Ginsenoside Compound K Ameliorates Development of Diabetic Kidney Disease through Inhibiting TLR4 Activation Induced by Microbially Produced Imidazole Propionate
Abstract
1. Introduction
2. Results
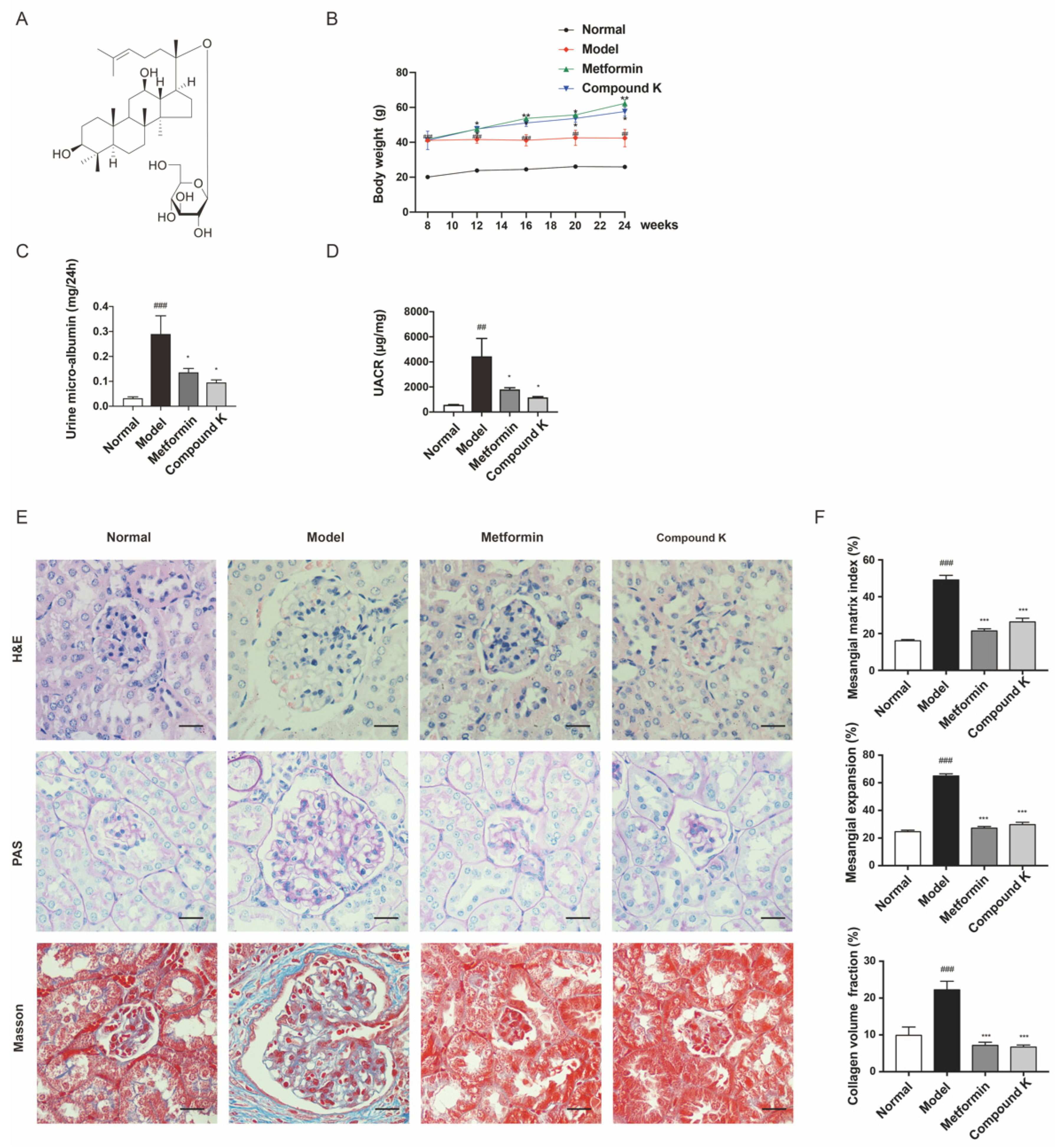
2.1. CK Supplementation Protects against Diabetic Kidney Injury in db/db Mice
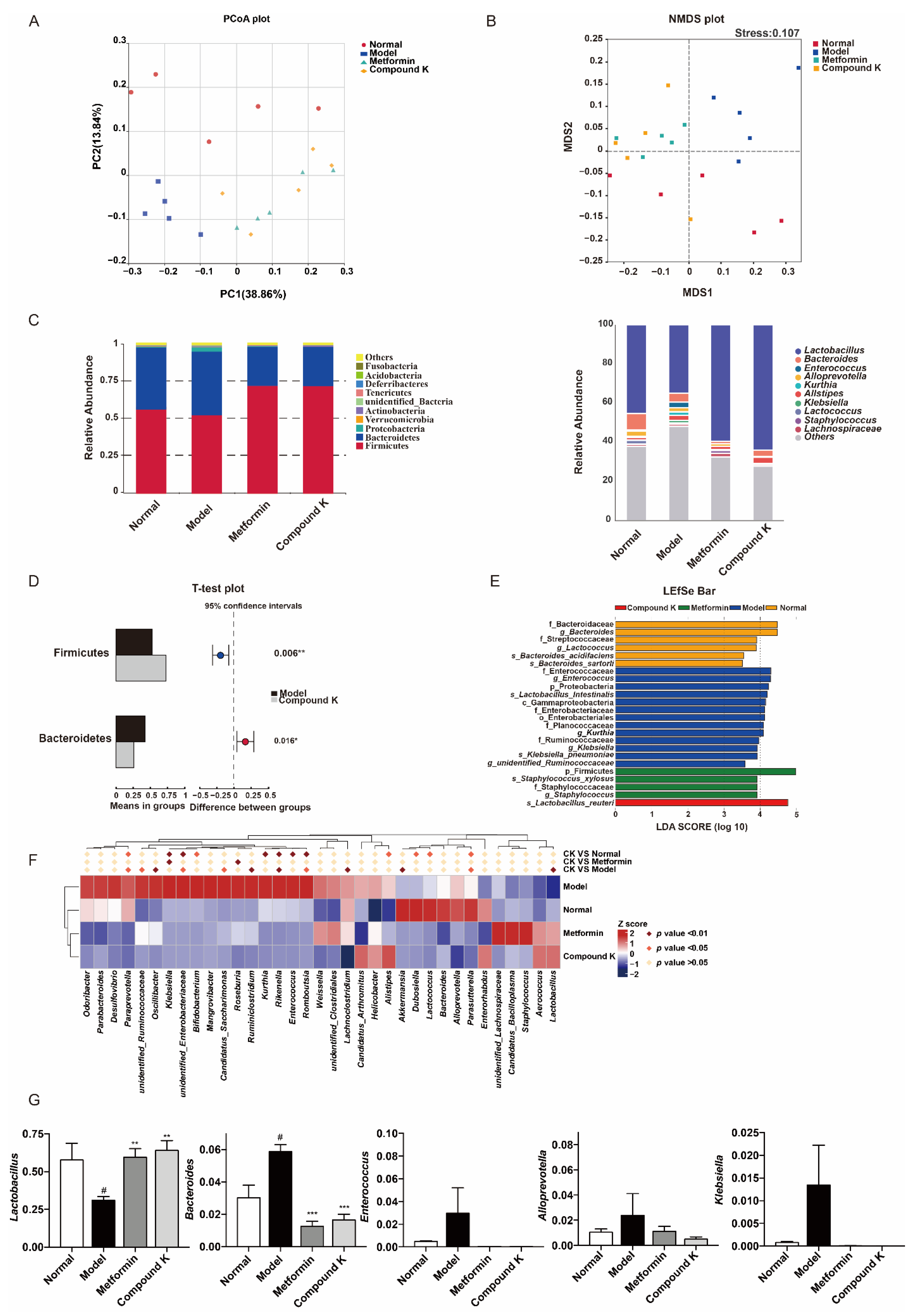
2.2. CK Supplementation Modifies the Diabetic Mice Gut Microbial Composition to Modulate Renal Function
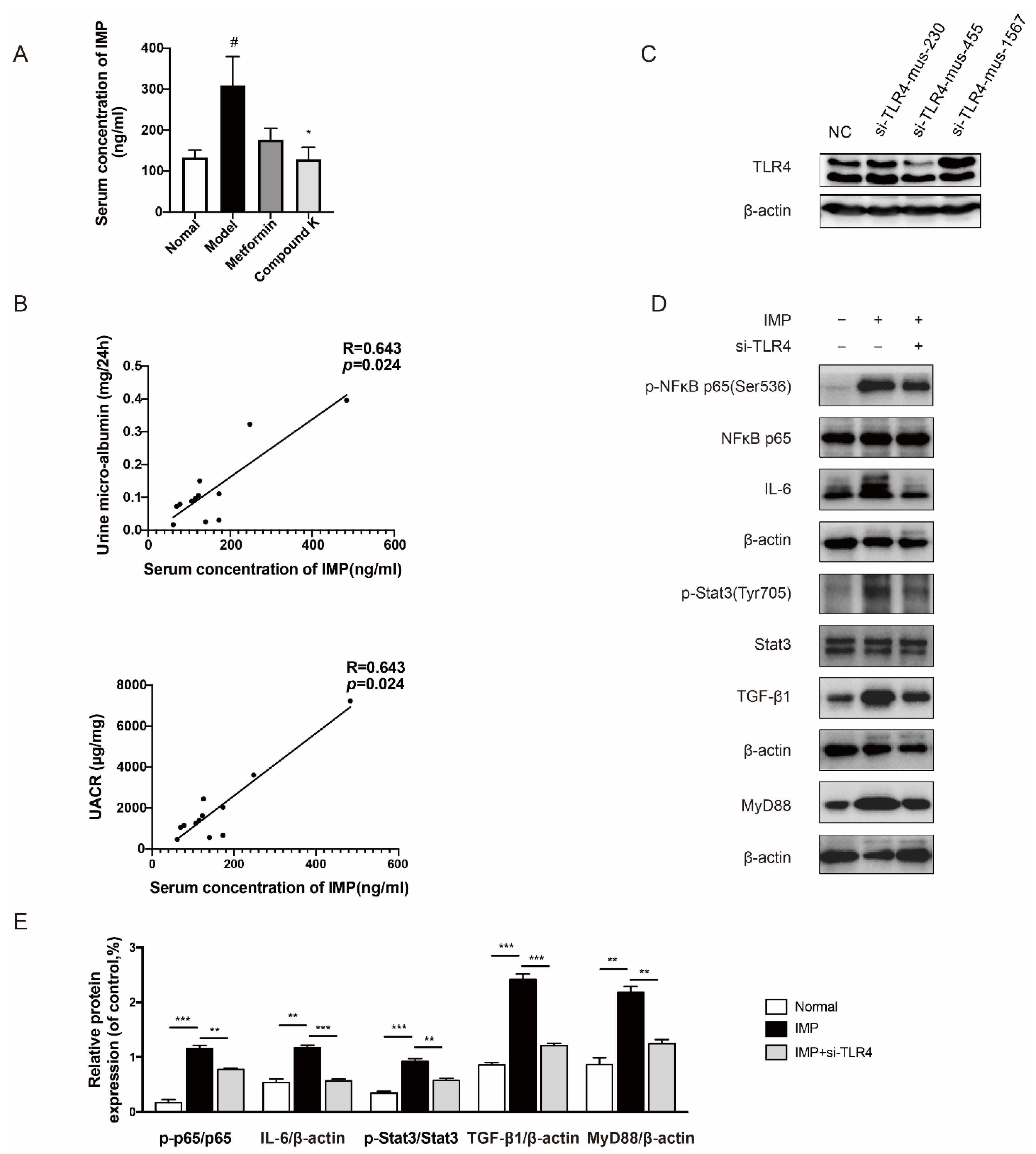
2.3. CK Supplementation Reduced Microbial Metabolite IMP as a TLR4 Agonist Related to Proteinuria in DKD
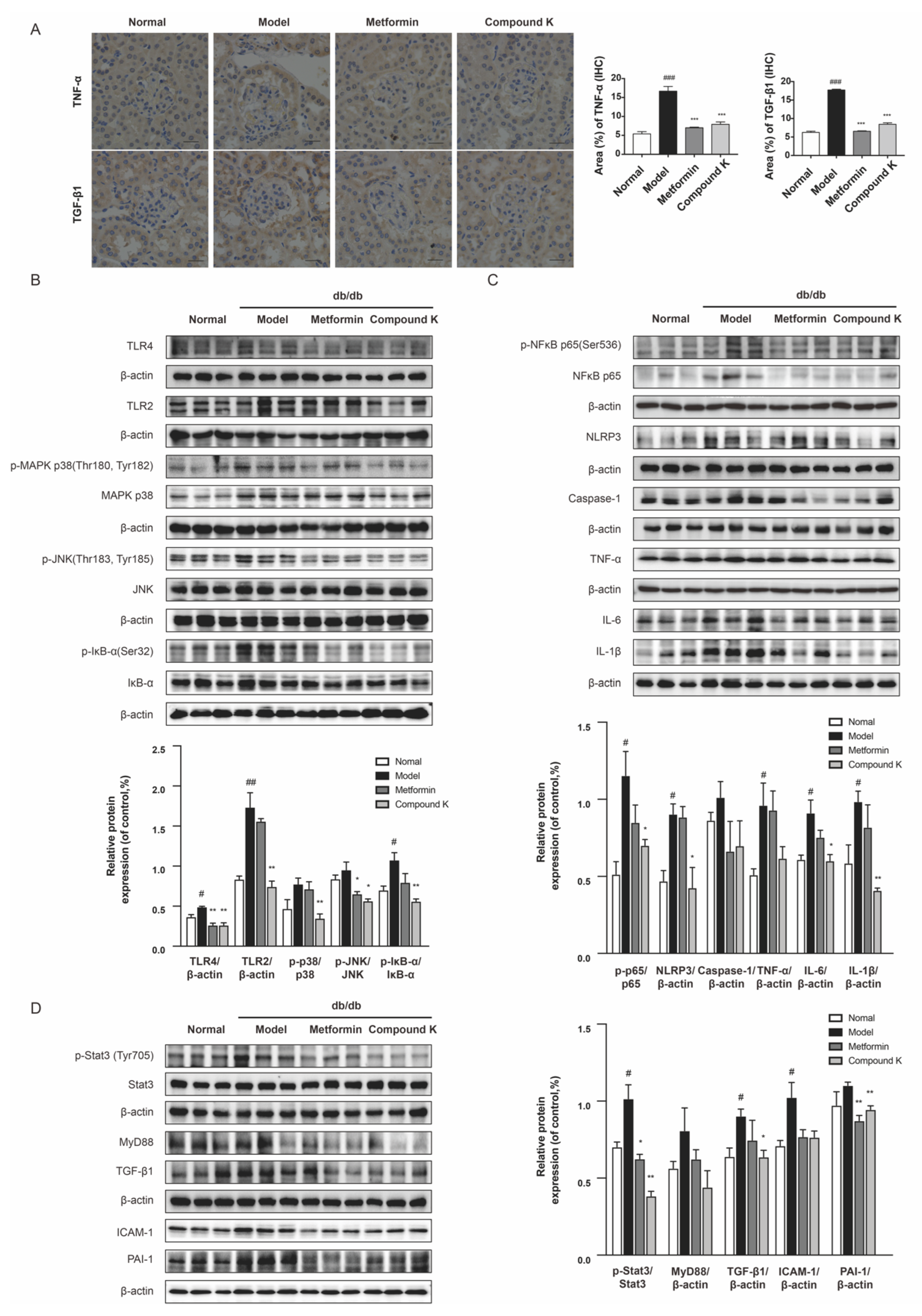
2.4. CK Supplementation Presents Inhibiting Effects on TLR4 Signaling Pathway in db/db Mice
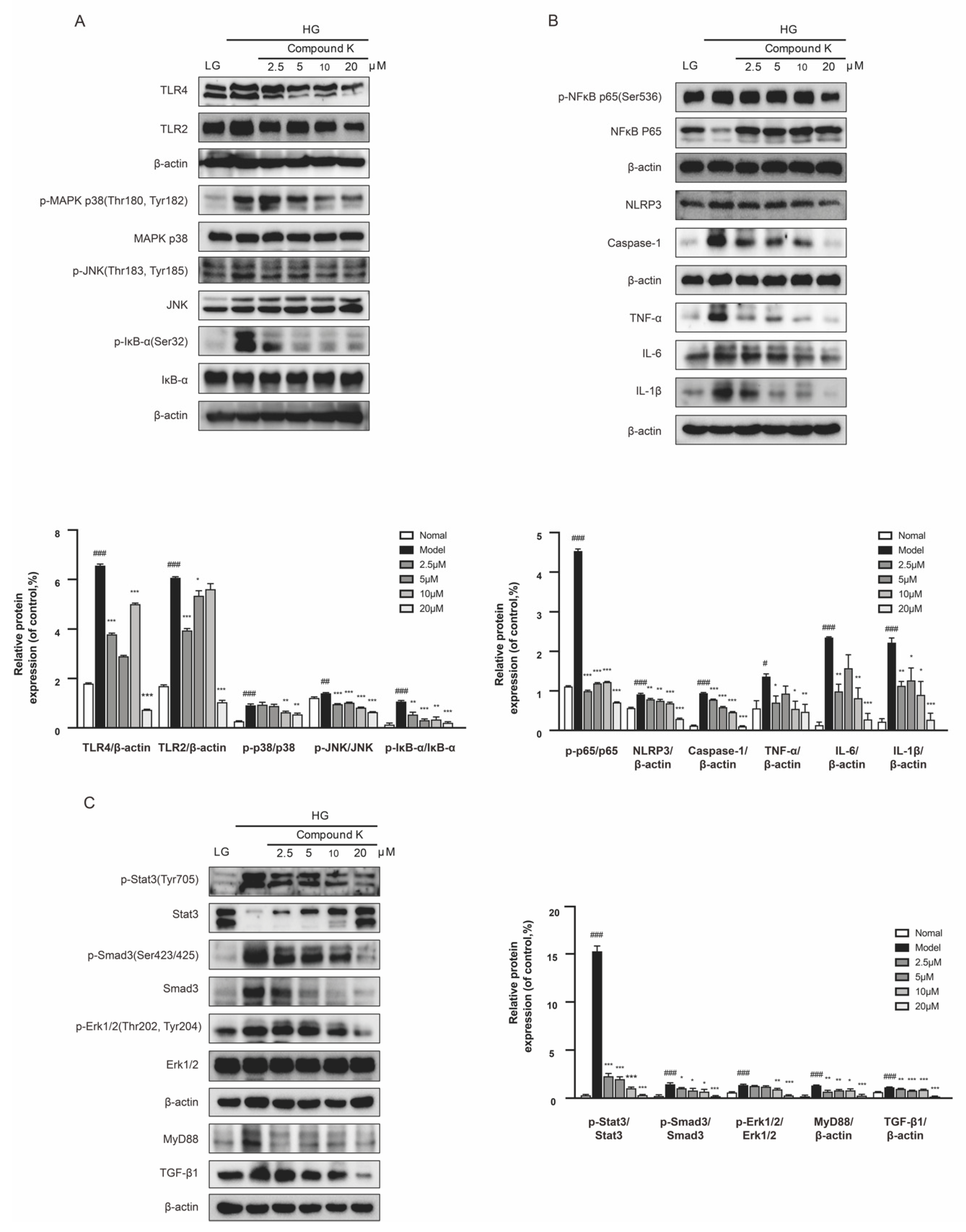
2.5. CK Suppresses TLR4 Signaling Pathway in the Presence of High Glucose Concentration
2.6. CK Attenuates DKD Renal Injury through Inhibiting IMP-Induced Inflammation and Fibrosis
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Animals and Experimental Design
4.3. Analysis of Biochemical Parameters
4.4. Morphological Changes
4.5. Microbial Diversity Analysis
4.6. Metabolite Analysis
4.7. Immunohistochemistry (IHC) Staining Analysis
4.8. Cell Culture and Treatment
4.9. Western Blot Analysis
4.10. Statistical Analysis
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vallon, V.; Thomson, S. Renal function in diabetic disease models: The tubular system in the pathophysiology of the diabetic kidney. Annu. Rev. Physiol. 2012, 74, 351–375. [Google Scholar] [CrossRef]
- Gilbert, S.J.; Weiner, D.E.; National Kidney Foundation. National Kidney Foundation Primer on Kidney Diseases, 8th ed.; Elevier Health Sciences: Amsterdam, The Netherlands, 2017; p. 1. [Google Scholar]
