Targeting mTOR-CCL20 Signaling May Improve Response to Docetaxel in Head and Neck Squamous Cell Carcinoma
Abstract
1. Introduction
2. Results
2.1. In Vitro Cell Growth and In Vivo Tumor Growth
2.2. Immunohistochemical Staining for mTOR in NU/NU Mouse Xenograft Models
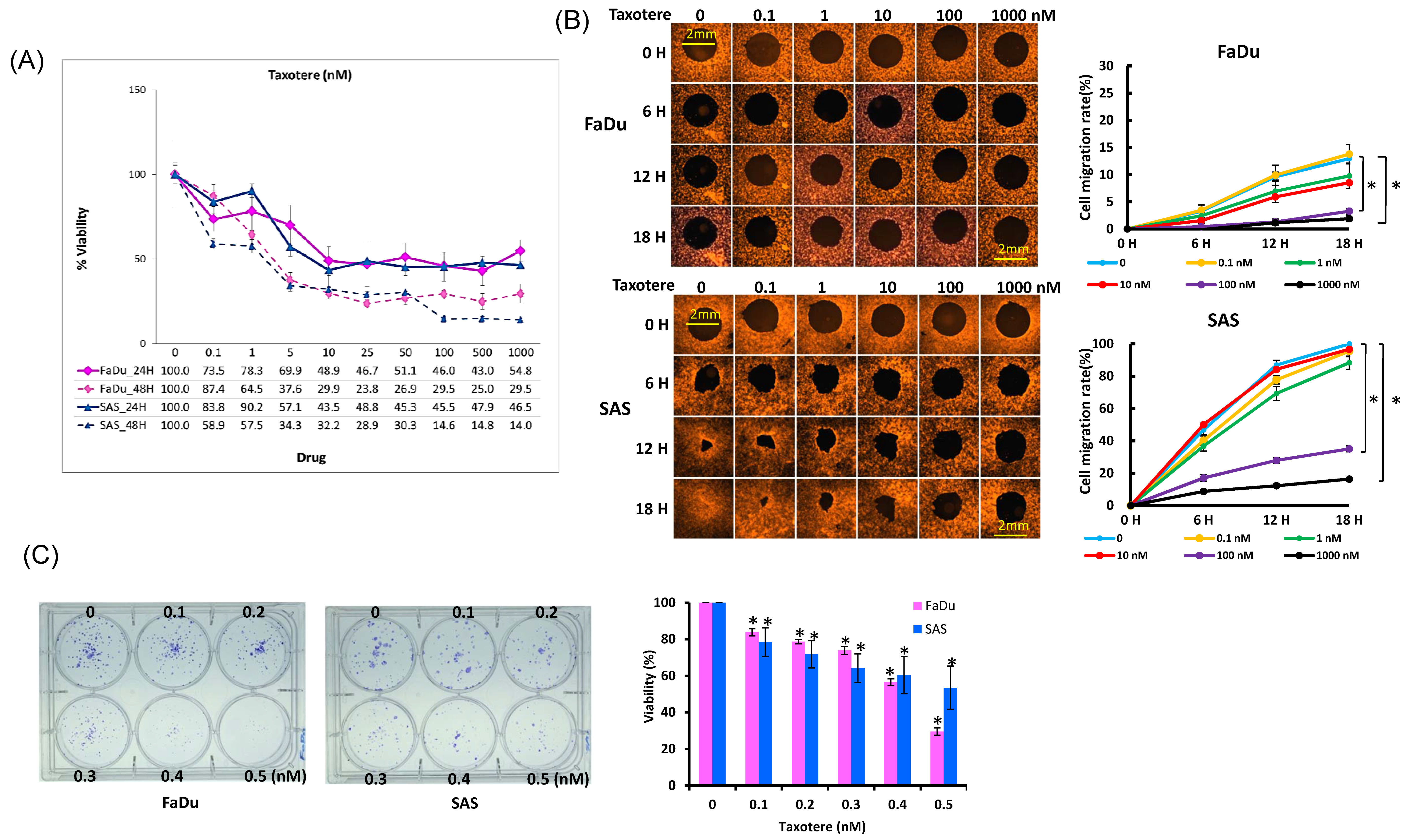
2.3. Cytotoxic Activity of Docetaxel on HNSCC Cell Lines
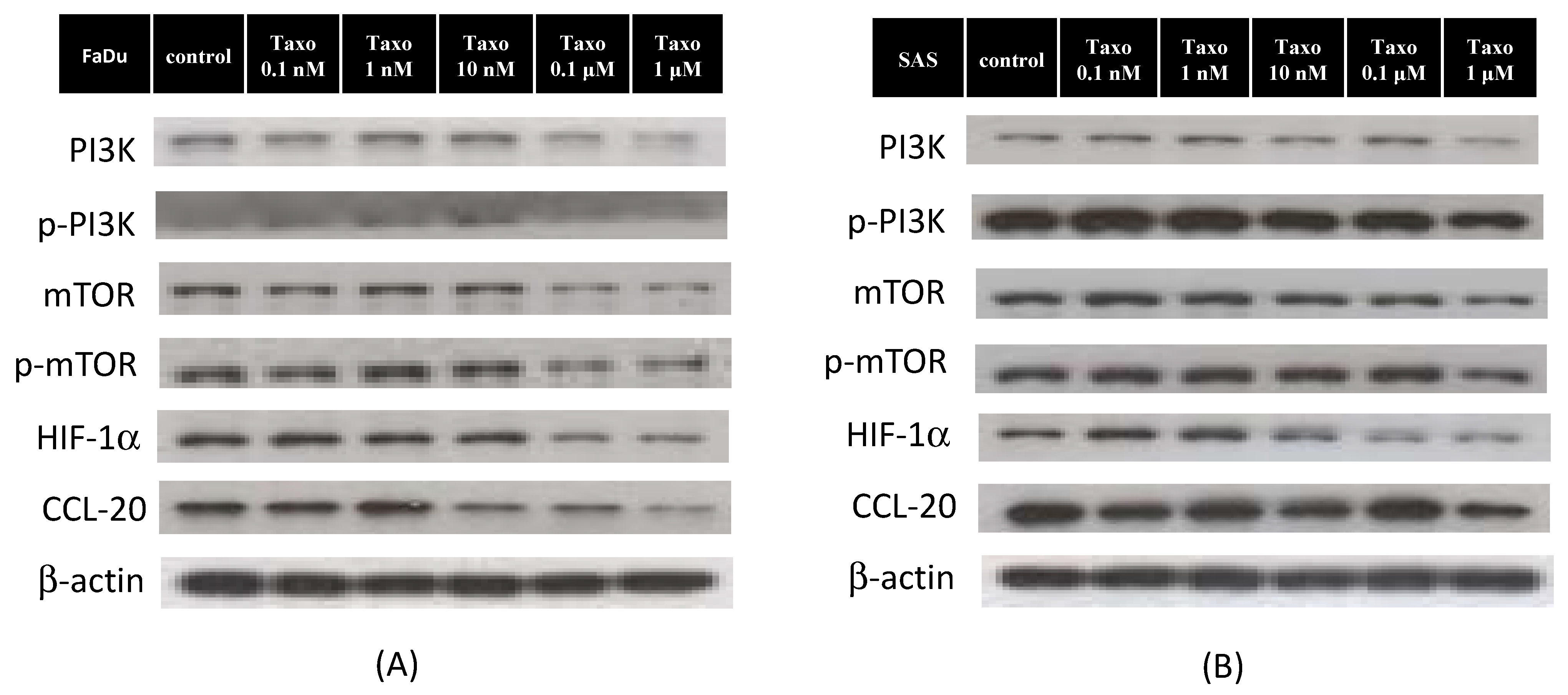
2.4. Docetaxel Inhibits mTOR-CCL20 Expression in HNSCC Cells
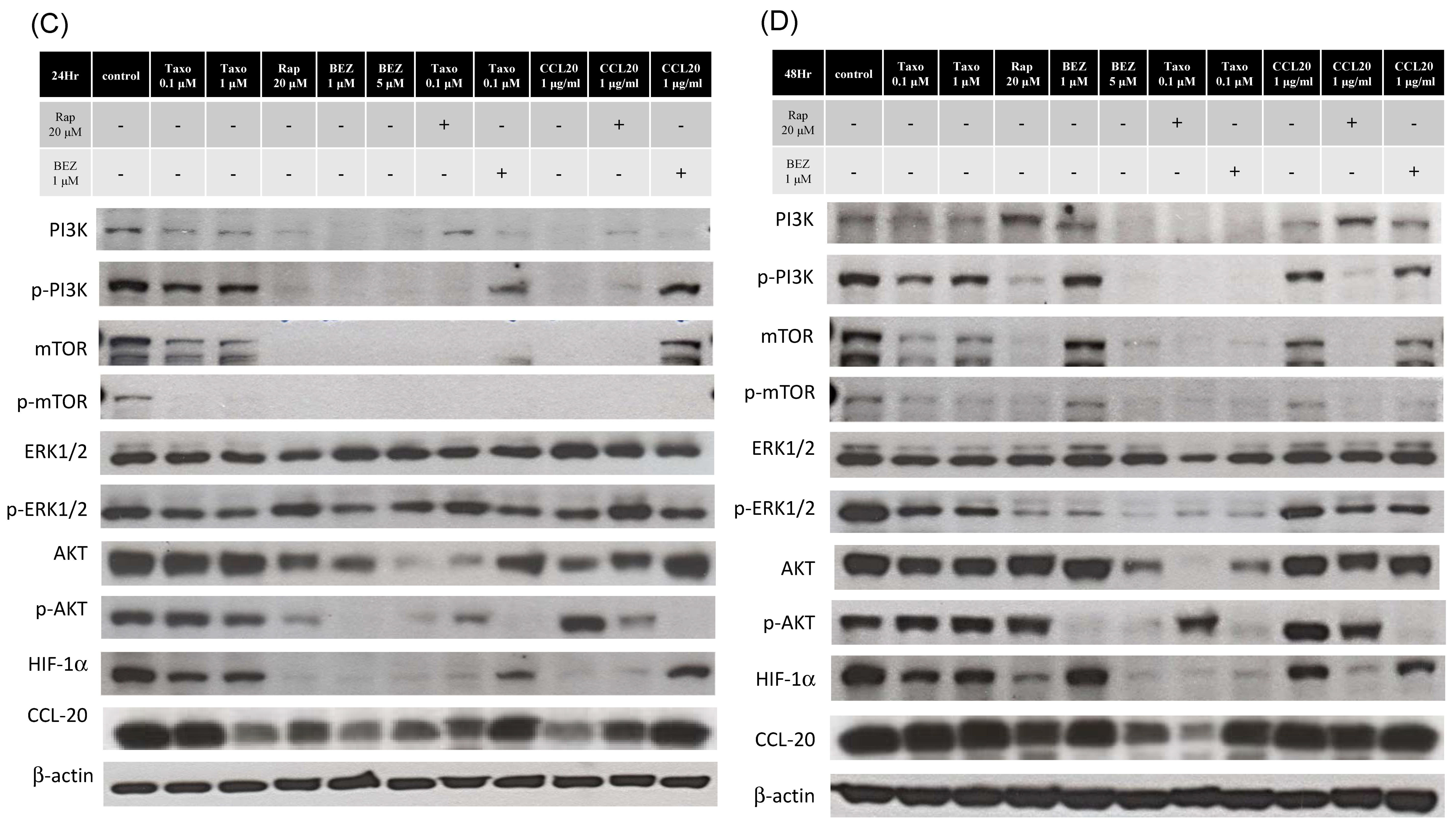
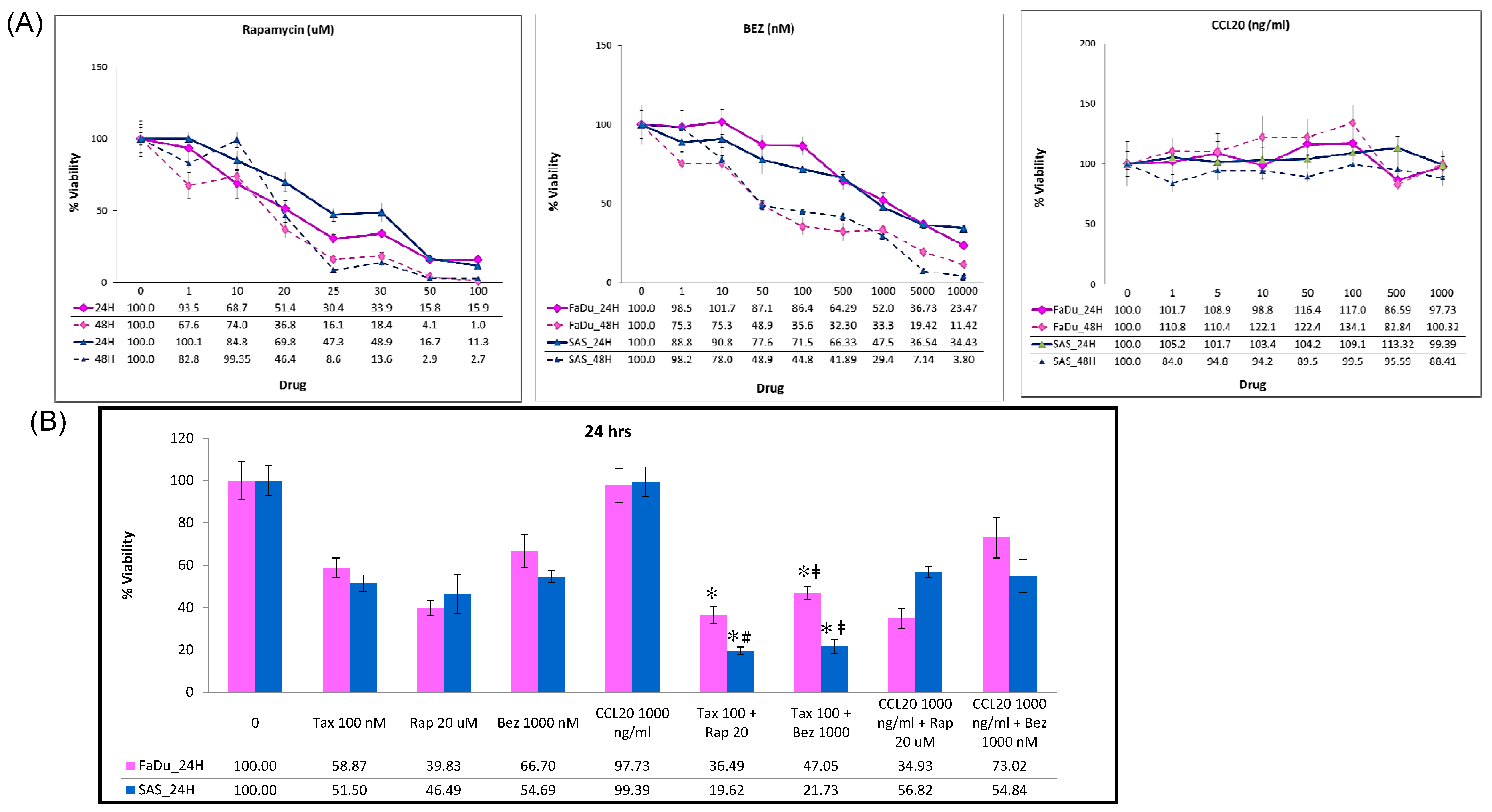
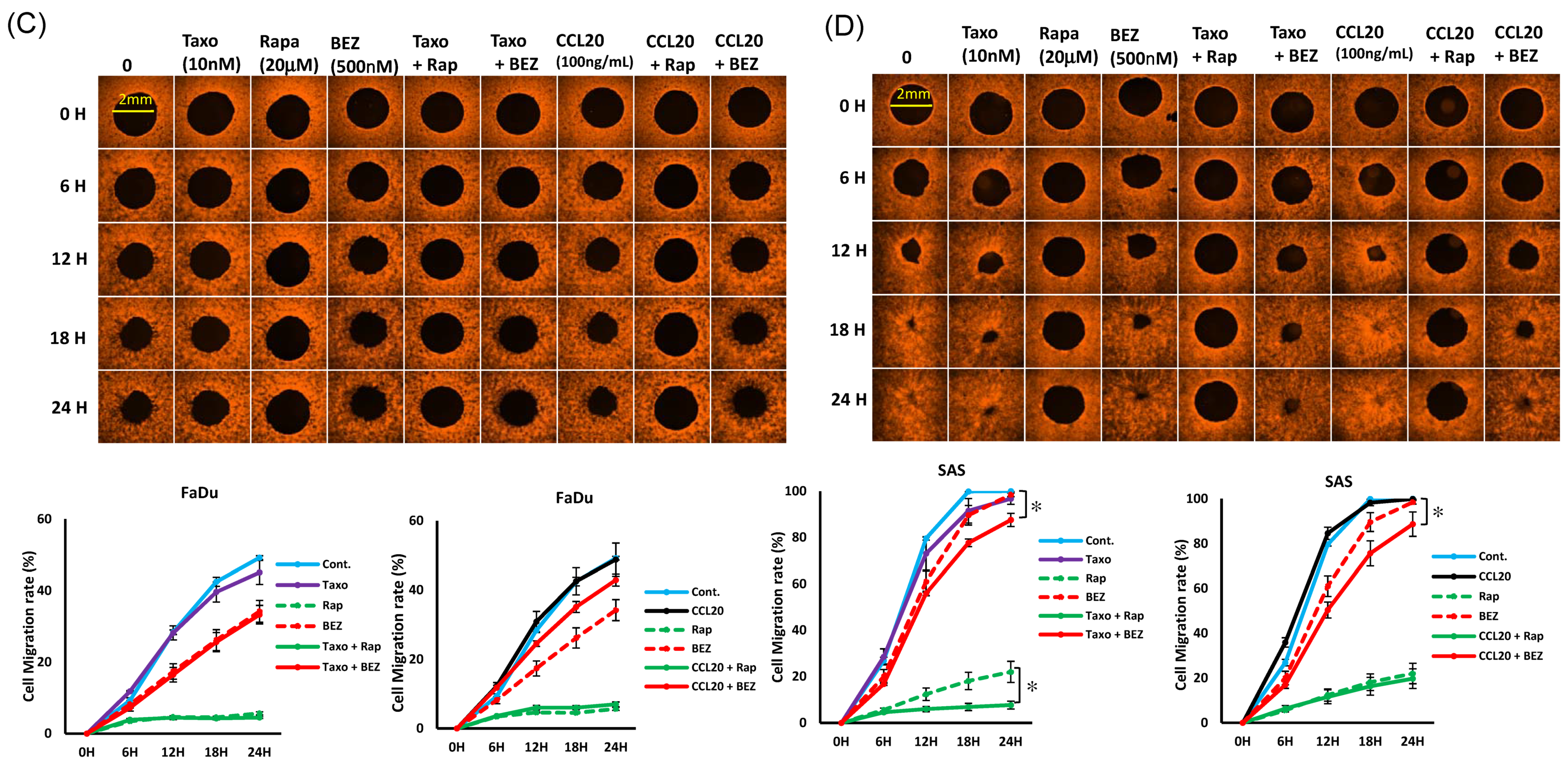
2.5. mTOR Inhibitors Enhance the Effects of Docetaxel to Inhibit PI3K/mTOR/CCL-20 Signaling and HNSCC Cell Proliferation/Migration
3. Discussion
4. Materials and Methods
4.1. HNSCC Cell Cultures
4.2. Cell Growth Assay
4.3. Cell Viability Analysis (WST1)
4.4. Clonogenic Assay
4.5. Western Blot Analysis
4.6. Oris™ Cell Migration Assay
4.7. Animal Care
4.8. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HNSCC | head and neck squamous cell carcinoma |
| GLOBOCAN | Global Cancer Observatory CANCER TODAY |
| CRT | chemoradiation therapy |
| PI3K/AKT/mTOR | phosphoinositide 3-kinase/protein kinase B/mammalian target of rapamycin |
| CCL20 | Chemokine (C-C motif) ligand 20 |
| HIF-1α | Hypoxia-Inducible Factor-1α |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021. [Google Scholar] [CrossRef] [PubMed]
