Cinnamomum zeylanicum Blume Essential Oil Inhibits Metastatic Melanoma Cell Proliferation by Triggering an Incomplete Tumour Cell Stress Response
Abstract
1. Introduction
2. Results
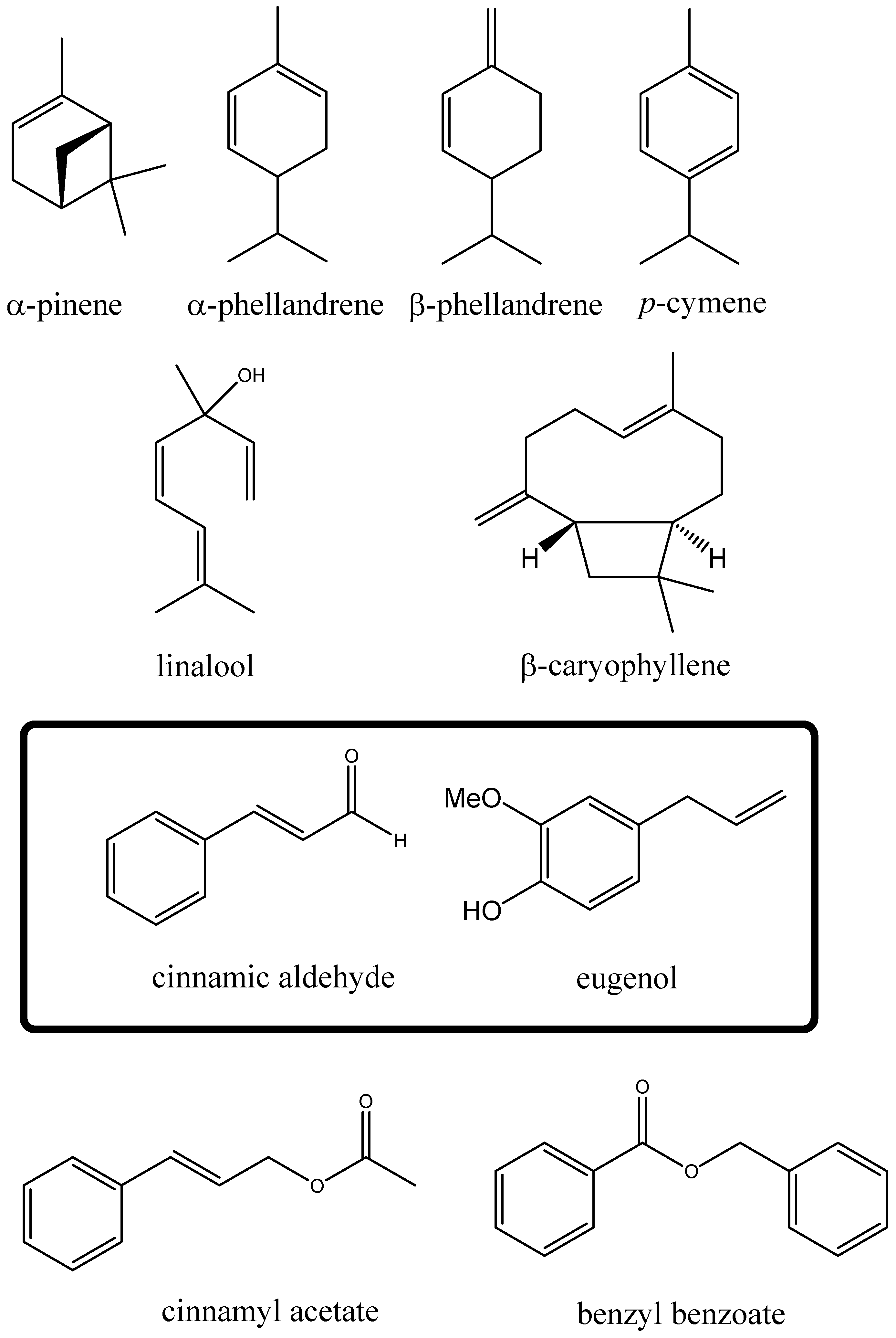
2.1. Cinnamomum zeylanicum Whole Essential Oil Composition
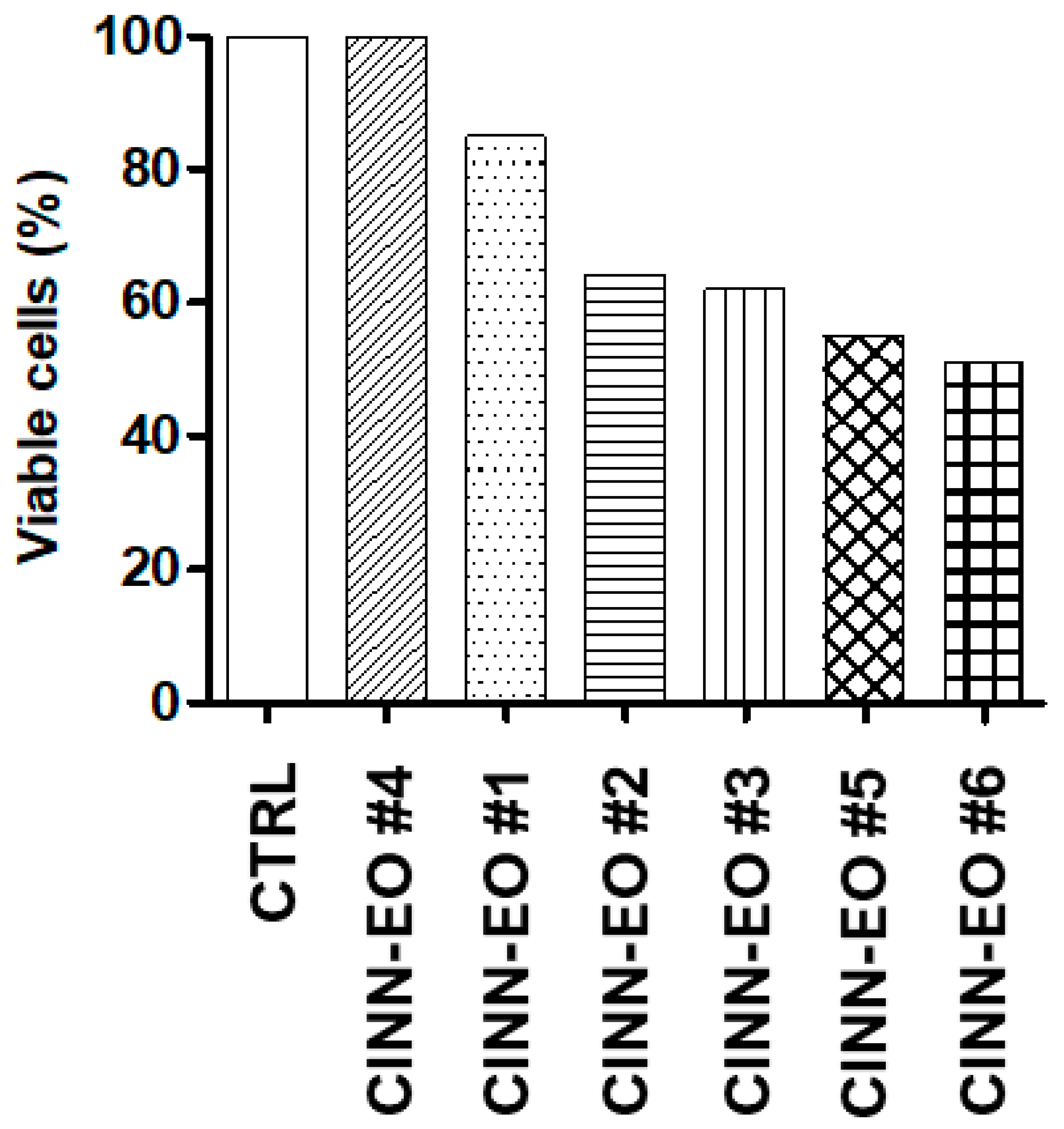
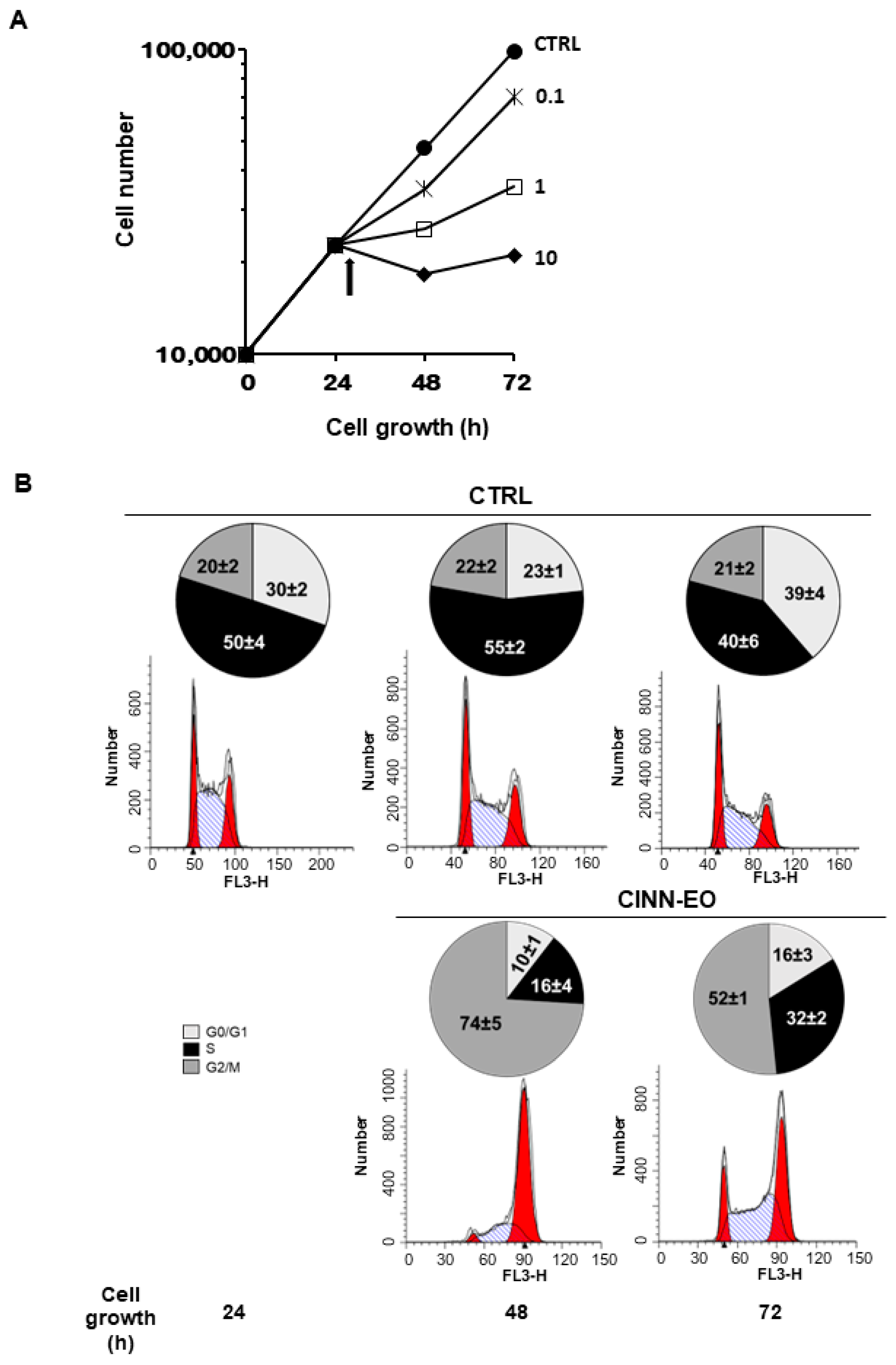
2.2. C. zeylanicum Essential Oil Cytotoxic Effects on the Human Melanoma Cell Line M14
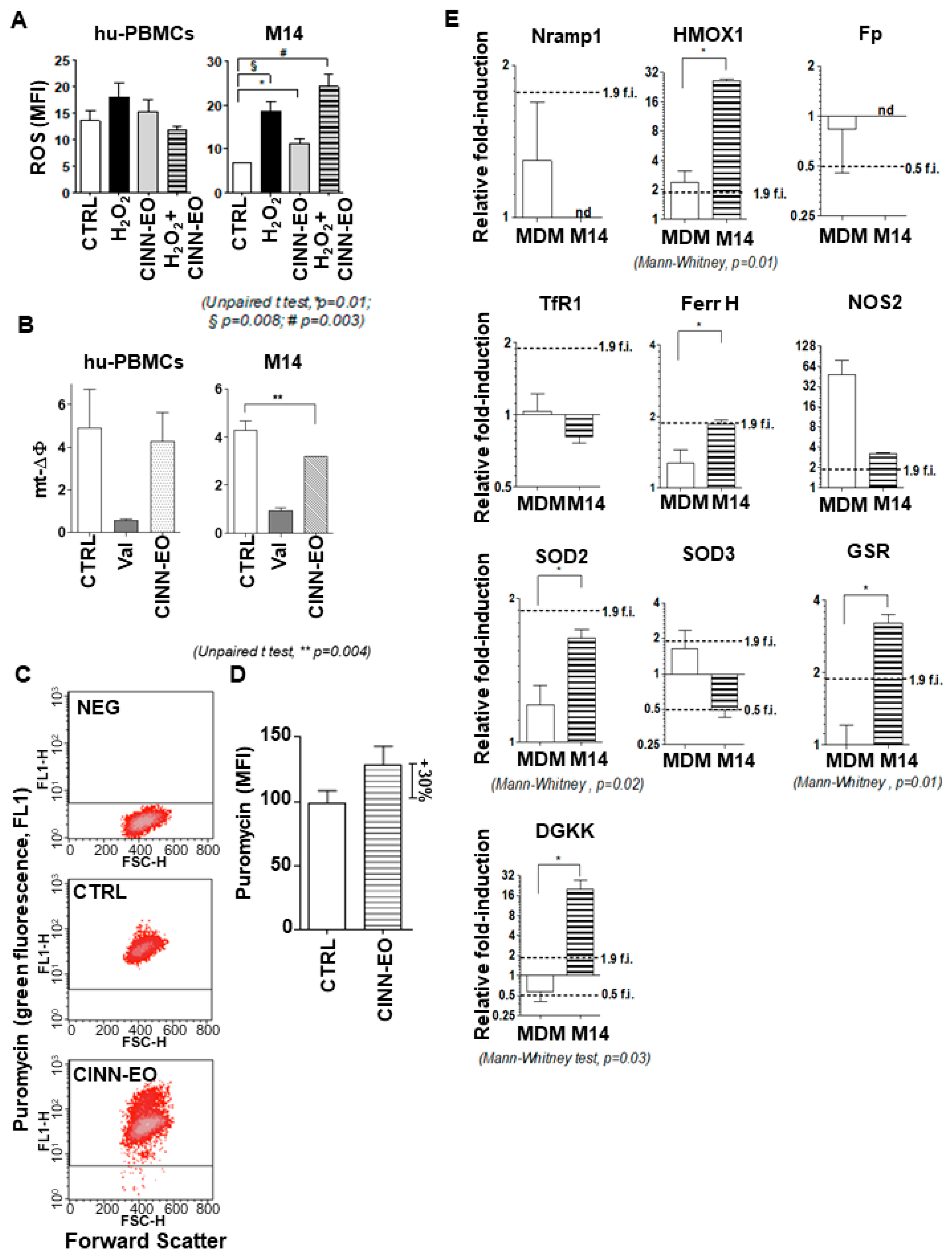
2.3. CINN-EO Affects Intracellular Oxidative Properties and Iron Metabolism
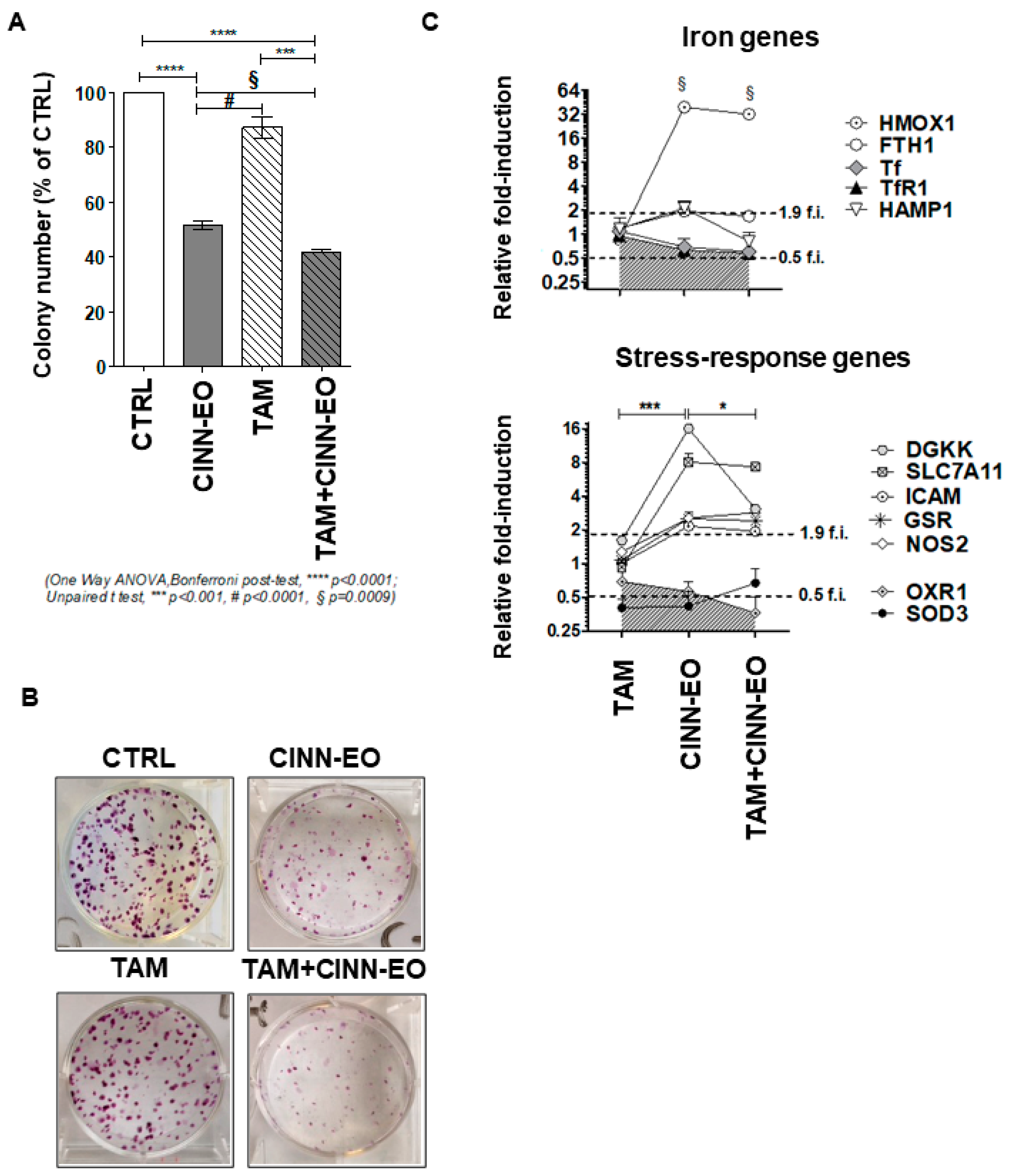
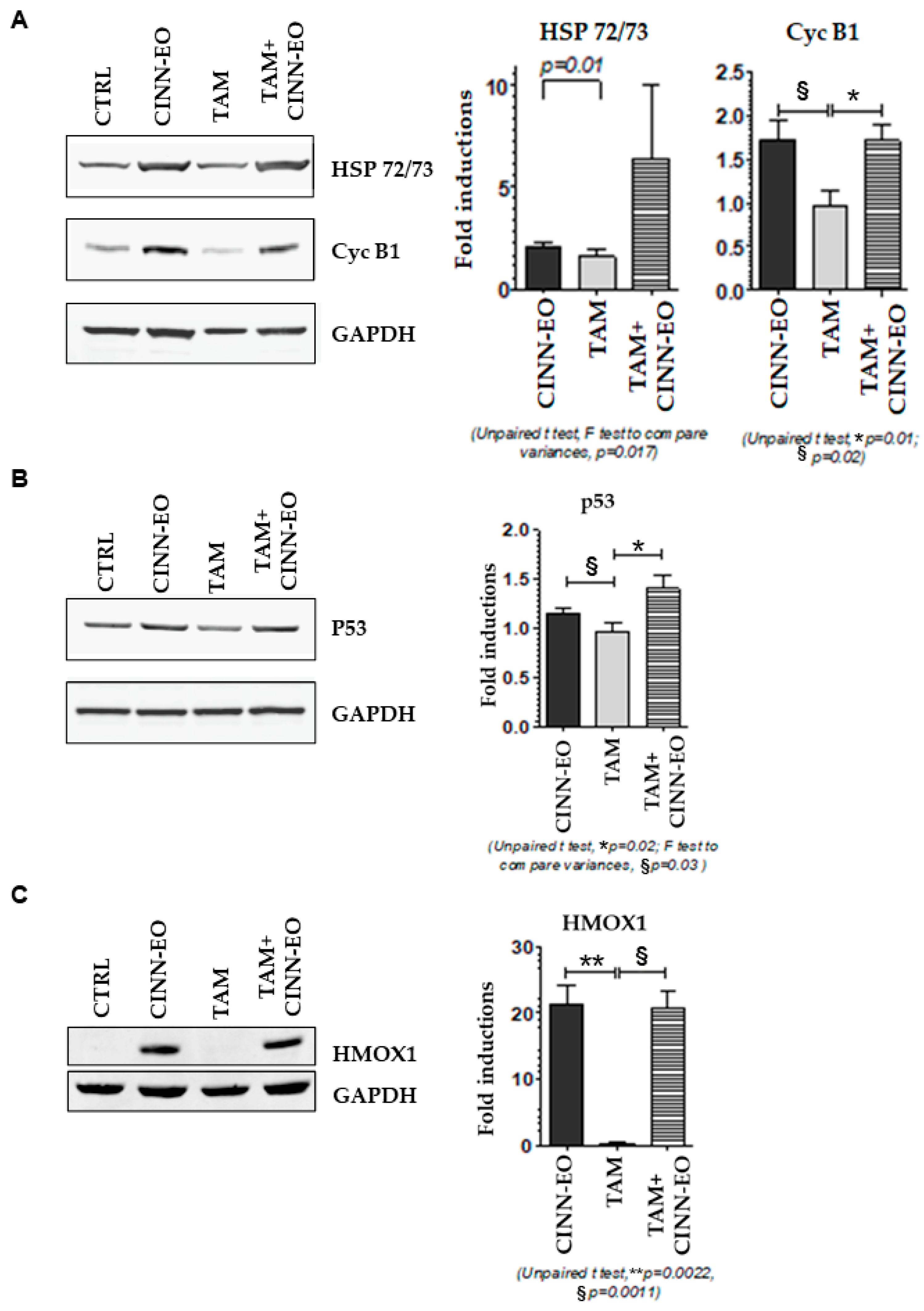
2.4. Effects of CINN-EO and Tamoxifen Co-Administration on M14 Cell Survival, Gene Expression and Protein Level
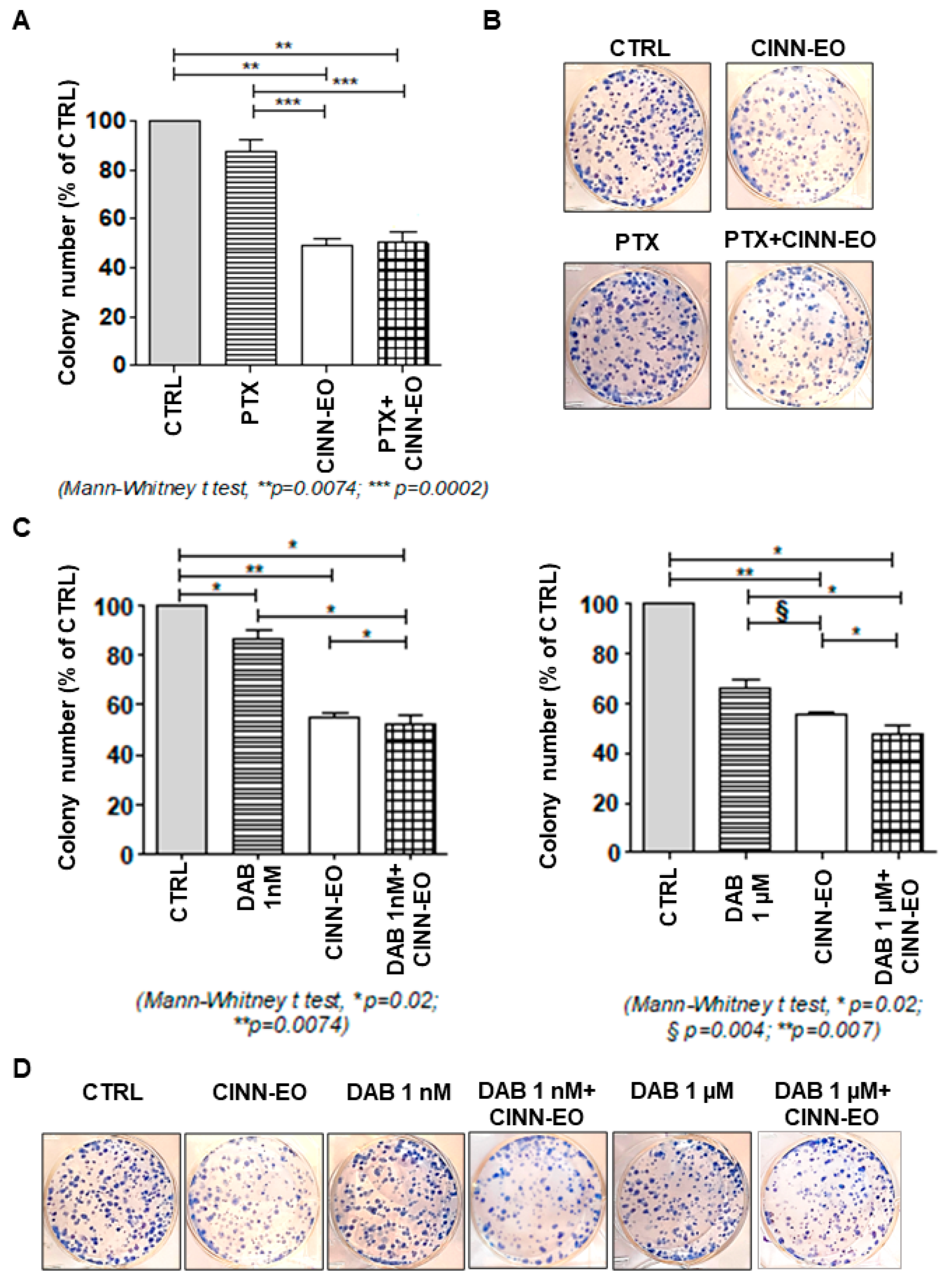
2.5. Effects of CINN-EO and Paclitaxel or Dabrafenib Co-Administration on M14 Cell Survival
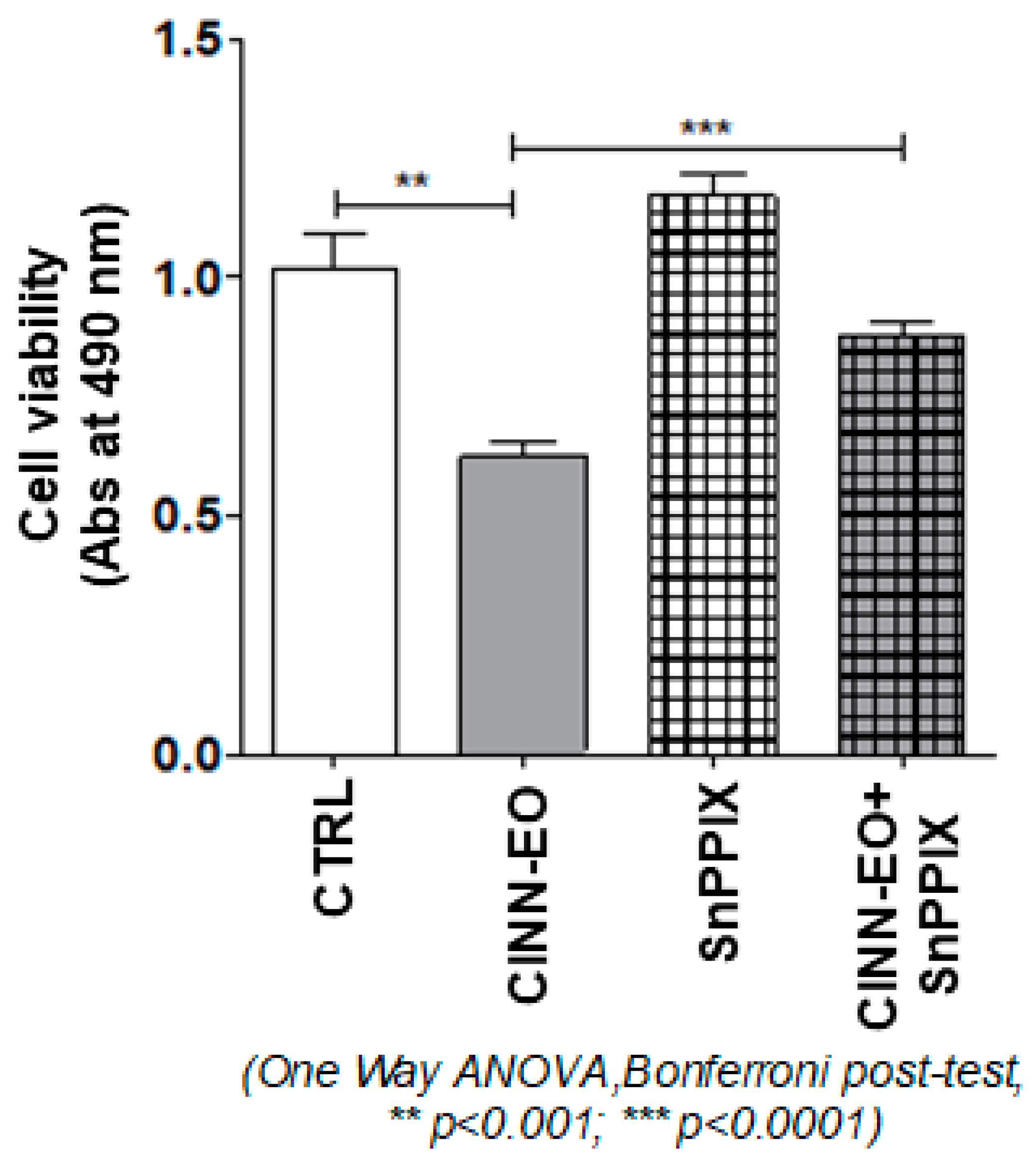
2.6. Effect of an HMOX1 Inhibitor on CINN-EO-induced Cytotoxicity
3. Discussion
4. Materials and Methods
4.1. Cinnamomum zeylanicum Essential Oils
4.2. GC and GC-MS Analyses of Essential Oils
4.3. Identification of Components of the Essential Oils
4.4. Cell Culture and EO Treatments
4.5. Cell Cycle Analysis
4.6. ROS Production and Mitochondrial Potential Assays
4.7. Intracellular Ferrous Iron Measurement with a Trx-puromycin Probe: Puromycin Incorporation Analysis Via In-Cell Immunofluorescence
4.8. Gene Expression Profiling by qRT-PCR
4.9. Drugs and C. zeylanicum EO Co-administration and Colony Formation Assay
4.10. Western Blot Analysis
4.11. Effect of the HMOX1 Inhibitor SnPPIX on M14 Cell Proliferation upon CINN-EO Treatment
4.12. Statistical Analysis
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Glossary
References
- Heistein, J.B.; Acharya, U.; Mukkamalla, S.K.R. Malignant Melanoma; StatPearls Publishing: St. Petersburg, FL, USA, 2022. [Google Scholar]