- Ekinci, E.; Jerums, G.; Skene, A.; Crammer, P.; Power, D.; Cheong, K.; Panagiotopoulos, S.; McNeil, K.; Baker, S.; Fioretto, P.; et al. Renal structure in normoalbuminuric and albuminuric patients with type 2 diabetes and impaired renal function. Diabetes Care 2013, 36, 3620–3626. [Google Scholar] [CrossRef] [PubMed]
- Skupien, J.; Warram, J.; Smiles, A.; Stanton, R.; Krolewski, A. Patterns of estimated glomerular filtration rate decline leading to end-stage renal disease in type 1 diabetes. Diabetes Care 2016, 39, 2262–2269. [Google Scholar] [CrossRef] [PubMed]
- Ihara, K.; Skupien, J.; Kobayashi, H.; Md Dom, Z.; Wilson, J.; O’Neil, K.; Badger, H.; Bowsman, L.; Satake, E.; Breyer, M.; et al. Profibrotic circulating proteins and risk of early progressive renal decline in patients with type 2 diabetes with and without albuminuria. Diabetes Care 2020, 43, 2760–2767. [Google Scholar] [CrossRef] [PubMed]
- Buyadaa, O.; Magliano, D.; Salim, A.; Koye, D.; Shaw, J. Risk of rapid kidney function decline, all-cause mortality, and major cardiovascular events in nonalbuminuric chronic kidney disease in type 2 diabetes. Diabetes Care 2020, 43, 122–129. [Google Scholar] [CrossRef]
- Taylor, A. Intensive therapy and gfr in type 1 diabetes. N. Engl. J. Med. 2012, 366, 857. [Google Scholar] [PubMed]
- Kalantar-Zadeh, K.; Jafar, T.; Nitsch, D.; Neuen, B.; Perkovic, V. Chronic kidney disease. Lancet 2021, 398, 786–802. [Google Scholar] [CrossRef]
- Bos, M.; Robert, V.; Tommassen, J. Biogenesis of the gram-negative bacterial outer membrane. Annu. Rev. Microbiol. 2007, 61, 191–214. [Google Scholar] [CrossRef] [PubMed]