- Hsu, W.-L.; Kelly, J.Y.; Chiang, C.-J.; Chen, T.-C.; Wang, C.-P. Head and Neck Cancer Incidence Trends in Taiwan, 1980–2014. Int. J. Head Neck Sci. 2017, 1, 180–190. [Google Scholar]
- Hung, L.C.; Kung, P.T.; Lung, C.H.; Tsai, M.H.; Liu, S.A.; Chiu, L.T.; Huang, K.H.; Tsai, W.C. Assessment of the Risk of Oral Cancer Incidence in a High-Risk Population and Establishment of a Predictive Model for Oral Cancer Incidence Using a Population-Based Cohort in Taiwan. Int. J. Environ. Res. Public Health 2020, 17. [Google Scholar] [CrossRef] [PubMed]
- Posner, M.R.; Hershock, D.M.; Blajman, C.R.; Mickiewicz, E.; Winquist, E.; Gorbounova, V.; Tjulandin, S.; Shin, D.M.; Cullen, K.; Ervin, T.J.; et al. Cisplatin and fluorouracil alone or with docetaxel in head and neck cancer. N. Engl. J. Med. 2007, 357, 1705–1715. [Google Scholar] [CrossRef]
- Vermorken, J.B.; Remenar, E.; van Herpen, C.; Gorlia, T.; Mesia, R.; Degardin, M.; Stewart, J.S.; Jelic, S.; Betka, J.; Preiss, J.H.; et al. Cisplatin, fluorouracil, and docetaxel in unresectable head and neck cancer. N. Engl. J. Med. 2007, 357, 1695–1704. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, H.; Pammer, J.; Minichsdorfer, C.; Posch, D.; Kornek, G.; Aretin, M.B.; Fuereder, T. Modified biweekly cisplatin, docetaxel plus cetuximab (TPEx) as first-line treatment for patients with recurrent/metastatic head and neck cancer. Med. Oncol. 2018, 35, 32. [Google Scholar] [CrossRef]