- Arslanbaeva, L.R.; Santoro, M.M. Adaptive redox homeostasis in cutaneous melanoma. Redox Biol. 2020, 37, 101753. [Google Scholar] [CrossRef]
- Tabolacci, C.; De Vita, D.; Facchiano, A.; Bozzuto, G.; Beninati, S.; Failla, C.M.; Di Martile, M.; Lintas, C.; Mischiati, C.; Stringaro, A.; et al. Phytochemicals as Immunomodulatory Agents in Melanoma. Int. J. Mol. Sci. 2023, 24, 2657. [Google Scholar] [CrossRef]
- Obrador, E.; Salvador-Palmer, R.; López-Blanch, R.; Oriol-Caballo, M.; Moreno-Murciano, P.; Estrela, J.M. Survival Mechanisms of Metastatic Melanoma Cells: The Link between Glucocorticoids and the Nrf2-Dependent Antioxidant Defense System. Cells 2023, 12, 418. [Google Scholar] [CrossRef] [PubMed]
- Cabello, C.M.; Bair, W.B., 3rd; Wondrak, G.T. Experimental therapeutics: Targeting the redox Achilles heel of cancer. Curr. Opin. Investig. Drugs 2007, 8, 1022–1037. [Google Scholar]
- Bhooshan, K.P.; Pandey, K.B.; Rizv, S.I. Plant polyphenols as dietary antioxidants in human health and disease. Oxid. Med. Cell Longev. 2009, 2, 270–278. [Google Scholar]
- Harasym, J.; Oledzki, R. Effect of fruit and vegetable antioxidants on total antioxidant capacity of blood plasma. Nutrition 2014, 30, 511–517. [Google Scholar] [CrossRef] [PubMed]
- Mehmet, U.; Emel, E.; Gulhan Vardar, U.; Hulya Sivas, Z.; Nilufer, V. Composition, antimicrobial activity and in vitro cytotoxicity of essential oil from Cinnamomum zeylanicum Blume (Lauraceae). Food Chem. Toxicol. 2010, 48, 3274–3280. [Google Scholar]
- Chou, S.T.; Chang, W.L.; Chang, C.T.; Hsu, S.L.; Lin, Y.C.; Shih, Y. Cinnamomum cassia Essential Oil Inhibits α-MSH-Induced Melanin Production and Oxidative Stress in Murine B16 Melanoma Cells. Int. J. Mol. Sci 2013, 14, 19186–19201. [Google Scholar] [CrossRef]
- Mijatovic, S.A.; Timotijevic, G.S.; Miljkovic, D.M.; Radovic, J.M.; Maksimovic-Ivanic, D.D.; Dekanski, D.P.; Stosic-Grujicic, S.D. Multiple antimelanoma potential of dry olive leaf extract. Int. J. Cancer 2011, 128, 1955–1965. [Google Scholar] [CrossRef] [PubMed]
