 61.79% women) living in rural communities. | Diagnosis of dementia, Alzheimer’s disease (AD), and vascular dementia (VaD) following international criteria. | Out of 5129 participants, 455 (8.87%) had moderate-to-severe NAFLD. Dementia was diagnosed in 292 participants (5.69%), including 188 with AD and 96 with VaD. The study found that moderate-to-severe NAFLD (compared to no-to-mild NAFLD) had odds ratios of 2.22 for all-cause dementia, 1.88 for AD, and 2.62 for VaD. Additionally, in the cytokine subsample, moderate-to-severe NAFLD was significantly associated with higher levels of certain serum cytokines, such as interleukin-6, which mediated 12.56% of the association between NAFLD and VaD. |
| Authors | Location |
Study Type and
Patient Sample | Test Used | Findings |
|---|---|---|---|---|
| Gerber et al. [58] | United States | Longitudinal Cohort Study (CARDIA). Participants included 2809 middle-aged adults (average age 50.1 years, 57% female, 48% black) with CT examination and cognitive assessment at Year 25 (Y25, 2010–2011) and reassessed at Year 30 (Y30, 2015–2016). | DDST, RAVLT | The study found that NAFLD was inversely associated with cognitive scores at baseline, but after adjustment for cardiovascular disease (CVD) risk factors, no associations were shown between NAFLD and cognitive scores. Similarly, no associations were observed with 5-year cognitive decline. The study concluded that inverse associations between NAFLD and cognitive scores among middle-aged adults were attenuated after adjustment for CVD risk factors, with the latter being predictive of poorer cognitive performance both at baseline and follow-up. |
| Shang et al. [61] | Sweden | Retrospective matched cohort study. 656 patients with biopsy-proven NAFLD and 6436 matched controls from the general population. | Dementia incidence was ascertained using National registers | There was no significant association between NAFLD and the incidence of dementia. However, adding histological markers, particularly fibrosis stage, to a conventional risk model for dementia did enhance its predictive capacity. This suggests a potential shared metabolic origin between NAFLD and dementia. |
| Basu et al. [59] | United States | Post hoc analyses of data from two randomized controlled trials (ACCORD and SPRINT studies). The ACCORD trial included 2969 diabetic participants with a mean age of 62 years, and the SPRINT trial included 2890 hypertensive participants with a mean age of 68 years. | Cognitive function tests (Mini-Mental Status Examination, Digital Symbol Substitution Test, Stroop Color–Word Test, Rey Auditory Verbal Learning Test) and brain magnetic resonance imaging volume measurements. | The study found no consistent associations between liver disease and cognitive performance or brain volumes at baseline or longitudinally after adjustment in both the ACCORD and SPRINT populations. The study concluded that markers of chronic liver disease were not associated with cognitive impairment or related brain-imaging markers among individuals with diabetes and hypertension. |
| Xiao et al. [63] | Netherlands | Longitudinal and cross-sectional analyses within the Rotterdam Study. Participants included three different sets: Set 1 (3975 participants aged 70 years, follow-up 15.5 years), Set 2 (4577 participants aged 69.9 years, follow-up 5.7 years), and Set 3 (3300 participants aged 67.6 years, follow-up 5.6 years). | Dementia diagnosis according to the DSM-III-R criteria, cognitive function assessment using neuropsychological tests (Stroop test, Letter Digit Substitution Test, Word Fluency Test, 15-Word Learning Test, and Purdue Pegboard Test). | NAFLD and fibrosis were not consistently associated with an increased risk for dementia or worse cognitive function in fully adjusted models. Interestingly, NAFLD was associated with a significantly decreased risk for incident dementia until 5 years after Fatty Liver Index assessment. The study concluded that NAFLD and fibrosis were not linked to increased dementia risk, nor was NAFLD associated with impaired cognitive function. |
| Felipo et al. [64] | Spain | The study included patients with different liver or dermatological diseases, assessing the presence of mild cognitive impairment. The groups included patients with liver cirrhosis (n = 35), NAFLD (n = 11), NASH (n = 11), psoriasis (n = 20), and keloids (n = 22). | PHES [comprises the Digit Symbol Test (DST), the Number Connection Test A and B (NCT-A and NCT-B), the Serial Dotting Test (SD), and the Line Tracing Test (LTT)] | The study found that 5/11 of patients with NASH had mild cognitive impairment (MCI), thus presenting a minimal hepatic encephalopathy, while cognitive functions were not affected in patients with only NAFLD Hyperammonemia or inflammation alone did not induce cognitive impairment. However, the combination of certain levels of hyperammonemia and inflammation was enough to induce cognitive impairment, even in the absence of liver disease. |
| Wernberg et al. [64] | Denmark | Cross-sectional study. The study included 180 patients undergoing evaluation for bariatric surgery with a body mass index of 35 kg/m2. Of these, 72% were women, the average age was 46 ± 12 years, 78% had NAFLD, and 30% had NASH without cirrhosis. | Continuous Reaction Time Test, Portosystemic Encephalopathy Syndrome Test, and the Stroop Test. A representative subgroup also underwent RBANS. The triggering receptor expressed on myeloid cells 2 (TREM2) was used as a biomarker for neuronal damage. | 8% of the patients were cognitively impaired according to the basic tests, and 41% showed cognitive impairment based on RBANS results. The most affected cognitive functions were executive and short-term memory. The study found no associations between cognitive impairment and BMI, NAFLD presence or severity, or metabolic comorbidities. However, male sex and the use of two or more psychoactive medications were associated with cognitive impairment. TREM2 levels were not associated with cognitive impairment. |
| Huang et al. [56] | United Kingdom | Prospective analysis of 179,222 UK Biobank participants. NAFLD was diagnosed based on the Fatty Liver Index. | Cox proportional hazards models were used to estimate the adjusted hazard ratio (HR) and 95% confidence interval (CI) for incidence. | During a median follow-up of 12.4 years, 4950 incident dementia cases were identified, including 2318 Alzheimer’s disease (AD) cases and 1135 vascular dementia (VD) cases. There was no significant association between NAFLD and the risks of all-cause dementia (HR: 0.97, 95% CI: 0.90–1.06), AD (HR: 0.95, 95% CI: 0.84–1.07), or VD (HR: 1.03, 95% CI: 0.88–1.22). The meta-analysis of prospective studies, which included 879,749 subjects, also found no significant association between NAFLD and incident dementia, with a pooled HR for all-cause dementia of 1.01 (95% CI: 0.94–1.08) and for VD of 0.99 (95% CI: 0.86–1.13). The study concluded that there was no evidence of an association between NAFLD and incident dementia. |
