Cell-Molecular Interactions of Nano- and Microparticles in Dental Implantology
Abstract
1. Introduction
2. Results
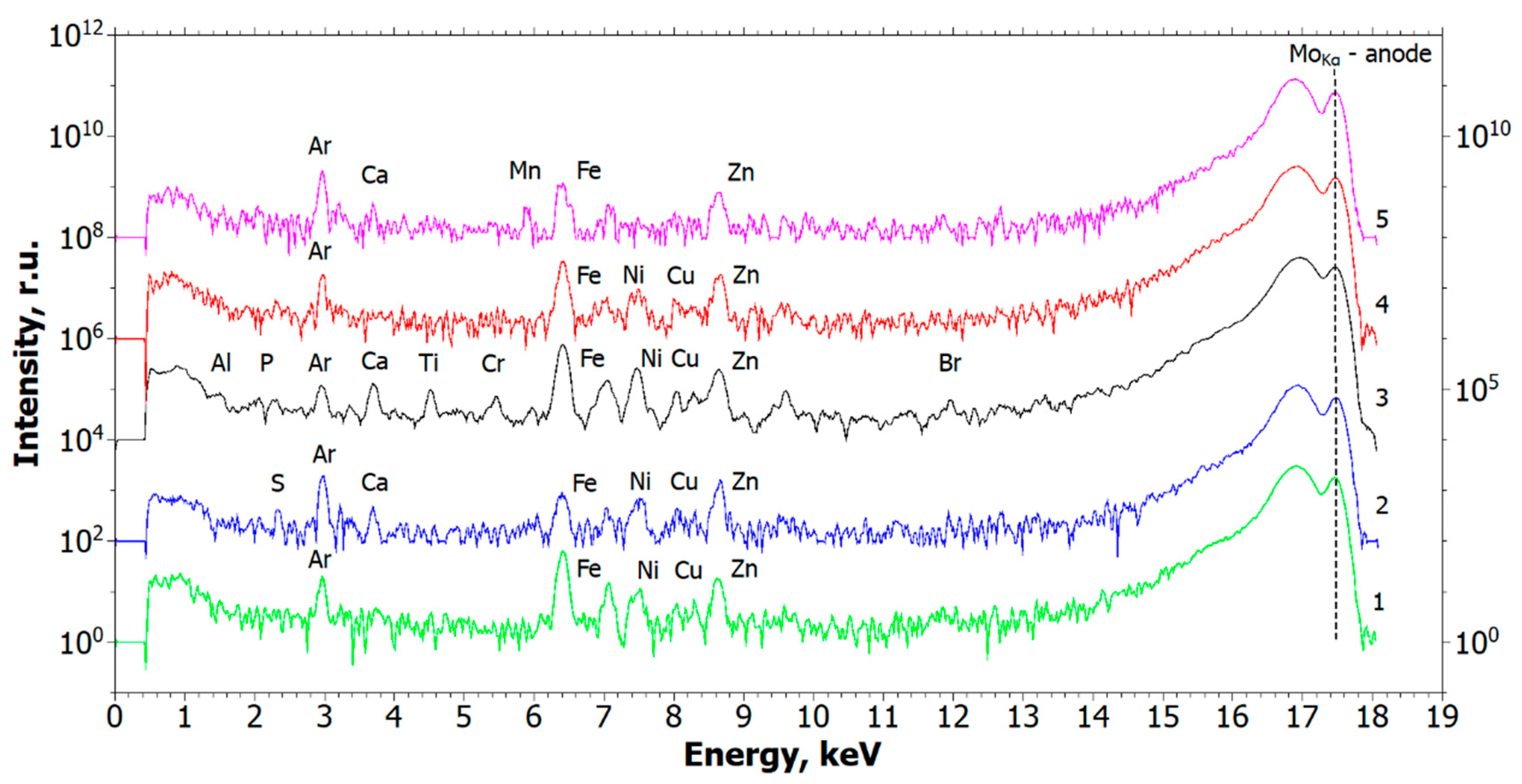
2.1. Results of X-Ray Studies
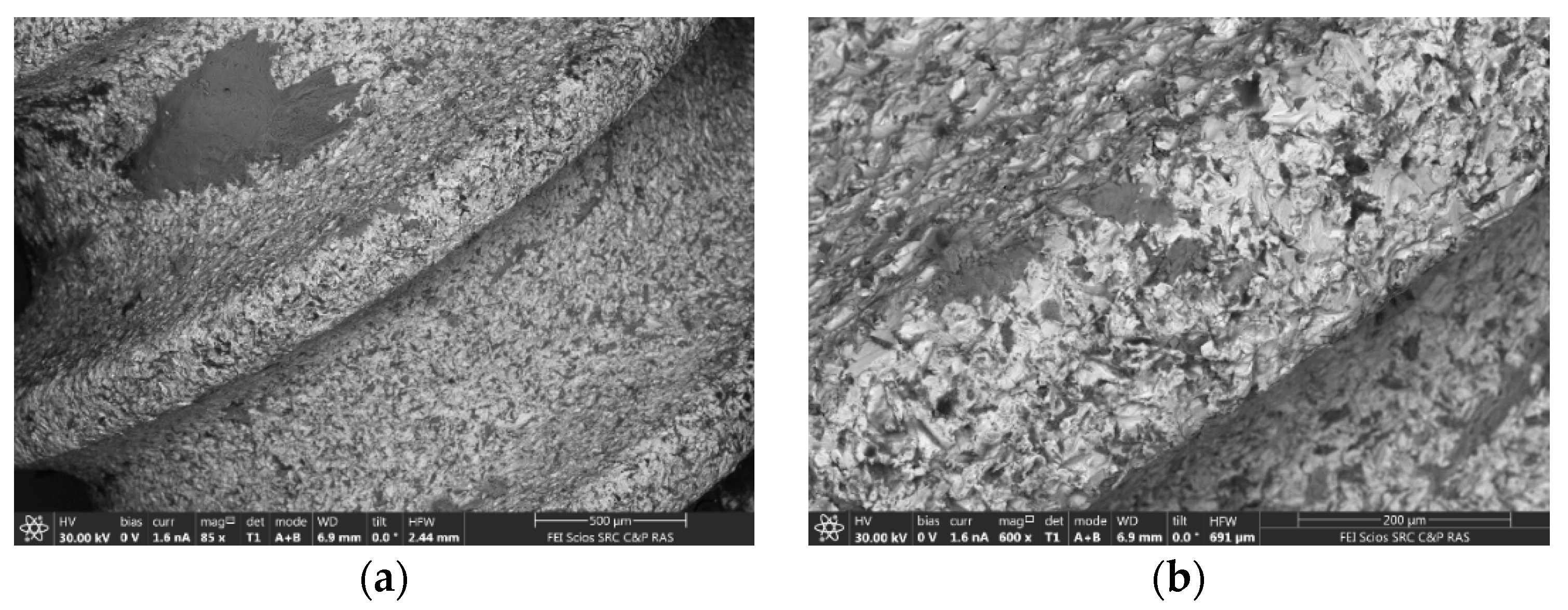
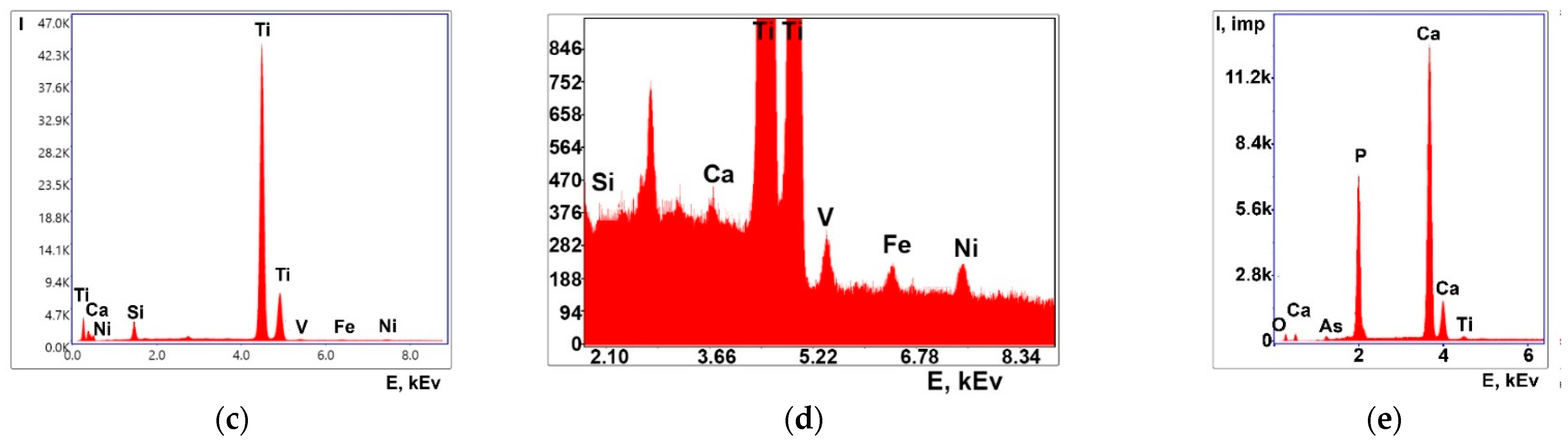
2.2. Results of Electron Microscopic Studies
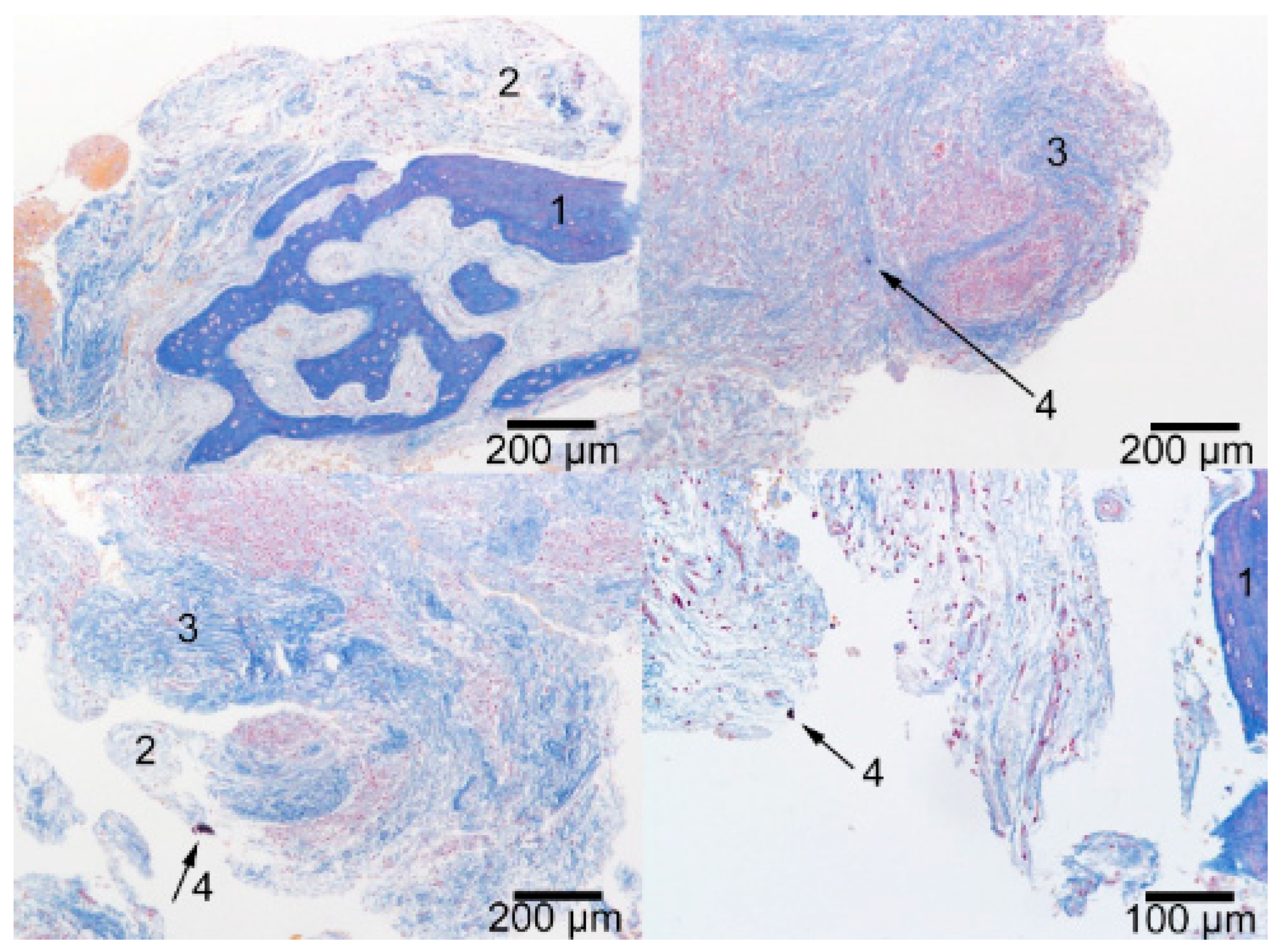
2.3. Results of the Histological Study
2.4. Results of Dynamic Light Scattering (DLS) Studies
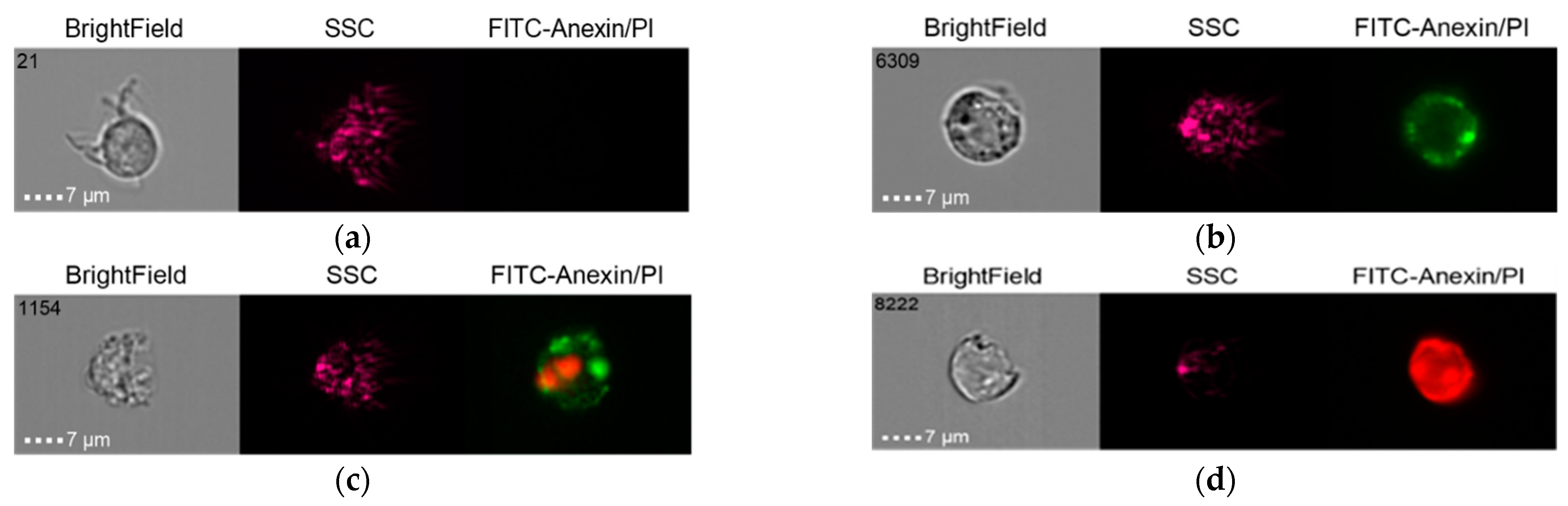
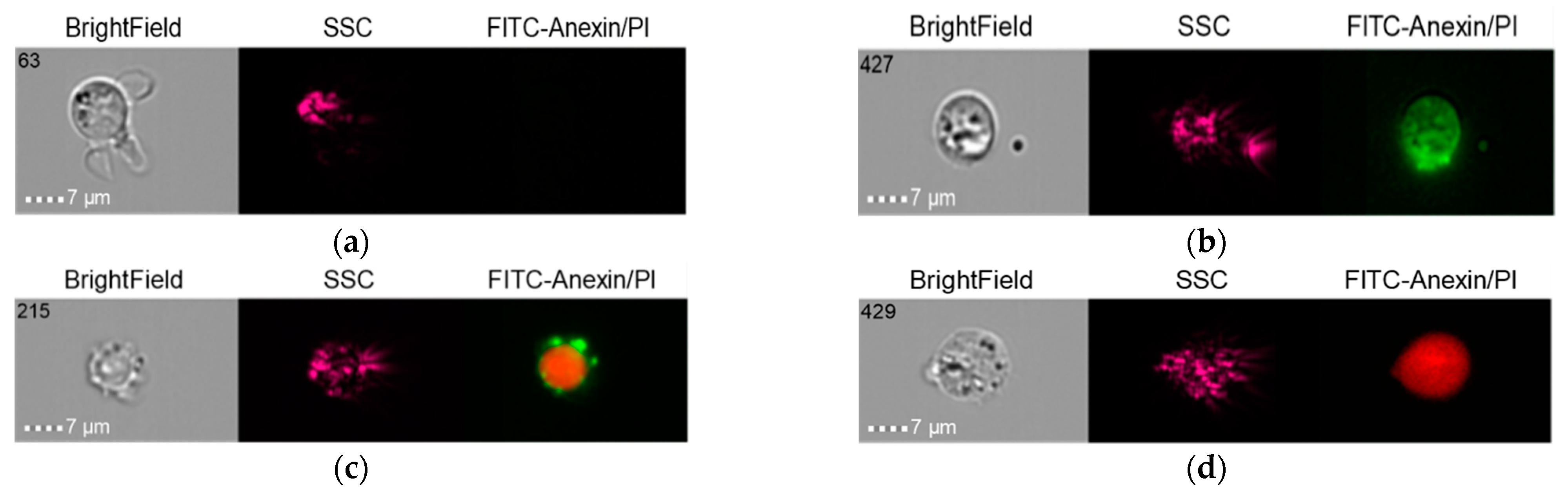
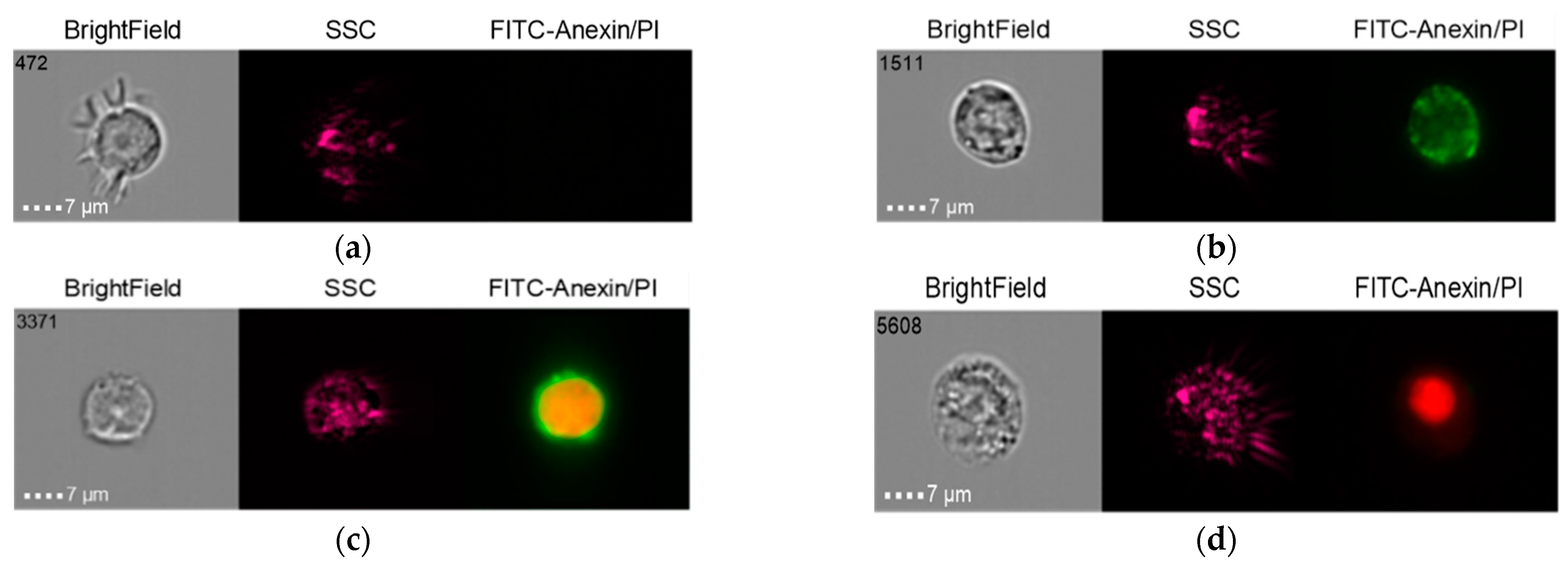
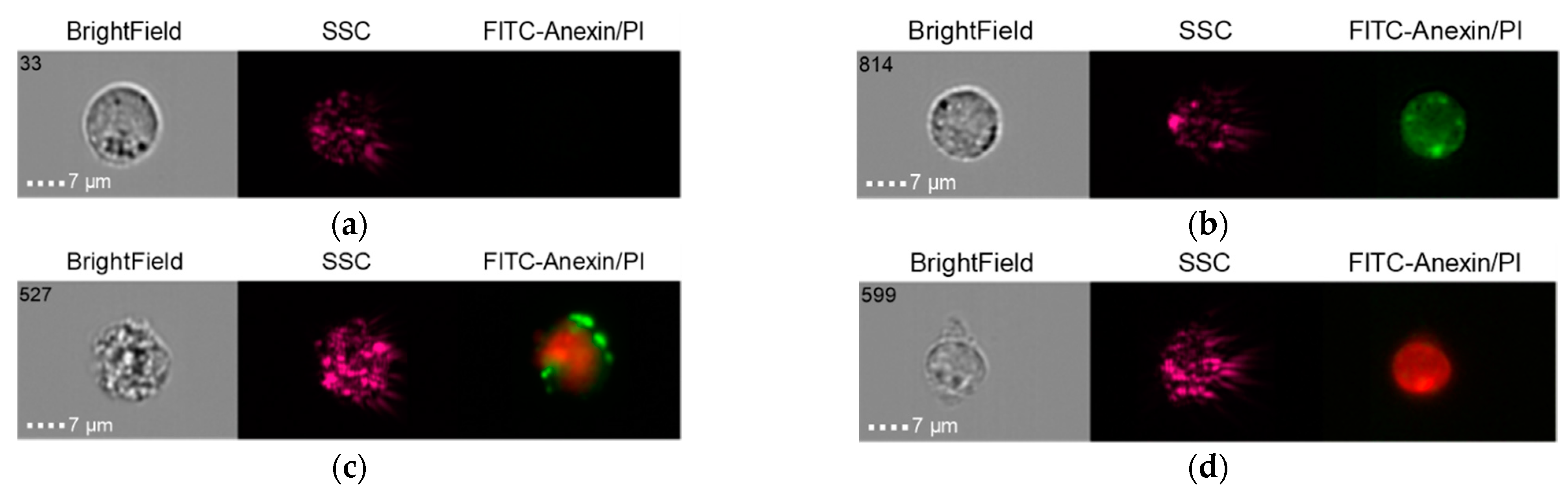
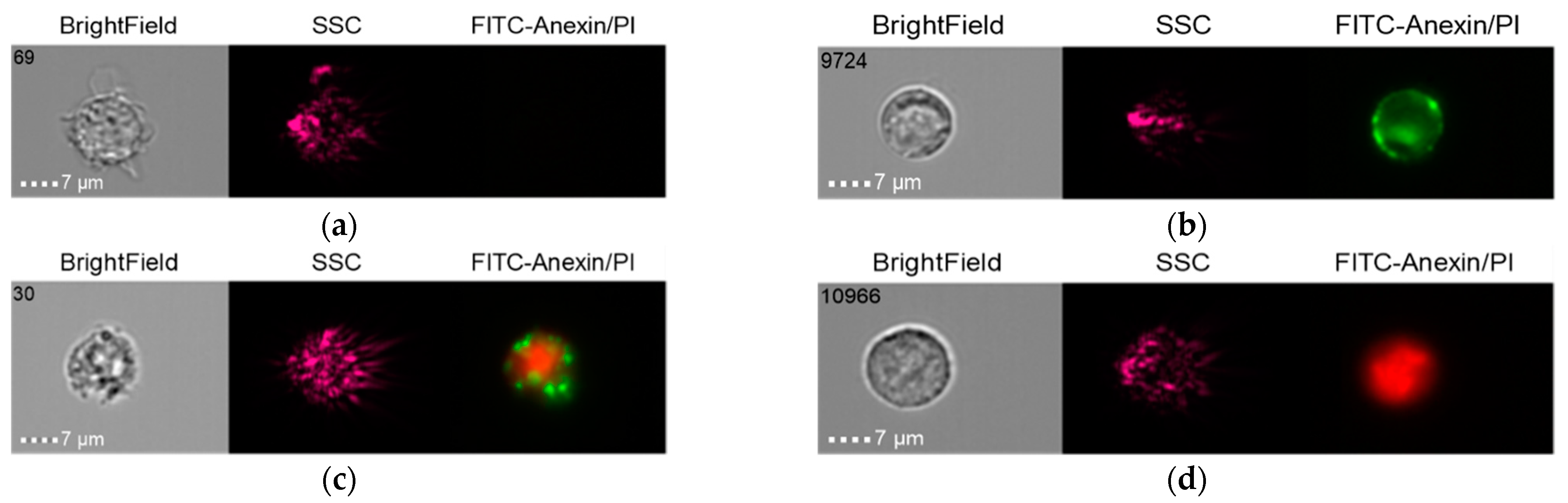
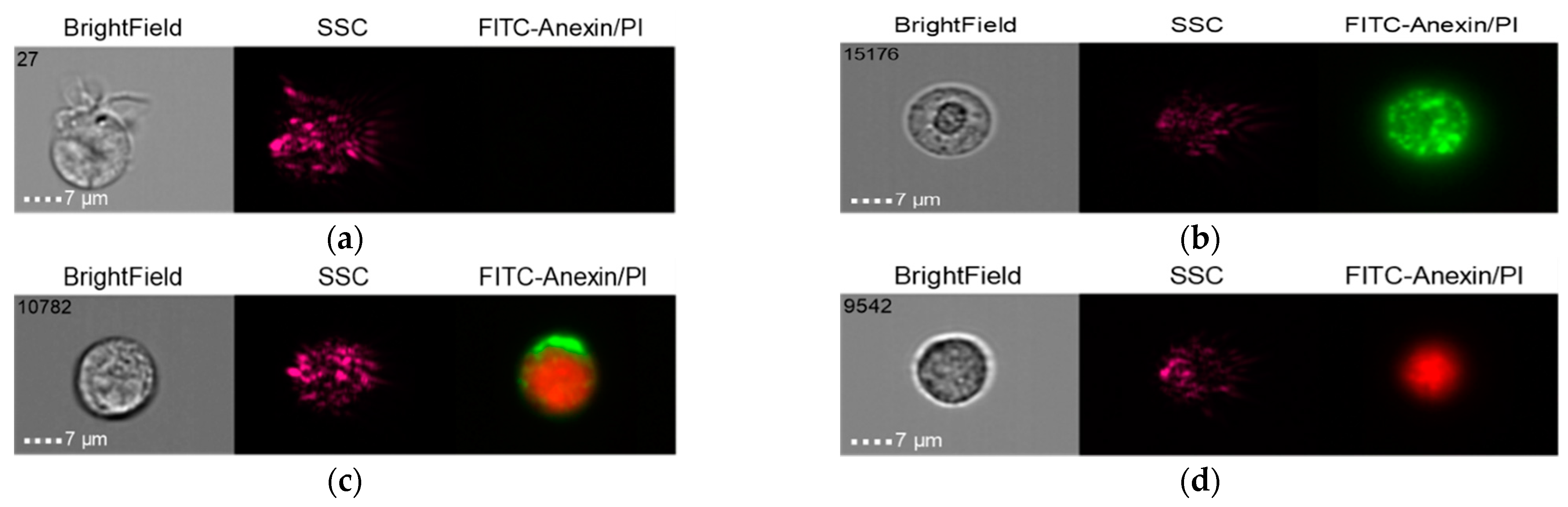
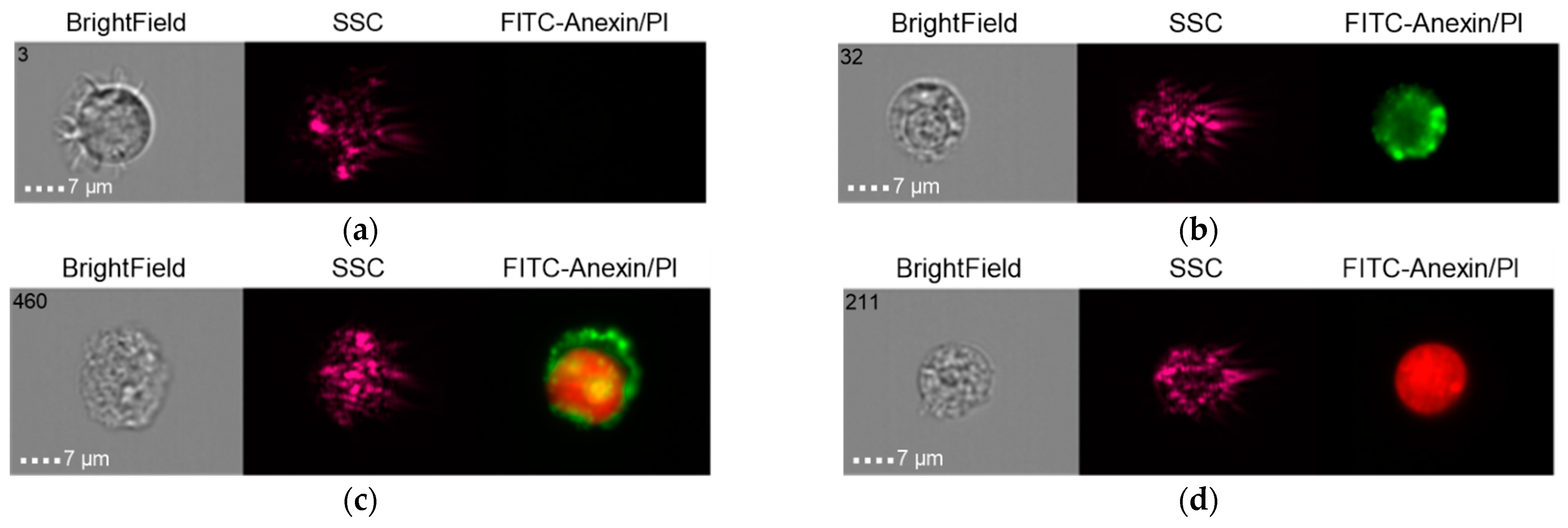
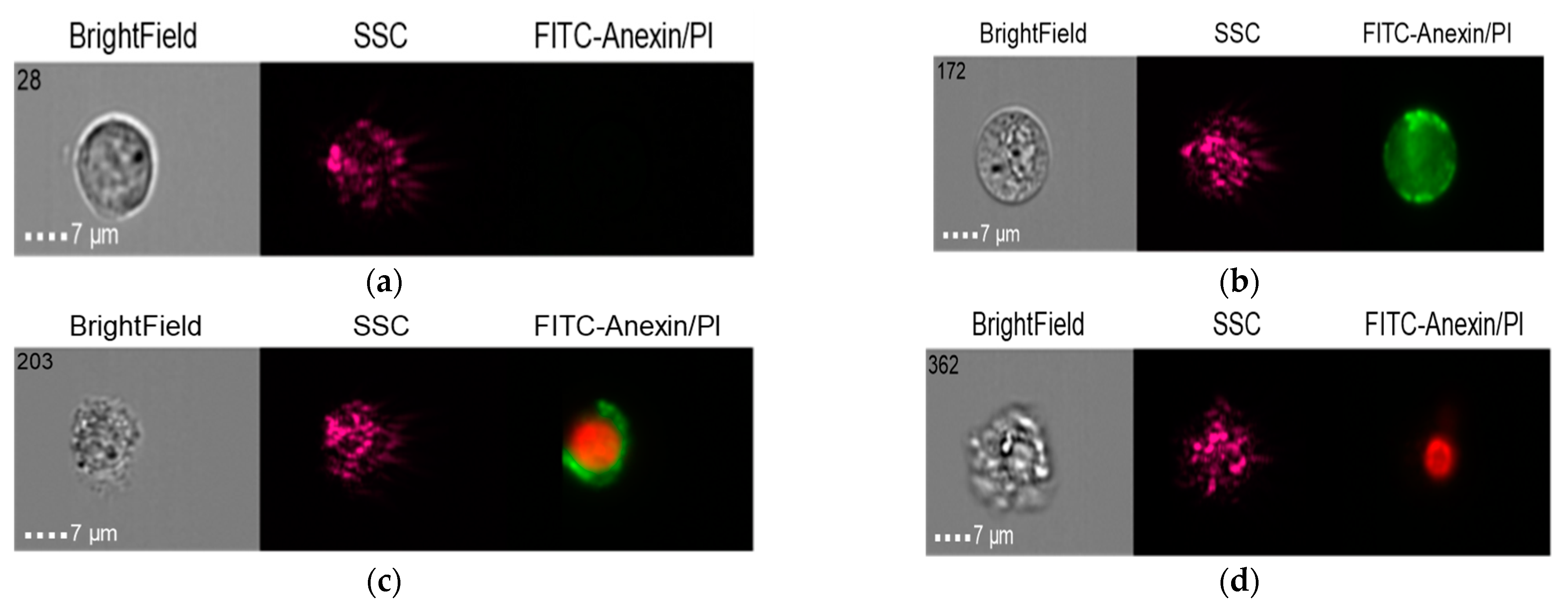
2.5. Results of Visualizing Cytometry Studies
2.5.1. Group 1
2.5.2. Group 2
2.5.3. Group 3 (Control)
3. Discussion
4. Materials and Methods
4.1. Clinical Case
4.2. Surgical Revision
4.3. X-Ray Microtomography (XMCT)
4.4. X-Ray Fluorescence Analysis (XRF)
4.5. Scanning Electron Microscopy (SEM)
4.6. Histological Studies
4.7. Preparation of NSMP Supernatants from the Surfaces of Two Nobel Replace and Alpha Bio Dental Implant Systems
4.8. Dynamic Light Scattering (DLS)
