The Role of the Oral Microbiome in the Development of Diseases
Abstract
1. Introduction
2. Microbiome in the Oral Health
3. Oral Microbiome in Periodontal Diseases
4. Oral Microbiome in Systemic Diseases
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hernández, M.; Mayer, M.P.A.; Santi-Rocca, J. Editorial: The Human Microbiota in Periodontitis. Front. Cell. Infect. Microbiol. 2022, 12, 952205. [Google Scholar] [CrossRef]
- Greenwood, D.; Afacan, B.; Emingil, G.; Bostanci, N.; Belibasakis, G.N. Salivary Microbiome Shifts in Response to Periodontal Treatment Outcome. Proteom. Clin. Appl. 2020, 14, e2000011. [Google Scholar] [CrossRef]
- Zhang, Y.; Ding, Y.; Guo, Q. Probiotic Species in the Management of Periodontal Diseases: An Overview. Front. Cell. Infect. Microbiol. 2022, 12, 806463. [Google Scholar] [CrossRef]
- Van Dyke, T.E. Pro-resolving mediators in the regulation of periodontal disease. Mol. Asp. Med. 2017, 58, 21–36. [Google Scholar] [CrossRef] [PubMed]
- Herrero, E.R.; Fernandes, S.; Verspecht, T.; Ugarte-Berzal, E.; Boon, N.; Proost, P.; Teughels, W. Dysbiotic biofilms deregulate the periodontal inflammatory response. J. Dent. Res. 2018, 97, 547–555. [Google Scholar] [CrossRef]
- Kozak, M.; Dabrowska-Zamojcin, E.; Mazurek-Mochol, M.; Pawlik, A. Cytokines and Their Genetic Polymorphisms Related to Periodontal Disease. J. Clin. Med. 2020, 9, 4045. [Google Scholar] [CrossRef]
- Kirst, M.E.; Li, E.C.; Alfant, B.; Chi, Y.Y.; Walker, C.; Magnusson, I.; Wang, G.P. Dysbiosis and alterations in predicted functions of the subgingival microbiome in chronic periodontitis. Appl. Environ. Microbiol. 2015, 81, 783–793. [Google Scholar] [CrossRef] [PubMed]
- Heidari, Z. The association between proinflammatory gene polymorphisms and level of gingival tissue degrada tion in chronic periodontal disease. Gene Cell Tissue 2014, 1, e21898. [Google Scholar] [CrossRef]
- Heidari, Z.; Moudi, B.; Mahmoudzadeh-Sagheb, H. Immunomodulatory factors gene polymorphisms in chronic periodontal disease: An overview. BMC Oral Health 2019, 19, 29. [Google Scholar] [CrossRef]
- Di Stefano, M.; Polizzi, A.; Santonocito, S.; Romano, A.; Lombardi, T.; Isola, G. Impact of Oral Microbiome in Periodontal Health and Periodontitis: A Critical Review on Prevention and Treatment. Int. J. Mol. Sci. 2022, 23, 5142. [Google Scholar] [CrossRef]
- Cheng, W.C.; van Asten, S.D.; Burns, L.A.; Evans, H.G.; Walter, G.J.; Hashim, A.; Hughesand, F.J.; Taams, L.S. Periodontal disease-associated pathogens P. gingivalis and A. actinomycetemcomitans activate human CD14+ mono cytes leading to enhanced Th17/IL-17 responses. Eur. J. Immunol. 2016, 46, 2211–2221. [Google Scholar] [CrossRef]
- Johnson, G.K.; Guthmiller, J.M. The impact of cigarette smoking on periodontal disease and treatment. Periodontol. 2000 2007, 44, 178–194. [Google Scholar] [CrossRef]
- Popa, G.V.; Costache, A.; Badea, O.; Cojocaru, M.O.; Mitroi, G.; Lazăr, A.C.; Olimid, D.-A.; Mogoantă, L. Histopathological and immunohistochemical study of periodontal changes in chronic smokers. Rom. J. Morphol. Embryol. 2021, 62, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Sawant, S.; Dugad, J.; Parikh, D.; Srinivasan, S.; Singh, H. Oral Microbial Signatures of Tobacco Chewers and Oral Cancer Patients in India. Pathogens 2023, 12, 78. [Google Scholar] [CrossRef] [PubMed]
- Genco, R.J.; Grossi, S.G.; Ho, A.; Nishimura, F.; Murayama, Y. A proposed model linking inflammation to obesity, diabetes, and periodontal infections. J. Periodontol. 2005, 76 (Suppl. S11), 2075–2084. [Google Scholar] [CrossRef] [PubMed]
- Carrizales-Sepúlveda, E.F.; Ordaz-Farías, A.; Vera-Pineda, R.; Flores-Ramírez, R. Periodontal disease, systemic in flammation and the risk of cardiovascular disease. Heart Lung Circ. 2018, 27, 1327–1334. [Google Scholar] [CrossRef]
- Kim, J.; Amar, S. Periodontal disease and systemic conditions: A bidirectional relationship. Odontology 2006, 94, 10–21. [Google Scholar] [CrossRef]
- Nibali, L.; Bayliss-Chapman, J.; Almofareh, S.A.; Zhou, Y.; Divaris, K.; Vieira, A.R. What is the heritability periodotitis? A systematic review. J. Dent. Res. 2019, 98, 632–641. [Google Scholar] [CrossRef] [PubMed]
- López, R.; Smith, P.; Göstemeyer, G.; Schwendicke, F. Ageing, dental caries and periodontal diseases. J. Clin. Periodontol. 2017, 44, S145–S152. [Google Scholar] [CrossRef]
- Belibasakis, G.N. Microbiological changes of the ageing oral cavity. Arch. Oral Biol. 2018, 96, 230–232. [Google Scholar] [CrossRef]