- Cabello, C.M.; Bair, W.B., 3rd; Lamore, S.D.; Ley, S.; Bause, A.S.; Azimian, S.; Wondrak, G.T. The cinnamon-derived Michael acceptor cinnamic aldehyde impairs melanoma cell proliferation, invasiveness, and tumor growth. Free Radic. Biol. Med. 2009, 46, 220–231. [Google Scholar] [CrossRef] [PubMed]
- Hussain, T.; Tan, B.; Yin, Y.; Blachier, F.; Tossou, M.C.; Rahu, N. Oxidative Stress and Inflammation: What Polyphenols Can Do for Us? Oxid. Med. Cell Longev. 2016, 2016, 7432797. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Pandey, A.K. Chemistry and biological activities of flavonoids: An overview. Sci. World J. 2013, 2013, 162750. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Young, M.R.; Bobe, G.; Colburn, N.H.; Milner, J.A. Bioactive food components, inflammatory targets, and cancer prevention. Cancer Prev. Res. 2009, 3, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Spangler, B.; Morgan, C.W.; Fontaine, S.D.; Vander Wal, M.N.; Chang, C.J.; Wells, J.A.; Renslo, A.R. A reactivity-based probe of the intracellular labile ferrous iron pool. Nat. Chem. Biol. 2016, 12, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Torti, S.V.; Torti, F.M. Iron and cancer: More ore to be mined. Nat. Rev. Cancer 2013, 13, 342–355. [Google Scholar] [CrossRef]
- Hao, S.; Liang, B.; Huang, Q.; Dong, S.; Wu, Z.; He, W.; Shi, M. Metabolic networks in ferroptosis. Oncol. Lett. 2018, 15, 5405–5411. [Google Scholar] [CrossRef]
- Lu, B.; Chen, X.B.; Ying, M.D.; He, Q.J.; Cao, J.; Yang, B. The Role of Ferroptosis in Cancer Development and Treatment Response. Front. Pharmacol. 2018, 8, 992. [Google Scholar] [CrossRef]
- Kwon, M.Y.; Park, E.; Lee, S.J.; Chung, S.W. Heme oxygenase-1 accelerates erastin-induced ferroptotic cell death. Oncotarget 2015, 6, 24393–24403. [Google Scholar] [CrossRef]
