Machine Learning Approaches in Diagnosis, Prognosis and Treatment Selection of Cardiac Amyloidosis
Abstract
1. Introduction
General Considerations on Amyloidosis
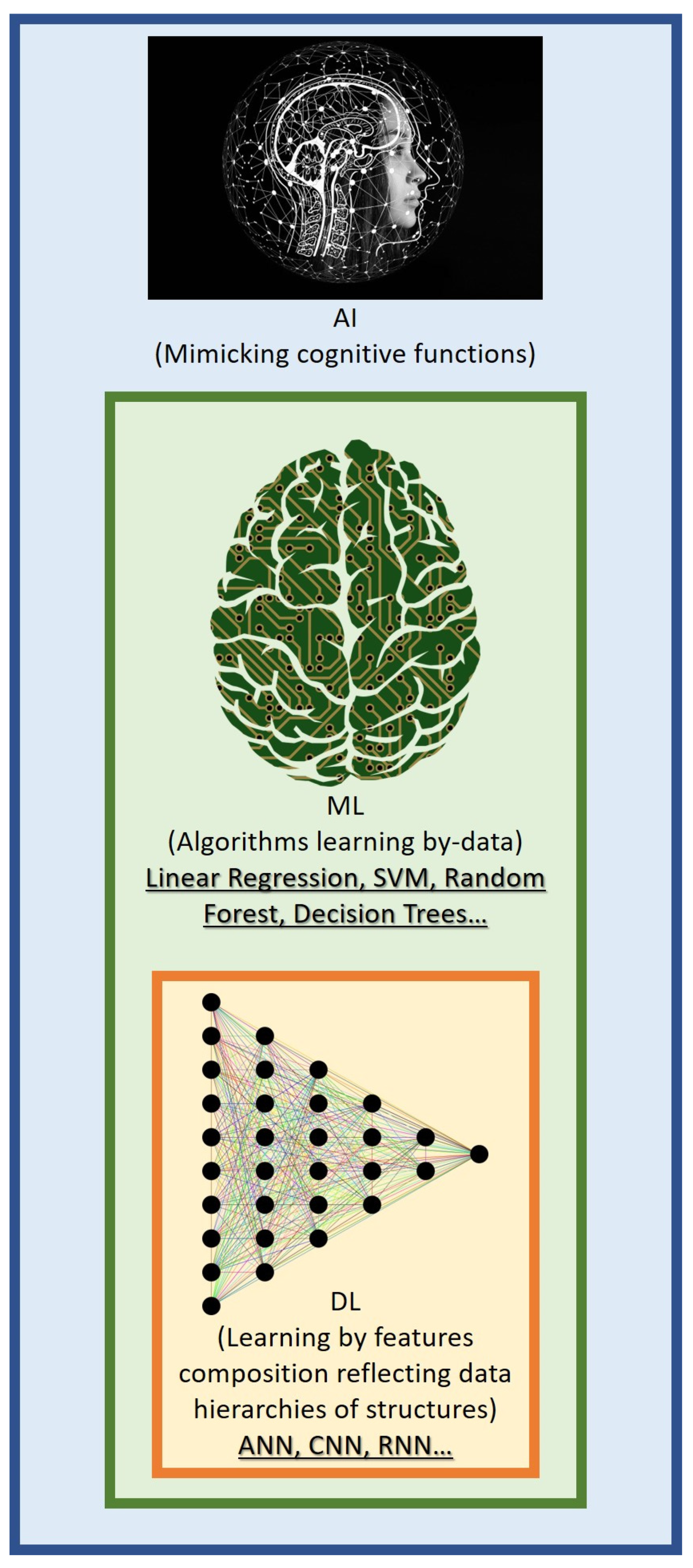
2. Machine Learning and Deep Learning
3. Diagnosis of Amyloidosis
3.1. Electrocardiographic Evaluation in the Diagnostic Work-Up for CA
3.2. Echocardiography Evaluation in the Diagnostic Work-Up for CA
3.3. Magnetic Resonance Evaluation in the Diagnostic Work-Up for CA
3.4. Mass Spectrometry Evaluation in the Diagnostic Work-Up for CA
3.5. Medical Data and Radiomics in the Diagnostic Work-Up for CA
4. Computational Methods for Amyloid Fibril Identification
5. Prognosis
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- DeArmond, S.J. Alzheimer’s disease and Creutzfeldt-Jakob disease: Overlap of pathogenic mechanisms. Curr. Opin. Neurol. 1993, 6, 872–881. [Google Scholar] [CrossRef] [PubMed]
- Wechalekar, A.D.; Gillmore, J.D.; Hawkins, P.N. Systemic amyloidosis. Lancet 2016, 387, 2641–2654. [Google Scholar] [CrossRef] [PubMed]
- Scott, P.P.; Scott, W.W., Jr.; Siegelman, S.S. Amyloidosis: An overview. In Seminars in Roentgenology; WB Saunders: Philadelphia, PA, USA, 1986; Volume 21, pp. 103–112. [Google Scholar]
- Ruberg, F.L.; Berk, J.L. Transthyretin (TTR) cardiac amyloidosis. Circulation 2012, 126, 1286–1300. [Google Scholar] [CrossRef] [PubMed]
- Kittleson, M.M.; Maurer, M.S.; Ambardekar, A.V.; Bullock-Palmer, R.P.; Chang, P.P.; Eisen, H.J.; Nair, A.P.; Nativi-Nicolau, J.; Ruberg, F.L.; American Heart Association Heart Failure and Transplantation Committee of the Council on Clinical Cardiology. Cardiac Amyloidosis: Evolving Diagnosis and Management: A Scientific Statement From the American Heart Association. Circulation 2020, 142, e7–e22. [Google Scholar] [CrossRef] [PubMed]
- González-López, E.; Gallego-Delgado, M.; Guzzo-Merello, G.; de Haro-Del Moral, F.J.; Cobo-Marcos, M.; Robles, C.; Bornstein, B.; Salas, C.; Lara-Pezzi, E.; Alonso-Pulpon, L.; et al. Wild-type transthyretin amyloidosis as a cause of heart failure with preserved ejection fraction. Eur. Heart J. 2015, 36, 2585–2594. [Google Scholar] [CrossRef]
- Castaño, A.; Narotsky, D.L.; Hamid, N.; Khalique, O.K.; Morgenstern, R.; DeLuca, A.; Rubin, J.; Chiuzan, C.; Nazif, T.; Vahl, T.; et al. Unveiling transthyretin cardiac amyloidosis and its predictors among elderly patients with severe aortic stenosis undergoing transcatheter aortic valve replacement. Eur. Heart J. 2017, 38, 2879–2887. [Google Scholar] [CrossRef]
- Rapezzi, C.; Quarta, C.C.; Riva, L.; Longhi, S.; Gallelli, I.; Lorenzini, M.; Ciliberti, P.; Biagini, E.; Salvi, F.; Branzi, A. Transthyretin-related amyloidoses and the heart: A clinical overview. Nat. Rev. Cardiol. 2010, 7, 398–408. [Google Scholar] [CrossRef]
- Fosbøl, E.L.; Rørth, R.; Leicht, B.P.; Schou, M.; Maurer, M.S.; Kristensen, S.L.; Kober, L.; Gustafsson, F. Association of Carpal Tunnel Syndrome With Amyloidosis, Heart Failure, and Adverse Cardiovascular Outcomes. J. Am. Coll. Cardiol. 2019, 74, 15–23. [Google Scholar] [CrossRef]
- Witteles, R.M.; Bokhari, S.; Damy, T.; Elliott, P.M.; Falk, R.H.; Fine, N.M.; Gospodinova, M.; Obici, L.; Rapezzi, C.; Garcia-Pavia, P. Screening for Transthyretin Amyloid Cardiomyopathy in Everyday Practice. JACC Heart Fail. 2019, 7, 709–716. [Google Scholar] [CrossRef]
- Abou Ezzeddine, O.F.; Davies, D.R.; Scott, C.G.; Fayyaz, A.U.; Askew, J.W.; McKie, P.M.; Noseworthy, P.A.; Johnson, G.B.; Dunlay, S.M.; Borlaug, B.A.; et al. Prevalence of Transthyretin Amyloid Cardiomyopathy in Heart Failure With Preserved Ejection Fraction. JAMA Cardiol. 2021, 6, 1267–1274. [Google Scholar] [CrossRef]
- Bishop, E.; Brown, E.E.; Fajardo, J.; Barouch, L.A.; Judge, D.P.; Halushka, M.K. Seven factors predict a delayed diagnosis of cardiac amyloidosis. Amyloid 2018, 25, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Lousada, I. The amyloidosis forum: A public private partnership to advance drug development in AL amyloidosis. Orphanet J. Rare Dis. 2020, 15, 268. [Google Scholar] [PubMed]
- Desport, E.; Bridoux, F.; Sirac, C.; Delbes, S.; Bender, S.; Fernandez, B.; Quellard, N.; Lacombe, C.; Goujon, J.M.; Lavergne, D.; et al. AL amyloidosis. Orphanet J. Rare Dis. 2012, 7, 54. [Google Scholar] [CrossRef]
- Quock, T.P.; Yan, T.; Chang, E.; Guthrie, S.; Broder, M.S. Epidemiology of AL amyloidosis: A real-world study using US claims data. Blood Adv. 2018, 2, 1046–1053. [Google Scholar] [CrossRef] [PubMed]
- Vaxman, I.; Gertz, M. Recent advances in the diagnosis, risk stratification, and management of systemic light-chain amyloidosis. Acta Haematol. 2019, 141, 93–106. [Google Scholar] [CrossRef]
- Escher, F.; Senoner, M.; Doerler, J.; Zaruba, M.M.; Messner, M.; Mussner-Seeber, C.; Ebert, M.; Ensinger, C.; Mair, A.; Kroiss, A.; et al. When and how do patients with cardiac amyloidosis die? Clin. Res. Cardiol. 2020, 109, 78–88. [Google Scholar] [CrossRef]
- Kumar, S.; Dispenzieri, A.; Lacy, M.Q.; Hayman, S.R.; Buadi, F.K.; Colby, C.; Laumann, K.; Zeldenrust, S.R.; Leung, N.; Dingli, D.; et al. Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum free light chain measurements. J. Clin. Oncol. 2012, 30, 989–995. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.K.; Gertz, M.A.; Lacy, M.Q.; Dingli, D.; Hayman, S.R.; Buadi, F.K.; Short-Detweiler, K.; Zeldenrust, S.R.; Leung, N.; Greipp, P.R.; et al. Recent improvements in survival in primary systemic amyloidosis and the importance of an early mortality risk score. In Mayo Clinic Proceedings; Elsevier: Amsterdam, The Netherlands, 2011; Volume 86, pp. 12–18. [Google Scholar]
- Manwani, R.; Cohen, O.; Sharpley, F.; Mahmood, S.; Sachchithanantham, S.; Foard, D.; Lachmann, H.J.; Quarta, C.; Fontana, M.; Gillmore, J.D.; et al. A prospective observational study of 915 patients with systemic AL amyloidosis treated with upfront bortezomib. Blood 2019, 134, 2271–2280. [Google Scholar] [CrossRef]
- Barrett, C.D.; Dobos, K.; Liedtke, M.; Tuzovic, M.; Haddad, F.; Kobayashi, Y.; Lafayette, R.; Fowler, M.B.; Arai, S.; Schrier, S.; et al. A changing landscape of mortality for systemic light chain amyloidosis. J. Am. Coll. Cardiol. HF 2019, 7, 958–966. [Google Scholar] [CrossRef]
- Muchtar, E.; Gertz, M.A.; Kumar, S.K.; Lacy, M.Q.; Dingli, D.; Buadi, F.K.; Grogan, M.; Hayman, S.R.; Kapoor, P.; Leung, N.; et al. Improved outcomes for newly diagnosed AL amyloidosis between 2000 and 2014: Cracking the glass ceiling of early death. Blood 2017, 129, 2111–2119. [Google Scholar] [CrossRef]