- Hajishengallis, G.; Lamont, R.J. Beyond the red complex and into more complexity: The Polymicrobial Synergy and Dysbiosis (PSD) model of periodontal disease etiology. Mol. Oral Microbiol. 2012, 27, 409–419. [Google Scholar] [CrossRef]
- Najmanova, L.; Sabova, L.; Lenartova, M.; Janatova, T.; Mysak, J.; Vetrovsky, T.; Tesinska, B.; Novotna, G.B.; Koberska, M.; Broukal, Z.; et al. R/G value—A numeric index of periodontal health. Front. Cell. Infect. Microbiol. 2021, 11, 602643. [Google Scholar] [CrossRef]
- Hajishengallis, G. Periodontitis: From microbial immune subversion to systemic inflammation. Nat. Rev. Immunol. 2015, 15, 30–44. [Google Scholar] [CrossRef]
- Deo, P.N.; Deshmukh, R. Oral microbiome: Unveiling the fundamentals. J. Oral. Maxillofac Pathol. JOMFP 2019, 23, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Mahasneh, S.A.; Mahasneh, A.M. Probiotics: A Promising Role in Dental Health. Dent J. 2017, 5, 26. [Google Scholar] [CrossRef] [PubMed]
- Thuy, D.; Devine, D.; Marsh, P. Oral biofilms: Molecular analysis, challenges, and future prospects in dental diagnostics. Clin. Cosm. Investig. Dent. 2013, 5, 11–19. [Google Scholar]
- Marsh, P.D.; Zaura, E. Dental biofilm: Ecological interactions in health and disease. J. Clin. Periodontol. 2017, 44 (Suppl. S18), S12–S22. [Google Scholar] [CrossRef] [PubMed]
- Escapa, I.F.; Chen, T.; Huang, Y.; Gajare, P.; Dewhirst, F.E.; Lemon, K.P. New insights into human nostril microbiome from the expanded Human Oral Microbiome Database (eHOMD): A resource for the microbiome of the human aerodigestive tract. MSystems 2018, 3, e00187-18. [Google Scholar] [CrossRef]
- Bartnicka, D.; Gonzalez-Gonzalez, M.; Sykut, J.; Koziel, J.; Ciaston, I.; Adamowicz, K.; Bras, G.; Zawrotniak, M.; Karkowska-Kuleta, J.; Satala, D.; et al. Candida albicans Shields the Periodontal Killer Porphyromonas gingivalis from Recognition by the Host Immune System and Supports the Bacterial Infection of Gingival Tissue. Int. J. Mol. Sci. 2020, 21, 1984. [Google Scholar] [CrossRef]
- Barros, P.P.; Ribeiro, F.C.; Rossoni, R.D. Influence of Candida krusei and Candida glabrata on Candida albicans gene expression In Vitro biofilms. Arch. Oral Biol. 2016, 64, 92–101. [Google Scholar] [CrossRef]
- Jorgensen, M.R.; Kragelund, C.; Jansen, P.; Keller, M.K.; Twetman, S. Probiotic Lactobacillus reuteri has antifungal effects on oral Candida species In Vitro. Arch. Oral Biol. 2017, 9, 127–135. [Google Scholar] [CrossRef]
- Nobbs, A.H.; Jenkinson, H.F. Interkingdom networking within the oral micro-biome. Microbes Infect. 2015, 17, 484–492. [Google Scholar] [CrossRef]
- Ng, H.M.; Kin, L.X.; Dashper, S.G.; Slakeski, N.; Butler, C.A.; Reynolds, E.C. Bacterial interactions in pathogenic subgingival plaque. Microb. Pathog. 2016, 94, 60–69. [Google Scholar] [CrossRef]
- Belstrøm, D.; Constancias, F.; Markvart, M.; Sikora, M.; Sorensen, C.E.; Givskov, M. Transcriptional Activity of Predominant Streptococcus Species at Multiple Oral Sites Associate With Periodontal Status. Front. Cell. Infect. Microbiol. 2021, 11, 752664. [Google Scholar] [CrossRef] [PubMed]
- López-López, A.; Camelo-Castillo, A.; Ferrer, M.D.; Simon-Soro, A.; Mira, A. Health-Associated Niche Inhabitants as Oral Probiotics: The Case of Streptococcus dentisani. Front. Microbiol. 2017, 8, 379. [Google Scholar] [CrossRef]
- Esteban-Fernandez, A.; Ferrer, M.D.; Zorraquin-Pena, I.; Lopez-Lopez, A.; Moreno-Arribas, M.V.; Mira, A. In Vitro Beneficial Effects of Streptococcus dentisani as Potential Oral Probiotic for Periodontal Diseases. J. Periodontol. 2019, 90, 1346–1355. [Google Scholar] [CrossRef] [PubMed]
- Di Pierro, F.; Zanvit, A.; Nobili, P.; Risso, P.; Fornaini, C. Cariogram Outcome After 90 Days of Oral Treatment With Streptococcus salivarius M18 in Children at High Risk for Dental Caries: Results of a Randomized, Controlled Study. Clin. Cosmet. Investig. Dent. 2015, 7, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Hill, C.; Guarner, F.; Reid, G.; Gibson, G.R.; Merenstein, D.J.; Pot, B.; Morelli, L.; Canani, R.B.; Flint, H.J.; Salminen, S.; et al. Expert Consensus Document. The International Scientific Association for Probiotics and Prebiotics Consensus Statement on the Scope and Appropriate Use of the Term Probiotic. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 506–514. [Google Scholar] [CrossRef] [PubMed]
- Ince, G.; Gursoy, H.; Ipci, S.D.; Cakar, G.; Emekli-Alturfan, E.; Yilmaz, S. Clinical and Biochemical Evaluation of Lozenges Containing Lactobacillus reuteri as an Adjunct to Non-Surgical Periodontal Therapy in Chronic Periodontitis. J. Periodontol. 2015, 86, 746–754. [Google Scholar] [CrossRef]