| Labenz et al. [62] | Germany | Population-based cohort study. Elderly patients (≥65 years) with NAFLD, total of 44,634 patients (22,317 with NAFLD and 22,317 without NAFLD) from 1262 general practices in Germany. | Analysis based on ICD-10 coding in the Disease Analyzer Database. Primary outcomes were all-cause dementia diagnoses, incidence of vascular dementia, and antidementive drug prescription. | Over 10 years, 16.0% of patients with NAFLD and 15.6% without NAFLD were diagnosed with dementia. The study found no association between NAFLD and the incidence of all-cause dementia (HR 0.97, 95% CI 0.92–1.04), vascular dementia (HR 0.89, 95% CI 0.78–1.02), or the new prescription of antidementive therapy (HR 0.87, 95% CI 0.76–1.01). |
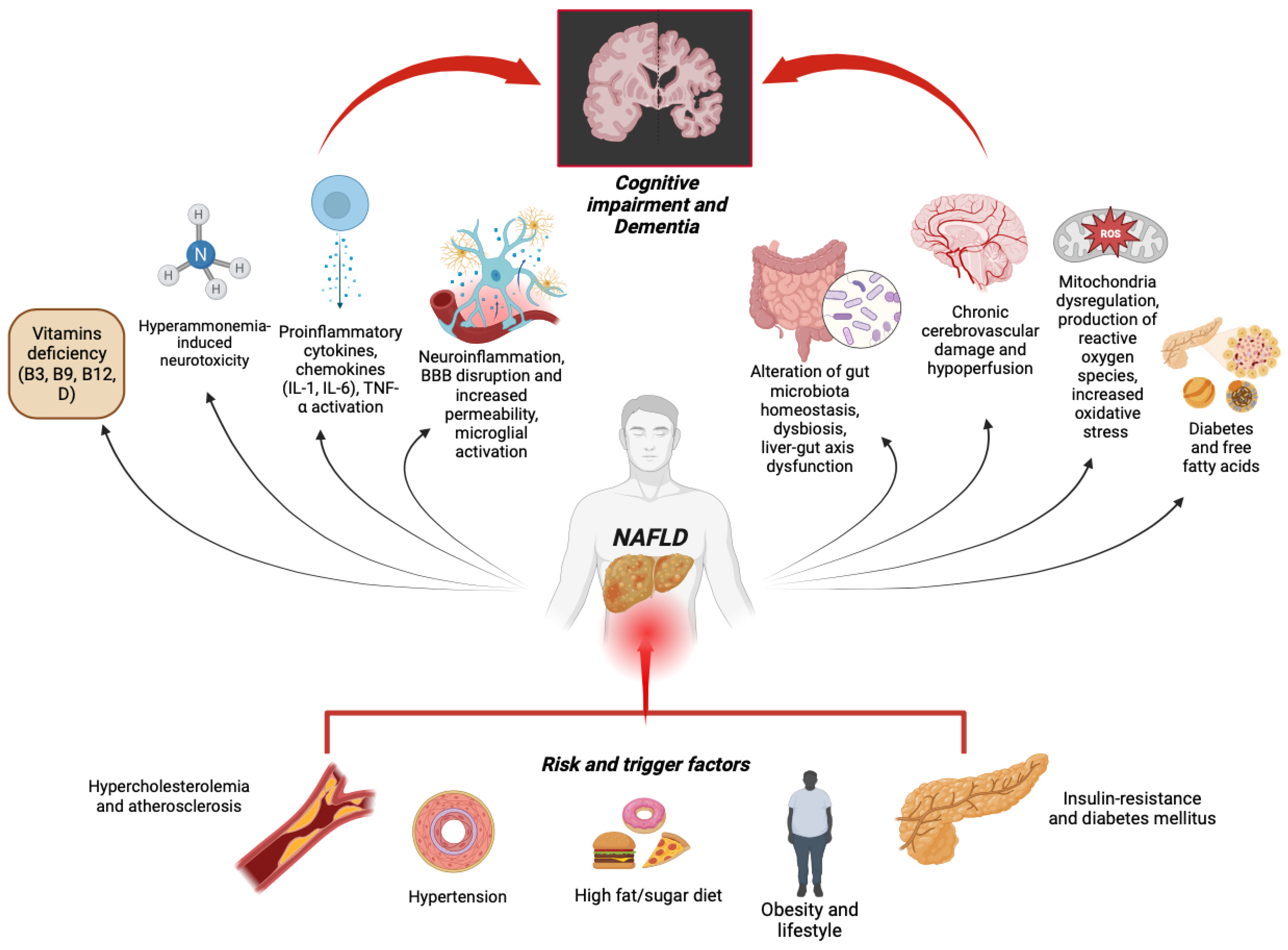
3. Molecular Evidence
3.1. Insulin Resistance and Diabetes-Promoted Neurodegeneration
3.2. Systemic Inflammation
3.3. Neuroinflammation
3.4. Gut–Liver–Brain Axis
3.5. Hyperammonemia-Induced Neurotoxicity
3.6. Free Fatty Acids
3.7. Vitamin Deficiency
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Estes, C.; Anstee, Q.M.; Arias-Loste, M.T.; Bantel, H.; Bellentani, S.; Caballeria, J.; Colombo, M.; Craxi, A.; Crespo, J.; Day, C.P.; et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016–2030. J. Hepatol. 2018, 69, 896–904. [Google Scholar] [CrossRef]
- George, E.S.; Sood, S.; Daly, R.M.; Tan, S.-Y. Is there an association between non-alcoholic fatty liver disease and cognitive function? A systematic review. BMC Geriatr. 2022, 22, 47. [Google Scholar] [CrossRef]
- Spiers, J.; Brindley, J.H.; Li, W.; Alazawi, W. What’s new in non-alcoholic fatty liver disease? Frontline Gastroenterol. 2022, 13, e102–e108. [Google Scholar] [CrossRef] [PubMed]
- Abeysekera, K.W.M.; Fernandes, G.S.; Hammerton, G.; Portal, A.J.; Gordon, F.H.; Heron, J.; Hickman, M. Prevalence of steatosis and fibrosis in young adults in the UK: A population-based study. Lancet Gastroenterol. Hepatol. 2020, 5, 295–305. [Google Scholar] [CrossRef]
- Alexander, M.; Loomis, A.K.; van der Lei, J.; Duarte-Salles, T.; Prieto-Alhambra, D.; Ansell, D.; Pasqua, A.; Lapi, F.; Rijnbeek, P.; Mosseveld, M.; et al. Risks and clinical predictors of cirrhosis and hepatocellular carcinoma diagnoses in adults with diagnosed NAFLD: Real-world study of 18 million patients in four European cohorts. BMC Med. 2019, 17, 95. [Google Scholar] [CrossRef]
- A Adams, L.; Roberts, S.K.; I Strasser, S.; E Mahady, S.; Powell, E.; Estes, C.; Razavi, H.; George, J. Nonalcoholic fatty liver disease burden: Australia, 2019–2030. J. Gastroenterol. Hepatol. 2020, 35, 1628–1635. [Google Scholar] [CrossRef]
- Trovato, F.M.; Castrogiovanni, P.; Malatino, L.; Musumeci, G. Nonalcoholic fatty liver disease (NAFLD) prevention: Role of Mediterranean diet and physical activity. Hepatobiliary Surg. Nutr. 2019, 8, 167–169. [Google Scholar] [CrossRef] [PubMed]
- Browning, J.D.; Szczepaniak, L.S.; Dobbins, R.; Nuremberg, P.; Horton, J.D.; Cohen, J.C.; Grundy, S.M.; Hobbs, H.H. Prevalence of hepatic steatosis in an urban population in the United States: Impact of ethnicity. Hepatology 2004, 40, 1387–1395. [Google Scholar] [CrossRef] [PubMed]
- Hassani Zadeh, S.; Mansoori, A.; Hosseinzadeh, M. Relationship between dietary patterns and non-alcoholic fatty liver disease: A systematic review and meta-analysis. J. Gastroenterol. Hepatol. 2021, 36, 1470–1478. [Google Scholar] [CrossRef]
- Kim, D.; Konyn, P.; Sandhu, K.K.; Dennis, B.B.; Cheung, A.C.; Ahmed, A. Metabolic dysfunction-associated fatty liver disease is associated with increased all-cause mortality in the United States. J. Hepatol. 2021, 75, 1284–1291. [Google Scholar] [CrossRef]
- Colognesi, M.; Gabbia, D.; de Martin, S. Depression and Cognitive Impairment-Extrahepatic Manifestations of NAFLD and NASH. Biomedicines 2020, 8, 229. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, Y.; Ozdogan, O. Liver disease as a risk factor for cognitive decline and dementia: An under-recognized issue. Hepatology 2009, 49, 698. [Google Scholar] [CrossRef] [PubMed]
- Bertolotti, M.; Lonardo, A.; Mussi, C.; Baldelli, E.; Pellegrini, E.; Ballestri, S.; Romagnoli, D.; Loria, P. Nonalcoholic fatty liver disease and aging: Epidemiology to management. World J. Gastroenterol. 2014, 20, 14185–14204. [Google Scholar] [CrossRef] [PubMed]
- GBD 2016 Dementia Collaborators. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016, a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 88–106. [Google Scholar] [CrossRef] [PubMed]
- Mavrodaris, A.; Powell, J.; Thorogood, M. Prevalences of dementia and cognitive impairment among older people in sub-Saharan Africa: A systematic review. Bull. World Health Organ. 2013, 91, 773–783. [Google Scholar] [CrossRef] [PubMed]
- Collie, A. Cognition in liver disease. Liver Int. 2005, 25, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Brodersen, C.; Koen, E.; Ponte, A.; Sánchez, S.; Segal, E.; Chiapella, A.; Fernández, M.; Torres, M.; Tripodi, V.; Lemberg, A. Cognitive function in patients with alcoholic and nonalcoholic chronic liver disease. J. Neuropsychiatry Clin. Neurosci. 2014, 26, 241–248. [Google Scholar] [CrossRef]
- Bajaj, J.S.; Wade, J.B.; Sanyal, A.J. Spectrum of neurocognitive impairment in cirrhosis: Implications for the assessment of hepatic encephalopathy. Hepatology 2009, 50, 2014–2021. [Google Scholar] [CrossRef]
- MacLin, J.M.A.; Wang, T.; Xiao, S. Biomarkers for the diagnosis of Alzheimer’s disease, dementia Lewy body, frontotemporal dementia and vascular dementia. Gen. Psychiatr. 2019, 32, 54. [Google Scholar] [CrossRef]
- Bai, W.; Chen, P.; Cai, H.; Zhang, Q.; Su, Z.; Cheung, T.; Jackson, T.; Sha, S.; Xiang, Y.-T. Worldwide prevalence of mild cognitive impairment among community dwellers aged 50 years and older: A meta-analysis and systematic review of epidemiology studies. Age Ageing 2022, 51, afac173. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Shiri-Feshki, M. Rate of progression of mild cognitive impairment to dementia--meta-analysis of 41 robust inception cohort studies. Acta Psychiatr. Scand. 2009, 119, 252–265. [Google Scholar] [CrossRef]
- Livingston, G.; Sommerlad, A.; Orgeta, V.; Costafreda, S.G.; Huntley, J.; Ames, D.; Ballard, C.; Banerjee, S.; Burns, A.; Cohen-Mansfield, J.; et al. Dementia prevention, intervention, and care. Lancet 2017, 390, 2673–2734. [Google Scholar] [CrossRef]
