Research Progress on Natural Small-Molecule Compounds for the Prevention and Treatment of Sepsis
Abstract
1. Introduction
2. Polyphenol Compounds
3. Anthraquinone Compounds
4. Glucoside Compounds
5. Sterol Compounds
6. Flavonoid Compounds
7. Biogenic Amines
8. Alkaloid Compounds
9. Amide Compounds
10. Discussion and Prospects
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Venet, F.; Monneret, G. Advances in the Understanding and Treatment of Sepsis-Induced Immunosuppression. Nat. Rev. Nephrol. 2018, 14, 121–137. [Google Scholar] [CrossRef] [PubMed]
- Jarczak, D.; Nierhaus, A. Cytokine Storm—Definition, Causes, and Implications. Int. J. Mol. Sci. 2022, 23, 11740. [Google Scholar] [CrossRef] [PubMed]
- Peerapornratana, S.; Manrique-Caballero, C.L.; Gómez, H.; Kellum, J.A. Acute Kidney Injury From Sepsis: Current Concepts, Epidemiology, Pathophysiology, Prevention and Treatment. Kidney Int. 2019, 96, 1083–1099. [Google Scholar] [CrossRef] [PubMed]
- Matthay, M.A.; Zemans, R.L.; Zimmerman, G.A.; Arabi, Y.M.; Beitler, J.R.; Mercat, A.; Herridge, M.; Randolph, A.G.; Calfee, C.S. Acute Respiratory Distress Syndrome. Nat. Rev. Dis. Primers 2019, 5, 18. [Google Scholar] [CrossRef]
- Woźnica, E.A.; Inglot, M.; Woźnica, R.K.; Łysenko, L. Liver Dysfunction in Sepsis. Adv. Clin. Exp. Med. 2018, 27, 547–551. [Google Scholar] [CrossRef]
- L’Heureux, M.; Sternberg, M.; Brath, L.; Turlington, J.; Kashiouris, M.G. Sepsis-Induced Cardiomyopathy: A Comprehensive Review. Curr. Cardiol. Rep. 2020, 22, 35. [Google Scholar] [CrossRef]
- Thomas, H. Sepsis: Bile Acids Promote Inflammation in Cholestasis-Associated Sepsis. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 324–325. [Google Scholar] [CrossRef]
- Ma, Y.; Zhou, Y.; Wu, F.; Ji, W.; Zhang, J.; Wang, X. The Bidirectional Interactions Between Inflammation and Coagulation in Fracture Hematoma. Tissue Eng. Part B Rev. 2019, 25, 46–54. [Google Scholar] [CrossRef]
- Huang, M.; Cai, S.; Su, J. The Pathogenesis of Sepsis and Potential Therapeutic Targets. Int. J. Mol. Sci. 2019, 20, 5376. [Google Scholar] [CrossRef]
- Wang, P.; Feng, Z.; Sang, X.; Chen, W.; Zhang, X.; Xiao, J.; Chen, Y.; Chen, Q.; Yang, M.; Su, J. Kombucha Ameliorates LPS-Induced Sepsis in a Mouse Model. Food Funct. 2021, 12, 10263–10280. [Google Scholar] [CrossRef] [PubMed]
- de Pádua Lúcio, K.; Rabelo, A.C.S.; Araújo, C.M.; Brandão, G.C.; de Souza, G.H.B.; da Silva, R.G.; de Souza, D.M.S.; Talvani, A.; Bezerra, F.S.; Cruz Calsavara, A.J.; et al. Anti-Inflammatory and Antioxidant Properties of Black Mulberry (Morus nigra L.) in a Model of LPS-Induced Sepsis. Oxid. Med. Cell. Longev. 2018, 2018, 5048031. [Google Scholar] [CrossRef] [PubMed]
- Su, J.; Guo, K.; Huang, M.; Liu, Y.; Zhang, J.; Sun, L.; Li, D.; Pang, K.L.; Wang, G.; Chen, L.; et al. Fucoxanthin, a Marine Xanthophyll Isolated From Conticribra weissflogii ND-8: Preventive Anti-Inflammatory Effect in a Mouse Model of Sepsis. Front. Pharmacol. 2019, 10, 906. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Dou, H.; Gong, W.; Liu, X.; Yu, Z.; Li, E.; Tan, R.; Hou, Y. Bis-N-norgliovictin, a Small-Molecule Compound From Marine Fungus, Inhibits LPS-Induced Inflammation in Macrophages and Improves Survival in Sepsis. Eur. J. Pharmacol. 2013, 705, 49–60. [Google Scholar] [CrossRef]
- Rasmi, R.R.; Sakthivel, K.M.; Guruvayoorappan, C. NF-κB Inhibitors in Treatment and Prevention of Lung Cancer. Biomed. Pharmacother. 2020, 130, 110569. [Google Scholar] [CrossRef]
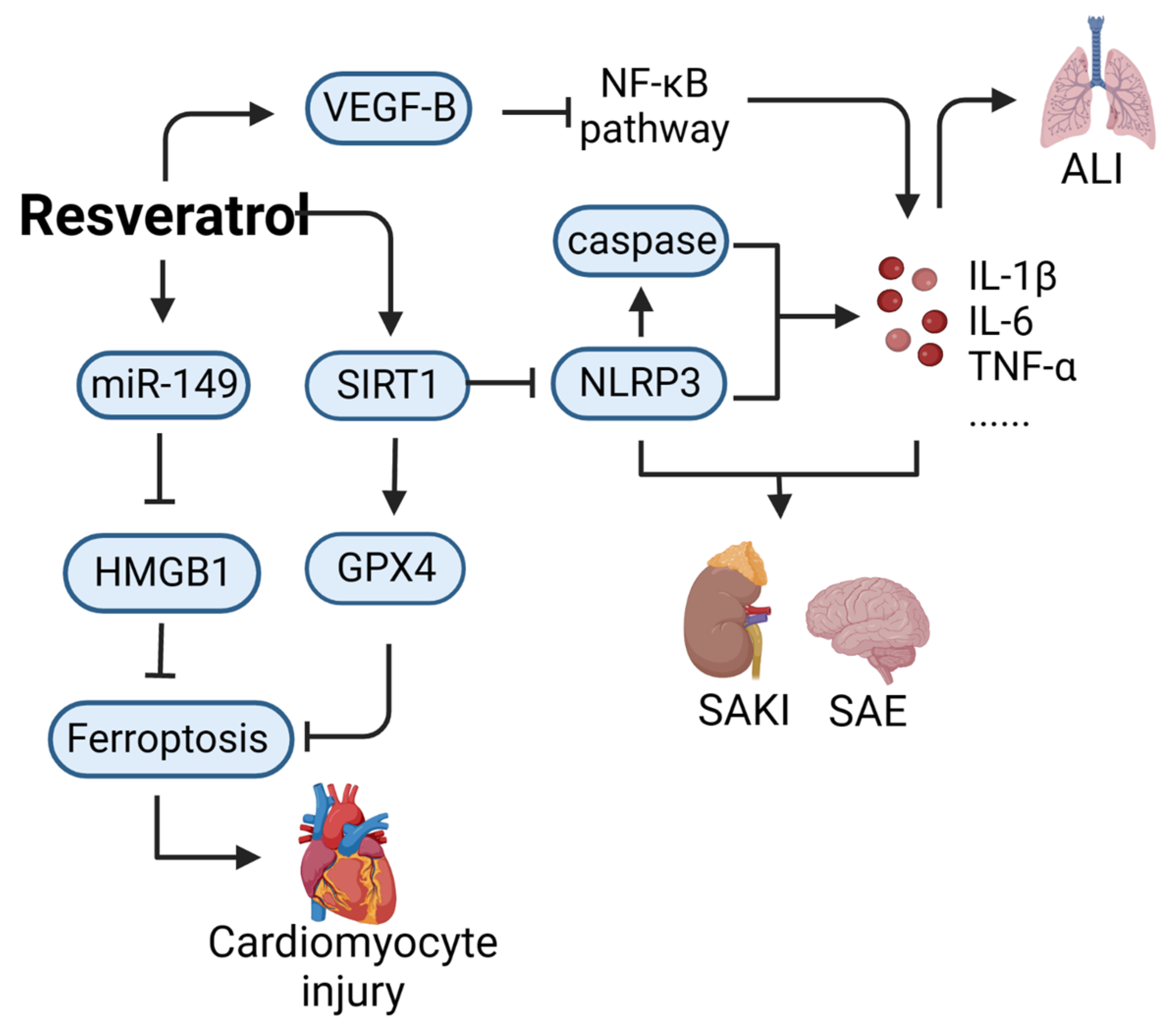