- Guigay, J.; Fayette, J.; Dillies, A.F.; Sire, C.; Kerger, J.N.; Tennevet, I.; Machiels, J.P.; Zanetta, S.; Pointreau, Y.; Bozec Le Moal, L.; et al. Cetuximab, docetaxel, and cisplatin as first-line treatment in patients with recurrent or metastatic head and neck squamous cell carcinoma: A multicenter, phase II GORTEC study. Ann. Oncol. 2015, 26, 1941–1947. [Google Scholar] [CrossRef] [PubMed]
- Lui, V.W.; Hedberg, M.L.; Li, H.; Vangara, B.S.; Pendleton, K.; Zeng, Y.; Lu, Y.; Zhang, Q.; Du, Y.; Gilbert, B.R.; et al. Frequent mutation of the PI3K pathway in head and neck cancer defines predictive biomarkers. Cancer Discov. 2013, 3, 761–769. [Google Scholar] [CrossRef]
- Kang, S.; Bader, A.G.; Vogt, P.K. Phosphatidylinositol 3-kinase mutations identified in human cancer are oncogenic. Proc. Natl. Acad. Sci. USA 2005, 102, 802–807. [Google Scholar] [CrossRef]
- Saidak, Z.; Clatot, F.; Chatelain, D.; Galmiche, A. A gene expression profile associated with perineural invasion identifies a subset of HNSCC at risk of post-surgical recurrence. Oral Oncol. 2018, 86, 53–60. [Google Scholar] [CrossRef]
- Xia, Y.; Jiang, L.; Zhong, T. The role of HIF-1alpha in chemo-/radioresistant tumors. Onco Targets Ther. 2018, 11, 3003–3011. [Google Scholar] [CrossRef] [PubMed]