4.9. Co-Cultivation of THP-1 and NSMP Obtained from the Surfaces of Two Nobel Replace and Alpha Bio Dental Implant Systems
4.10. Methodology of Cell Preparation and Staining for the Analysis of Experimental Results by Visualizing Cytometry
4.11. Data Recording and Analysis on an ImageStream Mk II Flow Cytofluorimeter
4.12. Assessment Method for Early and Late Cell Apoptosis Using FITS Annexin V Apoptosis Detection Kit with PI
4.13. Study Groups in the Investigation of the Role of Metallic Nano- and Microparticles in the Development of Immunopathological Inflammation in Tissues
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Becker, S.T.; Dörfer, C.; Graetz, C.; De Buhr, W.; Wiltfang, J.; Podschun, R. A pilot study: Microbiological conditions of the oral cavity in minipigs for peri-implantitis models. Lab. Anim. 2011, 45, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Sahrmann, P.; Gilli, F.; Wiedemeier, D.B.; Attin, T.; Schmidlin, P.R.; Karygianni, L. The Microbiome of Peri-Implantitis: A Systematic Review and Meta-Analysis. Microorganisms 2020, 8, 661. [Google Scholar] [CrossRef] [PubMed]
- De Avila, E.D.; Oirschot, B.A.; Van den Beucken, J.J.J.P. Biomaterial-based possibilities for managing peri-implantitis. J. Periodontal Res. 2020, 55, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Retamal-Valdes, B.; Formiga, M.; Almeida, M.L.; Fritoli, A.; Figueiredo, K.A.; Westphal, M.; Gomes, P.; Feres, M. Does subgingival bacterial colonization differ between implants and teeth? A systematic review. Braz. Oral Res. 2019, 33, e064. [Google Scholar] [CrossRef] [PubMed]
- Skripitz, R.; Aspenberg, P. Tensile bond between bone and titanium: A reappraisal of osseointegration. Acta Orthop. Scand. 1998, 69, 315–319. [Google Scholar] [CrossRef]
- Branemark, P.-I. Osseointegration and its experimental background. J. Prosthet. Dent. 1983, 50, 399–410. [Google Scholar] [CrossRef]
- Sicilia, A.; Cuesta, S.; Coma, G.; Arregui, I.; Guisasola, C.; Ruiz, E.; Maestro, A. Titanium allergy in dental implant patients: A clinical study on 1500 consecutive patients. Clin. Oral Implants Res. 2008, 19, 823–835. [Google Scholar] [CrossRef]
- Medzhitov, R.; Preston-Hurlburt, P.; Janeway, C.A. A human homologue of the Drosophila Toll protein signals activation of adaptive immunity. Nature 1997, 388, 394–397. [Google Scholar] [CrossRef]
- Li, S.; Qiu, J.; Qin, L.; Peng, P.; Li, C.; Mao, J.; Fang, G.; Chen, Z.; Lin, S.; Fu, Y.; et al. NOD2 negatively regulated titanium particle-induced osteolysis in mice. Biomater. Sci. 2019, 7, 2702–2715. [Google Scholar] [CrossRef]