- Elliott, C.; Frith, J.; Day, C.P.; Jones, D.E.J.; Newton, J.L. Functional Impairment in Alcoholic Liver Disease and Non-alcoholic Fatty Liver Disease Is Significant and Persists over 3 Years of Follow-Up. Dig. Dis. Sci. 2013, 58, 2383–2391. [Google Scholar] [CrossRef]
- Doward, L.C.; Balp, M.-M.; Twiss, J.; Slota, C.; Cryer, D.; Brass, C.A.; Anstee, Q.M.; Sanyal, A.J. Development of a Patient-Reported Outcome Measure for Non-Alcoholic Steatohepatitis (NASH-CHECK): Results of a Qualitative Study. Patient Patient-Centered Outcomes Res. 2021, 14, 533–543. [Google Scholar] [CrossRef]
- Kjærgaard, K.; Mikkelsen, A.C.D.; Wernberg, C.W.; Grønkjær, L.L.; Eriksen, P.L.; Damholdt, M.F.; Mookerjee, R.P.; Vilstrup, H.; Lauridsen, M.M.; Thomsen, K.L. Cognitive Dysfunction in Non-Alcoholic Fatty Liver Disease—Current Knowledge, Mechanisms and Perspectives. J. Clin. Med. 2021, 10, 673. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, A.A.; de Avila, L.; Paik, J.; Golabi, P.; Escheik, C.; Gerber, L.; Younossi, Z.M. Cognitive Performance in Individuals With Non-Alcoholic Fatty Liver Disease and/or Type 2 Diabetes Mellitus. Psychosomatics 2018, 59, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Staugaard, B.; Hansen, J.F.; Mössner, B.K.; Madsen, B.S.; Krag, A.; Christensen, P.B.; Thiele, M. Poster Session 2, Advances in Imaging and Noninvasive Markers of Fibrosis; Bile Acids, Cholangiocyte Biology, and Experimental Cholestasis. Hepatology 2015, 62, 594A–624A. [Google Scholar]
- Weinstein, G.; Davis-Plourde, K.; Himali, J.J.; Zelber-Sagi, S.; Beiser, A.S.; Seshadri, S. Non-alcoholic fatty liver disease, liver fibrosis score and cognitive function in middle-aged adults: The Framingham Study. Liver Int. 2019, 39, 1713–1721. [Google Scholar] [CrossRef]
- Petta, S.; Tuttolomondo, A.; Gagliardo, C.; Zafonte, R.; Brancatelli, G.; Cabibi, D.; Cammà, C.; Di Marco, V.; Galvano, L.; La Tona, G.; et al. The Presence of White Matter Lesions Is Associated With the Fibrosis Severity of Nonalcoholic Fatty Liver Disease. Medicine 2016, 95, e3446. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Liu, C.; Hu, F.; Deng, X.; Zhang, Y. Non-alcoholic Fatty Liver Disease and Longitudinal Cognitive Changes in Middle-Aged and Elderly Adults. Front. Med. 2022, 8, 2642. [Google Scholar] [CrossRef] [PubMed]
- Seo, S.W.; Gottesman, R.F.; Clark, J.M.; Hernaez, R.; Chang, Y.; Kim, C.; Ha, K.H.; Guallar, E.; Lazo, M. Nonalcoholic fatty liver disease is associated with cognitive function in adults. Neurology 2016, 86, 1136–1142. [Google Scholar] [CrossRef] [PubMed]
- Filipović, B.; Marković, O.; Đurić, V.; Filipović, B. Cognitive Changes and Brain Volume Reduction in Patients with Nonalcoholic Fatty Liver Disease. Can. J. Gastroenterol. Hepatol. 2018, 2018, 2097435. [Google Scholar] [CrossRef] [PubMed]
- Celikbilek, A.; Celikbilek, M.; Bozkurt, G. Cognitive assessment of patients with nonalcoholic fatty liver disease. Eur. J. Gastroenterol. Hepatol. 2018, 30, 944–950. [Google Scholar] [CrossRef] [PubMed]
- Cushman, M.; Callas, P.W.; Alexander, K.S.; Wadley, V.; Zakai, N.A.; Lidofsky, S.D.; Unverzagt, F.W.; Judd, S.E. Nonalcoholic fatty liver disease and cognitive impairment: A prospective cohort study. PLoS ONE 2023, 18, e0282633. [Google Scholar] [CrossRef] [PubMed]
- Yu, Q.; He, R.; Jiang, H.; Wu, J.; Xi, Z.; He, K.; Liu, Y.; Zhou, T.; Feng, M.; Wan, P.; et al. Association between Metabolic Dysfunction-associated Fatty Liver Disease and Cognitive Impairment. J. Clin. Transl. Hepatol. 2022, 10, 1034–1041. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Kim, E.; Cho, H.; Kim, D.J.; Kim, H.C.; Jung, S.J. Associations between non-alcoholic fatty liver disease and cognitive impairment and the effect modification of inflammation. Sci. Rep. 2022, 12, 12614. [Google Scholar] [CrossRef]
- Shang, Y.; Widman, L.; Hagström, H. Nonalcoholic Fatty Liver Disease and Risk of Dementia. Neurology 2022, 99, e574–e582. [Google Scholar] [CrossRef]
- Jeong, S.; Oh, Y.H.; Choi, S.; Chang, J.; Kim, S.M.; Son, J.S.; Lee, G.; Ahn, J.C.; Lee, D.H.; Koo, B.K.; et al. Association of non-alcoholic fatty liver disease with incident dementia later in life among elder adults. Clin. Mol. Hepatol. 2022, 28, 510–521. [Google Scholar] [CrossRef]
- Solfrizzi, V.; Scafato, E.; Custodero, C.; Loparco, F.; Ciavarella, A.; Panza, F.; Seripa, D.; Imbimbo, B.P.; Lozupone, M.; Napoli, N.; et al. Liver fibrosis score, physical frailty, and the risk of dementia in older adults: The Italian Longitudinal Study on Aging. Alzheimers Dement. 2020, 6, e12065. [Google Scholar] [CrossRef]
- Moretti, R.; Giuffré, M.; Crocè, L.S.; Gazzin, S.; Tiribelli, C. Nonalcoholic Fatty Liver Disease and Altered Neuropsychological Functions in Patients with Subcortical Vascular Dementia. J. Pers. Med. 2022, 12, 1106. [Google Scholar] [CrossRef]
- Wang, Y.; Li, Y.; Liu, K.; Han, X.; Dong, Y.; Wang, X.; Wang, M.; Cong, L.; Zhang, Q.; Tang, S.; et al. Nonalcoholic fatty liver disease, serum cytokines, and dementia among rural-dwelling older adults in China: A population-based study. Eur. J. Neurol. 2022, 29, 2612–2621. [Google Scholar] [CrossRef]
- Tuttolomondo, A.; Petta, S.; Casuccio, A.; Maida, C.; Della Corte, V.; Daidone, M.; Di Raimondo, D.; Pecoraro, R.; Fonte, R.; Cirrincione, A.; et al. Reactive hyperemia index (RHI) and cognitive performance indexes are associated with histologic markers of liver disease in subjects with non-alcoholic fatty liver disease (NAFLD): A case control study. Cardiovasc. Diabetol. 2018, 17, 28. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, A.; Kono, S.; Wada, A.; Oshima, S.; Abe, K.; Imaizumi, H.; Fujita, M.; Hayashi, M.; Okai, K.; Miura, I.; et al. Reduced brain activity in female patients with non-alcoholic fatty liver disease as measured by near-infrared spectroscopy. PLoS ONE 2017, 12, e0174169. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, G.; Zelber-Sagi, S.; Preis, S.R.; Beiser, A.S.; DeCarli, C.; Speliotes, E.K.; Satizabal, C.L.; Vasan, R.S.; Seshadri, S. Association of Nonalcoholic Fatty Liver Disease With Lower Brain Volume in Healthy Middle-aged Adults in the Framingham Study. JAMA Neurol. 2018, 75, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Miao, Y.; Zhang, B.; Sun, X.; Ma, X.; Fang, D.; Zhang, W.; Wu, T.; Xu, X.; Yu, C.; Hou, Y. The Presence and Severity of NAFLD are Associated With Cognitive Impairment and Hippocampal Damage. J. Clin. Endocrinol. Metab. 2023, 108, 3239–3249. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, G.; O’Donnell, A.; Frenzel, S.; Xiao, T.; Yaqub, A.; Yilmaz, P.; de Knegt, R.J.; Maestre, G.E.; van Lent, D.M.; Long, M.; et al. Nonalcoholic fatty liver disease, liver fibrosis, and structural brain imaging: The Cross-Cohort Collaboration. Eur. J. Neurol. 2024, 31, e16048. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.-L.; Gu, J.-P.; Wang, L.-Y.; Zhu, Q.-R.; You, N.-N.; Li, J.; Shi, J.-P. Aberrant Spontaneous Brain Activity and its Association with Cognitive Function in Non-Obese Nonalcoholic Fatty Liver Disease: A Resting-State fMRI Study. J. Integr. Neurosci. 2023, 22, 8. [Google Scholar] [CrossRef]
