Abstract
Glutathione (GSH) is necessary for maintaining physiological antioxidant function, which is responsible for maintaining free radicals derived from reactive oxygen species at low levels and is associated with improved cognitive performance after brain injury. GSH is produced by the linkage of tripeptides that consist of glutamic acid, cysteine, and glycine. The adequate supplementation of GSH has neuroprotective effects in several brain injuries such as cerebral ischemia, hypoglycemia, and traumatic brain injury. Brain injuries produce an excess of reactive oxygen species through complex biochemical cascades, which exacerbates primary neuronal damage. GSH concentrations are known to be closely correlated with the activities of certain genes such as excitatory amino acid carrier 1 (EAAC1), glutamate transporter-associated protein 3–18 (Gtrap3-18), and zinc transporter 3 (ZnT3). Following brain-injury-induced oxidative stress, EAAC1 function is negatively impacted, which then reduces cysteine absorption and impairs neuronal GSH synthesis. In these circumstances, vesicular zinc is also released into the synaptic cleft and then translocated into postsynaptic neurons. The excessive influx of zinc inhibits glutathione reductase, which inhibits GSH’s antioxidant functions in neurons, resulting in neuronal damage and ultimately in the impairment of cognitive function. Therefore, in this review, we explore the overall relationship between zinc and GSH in terms of oxidative stress and neuronal cell death. Furthermore, we seek to understand how the modulation of zinc can rescue brain-insult-induced neuronal death after ischemia, hypoglycemia, and traumatic brain injury.
1. Introduction
Glutathione (GSH) is well known as an antioxidant that protects cells from brain-injury-induced reactive oxygen species (ROS) production [1]. GSH is synthesized as a tripeptide consisting of L-cysteine, L-glutamate, and glycine [2]. The concentration of GSH is regulated by glutathione disulfide (GSSG) during the redox cycle [3,4]. GSH peroxidase converts GSH to GSSG with H2O2, and GSH reductase converts GSSG to GSH with NADPH+H+ [5]. In various brain injury conditions, the presynaptic release of zinc activates a reaction with free radicals to oxidize the reduced form of GSH to its dimer form (GSSG). Additionally, zinc interferes with the formation of GSH by inhibiting glutathione reductase (GR), an enzyme that converts the dimer GSSG to the GSH form [6]. Consequently, a reduction in GSH concentration contributes to an elevation in intracellular ROS and free zinc levels, leading to the disruption of homeostasis and apoptotic cell death [6].
Zinc has important physiological functions in processes such as protein synthesis, signal transduction, and cell proliferation [7,8]. Under normal conditions, released zinc ionotropically and metabotropically modulates postsynaptic receptors [9,10]. However, under pathological conditions such as stroke, epilepsy, or traumatic brain injury, the excessive influx of zinc into neurons causes neurotoxicity, damage to neurons, and a reduction in GSH [11]. Zinc inhibits glutathione reductase and causes intracellular mitochondrial dysfunction, thereby interfering with GSH synthesis [11,12,13]. Zinc transporter 3 (ZnT3) regulates the homeostasis of zinc and GSH in neurons [12,13]. ZnT3 knockout reduced the translocation of zinc into synaptic vesicles and lowered vesicular zinc concentrations, which enhanced GSH levels through the activation of the GSH synthesis pathway [14,15].
GSH is also associated with excitatory amino acid transporters (EAAT1, 2, 3, 4, and 5) [16,17]. EAATs serve a role as the transmembrane complexes that transport glutamate, a major excitatory neurotransmitter, and function as sodium-dependent high-affinity glutamate transporters [16,17]. EAAT1, 2, and 3 are related to the regulation of glutamatergic transmission. EAAT1 is localized in the cerebellum, particularly in astrocytes. EAAT2 is expressed in the forebrain and presynaptic terminals [18,19]. EAAT3 is located in the hippocampus, striatum, and cerebellum [16,17,19]. EAAT4 is primarily present in the cerebellum and is mostly expressed in astrocyte-lineage Bergmann glia and neuronal Purkinje cells. It has a high affinity for the excitatory amino acids L-aspartate and L-glutamate, and previous results suggest that the loss of EAAT4 may contribute to the pathogenesis of spinal cerebellar ataxia type 5 (SCA5) [17,20]. EAAT5 is mainly present in retinal neurons, where it functions to influence light-activated chloride currents mediated by the glutamate activation of EAAT5 [17,20,21]. Among these transporters, mouse EAAT1, which corresponds to human EAAC3, is encoded by the SLC1A1 gene. Mouse EAAT1 has a high affinity with cysteine, which is one of components of GSH [17,19]. Thus, EAAC1 gene-deleted mice show a significant decrease in neural GSH levels with an increase in ROS levels, leading to oxidative damage [22,23]. Previous studies found that cysteine supplementation via N-acetyl-cysteine (NAC) promoted GSH synthesis, eventually exerting a neuroprotective effect. In addition, glutamate transporter-associated protein 3–18 (GTRAP3-18) is known to be a negative regulator of EAAC1 expression [24,25]. Thus, reducing GTRAP3-18 activity enhances GSH synthesis by increasing EAAC1 expression, which modulates the amount of cysteine translocation into the intracellular space [24,25].
In the present review, we show that specific genes such as Gtrap3 and EAAC1 are correlated with the formation of GSH. In the case of brain injury conditions, an excessive amount of free zinc is accumulated in the neuron, which produces ROS via the NADPH oxidase activation pathway. Accumulated zinc also reduces GSH synthesis by the inhibition of glutathione reductase, which aggravates neuron death after stroke, traumatic brain injury, hypoglycemia, and epilepsy. Thus, this review discusses the role of GSH on zinc-induced neuronal death.
2. Glutathione Synthesis
Glutathione (GSH) is an antioxidant that protects the brain from the overproduction of reactive oxygen species (ROS), ROS-induced free radical formation, and oxidative stress [26]. GSH consists of L-glutamate, L-cysteine, and glycine, which are linked by adenosine-triphosphate-dependent steps. The GSH formation process is defined as follows [27,28].
L-glutamate and L-cysteine form gamma-glutamylcysteine via the glutamate–cysteine-binding enzyme [29]. Glutamate–cysteine ligase (GCL) catalyzes the synthesis process, which involves ATP-dependent synthesis from L-cysteine and L-glutamate to γ-glutamylcysteine [30]. Glycine binds to γ-glutamyl cysteine to form glutathione synthase for GSH synthesis [31]. GSH has a thiol group (-SH) and its hydrogen provides electrons to remove ROS-induced free radicals. Glutathione exists in its reduced form of GSH (glutathione-SH) and as an oxidized form, GSSG (glutathione-SS-glutathione) [32]. Reduced GSH is oxidized by hydroperoxides and thereby converted to GSSG. Electrons of NADPH are transferred to GSSG by glutathione reductase, which is then transformed to GSH [31,33]. In other words, NADP+ is converted to NADPH by glucose-6-phosphate dehydrogenase and the converted NADPH is converted to NADP+ by glutathione reductase, which reduces GSSG to GSH [31,33]. GSH is produced by the NADPH present in the cytoplasm through glycolysis [34]. The pentose phosphate pathway (PPP) is a metabolic pathway that oxidizes glucose 6-phosphate (G6P) to pentose phosphate. In addition, astrocytes promote a high influx of glucose into the PPP pathway, which results in the production of ATP and GSH [34,35]. Thus, astrocytes and their normal metabolism play an important role in reducing oxidative stress in the brain and can provide GSH and ATP to neurons by the astrocyte–neuron glutathione shuttle [36,37] (Figure 1).