- Sivamaruthi, B.S.; Kesika, P.; Chaiyasut, C. A Review of the Role of Probiotic Supplementation in Dental Caries. Probiotics Antimicrob. Proteins 2020, 12, 1300–1309. [Google Scholar] [CrossRef]
- Ohshima, T.; Kojima, Y.; Seneviratne, C.J.; Maeda, N. Therapeutic Application of Synbiotics, a Fusion of Probiotics and Prebiotics, and Biogenics as a New Concept for Oral Candida Infections: A Mini Review. Front. Microbiol. 2016, 7, 10. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.I.; Shin, I.S.; Jeon, J.G.; Yang, Y.M.; Kim, J.G.; Lee, D.W. The Effect of Probiotics on Halitosis: A Systematic Review and Meta-Analysis. Probiotics Antimicrob. Proteins 2019, 11, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Allaker, R.P.; Stephen, A.S. Use of Probiotics and Oral Health. Curr. Oral. Health Rep. 2017, 4, 309–318. [Google Scholar] [CrossRef]
- Kawai, T.; Ohshima, T.; Tanaka, T.; Ikawa, S.; Tani, A.; Inazumi, N.; Shin, R.; Itoh, Y.; Meyer, K.; Maeda, N. Limosi lactobacillus (Lactobacillus) fermentum ALAL020, a Probiotic Candidate Bacterium, Produces a Cyclic Dipeptide That Suppresses the Periodontal Pathogens Porphyromonas gingivalis and Prevotella intermedia. Front Cell. Infect Microbiol. 2022, 12, 804334. [Google Scholar] [CrossRef] [PubMed]
- Swanson, K.S.; Gibson, G.R.; Hutkins, R.; Reimer, R.A.; Reid, G.; Verbeke, K.; Scott, K.P.; Holscher, H.D.; Azad, M.B.; Delzenne, N.M.; et al. The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of synbiotics. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 687–701. [Google Scholar] [CrossRef] [PubMed]
- Duraisamy, V.; Geethapriya, P.R.; Bharath, C.; Niveditha, R.S.; John, J.B. Role of probiotics and synbiotics on inhibiting Streptococcus mutans level in saliva of children: A randomized controlled trial. J. Indian Soc. Pedod. Prev. Dent. 2021, 39, 275–278. [Google Scholar] [CrossRef]
- Willis, J.R.; Gabaldón, T. The Human Oral Microbiome in Health and Disease: From Sequences to Ecosystems. Microorganisms 2020, 8, 308. [Google Scholar] [CrossRef]
- Wilson, M. Bacteriology of Humans: An Ecological Perspective; Blackwell Publishing Ltd.: Hoboken, NJ, USA, 2008. [Google Scholar]
- Liu, B.; Faller, L.L.; Klitgord, N.; Mazumdar, V.; Ghodsi, M.; Sommer, D.D.; Gibbons, T.R.; Treangen, T.J.; Chang, Y.-C.; Li, S.; et al. Deep sequencing of the oral microbiome reveals signatures of periodontal disease. PLoS ONE 2012, 7, e37919. [Google Scholar] [CrossRef]
- Stamatova, I.; Meurman, J.H. Probiotics: Health benefits in the mouth. Am. J. Dent. 2009, 22, 329–338. [Google Scholar]
- De Geest, S.; Laleman, I.; Teughels, W.; Dekeyser, C.; Quirynen, M. Periodontal diseases as a source of halitosis: A review of the evidence and treatment approaches for dentists and dental hygienists. Periodontol. 2000 2016, 71, 213–227. [Google Scholar] [CrossRef]
- Sterer, N.; Shaharabany, M.; Rosenberg, M. Beta-Galactosidase activity and H(2)S production in an experimental oral biofilm. J. Breath Res. 2009, 3, 016006. [Google Scholar] [CrossRef] [PubMed]
- Bornstein, M.M.; Kislig, K.; Hoti, B.B.; Seemann, R.; Lussi, A. Prevalence of halitosis in the population of the city of Bern, Switzerland: A study comparing self-reported and clinical data. Eur. J. Oral Sci. 2009, 117, 261–267. [Google Scholar] [CrossRef] [PubMed]
- De Lima, P.O.; Nani, B.D.; Rolim, G.S.; Groppo, F.C.; Franz-Montan, M.; Alves De Moraes, A.B.; Cogo-Müller, K.; Marcondes, F.K. Effects of academic stress on the levels of oral volatile sulfur compounds, halitosis-related bacteria and stress biomarkers of healthy female undergraduate students. J. Breath Res. 2020, 14, 036005. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Cannon, R.D.; Ji, P.; Farella, M.; Mei, L. Halitosis: Prevalence, risk factors, sources, measurement and treatment—A review of the literature. Aust. Dent. J. 2020, 65, 4–11. [Google Scholar] [CrossRef]
- Hampelska, K.; Jaworska, M.M.; Babalska, Z.Ł.; Karpiński, T.M. The Role of Oral Microbiota in Intra-Oral Halitosis. J. Clin. Med. 2020, 9, 2484. [Google Scholar] [CrossRef]
- Nalcaci, R.; Sonmez, I.S. Evaluation of oral malodor in children. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2008, 106, 384–388. [Google Scholar] [CrossRef]
- Wu, Y.; Chi, X.; Zhang, Q.; Chen, F.; Deng, X. Characterization of the salivary microbiome in people with obesity. PeerJ 2018, 6, e4458. [Google Scholar] [CrossRef]