- Bressan, E.; Sbricoli, L.; Guazzo, R.; Tocco, I.; Roman, M.; Vindigni, V.; Stellini, E.; Gardin, C.; Ferroni, L.; Sivolella, S.; et al. Nanostructured Surfaces of Dental Implants. Int. J. Mol. Sci. 2013, 14, 1918–1931. [Google Scholar] [CrossRef]
- Auttachoat, W.; McLoughlin, C.E.; White, K.L.; Smith, M.J. Route-dependent systemic and local immune effects following exposure to solutions prepared from titanium dioxide nanoparticles. J. Immunotoxicol. 2014, 11, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Andersson-Willman, B.; Gehrmann, U.; Cansu, Z.; Buerki-Thurnherr, T.; Krug, H.F.; Gabrielsson, S.; Scheynius, A. Effects of subtoxic concentrations of TiO2 and ZnO nanoparticles on human lymphocytes, dendritic cells and exosome production. Toxicol. Appl. Pharmacol. 2012, 264, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Gopee, N.V.; Howard, P.C.; Yu, L.-R. Proteomic analysis of early response lymph node proteins in mice treated with titanium dioxide nanoparticles. J. Proteom. 2011, 74, 2745–2759. [Google Scholar] [CrossRef] [PubMed]
- Kou, P.M.; Schwartz, Z.; Boyan, B.D.; Babensee, J.E. Dendritic cell responses to surface properties of clinical titanium surfaces. Acta Biomater. 2011, 7, 1354–1363. [Google Scholar] [CrossRef] [PubMed]
