Evaluation of Polymeric Particles for Modular Tissue Cultures in Developmental Engineering
Abstract
1. Introduction
2. Results
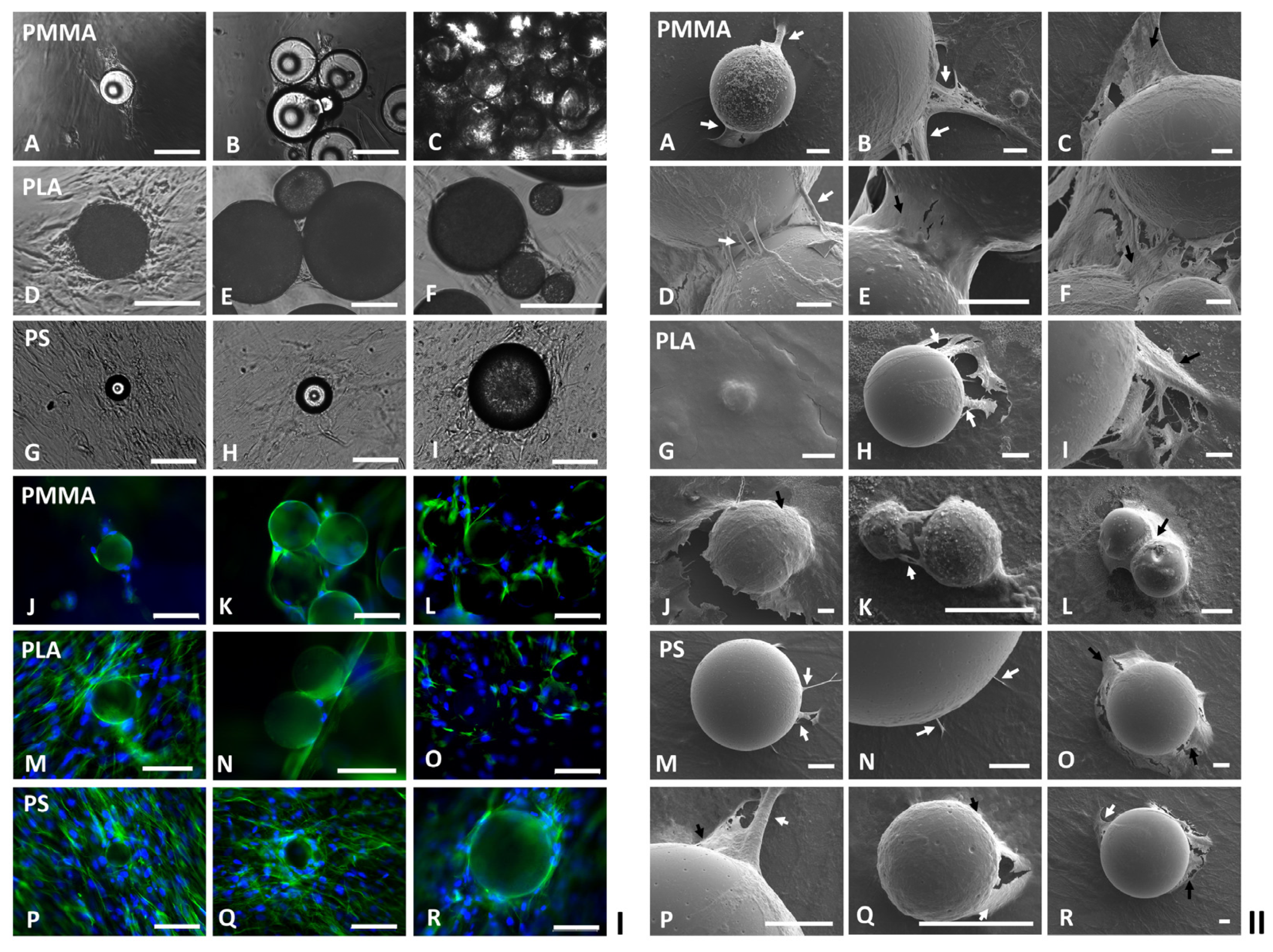
2.1. Influences of Scaffold Material and Particle Size on Modular Tissue Cultures
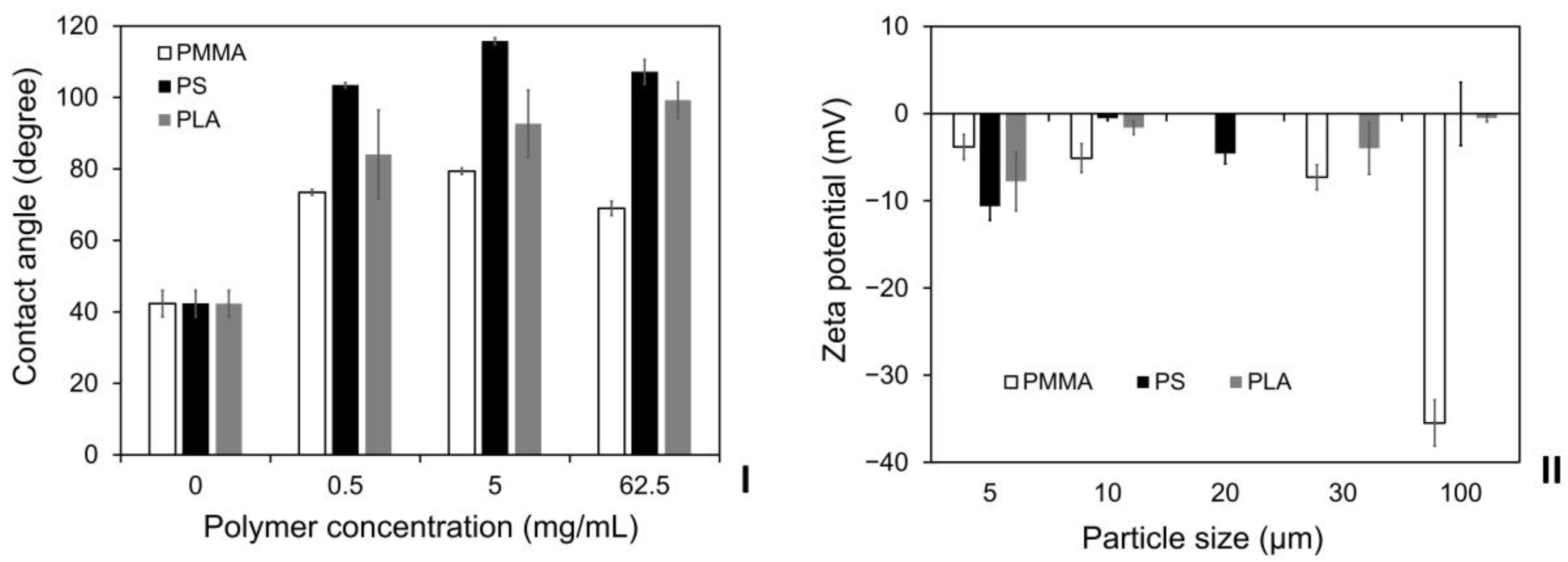
2.2. Influences of Particle Material and Number on Neighboring 2D Cell Cultures
2.3. Influences of Particle Material and Size on Neighboring 2D Cell Cultures
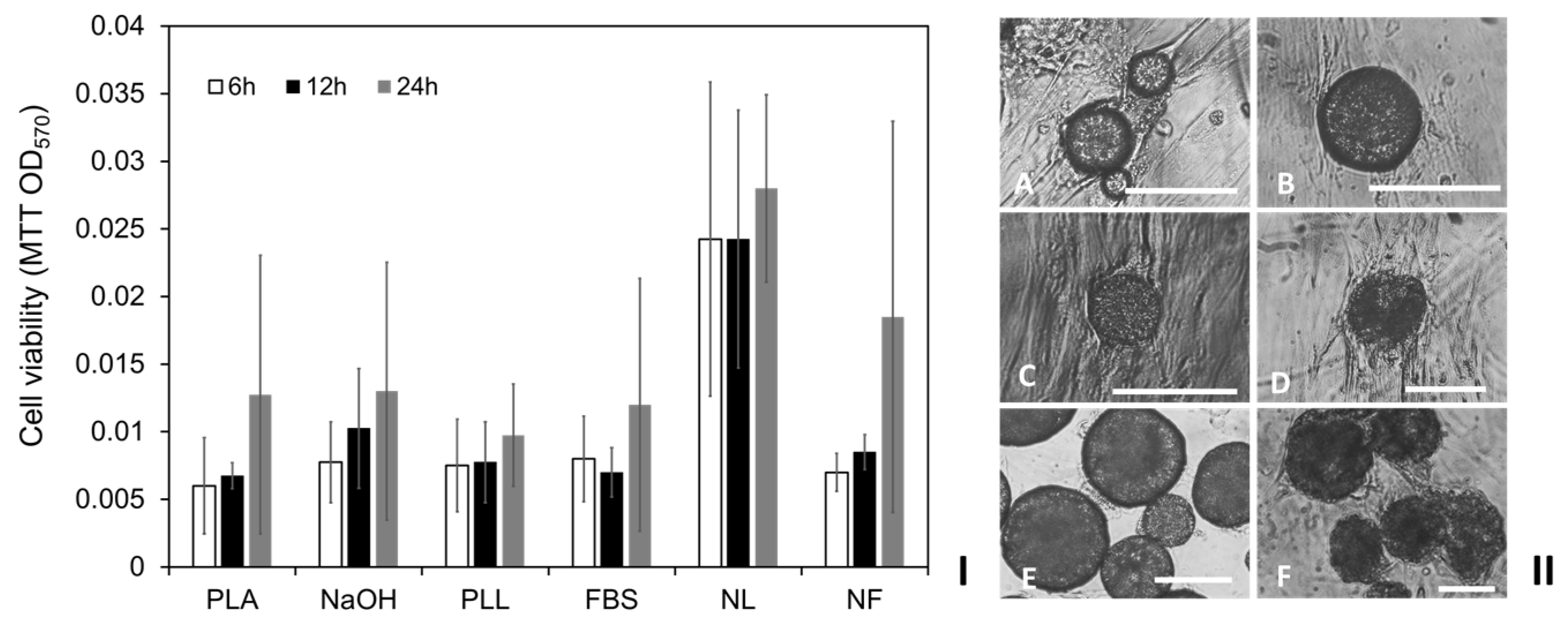
2.4. Influences of PLA Particle Surface Modifications on Modular Tissue Cultures
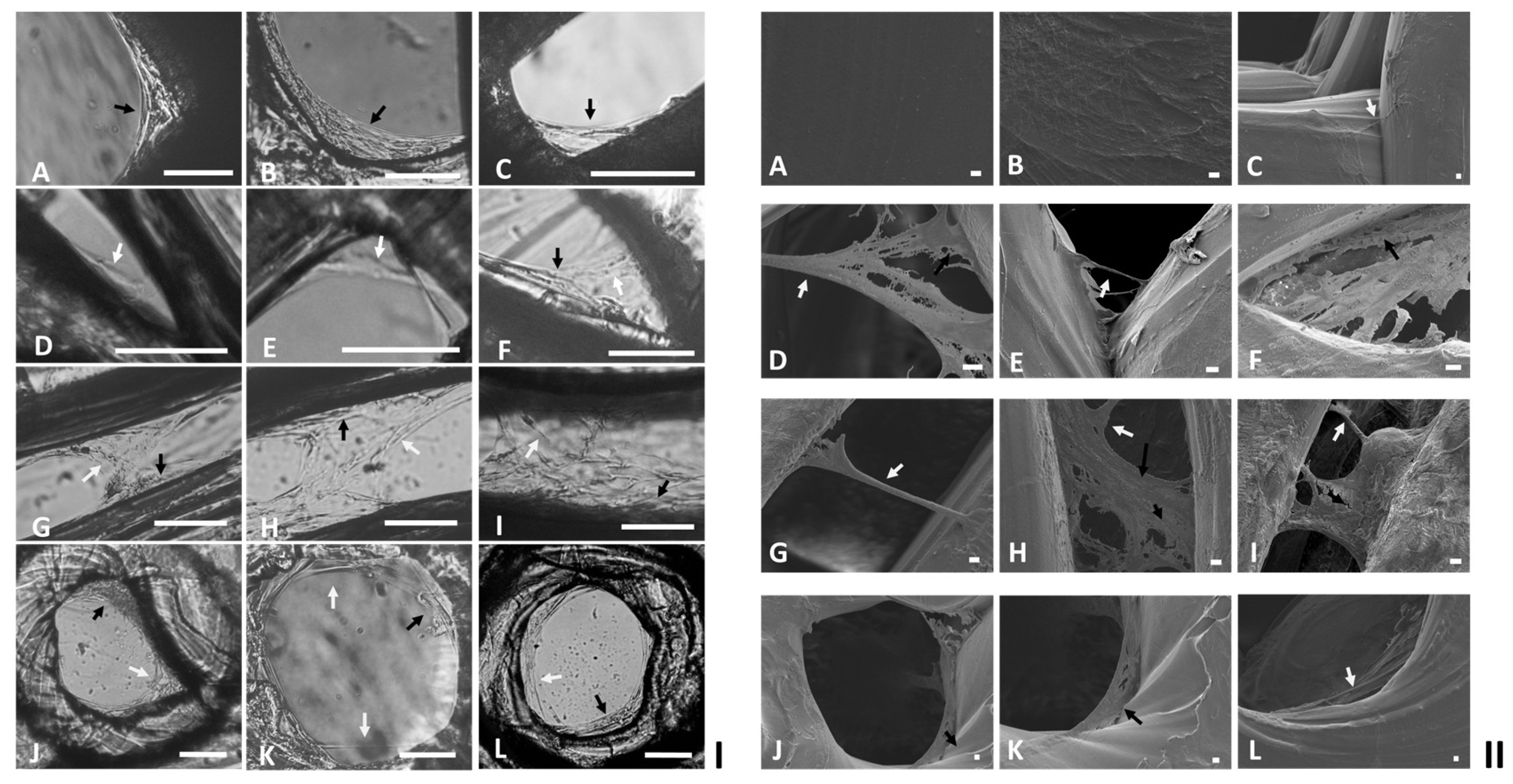
2.5. Cell Colonization within Finely Controlled Open Structures
3. Discussion
4. Materials and Methods
4.1. Fabrication of Polymeric Particles
4.2. 3D Printing of PLA Discs with Defined Open Structures
4.3. 2D Cell Culture
4.4. Small-Scale Modular Tissue Cultures on Spherical Modular Scaffolds
4.5. 3D Tissue Cultures on PLA Discs with Defined Open Structures
4.6. MTT Viability Assay
4.7. Phase Contrast Microscopy
4.8. Fluorescence Microscopy
4.9. Scanning Electron Microscopy
4.10. Collagen Analysis
4.11. Contact Angle Measurement
4.12. Zeta Potential Measurement
4.13. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lenas, P.; Moos, M.; Luyten, F.P. Developmental Engineering: A New Paradigm for the Design and Manufacturing of Cell-Based Products. Part I: From Three-Dimensional Cell Growth to Biomimetics of in Vivo Development. Tissue Eng. Part B Rev. 2009, 15, 381–394. [Google Scholar] [CrossRef] [PubMed]
- Lenas, P.; Moos, M.; Luyten, F.P. Developmental Engineering: A New Paradigm for the Design and Manufacturing of Cell-Based Products. Part II. from Genes to Networks: Tissue Engineering from the Viewpoint of Systems Biology and Network Science. Tissue Eng. Part B Rev. 2009, 15, 395–422. [Google Scholar] [CrossRef] [PubMed]
- Lenas, P.; Ikonomou, L. Developmental Engineering: Design of Clinically Efficacious Bioartificial Tissues through Developmental and Systems Biology. Sci. China Life Sci. 2018, 61, 978–981. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, T.; Xiang, Y.; Bao, X.; Sun, T. A Paradigm Shift in Tissue Engineering: From a Top–down to a Bottom–up Strategy. Processes 2021, 9, 935. [Google Scholar] [CrossRef]
- Liu, J.S.; Gartner, Z.J. Directing the Assembly of Spatially Organized Multicomponent Tissues from the Bottom Up. Trends Cell Biol. 2012, 22, 683–691. [Google Scholar] [CrossRef]
- Quint, C.; Kondo, Y.; Manson, R.J.; Lawson, J.H.; Dardik, A.; Niklason, L.E. Decellularized Tissue-Engineered Blood Vessel as an Arterial Conduit. Proc. Natl. Acad. Sci. USA 2011, 108, 9214–9219. [Google Scholar] [CrossRef]