- Yitzhaki, S.; Reshef, L.; Gophna, U.; Rosenberg, M.; Sterer, N. Microbiome associated with denture malodour. J. Breath Res. 2018, 12, 027103. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhu, C.; Cao, G.; Zhan, J.; Feng, X.; Chen, X. Dynamic Alterations of Oral Microbiota Related to Halitosis in Preschool Children. Front. Cell. Infect. Microbiol. 2021, 11, 599467. [Google Scholar] [CrossRef]
- Saito, A.; Kokubu, E.; Inagaki, S.; Imamura, K.; Kita, D.; Lamont, R.J.; Ishihara, K. Porphyromonas Gingivalis Entry Into Gingival Epithelial Cells Modulated by Fusobacterium nucleatum is Dependent on Lipid Rafts. Microb. Pathog. 2012, 53, 234–242. [Google Scholar] [CrossRef]
- Chen, Y.; Huang, Z.; Tang, Z.; Huang, Y.; Huang, M.; Liu, H.; Ziebolz, D.; Schmalz, G.; Jia, B.; Zhao, J. More Than Just a Periodontal Pathogen -the Research Progress on Fusobacterium nucleatum. Front. Cell. Infect. Microbiol. 2022, 12, 815318. [Google Scholar] [CrossRef]
- Kang, M.S.; Lim, H.S.; Kim, S.M.; Lee, H.C.; Oh, J.S. Effect of Weissella cibaria on Fusobacterium nucleatum induced Interleukin-6 and Interleukin-8 Production in KB Cells. J. Bacteriol. Virol. 2011, 41, 9–18. [Google Scholar] [CrossRef]
- Suzuki, N.; Yoneda, M.; Tanabe, K.; Fujimoto, A.; Iha, K.; Seno, K.; Yamada, K.; Iwamoto, T.; Masuo, Y.; Hirofuji, T. Lactobacillus salivarius WB21–containing Tablets for the Treatment of Oral Malodor: A Double-Blind, Randomized, Placebo-Controlled Crossover Trial. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2014, 117, 462–470. [Google Scholar] [CrossRef]
- Lenartova, M.; Tesinska, B.; Janatova, T.; Hrebicek, O.; Mysak, J.; Janata, J.; Najmanova, L. The Oral Microbiome in Periodontal Health. Front. Cell. Infect. Microbiol. 2021, 11, 629723. [Google Scholar] [CrossRef]
- Pignatelli, P.; Fabietti, G.; Ricci, A.; Piattelli, A.; Curia, M.C. How Periodontal Disease and Presence of Nitric Oxide Reducing Oral Bacteria Can Affect Blood Pressure. Int. J. Mol. Sci. 2020, 21, 7538. [Google Scholar] [CrossRef]
- Reher, V.G.; Zenóbio, E.G.; Costa, F.O.; Reher, P.; Soares, R.V. Nitric oxide levels in saliva increase with severity of chronic periodontitis. J. Oral Sci. 2007, 49, 271–276. [Google Scholar] [CrossRef]
- Sampaio-Maia, B.; Caldas, I.M.; Pereira, M.L.; Perez-Mongiovi, D.; Araujo, R. The oral microbiome in health and its implication in oral and systemic diseases. Adv. Appl. Microbiol. 2016, 97, 171–210. [Google Scholar] [PubMed]
- Melo-Dias, S.; Cabral, M.; Furtado, A.; Souto-Miranda, S.; Mendes, M.A.; Cravo, J.; Almeida, C.R.; Marques, A.; Sousa, A. Responsiveness to pulmonary rehabilitation in COPD is associated with changes in microbiota. Respir Res. 2023, 24, 29. [Google Scholar] [CrossRef] [PubMed]
- Millares, L.; Monso, E. The Microbiome in COPD: Emerging Potential for Microbiome-Targeted Interventions. Int. J. Chron. Obstruct. Pulmon. Dis. 2022, 17, 1835–1845. [Google Scholar] [CrossRef]
- Tiew, P.Y.; Jaggi, T.K.; Chan, L.L.Y.; Chotirmall, S.H. The airway microbiome in COPD, bronchiectasis and bronchiectasis-COPD overlap. Clin. Respir. J. 2021, 15, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Mammen, M.J.; Sethi, S. COPD and the microbiome. Respirology 2016, 21, 590–599. [Google Scholar] [CrossRef]
- Whiley, R.A.; Fleming, E.V.; Makhija, R.; Waite, R.D. Environment and colonisation sequence are key parameters driving cooperation and competition between Pseudomonas aeruginosa cystic fibrosis strains and oral commensal streptococci. PLoS ONE 2015, 10, e0115513. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Kreth, J. The role of hydrogen peroxide in environmental adaptation of oral microbial communities. Oxidative Med. Cell. Longev. 2012, 2012, 717843. [Google Scholar] [CrossRef] [PubMed]
- Haran, J.P.; Bradley, E.; Zeamer, A.L.; Cincotta, L.; Salive, M.C.; Dutta, P.; Mutaawe, S.; Anya, O.; Meza-Segura, M.; Moormann, A.M.; et al. Inflammation-type dysbiosis of the oral microbiome as sociates with the duration of COVID-19 symptoms and long COVID. JCI Insight 2021, 6, e152346. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Khan, Z. COVID-2019-associated overexpressed Prevotella proteins mediated host-pathogen interactions and their role in coronavirus outbreak. Bioinformatics 2020, 36, 4065–4069. [Google Scholar] [CrossRef]
- Van den Bogert, B.; Meijerink, M.; Zoetendal, E.G.; Wells, J.M.; Kleerebezem, M. Immunomodulatory properties of Streptococcus and Veillonella isolates from the human small intestine microbiota. PLoS ONE 2014, 9, e114277. [Google Scholar] [CrossRef]