- Reidy, K.; Kang, H.; Hostetter, T.; Susztak, K. Molecular mechanisms of diabetic kidney disease. J. Clin. Investig. 2014, 124, 2333–2340. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Lu, J.; Chen, P.; Lu, C.; Zhang, J.; Li, X.; Yuan, B.; Huang, S.; Ruan, X.; Liu, B.; et al. Dysbiosis of intestinal microbiota mediates tubulointerstitial injury in diabetic nephropathy via the disruption of cholesterol homeostasis. Acta Pharmacol. Sin. 2020, 10, 2803–2816. [Google Scholar] [CrossRef]
- Kikuchi, K.; Saigusa, D.; Kanemitsu, Y.; Matsumoto, Y.; Thanai, P.; Suzuki, N.; Mise, K.; Yamaguchi, H.; Nakamura, T.; Asaji, K.; et al. Gut microbiome-derived phenyl sulfate contributes to albuminuria in diabetic kidney disease. Nat. Commun. 2019, 10, 1835. [Google Scholar] [CrossRef]
- Fang, Q.; Liu, N.; Zheng, B.; Guo, F.; Zeng, X.; Huang, X.; Ouyang, D. Roles of gut microbial metabolites in diabetic kidney disease. Front. Endocrinol. 2021, 12, 636175. [Google Scholar] [CrossRef] [PubMed]
- Sapa, H.; Gutiérrez, O.; Shlipak, M.; Katz, R.; Ix, J.; Sarnak, M.; Cushman, M.; Rhee, E.; Kimmel, P.; Vasan, R.; et al. Association of uremic solutes with cardiovascular death in diabetic kidney disease. Am. J. Kidney Dis. 2022, 80, 502–512. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.; Gao, Y.; Teo, G.; Koh, H.; Tai, E.; Khoo, C.; Choi, K.; Zhou, L.; Choi, H. Plasma metabolome and lipidome associations with type 2 diabetes and diabetic nephropathy. Metabolites 2021, 11, 228. [Google Scholar] [CrossRef] [PubMed]