- Li, J.; Zeng, X.; Yang, F.; Wang, L.; Luo, X.; Liu, R.; Zeng, F.; Lu, S.; Huang, X.; Lei, Y.; et al. Resveratrol: Potential Application in Sepsis. Front. Pharmacol. 2022, 13, 821358. [Google Scholar] [CrossRef]
- Imperatore, F.; Maurizio, J.; Vargas Aguilar, S.; Busch, C.J.; Favret, J.; Kowenz-Leutz, E.; Cathou, W.; Gentek, R.; Perrin, P.; Leutz, A.; et al. SIRT1 Regulates Macrophage Self-Renewal. EMBO J. 2017, 36, 2353–2372. [Google Scholar] [CrossRef]
- Deng, Z.; Sun, M.; Wu, J.; Fang, H.; Cai, S.; An, S.; Huang, Q.; Chen, Z.; Wu, C.; Zhou, Z.; et al. SIRT1 Attenuates Sepsis-Induced Acute Kidney Injury via Beclin1 Deacetylation-Mediated Autophagy Activation. Cell Death Dis. 2021, 12, 217. [Google Scholar] [CrossRef]
- Wang, X.; Simayi, A.; Fu, J.; Zhao, X.; Xu, G. Resveratrol Mediates the miR-149/HMGB1 Axis and Regulates the Ferroptosis Pathway to Protect Myocardium in Endotoxemia Mice. Am. J. Physiol. Endocrinol. Metab. 2022, 323, E21–E32. [Google Scholar] [CrossRef]
- Sui, D.M.; Xie, Q.; Yi, W.J.; Gupta, S.; Yu, X.Y.; Li, J.B.; Wang, J.; Wang, J.F.; Deng, X.M. Resveratrol Protects Against Sepsis-Associated Encephalopathy and Inhibits the NLRP3/IL-1β Axis in Microglia. Mediators Inflamm. 2016, 2016, 1045657. [Google Scholar] [CrossRef]
- Yang, L.; Zhang, Z.; Zhuo, Y.; Cui, L.; Li, C.; Li, D.; Zhang, S.; Cui, N.; Wang, X.; Gao, H. Resveratrol Alleviates Sepsis-Induced Acute Lung Injury by Suppressing Inflammation and Apoptosis of Alveolar Macrophage Cells. Am. J. Transl. Res. 2018, 10, 1961–1975. [Google Scholar]
- Posadino, A.M.; Cossu, A.; Giordo, R.; Zinellu, A.; Sotgia, S.; Vardeu, A.; Hoa, P.T.; Nguyen, L.H.V.; Carru, C.; Pintus, G. Resveratrol Alters Human Endothelial Cells Redox State and Causes Mitochondrial-Dependent Cell Death. Food Chem. Toxicol. 2015, 78, 10–16. [Google Scholar] [CrossRef]
- Noureddin, S.A.; El-Shishtawy, R.M.; Al-Footy, K.O. Curcumin Analogues and Their Hybrid Molecules as Multifunctional Drugs. Eur. J. Med. Chem. 2019, 182, 111631. [Google Scholar] [CrossRef] [PubMed]
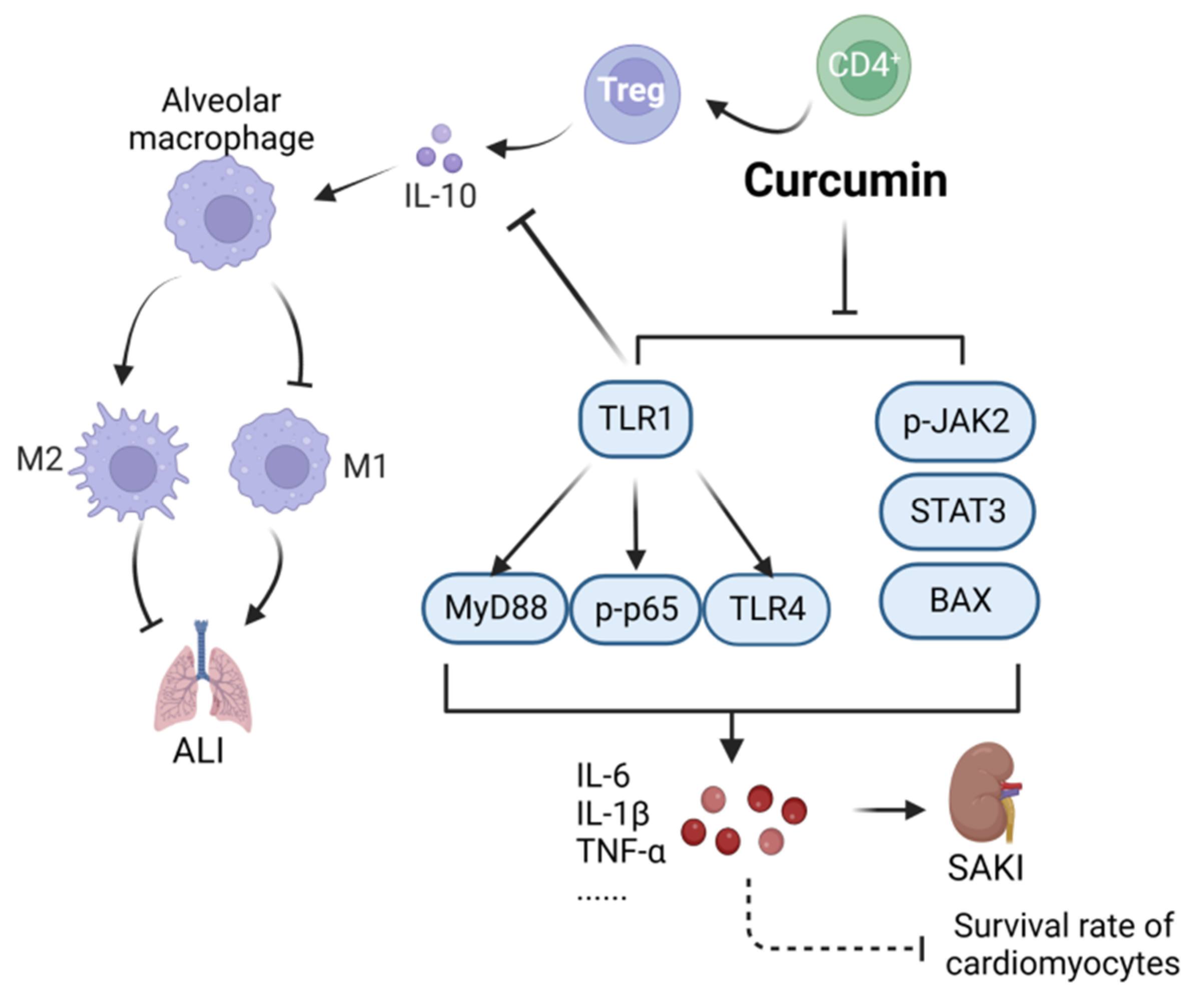
- Chai, Y.S.; Chen, Y.Q.; Lin, S.H.; Xie, K.; Wang, C.J.; Yang, Y.Z.; Xu, F. Curcumin Regulates the Differentiation of Naïve CD4+ T Cells and Activates IL-10 Immune Modulation Against Acute Lung Injury in Mice. Biomed. Pharmacother. 2020, 125, 109946. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Wang, H.; Cai, X. Curcumin Interferes With Sepsis-Induced Cardiomyocyte Apoptosis via TLR1 Inhibition. Rev. Port. Cardiol. 2023, 42, 209–221. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Wang, X.; Wang, X.; Liu, B.; Yuan, Y.; Zuo, X. Curcumin Attenuates Inflammation and Cell Apoptosis Through Regulating NF-κB and JAK2/STAT3 Signaling Pathway Against Acute Kidney Injury. Cell Cycle 2020, 19, 1941–1951. [Google Scholar] [CrossRef]
- Cárdenas Garza, G.R.; Elizondo Luévano, J.H.; Bazaldúa Rodríguez, A.F.; Chávez Montes, A.; Pérez Hernández, R.A.; Martínez Delgado, A.J.; López Villarreal, S.M.; Rodríguez Rodríguez, J.; Sánchez Casas, R.M.; Castillo Velázquez, U.; et al. Benefits of Cardamom (Elettaria cardamomum (L.) Maton) and Turmeric (Curcuma longa L.) Extracts for Their Applications as Natural Anti-Inflammatory Adjuvants. Plants 2021, 10, 1908. [Google Scholar] [CrossRef]
- Chen, M.; Chang, Y.Y.; Huang, S.; Xiao, L.H.; Zhou, W.; Zhang, L.Y.; Li, C.; Zhou, R.P.; Tang, J.; Lin, L.; et al. Aromatic-Turmerone Attenuates LPS-Induced Neuroinflammation and Consequent Memory Impairment by Targeting TLR4-Dependent Signaling Pathway. Mol. Nutr. Food Res. 2018, 62, 10. [Google Scholar] [CrossRef]