- Wang, S.J.; Ou, Y.; Jiang, L.; Gu, W. Ferroptosis: A missing puzzle piece in the p53 blueprint? Mol. Cell Oncol. 2015, 3, e1046581. [Google Scholar] [CrossRef]
- Jayaprakasha, G.K.; Rao, L.J.M. Chemistry, biogenesis, and biological activities of Cinnamomum zeylanicum. Crit. Rev. Food Sci. Nutr. 2011, 51, 547–562. [Google Scholar] [CrossRef]
- Rao, P.V.; Gan, S.H. Cinnamon: A multifaceted medicinal plant. Evid. Based Compl. Alter. Med. 2014, 2014, 642942–642954. [Google Scholar] [CrossRef]
- Friedman, M. Chemistry, Antimicrobial mechanisms, and antibiotic activities of cinnamaldehyde against pathogenic bacteria in animal feeds and human foods. J. Agric. Food Chem. 2017, 65, 10406–10423. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro-Santos, R.; Andrade, M.; Madella, D.; Martinazzo, A.P.; Moura, L.A.G.; Melo, N.R.; Silva, S.A. Revisiting an ancient spice with medicinal purposes: Cinnamon. Trends Food Sci. Technol. 2017, 62, 154–169. [Google Scholar] [CrossRef]
- Fiocco, D.; Arciuli, M.; Arena, M.P.; Benvenuti, S.; Gallone, A. Chemical composition and the anti-melanogenic potential of different essential oils. Flavour. Fragr. J. 2016, 31, 255–261. [Google Scholar] [CrossRef]
- Chatterjee, S.J.; Pandey, S. Chemo-resistant melanoma sensitized by tamoxifen to low dose curcumin treatment through induction of apoptosis and autophagy. Cancer Biol. Ther. 2011, 11, 216–228. [Google Scholar] [CrossRef]
- Chatterjee, S.J.; McNulty, J.; Pandey, S. Sensitization of human melanoma cells by tamoxifen to apoptosis induction by pancratistatin, a nongenotoxic natural compound. Melanoma Res. 2011, 21, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, J.; Amorim, R.; Santos, K.; Soares, P.; Datta, S.; Cortopassi, G.A.; Serafim, T.L.; Sardão, V.A.; Garrido, J.; Borges, F.; et al. Disruption of mitochondrial function as mechanism for anti-cancer activity of a novel mitochondriotropic menadione derivative. Toxicology 2018, 393, 123–139. [Google Scholar] [CrossRef] [PubMed]