- Guru, S.K.; Pathania, A.S.; Kumar, S.; Ramesh, D.; Kumar, M.; Rana, S.; Kumar, A.; Malik, F.; Sharma, P.R.; Chandan, B.K.; et al. Secalonic Acid-D Represses HIF1alpha/VEGF-Mediated Angiogenesis by Regulating the Akt/mTOR/p70S6K Signaling Cascade. Cancer Res. 2015, 75, 2886–2896. [Google Scholar] [CrossRef]
- Marques, A.E.; Elias, S.T.; Porporatti, A.L.; Castilho, R.M.; Squarize, C.H.; De Luca Canto, G.; Guerra, E.N. mTOR pathway protein immunoexpression as a prognostic factor for survival in head and neck cancer patients: A systematic review and meta-analysis. J. Oral Pathol. Med. 2016, 45, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Jia, Y.; Ma, J.; Wu, S.; Jiang, H.; Cao, Y.; Sun, X.; Yin, X.; Yan, S.; Shang, M.; et al. Tumor-associated macrophage-derived CCL20 enhances the growth and metastasis of pancreatic cancer. Acta Biochim. Biophys. Sin. 2016, 48, 1067–1074. [Google Scholar] [CrossRef] [PubMed]
- Faes, S.; Demartines, N.; Dormond, O. Resistance to mTORC1 Inhibitors in Cancer Therapy: From Kinase Mutations to Intratumoral Heterogeneity of Kinase Activity. Oxid. Med. Cell Longev. 2017, 2017, 1726078. [Google Scholar] [CrossRef] [PubMed]
- Tian, T.; Li, X.; Zhang, J. mTOR Signaling in Cancer and mTOR Inhibitors in Solid Tumor Targeting Therapy. Int. J. Mol. Sci. 2019, 20, 755. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Lewis, C.; Nadel, J.A. CCL20/CCR6 feedback exaggerates epidermal growth factor receptor-dependent MUC5AC mucin production in human airway epithelial (NCI-H292) cells. J. Immunol. 2011, 186, 3392–3400. [Google Scholar] [CrossRef]