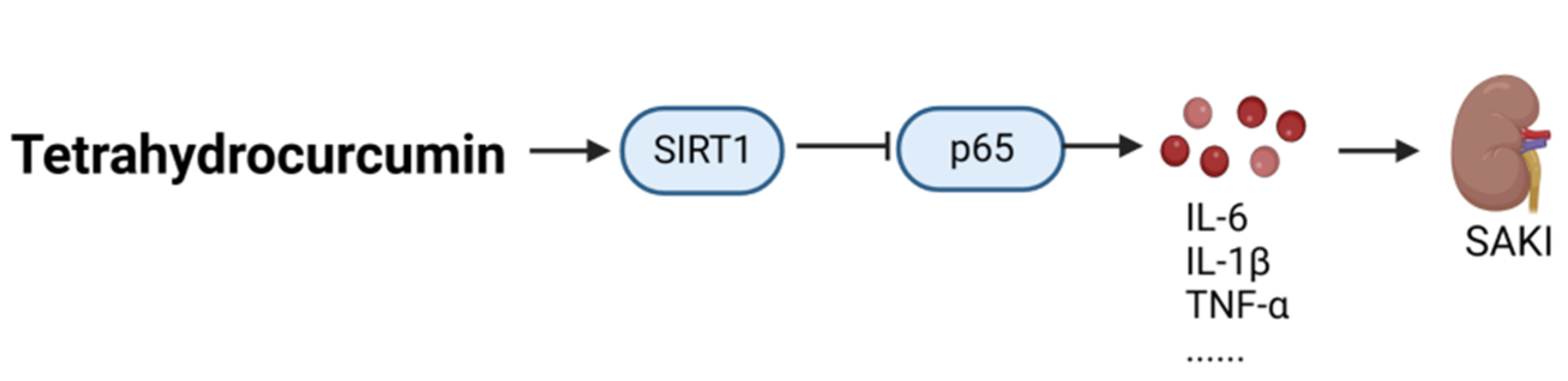
- Li, L.; Liu, X.; Li, S.; Wang, Q.; Wang, H.; Xu, M.; An, Y. Tetrahydrocurcumin Protects Against Sepsis-Induced Acute Kidney Injury via the SIRT1 Pathway. Ren. Fail. 2021, 43, 1028–1040. [Google Scholar] [CrossRef]
- Li, Y.; Jiang, J.G. Health Functions and Structure-Activity Relationships of Natural Anthraquinones from Plants. Food Funct. 2018, 9, 6063–6080. [Google Scholar] [CrossRef]
- Dong, X.; Zeng, Y.; Liu, Y.; You, L.; Yin, X.; Fu, J.; Ni, J. Aloe-Emodin: A Review of Its Pharmacology, Toxicity, and Pharmacokinetics. Phytother. Res. 2020, 34, 270–281. [Google Scholar] [CrossRef] [PubMed]
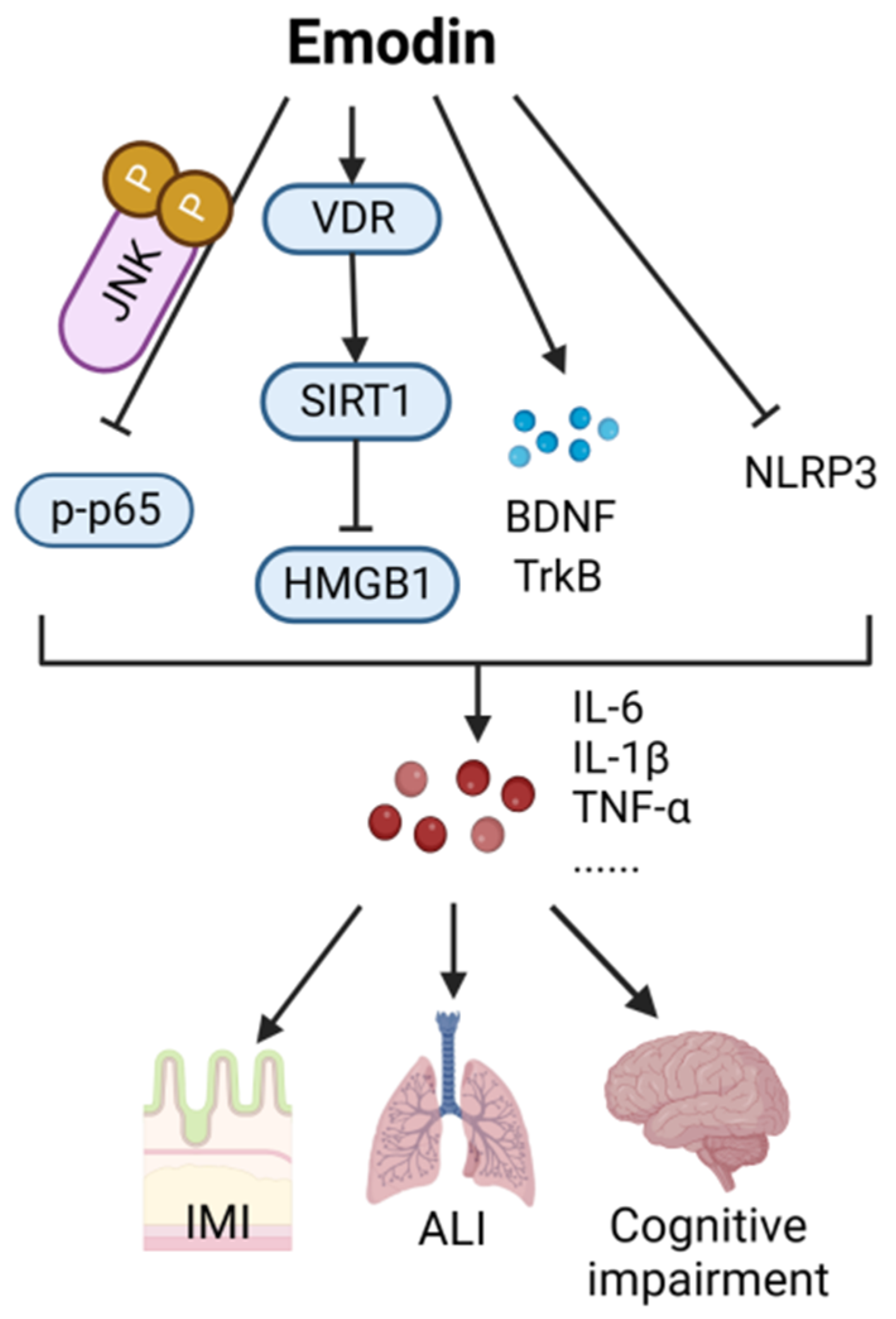
- Liu, F.J.; Gu, T.J.; Wei, D.Y. Emodin Alleviates Sepsis-Mediated Lung Injury via Inhibition and Reduction of NF-kB and HMGB1 Pathways Mediated by SIRT1. Kaohsiung J. Med. Sci. 2022, 38, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Yao, B.; He, J.; Yin, X.; Shi, Y.; Wan, J.; Tian, Z. The Protective Effect of Lithocholic Acid on the Intestinal Epithelial Barrier Is Mediated by the Vitamin D Receptor via a SIRT1/Nrf2 and NF-κB Dependent Mechanism in Caco-2 Cells. Toxicol. Lett. 2019, 316, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Shang, L.; Liu, Y.; Li, J.; Pan, G.; Zhou, F.; Yang, S. Emodin Protects Sepsis Associated Damage to the Intestinal Mucosal Barrier Through the VDR/Nrf2/HO-1 Pathway. Front. Pharmacol. 2021, 12, 724511. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Lian, B.; Zhang, R.; Guo, Y.; Zhao, J.; He, S.; Bai, Y.; Wang, N.; Lin, Y.; Wang, X.; et al. Emodin Ameliorates Intestinal Dysfunction by Maintaining Intestinal Barrier Integrity and Modulating the Microbiota in Septic Mice. Mediat. Inflamm. 2022, 2022, 5026103. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.L.; Wang, Z.H.; Mu, Y.H.; Liu, Z.L.; Pang, L. Emodin Promotes Autophagy and Prevents Apoptosis in Sepsis-Associated Encephalopathy Through Activating BDNF/TrkB Signaling. Pathobiology 2022, 89, 135–145. [Google Scholar] [CrossRef]
- Xiao, J.; Chen, S.; Chen, Y.; Su, J. The Potential Health Benefits of Aloin From Genus Aloe. Phytother. Res. 2022, 36, 873–890. [Google Scholar] [CrossRef]
- Zhou, Y.; Wang, J.; Yang, W.; Qi, X.; Lan, L.; Luo, L.; Yin, Z. Bergapten Prevents Lipopolysaccharide-Induced Inflammation in RAW264.7 Cells Through Suppressing JAK/STAT Activation and ROS Production and Increases the Survival Rate of Mice After LPS Challenge. Int. Immunopharmacol. 2017, 48, 159–168. [Google Scholar] [CrossRef]
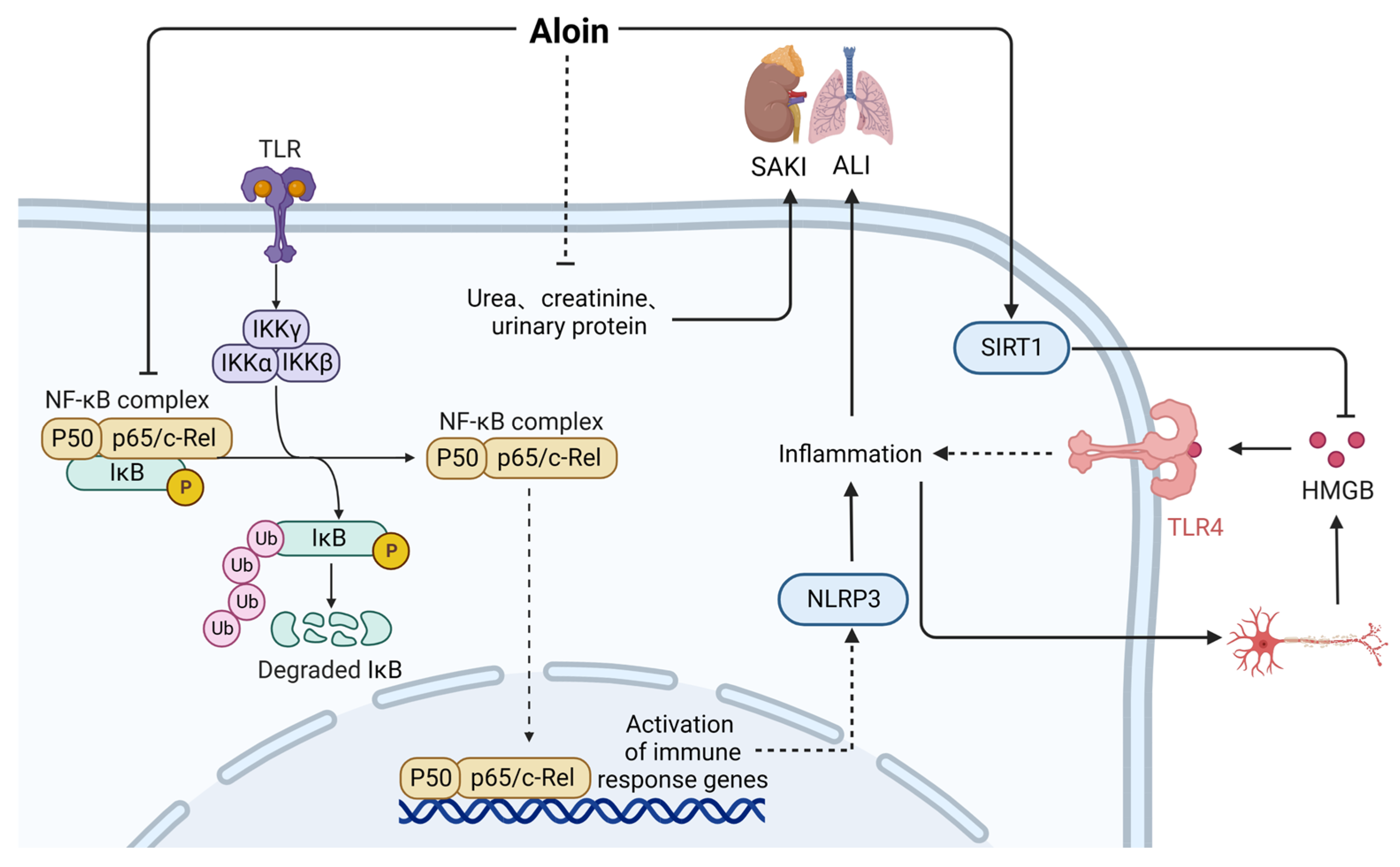
- Luo, X.; Zhang, H.; Wei, X.; Shi, M.; Fan, P.; Xie, W.; Zhang, Y.; Xu, N. Aloin Suppresses Lipopolysaccharide-Induced Inflammatory Response and Apoptosis by Inhibiting the Activation of NF-κB. Molecules 2018, 23, 517. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Shen, Y.; Xv, G.; Di, Z.; Li, Y.; Li, G. Aloin Suppresses Lipopolysaccharide-Induced Acute Lung Injury by Inhibiting NLRP3/NF-κB via Activation of SIRT1 in Mice. Immunopharmacol. Immunotoxicol. 2020, 42, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Lee, W.; Lee, B.S.; Lee, C.; Park, E.K.; Ku, S.K.; Bae, J.S. Aloin Reduces HMGB1-Mediated Septic Responses and Improves Survival in Septic Mice by Activation of the SIRT1 and PI3K/Nrf2/HO-1 Signaling Axis. Am. J. Chin. Med. 2019, 47, 613–633. [Google Scholar] [CrossRef]