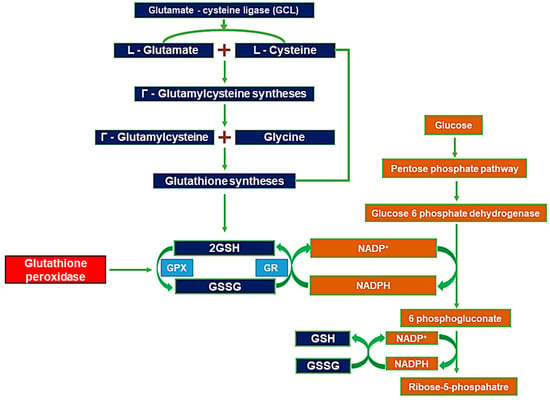
Figure 1.
L-glutamate and L-cysteine are bound by glutamate–cysteine ligase enzyme. γ-glutamyl cysteine and glycine combine to form glutathione synthase [31,38,39,40]. GSH and GSSG conversion is mediated by hydroxy peroxide and GSH reductase [41,42,43]. Pentose phosphate pathway (PPP)-derived NADPH supplies electrons to GSSG via GSH reductase [44,45].
Glucose-6-phosphate dehydrogenase is involved in the PPP process and converts nicotinamide adenine dinucleotide phosphate (NADP+) to NADPH [46]. Transformed by glucose-6-phosphate dehydrogenase, NADPH delivers high-energy electrons (i.e., reducing equivalents) to cells, maintains cellular redox balance, and supplies reductive biosynthesis [46]. In its reduced form (GSH), it plays a role in removing ROS that cause cellular damage. The sulfhydryl (-SH) moiety, a residue of GSH, neutralizes ROS, and is oxidized to its inactive dimer form (GSSG) when the GSH monomer reacts with ROS [47]. After that, GSH is reduced again by the coenzyme NADPH, formed through a G6PD-6PD-dependent pathway [46,47].
Glutathione peroxidase 4 (GPX4) is an enzyme that converts active GSH to GSSG by replacing lipid hydroperoxide (LOOH) with a lipid hydroperoxyl radical (LOO), which is a glucose-6-phosphate dehydrogenase (G6PD) of pentose phosphate. Importantly, glutathione peroxidase 4 (GPX4) converts GSH to GSSG and at the same time converts ROS-induced lipid peroxidase into lipid alcohols, with it being known to play a role in preventing an apoptotic mechanism called ferroptosis [48,49]. The signaling pathway associated with ferroptosis is mainly split into two main pathways: The exogenous, transporter-dependent pathway, which is derived from the amino acid anti-porter system Xc− inhibition of iron carrier activation, and the intrinsic, enzyme-dependent pathway, which is derived from the reduction of antioxidant enzymes such as GSH or GPX4 [48,49,50]. Finally, the inactivation of GPX4 induced by the GSH depletion caused by multiple neuronal injuries increases intracellular lipid peroxide and induces ferroptosis, which greatly affects neuronal apoptosis [47] (Figure 1).
Therefore, GSH plays a major role in the suppression of reactive oxygen species, which induce neuronal cell death if unchecked [51]. GSH is synthesized through complex biochemical and cellular mechanisms, and GSH deficiency has been proven to be an important factor that can lead to the upregulation of apoptosis and exacerbate neurological diseases [27,32,33].
3. Zinc-Induced Glutathione Deficiency
Zinc is the most abundant metal ion in the brain and is essential for cell growth and proliferation and tissue development [52]. However, the excessive accumulation of zinc in postsynaptic neurons accelerates neuronal injuries [53]. Zinc mediates nicotinamide adenine dinucleotide phosphate oxidase (NOX) activation, which results in intracellular ROS production through an NADPH-oxidase-dependent pathway [54,55]. ROS promotes zinc-induced PARP activation, resulting in ATP depletion and neuronal death [54,55].
Zinc accumulation induces oxidative stress by interfering with endogenous antioxidant systems and causing neuronal damage [56,57]. Zinc impairs thiol residue homeostasis, increases lipid peroxidation, and inhibits glutathione reductase to maintain an oxidation-promoting state [56,58]. Astrocytic GSSG was increased under conditions of zinc overload and led to a decreased ratio of GSH transfer to neurons through the astrocyte–neuron glutathione shuttle [36]. In addition, zinc itself makes several contributions to the induction of the lipid peroxidation of sulfhydryl groups in the phosphorus membrane, mitochondrial dysfunction, thioredoxin reductase, and ROS production [58,59]. Consequently, a low concentration of GSH in neurons contributes to oxidative damage after several brain insults [58,59] (Figure 2).
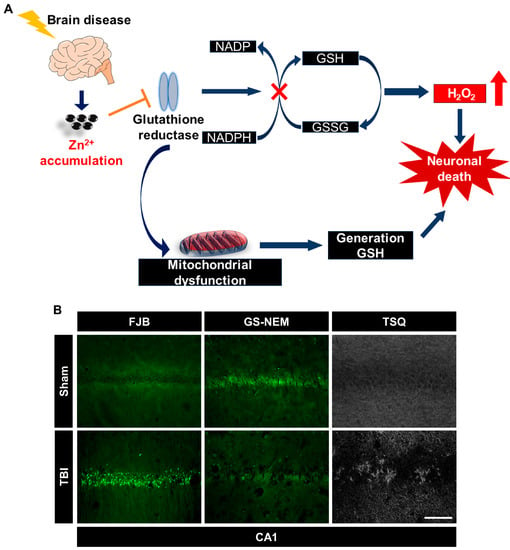
Figure 2.
(A) Zinc inhibits glutathione reductase (GR) [60]. GR-mediated conversion of GSSG to GSH is inhibited by accumulated zinc [60]. Abnormal GR function leads to mitochondrial dysfunction and disturbs GSH synthesis [59]. Depletion of GSH inhibits GR activity following zinc overload and induces neuronal damage [56]. (B) Immunofluorescence images show degenerating neurons in the hippocampal CA1 region 24 h after traumatic brain injury (TBI), detected using Fluoro-Jade B (FJB, green color); immunofluorescence images show degenerating neurons detected using a glutathione antibody, N-ethylmaleimide adduct (GS-NEM, green color), in the hippocampal CA1 region 24 h after TBI; zinc-specific representative fluorescence image displays TSQ (+) neurons by N-(6-methoxy-8-quinolyl)-para-toluene sulfonamide (TSQ) in the hippocampal CA1 region 24 h after TBI. Scale bar = 100 μm.