- An, K.; Starkweather, A.; Sturgill, J.; Salyer, J.; Sterling, R.K. Association of CTRP13 With Liver Enzymes and Cognitive Symptoms in Nonalcoholic Fatty Liver Disease. Nurs. Res. 2019, 68, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Karbalaei, R.; Allahyari, M.; Rezaei-Tavirani, M.; Asadzadeh-Aghdaei, H.; Zali, M.R. Protein-protein interaction analysis of Alzheimer`s disease and NAFLD based on systems biology methods unhide common ancestor pathways. Gastroenterol. Hepatol. Bed. Bench. 2018, 11, 27. [Google Scholar]
- Kim, D.-G.; Krenz, A.; Toussaint, L.E.; Maurer, K.J.; Robinson, S.-A.; Yan, A.; Torres, L.; Bynoe, M.S. Non-alcoholic fatty liver disease induces signs of Alzheimer’s disease (AD) in wild-type mice and accelerates pathological signs of AD in an AD model. J. Neuroinflammation 2016, 13, 1. [Google Scholar] [CrossRef]
- Nho, K.; Kueider-Paisley, A.; Ahmad, S.; MahmoudianDehkordi, S.; Arnold, M.; Risacher, S.L.; Louie, G.; Blach, C.; Baillie, R.; Han, X.; et al. Association of Altered Liver Enzymes With Alzheimer Disease Diagnosis, Cognition, Neuroimaging Measures, and Cerebrospinal Fluid Biomarkers. JAMA Netw. Open 2019, 2, e197978. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, G.; O’Donnell, A.; Davis-Plourde, K.; Zelber-Sagi, S.; Ghosh, S.; DeCarli, C.S.; Seshadri, S. Non-Alcoholic Fatty Liver Disease, Liver Fibrosis, and Regional Amyloid-β and Tau Pathology in Middle-Aged Adults: The Framingham Study. J. Alzheimers Dis. 2022, 86, 1371–1383. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Sang, B.; Zheng, Z. Risk of dementia or cognitive impairment in non-alcoholic fatty liver disease: A systematic review and meta-analysis. Front. Aging Neurosci. 2022, 14, 985109. [Google Scholar] [CrossRef] [PubMed]
- Cheon, S.Y.; Song, J. Novel insights into non-alcoholic fatty liver disease and dementia: Insulin resistance, hyperammonemia, gut dysbiosis, vascular impairment, and inflammation. Cell Biosci. 2022, 12, 99. [Google Scholar] [CrossRef] [PubMed]
- Han, E.; Lee, J.-Y.; Han, K.-D.; Cho, H.; Kim, K.J.; Lee, B.-W.; Kang, E.S.; Cha, B.-S.; Younossi, Z.M.; Lee, Y.-H. Gamma glutamyltransferase and risk of dementia in prediabetes and diabetes. Sci. Rep. 2020, 10, 6800. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Zeng, M.; Wang, Z.; Qin, F.; Chen, J.; He, Z. Dietary Polyphenols to Combat Nonalcoholic Fatty Liver Disease via the Gut–Brain–Liver Axis: A Review of Possible Mechanisms. J. Agric. Food Chem. 2021, 69, 3585–3600. [Google Scholar] [CrossRef] [PubMed]
- VanWagner, L.B.; Terry, J.G.; Chow, L.S.; Alman, A.C.; Kang, H.; Ingram, K.H.; Jeffrey Carr, J. Nonalcoholic fatty liver disease and measures of early brain health in middle-aged adults: The CARDIA study. Obesity 2017, 25, 642–651. [Google Scholar] [CrossRef] [PubMed]
- Gerber, Y.; VanWagner, L.B.; Yaffe, K.; Terry, J.G.; Rana, J.S.; Reis, J.P.; Sidney, S. Non-alcoholic fatty liver disease and cognitive function in middle-aged adults: The CARDIA study. BMC Gastroenterol. 2021, 21, 96. [Google Scholar] [CrossRef]
- Basu, E.; Mehta, M.; Zhang, C.; Zhao, C.; Rosenblatt, R.; Tapper, E.B.; Parikh, N.S. Association of chronic liver disease with cognition and brain volumes in two randomized controlled trial populations. J. Neurol. Sci. 2022, 434, 120117. [Google Scholar] [CrossRef]
- Felipo, V.; Urios, A.; Montesinos, E.; Molina, I.; Garcia-Torres, M.L.; Civera, M.; Montoliu, C. Contribution of hyperammonemia and inflammatory factors to cognitive impairment in minimal hepatic encephalopathy. Metab. Brain Dis. 2012, 27, 51–58. [Google Scholar] [CrossRef]
- Shang, Y.; Nasr, P.; Ekstedt, M.; Widman, L.; Stål, P.; Hultcrantz, R.; Kechagias, S.; Hagström, H. Non-alcoholic fatty liver disease does not increase dementia risk although histology data might improve risk prediction. JHEP Rep. 2021, 3, 100218. [Google Scholar] [CrossRef] [PubMed]
- Labenz, C.; Kostev, K.; Kaps, L.; Galle, P.R.; Schattenberg, J.M. Incident Dementia in Elderly Patients with Nonalcoholic Fatty Liver Disease in Germany. Dig. Dis. Sci. 2021, 66, 3179–3185. [Google Scholar] [CrossRef] [PubMed]
- Xiao, T.; van Kleef, L.A.; Ikram, M.K.; de Knegt, R.J.; Ikram, M.A. Association of Nonalcoholic Fatty Liver Disease and Fibrosis With Incident Dementia and Cognition: The Rotterdam Study. Neurology 2022, 99, E565–E573. [Google Scholar] [CrossRef]
- Wernberg, C.W.; Grønkjær, L.L.; Jacobsen, B.G.; Chandran, V.I.; Krag, A.; Graversen, J.H.; Weissenborn, K.; Vilstrup, H.; Lauridsen, M.M. The prevalence and risk factors for cognitive impairment in obesity and NAFLD. Hepatol. Commun. 2023, 7, e00203. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Liu, Z.; Xie, J.; Xu, C. NAFLD does not increase the risk of incident dementia: A prospective study and meta-analysis. J. Psychiatr. Res. 2023, 161, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Scherer, T.; Sakamoto, K.; Buettner, C. Brain insulin signalling in metabolic homeostasis and disease. Nat. Rev. Endocrinol. 2021, 17, 468–483. [Google Scholar] [CrossRef]
- Li, M.; Zhang, S.; Wu, Y.; Ye, J.; Cao, X.; Liu, J.; Sun, Y.; Zhong, B. Prevalence of Insulin Resistance in Subjects with Nonalcoholic Fatty Liver Disease and Its Predictors in a Chinese Population. Dig. Dis. Sci. 2015, 60, 2170–2176. [Google Scholar] [CrossRef]
- Mielke, J.G.; Taghibiglou, C.; Liu, L.; Zhang, Y.; Jia, Z.; Adeli, K.; Wang, Y.T. A biochemical and functional characterization of diet-induced brain insulin resistance. J. Neurochem. 2005, 93, 1568–1578. [Google Scholar] [CrossRef]
- Sun, Y.; Ma, C.; Sun, H.; Wang, H.; Peng, W.; Zhou, Z.; Wang, H.; Pi, C.; Shi, Y.; He, X. Metabolism: A Novel Shared Link between Diabetes Mellitus and Alzheimer’s Disease. J. Diabetes Res. 2020, 2020, 4981814. [Google Scholar] [CrossRef]
- Moloney, A.M.; Griffin, R.J.; Timmons, S.; O’Connor, R.; Ravid, R.; O’Neill, C. Defects in IGF-1 receptor, insulin receptor and IRS-1/2 in Alzheimer’s disease indicate possible resistance to IGF-1 and insulin signalling. Neurobiol. Aging 2010, 31, 224–243. [Google Scholar] [CrossRef]
- Ghareeb, D.A.; Hafez, H.S.; Hussien, H.M.; Kabapy, N.F. Non-alcoholic fatty liver induces insulin resistance and metabolic disorders with development of brain damage and dysfunction. Metab. Brain Dis. 2011, 26, 253–267. [Google Scholar] [CrossRef]
- Craft, S.; Watson, G.S. Insulin and neurodegenerative disease: Shared and specific mechanisms. Lancet Neurol. 2004, 3, 169–178. [Google Scholar] [CrossRef]