- Frick, V.O.; Rubie, C.; Kolsch, K.; Wagner, M.; Ghadjar, P.; Graeber, S.; Glanemann, M. CCR6/CCL20 chemokine expression profile in distinct colorectal malignancies. Scand. J. Immunol. 2013, 78, 298–305. [Google Scholar] [CrossRef]
- Du, D.; Liu, Y.; Qian, H.; Zhang, B.; Tang, X.; Zhang, T.; Liu, W. The effects of the CCR6/CCL20 biological axis on the invasion and metastasis of hepatocellular carcinoma. Int. J. Mol. Sci. 2014, 15, 6441–6452. [Google Scholar] [CrossRef]
- Kapur, N.; Mir, H.; Clark Iii, C.E.; Krishnamurti, U.; Beech, D.J.; Lillard, J.W.; Singh, S. CCR6 expression in colon cancer is associated with advanced disease and supports epithelial-to-mesenchymal transition. Br. J. Cancer 2016, 114, 1343–1351. [Google Scholar] [CrossRef] [PubMed]
- Kadomoto, S.; Izumi, K.; Mizokami, A. The CCL20-CCR6 Axis in Cancer Progression. Int. J. Mol. Sci. 2020, 21, 5186. [Google Scholar] [CrossRef]
- Chen, C.H.; Chuang, H.C.; Lin, Y.T.; Fang, F.M.; Huang, C.C.; Chen, C.M.; Lu, H.; Chien, C.Y. Circulating CD105 shows significant impact in patients of oral cancer and promotes malignancy of cancer cells via CCL20. Tumour Biol. 2016, 37, 1995–2005. [Google Scholar] [CrossRef]