- Thottappillil, N.; Nair, P.D. Scaffolds in Vascular Regeneration: Current Status. Vasc. Health Risk Manag. 2015, 11, 79–91. [Google Scholar] [CrossRef]
- Gui, L.; Dash, B.C.; Luo, J.; Qin, L.; Zhao, L.; Yamamoto, K.; Hashimoto, T.; Wu, H.; Dardik, A.; Tellides, G.; et al. Implantable Tissue-Engineered Blood Vessels from Human Induced Pluripotent Stem Cells. Biomaterials 2016, 102, 120–129. [Google Scholar] [CrossRef]
- Elomaa, L.; Yang, Y.P. Additive Manufacturing of Vascular Grafts and Vascularized Tissue Constructs. Tissue Eng. Part B Rev. 2017, 23, 436–450. [Google Scholar] [CrossRef]
- Zhao, X.; Lang, Q.; Yildirimer, L.; Lin, Z.Y.; Cui, W.; Annabi, N.; Ng, K.W.; Dokmeci, M.R.; Ghaemmaghami, A.M.; Khademhosseini, A. Photocrosslinkable Gelatin Hydrogel for Epidermal Tissue Engineering. Adv. Healthc. Mater. 2016, 5, 108–118. [Google Scholar] [CrossRef]
- Pedram, P.; Mazio, C.; Imparato, G.; Netti, P.A.; Salerno, A. Bioinspired Design of Novel Microscaffolds for Fibroblast Guidance toward in Vitro Tissue Building. ACS Appl. Mater. Interfaces 2021, 13, 9589–9603. [Google Scholar] [CrossRef]
- Ghasemi-Mobarakeh, L.; Prabhakaran, M.P.; Morshed, M.; Nasr-Esfahani, M.H.; Ramakrishna, S. Electrical Stimulation of Nerve Cells Using Conductive Nanofibrous Scaffolds for Nerve Tissue Engineering. Tissue Eng. Part A 2009, 15, 3605–3619. [Google Scholar] [CrossRef]
- Zamani, F.; Amani-Tehran, M.; Latifi, M.; Shokrgozar, M.A. The Influence of Surface Nanoroughness of Electrospun PLGA Nanofibrous Scaffold on Nerve Cell Adhesion and Proliferation. J. Mater. Sci. Mater. Med. 2013, 24, 1551–1560. [Google Scholar] [CrossRef]
- Farkhondehnia, H.; Amani Tehran, M.; Zamani, F. Fabrication of Biocompatible PLGA/PCL/PANI Nanofibrous Scaffolds with Electrical Excitability. Fibers Polym. 2018, 19, 1813–1819. [Google Scholar] [CrossRef]
- Wang, L.; Wang, Z.H.; Shen, C.Y.; You, M.L.; Xiao, J.F.; Chen, G.Q. Differentiation of Human Bone Marrow Mesenchymal Stem Cells Grown in Terpolyesters of 3-Hydroxyalkanoates Scaffolds into Nerve Cells. Biomaterials 2010, 31, 1691–1698. [Google Scholar] [CrossRef]
- Tayton, E.; Purcell, M.; Aarvold, A.; Smith, J.O.; Briscoe, A.; Kanczler, J.M.; Shakesheff, K.M.; Howdle, S.M.; Dunlop, D.G.; Oreffo, R.O.C. A Comparison of Polymer and Polymer-Hydroxyapatite Composite Tissue Engineered Scaffolds for Use in Bone Regeneration. An in Vitro and in Vivo Study. J. Biomed. Mater. Res. A 2014, 102A, 2613–2624. [Google Scholar] [CrossRef]
- Wu, S.; Wang, Y.; Streubel, P.N.; Duan, B. Living Nanofiber Yarn-Based Woven Biotextiles for Tendon Tissue Engineering Using Cell Tri-Culture and Mechanical Stimulation. Acta Biomater. 2017, 62, 102–115. [Google Scholar] [CrossRef]