- de La Monte, S.M.; Tong, M. Brain metabolic dysfunction at the core of Alzheimer’s disease. Biochem. Pharmacol. 2014, 88, 548–559. [Google Scholar] [CrossRef]
- Younossi, Z.M.; Golabi, P.; de Avila, L.; Paik, J.M.; Srishord, M.; Fukui, N.; Qiu, Y.; Burns, L.; Afendy, A.; Nader, F. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis. J. Hepatol. 2019, 71, 793–801. [Google Scholar] [CrossRef] [PubMed]
- Sajja, R.K.; Prasad, S.; Cucullo, L. Impact of altered glycaemia on blood-brain barrier endothelium: An in vitro study using the hCMEC/D3 cell line. Fluids Barriers CNS 2014, 11, 8. [Google Scholar] [CrossRef]
- Starr, J.M.; Wardlaw, J.; Ferguson, K.; MacLullich, A.; Deary, I.J.; Marshall, I. Increased blood-brain barrier permeability in type II diabetes demonstrated by gadolinium magnetic resonance imaging. J. Neurol. Neurosurg. Psychiatry 2003, 74, 70–76. [Google Scholar] [CrossRef]
- Liu, S.; Weng, R.; Gu, X.; Li, L.; Zhong, Z. Association between apolipoprotein E gene polymorphism and nonalcoholic fatty liver disease in Southern China: A case-control study. J. Clin. Lab. Anal. 2021, 35, e24061. [Google Scholar] [CrossRef]
- Rizzo, M.R.; Fasano, R.; Paolisso, G. Adiponectin and Cognitive Decline. Int. J. Mol. Sci. 2020, 21, 2010. [Google Scholar] [CrossRef] [PubMed]
- Farrell, G.C.; van Rooyen, D.; Gan, L.; Chitturi, S. NASH is an Inflammatory Disorder: Pathogenic, Prognostic and Therapeutic Implications. Gut Liver 2012, 6, 149–171. [Google Scholar] [CrossRef]
- Fricker, Z.P.; Pedley, A.; Massaro, J.M.; Vasan, R.S.; Hoffmann, U.; Benjamin, E.J.; Long, M.T. Liver Fat Is Associated With Markers of Inflammation and Oxidative Stress in Analysis of Data From the Framingham Heart Study. Clin. Gastroenterol. Hepatol. 2019, 17, 1157–1164.e4. [Google Scholar] [CrossRef] [PubMed]
- Tucker, B.; Li, H.; Long, X.; Rye, K.-A.; Ong, K.L. Fibroblast growth factor 21 in non-alcoholic fatty liver disease. Metabolism 2019, 101, 153994. [Google Scholar] [CrossRef]
- Huang, H.; Xu, C. Retinol-binding protein-4 and nonalcoholic fatty liver disease. Chin. Med. J. 2022, 135, 1182–1189. [Google Scholar] [CrossRef]
- Hong, T.; Chen, Y.; Li, X.; Lu, Y. The Role and Mechanism of Oxidative Stress and Nuclear Receptors in the Development of NAFLD. Oxid. Med. Cell. Longev. 2021, 2021, 6889533. [Google Scholar] [CrossRef]
- Haukeland, J.W.; Dahl, T.B.; Yndestad, A.; Gladhaug, I.P.; Løberg, E.M.; Haaland, T.; Konopski, Z.; Wium, C.; Aasheim, E.T.; Johansen, O.E.; et al. Fetuin A in nonalcoholic fatty liver disease: In vivo and in vitro studies. Eur. J. Endocrinol. 2012, 166, 503–510. [Google Scholar] [CrossRef]
- Nooteboom, A.; van der Linden, G.J.; Hendriks, T. Tumor necrosis factor-alpha and interleukin-1beta mediate endothelial permeability induced by lipopolysaccharide-stimulated whole blood. Crit. Care Med. 2002, 30, 2063–2068. [Google Scholar] [CrossRef]
- Zhou, X.; Cai, J.; Liu, W.; Wu, X.; Gao, C. Cysteinyl leukotriene receptor type 1 (CysLT1R) antagonist zafirlukast protects against TNF-α-induced endothelial inflammation. Biomed. Pharmacother. 2019, 111, 452–459. [Google Scholar] [CrossRef]
- Hou, X.; Yin, S.; Ren, R.; Liu, S.; Yong, L.; Liu, Y.; Wang, H. Myeloid-Cell-Specific IL-6 Signaling Promotes MicroRNA-223-Enriched Exosome Production to Attenuate NAFLD-Associated Fibrosis. Hepatology 2021, 74, 116–132. [Google Scholar] [CrossRef]
- Giraldez, M.D.; Carneros, D.; Garbers, C.; Rose-John, S.; Bustos, M. New insights into IL-6 family cytokines in metabolism, hepatology and gastroenterology. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 787–803. [Google Scholar] [CrossRef] [PubMed]
- Ding, J.-H.; Jin, Z.; Yang, X.-X.; Lou, J.; Shan, W.-X.; Hu, Y.-X.; Du, Q.; Liao, Q.-S.; Xie, R.; Xu, J.-Y. Role of gut microbiota via the gut-liver-brain axis in digestive diseases. World J. Gastroenterol. 2020, 26, 6141. [Google Scholar] [CrossRef] [PubMed]
- Jang, D.-I.; Lee, A.-H.; Shin, H.-Y.; Song, H.-R.; Park, J.-H.; Kang, T.-B.; Lee, S.-R.; Yang, S.-H. The Role of Tumor Necrosis Factor Alpha (TNF-α) in Autoimmune Disease and Current TNF-α Inhibitors in Therapeutics. Int. J. Mol. Sci. 2021, 22, 2719. [Google Scholar] [CrossRef] [PubMed]
- Tsutsui, H.; Cai, X.; Hayashi, S. Interleukin-1 Family Cytokines in Liver Diseases. Mediat. Inflamm. 2015, 2015, 630265. [Google Scholar] [CrossRef]
- Maruo, N.; Morita, I.; Shirao, M.; Murota, S. IL-6 increases endothelial permeability in vitro. Endocrinology 1992, 131, 710–714. [Google Scholar]
- Mirea, A.M.; Tack, C.J.; Chavakis, T.; Joosten, L.A.; Toonen, E.J. IL-1 family cytokine pathways underlying NAFLD: Towards new treatment strategies. Trends Mol. Med. 2018, 24, 458. [Google Scholar] [CrossRef] [PubMed]
- Larsson, P.; Ulfhammer, E.; Karlsson, L.; Bokarewa, M.; Wåhlander, K.; Jern, S. Effects of IL-1beta and IL-6 on tissue-type plasminogen activator expression in vascular endothelial cells. Thromb. Res. 2008, 123, 342–351. [Google Scholar] [CrossRef]
- Nooteboom, A.; Bleichrodt, R.P.; Hendriks, T. Modulation of endothelial monolayer permeability induced by plasma obtained from lipopolysaccharide-stimulated whole blood. Clin. Exp. Immunol. 2006, 144, 362–369. [Google Scholar] [CrossRef]
- Goumans, M.J.; ten Dijke, P. TGF-β Signaling in Control of Cardiovascular Function. Cold Spring Harb. Perspect. Biol. 2018, 10, a022210. [Google Scholar] [CrossRef]
- Paul Stroemer, R.; Rothwell, N.J. Exacerbation of ischemic brain damage by localized striatal injection of interleukin-1beta in the rat. J. Cereb. Blood Flow Metab. 1998, 18, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, J.; Dohgu, S.; Takata, F.; Machida, T.; Hatip FF, B.; Hatip-Al-Khatib, I.; Kataoka, Y. TNF-α-sensitive brain pericytes activate microglia by releasing IL-6 through cooperation between IκB-NFκB and JAK-STAT3 pathways. Brain Res. 2018, 1692, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Vegas-Suárez, S.; Simón, J.; Martínez-Chantar, M.L.; Moratalla, R. Metabolic Diffusion in Neuropathologies: The Relevance of Brain-Liver Axis. Front. Physiol. 2022, 13, 929. [Google Scholar] [CrossRef] [PubMed]
- Tsai, T.-H.; Chen, S.-L.; Xiao, X.; Chiang, Y.-H.; Tsao, Y.-P. Gene therapy of focal cerebral ischemia using defective recombinant adeno-associated virus vectors. Front. Biosci. 2006, 11, 2061–2070. [Google Scholar] [CrossRef][Green Version]
- Heyser, C.J.; Masliah, E.; Samimi, A.; Campbell, I.L.; Gold, L.H. Progressive decline in avoidance learning paralleled by inflammatory neurodegeneration in transgenic mice expressing interleukin 6 in the brain. Proc. Natl. Acad. Sci. USA 1997, 94, 1500. [Google Scholar] [CrossRef]
- Campbell, I.L.; Abraham, C.R.; Masliah, E.; Kemper, P.; Inglis, J.D.; Oldstone, M.B.; Mucke, L. Neurologic disease induced in transgenic mice by cerebral overexpression of interleukin 6. Proc. Natl. Acad. Sci. USA 1993, 90, 10061–10065. [Google Scholar] [CrossRef]