- De Vos, W.; Tilg, H.; van Hul, M.; Cani, P. Gut microbiome and health: Mechanistic insights. Gut 2022, 71, 1020–1032. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Beltrán, J.; Brito, I. Host-microbiome protein-protein interactions capture disease-relevant pathways. Genome Biol. 2022, 23, 72. [Google Scholar] [CrossRef]
- Lobel, L.; Cao, Y.; Fenn, K.; Glickman, J.; Garrett, W. Diet posttranslationally modifies the mouse gut microbial proteome to modulate renal function. Science 2020, 369, 1518–1524. [Google Scholar] [CrossRef] [PubMed]
- Karunasagara, S.; Hong, G.; Park, S.; Lee, N.; Jung, D.; Kim, T.; Jung, J. Korean red ginseng attenuates hyperglycemia-induced renal inflammation and fibrosis via accelerated autophagy and protects against diabetic kidney disease. J. Ethnopharmacol. 2020, 254, 112693. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Chung, S.; Chung, M.; Choi, H.; Hwang, J.; Park, J. Effects of panax ginseng on hyperglycemia, hypertension, and hyperlipidemia: A systematic review and meta-analysis. J. Ginseng Res. 2022, 46, 188–205. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Hong, Q.; Chen, B.; Cui, S.; Liu, R.; Cai, G.; Guo, J.; Chen, X. Ginsenoside rb1 alleviates diabetic kidney podocyte injury by inhibiting aldose reductase activity. Acta Pharmacol. Sin. 2022, 43, 342–353. [Google Scholar] [CrossRef] [PubMed]
- Miao, L.; Yang, Y.; Li, Z.; Fang, Z.; Zhang, Y.; Han, C. Ginsenoside rb2: A review of pharmacokinetics and pharmacological effects. J. Ginseng Res. 2022, 46, 206–213. [Google Scholar] [CrossRef] [PubMed]
- Ratan, Z.; Haidere, M.; Hong, Y.; Park, S.; Lee, J.; Lee, J.; Cho, J. Pharmacological potential of ginseng and its major component ginsenosides. J. Ginseng Res. 2021, 45, 199–210. [Google Scholar] [CrossRef]