To enhance neuronal GSH concentrations, several studies have evaluated the chelation of synaptically released zinc using a thiol-containing chemical compound, N-acetyl-cysteine (NAC). The administration of NAC showed a neuroprotective effect after several brain insults [14,15,61]. Brain insults induce the liberation of zinc from zinc-binding proteins such as metallothionein [24,62]. NAC treatment after brain insults revealed that cysteine, an essential component of GSH, supplied the thiol residue of NAC, which has the ability to chelate presynaptically released or detached intraneuronal zinc [24,62]. NAC inhibits transient receptor potential melastatin 2 (TRPM2), one of the nonselective cation channels induced by ROS production, to block the influx of zinc into the cytoplasm of neurons, thereby reducing neuronal cell death and oxidative damage [63]. Moreover, EAAC1 deficiency inhibits the influx of L-cysteine, which reduces the formation of internal GSH [61,62]. Finally, it was found that EAAC1 gene deletion increased basal levels of cytoplasmic free zinc, which later increased neuronal death in hippocampus and cerebral cortex after brain insults [61,62].
Based on the above-mentioned results, there is a clear correlation between the amount of zinc and the processes responsible for the synthesis of GSH. The excessive release of zinc from synaptic vesicles or cytoplasmic proteins decreases the synthesis of GSH, which causes neuronal cell death [15,62,63]. Targeting presynaptically released zinc or GSH components via supplementation may have the potential to provide new therapeutic tools to prevent neuronal death after various brain insults [15,62,63].
4. EAAC1 and Glutathione Formation
Excitatory amino acid transporters (EAATs, EAACs) regulate neuronal signaling through the influx of glutamate from the synaptic cleft into the neuron. EAATs have five isoforms, of which EAAT1-3 are the most abundantly distributed in the brain [64,65]. EAAT1 (glutamate-aspartate transporter, GLAST) and EAAT2 (glutamate transporter-1, GLT-1) are expressed in neuroglia cells. EAAT3 (exciting amino acid carrier 1, EAAC1) is expressed in mature neurons [64,65,66].
EAAC1 is the primary neuronal glutamate transporter and is responsible for the transport of high-affinity sodium-dependent L-glutamate. EAAC1 also plays an important role in GSH synthesis in the midbrain via the uptake of cysteine into neurons [64,65,66,67,68]. When brain-disease-induced oxidative stress induces EAAC1 dysfunction, caused by peroxynitrite or H2O2, this reduces the concentration of neuronal cysteine, indicating a disturbance of GSH synthesis in the mouse midbrain [24,63,65,67,68]. The oxidative-stress-induced dysfunction of EAAC1 was further revealed to contribute to neuronal damage in Alzheimer’s and ischemic stroke patients [24,63,65]. In addition, the GTRAP3-18 gene, which is functionally related to the EAAC1 gene, contributes to GSH regulation [25,69,70,71]. GTRAP3-18 is a family of RAB receptors (PRA) that have subtypes of PRA1 and PRA2 [25,69]. The subtypes of PRA1 and PRA2 have been shown to have intracellular positions in the Golgi complex and vesicles (ER) [25].
The hydrophobic domain interaction between GTRAP3-18 and EAAC1 inhibits EAAC1 translocation from the ER [25,69]. Thereafter, GTRAP3-18 binds to the C-terminal domain of EAAC1 and inhibits glutamate uptake [25,67,69]. It was also confirmed that EAAC1 was increased in the plasma membrane in GTRAP3-18 gene-deleted mice and the concentrations of cysteine and GSH in the brain were elevated in GTRAP3-18 gene-deleted mice [25,69]. In other words, as GTRAP3-18 gene expression increased, the expression of the EAAC1 gene decreased, and it was confirmed that the two genes play opposite roles. Finally, it was confirmed that the increased expression of GTRAP3-18 caused an increase in oxidative stress, a decrease in GSH levels, and was deleterious to neurons [25,66,69].
In particular, the EAAC1 gene is highly involved in the entire process of neurogenesis, including cell proliferation, differentiation, and survival after cerebral ischemia [72]. It is important for hippocampal neurogenesis via the regulation of cysteine influx through EAAC1 and its interaction with glutamate [72,73]. EAAC1 deletion promotes increased ischemic damage due to low concentrations of glutathione owing to a lack of cysteine uptake [72,73]. However, when NAC is administered, it acts as a substitute for cysteine, is combined with glutamate, and facilitates GSH synthesis through the GSH synthetic pathway [72,74]. It regulates ROS and glutamate, neurotrophic, and inflammatory pathways via GSH synthesized by NAC and ultimately plays a role in reducing neuronal cell death after cerebral ischemia [63,65,69,72,73,74] (Figure 3).
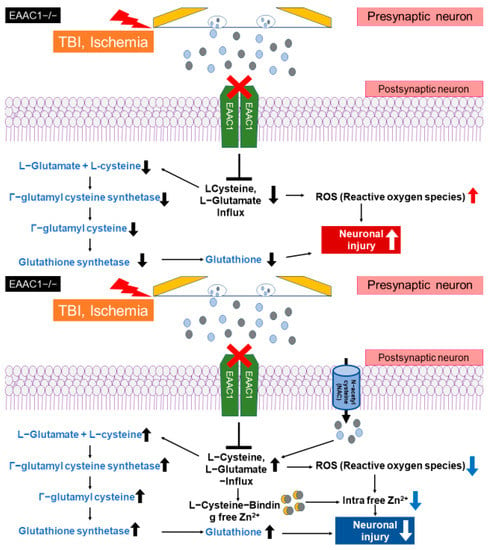
Figure 3.
Traumatic brain injury or ischemic stroke when EAAC1 knockout inhibits cysteine translocation [13,73]. Deletion of EAAC1 induced loss of L-cysteine and L-glutamate uptake, and ROS-mediated neuronal damage was preserved [13,73]. NAC can bind to presynaptically released zinc, and cysteine supplementation promotes enhanced GSH synthesis and zinc binding [13,73].