- Chuang, H.C.; Chou, M.H.; Chien, C.Y.; Chuang, J.H.; Liu, Y.L. Triggering TLR3 pathway promotes tumor growth and cisplatin resistance in head and neck cancer cells. Oral. Oncol. 2018, 86, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Myers, J.N.; Holsinger, F.C.; Jasser, S.A.; Bekele, B.N.; Fidler, I.J. An orthotopic nude mouse model of oral tongue squamous cell carcinoma. Clin. Cancer Res. 2002, 8, 293–298. [Google Scholar] [PubMed]
- Haddad, R.I.; Posner, M.; Hitt, R.; Cohen, E.E.W.; Schulten, J.; Lefebvre, J.L.; Vermorken, J.B. Induction chemotherapy in locally advanced squamous cell carcinoma of the head and neck: Role, controversy, and future directions. Ann. Oncol. 2018, 29, 1130–1140. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, Y.; Kuriyama, H.; Umezu, H.; Tanaka, J.; Yoshimasu, T.; Furukawa, T.; Tanaka, H.; Kagamu, H.; Gejyo, F.; Yoshizawa, H. Class III beta-tubulin expression in tumor cells is correlated with resistance to docetaxel in patients with completely resected non-small-cell lung cancer. Intern. Med. 2009, 48, 203–208. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kulkarni, S.A.; Hicks, D.G.; Watroba, N.L.; Murekeyisoni, C.; Hwang, H.; Khoury, T.; Beck, R.A.; Ring, B.Z.; Estopinal, N.C.; Schreeder, M.T.; et al. TLE3 as a candidate biomarker of response to taxane therapy. Breast Cancer Res. 2009, 11, R17. [Google Scholar] [CrossRef]