- Fruehauf, J.P.; Trapp, V. Reactive oxygen species: An Achilles’ heel of melanoma? Expert Rev. Anticancer. Ther. 2008, 8, 1751–1757. [Google Scholar] [CrossRef] [PubMed]
- Tuma, R.S. Reactive oxygen species may have antitumor activity in metastatic melanoma. J. Natl. Cancer Inst. 2008, 100, 11–12. [Google Scholar] [CrossRef]
- Chang, L.C.; Chiang, S.K.; Che, S.E.; Yu, Y.L.; Chou, R.H.; Chang, W.C. Heme oxygenase-1 mediates BAY 11-7085 induced ferroptosis. Cancer Lett. 2018, 416, 124–137. [Google Scholar] [CrossRef]
- Jin, S.A.; Park, J.J.; Lee, J.B.; Lee, S.C.; Yun, S.J. Decreased heme oxygenase-1 expression distinguishes human melanomas from melanocytic nevi. Pigment. Cell Melanoma Res. 2010, 23, 841–844. [Google Scholar] [CrossRef] [PubMed]
- Torisu-Itakura, H.; Furue, M.; Kuwano, M.; Ono, M. Co-expression of thymidine phosphorylase and heme oxygenase-1 in macrophages in human malignant vertical growth melanomas. Jpn. J. Cancer Res. 2000, 91, 906–910. [Google Scholar] [CrossRef] [PubMed]
- Di Domenico, F.; Perluigi, M.; Foppoli, C.; Blarzino, C.; Coccia, R.; De Marco, F.; Butterfield, D.A.; Cini, C. Protective effect of ferulic acid ethyl ester against oxidative stress mediated by UVB irradiation in human epidermal melanocytes. Free Radic. Res. 2009, 43, 365–375. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, M.P.; Santos, A.E.; Custódio, J.B. Rethinking tamoxifen in the management of melanoma: New answers for an old question. Eur. J. Pharmacol. 2015, 764, 372–378. [Google Scholar] [CrossRef]
- Gupta, R.S.; Epand, R.M. Phylogenetic analysis of the diacylglycerol kinase family of proteins and identification of multiple highly-specific conserved inserts and deletions within the catalytic domain that are distinctive characteristics of different classes of DGK homologs. PLoS ONE 2017, 12, e0182758. [Google Scholar] [CrossRef]