- Lee, W.; Jeong, G.S.; Baek, M.C.; Ku, S.K.; Bae, J.S. Renal Protective Effects of Aloin in a Mouse Model of Sepsis. Food Chem. Toxicol. 2019, 132, 110651. [Google Scholar] [CrossRef]
- Xu, F.; Xu, J.; Xiong, X.; Deng, Y. Salidroside Inhibits MAPK, NF-κB, and STAT3 Pathways in Psoriasis-Associated Oxidative Stress via SIRT1 Activation. Redox Rep. 2019, 24, 70–74. [Google Scholar] [CrossRef]
- Wu, M.; Hu, R.; Wang, J.; An, Y.; Lu, L.; Long, C.; Yan, L. Salidroside Suppresses IL-1β-Induced Apoptosis in Chondrocytes via Phosphatidylinositol 3-Kinases (PI3K)/Akt Signaling Inhibition. Med. Sci. Monit. 2019, 25, 5833–5840. [Google Scholar] [CrossRef]
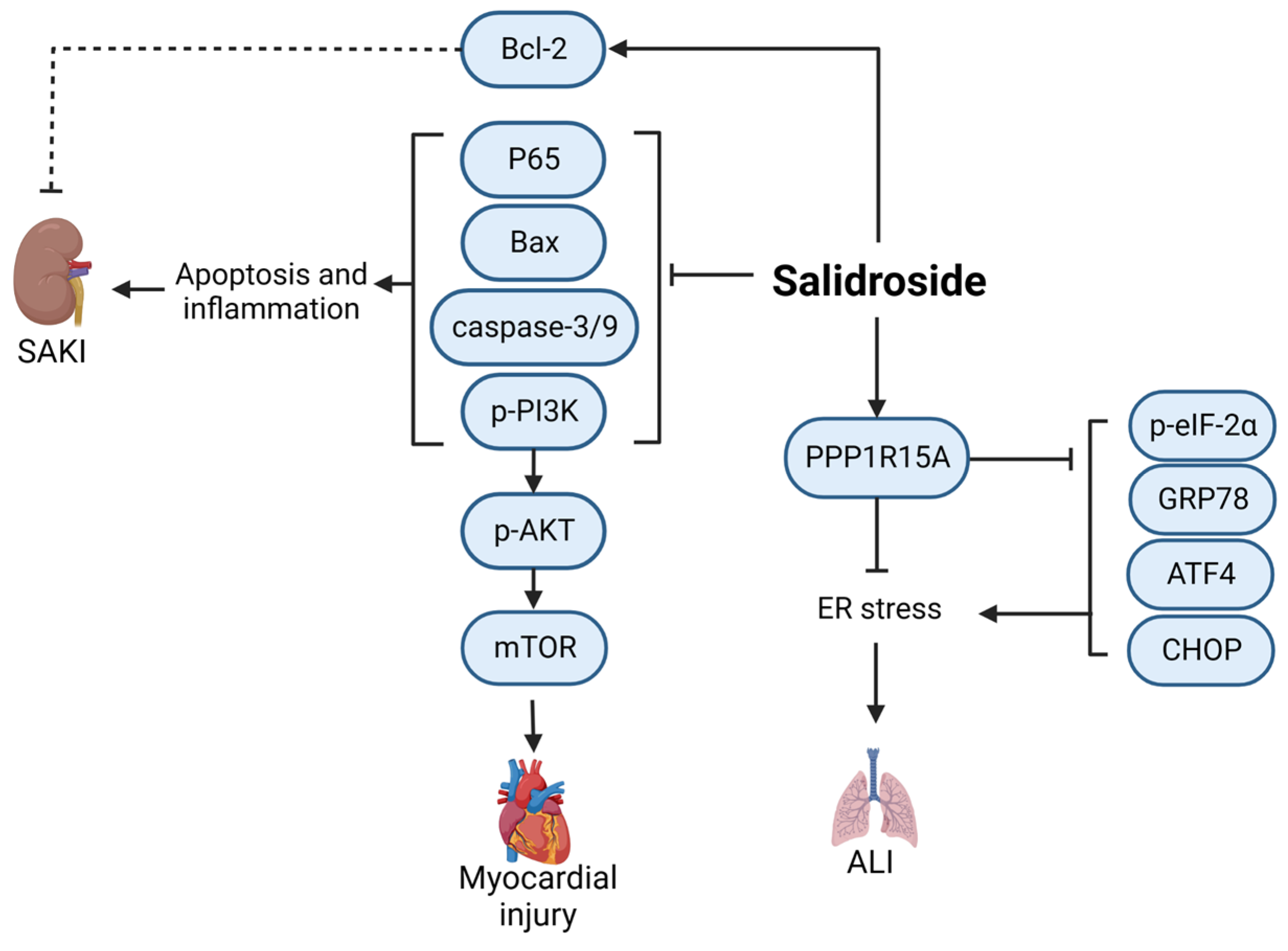
- Fan, H.; Su, B.J.; Le, J.W.; Zhu, J.H. Salidroside Protects Acute Kidney Injury in Septic Rats by Inhibiting Inflammation and Apoptosis. Drug Des. Dev. Ther. 2022, 16, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Xu, L.; Zheng, L.; Wang, Y.; Zhuang, M.; Yang, D. Salidroside Attenuates Sepsis-Associated Acute Lung Injury Through PPP1R15A Mediated Endoplasmic Reticulum Stress Inhibition. Bioorg. Med. Chem. 2022, 71, 116865. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Liu, P.; Feng, X.; Ma, C. Salidroside Suppressing LPS-Induced Myocardial Injury by Inhibiting ROS-Mediated PI3K/Akt/mTOR Pathway In Vitro and In Vivo. J. Cell. Mol. Med. 2017, 21, 3178–3189. [Google Scholar] [CrossRef] [PubMed]
- Pan, T.; Shi, X.; Chen, H.; Chen, R.; Wu, D.; Lin, Z.; Zhang, J.; Pan, J. Correction to: Geniposide Suppresses Interleukin-1β-Induced Inflammation and Apoptosis in Rat Chondrocytes via the PI3K/Akt/NF-κB Signaling Pathway. Inflammation 2019, 42, 404–405. [Google Scholar] [CrossRef] [PubMed]
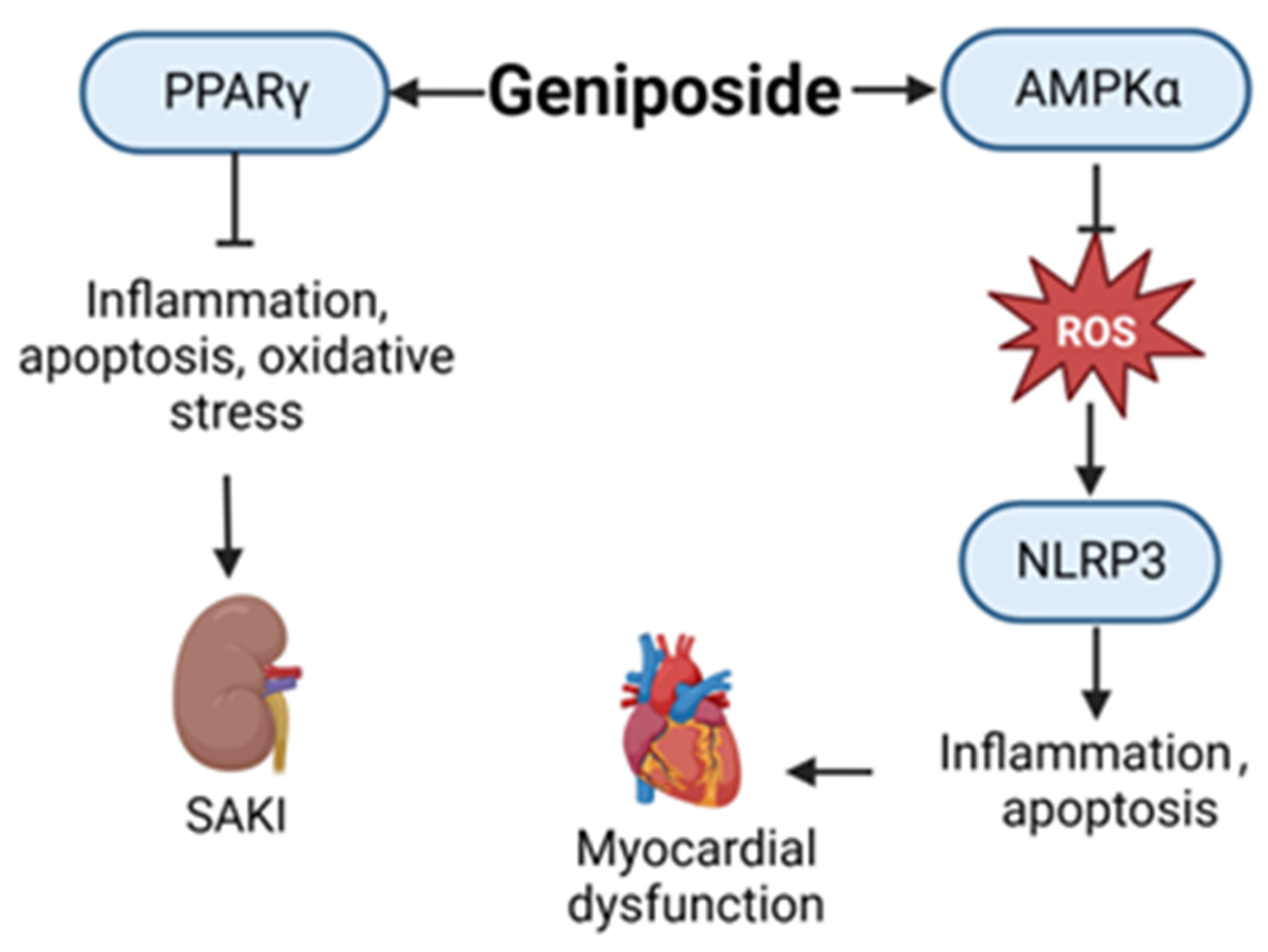
- Song, P.; Shen, D.F.; Meng, Y.Y.; Kong, C.Y.; Zhang, X.; Yuan, Y.P.; Yan, L.; Tang, Q.Z.; Ma, Z.G. Geniposide Protects Against Sepsis-Induced Myocardial Dysfunction Through AMPKα-Dependent Pathway. Free Radic. Biol. Med. 2020, 152, 186–196. [Google Scholar] [CrossRef]
- Liu, J.; Zhao, N.; Shi, G.; Wang, H. Geniposide Ameliorated Sepsis-Induced Acute Kidney Injury by Activating PPARγ. Aging 2020, 12, 22744–22758. [Google Scholar] [CrossRef]
- Wu, L.L.; Jia, B.H.; Sun, J.; Chen, J.X.; Liu, Z.Y.; Liu, Y. Protective Effects of Ginsenoside Rb1 on Septic Rats and Its Mechanism. Biomed. Environ. Sci. 2014, 27, 300–303. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.; Ji, Y.; Li, Z.; Chen, R.; Zhou, S.; Liu, C.; Du, M. Ginsenoside Rb3 Inhibits Pro-inflammatory Cytokines via MAPK/AKT/NF-κB Pathways and Attenuates Rat Alveolar Bone Resorption in Response to Porphyromonas gingivalis LPS. Molecules 2020, 25, 4815. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Liu, M.; Chen, G.; Wu, Y.; Xie, L.; Han, X.; Zhang, G.; Tan, Z.; Ding, W.; Fan, H.; et al. Anti-Inflammatory Effects of Ginsenoside Rb3 in LPS-Induced Macrophages Through Direct Inhibition of TLR4 Signaling Pathway. Front. Pharmacol. 2022, 13, 714554. [Google Scholar] [CrossRef]
- Hwang, S.J.; Wang, J.H.; Lee, J.S.; Kang, J.Y.; Baek, D.C.; Kim, G.H.; Ahn, Y.C.; Son, C.G. Ginseng Sprouts Attenuate Mortality and Systemic Inflammation by Modulating TLR4/NF-κB Signaling in an LPS-Induced Mouse Model of Sepsis. Int. J. Mol. Sci. 2023, 24, 1583. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.; Tang, Y.; Zhang, F.; Zhang, L. Roles of Ginsenosides in Sepsis. J. Ginseng Res. 2023, 47, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.L.; Yang, L.; Peng, Y.; Gao, M.; Yang, M.S.; Xing, W.; Xiao, X.Z. Ginsenoside Rg1 Regulates SIRT1 to Ameliorate Sepsis-Induced Lung Inflammation and Injury via Inhibiting Endoplasmic Reticulum Stress and Inflammation. Mediat. Inflamm. 2019, 2019, 6453296. [Google Scholar] [CrossRef]