- Ren, Z.; Fan, Y.; Li, A.; Shen, Q.; Wu, J.; Ren, L.; Lu, H.; Ding, S.; Ren, H.; Liu, C.; et al. Alterations of the human gut microbiome in chronic kidney disease. Sci. Adv. 2020, 7, 2001936. [Google Scholar] [CrossRef]
- Zhang, B.; Wan, Y.; Zhou, X.; Zhang, H.; Zhao, H.; Ma, L.; Dong, X.; Yan, M.; Zhao, T.; Li, P. Characteristics of serum metabolites and gut microbiota in diabetic kidney disease. Front. Pharmacol. 2022, 13, 872988. [Google Scholar] [CrossRef]
- Wu, J.; Wu, Y.; Feng, W.; Chen, Q.; Wang, D.; Liu, M.; Yu, H.; Zhang, Y.; Wang, T. Role of microbial metabolites of histidine in the development of colitis. Mol. Nutr. Food Res. 2022, 66, e2101175. [Google Scholar] [CrossRef]
- Tang, S.; Yiu, W. Innate immunity in diabetic kidney disease. Nat. Rev. Nephrol. 2020, 16, 206–222. [Google Scholar] [CrossRef] [PubMed]
- Sheng, X.; Qiu, C.; Liu, H.; Gluck, C.; Hsu, J.; He, J.; Hsu, C.; Sha, D.; Weir, M.; Isakova, T.; et al. Systematic integrated analysis of genetic and epigenetic variation in diabetic kidney disease. Proc. Natl. Acad. Sci. USA 2020, 117, 29013–29024. [Google Scholar] [CrossRef]
- Feng, Y.; Yang, S.; Ma, Y.; Bai, X.; Chen, X. Role of toll-like receptors in diabetic renal lesions in a miniature pig model. Sci. Adv. 2015, 1, e1400183. [Google Scholar] [CrossRef] [PubMed]
- Velloso, L.; Folli, F.; Saad, M. Tlr4 at the crossroads of nutrients, gut microbiota, and metabolic inflammation. Endocr. Rev. 2015, 36, 245–271. [Google Scholar] [CrossRef] [PubMed]
- Van Heck, J.; Gacesa, R.; Stienstra, R.; Fu, J.; Zhernakova, A.; Harmsen, H.; Weersma, R.; Joosten, L.; Tack, C. The gut microbiome composition is altered in long-standing type 1 diabetes and associates with glycemic control and disease-related complications. Diabetes Care 2022, 45, 2084–2094. [Google Scholar] [CrossRef]