- Shionoya, T.; Usuki, T.; Komenoi, S.; Isozaki, T.; Sakai, H.; Sakane, F. Distinct expression and localization of the type II diacylglycerol kinase isozymes δ, η and κ in the mouse reproductive organs. BMC Dev. Biol. 2015, 15, 6. [Google Scholar] [CrossRef]
- Imai, S.; Kai, M.; Yasuda, S.; Kanoh, H.; Sakane, F. Identification and characterization of a novel human type II diacylglycerol kinase, DGK kappa. J. Biol. Chem. 2005, 280, 39870–39881. [Google Scholar] [CrossRef]
- Dixon, S.J.; Patel, D.N.; Welsch, M.; Skouta, R.; Lee, E.D.; Hayano, M.; Thomas, A.G.; Gleason, C.E.; Tatonetti, N.P.; Slusher, B.S.; et al. Pharmacological inhibition of cystine-glutamate exchange induces endoplasmic reticulum stress and ferroptosis. Elife 2014, 3, e02523. [Google Scholar] [CrossRef]
- Goldshmit, Y.; Jona, G.; Schmukler, E.; Solomon, S.; Pinkas-Kramarski, R.; Ruban, A. Blood Glutamate Scavenger as a Novel Neuroprotective Treatment in Spinal Cord Injury. J. Neurotrauma 2018, 35, 2581–2590. [Google Scholar] [CrossRef]
- Vrajová, M.; Peková, S.; Horácek, J.; Höschl, C. The effects of siRNA-mediated RGS4 gene silencing on the whole genome transcription profile: Implications for schizophrenia. Neuroendocr. Lett. 2011, 32, 246–252. [Google Scholar]
- Yang, M.; Luna, L.; Sørbø, J.G.; Alseth, I.; Johansen, R.F.; Backe, P.H.; Danbolt, N.C.; Eide, L.; Bjørås, M. Human OXR1 maintains mitochondrial DNA integrity and counteracts hydrogen peroxide-induced oxidative stress by regulating antioxidant pathways involving p21. Free Radic. Biol. Med. 2014, 77, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhang, S.; Liu, X.; Wang, Y.; Chang, J.; Zhang, X.; Mackintosh, S.G.; Tackett, A.J.; He, Y.; Lv, D.; et al. Oxidation resistance 1 is a novel senolytic target. Aging Cell 2018, 15, e12780. [Google Scholar] [CrossRef] [PubMed]