- Segal, L.N.; Clemente, J.C.; Tsay, J.-C.J.; Koralov, S.B.; Keller, B.C.; Wu, B.G.; Alison, M.; Shen, N.; Ghedin, E.; Morris, A.; et al. Enrichment of the lung microbiome with oral taxa is associated with lung inflammation of a Th17 phenotype. Nat. Microbiol. 2016, 1, 16031. [Google Scholar] [CrossRef]
- Quigley, E.M.M. Microbiota-brain-gut axis and neurodegenerative diseases. Curr. Neurol. Neurosci. Rep. 2017, 17, 94. [Google Scholar] [CrossRef]
- Nagarajan, A.; Srivastava, H.; Morrow, C.D.; Sun, L.Y. Characterizing the gut microbiome changes with aging in a Novel Alzheimer’s disease rat model. Aging 2023, 15, 59–471. [Google Scholar] [CrossRef]
- Jin, J.; Xu, Z.; Zhang, L.; Zhang, C.; Zhao, X.; Mao, Y.; Zhang, H.; Liang, X.; Wu, J.; Yang, Y.; et al. Gut-derived β-amyloid: Likely a centerpiece of the gut-brain axis contributing to Alzheimer’s pathogenesis. Gut Microbes 2023, 15, 2167172. [Google Scholar] [CrossRef]
- Barrett, E.; Ross, R.P.; O’Toole, P.W.; Fitzgerald, G.F.; Stanton, C. γ-Aminobutyric acid production by culturable bacteria from the human intestine. J. Appl. Microbiol. 2012, 113, 411–417. [Google Scholar] [CrossRef]
- Lyte, M. Probiotics function mechanistically as delivery vehicles for neuroactive compounds: Microbial endocrinology in the design and use of probiotics. Bioessays 2011, 33, 574–581. [Google Scholar] [CrossRef]
- Ruddick, J.P.; Evans, A.K.; Nutt, D.J.; Lightman, S.; Rook, G.; Lowry, C.A. Tryptophan metabolism in the central nervous system: Medical implications. Expert Rev. Mol. Med. 2006, 31, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Widner, B.; Leblhuber, F.; Walli, J.; Tilz, G.P.; Demel, U.; Fuchs, D. Tryptophan degradation and immune activation in Alzheimer’s disease. J. Neural. Transm. 1996, 107, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Gulaj, E.; Pawlak, K.; Bien, B.; Pawlak, D. Kynurenine and its metabolites in Alzheimer’s disease patients. Adv. Med. Sci. 2010, 55, 204–211. [Google Scholar] [CrossRef]
- Du, X.; Wang, X.; Geng, M. Alzheimer’s disease hypothesis and related therapies. Transl. Neurodegener. 2018, 7, 2. [Google Scholar] [CrossRef] [PubMed]
- Bienenstock, J.; Kunze, W.; Forsythe, P. Microbiota and the gut-brain axis. Nutr. Rev. 2015, 73 (Suppl. S1), 28–31. [Google Scholar] [CrossRef]
- Frost, G.; Sleeth, M.L.; Sahuri-Arisoylu, M.; Lizarbe, B.; Cerdan, S.; Brody, L.; Anastasovska, J.; Ghourab, S.; Hankir, M.; Zhang, S.; et al. The short-chain fatty acid acetate reduces appetite via a central homeostatic mechanism. Nat. Commun. 2014, 5, 3611. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Lukiw, W.J. Microbiome-generated amyloid and potential impact on amyloidogenesis in Alzheimer’s disease (AD). Nat. Sci. 2015, 1, e138. [Google Scholar]
- Hill, J.M.; Lukiw, W.J. Microbial-generated amyloids and Alzheimer’s disease (AD). Front. Aging Neurosci. 2015, 7, 9. [Google Scholar] [CrossRef]
- Sanchez-Ramos, J.; Song, S.; Sava, V.; Catlow, B.; Lin, X.; Mori, T.; Cao, C.; Arendash, G.W. Granulocyte colony stimulating factor decreases brain amyloid burden and reverses cognitive impairment in Alzheimer’s mice. Neuroscience 2009, 163, 55–72. [Google Scholar] [CrossRef] [PubMed]
- Hassan, W.M.; Dostal, V.; Huemann, B.N.; Yerg, J.E.; Link, C.D. Identifying Aβ-specific pathogenic mechanisms using a nematode model of Alzheimer’s disease. Neurobiol. Aging 2015, 36, 857–866. [Google Scholar] [CrossRef] [PubMed]
- Arimatsu, K.; Yamada, H.; Miyazawa, H.; Minagawa, T.; Nakajima, M.; Ryder, M.I.; Gotoh, K.; Motooka, D.; Nakamura, S.; Iida, T.; et al. Oral pathobiont induces systemic inflammation and metabolic changes associated with alteration of gut microbiota. Sci. Rep. 2014, 4, 4828. [Google Scholar] [CrossRef] [PubMed]
- Dominy, S.S.; Lynch, C.; Ermini, F.; Benedyk, M.; Marczyk, A.; Konradi, A.; Nguyen, M.; Haditsch, U.; Raha, D.; Griffin, C.; et al. Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treat ment with small-molecule inhibitors. Sci. Adv. 2019, 5, eaau3333. [Google Scholar] [CrossRef] [PubMed]
- Miklossy, J. Bacterial amyloid and DNA are important constituents of senile plaques: Further evidence of the spirochetal and biofilm nature of senile plaques. J. Alzheimers Dis. 2016, 53, 1459–1473. [Google Scholar] [CrossRef]
- Meregildo-Rodriguez, E.D.; Robles-Arce, L.G.; Chunga-Chévez, E.V.; Asmat-Rubio, M.G.; Zavaleta-Alaya, P.; Vásquez-Tirado, G.A. Periodontal disease as a non-traditional risk factor for acute coronary syndrome: A systematic review and meta-analysis. Infez. Med. 2022, 30, 501–515. [Google Scholar] [CrossRef]