- Schulman, A.; Connors, L.H.; Weinberg, J.; Mendelson, L.M.; Joshi, T.; Shelton, A.C.; Sanchorawala, V. Patient outcomes in light chain (AL) amyloidosis: The clock is ticking from symptoms to diagnosis. Eur. J. Haematol. 2020, 105, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Vaxman, I.; Kumar, S.K.; Buadi, F.; Lacy, M.Q.; Dingli, D.; Hwa, Y.; Fonder, A.; Hobbs, M.; Hayman, S.; Kourelis, T.; et al. Outcomes among newly diagnosed AL amyloidosis patients with a very high NT-proBNP: Implications for trial design. Leukemia 2021, 35, 3604–3607. [Google Scholar] [CrossRef] [PubMed]
- Baker, K.R.; Rice, L. The amyloidoses: Clinical features, diagnosis and treatment. Methodist DeBakey Cardiovasc. J. 2012, 8, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Merlini, G. AL amyloidosis: From molecular mechanisms to targeted therapies. Hematol. Am. Soc. Hematol. Educ. Program 2017, 2017, e009586. [Google Scholar] [CrossRef]
- Imperlini, E.; Gnecchi, M.; Rognoni, P.; Sabidò, E.; Ciuffreda, M.C.; Palladini, G.; Espadas, G.; Mancuso, F.M.; Bozzola, M.; Malpasso, G.; et al. Proteotoxicity in cardiac amyloidosis: Amyloidogenic light chains affect the levels of intracellular proteins in human heart cells. Sci. Rep. 2017, 7, 15661. [Google Scholar] [CrossRef]
- Lavatelli, F.; Imperiini, E.; Orrù, S.; Rognoni, P.; Sarnataro, D.; Palladini, G.; Malpasso, G.; Soriano, M.E.; Di Fonzo, A.; Valentini, V.; et al. Novel mitochondrial protein interactors of immunoglobulin light chains causing heart amyloidosis. FASEB J. 2015, 29, 4614–4628. [Google Scholar] [CrossRef]
- Oerlemans, M.I.F.J.; Rutten, K.H.G.; Minnema, M.C.; Raymakers, R.A.P.; Asselbergs, F.W.; de Jonge, N. Cardiac amyloidosis: The need for early diagnosis. Neth. Heart J. 2019, 27, 525–536. [Google Scholar] [CrossRef]
- Gertz, M.A.; Dispenzieri, A. Systemic amyloidosis recognition, prognosis, and therapy: A systematic review. JAMA 2020, 324, 79–89. [Google Scholar] [CrossRef]
- Gillmore, J.D.; Hawkins, P.N. Pathophysiology and treatment of systemic amyloidosis. Nat. Rev. Nephrol. 2013, 9, 574–586. [Google Scholar] [CrossRef]
- Bhuva, A.N.; Bai, W.; Lau, C.; Davies, R.H.; Ye, Y.; Bulluck, H.; McAlindon, E.; Culotta, V.; Swoboda, P.P.; Captur, G.; et al. A Multicenter, Scan-Rescan, Human and Machine Learning CMR Study to Test Generalizability and Precision in Imaging Biomarker Analysis. Circ. Cardiovasc. Imaging 2019, 12, e009214. [Google Scholar] [CrossRef]
- Henglin, M.; Stein, G.; Hushcha, P.V.; Snoek, J.; Wiltschko, A.B.; Cheng, S. Machine Learning Approaches in Cardiovascular Imaging. Circ. Cardiovasc. Imaging 2017, 10, e005614. [Google Scholar] [CrossRef]
- Leiner, T.; Rueckert, D.; Suinesiaputra, A.; Baeßler, B.; Nezafat, R.; Išgum, I.; Young, A.A. Machine learning in cardiovascular magnetic resonance: Basic concepts and applications. J. Cardiovasc. Magn. Reson. 2019, 21, 61. [Google Scholar] [CrossRef]
- Martin-Isla, C.; Campello, V.M.; Izquierdo, C.; Raisi-Estabragh, Z.; Baeßler, B.; Petersen, S.E.; Lekadir, K. Image-Based Cardiac Diagnosis With Machine Learning: A Review. Front. Cardiovasc. Med. 2020, 7, 1. [Google Scholar] [CrossRef]
- Danieli, M.G.; Tonacci, A.; Paladini, A.; Longhi, E.; Moroncini, G.; Allegra, A.; Sansone, F.; Gangemi, S. A machine learning analysis to predict the response to intravenous and subcutaneous immunoglobulin in inflammatory myopathies. A proposal for a future multi-omics approach in autoimmune diseases. Autoimmun. Rev. 2022, 21, 103105. [Google Scholar] [CrossRef]
- Allegra, A.; Tonacci, A.; Sciaccotta, R.; Genovese, S.; Musolino, C.; Pioggia, G.; Gangemi, S. Machine Learning and Deep Learning Applications in Multiple Myeloma Diagnosis, Prognosis, and Treatment Selection. Cancers 2022, 14, 606. [Google Scholar] [CrossRef]
- Kumar, S.; Dispenzieri, A.; Katzmann, J.A.; Larson, D.R.; Colby, C.L.; Lacy, M.Q.; Hayman, S.R.; Buadi, F.K.; Leung, N.; Zeldenrust, S.R.; et al. Serum immunoglobulin free light-chain measurement in primary amyloidosis: Prognostic value and correlations with clinical features. Blood 2010, 116, 5126–5129. [Google Scholar] [CrossRef]
- Kim, H.-S.; Kim, H.S.; Shin, K.-S.; Song, W.; Kim, H.J.; Kim, H.S.; Park, M.J. Clinical comparisons of two free light chain assays to immunofixation electrophoresis for detecting monoclonal gammopathy. Biomed. Res. Int. 2014, 2014, 647238. [Google Scholar] [CrossRef]
- Rubinstein, S.M.; Stockerl-Goldstein, K. How to screen for monoclonal gammopathy in patients with a suspected amyloidosis. J. Am. Coll. Cardiol. CardioOnc. 2021, 3, 590–593. [Google Scholar] [CrossRef]
- Sanchorawala, V. Light-chain (AL) amyloidosis: Diagnosis and treatment. Clin. J. Am. Soc. Nephrol. 2006, 1, 1331–1341. [Google Scholar] [CrossRef]
- Palladini, G.; Russo, P.; Bosoni, T.; Verga, L.; Sarais, G.; Lavatelli, F.; Nuvolone, M.; Obici, L.; Casarini, S.; Donadei, S.; et al. Identification of amyloidogenic light chains requires the combination of serum-free light chain assay with immunofixation of serum and urine. Clin. Chem. 2009, 55, 499–504. [Google Scholar] [CrossRef]
- Wisniowski, B.; Wechalekar, A. Confirming the diagnosis of amyloidosis. Acta Haematol. 2020, 143, 312–321. [Google Scholar] [CrossRef] [PubMed]
- Gertz, M.A. Immunoglobulin light chain amyloidosis: 2016 update on diagnosis, prognosis, and treatment. Am. J. Hematol. 2016, 91, 947–956. [Google Scholar] [CrossRef] [PubMed]
- Lane, T.; Fontana, M.; Martinez-Naharro, A.; Quarta, C.C.; Whelan, C.J.; Petrie, A.; Rowczenio, D.M.; Gilbertson, J.A.; Hutt, D.F.; Rezk, T.; et al. Natural History, Quality of Life, and Outcome in Cardiac Transthyretin Amyloidosis. Circulation 2019, 140, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Ladefoged, B.; Dybro, A.; Povlsen, J.A.; Vase, H.; Clemmensen, T.S.; Poulsen, S.H. Diagnostic delay in wild type transthyretin cardiac amyloidosis—A clinical challenge. Int. J. Cardiol. 2020, 304, 138–143. [Google Scholar] [CrossRef]
- Adams, D.; Gonzalez-Duarte, A.; O’Riordan, W.D.; Yang, C.C.; Ueda, M.; Kristen, A.V.; Tournev, I.; Schmidt, H.H.; Coelho, T.; Berk, J.L.; et al. Patisiran, an RNAi Therapeutic, for Hereditary Transthyretin Amyloidosis. N. Engl. J. Med. 2018, 379, 11–21. [Google Scholar] [CrossRef]
- Bloom, M.W.; Gorevic, P.D. Cardiac Amyloidosis. Ann. Intern. Med. 2023. [Google Scholar] [CrossRef]
- Ruberg, F.L.; Grogan, M.; Hanna, M.; Kelly, J.W.; Maurer, M.S. Transthyretin Amyloid Cardiomyopathy: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2019, 73, 2872. [Google Scholar] [CrossRef]