- Luo, M.; Yan, D.; Sun, Q.; Tao, J.; Xu, L.; Sun, H.; Zhao, H. Ginsenoside Rg1 Attenuates Cardiomyocyte Apoptosis and Inflammation via the TLR4/NF-kB/NLRP3 Pathway. J. Cell. Biochem. 2020, 121, 2994–3004. [Google Scholar] [CrossRef]
- Kim, T.W.; Joh, E.H.; Kim, B.; Kim, D.H. Ginsenoside Rg5 Ameliorates Lung Inflammation in Mice by Inhibiting the Binding of LPS to Toll-Like Receptor-4 on Macrophages. Int. Immunopharmacol. 2012, 12, 110–116. [Google Scholar] [CrossRef]
- Paik, S.; Choe, J.H.; Choi, G.E.; Kim, J.E.; Kim, J.M.; Song, G.Y.; Jo, E.K. Rg6, a Rare Ginsenoside, Inhibits Systemic Inflammation through the Induction of Interleukin-10 and microRNA-146a. Sci. Rep. 2019, 9, 4342. [Google Scholar] [CrossRef]
- Nguyen, T.L.L.; Huynh, D.T.N.; Jin, Y.; Jeon, H.; Heo, K.S. Protective Effects of Ginsenoside-Rg2 and -Rh1 on Liver Function Through Inhibiting TAK1 and STAT3-Mediated Inflammatory Activity and Nrf2/ARE-Mediated Antioxidant Signaling Pathway. Arch. Pharm. Res. 2021, 44, 241–252. [Google Scholar] [CrossRef]
- Lee, W.; Cho, S.H.; Kim, J.E.; Lee, C.; Lee, J.H.; Baek, M.C.; Song, G.Y.; Bae, J.S. Suppressive Effects of Ginsenoside Rh1 on HMGB1-Mediated Septic Responses. Am. J. Chin. Med. 2019, 47, 119–133. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Park, J.S.; Ma, Y.; Ma, H.; Lee, Y.J.; Lee, G.R.; Yoo, H.S.; Hong, J.T.; Roh, Y.S. Ginseng Saponin Enriched in Rh1 and Rg2 Ameliorates Nonalcoholic Fatty Liver Disease by Inhibiting Inflammasome Activation. Nutrients 2021, 13, 856. [Google Scholar] [CrossRef] [PubMed]
- Xing, W.; Yang, L.; Peng, Y.; Wang, Q.; Gao, M.; Yang, M.; Xiao, X. Ginsenoside Rg3 Attenuates Sepsis-Induced Injury and Mitochondrial Dysfunction in Liver via AMPK-Mediated Autophagy Flux. Biosci. Rep. 2017, 37, BSR20170934. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.O.; Kim, N.; Song, G.Y.; Bae, J.S. Inhibitory Activities of Rare Ginsenoside Rg4 on Cecal Ligation and Puncture-Induced Sepsis. Int. J. Mol. Sci. 2022, 23, 10836. [Google Scholar] [CrossRef] [PubMed]
- Sun, R.; Li, Y.; Chen, W.; Zhang, F.; Li, T. Total Ginsenosides Synergize With Ulinastatin Against Septic Acute Lung Injury and Acute Respiratory Distress Syndrome. Int. J. Clin. Exp. Pathol. 2015, 8, 7385–7390. [Google Scholar] [CrossRef]
- Liu, Y.; Wen, P.H.; Zhang, X.X.; Dai, Y.; He, Q. Breviscapine Ameliorates CCl4-Induced Liver Injury in Mice Through Inhibiting Inflammatory Apoptotic Response and ROS Generation. Int. J. Mol. Med. 2018, 42, 755–768. [Google Scholar] [CrossRef]
- Chen, Z.Q.; Zhou, Y.; Chen, F.; Huang, J.W.; Zheng, J.; Li, H.L.; Li, T.; Li, L. Breviscapine Pretreatment Inhibits Myocardial Inflammation and Apoptosis in Rats After Coronary Microembolization by Activating the PI3K/Akt/GSK-3β Signaling Pathway. Drug Des. Dev. Ther. 2021, 15, 843–855. [Google Scholar] [CrossRef] [PubMed]
- Dinda, B.; Dinda, S.; Dassharma, S.; Banik, R.; Chakraborty, A.; Dinda, M. Therapeutic Potentials of Baicalin and Its Aglycone, Baicalein Against Inflammatory Disorders. Eur. J. Med. Chem. 2017, 131, 68–80. [Google Scholar] [CrossRef]
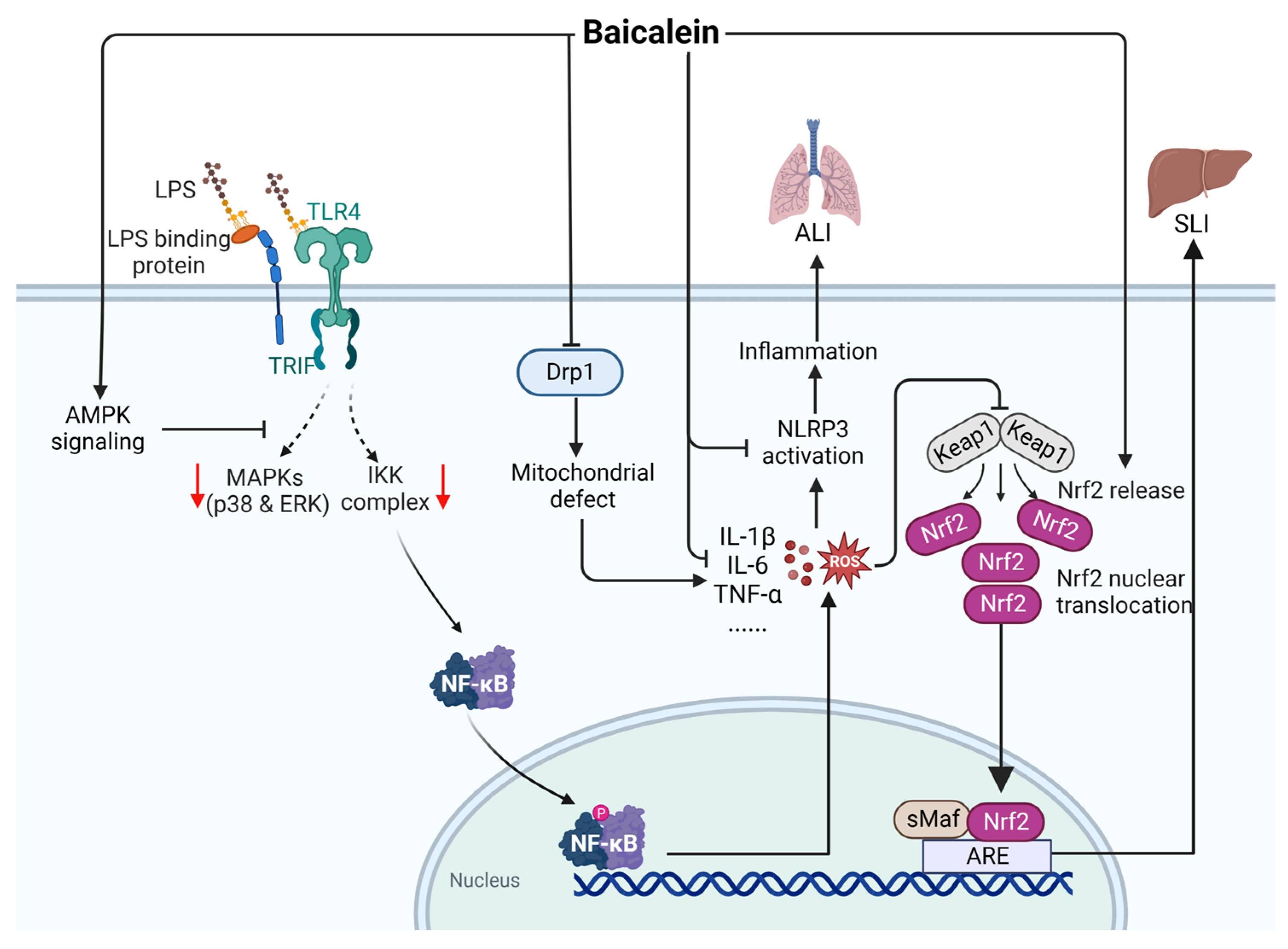
- Zhang, X.; Qin, Y.; Ruan, W.; Wan, X.; Lv, C.; He, L.; Lu, L.; Guo, X. Targeting Inflammation-Associated AMPK/Mfn-2/MAPKs Signaling Pathways by Baicalein Exerts Anti-atherosclerotic Action. Phytother. Res. 2021, 35, 4442–4455. [Google Scholar] [CrossRef]