- Larvin, H.; Kang, J.; Aggarwal, V.R.; Pavitt, S.; Wu, J. Risk of incident cardiovascular disease in people with perio dontal disease: A systematic review and meta-analysis. Clin. Exp. Dent. Res. 2021, 7, 109–122. [Google Scholar] [CrossRef]
- Teles, R.; Wang, C.Y. Mechanisms involved in the association between periodontal diseases and cardiovascular disease. Oral Dis. 2011, 17, 450–461. [Google Scholar] [CrossRef]
- Wang, Z.; Klipfell, E.; Bennett, B.J.; Koeth, R.; Levison, B.S.; DuGar, B.; Feldstein, A.E.; Britt, E.B.; Fu, X.; Chung, Y.-M.; et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular diease. Nature 2011, 472, 57–63. [Google Scholar] [CrossRef]
- Ma, G.; Pan, B.; Chen, Y.; Guo, C.; Zhao, M.; Zheng, L.; Chen, B. Trimethylamine N-oxide in atherogenesis: Impairing endothelial self-repair capacity and enhancing monocyte adhesion. Biosci. Rep. 2017, 37, BSR20160244. [Google Scholar] [CrossRef]
- Makrecka-Kuka, M.; Volska, K.; Antone, U.; Vilskersts, R.; Grinberga, S.; Bandere, D.; Liepinsh, E.; Dambrova, M. Trimethylamine N-oxide impairs pyruvate and fatty acid oxidetion in cardiac mitochondria. Toxicol. Lett. 2017, 267, 32–38. [Google Scholar] [CrossRef]
- Ohira, H.; Tsutsui, W.; Fujioka, Y. Are Short Chain Fatty Acids in Gut Microbiota Defensive Players for Inflammation and Atherosclerosis? J. Atheroscler. Thromb. 2017, 24, 660–672. [Google Scholar] [CrossRef]
- Lan, T.H.; Huang, X.Q.; Tan, H.M. Vascular fibrosis in atherosclerosis. Cardiovasc. Pathol. 2013, 22, 401–407. [Google Scholar] [CrossRef]
- Chacón, M.R.; Lozano-Bartolomé, J.; Portero-Otín, M.; Rodríguez, M.; Xifra, G.; Puig, J.; Blasco, G.; Ricart, W.; Chaves, F.; Fernández-Real, J. The gut mycobiome composition is linked to carotid atherosclerosis. Benef. Microbes 2018, 9, 185–198. [Google Scholar] [CrossRef]
- Chambers, E.S.; Preston, T.; Frost, G.; Morrison, D.J. Role of Gut Microbiota-Generated Short-Chain Fatty Acids in Metabolic and Cardiovascular Health. Curr. Nutr. Rep. 2018, 7, 198–206. [Google Scholar] [CrossRef]
- Hernández, M.A.G.; Canfora, E.E.; Jocken, J.W.E.; Blaak, E.E. The Short-Chain Fatty Acid Acetate in Body Weight Control and Insulin Sensitivity. Nutrients 2019, 11, 1943. [Google Scholar] [CrossRef]
- Guo, X.; Okpara, E.S.; Hu, W.; Yan, C.; Wang, Y.; Liang, Q.; Chiang, J.Y.L.; Han, S. Interactive Relationships between Intestinal Flora and Bile Acids. Int. J. Mol. Sci. 2022, 23, 8343. [Google Scholar] [CrossRef]
- Tanase, D.M.; Gosav, E.M.; Neculae, E.; Costea, C.F.; Ciocoiu, M.; Hurjui, L.L.; Tarniceriu, C.C.; Maranduca, M.A.; Lacatusu, C.M.; Floria, M.; et al. Role of Gut Microbiota on Onset and Progression of Microvascular Complications of Type 2 Diabetes (T2DM). Nutrients 2020, 12, 3719. [Google Scholar] [CrossRef] [PubMed]
- Xiao, E.; Mattos, M.; Vieira, G.H.A.; Chen, S.; Corrêa, J.D.; Wu, Y.; Albiero, M.L.; Bittinger, K.; Graves, D.T. Diabtes enhances IL-17 expression and alters the oral microbiome to increase its pathogenicity. Cell Host Microbe 2017, 22, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Dissick, A.; Redman, R.S.; Jones, M.; Rangan, B.V.; Reimold, A.; Griffiths, G.R.; Mikuls, T.R.; Amdur, R.L.; Richards, J.S.; Kerr, G.S. Association of periodontitis with rheumatoid arthritis: A pilot study. J. Periodontol. 2010, 81, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Scher, J.U.; Ubeda, C.; Equinda, M.; Khanin, R.; Buischi, Y.; Viale, A.; Lipuma, L.; Attur, M.; Pillinger, M.H.; Weissmann, G.; et al. Periodontal disease and the oral microbiota in new-onset rheumatoid arthritis. Arthritis Rheum. 2012, 64, 3083–3094. [Google Scholar] [CrossRef] [PubMed]
- Nik-Azis, N.M.; Mohd, N.; Baharin, B.; Said, M.S.M.; Fadzilah, F.M.; Haflah, N.H.M. Periodontal disease in sero. positive rheumatoid arthritis: Scoping review of the epidemiological evidence. Germs 2021, 11, 266–286. [Google Scholar] [CrossRef]
- De Smit, M.; Westra, J.; Vissink, A.; Doornbos-van der Meer, B.; Brouwer, E.; van Winkelhoff, A.J. Periodontitis in established rheumatoid arthritis patients: A cross-sectional clinical, microbiological and serological study. Arthritis Res. Ther. 2012, 14, R222. [Google Scholar] [CrossRef]
- Ortiz, P.; Bissada, N.F.; Palomo, L.; Han, Y.W.; Al-Zahrani, M.S.; Panneerselvam, A.; Askari, A. Periodontal therapy reduces the severity of active rheumatoid arthritis in patients treated with or without tumor necrosis factor inhibitors. J. Periodontol. 2009, 80, 535–540. [Google Scholar] [CrossRef]