5. The Role of Glutathione in Zinc-Induced Neuron Death after Brain Injury
5.1. Zinc and Glutathione in Stroke
Global cerebral ischemia (GCI) is caused by a sudden and drastically decreased blood flow to the brain, resulting in primary neuronal damage due to lack of oxygen and energy supply [75]. Secondary damage leads to the disruption of the blood–brain barrier (BBB), activation of microglia, and production of ROS [75]. ROS-mediated free radicals trigger oxidative damage by releasing zinc and glutamate from the presynaptic terminal, leading to the activation of neuronal death cascades [75]. GSH neutralizes free radicals generated through excessive free zinc release after cerebral ischemia and is critical for neuronal survival [75]. Previous studies have demonstrated that EAAC1 gene deletion exacerbates neuronal cell death after cerebral ischemia [13]. In addition, it has been demonstrated that the accumulation of a large amount of zinc after cerebral ischemia is also directly linked to the deletion of the EAAC1 gene [13,72,73,74]. Cysteine uptake via EAAC1 contributes to the production of glutathione (GSH), a potent cellular antioxidant. Furthermore, cysteine, a thiol-containing amino acid, has been demonstrated to have a zinc-chelating effect and, consequently, to protect neurons against brain damage [13,72,73,74]. Restricted neuronal cysteine transport due to the deletion of the EAAC1 gene leads to elevated levels of free zinc in the presynaptic terminal and cytoplasm, suggesting that zinc accumulation exacerbates subsequent neuronal cell death after brain injury. In addition, zinc accumulation in neurons triggers the inhibition of glutathione reductase, ROS production, and increased neuronal death [13,72,73,74]. In the absence of functional EAAC1, the administration of the transmembrane cysteine prodrug N-acetylcysteine (NAC) rescues neuronal cysteine homeostasis, a function normally provided by EAAC1, allowing the free passage of cysteine through the cell membrane of neurons into the cytoplasmic compartment [13,72,73,74]. Taken together, we can infer that cysteine introduced through NAC administration inhibits neuronal free zinc influx, strongly suggesting that it plays a protective role in neurons by the enhancing synthesis of glutathione [13,72,73,74]. Although the impairment of cysteine uptake by EAAC1 gene deletion increases free zinc levels in neurons, we demonstrated that NAC treatment reduced neuronal free zinc levels in EAAC1-knockout mice [13,72,73,74]. Therefore, these results demonstrate the important role of EAAC1 in zinc homeostasis and in bolstering endogenous antioxidant defense mechanisms after acute brain injury [72,73,74]. Finally, after the administration of N-acetylcysteine (NAC, 150 mg/kg, i.p.), a membrane-permeable cysteine prodrug, we observed increased GSH content and reduced BBB destruction, vascular disorganization, and neuronal cell death after GCI [73].
Protocatechuic acid (PCA), one of the major metabolites of antioxidant polyphenols, has a strong antioxidant effect on cells, an antiproliferative effect on tumor cells, and a protective effect against neuronal apoptosis after cerebral ischemia [75]. In particular, PCA has a neuroprotective effect against neuronal cell death through the inhibition of ROS due to the antioxidant effect of PCA [75]. The administration of PCA (30 mg/kg, p.o.) after GCI increased hippocampal glutathione levels and reduced neuronal cell death, ROS production, and BBB disruption. In addition, as an inflammatory mediator, PCA plays a key role in reducing the activity of microglia and astrocytes [75] (Table 1).

Table 1.
Neuroprotective effects of GSH supplementation in several brain insults.
5.2. Zinc and Glutathione in Traumatic Brain Injury
Traumatic brain injury (TBI) is one of the most prevalent brain disorders and is caused by physical trauma from an accident or violent impact to the head [24,80]. TBI causes edema of the brain as a primary injury and a vast and diverse inflammatory response, followed by secondary damage which leads to neuronal death [24,80,81]. In the secondary damage of TBI, oxidative stress and the activation of microglia and astrocytes play a large role [24,76]. Glutathione deletion and the accumulation of zinc in neurons induces oxidative stress, which promotes neuronal death [24,76]. It is significant that the neuronal death that occurs when a traumatic brain injury is induced in mice deficient in the EAAC1 gene, which is related to deficient glutathione synthesis, can be prevented by a single dose of NAC (150 mg/kg, i.p.), which acts as an alternative source of cysteine in the absence of functional EAAC1 [24,72].
In addition, the TBI-induced loss of GSH via the influx of excessive presynaptically released zinc and ROS production was shown to trigger neuronal cell death and cognitive impairment [76]. However, previous studies found that the administration of PCA (30 mg/kg, i.p.), known as a powerful antioxidant, had a neuroprotective effect in the context of TBI by enhancing GSH levels. Moreover, PCA treatment after TBI reduced dendritic damage in the hippocampus and cortex, reduced microglia and macrophage activation, and prevented delayed neuronal death after TBI [76] (Table 1).
5.3. Zinc and Glutathione in Hypoglycemia
Hypoglycemic brain damage is caused by insufficient glucose supply, especially in diabetic patients on insulin therapy [78,79]. Hypoglycemia induces low-frequency EEG activity, which can lead to cognitive impairment and neuronal cell death due to low glucose and ATP depletion [78,79]. To recover from the hypoglycemic condition, glucose reperfusion is necessary. However, rapid glucose reperfusion also triggers secondary damage, called “glucose-reperfusion injury”. Glucose reperfusion causes ROS production, the activation of glutamate receptors, and the release of extracellular zinc, triggering neuronal cell death [78,79]. In particular, when zinc influx arises from presynaptic terminals, poly(ADP-ribose)polymerase (PARP) is activated, resulting in ATP depletion, superoxide production, and a lack of GSH [78,79]. However, as a result of administering NAC (300 mg/kg, i.p.) after hypoglycemia, translocated zinc into the hippocampal neurons is chelated and GSH levels are increased, thereby reducing oxidative damage, BBB disruption, microglia activation, and neuronal death [78,79] (Table 1).
Recurrent moderate hypoglycemia (R/M hypoglycemia)-induced PARP-1 activation depends on cytoplasmic NAD. NAD is an essential component of glycolysis, and even when glucose availability is restored by PARP-1 activation after hypoglycemia, cells become unable to use glucose, resulting in ATP depletion [78,79]. The depletion of ATP leads to oxidative damage, zinc accumulation, and the depletion of GSH [78,79]. However, the administration of pyruvate acid (500 mg/kg, i.p.), which provides an alternative source of ATP production through the TCA cycle, has been shown to decrease dendritic damage, microglia activation, vascular loss, and zinc accumulation [78,79] (Table 1).
5.4. Zinc and Glutathione in Epilepsy
Epilepsy is caused by the excessive activation of excitatory synaptic neurotransmission, or the imbalanced regulation of inhibitory neurotransmission and oxidative stress caused by an imbalance in free radical and nitrogen production [77]. In particular, epilepsy has been identified to lead to a significant increase in oxidative stress, and it has been found that an alteration in the antioxidant system in epilepsy is therefore of considerable importance [77]. Previous studies verified that PCA (25 mg/kg) treatment after pilocarpine-induced (25 mg/kg) epilepsy reduced oxidative damage, microglia activation, and neuronal death, and prevented a deficiency in GSH [77] (Table 1).
5.5. Zinc and Glutathione in Brain Injuries
Taken together, when brain insult occurs, excessive amount of vesicular zinc is released from the presynaptic terminals and translocated into the postsynaptic neurons. Then, accumulated zinc activates PKC (Protein kinase c), which translocates NADPH subunits P47(phox) and P67(phox) to the cytoplasmic membrane [81,82,83,84]. Moved subunits P47(phox) and P67(phox) activate membrane components of gp91 (phox) and p22(phox)) to form superoxide-generating enzyme components [81,82,83,84]. This reaction increases ROS production and increases oxidative stress [78,79,81,82,83,84]. Oxidative stress activates PARP-1 (Poly ADP-Ribose Polimerase-1), which consumes the existing ATP and results in severe neuron damage [78,79,81,82,83,84] (Figure 4A). However, when GSH is present in the postsynaptic neurons, it binds free zinc translocated from the synaptic cleft, thereby reducing the free zinc level, and inhibiting PKC activation [13,72,73,74]. Then zinc-induced PKC activation and ROS production is inhibited [13,72,73,74,77]. Additionally, GSH itself functions as an antioxidant component to reduce ROS, thereby having a protective role against neuronal death after stoke, traumatic brain injury, hypoglycemia and epilepsy [13,72,73,74,77] (Table 1).