- Liu, Y.; Jing, Y.Y.; Zeng, C.Y.; Li, C.G.; Xu, L.H.; Yan, L.; Bai, W.J.; Zha, Q.B.; Ouyang, D.Y.; He, X.H. Scutellarin Suppresses NLRP3 Inflammasome Activation in Macrophages and Protects Mice Against Bacterial Sepsis. Front. Pharmacol. 2017, 8, 975. [Google Scholar] [CrossRef]
- Jiang, C.; Zhang, J.; Xie, H.; Guan, H.; Li, R.; Chen, C.; Dong, H.; Zhou, Y.; Zhang, W. Baicalein Suppresses Lipopolysaccharide-Induced Acute Lung Injury by Regulating Drp1-Dependent Mitochondrial Fission of Macrophages. Biomed. Pharmacother. 2022, 145, 112408. [Google Scholar] [CrossRef]
- Dai, J.M.; Guo, W.N.; Tan, Y.Z.; Niu, K.W.; Zhang, J.J.; Liu, C.L.; Yang, X.M.; Tao, K.S.; Chen, Z.N.; Dai, J.Y. Wogonin Alleviates Liver Injury in Sepsis Through Nrf2-Mediated NF-κB Signalling Suppression. J. Cell. Mol. Med. 2021, 25, 5782–5798. [Google Scholar] [CrossRef]
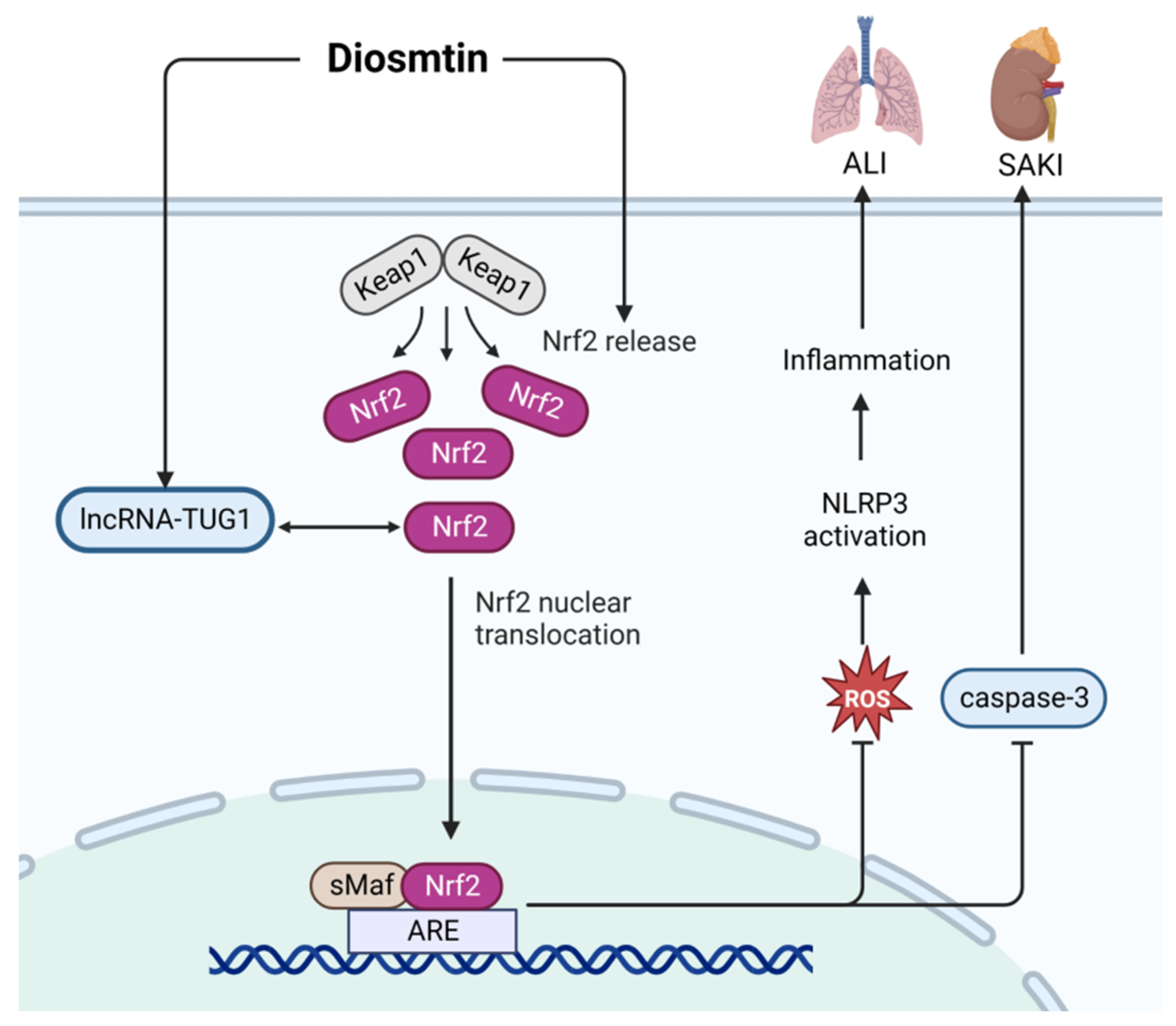
- Yang, Y.; Gong, X.B.; Huang, L.G.; Wang, Z.X.; Wan, R.Z.; Zhang, P.; Zhang, Q.Y.; Chen, Z.; Zhang, B.S. Diosmetin Exerts Anti-oxidative, Anti-Inflammatory and Anti-apoptotic Effects to Protect against Endotoxin-Induced Acute Hepatic Failure in Mice. Oncotarget 2017, 8, 30723–30733. [Google Scholar] [CrossRef]
- Wang, W.; Zhang, S.; Yang, F.; Xie, J.; Chen, J.; Li, Z. Diosmetin Alleviates Acute Kidney Injury by Promoting the TUG1/Nrf2/HO-1 Pathway in Sepsis Rats. Int. Immunopharmacol. 2020, 88, 106965. [Google Scholar] [CrossRef]
- Liu, Q.; Ci, X.; Wen, Z.; Peng, L. Diosmetin Alleviates Lipopolysaccharide-Induced Acute Lung Injury Through Activating the Nrf2 Pathway and Inhibiting the NLRP3 Inflammasome. Biomol. Ther. 2018, 26, 157–166. [Google Scholar] [CrossRef]
- Kotagale, N.R.; Taksande, B.G.; Inamdar, N.N. Neuroprotective Offerings by Agmatine. Neurotoxicology 2019, 73, 228–245. [Google Scholar] [CrossRef]
- El-Awady, M.S.; Nader, M.A.; Sharawy, M.H. The Inhibition of Inducible Nitric Oxide Synthase and Oxidative Stress by Agmatine Attenuates Vascular Dysfunction in Rat Acute Endotoxemic Model. Environ. Toxicol. Pharmacol. 2017, 55, 74–80. [Google Scholar] [CrossRef]
- Li, X.; Zhu, J.; Tian, L.; Ma, X.; Fan, X.; Luo, L.; Yu, J.; Sun, Y.; Yang, X.; Tang, W.; et al. Agmatine Protects Against the Progression of Sepsis Through the Imidazoline I2 Receptor-Ribosomal S6 Kinase 2-Nuclear Factor-κB Signaling Pathway. Crit. Care Med. 2020, 48, e40–e47. [Google Scholar] [CrossRef]
- Liu, X.; Zheng, X.; Wang, N.; Cao, H.; Lu, Y.; Long, Y.; Zhao, K.; Zhou, H.; Zheng, J. Kukoamine B, a Novel Dual Inhibitor of LPS and CpG DNA, Is a Potential Candidate for Sepsis Treatment. Br. J. Pharmacol. 2011, 162, 1274–1290. [Google Scholar] [CrossRef]
- Wang, H.; Hu, X.; Wang, T.; Cui, C.; Jiang, J.; Dong, K.; Chen, S.; Jin, C.; Zhao, Q.; Du, B.; et al. Exposure-Response Modeling to Support Dosing Selection for Phase IIb Development of Kukoamine B in Sepsis Patients. Front. Pharmacol. 2021, 12, 645130. [Google Scholar] [CrossRef]
- Zhao, Q.; Liu, H.; Wang, Z.; Wang, T.; Cui, C.; Wang, H.; Li, L.; Zhong, W.; Jiang, J.; Dong, K.; et al. Safety, Tolerability, and Pharmacokinetics of Kukoamine B in Healthy Volunteers: A Randomized, Double-Blind, Placebo-Controlled, Multiple-Dose Phase I Study. Adv. Ther. 2023, 40, 3186–3198. [Google Scholar] [CrossRef]
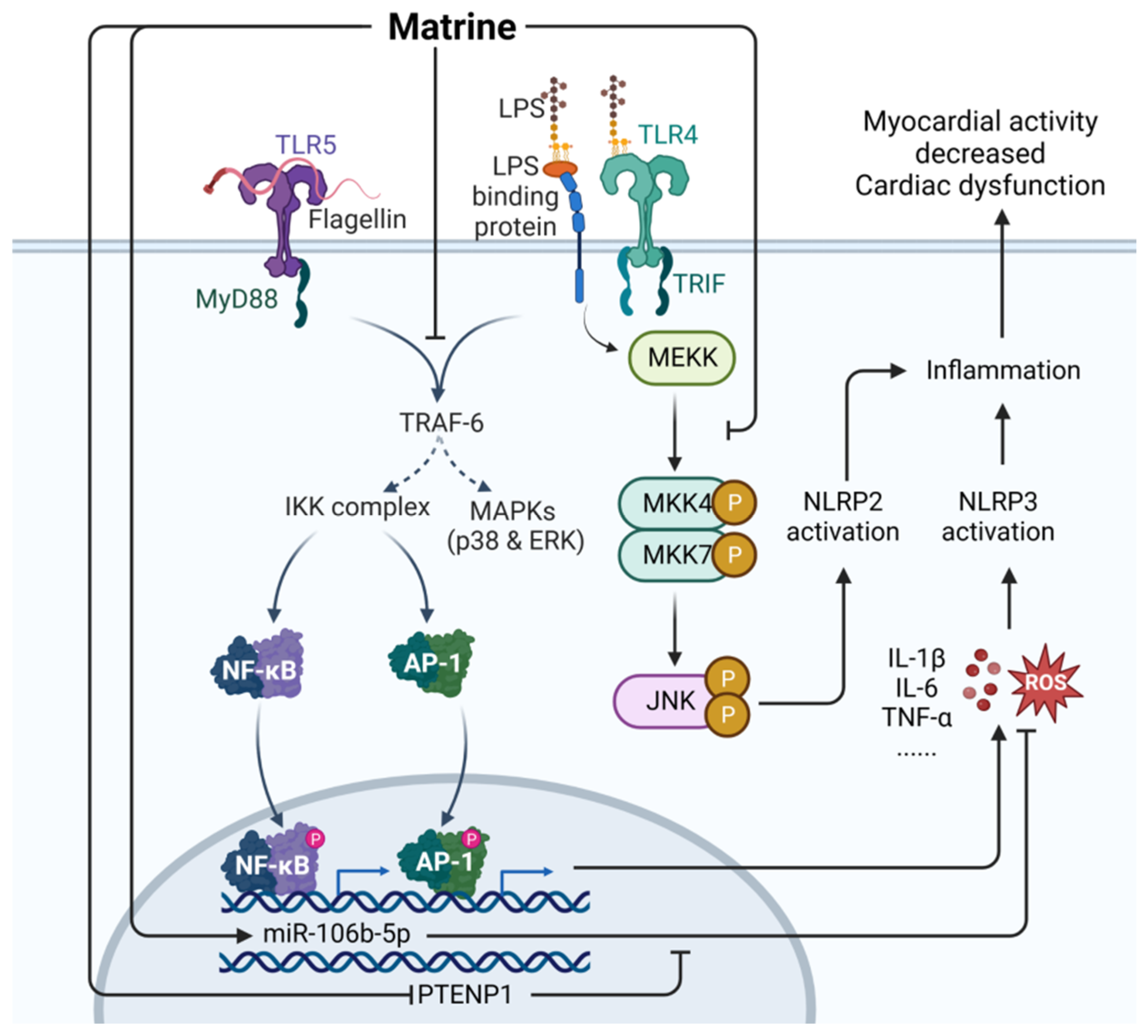
- Cai, X.H.; Guo, H.; Xie, B. Structural Modifications of Matrine-Type Alkaloids. Mini Rev. Med. Chem. 2018, 18, 730–744. [Google Scholar] [CrossRef]