- Lau, W.; Vaziri, N. Gut microbial short-chain fatty acids and the risk of diabetes. Nat. Rev. Nephrol. 2019, 15, 389–390. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhao, J.; Qin, Y.; Yu, Z.; Zhang, Y.; Ning, X.; Sun, S. The specific alteration of gut microbiota in diabetic kidney diseases-a systematic review and meta-analysis. Front. Immunol. 2022, 13, 908219. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Hu, Z.; Wang, R.; Hong, Z.; Lu, J.; Chen, P.; Zhang, J.; Li, X.; Yuan, B.; Huang, S.; et al. Gut microbiota dysbiosis-induced activation of the intrarenal renin-angiotensin system is involved in kidney injuries in rat diabetic nephropathy. Acta Pharmacol. Sin. 2020, 41, 1111–1118. [Google Scholar] [CrossRef]
- Ricciardi, C.; Gnudi, L. Kidney disease in diabetes: From mechanisms to clinical presentation and treatment strategies. Metabolism 2021, 124, 154890. [Google Scholar] [CrossRef] [PubMed]
- Jin, D.; Zhang, Y.; Zhang, Y.; Duan, L.; Zhou, R.; Duan, Y.; Sun, Y.; Lian, F.; Tong, X. Panax ginseng c.A.Mey. As medicine: The potential use of panax ginseng c.A.Mey. As a remedy for kidney protection from a pharmacological perspective. Front. Pharmacol. 2021, 12, 734151. [Google Scholar] [CrossRef]
- Sen, S.; Chen, S.; Feng, B.; Wu, Y.; Lui, E.; Chakrabarti, S. Preventive effects of north american ginseng (panax quinquefolium) on diabetic nephropathy. Phytomedicine 2012, 19, 494–505. [Google Scholar] [CrossRef]