- Yang, G.-Y.; Zhao, Y.-J.; Davidson, B.L.; Betz, A. Overexpression of interleukin-1 receptor antagonist in the mouse brain reduces ischemic brain injury. Brain Res. 1997, 751, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Dove, A.; Shang, Y.; Xu, W.; Grande, G.; Laukka, E.J.; Fratiglioni, L.; Marseglia, A. The impact of diabetes on cognitive impairment and its progression to dementia. Alzheimers Dement. 2021, 17, 1769–1778. [Google Scholar] [CrossRef]
- Kinney, J.W.; Bemiller, S.M.; Murtishaw, A.S.; Leisgang, A.M.; Salazar, A.M.; Lamb, B.T. Inflammation as a central mechanism in Alzheimer’s disease. Alzheimers Dement. 2018, 4, 575–590. [Google Scholar] [CrossRef]
- Fiorillo, A.; Gallego, J.-J.; Casanova-Ferrer, F.; Giménez-Garzó, C.; Urios, A.; Ballester, M.-P.; Durbán, L.; Rios, M.-P.; Megías, J.; Miguel, T.S.; et al. Mild Cognitive Impairment Is Associated with Enhanced Activation of Th17 Lymphocytes in Non-Alcoholic Fatty Liver Disease. Int. J. Mol. Sci. 2023, 24, 10407. [Google Scholar] [CrossRef]
- Hadjihambi, A.; Konstantinou, C.; Klohs, J.; Monsorno, K.; Le Guennec, A.; Donnelly, C.; Cox, I.J.; Kusumbe, A.; Hosford, P.S.; Soffientini, U.; et al. Partial MCT1 invalidation protects against diet-induced non-alcoholic fatty liver disease and the associated brain dysfunction. J. Hepatol. 2023, 78, 180–190. [Google Scholar] [CrossRef]
- Carneiro, L.; Asrih, M.; Repond, C.; Sempoux, C.; Stehle, J.C.; Leloup, C.; Pellerin, L. AMPK activation caused by reduced liver lactate metabolism protects against hepatic steatosis in MCT1 haploinsufficient mice. Mol. Metab. 2017, 6, 1625–1633. [Google Scholar] [CrossRef] [PubMed]
- Giuffrè, M.; Campigotto, M.; Campisciano, G.; Comar, M.; Crocè, L.S. A story of liver and gut microbes: How does the intestinal flora affect liver disease? A review of the literature. Am. J. Physiol. Gastrointest Liver Physiol. 2020, 318, G889–G906. [Google Scholar] [CrossRef] [PubMed]
- Giuffrè, M.; Moretti, R.; Campisciano, G.; da Silveira, A.B.M.; Monda, V.M.; Comar, M.; Di Bella, S.; Antonello, R.M.; Luzzati, R.; Crocè, L.S. You Talking to Me? Says the Enteric Nervous System (ENS) to the Microbe. How Intestinal Microbes Interact with the ENS. J. Clin. Med. 2020, 9, 3705. [Google Scholar] [CrossRef]
- Giuffrè, M.; Gazzin, S.; Zoratti, C.; Llido, J.P.; Lanza, G.; Tiribelli, C.; Moretti, R. Celiac Disease and Neurological Manifestations: From Gluten to Neuroinflammation. Int. J. Mol. Sci. 2022, 23, 15564. [Google Scholar] [CrossRef]
- Giuffrè, M.; Moretti, R. The Gut-Liver-Brain Axis: From the Head to the Feet. Int. J. Mol. Sci. 2023, 24, 15662. [Google Scholar] [CrossRef] [PubMed]
- Peh, A.; O’donnell, J.A.; Broughton, B.R.; Marques, F.Z. Gut Microbiota and Their Metabolites in Stroke: A Double-Edged Sword. Stroke 2022, 53, 1788–1801. [Google Scholar] [CrossRef] [PubMed]
- Ferri, C.; Castellazzi, M.; Merli, N.; Laudisi, M.; Baldin, E.; Baldi, E.; Mancabelli, L.; Ventura, M.; Pugliatti, M. Gut Microbiota Changes during Dimethyl Fumarate Treatment in Patients with Multiple Sclerosis. Int. J. Mol. Sci. 2023, 24, 2720. [Google Scholar] [CrossRef]
- Varesi, A.; Pierella, E.; Romeo, M.; Piccini, G.B.; Alfano, C.; Bjørklund, G.; Oppong, A.; Ricevuti, G.; Esposito, C.; Chirumbolo, S.; et al. The Potential Role of Gut Microbiota in Alzheimer’s Disease: From Diagnosis to Treatment. Nutrients 2022, 14, 668. [Google Scholar] [CrossRef]
- Cattaneo, A.; Cattane, N.; Galluzzi, S.; Provasi, S.; Lopizzo, N.; Festari, C.; Ferrari, C.; Guerra, U.P.; Paghera, B.; Muscio, C.; et al. Association of brain amyloidosis with pro-inflammatory gut bacterial taxa and peripheral inflammation markers in cognitively impaired elderly. Neurobiol. Aging 2017, 49, 60–68. [Google Scholar] [CrossRef]
- Vogt, N.M.; Kerby, R.L.; Dill-McFarland, K.A.; Harding, S.J.; Merluzzi, A.P.; Johnson, S.C.; Carlsson, C.M.; Asthana, S.; Zetterberg, H.; Blennow, K.; et al. Gut microbiome alterations in Alzheimer’s disease. Sci. Rep. 2017, 7, 13537. [Google Scholar] [CrossRef] [PubMed]
- Lang, S.; Schnabl, B. Microbiota and Fatty Liver Disease—The Known, the Unknown, and the Future. Cell Host Microbe 2020, 28, 233–244. [Google Scholar] [CrossRef]
- Alkasir, R.; Li, J.; Li, X.; Jin, M.; Zhu, B. Human gut microbiota: The links with dementia development. Protein Cell 2017, 8, 90–102. [Google Scholar] [CrossRef]
- Zhang, Q.; Xing, W.; Wang, Q.; Tang, Z.; Wang, Y.; Gao, W. Gut microbiota–mitochondrial inter-talk in non-alcoholic fatty liver disease. Front. Nutr. 2022, 9, 934113. [Google Scholar] [CrossRef]
- Higarza, S.G.; Arboleya, S.; Gueimonde, M.; Gómez-Lázaro, E.; Arias, J.L.; Arias, N. Neurobehavioral dysfunction in non-alcoholic steatohepatitis is associated with hyperammonemia, gut dysbiosis, and metabolic and functional brain regional deficits. PLoS ONE 2019, 14, e0223019. [Google Scholar] [CrossRef]
- Mohammed, S.K.; Magdy, Y.M.; El-Waseef, D.A.; Nabih, E.S.; Hamouda, M.A.; El-Kharashi, O.A. Modulation of hippocampal TLR4/BDNF signal pathway using probiotics is a step closer towards treating cognitive impairment in NASH model. Physiol. Behav. 2020, 214, 112762. [Google Scholar] [CrossRef]
- Li, Y.; Liang, X.; Lyu, Y.; Wang, K.; Han, L.; Wang, Y.; Sun, J.; Chi, C. Association between the gut microbiota and nonalcoholic fatty liver disease: A two-sample Mendelian randomization study. Dig. Liver Dis. 2023, 55, 1464–1471. [Google Scholar] [CrossRef]
- Oja, S.S.; Saransaari, P.; Korpi, E.R. Neurotoxicity of Ammonia. Neurochem. Res. 2017, 42, 713–720. [Google Scholar] [CrossRef]
- Adlimoghaddam, A.; Sabbir, M.G.; Albensi, B.C. Ammonia as a Potential Neurotoxic Factor in Alzheimer’s Disease. Front. Mol. Neurosci. 2016, 9, 57. [Google Scholar] [CrossRef]
- Goldbecker, A.; Buchert, R.; Berding, G.; Bokemeyer, M.; Lichtinghagen, R.; Wilke, F.; Ahl, B.; Weissenborn, K. Blood–brain barrier permeability for ammonia in patients with different grades of liver fibrosis is not different from healthy controls. J. Cereb. Blood Flow Metab. 2010, 30, 1384. [Google Scholar] [CrossRef]
- Elahy, M.; Jackaman, C.; Mamo, J.C.; Lam, V.; Dhaliwal, S.S.; Giles, C.; Nelson, D.; Takechi, R. Blood-brain barrier dysfunction developed during normal aging is associated with inflammation and loss of tight junctions but not with leukocyte recruitment. Immun. Ageing 2015, 12, 2. [Google Scholar] [CrossRef] [PubMed]
- Lemberg, A.; Fernández, M.A. Hepatic encephalopathy, ammonia, glutamate, glutamine and oxidative stress. Ann. Hepatol. 2009, 8, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Ott, P.; Vilstrup, H. Cerebral effects of ammonia in liver disease: Current hypotheses. Metab. Brain Dis. 2014, 29, 901–911. [Google Scholar] [CrossRef] [PubMed]