- Lin, Y.; He, F.; Wu, L.; Xu, Y.; Du, Q. Matrine Exerts Pharmacological Effects Through Multiple Signaling Pathways: A Comprehensive Review. Drug Des. Dev. Ther. 2022, 16, 533–569. [Google Scholar] [CrossRef]
- Sun, P.; Sun, N.; Yin, W.; Sun, Y.; Fan, K.; Guo, J.; Khan, A.; He, Y.; Li, H. Matrine Inhibits IL-1β Secretion in Primary Porcine Alveolar Macrophages Through the MyD88/NF-κB Pathway and NLRP3 Inflammasome. Vet. Res. 2019, 50, 53. [Google Scholar] [CrossRef]
- Wang, X.; Wu, F.P.; Huang, Y.R.; Li, H.D.; Cao, X.Y.; You, Y.; Meng, Z.F.; Sun, K.Y.; Shen, X.Y. Matrine Suppresses NLRP3 Inflammasome Activation via Regulating PTPN2/JNK/SREBP2 Pathway in Sepsis. Phytomedicine 2023, 109, 154574. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, L.; Zhang, J. Protective Role of Matrine in Sepsis-Associated Cardiac Dysfunction Through Regulating the lncRNA PTENP1/miR-106b-5p Axis. Biomed. Pharmacother. 2021, 134, 111112. [Google Scholar] [CrossRef]
- Wan, F.; Du, X.; Liu, H.; He, X.; Zeng, Y. Protective Effect of Anisodamine Hydrobromide on Lipopolysaccharide-Induced Acute Kidney Injury. Biosci. Rep. 2020, 40, BSR20201812. [Google Scholar] [CrossRef]
- Li, Z.; Xu, C.; Tao, Y.; Liang, Y.; Liang, Q.; Li, J.; Li, R.; Ye, H. Anisodamine Alleviates Lipopolysaccharide-Induced Pancreatic Acinar Cell Injury Through NLRP3 Inflammasome and NF-κB Signaling Pathway. J. Recept. Signal Transduct. Res. 2020, 40, 58–66. [Google Scholar] [CrossRef]
- Zeng, Y.; Du, X.; Jiang, W.; Qiu, Y. Anisodamine Hydrobromide Protects Against Acute Lung Injury in Septic Rats Induced by Lipopolysaccharide or Cecal Ligation and Puncture via Inhibiting Apoptosis and Pyroptosis. FASEB. J. 2021, 35. [Google Scholar] [CrossRef]
- Du, X.; Liu, H.; Yue, Y.; Wu, Q.; Jiang, W.; Qiu, Y.; Zeng, Y. Anisodamine Hydrobromide Protects Glycocalyx and Against the Lipopolysaccharide-Induced Increases in Microvascular Endothelial Layer Permeability and Nitric Oxide Production. Cardiovasc. Eng. Technol. 2021, 12, 91–100. [Google Scholar] [CrossRef]
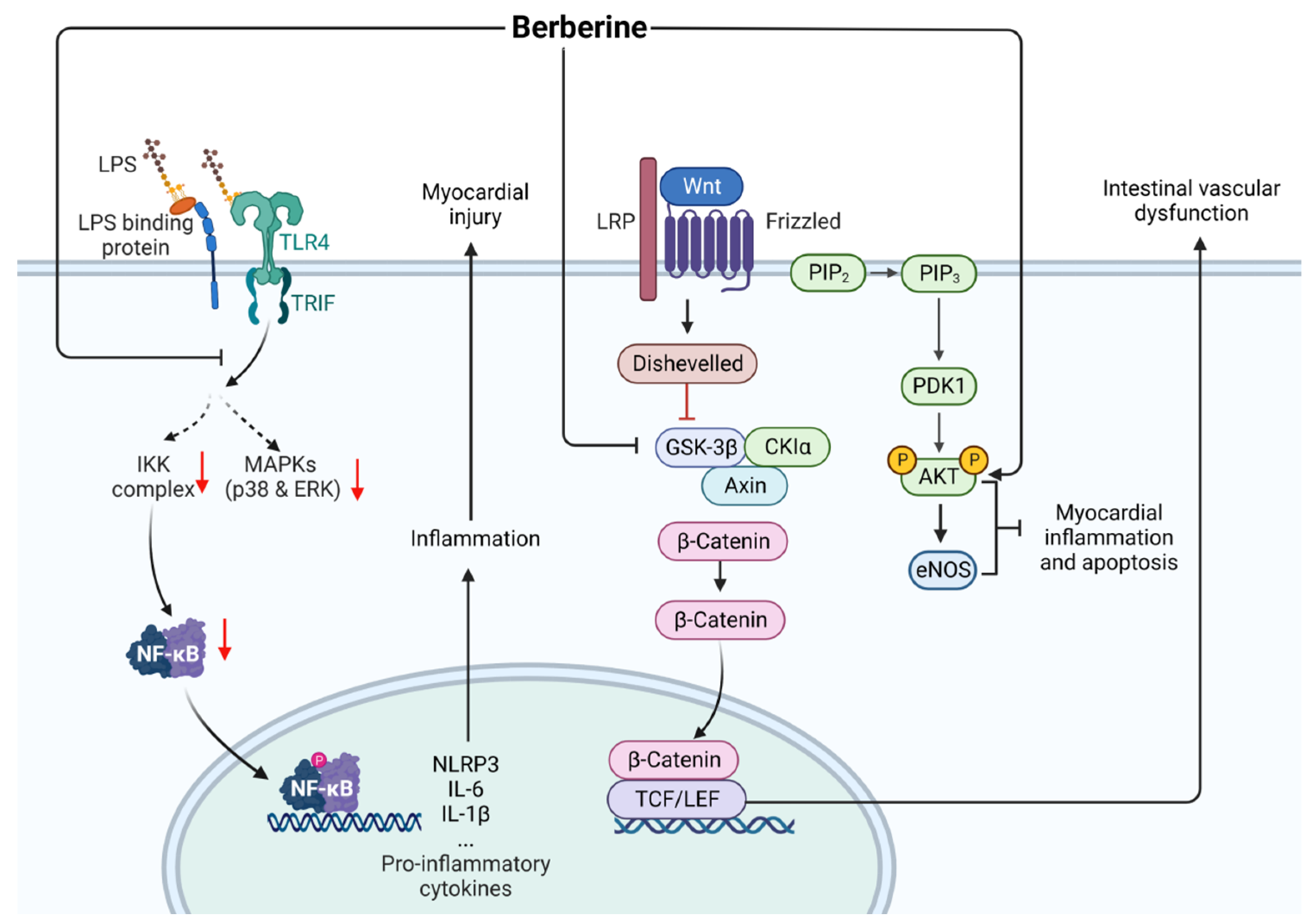
- Takahara, M.; Takaki, A.; Hiraoka, S.; Adachi, T.; Shimomura, Y.; Matsushita, H.; Nguyen, T.T.T.; Koike, K.; Ikeda, A.; Takashima, S.; et al. Berberine Improved Experimental Chronic Colitis by Regulating Interferon-γ- and IL-17A-producing Lamina Propria CD4+ T Cells Through AMPK Activation. Sci. Rep. 2019, 9, 11934. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Wu, X.; Tao, Y.; Lu, G. Berberine Attenuates Sepsis-Induced Cardiac Dysfunction by Upregulating the Akt/eNOS Pathway in Mice. Exp. Ther. Med. 2022, 23, 371. [Google Scholar] [CrossRef]
- Chen, H.; Liu, Q.; Liu, X.; Jin, J. Berberine Attenuates Septic Cardiomyopathy by Inhibiting TLR4/NF-κB Signalling in Rats. Pharm. Biol. 2021, 59, 121–128. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Yuan, X.; Zuo, H.; Sun, Y.; Feng, A. Berberine Exerts a Protective Effect on Gut-Vascular Barrier via the Modulation of the Wnt/Beta-Catenin Signaling Pathway During Sepsis. Cell. Physiol. Biochem. 2018, 49, 1342–1351. [Google Scholar] [CrossRef]
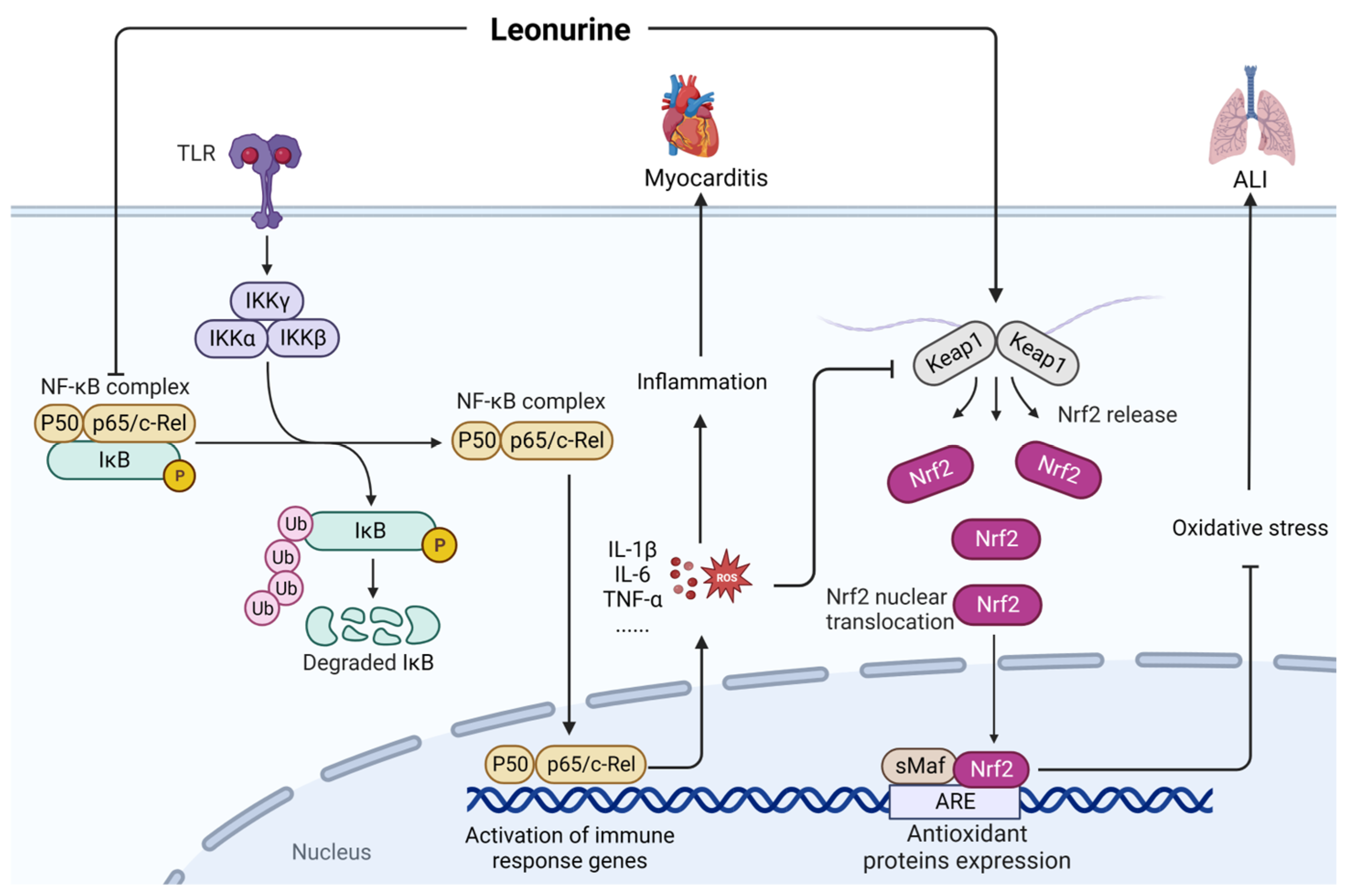
- Zhang, G.; Wang, L. Leonurine: A Compound With the Potential to Prevent Acute Lung Injury. Exp. Ther. Med. 2022, 23, 358. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Li, D.; Ouyang, J.; Tian, X.; Zhao, Y.; Peng, X.; Li, S.; Yu, G.; Yang, J. Leonurine Alleviates LPS-Induced Myocarditis Through Suppressing the NF-κB Signaling Pathway. Toxicology 2019, 422, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Cruzat, V.; Macedo Rogero, M.; Noel Keane, K.; Curi, R.; Newsholme, P. Glutamine: Metabolism and Immune Function, Supplementation and Clinical Translation. Nutrients 2018, 10, 1564. [Google Scholar] [CrossRef]