- Canepa, M.; Fumagalli, C.; Tini, G.; Vincent-Tompkins, J.; Day, S.M.; Ashley, E.A.; Mazzarotto, F.; Ware, J.S.; Michels, M.; Jacoby, D.; et al. Temporal Trend of Age at Diagnosis in Hypertrophic Cardiomyopathy: An Analysis of the International Sarcomeric Human Cardiomyopathy Registry. Circ. Heart Fail. 2020, 13, e007230. [Google Scholar] [CrossRef]
- Canepa, M.; Vianello, P.F.; Porcari, A.; Merlo, M.; Scarpa, M. Cardiac amyloidosis: A changing epidemiology with open challenges. Vessel Plus 2022, 6, 30. [Google Scholar] [CrossRef]
- Gillmore, J.D.; Maurer, M.S.; Falk, R.H.; Merlini, G.; Damy, T.; Dispenzieri, A.; Wechalekar, A.D.; Berk, J.L.; Quarta, C.C.; Grogan, M.; et al. Nonbiopsy diagnosis of cardiac transthyretin amyloidosis. Circulation 2016, 133, 2404–2412. [Google Scholar] [CrossRef]
- Fontana, M.; Chung, R.; Hawkins, P.N.; Moon, J.C. Cardiovascular magnetic resonance for amyloidosis. Heart Fail. Rev. 2015, 20, 133–144. [Google Scholar] [CrossRef]
- Pandey, T.; Jambhekar, K.; Shaikh, R.; Lensing, S.; Viswamitra, S. Utility of the inversion scout sequence (TI scout) in diagnosing myocardial amyloid infltration. Int. J. Cardiovasc. Imaging 2013, 29, 103–112. [Google Scholar] [CrossRef]
- Aquaro, G.D.; Pugliese, N.R.; Perfetto, F.; Cappelli, F.; Barison, A.; Masci, P.G.; Passino, C.; Emdin, M. Myocardial signal intensity decay after gadolinium injection: A fast and effective method for the diagnosis of cardiac amyloidosis. Int. J. Cardiovasc. Imaging 2014, 30, 1105–1115. [Google Scholar] [CrossRef]
- Fontana, M.; Pica, S.; Reant, P.; Abdel-Gadir, A.; Treibel, T.A.; Banypersad, S.M.; Maestrini, V.; Barcella, W.; Rosmini, S.; Bulluck, H.; et al. Prognostic Value of Late Gadolinium Enhancement Cardiovascular Magnetic Resonance in Cardiac Amyloidosis. Circulation 2015, 132, 1570–1579. [Google Scholar] [CrossRef]
- Karamitsos, T.D.; Piechnik, S.K.; Banypersad, S.M.; Fontana, M.; Ntusi, N.B.; Ferreira, V.M.; Whelan, C.J.; Myerson, S.G.; Robson, M.D.; Hawkins, P.N.; et al. Noncontrast T1 mapping for the diagnosis of cardiac amyloidosis. JACC Cardiovasc. Imaging 2013, 6, 488–497. [Google Scholar] [CrossRef]
- Barison, A.; Aquaro, G.D.; Pugliese, N.R.; Cappelli, F.; Chiappino, S.; Vergaro, G.; Mirizzi, G.; Todiere, G.; Passino, C.; Masci, P.G.; et al. Measurement of myocardial amyloid deposition in systemic amyloidosis: Insights from cardiovascular magnetic resonance imaging. J. Intern. Med. 2015, 277, 605–614. [Google Scholar] [CrossRef]
- Rahman, J.E.; Helou, E.F.; Gelzer-Bell, R.; Thompson, R.E.; Kuo, C.; Rodriguez, E.R.; Hare, J.M.; Baughman, K.L.; Kasper, E.K. Noninvasive diagnosis of biopsy-proven cardiac amyloidosis. J. Am. Coll. Cardiol. 2004, 43, 410–415. [Google Scholar] [CrossRef]
- Cyrille, N.B.; Goldsmith, J.; Alvarez, J.; Maurer, M.S. Prevalence and prognostic significance of low QRS voltage among the three main types of cardiac amyloidosis. Am. J. Cardiol. 2014, 114, 1089–1093. [Google Scholar] [CrossRef]
- Rapezzi, C.; Merlini, G.; Quarta, C.C.; Riva, L.; Longhi, S.; Leone, O.; Salvi, F.; Ciliberti, P.; Pastorelli, F.; Biagini, E.; et al. Systemic cardiac amyloidoses: Disease profiles and clinical courses of the 3 main types. Circulation 2009, 120, 1203–1212. [Google Scholar] [CrossRef]
- Ramanathan, C.; Ghanem, R.; Jia, P.; Ryu, K.; Rudy, Y. Noninvasive electrocardiographic imaging for cardiac electrophysiology and arrhythmia. Nat. Med. 2004, 10, 422–428. [Google Scholar] [CrossRef]
- Murtagh, B.; Hammill, S.C.; Gertz, M.A.; Kyle, R.A.; Tajik, A.J.; Grogan, M. Electrocardiographic findings in primary systemic amyloidosis and biopsy-proven cardiac involvement. Am. J. Cardiol. 2005, 95, 535–537. [Google Scholar] [CrossRef]
- Merlo, M.; Porcari, A.; Pagura, L.; Cameli, M.; Vergaro, G.; Musumeci, B.; Biagini, E.; Canepa, M.; Crotti, L.; Imazio, M.; et al. A national survey on prevalence of possible echocardiographic red flags of amyloid cardiomyopathy in consecutive patients undergoing routine echocardiography: Study design and patients characterization-the first insight from the AC-TIVE Study. Eur. J. Prev. Cardio. 2021, 29, e173–e177. [Google Scholar] [CrossRef] [PubMed]
- Boldrini, M.; Cappelli, F.; Chacko, L.; Restrepo-Cordoba, M.A.; Lopez-Sainz, A.; Giannoni, A.; Aimo, A.; Baggiano, A.; Martinez-Naharro, A.; Whelan, C.; et al. Multiparametric Echocardiography Scores for the Diagnosis of Cardiac Amyloidosis. JACC Cardiovasc. Imaging. 2020, 13, 909–920. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.W.; Zheng, J.L.; Kaung, L.; Yan, H. Machine learning algorithms to automate differentiating cardiac amyloidosis from hypertrophic cardiomyopathy. Int. J. Cardiovasc. Imaging 2022, 39, 339–348. [Google Scholar] [CrossRef] [PubMed]
- Goto, S.; Solanki, D.; John, J.E.; Yagi, R.; Homilies, M.; Ichihara, G.; Katsumata, Y.; Gagging, H.K.; Itabashi, Y.; Macrae, C.A.; et al. Multinational Federated Learning Approach to Train ECG and Echocardiogram Models for Hypertrophic Cardiomyopathy Detection. Circulation 2022, 146, 755–769. [Google Scholar] [CrossRef] [PubMed]
- Duffy, G.; Cheng, P.P.; Yuan, N.; He, B.; Kwan, A.C.; Shun-Shin, M.J.; Alexander, K.M.; Ebinger, J.; Lungren, M.P.; Rader, F.; et al. High-Throughput Precision Phenotyping of Left Ventricular Hypertrophy With Cardiovascular Deep Learning. JAMA Cardiol. 2022, 7, 386–395. [Google Scholar] [CrossRef] [PubMed]
- Sammani, A.; Jansen, M.; de Vries, N.M.; de Jonge, N.; Baas, A.F.; Te Riele, A.S.J.M.; Asselbergs, F.W.; Oerlemans, M.I.F.J. Automatic Identification of Patients With Unexplained Left Ventricular Hypertrophy in Electronic Health Record Data to Improve Targeted Treatment and Family Screening. Front. Cardiovasc. Med. 2022, 9, 768847. [Google Scholar] [CrossRef] [PubMed]
- Davies, D.R.; Redfield, M.M.; Scott, C.G.; Minamisawa, M.; Grogan, M.; Dispenzieri, A.; Chareonthaitawee, P.; Shah, A.M.; Shah, S.J.; Wehbe, R.M.; et al. A Simple Score to Identify Increased Risk of Transthyretin Amyloid Cardiomyopathy in Heart Failure With Preserved Ejection Fraction. JAMA Cardiol. 2022, 7, 1036–1044. [Google Scholar] [CrossRef]
- Vassilios, V.S.; Cameron, D.; Prasad, S.K.; Gatehouse, P.D. Magnetic resonance imaging: Physics basics for the cardiologist. JRSM Cardiovasc. Dis. 2018, 7, 2048004018772237. [Google Scholar]
- Antonopoulos, A.S.; Almogheer, B.; Azzu, A.; Alati, E.; Papagkikas, P.; Cheong, J.; Clague, J.; Wechalekar, K.; Baksi, J.; Alpendurada, F. Typical and atypical imaging features of cardiac amyloidosis. Hell. J. Cardiol. 2021, 62, 312–314. [Google Scholar] [CrossRef]