- Yang, J.; Guertin, P.; Jia, G.; Lv, Z.; Yang, H.; Ju, D. Large-Scale Microcarrier Culture of HEK293T Cells and Vero Cells in Single-Use Bioreactors. AMB Express 2019, 9, 70. [Google Scholar] [CrossRef]
- Koh, B.; Sulaiman, N.; Fauzi, M.B.; Law, J.X.; Ng, M.H.; Idrus, R.B.H.; Yazid, M.D. Three Dimensional Microcarrier System in Mesenchymal Stem Cell Culture: A Systematic Review. Cell Biosci. 2020, 10, 75. [Google Scholar] [CrossRef]
- Yan, X.; Zhang, K.; Yang, Y.; Deng, D.; Lyu, C.; Xu, H.; Liu, W.; Du, Y. Dispersible and Dissolvable Porous Microcarrier Tablets Enable Efficient Large-Scale Human Mesenchymal Stem Cell Expansion. Tissue Eng. Part C Methods 2020, 26, 263–275. [Google Scholar] [CrossRef]
- Luo, X.; Niu, Y.; Fu, X.; Lin, Q.; Liang, H.; Liu, L.; Li, N. Large-Scale Microcarrier Culture of Chinese Perch Brain Cell for Viral Vaccine Production in a Stirred Bioreactor. Vaccines 2021, 9, 1003. [Google Scholar] [CrossRef] [PubMed]
- Botchwey, E.A.; Pollack, S.R.; Levine, E.M.; Laurencin, C.T. Bone Tissue Engineering in a Rotating Bioreactor Using a Microcarrier Matrix System. J. Biomed. Mater. Res. 2001, 55, 242–253. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.W.; Yoon, J.R.; Lee, J.S.; Kim, H.J.; Lim, H.W.; Lim, H.C.; Park, J.H.; Kim, B.S. The Use of Poly(Lactic-Co-Glycolic Acid) Microspheres as Injectable Cell Carriers for Cartilage Regeneration in Rabbit Knees. J. Biomater. Sci. Polym. Ed. 2006, 17, 925–939. [Google Scholar] [CrossRef] [PubMed]
- Jgamadze, D.; Liu, L.; Vogler, S.; Chu, L.-Y.; Pautot, S. Thermoswitching Microgel Carriers Improve Neuronal Cell Growth and Cell Release for Cell Transplantation. Tissue Eng. Part C Methods 2015, 21, 65–76. [Google Scholar] [CrossRef]
- Taek, K.K.; Jun, J.Y.; Doo, S.L.; Park, T.G. Gas Foamed Open Porous Biodegradable Polymeric Microspheres. Biomaterials 2006, 27, 152–159. [Google Scholar] [CrossRef]
- Tsaryk, R.; Gloria, A.; Russo, T.; Anspach, L.; de Santis, R.; Ghanaati, S.; Unger, R.E.; Ambrosio, L.; Kirkpatrick, C.J. Collagen-Low Molecular Weight Hyaluronic Acid Semi-Interpenetrating Network Loaded with Gelatin Microspheres for Cell and Growth Factor Delivery for Nucleus Pulposus Regeneration. Acta Biomater. 2015, 20, 10–21. [Google Scholar] [CrossRef]
- Badenes, S.M.; Fernandes, T.G.; Rodrigues, C.A.V.; Diogo, M.M.; Cabral, J.M.S. Microcarrier-Based Platforms for In Vitro Expansion and Differentiation of Human Pluripotent Stem Cells in Bioreactor Culture Systems. J. Biotechnol. 2016, 234, 71–82. [Google Scholar] [CrossRef]
- Tsai, A.C.; Ma, T. Expansion of Human Mesenchymal Stem Cells in a Microcarrier Bioreactor. In Bioreactors in Stem Cell Biology; Kursad, T., Ed.; Humana Press: New York, NY, USA, 2016; Volume 1502, pp. 77–86. [Google Scholar]