- Dutzan, N.; Kajikawa, T.; Abusleme, L.; Greenwell-Wild, T.; Zuazo, C.E.; Ikeuchi, T.; Brenchley, L.; Abe, T.; Hurabielle, C.; Martin, D.; et al. A dysbiotic microbiome triggers T H 17 cells to mediate oral mucosal immunopathology in mice and humans. Sci. Transl. Med. 2018, 10, eaat0797. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, L.; Fan, Y. Adverse Biological Effect of TiO2 and Hydroxyapatite Nanoparticles Used in Bone Repair and Replacement. Int. J. Mol. Sci. 2016, 17, 798. [Google Scholar] [CrossRef] [PubMed]
- Maurer, M.M.; Donohoe, G.C.; Maleki, H.; Yi, J.; McBride, C.; Nurkiewicz, T.R.; Valentine, S.J. Comparative plasma proteomic studies of pulmonary TiO2 nanoparticle exposure in rats using liquid chromatography tandem mass spectrometry. J. Proteom. 2016, 130, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.F.; Hoque, R.; Ouyang, X.; Ghani, A.; Hong, E.; Khan, K.; Moore, L.B.; Ng, G.; Munro, F.; Flavell, R.A.; et al. Inflammasome components Asc and caspase-1 mediate biomaterial-induced inflammation and foreign body response. Proc. Natl. Acad. Sci. USA 2011, 108, 20095–20100. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Raghavan, B.; Müller, V.; Vogl, T.; Fejer, G.; Tchaptchet, S.; Keck, S.; Kalis, C.; Nielsen, P.J.; Galanos, C.; et al. Crucial role for human Toll-like receptor 4 in the development of contact allergy to nickel. Nat. Immunol. 2010, 11, 814–819. [Google Scholar] [CrossRef]