- Kwon, M.J.; Kim, B.; Lee, Y.S.; Kim, T.Y. Role of superoxide dismutase 3 in skin inflammation. J. Dermatol. Sci. 2012, 67, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Sanada, Y.; Asai, S.; Ikemoto, A.; Moriwaki, T.; Nakamura, N.; Miyaji, M.; Zhang-Akiyama, Q.M. Oxidation resistance 1 is essential for protection against oxidative stress and participates in the regulation of aging in Caenorhabditis elegans. Free Radic. Res. 2014, 48, 919–928. [Google Scholar] [CrossRef]
- Roth-Walter, F.; Moskovskich, A.; Gomez-Casado, C.; Diaz-Perales, A.; Oida, K.; Singer, J.; Kinaciyan, T.; Fuchs, H.C.; Jensen-Jarolim, E. Immune suppressive effect of cinnamaldehyde due to inhibition of proliferation and induction of apoptosis in immune cells: Implications in cancer. PLoS ONE 2014, 9, e108402. [Google Scholar] [CrossRef]
- NIST. Mass Spectral Library; National Institute of Standard and Technology: Gaithersburg, MD, USA, 1998.
- Adams, R.P. Identification of Essential Oil Components by Gas Chromatography/Mass Spectrometry, 4th ed.; Allured Publishing Corp: Carol Stream, IL, USA, 2007. [Google Scholar]
- Gatti, G.; Maresca, G.; Natoli, M.; Florenzano, F.; Nicolin, A.; Felsani, A.; D’Agnano, I. MYC prevents apoptosis and enhances endoreduplication induced by paclitaxel. PLoS ONE 2009, 4, e5442. [Google Scholar] [CrossRef]
- Volpe, E.; Cappelli, G.; Grassi, M.; Martino, A.; Serafino, A.; Colizzi, V.; Sanarico, N.; Mariani, F. Gene expression profiling of human macrophages at late time of infection with Mycobacterium tuberculosis. Immunology 2006, 4, 449–460. [Google Scholar] [CrossRef]
- Chomczynski, P.; Sacchi, N. The single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction: Twenty-something years on. Nat. Protoc. 2006, 2, 581–585. [Google Scholar] [CrossRef]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 2001, 4, 402–408. [Google Scholar] [CrossRef]
| Samples | Label |
|---|---|
| SAMPLE 1—commercial from ERBA VITA GROUP S.p.A., Chiesanuova (RSM), batch # 34514 | EO1 |
| SAMPLE 2–commercial from ERBA VITA GROUP S.p.A., batch # 31913 | EO2 |