- Kolossváry, M.; Karády, J.; Szilveszter, B.; Kitslaar, P.; Hoffmann, U.; Merkely, B.; Maurovich-Horvat, P. Radiomic Features Are Superior to Conventional Quantitative Computed Tomographic Metrics to Identify Coronary Plaques With Napkin-Ring Sign. Circ. Cardiovasc. Imaging 2017, 10, e006843. [Google Scholar] [CrossRef] [PubMed]
- Kolossváry, M.; Kellermayer, M.; Merkely, B.; Maurovich-Horvat, P. Cardiac computed tomography radiomics: A comprehensive review on radiomic techniques. J. Thorac. Imaging 2018, 33, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Ioannou, A.; Patel, R.K.; Razvi, Y.; Porcari, A.; Knight, D.; Martinez-Naharro, A.; Kotecha, T.; Venneri, L.; Chacko, L.; Brown, J.; et al. Multi-Imaging Characterization of Cardiac Phenotype in Different Types of Amyloidosis. JACC Cardiovasc. Imaging, 2022; Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Li, J.; Lin, L.; Shen, K.; Tian, Z.; Sun, J.; Zhang, C.; An, J.; Jin, Z.; Vliegenthart, R.; et al. Left and right ventricular myocardial deformation and late gadolinium enhancement: Incremental prognostic value in amyloid light-chain amyloidosis. Cardiovasc. Diagn. Ther. 2020, 10, 470–480. [Google Scholar] [CrossRef]
- Giusca, S.; Steen, H.; Montenbruck, M.; Patel, A.R.; Pieske, B.; Erley, J.; Kelle, S.; Korosoglou, G. Multi-parametric assessment of left ventricular hypertrophy using late gadolinium enhancement, T1 mapping and strain-encoded cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 2021, 23, 92. [Google Scholar] [CrossRef]
- Mohty, D.; Pradel, S.; Magne, J.; Fadel, B.; Boulogne, C.; Petitalot, V.; Raboukhi, S.; Darodes, N.; Damy, T.; Aboyans, V.; et al. Prevalence and prognostic impact of left-sided valve thickening in systemic light-chain amyloidosis. Clin. Res. Cardiol. 2016, 106, 331–340. [Google Scholar] [CrossRef]
- Steen, H.; Giusca, S.; Montenbruck, M.; Patel, A.R.; Pieske, B.; Florian, A.; Erley, J.; Kelle, S.; Korosoglou, G. Left and right ventricular strain using fast strain-encoded cardiovascular magnetic resonance for the diagnostic classification of patients with chronic non-ischemic heart failure due to dilated, hypertrophic cardiomyopathy or cardiac amyloidosis. J. Cardiovasc. Magn. Reson. 2021, 23, 45. [Google Scholar] [CrossRef]
- Sciacca, V.; Eckstein, J.; Körperich, H.; Fink, T.; Bergau, L.; El Hamriti, M.; Imnadze, G.; Guckel, D.; Fox, H.; Gerçek, M.; et al. Magnetic-Resonance-Imaging-Based Left Atrial Strain and Left Atrial Strain Rate as Diagnostic Parameters in Cardiac Amyloidosis. J. Clin. Med. 2022, 11, 3150. [Google Scholar] [CrossRef]
- Nemes, A.; Földeák, D.; Domsik, P.; Kalapos, A.; Kormányos, Á.; Borbényi, Z.; Forster, T. Right Atrial Deformation Analysis in Cardiac Amyloidosis–Results from the Three-Dimensional Speckle-Tracking Echocardiographic MAGYAR-Path Study. Arq. Bras. Cardiol. 2018, 111, 384–391. [Google Scholar] [CrossRef]
- Higashi, H.; Inoue, K.; Inaba, S.; Nakao, Y.; Kinoshita, M.; Miyazaki, S.; Miyoshi, T.; Akazawa, Y.; Kawakami, H.; Uetani, T.; et al. Restricted left atrial dilatation can visually differentiate cardiac amyloidosis from hypertrophic cardiomyopathy. ESC Heart Fail. 2021, 8, 3198–3205. [Google Scholar] [CrossRef]
- Liu, H.; Bai, P.; Xu, H.-Y.; Li, Z.-L.; Xia, C.-C.; Zhou, X.-Y.; Gong, L.-G.; Guo, Y.-K. Distinguishing Cardiac Amyloidosis and Hypertrophic Cardiomyopathy by Thickness and Myocardial Deformation of the Right Ventricle. Cardiol. Res. Pract. 2022, 2022, 4364279. [Google Scholar] [CrossRef]
- Nochioka, K.; Quarta, C.C.; Claggett, B.; Roca, G.Q.; Rapezzi, C.; Falk, R.H.; Solomon, S.D. Left atrial structure and function in cardiac amyloidosis. Eur. Heart J. Cardiovasc. Imaging 2017, 18, 1128–1137. [Google Scholar] [CrossRef] [PubMed]
- Eckstein, J.; Moghadasi, N.; Körperich, H.; Weise Valdés, E.; Sciacca, V.; Paluszkiewicz, L.; Burchert, W.; Piran, M. A Machine Learning Challenge: Detection of Cardiac Amyloidosis Based on Bi-Atrial and Right Ventricular Strain and Cardiac Function. Diagnostics 2022, 12, 2693. [Google Scholar] [CrossRef] [PubMed]
- Kellman, P.; Hansen, M.S. T1-mapping in the heart: Accuracy and precision. J. Cardiovasc. Magn. Reson. 2014, 16, 2. [Google Scholar] [CrossRef] [PubMed]
- Giri, S.; Chung, Y.C.; Merchant, A.; Mihai, G.; Rajagopalan, S.; Raman, S.V.; Simonetti, O.P. T2 quantification for improved detection of myocardial edema. J. Cardiovasc. Magn. Reson. 2009, 11, 56. [Google Scholar] [CrossRef] [PubMed]
- Kellman, P.; Hernando, D.; Arai, A.E. Myocardial fat imaging. Curr. Cardiovasc. Imaging Rep. 2010, 3, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Xue, H.; Brown, L.A.E.; Nielles-Vallespin, S.; Plein, S.; Kellman, P. Automatic in-line quantitative myocardial perfusion mapping: Processing algorithm and implementation. Magn. Reson. Med. 2020, 83, 712–730. [Google Scholar] [CrossRef]
- Kellman, P.; Hansen, M.S.; Nielles-Vallespin, S.; Nickander, J.; Themudo, R.; Ugander, M.; Xue, H. Myocardial perfusion cardiovascular magnetic resonance: Optimized dual sequence and reconstruction for quantification. J. Cardiovasc. Magn. Reson. 2017, 19, 43. [Google Scholar] [CrossRef]
- Nickander, J.; Themudo, R.; Sigfridsson, A.; Xue, H.; Kellman, P.; Ugander, M. Females have higher myocardial perfusion, blood volume and extracellular volume compared to males: An adenosine stress cardiovascular magnetic resonance study. Sci. Rep. 2020, 10, 10380. [Google Scholar] [CrossRef]
- Schulz-Menger, J.; Bluemke, D.A.; Bremerich, J.; Flamm, S.D.; Fogel, M.A.; Friedrich, M.G.; Kim, R.J.; von Knobelsdorff-Brenkenhoff, F.; Kramer, C.M.; Pennell, D.J.; et al. Standardized image interpretation and post-processing in cardiovascular magnetic resonance: 2020 update—Society for Cardiovascular Magnetic Resonance (SCMR): Board of Trustees Task Force on Standardized Post-Processing. J. Cardiovasc. Magn. Reson. 2020, 22, 19. [Google Scholar] [CrossRef]
- Bai, W.; Sinclair, M.; Tarroni, G.; Oktay, O.; Rajchl, M.; Vaillant, G.; Lee, A.M.; Aung, N.; Lukaschuk, E.; Sanghvi, M.M.; et al. Automated cardiovascular magnetic resonance image analysis with fully convolutional networks. J. Cardiovasc. Magn. Reson. 2018, 20, 65. [Google Scholar] [CrossRef] [PubMed]
- Bernard, O.; Lalande, A.; Zotti, C.; Cervenansky, F.; Yang, X.; Heng, P.A.; Cetin, I.; Lekadir, K.; Camara, O.; Gonzalez Ballester, M.A.; et al. Deep learning techniques for automatic MRI cardiac multi-structures segmentation and diagnosis: Is the problem solved? IEEE Trans. Med. Imaging 2018, 37, 2514–2525. [Google Scholar] [CrossRef] [PubMed]