- YekrangSafakar, A.; Acun, A.; Choi, J.W.; Song, E.; Zorlutuna, P.; Park, K. Hollow Microcarriers for Large-Scale Expansion of Anchorage-Dependent Cells in a Stirred Bioreactor. Biotechnol. Bioeng. 2018, 115, 1717–1728. [Google Scholar] [CrossRef]
- Xu, H.; Cong, Z.; Zhang, Y.; Liu, W.; Yan, X.; Du, Y. Large-Scale Expansion of Umbilical Cord Mesenchymal Stem Cells with Microcarrier Tablets in Bioreactor. In Bioreactors in Stem Cell Biology: Methods and Protocols, 2nd ed.; Kursad, T., Ed.; Humana Press: New York, NY, USA, 2021; Volume 2436, pp. 113–125. [Google Scholar]
- Chen, L.; An, H.Z.; Haghgooie, R.; Shank, A.T.; Martel, J.M.; Toner, M.; Doyle, P.S. Flexible Octopus-Shaped Hydrogel Particles for Specific Cell Capture. Small 2016, 12, 2001–2008. [Google Scholar] [CrossRef]
- Wu, C.Y.; Stoecklein, D.; Kommajosula, A.; Lin, J.; Owsley, K.; Ganapathysubramanian, B.; di Carlo, D.; Leber, J.; Barekzai, J.; Blumenstock, M.; et al. Shaped 3D Microcarriers for Adherent Cell Culture and Analysis. Microsyst. Nanoeng. 2018, 12, 2001–2008. [Google Scholar] [CrossRef]
- Ma, S.; Natoli, M.; Liu, X.; Neubauer, M.P.; Watt, F.M.; Fery, A.; Huck, W.T.S. Monodisperse Collagen-Gelatin Beads as Potential Platforms for 3D Cell Culturing. J. Mater. Chem. B 2013, 1, 5128–5136. [Google Scholar] [CrossRef]
- Xin, S.; Wyman, O.M.; Alge, D.L. Assembly of PEG Microgels into Porous Cell-Instructive 3D Scaffolds via Thiol-Ene Click Chemistry. Adv. Healthc. Mater. 2018, 7, 1800160. [Google Scholar] [CrossRef]
- Tavassoli, H.; Alhosseini, S.N.; Tay, A.; Chan, P.P.Y.; Weng Oh, S.K.; Warkiani, M.E. Large-Scale Production of Stem Cells Utilizing Microcarriers: A Biomaterials Engineering Perspective from Academic Research to Commercialized Products. Biomaterials 2018, 181, 333–346. [Google Scholar] [CrossRef]
- Dosta, P.; Ferber, S.; Zhang, Y.; Wang, K.; Ros, A.; Uth, N.; Levinson, Y.; Abraham, E.; Artzi, N. Scale-up Manufacturing of Gelatin-Based Microcarriers for Cell Therapy. J. Biomed. Mater. Res. B Appl. Biomater. 2020, 108, 2937–2949. [Google Scholar] [CrossRef]
- Zhang, Y.; Na, T.; Zhang, K.; Yang, Y.; Xu, H.; Wei, L.; Xu, L.; Yan, X.; Liu, W.; Liu, G.; et al. GMP-Grade Microcarrier and Automated Closed Industrial Scale Cell Production Platform for Culture of MSCs. J. Tissue Eng. Regen. Med. 2022, 16, 934–944. [Google Scholar] [CrossRef]
- Li, B.; Wang, X.; Wang, Y.; Gou, W.; Yuan, X.; Peng, J.; Guo, Q.; Lu, S. Past, Present, and Future of Microcarrier-Based Tissue Engineering. J. Orthop. Translat. 2015, 3, 51–57. [Google Scholar] [CrossRef]