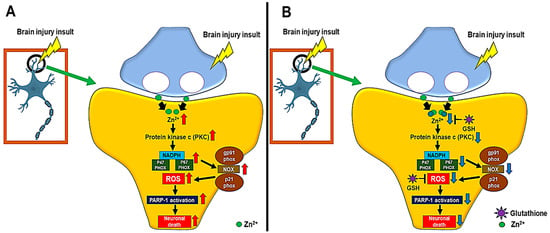
Figure 4.
(A) When a brain injury occurs, excess vesicular zinc influxes into the cytoplasm of neurons. Then, protein kinase c (PKC) is overexpressed by the vesicular zinc [81,82,83,84]. Due to activated PKC, nicotinamide adenine dinucleotide phosphate (NADPH) is activated, and, as a result, p47(phox) and p67(phox) of NADPH subunits activate gp91(phox) and p21(phox) present in the neuron membrane to generate superoxide [81,82,83,84]. (B) However, when GSH is formed, it binds to free zinc to reduce NADPH oxidase activation, which thereby reduces the final product, ROS, or GSH prevents neuronal death by acting as an antioxidant, reducing ROS directly [13,72,73,74].
6. Conclusions
Glutathione (GSH) is a major component of cellular antioxidant systems and has a neuroprotective role in several brain insults. Previous studies have demonstrated that GSH plays a neuroprotective role by inhibiting the generation of reactive oxygen species after cerebral ischemia, traumatic brain injury, hypoglycemia, and epilepsy. The excessive neuronal accumulation of zinc downregulates GSH synthesis, which aggravates neuronal injuries after the above brain insults. Thus, in this review, we discussed evidence that GSH is an essential factor for preventing zinc-induced neuronal death. Furthermore, we suggest that the modulation of zinc in the brain may have neuroprotective effects via the protection or conservation of the integrity of GSH-dependent cellular antioxidant systems.
Author Contributions
M.K.P. performed the data analysis and reviewed and edited the manuscript. B.Y.C., A.R.K., S.H.L. (Song Hee Lee), D.K.H., B.S.K. and S.H.L. (Si Hyun Lee) reviewed and edited the manuscript. S.W.S. contributed to the discussion and wrote, reviewed, and edited the manuscript. S.W.S. takes full responsibility for the manuscript and its originality. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by funding from the National Research Foundation of Korea (NRF) (NRF-2020R1A2C2008480 to S.W.S.). Additionally, this work was supported by the Hallym University Research Fund (HRF-202204-009).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest in this study.
References
- Lee, K.H.; Cha, M.; Lee, B.H. Neuroprotective Effect of Antioxidants in the Brain. Int. J. Mol. Sci. 2020, 21, 7152. [Google Scholar] [CrossRef] [PubMed]
- Porteous, J.W. Glutamate, glutamine, aspartate, asparagine, glucose and ketone-body metabolism in chick intestinal brush-border cells. Biochem. J. 1980, 188, 619–632. [Google Scholar] [CrossRef] [PubMed]
- Espinosa-Diez, C.; Miguel, V.; Mennerich, D.; Kietzmann, T.; Sanchez-Perez, P.; Cadenas, S.; Lamas, S. Antioxidant responses and cellular adjustments to oxidative stress. Redox Biol. 2015, 6, 183–197. [Google Scholar] [CrossRef] [PubMed]
- Couto, N.; Wood, J.; Barber, J. The role of glutathione reductase and related enzymes on cellular redox homoeostasis network. Free Radic. Biol. Med. 2016, 95, 27–42. [Google Scholar] [CrossRef]
- Anjaneyulu, M.; Berent-Spillson, A.; Russell, J.W. Metabotropic glutamate receptors (mGluRs) and diabetic neuropathy. Curr. Drug Targets 2008, 9, 85–93. [Google Scholar] [CrossRef]
- Jiang, L.J.; Maret, W.; Vallee, B.L. The glutathione redox couple modulates zinc transfer from metallothionein to zinc-depleted sorbitol dehydrogenase. Proc. Natl. Acad. Sci. USA 1998, 95, 3483–3488. [Google Scholar] [CrossRef]
- Choi, S.; Hong, D.K.; Choi, B.Y.; Suh, S.W. Zinc in the Brain: Friend or Foe? Int. J. Mol. Sci. 2020, 21, 8941. [Google Scholar] [CrossRef]
- MacDonald, R.S. The role of zinc in growth and cell proliferation. J. Nutr. 2000, 130 (Suppl. S5), 1500S–1508S. [Google Scholar] [CrossRef]
- Beyersmann, D.; Haase, H. Functions of zinc in signaling, proliferation and differentiation of mammalian cells. Biometals 2001, 14, 331–341. [Google Scholar] [CrossRef]
- Besser, L.; Chorin, E.; Sekler, I.; Silverman, W.F.; Atkin, S.; Russell, J.T.; Hershfinkel, M. Synaptically released zinc triggers metabotropic signaling via a zinc-sensing receptor in the hippocampus. J. Neurosci. 2009, 29, 2890–2901. [Google Scholar] [CrossRef]
- Morris, D.R.; Levenson, C.W. Ion channels and zinc: Mechanisms of neurotoxicity and neurodegeneration. J. Toxicol. 2012, 2012, 785647. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.Y.; Hong, D.K.; Jeong, J.H.; Lee, B.E.; Koh, J.Y.; Suh, S.W. Zinc transporter 3 modulates cell proliferation and neuronal differentiation in the adult hippocampus. Stem Cells 2020, 38, 994–1006. [Google Scholar] [CrossRef] [PubMed]
- Jang, B.G.; Won, S.J.; Kim, J.H.; Choi, B.Y.; Lee, M.W.; Sohn, M.; Song, H.K.; Suh, S.W. EAAC1 gene deletion alters zinc homeostasis and enhances cortical neuronal injury after transient cerebral ischemia in mice. J. Trace Elem. Med. Biol. 2012, 26, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.Y.; Suh, S.W. Antimicrotubule Agent-Induced Zinc Neurotoxicity. Biol. Pharm. Bull. 2018, 41, 1001–1005. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.Y.; Hong, D.K.; Suh, S.W. ZnT3 Gene Deletion Reduces Colchicine-Induced Dentate Granule Cell Degeneration. Int. J. Mol. Sci. 2017, 18, 2189. [Google Scholar] [CrossRef]