- Xue, H.; Davies, R.H.; Brown, L.A.E.; Knott, K.D.; Kotecha, T.; Fontana, M.; Plein, S.; Moon, J.C.; Kellman, P. Automated inline analysis of myocardial perfusion MRI with deep learning. Radiol. Artif. Intell. 2020, 2, e200009. [Google Scholar] [CrossRef]
- Tao, Q.; Yan, W.; Wang, Y.; Paiman, E.H.M.; Shamonin, D.P.; Garg, P.; Plein, S.; Huang, L.; Xia, L.; Sramko, M.; et al. Deep learning-based method for fully automatic quantification of left ventricle function from cine MR images: A multivendor, multicenter study. Radiology 2019, 290, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Davies, R.H.; Augusto, J.B.; Bhuva, A.; Xue, H.; Treibel, T.A.; Ye, Y.; Hughes, R.K.; Bai, W.; Lau, C.; Shiwani, H.; et al. Precision measurement of cardiac structure and function in cardiovascular magnetic resonance using machine learning. J. Cardiovasc. Magn. Reson. 2022, 24, 16. [Google Scholar] [CrossRef]
- Xue, H.; Artico, J.; Fontana, M.; Moon, J.C.; Davies, R.H.; Kellman, P. Landmark Detection in Cardiac MRI by Using a Convolutional Neural Network. Radiology: Artif. Intell. 2021, 3, e200197. [Google Scholar] [CrossRef]
- Jiang, S.; Zhang, L.; Wang, J.; Li, X.; Hu, S.; Fu, Y.; Wang, X.; Hao, S.; Hu, C. Differentiating between cardiac amyloidosis and hypertrophic cardiomyopathy on non-contrast cine-magnetic resonance images using machine learning-based radiomics. Front. Cardiovasc. Med. 2022, 9, 1001269. [Google Scholar] [CrossRef]
- Antonopoulos, A.S.; Boutsikou, M.; Simantiris, S.; Angelopoulos, A.; Lazaros, G.; Panagiotopoulos, I.; Oikonomou, E.; Kanoupaki, M.; Tousoulis, D.; Mohiaddin, R.H.; et al. Machine learning of native T1 mapping radiomics for classification of hypertrophic cardiomyopathy phenotypes. Sci. Rep. 2021, 11, 23596. [Google Scholar] [CrossRef]
- Martini, N.; Aimo, A.; Barison, A.; Della Latta, D.; Vergaro, G.; Aquaro, G.D.; Ripoli, A.; Emdin, M.; Chiappino, D. Deep learning to diagnose cardiac amyloidosis from cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 2020, 22, 84. [Google Scholar] [CrossRef]
- Satriano, A.; Afzal, Y.; Sarim Afzal, M.; Fatehi Hassanabad, A.; Wu, C.; Dykstra, S.; Flewitt, J.; Feuchter, P.; Sandonato, R.; Heydari, B.; et al. Neural-Network-Based Diagnosis Using 3-Dimensional Myocardial Architecture and Deformation: Demonstration for the Differentiation of Hypertrophic Cardiomyopathy. Front. Cardiovasc. Med. 2020, 7, 584727. [Google Scholar] [CrossRef]
- Moharram, M.A.; Lamberts, R.R.; Whalley, G.; Williams, M.J.A.; Coffey, S. Myocardial tissue characterisation using echocardiographic deformation imaging. Cardiovasc. Ultrasound 2019, 17, 27. [Google Scholar] [CrossRef] [PubMed]
- Haland, T.F.; Almaas, V.M.; Hasselberg, N.E.; Saberniak, J.; Leren, I.S.; Hopp, E.; Edvardsen, T.; Haugaa, K.H. Strain echocardiography is related to fibrosis and ventricular arrhythmias in hypertrophic cardiomyopathy. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 613–621. [Google Scholar] [CrossRef] [PubMed]
- Popovic, Z.B.; Kwon, D.H.; Mishra, M.; Buakhamsri, A.; Greenberg, N.L.; Thamilarasan, M.; Flamm, S.D.; Thomas, J.D.; Lever, H.M.; Desai, M.Y. Association between regional ventricular function and myocardial fibrosis in hypertrophic cardiomyopathy assessed by speckle tracking echocardiography and delayed hyperenhancement magnetic resonance imaging. J. Am. Soc. Echocardiogr. 2008, 21, 1299–1305. [Google Scholar] [CrossRef]
- Delgado, V.; Marsan, N.A. Global and regional longitudinal strain assessment in hypertrophic cardiomyopathy. Circ. Cardiovasc. Imaging 2019, 12, e009586. [Google Scholar] [CrossRef] [PubMed]
- Pagourelias, E.D.; Mirea, O.; Duchenne, J.; Van Cleemput, J.; Delforge, M.; Bogaert, J.; Kuznetsova, T.; Voigt, J.U. Echo parameters for differential diagnosis in cardiac amyloidosis: A head-to-head comparison of deformation and nondeformation parameters. Circ. Cardiovasc. Imaging 2017, 10, e005588. [Google Scholar] [CrossRef]
- Gotschy, A.; Von Deuster, C.; Van Gorkum, R.J.H.; Gastl, M.; Vintschger, E.; Schwotzer, R.; Flammer, A.J.; Manka, R.; Stoeck, C.T.; Kozerke, S. Characterizing cardiac involvement in amyloidosis using cardiovascular magnetic resonance diffusion tensor imaging. J. Cardiovasc. Magn. Reson. 2019, 21, 56. [Google Scholar] [CrossRef]
- Satoskar, A.A.; Efebera, Y.; Hasan, A.; Brodsky, S.; Nadasdy, G.; Dogan, A.; Nadasdy, T. Strong transthyretin immunostaining: Potential pitfall in cardiac amyloid typing. Am. J. Surg. Pathol. 2011, 35, 1685–1690. [Google Scholar] [CrossRef]
- Solomon, A.; Murphy, C.L.; Westermark, P. Unreliability of immunohistochemistry for typing amyloid deposits. Arch. Pathol. Lab. Med. 2008, 132, 14. [Google Scholar] [CrossRef]
- Gilbertson, J.A.; Theis, J.D.; Vrana, J.A.; Lachmann, H.; Wechalekar, A.; Whelan, C.; Hawkins, P.N.; Dogan, A.; Gillmore, J.D. A comparison of immunohistochemistry and mass spectrometry for determining the amyloid fibril protein from formalin-fixed biopsy tissue. J. Clin. Pathol. 2015, 68, 314–317. [Google Scholar] [CrossRef]
- Lachmann, H.; Booth, D.R.; Booth, S.E.; Bybee, A.; Gilbertson, J.A.; Gillmore, J.D.; Pepys, M.B.; Hawkins, P.N. Misdiagnosis of Hereditary Amyloidosis as AL (Primary) Amyloidosis. N. Engl. J. Med. 2002, 346, 1786–1791. [Google Scholar] [CrossRef]
- Satoskar, A.A.; Burdge, K.; Cowden, D.J.; Nadasdy, G.M.; Hebert, L.A.; Nadasdy, T. Typing of amyloidosis in renal biopsies: Diagnostic pitfalls. Arch. Pathol. Lab. Med. 2007, 131, 917–922. [Google Scholar] [CrossRef] [PubMed]
- Schönland, S.O.; Hegenbart, U.; Bochtler, T.; Mangatter, A.; Hansberg, M.; Ho, A.D.; Lohse, P.; Röcken, C. Immunohistochemistry in the classification of systemic forms of amyloidosis: A systematic investigation of 117 patients. Blood 2012, 119, 488–493. [Google Scholar] [CrossRef] [PubMed]
- Abildgaard, N.; Rojek, A.M.; Møller, H.E.; Palstrøm, N.B.; Nyvold, C.G.; Rasmussen, L.M.; Hansen, C.T.; Beck, H.C.; Marcussen, N. Immunoelectron microscopy and mass spectrometry for classification of amyloid deposits. Amyloid 2020, 27, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Vrana, J.A.; Gamez, J.D.; Madden, B.J.; Theis, J.D.; Bergen, H.R., 3rd; Dogan, A. Classification of amyloidosis by laser microdissection and mass spectrometry-based proteomic analysis in clinical biopsy specimens. Blood 2009, 114, 4957–4959. [Google Scholar] [CrossRef]
- Brambilla, F.; Lavatelli, F.; Di Silvestre, D.; Valentini, V.; Rossi, R.; Palladini, G.; Obici, L.; Verga, L.; Mauri, P.; Merlini, G. Reliable typing of systemic amyloidoses through proteomic analysis of subcutaneous adipose tissue. Blood 2012, 119, 1844–1847. [Google Scholar] [CrossRef]