- Chen, X.Y.; Chen, J.Y.; Tong, X.M.; Mei, J.G.; Chen, Y.F.; Mou, X.Z. Recent Advances in the Use of Microcarriers for Cell Cultures and Their Ex Vivo and in Vivo Applications. Biotechnol. Lett. 2020, 42, 1–10. [Google Scholar] [CrossRef]
- Ornelas-González, A.; González-González, M.; Rito-Palomares, M. Microcarrier-Based Stem Cell Bioprocessing: GMP-Grade Culture Challenges and Future Trends for Regenerative Medicine. Crit. Rev. Biotechnol. 2021, 41, 1081–1095. [Google Scholar] [CrossRef]
- Sivandzade, F.; Mashayekhan, S. Design and Fabrication of Injectable Microcarriers Composed of Acellular Cartilage Matrix and Chitosan. J. Biomater. Sci. Polym. Ed. 2018, 29, 683–700. [Google Scholar] [CrossRef]
- Kurogi, H.; Takahashi, A.; Isogai, M.; Sakumoto, M.; Takijiri, T.; Hori, A.; Furuno, T.; Koike, T.; Yamada, T.; Nagamura-Inoue, T.; et al. Umbilical Cord Derived Mesenchymal Stromal Cells in Microcarrier Based Industrial Scale Culture Sustain the Immune Regulatory Functions. Biotechnol. J. 2021, 16, 2000558. [Google Scholar] [CrossRef]
- Chang, H.-I.; Wang, Y. Cell Responses to Surface and Architecture of Tissue Engineering Scaffolds. In Regenerative Medicine and Tissue Engineering—Cells and Biomaterials; Eberli, D., Ed.; IntechOpen: Rijeka, Croatia, 2011; pp. 569–588. [Google Scholar]
- Fan, H.; Guo, Z. Bioinspired Surfaces with Wettability: Biomolecule Adhesion Behaviors. Biomater. Sci. 2020, 8, 1502–1535. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Jin, L.; Shi, H.; Tong, W.; Gorin, D.; Kotelevtsev, Y.; Mao, Z. Recent Advances of Designing Dynamic Surfaces to Regulate Cell Adhesion. Colloids Interface Sci. Commun. 2020, 35, 100249. [Google Scholar] [CrossRef]
- Ferrari, M.; Cirisano, F.; Carmen Morán, M. Mammalian Cell Behavior on Hydrophobic Substrates: Influence of Surface Properties. Colloids Interfaces 2019, 3, 48. [Google Scholar] [CrossRef]
- Chen, S.; Guo, Y.; Liu, R.; Wu, S.; Fang, J.; Huang, B.; Li, Z.; Chen, Z.; Chen, Z. Tuning Surface Properties of Bone Biomaterials to Manipulate Osteoblastic Cell Adhesion and the Signaling Pathways for the Enhancement of Early Osseointegration. Colloids Surf. B Biointerfaces 2018, 164, 58–69. [Google Scholar] [CrossRef] [PubMed]
- Courtenay, J.C.; Johns, M.A.; Galembeck, F.; Deneke, C.; Lanzoni, E.M.; Costa, C.A.; Scott, J.L.; Sharma, R.I. Surface Modified Cellulose Scaffolds for Tissue Engineering. Cellulose 2017, 24, 253–267. [Google Scholar] [CrossRef]
- Spriano, S.; Sarath Chandra, V.; Cochis, A.; Uberti, F.; Rimondini, L.; Bertone, E.; Vitale, A.; Scolaro, C.; Ferrari, M.; Cirisano, F.; et al. How Do Wettability, Zeta Potential and Hydroxylation Degree Affect the Biological Response of Biomaterials? Mater. Sci. Eng. C 2017, 74, 542–555. [Google Scholar] [CrossRef]