- Stonoga, E.T.S.; Bueno, R.Z.; Nagano, T.A.; Martins, V.; Rocha, S.L. Effects of Intraperitoneal Glutamine in the Treatment of Experimental Sepsis. Arq. Bras. Cir. Dig. 2019, 32, e1431. [Google Scholar] [CrossRef]
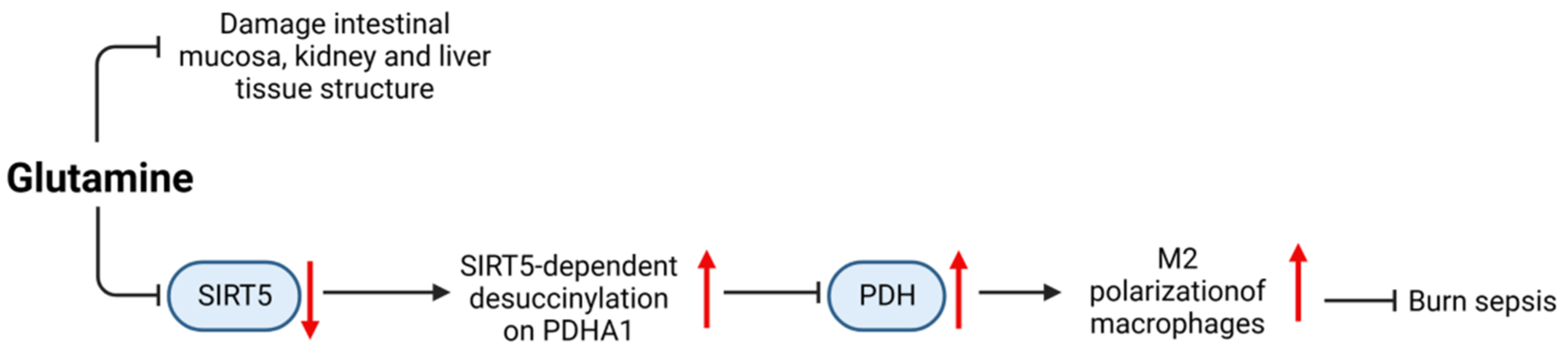
- Zhu, Y.; Chen, X.; Lu, Y.; Xia, L.; Fan, S.; Huang, Q.; Liu, X.; Peng, X. Glutamine Mitigates Murine Burn Sepsis by Supporting Macrophage M2 Polarization Through Repressing the SIRT5-Mediated Desuccinylation of Pyruvate Dehydrogenase. Burns Trauma 2022, 10, tkac041. [Google Scholar] [CrossRef]
- Koksal, G.M.; Erbabacan, E.; Tunali, Y.; Karaoren, G.; Vehid, S.; Oz, H. The Effects of Intravenous, Enteral and Combined Administration of Glutamine on Malnutrition in Sepsis: A Randomized Clinical Trial. Asia Pac. J. Clin. Nutr. 2014, 23, 34–40. [Google Scholar] [CrossRef]





| Compound | Model | Improvement | Adverse Reaction | Research Progress |
|---|---|---|---|---|
| Resveratrol | CLP/LPS | SAKI/SAE/ALI/cardiomyocyte injury | High doses can increase intracellular oxidation | Animal experiment |
| Curcumin | CLP/LPS | SAKI/ALI | Animal experiment | |
| Tetrahydrocurcumin | CLP | SAKI | Animal experiment | |
| Emodin | CLP/LPS | ALI/IMI/cognitive dysfunction | Animal experiment | |
| Aloin | CLP/LPS | SAKI/ALI | Animal experiment | |
| Salidroside | CLP/LPS | SAKI/ALI/myocardial injury | Animal experiment | |
| Geniposide | CLP/LPS | SAKI/myocardial dysfunction | Animal experiment | |
| Ginsenoside | CLP/LPS | Inflammatory response and organ damage | Animal experiment | |
| Breviscapine | CME | Myocardium inflammation | Animal experiment | |
| Baicalein | CLP/LPS | ALI/SLI | Animal experiment | |
| Diosmtin | LPS | SAKI/ALI | Cell experiment | |
| Agmatine | LPS | Vascular dysfunction/systemic inflammation and organ failure | Animal experiment | |
| Kukoamine B | LPS | Inflammation | clinical trials | |
| Matrine | CLP/LPS | Cardiac insufficiency | Animal experiment | |
| Anisodamine hydrobromide | LPS | SAKI/ALI | Animal experiment | |
| Berberine | CLP/LPS | Cardiac dysfunction, myocardial injury, and intestinal vascular barrier dysfunction | Animal experiment | |
| Leonurine | LPS | ALI/myocarditis | Animal experiment | |
| Glutamine | CLP | Damage to the intestinal mucosa, kidney, and liver tissues | Clinical trials |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, J.; Zhou, F.; Wu, S.; Tong, Z. Research Progress on Natural Small-Molecule Compounds for the Prevention and Treatment of Sepsis. Int. J. Mol. Sci. 2023, 24, 12732. https://doi.org/10.3390/ijms241612732
Su J, Zhou F, Wu S, Tong Z. Research Progress on Natural Small-Molecule Compounds for the Prevention and Treatment of Sepsis. International Journal of Molecular Sciences. 2023; 24(16):12732. https://doi.org/10.3390/ijms241612732
Chicago/Turabian StyleSu, Jingqian, Fen Zhou, Shun Wu, and Zhiyong Tong. 2023. "Research Progress on Natural Small-Molecule Compounds for the Prevention and Treatment of Sepsis" International Journal of Molecular Sciences 24, no. 16: 12732. https://doi.org/10.3390/ijms241612732
APA StyleSu, J., Zhou, F., Wu, S., & Tong, Z. (2023). Research Progress on Natural Small-Molecule Compounds for the Prevention and Treatment of Sepsis. International Journal of Molecular Sciences, 24(16), 12732. https://doi.org/10.3390/ijms241612732