- Liu, H.; Chen, W.; Lu, P.; Ma, Y.; Liang, X.; Liu, Y. Ginsenoside rg1 attenuates the inflammation and oxidative stress induced by diabetic nephropathy through regulating the pi3k/akt/foxo3 pathway. Ann. Transl. Med. 2021, 9, 1789. [Google Scholar] [CrossRef]
- Su, W.; Li, Y.; Chen, X.; Li, X.; Wei, H.; Liu, Z.; Shen, Q.; Chen, C.; Wang, Y.; Li, W. Ginsenoside rh1 improves type 2 diabetic nephropathy through ampk/pi3k/akt-mediated inflammation and apoptosis signaling pathway. Am. J. Chin. Med. 2021, 49, 1215–1233. [Google Scholar] [CrossRef]
- Zhu, Y.; Zhu, C.; Yang, H.; Deng, J.; Fan, D. Protective effect of ginsenoside rg5 against kidney injury via inhibition of nlrp3 inflammasome activation and the mapk signaling pathway in high-fat diet/streptozotocin-induced diabetic mice. Pharmacol. Res. 2020, 155, 104746. [Google Scholar] [CrossRef]
- Wang, C.; Huang, Y.; Chan, F.; Su, S.; Kuo, Y.; Huang, S.; Hung, M.; Lin, H.; Chang, W.; Chang, T. A gut microbial metabolite of ginsenosides, compound k, induces intestinal glucose absorption and na(+)/glucose cotransporter 1 gene expression through activation of camp response element binding protein. Mol. Nutr. Food Res. 2015, 59, 670–684. [Google Scholar] [CrossRef]
- Molinaro, A.; Bel Lassen, P.; Henricsson, M.; Wu, H.; Adriouch, S.; Belda, E.; Chakaroun, R.; Nielsen, T.; Bergh, P.; Rouault, C.; et al. Imidazole propionate is increased in diabetes and associated with dietary patterns and altered microbial ecology. Nat. Commun. 2020, 11, 5881. [Google Scholar] [CrossRef] [PubMed]
- Mafra, D.; Borges, N.; Lindholm, B.; Shiels, P.; Evenepoel, P.; Stenvinkel, P. Food as medicine: Targeting the uraemic phenotype in chronic kidney disease. Nat. Rev. Nephrol. 2021, 17, 153–171. [Google Scholar] [CrossRef] [PubMed]