- Pilz, S.; März, W. Free fatty acids as a cardiovascular risk factor. Clin. Chem. Lab. Med. 2008, 46, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Pinçon, A.; De Montgolfier, O.; Akkoyunlu, N.; Daneault, C.; Pouliot, P.; Villeneuve, L.; Lesage, F.; Levy, B.I.; Thorin-Trescases, N.; Thorin, E.; et al. Non-Alcoholic Fatty Liver Disease, and the Underlying Altered Fatty Acid Metabolism, Reveals Brain Hypoperfusion and Contributes to the Cognitive Decline in APP/PS1 Mice. Metabolites 2019, 9, 104. [Google Scholar] [CrossRef] [PubMed]
- Bascoul-Colombo, C.; Guschina, I.A.; Maskrey, B.H.; Good, M.; O’Donnell, V.B.; Harwood, J.L. Dietary DHA supplementation causes selective changes in phospholipids from different brain regions in both wild type mice and the Tg2576 mouse model of Alzheimer’s disease. Biochim. Biophys. Acta 2016, 1861, 524–537. [Google Scholar] [CrossRef]
- Delpech, J.C.; Madore, C.; Joffre, C.; Aubert, A.; Kang, J.X.; Nadjar, A.; Layé, S. Transgenic increase in n-3/n-6 fatty acid ratio protects against cognitive deficits induced by an immune challenge through decrease of neuroinflammation. Neuropsychopharmacology 2015, 40, 525–536. [Google Scholar] [CrossRef] [PubMed]
- Sartorius, T.; Ketterer, C.; Kullmann, S.; Balzer, M.; Rotermund, C.; Binder, S.; Hennige, A.M. Monounsaturated fatty acids prevent the aversive effects of obesity on locomotion, brain activity, and sleep behavior. Diabetes 2012, 61, 1669–1679. [Google Scholar] [CrossRef] [PubMed]
- de Nardo, D. Toll-like receptors: Activation, signalling and transcriptional modulation. Cytokine 2015, 74, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Abe, R.A.M.; Masroor, A.; Khorochkov, A.; Prieto, J.; Singh, K.B.; Nnadozie, M.C.; Abdal, M.; Shrestha, N.; Mohammed, L. The Role of Vitamins in Non-Alcoholic Fatty Liver Disease: A Systematic Review. Cureus 2021, 13, e16855. [Google Scholar] [CrossRef] [PubMed]
- Zeng, J.; Chen, L.; Wang, Z.; Chen, Q.; Fan, Z.; Jiang, H.; Wu, Y.; Ren, L.; Chen, J.; Li, T.; et al. Marginal vitamin A deficiency facilitates Alzheimer’s pathogenesis. Acta Neuropathol. 2017, 133, 967–982. [Google Scholar] [CrossRef]
- Coelho, J.M.; Cansanção, K.; de Mello Perez, R.; Leite, N.C.; Padilha, P.; Ramalho, A.; Peres, W. Association between serum and dietary antioxidant micronutrients and advanced liver fibrosis in non-alcoholic fatty liver disease: An observational study. PeerJ 2020, 8, e9838. [Google Scholar] [CrossRef]
- Li, J.; Cordero, P.; Nguyen, V.; Oben, J.A. The Role of Vitamins in the Pathogenesis of Non-alcoholic Fatty Liver Disease. Integr. Med. Insights 2016, 11, 19–25. [Google Scholar] [CrossRef]
- Saeed, A.; Dullaart, R.P.F.; Schreuder, T.C.M.A.; Blokzijl, H.; Faber, K.N. Disturbed Vitamin A Metabolism in Non-Alcoholic Fatty Liver Disease (NAFLD). Nutrients 2017, 10, 29. [Google Scholar] [CrossRef]
- Maden, M. Retinoic acid in the development, regeneration and maintenance of the nervous system. Nat. Rev. Neurosci. 2007, 8, 755–765. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.A.; Petot, G.J.; Perry, G. Diet and oxidative stress: A novel synthesis of epidemiological data on Alzheimer’s disease. J. Alzheimers Dis. 1999, 1, 203–206. [Google Scholar] [CrossRef]
- Kennedy, D.O. B Vitamins and the Brain: Mechanisms, Dose and Efficacy—A Review. Nutrients 2016, 8, 68. [Google Scholar] [CrossRef]
- Uchida, Y.; Ito, K.; Ohtsuki, S.; Kubo, Y.; Terasaki, T. Major involvement of Na(+) -dependent multivitamin transporter (SLC5A6/SMVT) in uptake of biotin and pantothenic acid by human brain capillary endothelial cells. J. Neurochem. 2015, 134, 97–112. [Google Scholar] [CrossRef] [PubMed]
- Spector, R.; Johanson, C.E. Vitamin transport and homeostasis in mammalian brain: Focus on Vitamins B and E. J. Neurochem. 2007, 103, 425–438. [Google Scholar] [CrossRef]
- Zhou, C.C.; Yang, X.; Hua, X.; Liu, J.; Fan, M.B.; Li, G.Q.; Miao, C.Y. Hepatic NAD(+) deficiency as a therapeutic target for non-alcoholic fatty liver disease in ageing. Br. J. Pharmacol. 2016, 173, 2352–2368. [Google Scholar] [CrossRef]
- Imai, S.-I.; Johnson, S. NAD+ biosynthesis, aging, and disease. F1000Research 2018, 7, 132. [Google Scholar] [CrossRef]
- Guarino, M.; Dufour, J.F. Nicotinamide and NAFLD: Is There Nothing New Under the Sun? Metabolites 2019, 9, 180. [Google Scholar] [CrossRef]
- Gasperi, V.; Sibilano, M.; Savini, I.; Catani, M.V. Niacin in the Central Nervous System: An Update of Biological Aspects and Clinical Applications. Int. J. Mol. Sci. 2019, 20, 974. [Google Scholar] [CrossRef] [PubMed]
- Verdin, E. NAD+ in aging, metabolism, and neurodegeneration. Science 2015, 350, 1208–1213. [Google Scholar] [CrossRef] [PubMed]
- Kerr, J.S.; Adriaanse, B.A.; Greig, N.H.; Mattson, M.P.; Cader, M.Z.; Bohr, V.A.; Fang, E.F. Mitophagy and Alzheimer’s Disease: Cellular and Molecular Mechanisms. Trends Neurosci. 2017, 40, 151–166. [Google Scholar] [CrossRef] [PubMed]
- Burwinkel, M.; Lutzenberger, M.; Heppner, F.L.; Schulz-Schaeffer, W.; Baier, M. Intravenous injection of beta-amyloid seeds promotes cerebral amyloid angiopathy (CAA). Acta Neuropathol. Commun. 2018, 6, 23. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Hu, X.; Yang, Y.; Takata, T.; Sakurai, T. Nicotinamide mononucleotide protects against β-amyloid oligomer-induced cognitive impairment and neuronal death. Brain Res. 2016, 1643, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Mahamid, M.; Mahroum, N.; Bragazzi, N.L.; Shalaata, K.; Yavne, Y.; Adawi, M.; Amital, H.; Watad, A. Folate and B12 Levels Correlate with Histological Severity in NASH Patients. Nutrients 2018, 10, 440. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Quan, M.; Li, T.; Jia, J. Serum Homocysteine, Vitamin B12, Folate, and Their Association with Mild Cognitive Impairment and Subtypes of Dementia. J. Alzheimers Dis. 2022, 90, 681–691. [Google Scholar] [CrossRef] [PubMed]
- Moretti, R.; Giuffré, M.; Caruso, P.; Gazzin, S.; Tiribelli, C. Homocysteine in Neurology: A Possible Contributing Factor to Small Vessel Disease. Int. J. Mol. Sci. 2021, 22, 2051. [Google Scholar] [CrossRef] [PubMed]
- Raza, S.; Tewari, A.; Rajak, S.; Sinha, R.A. Vitamins and non-alcoholic fatty liver disease: A Molecular Insight⋆. Liver Res. 2021, 5, 62–71. [Google Scholar] [CrossRef]
- Pickett-Blakely, O.; Young, K.; Carr, R.M. Micronutrients in Nonalcoholic Fatty Liver Disease Pathogenesis. Cell. Mol. Gastroenterol. Hepatol. 2018, 6, 451–462. [Google Scholar] [CrossRef]
- Rucker, R.B.; Zempleni, J.; Suttie, J.W.; McCormick, D.B. Handbook of Vitamins; Taylor & Francis Ltd.: London, UK, 2007. [Google Scholar] [CrossRef]
- Reynolds, E. Vitamin B12, folic acid, and the nervous system. Lancet Neurol. 2006, 5, 949–960. [Google Scholar] [CrossRef]
- Stahl, S.M. L-methylfolate: A vitamin for your monoamines. J. Clin. Psychiatry 2008, 69, 1352–1353. [Google Scholar] [CrossRef]