- Al-Katma, M.K.; Bissada, N.F.; Bordeaux, J.M.; Sue, J.; Askari, A.D. Control of periodontal infection reduces the severity of active rheumatoid arthritis. J. Clin. Rheumatol. 2007, 13, 134–137. [Google Scholar] [CrossRef] [PubMed]
- Arvikar, S.L.; Collier, D.S.; Fisher, M.C.; Unizony, S.; Cohen, G.L.; McHugh, G.; Kawai, T.; Strle, K.; Steere, A.C. Clinical correlations with Porphyromonas gingivalis antibody responses in patients with early rheumatoid arthritis. Arthritis Res. Ther. 2013, 15, R109. [Google Scholar] [CrossRef] [PubMed]
- Wegner, N.; Wait, R.; Sroka, A.; Eick, S.; Nguyen, K.A.; Lundberg, K.; Kinloch, A.; Culshaw, S.; Potempa, J.; Venables, P.J. Peptidylarginine deiminase from Porphyromonas gingivalis citrullinates human fibrinogen and alpha-enolase: Implications for autoimmunity in rheumatoid arthritis. Arthritis Rheum. 2010, 62, 2662–2672. [Google Scholar] [CrossRef] [PubMed]
- Mikuls, T.R.; Payne, J.B.; Yu, F.; Thiele, G.M.; Reynolds, R.J.; Cannon, G.W.; Markt, J.; McGowan, D.; Kerr, G.S.; Redman, R.S.; et al. Periodontitis and Porphyromonas gingivalis in patients with rheumatoid arthritis. Arthritis Rheumatol. 2014, 66, 1090–1100. [Google Scholar] [CrossRef]
- Quirke, A.M.; Quirke, A.M.; Lugli, E.B.; Wegner, N.; Hamilton, B.C.; Charles, P.; Chowdhury, M.; Ytterberg, A.J.; Zubarev, R.A.; Potempa, J.; et al. Heightened immune response to autocitrullinated Porphyromonas gingivalis peptidylarginine deiminase: A potential mechanism for breaching immunologic tolerance in rheumatoid arthritis. Ann. Rheum. Dis. 2014, 73, 263–269. [Google Scholar] [CrossRef]
- De Aquino, S.G.; Abdollahi-Roodsaz, S.; Koenders, M.; Van De Loo, F.A.J.; Pruijn, G.J.M.; Marijnissen, R.J.; Walgreen, B.; Helsen, M.M.; van den Bersselaar, L.A.; de Molon, R.S.; et al. Periodontal pathogens directly promote autoimmune experimental arthritis by inducing a TLR2- and IL-1-driven Th17 response. J. Immunol. 2014, 192, 4103–4111. [Google Scholar] [CrossRef]
- Kulkarni, A.; Beckler, M.D.; Amini, S.S.; Kesselman, M.M. Oral Microbiome in Pre-Rheumatoid Arthritis: The Role of Aggregatibacter actinomycetemcomitans in Bacterial Composition. Cureus 2022, 14, e32201. [Google Scholar] [CrossRef] [PubMed]
- Looh, S.C.; Soo, Z.M.P.; Wong, J.J.; Yam, H.C.; Chow, S.K.; Hwang, J.S. Aggregatibacter actinomycetemcomitans as the Aetiological Cause of Rheumatoid Arthritis: What Are the Unsolved Puzzles? Toxins 2022, 14, 50. [Google Scholar] [CrossRef] [PubMed]
- Konig, M.F.; Abusleme, L.; Reinholdt, J.; Palmer, R.J.; Teles, R.P.; Sampson, K.; Rosen, A.; Nigrovic, P.A.; Sokolove, J.; Giles, J.T.; et al. Aggregatibacter actinomycetemcomitans-induced hypercitrullination links periodontal infection to autoimmunity in rheumatoid arthritis. Sci. Transl. Med. 2016, 8, 369ra176. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Bañuelos, E.; Mukherjee, A.; Darrah, E.; Andrade, F. Rheumatoid Arthritis-Associated Mechanisms of Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans. J. Clin. Med. 2019, 8, 1309. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Li, Y.; Cao, Y.; Xue, J.; Zhou, X. The oral microbiome diversity and its relation to human diseases. Folia Microbiol. 2015, 60, 69–80. [Google Scholar] [CrossRef]
- Sammallahti, H.; Kokkola, A.; Rezasoltani, S.; Ghanbari, R.; Asadzadeh Aghdaei, H.; Knuutila, S.; Puolakkainen, P.; Sarhadi, V.K. Microbiota Alterations and Their Association with Oncogenomic Changes in Pancreatic Cancer Patients. Int. J. Mol. Sci. 2021, 22, 12978. [Google Scholar] [CrossRef]
- Farrell, J.J.; Zhang, L.; Zhou, H.; Chia, D.; Elashoff, D.; Akin, D.; Paster, B.J.; Joshipura, K.; Wong, D.T. Variations of oral microbiota are associated with pancreatic diseases including pancreatic cancer. Gut 2012, 61, 582–588. [Google Scholar] [CrossRef]
- Feng, Q.; Liang, S.; Jia, H.; Stadlmayr, A.; Tang, L.; Lan, Z.; Zhang, D.; Xia, H.; Xu, X.; Jie, Z.; et al. Gut microbiome development along the colorectal along adenom-carcinoma sequence. Nat. Commun. 2015, 6, 6528. [Google Scholar] [CrossRef]
- Saus, E.; Iraola-Guzmán, S.; Willis, R.; Brunet-Vega, A.; Gabaldón, T. Microbiome and colorectal cancer. Roles in carcinogenesis and clinical potential. Mol. Aspects Med. 2019, 69, 93–106. [Google Scholar] [CrossRef]


| General Diseases | Bacteria | References |
|---|---|---|