- Koh, A.; Molinaro, A.; Ståhlman, M.; Khan, M.; Schmidt, C.; Mannerås-Holm, L.; Wu, H.; Carreras, A.; Jeong, H.; Olofsson, L.; et al. Microbially produced imidazole propionate impairs insulin signaling through mtorc1. Cell 2018, 175, 947.e917–961.e917. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Q.; Ren, D.; Liu, L.; Xu, J.; Wu, Y.; Yu, H.; Liu, M.; Zhang, Y.; Wang, T. Ginsenoside Compound K Ameliorates Development of Diabetic Kidney Disease through Inhibiting TLR4 Activation Induced by Microbially Produced Imidazole Propionate. Int. J. Mol. Sci. 2022, 23, 12863. https://doi.org/10.3390/ijms232112863
Chen Q, Ren D, Liu L, Xu J, Wu Y, Yu H, Liu M, Zhang Y, Wang T. Ginsenoside Compound K Ameliorates Development of Diabetic Kidney Disease through Inhibiting TLR4 Activation Induced by Microbially Produced Imidazole Propionate. International Journal of Molecular Sciences. 2022; 23(21):12863. https://doi.org/10.3390/ijms232112863
Chicago/Turabian StyleChen, Qian, Dongwen Ren, Luokun Liu, Jingge Xu, Yuzheng Wu, Haiyang Yu, Mengyang Liu, Yi Zhang, and Tao Wang. 2022. "Ginsenoside Compound K Ameliorates Development of Diabetic Kidney Disease through Inhibiting TLR4 Activation Induced by Microbially Produced Imidazole Propionate" International Journal of Molecular Sciences 23, no. 21: 12863. https://doi.org/10.3390/ijms232112863
APA StyleChen, Q., Ren, D., Liu, L., Xu, J., Wu, Y., Yu, H., Liu, M., Zhang, Y., & Wang, T. (2022). Ginsenoside Compound K Ameliorates Development of Diabetic Kidney Disease through Inhibiting TLR4 Activation Induced by Microbially Produced Imidazole Propionate. International Journal of Molecular Sciences, 23(21), 12863. https://doi.org/10.3390/ijms232112863