- Brånemark, P.-I.; Breine, U.; Adell, R.; Hansson, B.O.; Lindström, J.; Ohlsson, Å. Intra-Osseous Anchorage of Dental Prostheses: I. Experimental Studies. Scand. J. Plast. Reconstr. Surg. 1969, 3, 81–100. [Google Scholar] [CrossRef]
- Full Products Catalog 2020. Available online: https://alfa-gate.net (accessed on 23 March 2022).
- Labis, V.; Bazikyan, E.; Zhigalina, O.; Sizova, S.; Oleinikov, V.; Khmelenin, D.; Dyachkova, I.; Zolotov, D.; Buzmakov, A.; Asadchikov, V.; et al. Assessment of dental implant surface stability at the nanoscale level. Dent. Mater. 2022, 38, 924–934. [Google Scholar] [CrossRef]
- Zhigalina, O.M.; Khmelenin, D.N.; Labis, V.V.; Bazikyan, E.A.; Sizova, S.V.; Khaidukov, S.V.; Asadchikov, V.E.; Buzmakov, A.V.; Krivonosov, Y.S.; Zolotov, D.A.; et al. Electron Microscopy of the Surface of Dental Implants and Metal-Containing Nanoparticles Obtained in Supernatants. Crystallogr. Rep. 2019, 64, 798–805. [Google Scholar] [CrossRef]
- Labis, V.V.; Bazikyan, E.A.; Sizova, S.V.; Khaydukov, S.V.; Kozlov, I.G. Nanosized Particles Obtained in Supernatanes from Dental Implants of Systems A and B.; Bulletin of Orenburg Scientific Center, Ural Branch of Russian Academy of Sciences: Orenburg, Russia, 2016; Volume 2, pp. 1–16. [Google Scholar]