| Respiratory tract infection Chronic obstructive pulmonary disease Cystic fibrosis | Porphyromonas gingivalis Aggregatibacter actinomycetemcomitans Fusobacterium nucleatum Chlamydia pneumoniae | [69,70,71,72,73] |
| Alzheimer’s disease | Prevotella intermedia Tannerella forsythia Aggregatibacter actinomycetemcomitans Porphyromonas gingivalis Fusobacterium nucleatum | [79,80,81,82,83,84,85,86,87,88,89,90,91,92,93] |
| Cardiovascular diseases (atherosclerosis/coronary diseases) | Porphyromonas gingivalis Treponema denticola Aggregatibacter actinomycetemcomitans Prevotella intermedia Tannerella forsythia | [97,98,99,100,101,102,103,104,105,106] |
| Diabetes and insulin resistance | Porphyromonas gingivalis Aggregatibacter actinomycetemcomitans Fusobacterium nucleatum | [107,108,109,110] |
| Rheumatoid arthritis | Porphyromonas gingivalis Aggregatibacter actinomycetemcomitans. | [111,112,113,114,115,116,117,118,119,120,121,122,123,124,125] |
| Pancreatic cancer Colorectal carcinoma | Neisseria elongata Granulicatella adiacens Porphyromonas gingivalis Fusobacterium nucleatum | [126,127,128,129,130] |
| General Diseases | Mechanisms | References |
|---|---|---|
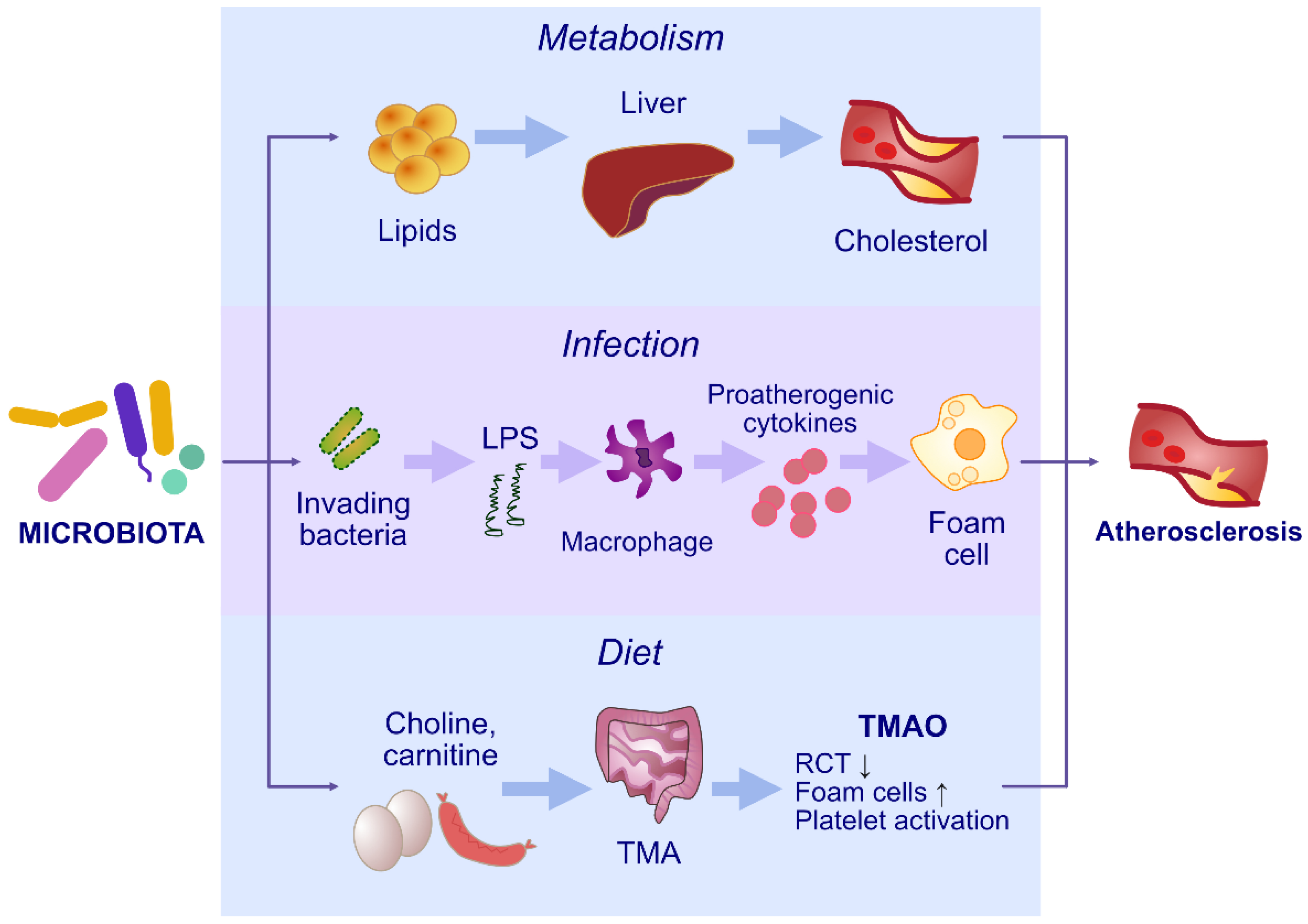
| Atherosclerosis and coronary artery disease | LPS induces the expression of chemokines and cell adhesion molecules Increased production of trimethylamine Increased foam cell generation Promoting monocyte adherence by up-regulating the level of vascular cell adhesion molecule-1 (VCAM-1) Activation of the protein kinase C (PKC) and nuclear factor-κB (NF-κB) pathways Damage to endothelial cells Disturbances in mitochondrial repair and myocardial metabolism Disturbances in bile acid circulation Disturbances in cholesterol and lipid metabolism Enhanced synthesis of pro-inflammatory cytokines Inflammatory response in endothelium Promotion of atherosclerotic plaque formation Plaque instability | [97,98,99,100,101,102,103,104,105,106] |
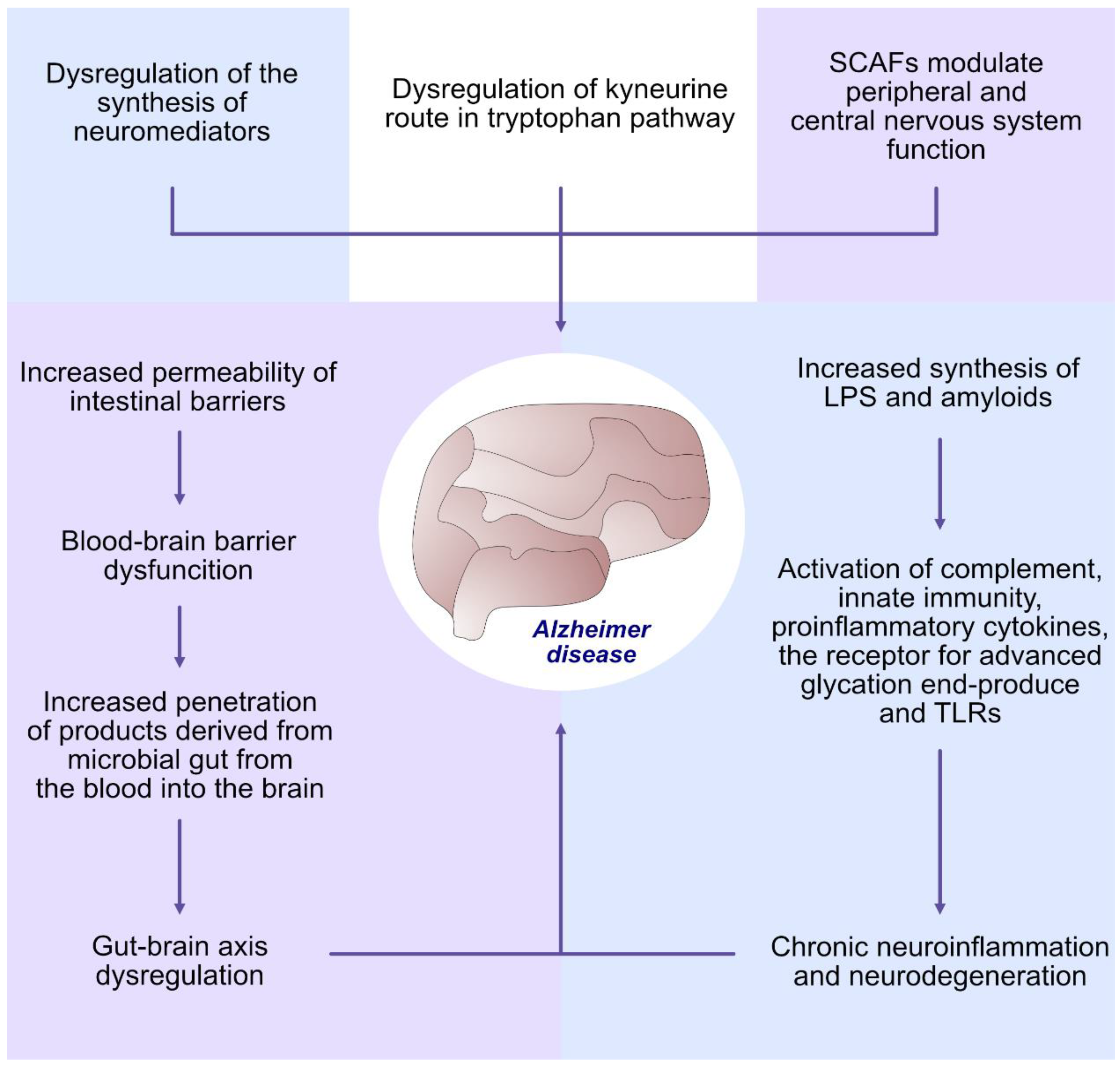
| Alzheimer’s disease | Dysregulation of the synthesis of neuromediators: serotonin, kynurenine, melatonin, GABA, catecholamines, histamine and acetylcholine Dysregulation of kynurenine route in tryptophan pathway Short-chain fatty acids (SCFAs), (acetate, butyrate and propionate) modulate peripheral and central nervous system function Increased permeability of intestinal barriers Blood–brain barrier dysfunction Increased penetration of products derived from microbial gut from the blood into the brain Gut–brain axis dysregulation Increased synthesis of LPS and amyloids Activation of complement, innate immunity, pro-inflammatory cytokines, the receptor for advanced glycation end-products (RAGE) and TLRs. Chronic neuroinflammation and neurodegeneration | [79,80,81,82,83,84,85,86,87,88,89,90,91,92,93] |
| Diabetes and insulin resistance | Short-chain fatty acids act on parasympathetic activity to increase food intake Stimulation of TLR-4 by bacterial LPS induces inflammatory response Disturbances in bile acid circulation Disturbances in cholesterol and lipid metabolism Enhanced synthesis of pro-inflammatory cytokines Chronic systemic inflammation Enhanced oxidative stress Insulin resistance | [107,108,109,110] |
| Rheumatoid arthritis | Induction of anti-CCP antibodies Hypercitrullination in neutrophils Increased production of IL-17 Formation of Th17 cells | [111,112,113,114,115,116,117,118,119,120,121,122,123,124,125] |
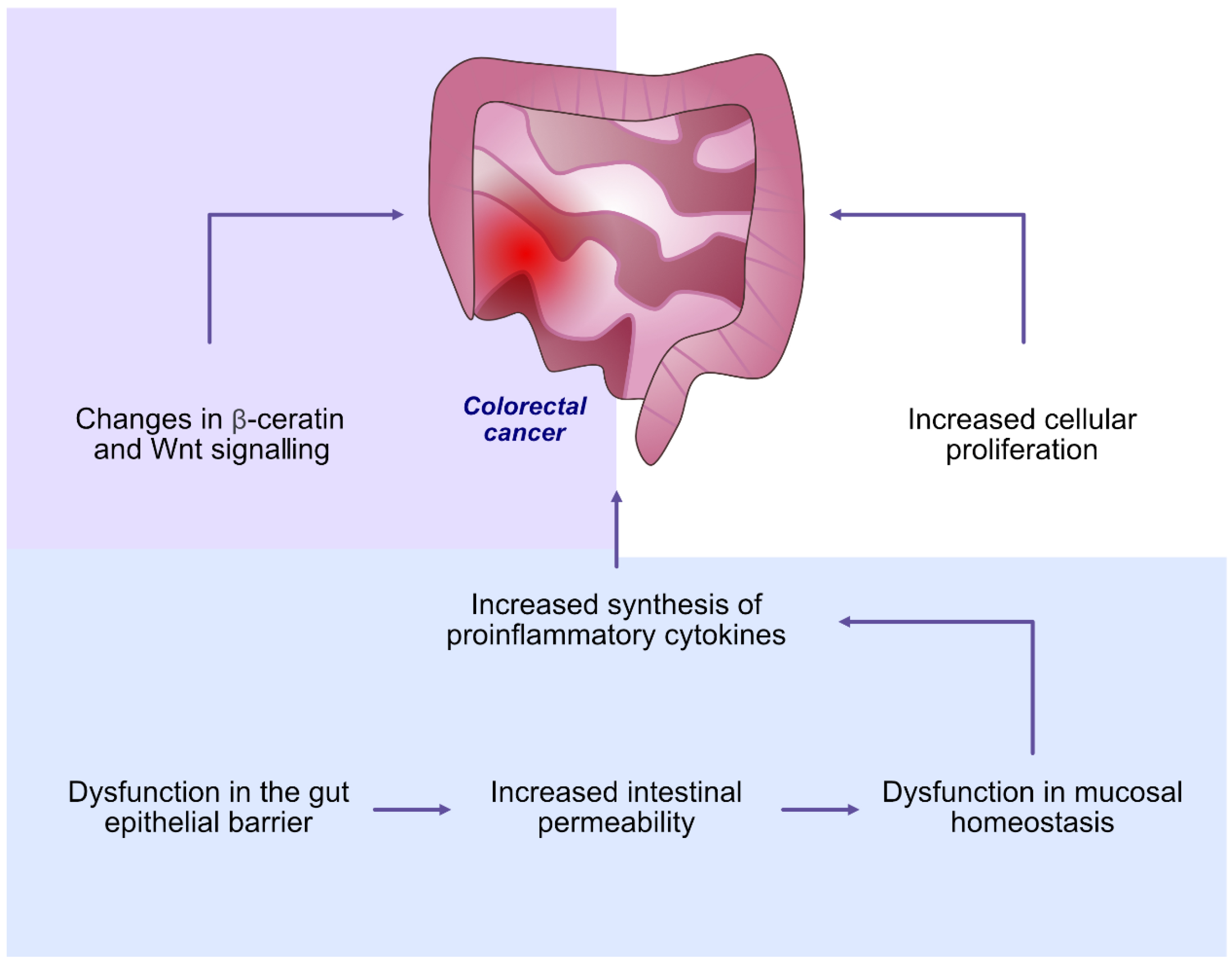
| Colorectal carcinoma | Dysfunction in mucosal homeostasis Dysfunction in the gut epithelial barrier Increased intestinal permeability Increased synthesis of pro-inflammatory cytokines Increased cellular proliferation Changes in β-catenin and Wnt signalling | [126,127,128,129,130] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kozak, M.; Pawlik, A. The Role of the Oral Microbiome in the Development of Diseases. Int. J. Mol. Sci. 2023, 24, 5231. https://doi.org/10.3390/ijms24065231
Kozak M, Pawlik A. The Role of the Oral Microbiome in the Development of Diseases. International Journal of Molecular Sciences. 2023; 24(6):5231. https://doi.org/10.3390/ijms24065231
Chicago/Turabian StyleKozak, Małgorzata, and Andrzej Pawlik. 2023. "The Role of the Oral Microbiome in the Development of Diseases" International Journal of Molecular Sciences 24, no. 6: 5231. https://doi.org/10.3390/ijms24065231
APA StyleKozak, M., & Pawlik, A. (2023). The Role of the Oral Microbiome in the Development of Diseases. International Journal of Molecular Sciences, 24(6), 5231. https://doi.org/10.3390/ijms24065231