| SAMPLE 3—commercial from ZUCCARI, Trento (TN), batch # 15 | EO3 |
| SAMPLE 4—commercial from RAO ERBE S.r.l., Valverde (CT) | EO4 |
| SAMPLE 5—commercial from GALENO S.r.l., Comeana (PO), batch # 02193319 | EO5 |
| SAMPLE 6—commercial from GALENO S.r.l., Comeana (PO), batch # 02202006 | EO6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cappelli, G.; Giovannini, D.; Vilardo, L.; Basso, A.; Iannetti, I.; Massa, M.; Ruberto, G.; Muir, R.; Pastore, C.; D’Agnano, I.; et al. Cinnamomum zeylanicum Blume Essential Oil Inhibits Metastatic Melanoma Cell Proliferation by Triggering an Incomplete Tumour Cell Stress Response. Int. J. Mol. Sci. 2023, 24, 5698. https://doi.org/10.3390/ijms24065698
Cappelli G, Giovannini D, Vilardo L, Basso A, Iannetti I, Massa M, Ruberto G, Muir R, Pastore C, D’Agnano I, et al. Cinnamomum zeylanicum Blume Essential Oil Inhibits Metastatic Melanoma Cell Proliferation by Triggering an Incomplete Tumour Cell Stress Response. International Journal of Molecular Sciences. 2023; 24(6):5698. https://doi.org/10.3390/ijms24065698
Chicago/Turabian StyleCappelli, Giulia, Daniela Giovannini, Laura Vilardo, Annalisa Basso, Ilaria Iannetti, Marianna Massa, Giuseppe Ruberto, Ryan Muir, Carlo Pastore, Igea D’Agnano, and et al. 2023. "Cinnamomum zeylanicum Blume Essential Oil Inhibits Metastatic Melanoma Cell Proliferation by Triggering an Incomplete Tumour Cell Stress Response" International Journal of Molecular Sciences 24, no. 6: 5698. https://doi.org/10.3390/ijms24065698
APA StyleCappelli, G., Giovannini, D., Vilardo, L., Basso, A., Iannetti, I., Massa, M., Ruberto, G., Muir, R., Pastore, C., D’Agnano, I., & Mariani, F. (2023). Cinnamomum zeylanicum Blume Essential Oil Inhibits Metastatic Melanoma Cell Proliferation by Triggering an Incomplete Tumour Cell Stress Response. International Journal of Molecular Sciences, 24(6), 5698. https://doi.org/10.3390/ijms24065698