- Labis, V.V.; Bazikyan, E.A.; Kozlov, I.G.; Sizova, S.V.; Hajdukov, S.V. Nanosized Particles—Participants of Osseointrgration; Bulletin of Orenburg Scientific Center, Ural Branch of Russian Academy of Sciences: Orenburg, Russia, 2016; Volume 1, pp. 1–18. [Google Scholar]
- Labis, V.; Bazikyan, E.; Sizova, S.; Oleinikov, V.; Trulioff, A.; Serebriakova, M.; Kudryavtsev, I.; Zhigalina, O.; Khmelenin, D.; Dyachkova, I.; et al. Immunopathological Inflammation in the Evolution of Mucositis and Peri-Implantitis. Int. J. Mol. Sci. 2022, 23, 15797. [Google Scholar] [CrossRef] [PubMed]
- Buzmakov, A.V.; Asadchikov, V.E.; Zolotov, D.A.; Roshchin, B.S.; Dymshits, Y.M.; Shishkov, V.A.; Chukalina, M.V.; Ingacheva, A.S.; Ichalova, D.E.; Krivonosov, Y.S.; et al. Laboratory Microtomographs: Design and Data Processing Algorithms. Crystallogr. Rep. 2018, 63, 1057–1061. [Google Scholar] [CrossRef]
- Ingacheva, A.S.; Chukalina, M.V. Polychromatic CT Data Improvement with One-Parameter Power Correction. Math. Probl. Eng. 2019, 7, 1405365. [Google Scholar] [CrossRef]
- Bazikyan, E.A.; Labis, V.V.; Kozlov, I.G.; Khaydukov, S.V.; Labis, Y.V. Patent for Invention. RU 2611013 C, 17 February 2017. Available online: https://patentdb.ru/patent/2611013 (accessed on 6 September 2022).