- Magi, S.; Piccirillo, S.; Amoroso, S.; Lariccia, V. Excitatory Amino Acid Transporters (EAATs): Glutamate Transport and Beyond. Int. J. Mol. Sci. 2019, 20, 5674. [Google Scholar] [CrossRef]
- Malik, A.R.; Willnow, T.E. Excitatory Amino Acid Transporters in Physiology and Disorders of the Central Nervous System. Int. J. Mol. Sci. 2019, 20, 5671. [Google Scholar] [CrossRef]
- Kim, K.; Lee, S.G.; Kegelman, T.P.; Su, Z.Z.; Das, S.K.; Dash, R.; Dasgupta, S.; Barral, P.M.; Hedvat, M.; Diaz, P.; et al. Role of excitatory amino acid transporter-2 (EAAT2) and glutamate in neurodegeneration: Opportunities for developing novel therapeutics. J. Cell. Physiol. 2011, 226, 2484–2493. [Google Scholar] [CrossRef]
- Parkin, G.M.; Udawela, M.; Gibbons, A.; Dean, B. Glutamate transporters, EAAT1 and EAAT2, are potentially important in the pathophysiology and treatment of schizophrenia and affective disorders. World J. Psychiatry 2018, 8, 51–63. [Google Scholar] [CrossRef]
- Furuta, A.; Martin, L.J.; Lin, C.L.; Dykes-Hoberg, M.; Rothstein, J.D. Cellular and synaptic localization of the neuronal glutamate transporters excitatory amino acid transporter 3 and 4. Neuroscience 1997, 81, 1031–1042. [Google Scholar] [CrossRef]
- Lukasiewcz, P.D.; Bligard, G.W.; DeBrecht, J.D. EAAT5 Glutamate Transporter-Mediated Inhibition in the Vertebrate Retina. Front. Cell. Neurosci. 2021, 15, 662859. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Ko, D.G.; Hong, D.K.; Lim, M.S.; Choi, B.Y.; Suh, S.W. Role of Excitatory Amino Acid Carrier 1 (EAAC1) in Neuronal Death and Neurogenesis After Ischemic Stroke. Int. J. Mol. Sci. 2020, 21, 5676. [Google Scholar] [CrossRef]
- Kim, H.B.; Yoo, J.Y.; Yoo, S.Y.; Lee, J.H.; Chang, W.; Kim, H.S.; Baik, T.K.; Woo, R.S. Neuregulin-1 inhibits CoCl2-induced upregulation of excitatory amino acid carrier 1 expression and oxidative stress in SH-SY5Y cells and the hippocampus of mice. Mol. Brain 2020, 13, 153. [Google Scholar] [CrossRef]
- Choi, B.Y.; Kim, I.Y.; Kim, J.H.; Lee, B.E.; Lee, S.H.; Kho, A.R.; Jung, H.J.; Sohn, M.; Song, H.K.; Suh, S.W. Decreased cysteine uptake by EAAC1 gene deletion exacerbates neuronal oxidative stress and neuronal death after traumatic brain injury. Amino Acids 2016, 48, 1619–1629. [Google Scholar] [CrossRef] [PubMed]
- Aoyama, K.; Nakaki, T. Inhibition of GTRAP3-18 may increase neuroprotective glutathione (GSH) synthesis. Int. J. Mol. Sci. 2012, 13, 12017–12035. [Google Scholar] [CrossRef] [PubMed]
- Kim, K. Glutathione in the Nervous System as a Potential Therapeutic Target to Control the Development and Progression of Amyotrophic Lateral Sclerosis. Antioxidants 2021, 10, 1011. [Google Scholar] [CrossRef] [PubMed]
- Aoyama, K. Glutathione in the Brain. Int. J. Mol. Sci. 2021, 22, 5010. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, L.; Sandhu, J.K.; Harper, M.E.; Cuperlovic-Culf, M. Role of Glutathione in Cancer: From Mechanisms to Therapies. Biomolecules 2020, 10, 1429. [Google Scholar] [CrossRef]
- Toroser, D.; Yarian, C.S.; Orr, W.C.; Sohal, R.S. Mechanisms of gamma-glutamylcysteine ligase regulation. Biochim. Biophys. Acta 2006, 1760, 233–244. [Google Scholar] [CrossRef]
- Krejsa, C.M.; Franklin, C.C.; White, C.C.; Ledbetter, J.A.; Schieven, G.L.; Kavanagh, T.J. Rapid activation of glutamate cysteine ligase following oxidative stress. J. Biol. Chem. 2010, 285, 16116–16124. [Google Scholar] [CrossRef]
- Lu, S.C. Glutathione synthesis. Biochim. Biophys. Acta 2013, 1830, 3143–3153. [Google Scholar] [CrossRef] [PubMed]
- Forman, H.J.; Zhang, H.; Rinna, A. Glutathione: Overview of its protective roles, measurement, and biosynthesis. Mol. Asp. Med. 2009, 30, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Hasanuzzaman, M.; Nahar, K.; Anee, T.I.; Fujita, M. Glutathione in plants: Biosynthesis and physiological role in environmental stress tolerance. Physiol. Mol. Biol. Plants 2017, 23, 249–268. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, S. Neuroprotective Function of High Glycolytic Activity in Astrocytes: Common Roles in Stroke and Neurodegenerative Diseases. Int. J. Mol. Sci. 2021, 22, 6568. [Google Scholar] [CrossRef] [PubMed]
- Tu, D.; Gao, Y.; Yang, R.; Guan, T.; Hong, J.S.; Gao, H.M. The pentose phosphate pathway regulates chronic neuroinflammation and dopaminergic neurodegeneration. J. Neuroinflamm. 2019, 16, 255. [Google Scholar] [CrossRef]
- Chen, Y.; Qin, C.; Huang, J.; Tang, X.; Liu, C.; Huang, K.; Xu, J.; Guo, G.; Tong, A.; Zhou, L. The role of astrocytes in oxidative stress of central nervous system: A mixed blessing. Cell Prolif. 2020, 53, e12781. [Google Scholar] [CrossRef]
- Takahashi, S.; Mashima, K. Neuroprotection and Disease Modification by Astrocytes and Microglia in Parkinson Disease. Antioxidants 2022, 11, 170. [Google Scholar] [CrossRef]
- Ookhtens, M.; Kaplowitz, N. Role of the liver in interorgan homeostasis of glutathione and cyst(e)ine. Semin. Liver Dis. 1998, 18, 313–329. [Google Scholar] [CrossRef]
- Lauterburg, B.H.; Adams, J.D.; Mitchell, J.R. Hepatic glutathione homeostasis in the rat: Efflux accounts for glutathione turnover. Hepatology 1984, 4, 586–590. [Google Scholar] [CrossRef]
- Bannai, S.; Tateishi, N. Role of membrane transport in metabolism and function of glutathione in mammals. J. Membr. Biol. 1986, 89, 1–8. [Google Scholar] [CrossRef]