- Palstrøm, N.B.; Rojek, A.M.; Møller, H.E.H.; Hansen, C.T.; Matthiesen, R.; Rasmussen, L.M.; Abildgaard, N.; Beck, H.C. Classification of Amyloidosis by Model-Assisted Mass Spectrometry-Based Proteomics. Int. J. Mol. Sci. 2021, 23, 319. [Google Scholar] [CrossRef]
- Leguit, R.J.; Vink, A.; de Jonge, N.; Minnema, M.C.; Oerlemans, M.I.F. Endomyocardial biopsy with co-localization of a lymphoplasmacytic lymphoma and AL amyloidosis. Cardiovasc. Pathol. 2021, 53, 107348. [Google Scholar] [CrossRef]
- Winburn, I.; Ishii, T.; Sumikawa, T.; Togo, K.; Yasunaga, H. Estimating the Prevalence of Transthyretin Amyloid Cardiomyopathy in a Large In-Hospital Database in Japan. Cardiol. Ther. 2019, 8, 297–316. [Google Scholar] [CrossRef]
- Isogai, T.; Yasunaga, H.; Matsui, H.; Ueda, T.; Tanaka, H.; Horiguchi, H.; Fushimi, K. Hospital volume and cardiac complications of endomyocardial biopsy: A retrospective cohort study of 9508 adult patients using a nationwide inpatient database in Japan. Clin. Cardiol. 2015, 38, 164–170. [Google Scholar] [CrossRef]
- Statistics Bureau, Ministry of Internal Affairs and Communications Japan. Monthly Report, 2018. Available online: http://www.stat.go.jp/english/data/jinsui/tsuki/index.html (accessed on 13 March 2019).
- Tsuchihashi-Makaya, M.; Hamaguchi, S.; Kinugawa, S.; Yokota, T.; Goto, D.; Yokoshiki, H.; Kato, N.; Takeshita, A.; Tsutsui, H.; JCARE-CARD Investigators. Characteristics and outcomes of hospitalized patients with heart failure and reduced vs preserved ejection fraction. Report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ. J. 2009, 73, 1893–1900. [Google Scholar] [CrossRef]
- Huda, A.; Castaño, A.; Niyogi, A.; Schumacher, J.; Stewart, M.; Bruno, M.; Hu, M.; Ahmad, F.S.; Deo, R.C.; Shah, S.J. A machine learning model for identifying patients at risk for wild-type transthyretin amyloid cardiomyopathy. Nat Commun. 2021, 12, 2725. [Google Scholar] [CrossRef] [PubMed]
- Agibetov, A.; Seirer, B.; Dachs, T.M.; Koschutnik, M.; Dalos, D.; Rettl, R.; Duca, F.; Schrutka, L.; Agis, H.; Kain, R.; et al. Machine Learning Enables Prediction of Cardiac Amyloidosis by Routine Laboratory Parameters: A Proof-of-Concept Study. J. Clin. Med. 2020, 9, 1334. [Google Scholar] [CrossRef] [PubMed]
- Makin, O.S.; Serpell, L.C. Structures for amyloid fibrils. FEBS J. 2005, 272, 5950–5961. [Google Scholar] [CrossRef]
- Cao, Y.; Tang, X.; Yuan, M.; Han, W. Computational studies of protein aggregation mediated by amyloid: Fibril elongation and secondary nucleation. Prog. Mol. Biol. Transl. Sci. 2020, 170, 461–504. [Google Scholar] [CrossRef] [PubMed]
- Tian, J.; Wu, N.; Guo, J.; Fan, Y. Prediction of amyloid fibril-forming segments based on a support vector machine. BMC Bioinform. 2009, 10 (Suppl. S1), S45. [Google Scholar] [CrossRef]
- Kawashima, S.; Kanehisa, M. Aaindex: Amino acid index database. Nucleic Acids Res. 2000, 28, 374. [Google Scholar] [CrossRef]
- Liu, B.; Liu, F.; Wang, X.; Chen, J.; Fang, L.; Chou, K.-C. Pse-in-one: A web server for generating various modes of pseudo components of DNA, RNA, and protein sequences. Nucleic Acids Res. 2015, 43, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhang, Z.; Teng, Z.; Liu, X. Predamyl-mlp: Prediction of amyloid proteins using multilayer perceptron. Comput. Math. Methods Med. 2020. [Google Scholar] [CrossRef]
- Teng, Z.; Zhang, Z.; Tian, Z.; Li, Y.; Wang, G. ReRF-Pred: Predicting amyloidogenic regions of proteins based on their pseudo amino acid composition and tripeptide composition. BMC Bioinform. 2021, 22, 545. [Google Scholar] [CrossRef]
- Chou, K.-C. Pseudo amino acid composition and its applications in bioinformatics, proteomics and system biology. Curr. Proteom. 2009, 6, 262–274. [Google Scholar] [CrossRef]
- Liao, B.; Jiang, J.-B.; Zeng, Q.-G.; Zhu, W. Predicting apoptosis protein subcellular location with pseaac by incorporating tripeptide composition. Protein Pept. Lett. 2011, 18, 1086–1092. [Google Scholar] [CrossRef] [PubMed]
- Burdukiewicz, M.; Sobczyk, P.; Rödiger, S.; Duda-Madej, A.; Mackiewicz, P.; Kotulska, M. Amyloidogenic motifs revealed by n-gram analysis. Sci. Rep. 2017, 7, 12961. [Google Scholar] [CrossRef] [PubMed]
- Keresztes, L.; Szögi, E.; Varga, B.; Farkas, V.; Perczel, A.; Grolmusz, V. The budapest amyloid predictor and its applications. Biomolecules 2021, 11, 500. [Google Scholar] [CrossRef] [PubMed]
- Beerten, J.; Van Durme, J.; Gallardo, R.; Capriotti, E.; Serpell, L.; Rousseau, F.; Schymkowitz, J. WALTZ-DB: A benchmark database of amyloidogenic hexapeptides. Bioinformatics 2015, 31, 1698–1700. [Google Scholar] [CrossRef]
- Auriemma Citarella, A.; Di Biasi, L.; Risi, M.; Tortora, G. Snarer: New molecular descriptors for snare proteins classifcation. BMC Bioinform. 2022, 23, 148. [Google Scholar] [CrossRef]
- Auriemma Citarella, A.; Di Biasi, L.; De Marco, F.; Tortora, G. ENTAIL: YEt aNoTher amyloid fIbrils cLassifier. BMC Bioinform. 2022, 23, 517. [Google Scholar] [CrossRef]
- Dimopoulos, M.A.; Alexanian, R. Waldenstrom’s macroglobulinemia. Blood 1994, 83, 1452–1459. [Google Scholar] [CrossRef]
- Lee, C.C.; Perchiacca, J.M.; Tessier, P.M. Toward aggregation-resistant antibodies by design. Trends Biotechnol. 2013, 31, 612–620. [Google Scholar] [CrossRef]
- Tangakani, A.M.; Kumar, S.; Nagarajan, R.; Velmurugan, D.; Gromiha, M.M. GAP: Towards almost 100 percent prediction for β-strand-mediated aggregating peptides with distinct morphologies. Bioinformatics 2014, 30, 1983–1990. [Google Scholar] [CrossRef]
- Fernandez-Escamilla, A.M.; Rousseau, F.; Schymkowitz, J.; Serrano, L. Prediction of sequence-dependent and mutational effects on the aggregation of peptides and proteins. Nat. Biotechnol. 2004, 22, 1302–1306. [Google Scholar] [CrossRef]
- Maurer-Stroh, S.; Debulpaep, M.; Kuemmerer, N.; Lopez de la Paz, M.; Martins, I.C.; Reumers, J.; Morris, K.L.; Copland, A.; Serpell, L.; Serrano, L.; et al. Exploring the sequence determinants of amyloid structure using position-specific scoring matrices. Nat. Methods 2010, 7, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Trovato, A.; Seno, F.; Tosatto, S.C. Te PASTA server for protein aggregation prediction. Protein Eng. Des. Sel. 2007, 20, 521–523. [Google Scholar] [CrossRef] [PubMed]
- Conchillo-Solé, O.; de Groot, N.S.; Avilés, F.X.; Vendrell, J.; Daura, X.; Ventura, S. AGGRESCAN: A server for the prediction and evaluation of “hot spots” of aggregation in polypeptides. BMC Bioinform. 2007, 8, 65. [Google Scholar] [CrossRef] [PubMed]