- Murphy, R.M. Static and dynamic light scattering of biological macromolecules: What can we learn? Curr. Opin. Biotechnol. 1997, 8, 25–30. [Google Scholar] [CrossRef]
- Ranganathan, P.; Jayakumar, C.; Navankasattusas, S.; Li, D.Y.; Kim, I.; Ramesh, G. UNC5B Receptor Deletion Exacerbates Tissue Injury in Response to AKI. J. Am. Soc. Nephrol. 2014, 25, 239–249. [Google Scholar] [CrossRef]
- Yu, J.; Zheng, J.; Zhao, X.; Liu, J.; Mao, Z.; Ling, Y.; Chen, D.; Chen, C.; Hui, L.; Cui, L.; et al. Aminoglycoside Stress Together with the 12S rRNA 1494C>T Mutation Leads to Mitophagy. PLoS ONE 2014, 9, e114650. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, J.; Yang, W.; Bi, Y.; Chi, J.; Tian, J.; Li, W. High-dose alcohol induces reactive oxygen species-mediated apoptosis via PKC-β/p66Shc in mouse primary cardiomyocytes. Biochem. Biophys. Res. Commun. 2015, 456, 656–661. [Google Scholar] [CrossRef]
- Jaishy, B.; Zhang, Q.; Chung, H.S.; Riehle, C.; Soto, J.; Jenkins, S.; Abel, P.; Cowart, L.A.; Van Eyk, J.E.; Abel, E.D. Lipid-induced NOX2 activation inhibits autophagic flux by impairing lysosomal enzyme activity. J. Lipid Res. 2015, 56, 546–561. [Google Scholar] [CrossRef]
- Labis, V.V.; Bazikyan, E.A.; Volkov, A.V.; Sizova, S.V.; Khaydukov, S.V.; Asadchikov, V.E.; Buzmakov, A.V.; Kozlov, I.G. Role of Immune Mechanisms in Oral Microflora in the Pathogenesis of Periimplantitis; Bulletin of Orenburg Scientific Center, Ural Branch of Russian Academy of Sciences: Orenburg, Russia, 2019; Volume 3, pp. 1–15. [Google Scholar]
- Abbasi-Oshaghi, E.; Mirzaei, F.; Pourjafar, M. NLRP3 inflammasome, oxidative stress, and apoptosis induced in the intestine and liver of rats treated with titanium dioxide nanoparticles: In vivo and in vitro study. Int. J. Nanomed. 2019, 14, 1919–1936. [Google Scholar] [CrossRef] [PubMed]






| Element | Weight % | Atomic % |
|---|---|---|
| NaK | 3.49 | 6.65 |
| AlK | 7.09 | 11.51 |
| SiK | 0.56 | 0.87 |
| CaK | 0.04 | 0.05 |
| TiK | 83.97 | 76.81 |
| VK | 4.26 | 3.66 |
| FeK | 0.23 | 0.18 |
| NiK | 0.36 | 0.27 |
| Element | Weight % | Atomic % |
|---|---|---|
| OK | 13.38 | 26.41 |
| AsL | 0.14 | 0.06 |
| PK | 23.83 | 24.30 |
| CaK | 61.72 | 48.62 |
| TiK | 0.93 | 0.61 |
| Element | Weight % | Atomic % |
|---|---|---|
| CK | 27.96 | 54.24 |
| NK | 6.42 | 10.68 |
| OK | 8.28 | 12.05 |
| MgK | 1.11 | 1.06 |
| WM | 4.65 | 0.59 |
| SK | 0.34 | 0.25 |
| CrK | 16.55 | 7.41 |
| CoK | 34.70 | 13.72 |
| Element | Weight % | Atomic % |
|---|---|---|
| SK | 33.98 | 48.92 |
| CaK | 0.17 | 0.20 |
| CrK | 12.79 | 11.36 |
| CoK | 49.22 | 38.56 |
| WL | 3.84 | 0.97 |
| Sample | D, nm | ACR, kcps | PD, % |
|---|---|---|---|
| Nobel Replace 0.1_100 | 88.16 | 36.6 | 0.324 |
| Nobel Replace 0.25_100 | 72.4 | 88.6 | 0.445 |
| Nobel Replace 1_100 | 74.92 | 228.2 | 0.273 |
| Alpha-Bio 0.1_100 | 47.57 | 34.4 | 0.434 |
| Alpha-Bio 0.25_100 | 27.89 | 38.8 | 0.339 |
| Alpha-Bio 1_100 | 13.74 | 148.3 | 0.328 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Labis, V.; Bazikyan, E.; Demin, D.; Dyachkova, I.; Zolotov, D.; Volkov, A.; Asadchikov, V.; Zhigalina, O.; Khmelenin, D.; Kuptsova, D.; et al. Cell-Molecular Interactions of Nano- and Microparticles in Dental Implantology. Int. J. Mol. Sci. 2023, 24, 2267. https://doi.org/10.3390/ijms24032267
Labis V, Bazikyan E, Demin D, Dyachkova I, Zolotov D, Volkov A, Asadchikov V, Zhigalina O, Khmelenin D, Kuptsova D, et al. Cell-Molecular Interactions of Nano- and Microparticles in Dental Implantology. International Journal of Molecular Sciences. 2023; 24(3):2267. https://doi.org/10.3390/ijms24032267
Chicago/Turabian StyleLabis, Varvara, Ernest Bazikyan, Denis Demin, Irina Dyachkova, Denis Zolotov, Alexey Volkov, Victor Asadchikov, Olga Zhigalina, Dmitry Khmelenin, Daria Kuptsova, and et al. 2023. "Cell-Molecular Interactions of Nano- and Microparticles in Dental Implantology" International Journal of Molecular Sciences 24, no. 3: 2267. https://doi.org/10.3390/ijms24032267
APA StyleLabis, V., Bazikyan, E., Demin, D., Dyachkova, I., Zolotov, D., Volkov, A., Asadchikov, V., Zhigalina, O., Khmelenin, D., Kuptsova, D., Petrichuk, S., Semikina, E., Sizova, S., Oleinikov, V., Khaidukov, S., & Kozlov, I. (2023). Cell-Molecular Interactions of Nano- and Microparticles in Dental Implantology. International Journal of Molecular Sciences, 24(3), 2267. https://doi.org/10.3390/ijms24032267