- Rahantaniaina, M.S.; Li, S.; Chatel-Innocenti, G.; Tuzet, A.; Mhamdi, A.; Vanacker, H.; Noctor, G. Glutathione oxidation in response to intracellular H2O2: Key but overlapping roles for dehydroascorbate reductases. Plant Signal. Behav. 2017, 12, e1356531. [Google Scholar] [CrossRef] [PubMed]
- Roxas, V.P.; Smith, R.K., Jr.; Allen, E.R.; Allen, R.D. Overexpression of glutathione S-transferase/glutathione peroxidase enhances the growth of transgenic tobacco seedlings during stress. Nat. Biotechnol. 1997, 15, 988–991. [Google Scholar] [CrossRef] [PubMed]
- Rouhier, N. Plant glutaredoxins: Pivotal players in redox biology and iron-sulphur centre assembly. New Phytol. 2010, 186, 365–372. [Google Scholar] [CrossRef]
- Chen, L.; Zhang, Z.; Hoshino, A.; Zheng, H.D.; Morley, M.; Arany, Z.; Rabinowitz, J.D. NADPH production by the oxidative pentose-phosphate pathway supports folate metabolism. Nat. Metab. 2019, 1, 404–415. [Google Scholar] [CrossRef] [PubMed]
- Ogasawara, Y.; Funakoshi, M.; Ishii, K. Determination of reduced nicotinamide adenine dinucleotide phosphate concentration using high-performance liquid chromatography with fluorescence detection: Ratio of the reduced form as a biomarker of oxidative stress. Biol. Pharm. Bull. 2009, 32, 1819–1823. [Google Scholar] [CrossRef]
- Dore, M.P.; Parodi, G.; Portoghese, M.; Pes, G.M. The Controversial Role of Glucose-6-Phosphate Dehydrogenase Deficiency on Cardiovascular Disease: A Narrative Review. Oxidative Med. Cell. Longev. 2021, 2021, 5529256. [Google Scholar] [CrossRef]
- Hao, S.; Liang, B.; Huang, Q.; Dong, S.; Wu, Z.; He, W.; Shi, M. Metabolic networks in ferroptosis. Oncol. Lett. 2018, 15, 5405–5411. [Google Scholar] [CrossRef]
- Li, J.; Cao, F.; Yin, H.L.; Huang, Z.J.; Lin, Z.T.; Mao, N.; Sun, B.; Wang, G. Ferroptosis: Past, present and future. Cell Death Dis. 2020, 11, 88. [Google Scholar] [CrossRef]
- Tang, D.; Chen, X.; Kang, R.; Kroemer, G. Ferroptosis: Molecular mechanisms and health implications. Cell Res. 2021, 31, 107–125. [Google Scholar] [CrossRef]
- Canli, O.; Alankus, Y.B.; Grootjans, S.; Vegi, N.; Hultner, L.; Hoppe, P.S.; Schroeder, T.; Vandenabeele, P.; Bornkamm, G.W.; Greten, F.R. Glutathione peroxidase 4 prevents necroptosis in mouse erythroid precursors. Blood 2016, 127, 139–148. [Google Scholar] [CrossRef]
- Ribas, V.; Garcia-Ruiz, C.; Fernandez-Checa, J.C. Glutathione and mitochondria. Front. Pharmacol. 2014, 5, 151. [Google Scholar] [CrossRef] [PubMed]
- Roohani, N.; Hurrell, R.; Kelishadi, R.; Schulin, R. Zinc and its importance for human health: An integrative review. J. Res. Med. Sci. 2013, 18, 144–157. [Google Scholar] [PubMed]
- Plum, L.M.; Rink, L.; Haase, H. The essential toxin: Impact of zinc on human health. Int. J. Environ. Res. Public Health 2010, 7, 1342–1365. [Google Scholar] [CrossRef] [PubMed]
- Li, M.S.; Adesina, S.E.; Ellis, C.L.; Gooch, J.L.; Hoover, R.S.; Williams, C.R. NADPH oxidase-2 mediates zinc deficiency-induced oxidative stress and kidney damage. Am. J. Physiol. Cell Physiol. 2017, 312, C47–C55. [Google Scholar] [CrossRef]
- Noh, K.M.; Koh, J.Y. Induction and activation by zinc of NADPH oxidase in cultured cortical neurons and astrocytes. J. Neurosci. 2000, 20, RC111. [Google Scholar] [CrossRef]
- Trevisan, R.; Flesch, S.; Mattos, J.J.; Milani, M.R.; Bainy, A.C.; Dafre, A.L. Zinc causes acute impairment of glutathione metabolism followed by coordinated antioxidant defenses amplification in gills of brown mussels Perna perna. Comp. Biochem. Physiol. C Toxicol. Pharmacol. 2014, 159, 22–30. [Google Scholar] [CrossRef]
- Slepchenko, K.G.; Lu, Q.; Li, Y.V. Cross talk between increased intracellular zinc (Zn(2+)) and accumulation of reactive oxygen species in chemical ischemia. Am. J. Physiol. Cell Physiol. 2017, 313, C448–C459. [Google Scholar] [CrossRef]
- Bishop, G.M.; Dringen, R.; Robinson, S.R. Zinc stimulates the production of toxic reactive oxygen species (ROS) and inhibits glutathione reductase in astrocytes. Free Radic. Biol. Med. 2007, 42, 1222–1230. [Google Scholar] [CrossRef]
- Ryu, R.; Shin, Y.; Choi, J.W.; Min, W.; Ryu, H.; Choi, C.R.; Ko, H. Depletion of intracellular glutathione mediates zinc-induced cell death in rat primary astrocytes. Exp. Brain Res. 2002, 143, 257–263. [Google Scholar] [CrossRef]
- Mize, C.E.; Langdon, R.G. Hepatic glutathione reductase. I. Purification and general kinetic properties. J. Biol. Chem. 1962, 237, 1589–1595. [Google Scholar] [CrossRef]
- Chen, C.J.; Liao, S.L. Zinc toxicity on neonatal cortical neurons: Involvement of glutathione chelation. J. Neurochem. 2003, 85, 443–453. [Google Scholar] [CrossRef] [PubMed]
- Higashi, Y.; Aratake, T.; Shimizu, T.; Shimizu, S.; Saito, M. Protective Role of Glutathione in the Hippocampus after Brain Ischemia. Int. J. Mol. Sci. 2021, 22, 7765. [Google Scholar] [CrossRef] [PubMed]
- Hong, D.K.; Kho, A.R.; Lee, S.H.; Jeong, J.H.; Kang, B.S.; Kang, D.H.; Park, M.K.; Park, K.H.; Lim, M.S.; Choi, B.Y.; et al. Transient Receptor Potential Melastatin 2 (TRPM2) Inhibition by Antioxidant, N-Acetyl-l-Cysteine, Reduces Global Cerebral Ischemia-Induced Neuronal Death. Int. J. Mol. Sci. 2020, 21, 6026. [Google Scholar] [CrossRef] [PubMed]
- Aoyama, K.; Nakaki, T. Glutathione in Cellular Redox Homeostasis: Association with the Excitatory Amino Acid Carrier 1 (EAAC1). Molecules 2015, 20, 8742–8758. [Google Scholar] [CrossRef] [PubMed]