- Molinolo, A.A.; Hewitt, S.M.; Amornphimoltham, P.; Keelawat, S.; Rangdaeng, S.; Meneses Garcia, A.; Raimondi, A.R.; Jufe, R.; Itoiz, M.; Gao, Y.; et al. Dissecting the Akt/mammalian target of rapamycin signaling network: Emerging results from the head and neck cancer tissue array initiative. Clin. Cancer Res. 2007, 13, 4964–4973. [Google Scholar] [CrossRef] [PubMed]
- Lionello, M.; Blandamura, S.; Loreggian, L.; Ottaviano, G.; Giacomelli, L.; Marchese-Ragona, R.; Velardita, C.; Staffieri, A.; Marioni, G. High mTOR expression is associated with a worse oncological outcome in laryngeal carcinoma treated with postoperative radiotherapy: A pilot study. J. Oral. Pathol. Med. 2012, 41, 136–140. [Google Scholar] [CrossRef]
- Zaytseva, Y.Y.; Valentino, J.D.; Gulhati, P.; Evers, B.M. mTOR inhibitors in cancer therapy. Cancer Lett. 2012, 319, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, S.A.; Walker, D.; Gillespie, M.B.; Gutkind, J.S.; Day, T.A. mTOR inhibitors and its role in the treatment of head and neck squamous cell carcinoma. Curr. Treat. Opt. Oncol. 2012, 13, 71–81. [Google Scholar] [CrossRef] [PubMed]
- Day, T.A.; Shirai, K.; O’Brien, P.E.; Matheus, M.G.; Godwin, K.; Sood, A.J.; Kompelli, A.; Vick, J.A.; Martin, D.; Vitale-Cross, L.; et al. Inhibition of mTOR Signaling and Clinical Activity of Rapamycin in Head and Neck Cancer in a Window of Opportunity Trial. Clin. Cancer Res. 2019, 25, 1156–1164. [Google Scholar] [CrossRef]