- Moat, S.J.; Clarke, Z.L.; Madhavan, A.K.; Lewis, M.J.; Lang, D. Folic acid reverses endothelial dysfunction induced by inhibition of tetrahydrobiopterin biosynthesis. Eur. J. Pharmacol. 2006, 530, 250–258. [Google Scholar] [CrossRef]
- Cai, J.; Zhang, Z.; Liu, J.; Xiao, X.; Wang, C.; Deng, M.; Chen, L. Correlation between serum 25-OH vitamin D expression and non-alcoholic fatty liver disease. Exp. Ther. Med. 2020, 19, 1681–1686. [Google Scholar] [CrossRef]
- Borges-Canha, M.; Neves, J.S.; Mendonça, F.; Silva, M.M.; Costa, C.; Cabral, P.M.; Carvalho, D. The Impact of Vitamin D in Non-Alcoholic Fatty Liver Disease: A Cross-Sectional Study in Patients with Morbid Obesity. Diabetes Metab. Syndr. Obes. 2021, 14, 487–495. [Google Scholar] [CrossRef]
- A Cimini, F.; Barchetta, I.; Carotti, S.; Bertoccini, L.; Baroni, M.G.; Vespasiani-Gentilucci, U.; Cavallo, M.-G.; Morini, S. Relationship between adipose tissue dysfunction, vitamin D deficiency and the pathogenesis of non-alcoholic fatty liver disease. World J. Gastroenterol. 2017, 23, 3407–3417. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Shu, X.B.; Yao, Z.; Ji, G.; Zhang, L. Is vitamin D receptor a druggable target for non-alcoholic steatohepatitis? World J. Gastroenterol. 2020, 26, 5812–5821. [Google Scholar] [CrossRef] [PubMed]
- Barchetta, I.; Cimini, F.A.; Cavallo, M.G. Vitamin D and Metabolic Dysfunction-Associated Fatty Liver Disease (MAFLD): An Update. Nutrients 2020, 12, 3302. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.; Gooch, H.; Petty, A.; McGrath, J.J.; Eyles, D. Vitamin D and the brain: Genomic and non-genomic actions. Mol. Cell. Endocrinol. 2017, 453, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Cui, C.; Xu, P.; Li, G.; Qiao, Y.; Han, W.; Geng, C.; Liao, D.; Yang, M.; Chen, D.; Jiang, P. Vitamin D receptor activation regulates microglia polarization and oxidative stress in spontaneously hypertensive rats and angiotensin II-exposed microglial cells: Role of renin-angiotensin system. Redox Biol. 2019, 26, 101295. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira LR, C.; Mimura LA, N.; Fraga-Silva TF, D.C.; Ishikawa LL, W.; Fernandes AA, H.; Zorzella-Pezavento SF, G.; Sartori, A. Calcitriol Prevents Neuroinflammation and Reduces Blood-Brain Barrier Disruption and Local Macrophage/Microglia Activation. Front. Pharmacol. 2020, 11, 161. [Google Scholar] [CrossRef]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef] [PubMed]
| Diagnostic Criteria and Key Characteristics | Prevalence |
|---|---|
| Cognitive Impairment | |
| Modest cognitive decline in one or more cognitive domains, based on: − Concern about mild decline, expressed by an individual or reliable informant or observed by the clinician; − Modest impairment, documented by objective cognitive assessment. No interference with independence in everyday activities, although these activities may require more time and effort, accommodation, or compensatory strategies. Cognitive impairment affects cognitive functions such as reasoning, perception, memory, verbal, mathematical, and problem-solving abilities and reduces the individual capability of performing more complex everyday tasks (e.g., housework, driving, and working). | Approximately 50 million individuals worldwide are affected by cognitive impairment, and it is estimated to increase to 2 billion individuals by 2050. The worldwide prevalence of mild cognitive impairment (MCI) among community inhabitants over 50 years of age is 15.56% according to a recent meta-analysis, and is affected by age, gender, education level, and region of study sites. A meta-analysis of 41 studies revealed a cumulative proportion of 39.2% of MCI cases who progressed to dementia in specialist settings. Moreover, around 22% in population studies develop a major cognitive disorder over the following 3 to 10 years, in contrast with 3% of the population without MCI. |
| Dementia | |
| Significant cognitive decline in one or more cognitive domains, based on: − Concern about significant decline, expressed by an individual or reliable informant or observed by the clinician; − Substantial impairment, documented by objective cognitive assessment. Interference with independence in everyday activities. Dementia can have different etiologies (vascular dementia, Alzheimer’s Disease, frontotemporal dementia, Lewy body disease) and is characterized by significant memory loss, confusion, personality changes, and difficulty in speaking, understanding, and expressing language, and reading and writing. Depending on the underlying etiology some forms may be characterized by visual hallucinations, Parkinsonian movement features, or even drastic changes in social behavior and personality. | Approximately 55 million individuals worldwide are affected by dementia, with Alzheimer’s Disease contributing to 60–70% of cases. Dementia is the seventh most common cause of death and a significant contributor to disability and dependency in the elderly worldwide. In 2019, dementia incurred a global economic cost of USD 1.3 trillion, with around 50% of these expenses being linked to care given by informal caregivers, such as family members and close friends, who typically offer 5 h of care and supervision daily. Women are more significantly impacted by dementia, both directly and indirectly. Women have a greater burden of disability-adjusted life years and mortality from dementia, while also contributing 70% of the caregiving hours for individuals with dementia. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giuffrè, M.; Merli, N.; Pugliatti, M.; Moretti, R. The Metabolic Impact of Nonalcoholic Fatty Liver Disease on Cognitive Dysfunction: A Comprehensive Clinical and Pathophysiological Review. Int. J. Mol. Sci. 2024, 25, 3337. https://doi.org/10.3390/ijms25063337
Giuffrè M, Merli N, Pugliatti M, Moretti R. The Metabolic Impact of Nonalcoholic Fatty Liver Disease on Cognitive Dysfunction: A Comprehensive Clinical and Pathophysiological Review. International Journal of Molecular Sciences. 2024; 25(6):3337. https://doi.org/10.3390/ijms25063337
Chicago/Turabian StyleGiuffrè, Mauro, Nicola Merli, Maura Pugliatti, and Rita Moretti. 2024. "The Metabolic Impact of Nonalcoholic Fatty Liver Disease on Cognitive Dysfunction: A Comprehensive Clinical and Pathophysiological Review" International Journal of Molecular Sciences 25, no. 6: 3337. https://doi.org/10.3390/ijms25063337
APA StyleGiuffrè, M., Merli, N., Pugliatti, M., & Moretti, R. (2024). The Metabolic Impact of Nonalcoholic Fatty Liver Disease on Cognitive Dysfunction: A Comprehensive Clinical and Pathophysiological Review. International Journal of Molecular Sciences, 25(6), 3337. https://doi.org/10.3390/ijms25063337