- Danbolt, N.C. Glutamate uptake. Prog. Neurobiol. 2001, 65, 1–105. [Google Scholar] [CrossRef]
- Rothstein, J.D.; Dykes-Hoberg, M.; Pardo, C.A.; Bristol, L.A.; Jin, L.; Kuncl, R.W.; Kanai, Y.; Hediger, M.A.; Wang, Y.; Schielke, J.P.; et al. Knockout of glutamate transporters reveals a major role for astroglial transport in excitotoxicity and clearance of glutamate. Neuron 1996, 16, 675–686. [Google Scholar] [CrossRef] [PubMed]
- Won, S.J.; Yoo, B.H.; Brennan, A.M.; Shin, B.S.; Kauppinen, T.M.; Berman, A.E.; Swanson, R.A.; Suh, S.W. EAAC1 gene deletion alters zinc homeostasis and exacerbates neuronal injury after transient cerebral ischemia. J. Neurosci. 2010, 30, 15409–15418. [Google Scholar] [CrossRef] [PubMed]
- Aoyama, K.; Suh, S.W.; Hamby, A.M.; Liu, J.; Chan, W.Y.; Chen, Y.; Swanson, R.A. Neuronal glutathione deficiency and age-dependent neurodegeneration in the EAAC1 deficient mouse. Nat. Neurosci. 2006, 9, 119–126. [Google Scholar] [CrossRef]
- Aoyama, K.; Wang, F.; Matsumura, N.; Kiyonari, H.; Shioi, G.; Tanaka, K.; Kinoshita, C.; Kikuchi-Utsumi, K.; Watabe, M.; Nakaki, T. Increased neuronal glutathione and neuroprotection in GTRAP3-18-deficient mice. Neurobiol. Dis. 2012, 45, 973–982. [Google Scholar] [CrossRef]
- Watabe, M.; Aoyama, K.; Nakaki, T. Regulation of glutathione synthesis via interaction between glutamate transport-associated protein 3-18 (GTRAP3-18) and excitatory amino acid carrier-1 (EAAC1) at plasma membrane. Mol. Pharmacol. 2007, 72, 1103–1110. [Google Scholar] [CrossRef]
- Watabe, M.; Aoyama, K.; Nakaki, T. A dominant role of GTRAP3-18 in neuronal glutathione synthesis. J. Neurosci. 2008, 28, 9404–9413. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.Y.; Won, S.J.; Kim, J.H.; Sohn, M.; Song, H.K.; Chung, T.N.; Kim, T.Y.; Suh, S.W. EAAC1 gene deletion reduces adult hippocampal neurogenesis after transient cerebral ischemia. Sci. Rep. 2018, 8, 6903. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.Y.; Kim, J.H.; Kim, H.J.; Lee, B.E.; Kim, I.Y.; Sohn, M.; Suh, S.W. EAAC1 gene deletion increases neuronal death and blood brain barrier disruption after transient cerebral ischemia in female mice. Int. J. Mol. Sci. 2014, 15, 19444–19457. [Google Scholar] [CrossRef] [PubMed]
- Bavarsad Shahripour, R.; Harrigan, M.R.; Alexandrov, A.V. N-acetylcysteine (NAC) in neurological disorders: Mechanisms of action and therapeutic opportunities. Brain Behav. 2014, 4, 108–122. [Google Scholar] [CrossRef]
- Kho, A.R.; Choi, B.Y.; Lee, S.H.; Hong, D.K.; Lee, S.H.; Jeong, J.H.; Park, K.H.; Song, H.K.; Choi, H.C.; Suh, S.W. Effects of Protocatechuic Acid (PCA) on Global Cerebral Ischemia-Induced Hippocampal Neuronal Death. Int. J. Mol. Sci. 2018, 19, 1420. [Google Scholar] [CrossRef]
- Lee, S.H.; Choi, B.Y.; Lee, S.H.; Kho, A.R.; Jeong, J.H.; Hong, D.K.; Suh, S.W. Administration of Protocatechuic Acid Reduces Traumatic Brain Injury-Induced Neuronal Death. Int. J. Mol. Sci. 2017, 18, 2510. [Google Scholar] [CrossRef]
- Lee, S.H.; Choi, B.Y.; Kho, A.R.; Jeong, J.H.; Hong, D.K.; Lee, S.H.; Lee, S.Y.; Lee, M.W.; Song, H.K.; Choi, H.C.; et al. Protective Effects of Protocatechuic Acid on Seizure-Induced Neuronal Death. Int. J. Mol. Sci. 2018, 19, 187. [Google Scholar] [CrossRef]
- Kho, A.R.; Choi, B.Y.; Kim, J.H.; Lee, S.H.; Hong, D.K.; Lee, S.H.; Jeong, J.H.; Sohn, M.; Suh, S.W. Prevention of hypoglycemia-induced hippocampal neuronal death by N-acetyl-L-cysteine (NAC). Amino Acids 2017, 49, 367–378. [Google Scholar] [CrossRef]
- Choi, B.Y.; Kim, J.H.; Kim, H.J.; Yoo, J.H.; Song, H.K.; Sohn, M.; Won, S.J.; Suh, S.W. Pyruvate administration reduces recurrent/moderate hypoglycemia-induced cortical neuron death in diabetic rats. PLoS ONE 2013, 8, e81523. [Google Scholar] [CrossRef]
- Choi, B.Y.; Lee, S.H.; Choi, H.C.; Lee, S.K.; Yoon, H.S.; Park, J.B.; Chung, W.S.; Suh, S.W. Alcohol dependence treating agent, acamprosate, prevents traumatic brain injury-induced neuron death through vesicular zinc depletion. Transl. Res. 2019, 207, 1–18. [Google Scholar] [CrossRef]
- Park, M.K.; Choi, B.Y.; Kho, A.R.; Lee, S.H.; Hong, D.K.; Jeong, J.H.; Kang, D.H.; Kang, B.S.; Suh, S.W. Effects of Transient Receptor Potential Cation 5 (TRPC5) Inhibitor, NU6027, on Hippocampal Neuronal Death after Traumatic Brain Injury. Int. J. Mol. Sci. 2020, 21, 8256. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.Y.; Jang, B.G.; Kim, J.H.; Lee, B.E.; Sohn, M.; Song, H.K.; Suh, S.W. Prevention of traumatic brain injury-induced neuronal death by inhibition of NADPH oxidase activation. Brain Res. 2012, 1481, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Choi, B.Y.; Kho, A.R.; Jeong, J.H.; Hong, D.K.; Kang, D.H.; Kang, B.S.; Song, H.K.; Choi, H.C.; Suh, S.W. Inhibition of NADPH Oxidase Activation by Apocynin Rescues Seizure-Induced Reduction of Adult Hippocampal Neurogenesis. Int. J. Mol. Sci. 2018, 19, 3087. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Jang, B.G.; Choi, B.Y.; Kim, H.S.; Sohn, M.; Chung, T.N.; Choi, H.C.; Song, H.K.; Suh, S.W. Post-treatment of an NADPH oxidase inhibitor prevents seizure-induced neuronal death. Brain Res. 2013, 1499, 163–172. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).