- Sousa, I.; Mendes, A.; Pereira, R.F.; Bártolo, P.J. Collagen Surface Modified Poly(ε-Caprolactone) Scaffolds with Improved Hydrophilicity and Cell Adhesion Properties. Mater. Lett. 2014, 134, 263–267. [Google Scholar] [CrossRef]
- Chuah, Y.J.; Koh, Y.T.; Lim, K.; Menon, N.V.; Wu, Y.; Kang, Y. Simple Surface Engineering of Polydimethylsiloxane with Polydopamine for Stabilized Mesenchymal Stem Cell Adhesion and Multipotency. Sci. Rep. 2015, 5, 18162. [Google Scholar] [CrossRef]
- Bean, A.C.; Tuan, R.S. Fiber Diameter and Seeding Density Influence Chondrogenic Differentiation of Mesenchymal Stem Cells Seeded on Electrospun Poly(ε-Caprolactone) Scaffolds. Biomed. Mater. 2015, 10, 18162. [Google Scholar] [CrossRef]
- Guex, A.G.; Puetzer, J.L.; Armgarth, A.; Littmann, E.; Stavrinidou, E.; Giannelis, E.P.; Malliaras, G.G.; Stevens, M.M. Highly Porous Scaffolds of PEDOT:PSS for Bone Tissue Engineering. Acta Biomater. 2017, 62, 91–101. [Google Scholar] [CrossRef]
- Huang, L.; Abdalla, A.M.E.; Xiao, L.; Yang, G. Biopolymer-Based Microcarriers for Three-Dimensional Cell Culture and Engineered Tissue Formation. Int. J. Mol. Sci. 2020, 21, 1895. [Google Scholar] [CrossRef]
- Sun, T.; Norton, D.; McKean, R.J.; Haycock, J.W.; Ryan, A.J.; MacNeil, S. Development of a 3D Cell Culture System for Investigating Cell Interactions with Electrospun Fibers. Biotechnol. Bioeng. 2007, 97, 1318–1328. [Google Scholar] [CrossRef]
- Gabbott, C.M.; Zhou, Z.X.; Han, G.X.; Sun, T. A Novel Scale-down Cell Culture and Imaging Design for the Mechanistic Insight of Cell Colonisation within Porous Substrate. J. Microsc. 2017, 267, 150–159. [Google Scholar] [CrossRef]
- Nie, Y.; Bergendahl, V.; Hei, D.J.; Jones, J.M.; Palecek, S.P. Scalable Culture and Cryopreservation of Human Embryonic Stem Cells on Microcarriers. Biotechnol. Progress 2009, 25, 20–31. [Google Scholar] [CrossRef]
- Moritz, M.S.M.; Verbruggen, S.E.L.; Post, M.J. Alternatives for Large-Scale Production of Cultured Beef: A Review. J. Integr. Agric. 2015, 14, 208–216. [Google Scholar] [CrossRef]
- Wang, Z.; Wu, D.; Zou, J.; Zhou, Q.; Liu, W.; Zhang, W.; Zhou, G.; Wang, X.; Pei, G.; Cao, Y.; et al. Development of Demineralized Bone Matrix-Based Implantable and Biomimetic Microcarrier for Stem Cell Expansion and Single-Step Tissue-Engineered Bone Graft Construction. J. Mater. Chem. B 2017, 5, 62–73. [Google Scholar] [CrossRef]
- Hewitt, C.J.; Lee, K.; Nienow, A.W.; Thomas, R.J.; Smith, M.; Thomas, C.R. Expansion of Human Mesenchymal Stem Cells on Microcarriers. Biotechnol. Lett. 2011, 33, 2325–2335. [Google Scholar] [CrossRef]