- Garbuzynskiy, S.O.; Lobanov, M.Y.; Galzitskaya, O.V. FoldAmyloid: A method of prediction of amyloidogenic regions from protein sequence. Bioinformatics 2010, 26, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Prabakaran, R.; Rawat, P.; Kumar, S.; Gromiha, M.M. ANuPP: A versatile tool to predict aggregation nucleating regions in peptides and proteins. J. Mol. Biol. 2020, 1, 166707. [Google Scholar] [CrossRef]
- Prabakaran, R.; Rawat, P.; Tangakani, A.M.; Kumar, S.; Gromiha, M.M. Protein aggregation: In silico algorithms and applications. Biophys. Rev. 2021, 13, 71–89. [Google Scholar] [CrossRef]
- Buck, P.M.; Kumar, S.; Wang, X.; Agrawal, N.J.; Trout, B.L.; Singh, S.K. Computational methods to predict therapeutic protein aggregation. Methods Mol. Biol. 2012, 899, 425–451. [Google Scholar]
- Buck, P.M.; Kumar, S.; Singh, S.K. On the role of aggregation prone regions in protein evolution, stability, and enzymatic catalysis: Insights from diverse analyses. PLoS Comput. Biol. 2013, 9, e1003291. [Google Scholar] [CrossRef]
- Prabakaran, R.; Goel, D.; Kumar, S.; Gromiha, M.M. Aggregation prone regions in human proteome: Insights from large-scale data analyses. Proteins 2017, 85, 1099–1118. [Google Scholar] [CrossRef]
- Rawat, P.; Kumar, S.; Gromiha, M.M. An in-silico method for identifying aggregation rate enhancer and mitigator mutations in proteins. Int. J. Biol. Macromol. 2018, 118, 1157–1167. [Google Scholar] [CrossRef]
- Rawat, P.; Prabakaran, R.; Kumar, S.; Gromiha, M.M. AggreRATE-Pred: A mathematical model for the prediction of change in aggregation rate upon point mutation. Bioinformatics 2020, 36, 1439–1444. [Google Scholar] [CrossRef]
- Rawat, P.; Prabakaran, R.; Sakthivel, R.; Mary Thangakani, A.; Kumar, S.; Gromiha, M.M. CPAD 20: A repository of curated experimental data on aggregating proteins and peptides. Amyloid 2020, 27, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Rawat, P.; Prabakaran, R.; Kumar, S.; Gromiha, M.M. AbsoluRATE: An in-silico method to predict the aggregation kinetics of native proteins. BBA-Proteins Proteom. 2021, 1, 140682. [Google Scholar] [CrossRef] [PubMed]
- Briney, B.; Inderbitzin, A.; Joyce, C.; Burton, D.R. Commonality despite exceptional diversity in the baseline human antibody repertoire. Nature 2019, 566, 393–397. [Google Scholar] [CrossRef] [PubMed]
- David, M.P.C.; Concepcion, G.P.; Padlan, E.A. Using simple artificial intelligence methods for predicting amyloidogenesis in antibodies. BMC Bioinform. 2010, 11, 79. [Google Scholar] [CrossRef]
- Rawat, P.; Prabakaran, R.; Kumar, S.; Gromiha, M.M. Exploring the sequence features determining amyloidosis in human antibody light chains. Sci Rep. 2021, 11, 13785. [Google Scholar] [CrossRef]
- Bonnefous, L.; Kharoubi, M.; Bézard, M.; Oghina, S.; Le Bras, F.; Poullot, E.; Molinier-Frenkel, V.; Fanen, P.; Deux, J.F.; Audard, V.; et al. Assessing Cardiac Amyloidosis Subtypes by Unsupervised Phenotype Clustering Analysis. J. Am. Coll. Cardiol. 2021, 78, 2177–2192. [Google Scholar] [CrossRef]
- Ruberg, F.L. Phenotype Mapping in Cardiac Amyloidosis. J. Am. Coll. Cardiol. 2021, 78, 2193–2195. [Google Scholar] [CrossRef]
- Poterucha, T.J.; Elias, P.; Ruberg, F.L.; DeLuca, A.; Kinkhabwala, M.; Johnson, L.L.; Griffin, J.M.; Pandey, S.; Einstein, A.J.; Maurer, M.S. False Positive 99mTc-Pyrophosphate Scanning Leading to Inappropriate Tafamidis Prescriptions. JACC Cardiovasc. Imaging 2021, 14, 2042–2044. [Google Scholar] [CrossRef]
- Hanna, M.; Ruberg, F.L.; Maurer, M.S.; Dispenzieri, A.; Dorbala, S.; Falk, R.H.; Hoffman, J.; Jaber, W.; Soman, P.; Witteles, R.M.; et al. Cardiac Scintigraphy With Technetium-99m-Labeled Bone-Seeking Tracers for Suspected Amyloidosis: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2020, 75, 2851–2862. [Google Scholar] [CrossRef]
- Hughes, S.E. The pathology of hypertrophic cardiomyopathy. Histopathology 2004, 44, 412–427. [Google Scholar] [CrossRef] [PubMed]
- López-Cuenca, D.; Muñoz-Esparza, C.; Peñalver, M.N.; Alberola, A.G.; Blanes, J.R.G. Hypertrophic or hypertensive cardiomyopathy? Int. J. Cardiol. 2016, 203, 891–892. [Google Scholar] [CrossRef] [PubMed]
- Maron, M.S.; Rowin, E.J.; Maron, B.J. How to image hypertrophic cardiomyopathy. Circ. Cardiovasc. Imaging 2017, 10, e005372. [Google Scholar] [CrossRef]
- Lemery, R.; Kleinebenne, A.; Nihoyannopoulos, P.; Aber, V.; Alfonso, F.; McKenna, W.J. Q waves in hypertrophic cardiomyopathy in relation to the distribution and severity of right and left ventricular hypertrophy. J. Am. Coll. Cardiol. 1990, 16, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Maron, B.J.; Wolfson, J.K.; Ciró, E.; Spirito, P. Relation of electrocardiographic abnormalities and patterns of left ventricular hypertrophy identified by 2-dimensional echocardiography in patients with hypertrophic cardiomyopathy. Am. J. Cardiol. 1983, 51, 189–194. [Google Scholar] [CrossRef]
- Usui, M.; Inoue, H.; Suzuki, J.; Watanabe, F.; Sugimoto, T.; Nishikawa, J. Relationship between distribution of hypertrophy and electrocardiographic changes in hypertrophic cardiomyopathy. Am. Heart J. 1993, 126, 177–183. [Google Scholar] [CrossRef]
- Tison, G.H.; Zhang, J.; Delling, F.N.; Deo, R.C. Automated and interpretable patient ECG profiles for disease detection, tracking, and discovery. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005289. [Google Scholar] [CrossRef]
- Morita, S.X.; Kusunose, K.; Haga, A.; Sata, M.; Hasegawa, K.; Raita, Y.; Reilly, M.P.; Fifer, M.A.; Maurer, M.S.; Shimada, Y.J. Deep learning analysis of echocardiographic images to predict positive genotype in patients with hypertrophic cardiomyopathy. Front. Cardiovasc. Med. 2021, 8, 669860. [Google Scholar] [CrossRef]
- Ko, W.-Y.; Siontis, K.C.; Attia, Z.I.; Carter, R.E.; Kapa, S.; Ommen, S.R.; Demuth, S.J.; Ackerman, M.J.; Gersh, B.J.; Arruda-Olson, A.M.; et al. Detection of hypertrophic cardiomyopathy using a convolutional neural network-enabled electrocardiogram. J. Am. Coll. Cardiol. 2020, 75, 722–733. [Google Scholar] [CrossRef]
- Zhang, J.; Gajjala, S.; Agrawal, P.; Tison, G.H.; Hallock, L.A.; Beussink-Nelson, L.; Lassen, M.H.; Fan, E.; Aras, M.A.; Jordan, C.; et al. Fully automated echocardiogram interpretation in clinical practice. Circulation 2018, 138, 1623–1635. [Google Scholar] [CrossRef]
- Wasfy, J.H.; Singal, G.; O’Brien, C.; Blumenthal, D.M.; Kennedy, K.F.; Strom, J.B.; Spertus, J.A.; Mauri, L.; Normand, S.L.T.; Yeh, R.V. Enhancing the prediction of 30-day readmission after percutaneous coronary intervention using data extracted by querying of the electronic health record. Circ. Cardiovasc. Qual. Outcomes 2015, 8, 477–485. [Google Scholar] [CrossRef] [PubMed]