- Tamura, A.; Nishi, M.; Kobayashi, J.; Nagase, K.; Yajima, H.; Yamato, M.; Okano, T. Simultaneous Enhancement of Cell Proliferation and Thermally Induced Harvest Efficiency Based on Temperature-Responsive Cationic Copolymer-Grafted Microcarriers. Biomacromolecules 2012, 13, 1765–1773. [Google Scholar] [CrossRef]
- Tamura, A.; Kobayashi, J.; Yamato, M.; Okano, T. Thermally Responsive Microcarriers with Optimal Poly(N-Isopropylacrylamide) Grafted Density for Facilitating Cell Adhesion/Detachment in Suspension Culture. Acta Biomater. 2012, 8, 3904–3913. [Google Scholar] [CrossRef]
- Hanga, M.P.; Holdich, R.G. Membrane Emulsification for the Production of Uniform Poly-N-Isopropylacrylamide-Coated Alginate Particles Using Internal Gelation. Chem. Eng. Res. Des. 2014, 92, 1664–1673. [Google Scholar] [CrossRef]
- Ferrari, C.; Balandras, F.; Guedon, E.; Olmos, E.; Chevalot, I.; Marc, A. Limiting Cell Aggregation during Mesenchymal Stem Cell Expansion on Microcarriers. Biotechnol. Prog. 2012, 28, 780–787. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Rostami, M.R.; Cadavid Olaya, D.P.; Tzanakakis, E.S. Oxygen Transport and Stem Cell Aggregation in Stirred-Suspension Bioreactor Cultures. PLoS ONE 2014, 9, e102486. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, I.; Sato, K.; Mera, H.; Wakitani, S.; Takagi, M. Effects of Agitation Rate on Aggregation during Beads-to-Beads Subcultivation of Microcarrier Culture of Human Mesenchymal Stem Cells. Cytotechnology 2017, 69, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Hanga, M.P.; de la Raga, F.A.; Moutsatsou, P.; Hewitt, C.J.; Nienow, A.W.; Wall, I. Scale-up of an Intensified Bioprocess for the Expansion of Bovine Adipose-Derived Stem Cells (BASCs) in Stirred Tank Bioreactors. Biotechnol. Bioeng. 2021, 118, 3175–3186. [Google Scholar] [CrossRef] [PubMed]
- Leber, J.; Barekzai, J.; Blumenstock, M.; Pospisil, B.; Salzig, D.; Czermak, P. Microcarrier Choice and Bead-to-Bead Transfer for Human Mesenchymal Stem Cells in Serum-Containing and Chemically Defined Media. Process Biochem. 2017, 59, 255–265. [Google Scholar] [CrossRef]
- Lembong, J.; Kirian, R.; Takacs, J.D.; Olsen, T.R.; Lock, L.T.; Rowley, J.A.; Ahsan, T. Bioreactor Parameters for Microcarrier-Based Human Msc Expansion under Xeno-Free Conditions in a Vertical-Wheel System. Bioengineering 2020, 7, 73. [Google Scholar] [CrossRef]
- Roach, P.; Farrar, D.; Perry, C.C. Surface Tailoring for Controlled Protein Adsorption: Effect of Topography at the Nanometer Scale and Chemistry. J. Am. Chem. Soc. 2006, 128, 3939–3945. [Google Scholar] [CrossRef]
- Gleadall, A. FullControl GCode Designer—Open-Source Software for Unconstrained Design in Additive Manufacturing. Addit. Manuf. 2021, 46, 102–109. [Google Scholar] [CrossRef]
- Yang, J.; Wan, Y.; Tu, C.; Cai, Q.; Bei, J.; Wang, S. Enhancing the Cell Affinity of Macroporous Poly(L-Lactide) Cell Scaffold by a Convenient Surface Modification Method. Polym. Int. 2003, 52, 1892–1899. [Google Scholar] [CrossRef]
- Yang, J.; Shi, G.; Bei, J.; Wang, S.; Cao, Y.; Shang, Q.; Yang, G.; Wang, W. Fabrication and Surface Modification of Macroporous Poly(L-Lactic Acid) and Poly(L-Lactic-Co-Glycolic Acid) (70/30) Cell Scaffolds for Human Skin Fibroblast Cell Culture. J. Biomed. Mater. Res. 2002, 62, 438–446. [Google Scholar] [CrossRef]
- Lu, S.; Zhu, K.; Song, W.; Song, G.; Chen, D.; Hayat, T.; Alharbi, N.S.; Chen, C.; Sun, Y. Impact of Water Chemistry on Surface Charge and Aggregation of Polystyrene Microspheres Suspensions. Sci. Total Environ. 2018, 630, 951–959. [Google Scholar] [CrossRef]
- Hwang, J.; Choi, D.; Han, S.; Jung, S.Y.; Choi, J.; Hong, J. Potential Toxicity of Polystyrene Microplastic Particles. Sci. Rep. 2020, 10, 7391. [Google Scholar] [CrossRef]


| Particle Diameter (µm) | 100 | 30 | 10 | 5 |
|---|---|---|---|---|
| Solvent | DCM 1 | Chloroform | Chloroform | Chloroform |
| Organic solution (mg/mL) | 62.5 | 5 | 5 | 5 |
| PVA 2 (%(w/v)) | 5 | 0.1 | 1 | 5 |
| O/A 3 ratio | 8:150 | 1:10 | 1:10 | 1:10 |
| Stirring speed (RPM) | 200 | 1500 | 1500 | 1500 |
| Temperature (°C) | RT 4 | 65 | 65 | 65 |
| Evaporation time (h) | 2.5 | 1.5 | 1.5 | 1.5 |
| Printing Parameters | Set Values |
|---|---|
| Nozzle temperature (°C) | 210 |
| Print bed temperature (°C) | 60 |
| Printing speed (mm/min) | 1000 |
| Set extrusion width (mm) | 0.4 |
| Layer height (mm) | 0.167 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xiang, Y.; Yan, J.; Bao, X.; Gleadall, A.; Roach, P.; Sun, T. Evaluation of Polymeric Particles for Modular Tissue Cultures in Developmental Engineering. Int. J. Mol. Sci. 2023, 24, 5234. https://doi.org/10.3390/ijms24065234
Xiang Y, Yan J, Bao X, Gleadall A, Roach P, Sun T. Evaluation of Polymeric Particles for Modular Tissue Cultures in Developmental Engineering. International Journal of Molecular Sciences. 2023; 24(6):5234. https://doi.org/10.3390/ijms24065234
Chicago/Turabian StyleXiang, Yu, Jiongyi Yan, Xujin Bao, Andrew Gleadall, Paul Roach, and Tao Sun. 2023. "Evaluation of Polymeric Particles for Modular Tissue Cultures in Developmental Engineering" International Journal of Molecular Sciences 24, no. 6: 5234. https://doi.org/10.3390/ijms24065234
APA StyleXiang, Y., Yan, J., Bao, X., Gleadall, A., Roach, P., & Sun, T. (2023). Evaluation of Polymeric Particles for Modular Tissue Cultures in Developmental Engineering. International Journal of Molecular Sciences, 24(6), 5234. https://doi.org/10.3390/ijms24065234