- García-García, E.; González-Romero, G.M.; Martín-Pérez, E.M.; Zapata Cornejo, E.D.; Escobar-Aguilar, G.; Cárdenas Bonnet, M.F. Real-World Data and Machine Learning to Predict Cardiac Amyloidosis. Int. J. Environ. Res. Public Health 2021, 18, 908. [Google Scholar] [CrossRef] [PubMed]
- Subbiah, V. The next generation of evidence-based medicine. Nat. Med. 2023, 29, 49–58. [Google Scholar] [CrossRef]
- Maurer, M.S.; Schwartz, J.H.; Gundapaneni, B.; Elliott, P.M.; Merlini, G.; Waddington-Cruz, M.; Kristen, A.V.; Grogan, M.; Witteles, R.; Damy, T.; et al. Tafamidis Treatment for Patients with Transthyretin Amyloid Cardiomyopathy. N. Engl. J. Med. 2018, 379, 1007–1016. [Google Scholar] [CrossRef] [PubMed]
- Falk, R.H.; Alexander, K.M.; Liao, R.; Dorbala, S. AL (Light-Chain) Cardiac Amyloidosis: A Review of Diagnosis and Therapy. J. Am. Coll. Cardiol. 2016, 68, 1323–1341. [Google Scholar] [CrossRef] [PubMed]
- Comenzo, R.L. Out, Out—Making Amyloid’s Candle Briefer. N. Engl. J. Med. 2015, 373, 1167–1169. [Google Scholar] [CrossRef] [PubMed]
- Rossi, M.; Varrà, G.G.; Porcari, A.; Saro, R.; Pagura, L.; Lalario, A.; Dore, F.; Bussani, R.; Sinagra, G.; Merlo, M. Re-Definition of the Epidemiology of Cardiac Amyloidosis. Biomedicines 2022, 10, 1566. [Google Scholar] [CrossRef]
| Amyloid Type | Protein | Distribution | Etiology | Diseases Associations |
|---|---|---|---|---|
| AL | Immunoglobulin light chain | Systemic and localized | Acquired | Plasma cell dyscrasia |
| AH | Immunoglobulin heavy chain | Systemic | Acquired | Plasma cell dyscrasia |
| ATTR | Transthyretin | Systemic | Acquired and hereditary | |
| ATTRwt | Wild-type transthyretin | Systemic | Acquired | Aging |
| ATTRv | TTR gene variant | Systemic | Hereditary | |
| AA | Serum amyloid A | Systemic | Acquired | Chronic inflammation |
| Aß2M | ß2-microglobulin | Systemic | Acquired and hereditary | Chronic hemodialysis |
| AANF | ANF | Localized | Acquired | Atrial fibrillation |
| Technique | Parameters | Population | IA Method | Ref. |
|---|---|---|---|---|
| Electrocardiographic evaluation | R-peak time | Treatment-naïve patients with CA | Unsupervised machine learning approach | [63] |
| Echocardiography data | Speckle tracking echocardiography | Monoclonal immunoglobulin light chain cardiac amyloidosis and patients with hypertrophic cardiomyopathy | Support vector machine, random forest, and gradient boosting machine | [66] |
| Time series of voltages recorded for 10 seconds at 250 Hz Echo videos standardized to 30 frames with 30 frames per second | Patients with hypertrophic cardiomyopathy | A federated learning approach | [67] | |
| Magnetic resonance | Multi-chamber strain and heart function | Patients with hypertrophic cardiomyopathy | Decision tree, k-nearest neighbor, SVM linear, and SVM radial basis function kernel algorithm processing | [85] |
| Left ventricular cavity and myocardium right ventricle | Adenosine stress and rest perfusion scans | A convolutional neural network | [95] | |
| Cine MRI images of left ventricle | Data from three major MR vendors | Convolutional neural networks | [96] | |
| Left ventricle blood volume and myocardium | Images from 1932 patients with multiple diseases from multiple centers | Convolutional neural networks | [97] | |
| Left ventricular volume in the end-systolic images | Patients with CA, HCM, and normal subjects | K-nearest neighbor, random forest, naïve Bayes, support vector machine, logistic regression, and artificial neural networks | [99] | |
| T1 mapping | Normal subjects, patients with left ventricular hypertrophy of various causes, patients with HCM, and patients with known cardiac amyloidosis | A random forest machine learning algorithm | [100] | |
| Biventricular systolic function | Subjects with suspected CA, unexplained left ventricular hypertrophy with blood dyscrasia and suspected light-chain amyloidosis | Three base convolutional neural networks | [101] | |
| Volumetric and strain markers | Patients from the Cardiovascular Imaging Registry of Canada | A neural-network-based model | [102] | |
| Mass spectrometry | Clusterin1, fibulin-1, vitronectin, complement, apolipoprotein E | Congo-red-positive and -negative amyloid-containing biopsies | A Boruta method applied on a random forest classifier | [118] |
| Method | Target | IA | Results | Ref. |
|---|---|---|---|---|
| Pafig | Hexpeptides associated with amyloid fibrillar aggregates | Support vector machine | Accuracy of 81% and Matthews correlation coefficient of 0.63 | [128] |
| Pse-in-One | DNA, RNA, and protein sequences | Support vector machine and neural network | Matthews correlation coefficient 0.739, sensitivity 0.781, specificity 0.927, F-measure 0.891, and accuracy 89.19% | [130] |
| PredAmylmultilayer | Protein sequences | Waikato environment for knowledge analysis | Accuracy 91.59%, specificity 0.950, and sensitivity 0.836 | [131] |
| ReRF-Pred | Composition of tripeptides and pseudo amino acids | Amyloidogenic regions | Accuracy 0.828, specificity 0.921, and Matthew correlation coefficient 0.619 | [132] |
| ENTAIL | Protein precursors | Machine learning | Accuracy 81.80%, sensibility 100%, and specificity 63.63% | [139] |
| VLAmY-Pred | Tripeptides composition | Random forest | Accuracy 79.7%, sensitivity 78.7%, and specificity 79.9% | [159] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Allegra, A.; Mirabile, G.; Tonacci, A.; Genovese, S.; Pioggia, G.; Gangemi, S. Machine Learning Approaches in Diagnosis, Prognosis and Treatment Selection of Cardiac Amyloidosis. Int. J. Mol. Sci. 2023, 24, 5680. https://doi.org/10.3390/ijms24065680
Allegra A, Mirabile G, Tonacci A, Genovese S, Pioggia G, Gangemi S. Machine Learning Approaches in Diagnosis, Prognosis and Treatment Selection of Cardiac Amyloidosis. International Journal of Molecular Sciences. 2023; 24(6):5680. https://doi.org/10.3390/ijms24065680
Chicago/Turabian StyleAllegra, Alessandro, Giuseppe Mirabile, Alessandro Tonacci, Sara Genovese, Giovanni Pioggia, and Sebastiano Gangemi. 2023. "Machine Learning Approaches in Diagnosis, Prognosis and Treatment Selection of Cardiac Amyloidosis" International Journal of Molecular Sciences 24, no. 6: 5680. https://doi.org/10.3390/ijms24065680
APA StyleAllegra, A., Mirabile, G., Tonacci, A., Genovese, S., Pioggia, G., & Gangemi, S. (2023). Machine Learning Approaches in Diagnosis, Prognosis and Treatment Selection of Cardiac Amyloidosis. International Journal of Molecular Sciences, 24(6), 5680. https://doi.org/10.3390/ijms24065680