- Kozakiewicz, P.; Grzybowska-Szatkowska, L. Application of molecular targeted therapies in the treatment of head and neck squamous cell carcinoma. Oncol. Lett. 2018, 15, 7497–7505. [Google Scholar] [CrossRef] [PubMed]
- Gao, W.; Li, J.Z.; Chan, J.Y.; Ho, W.K.; Wong, T.S. mTOR Pathway and mTOR Inhibitors in Head and Neck Cancer. ISRN Otolaryngol. 2012, 2012, 953089. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Luo, Y.; Huang, S. Updates of mTOR inhibitors. Anticancer Agents Med. Chem. 2010, 10, 571–581. [Google Scholar] [CrossRef]
- Ekshyyan, O.; Moore-Medlin, T.N.; Raley, M.C.; Sonavane, K.; Rong, X.; Brodt, M.A.; Abreo, F.; Alexander, J.S.; Nathan, C.A. Anti-lymphangiogenic properties of mTOR inhibitors in head and neck squamous cell carcinoma experimental models. BMC Cancer 2013, 13, 320. [Google Scholar] [CrossRef]
- Pal, I.; Mandal, M. PI3K and Akt as molecular targets for cancer therapy: Current clinical outcomes. Acta Pharmacol. Sin. 2012, 33, 1441–1458. [Google Scholar] [CrossRef]
- O’Brien, N.A.; McDonald, K.; Tong, L.; von Euw, E.; Kalous, O.; Conklin, D.; Hurvitz, S.A.; di Tomaso, E.; Schnell, C.; Linnartz, R.; et al. Targeting PI3K/mTOR overcomes resistance to HER2-targeted therapy independent of feedback activation of AKT. Clin. Cancer Res. 2014, 20, 3507–3520. [Google Scholar] [CrossRef]
- Saxton, R.A.; Sabatini, D.M. mTOR Signaling in Growth, Metabolism, and Disease. Cell 2017, 168, 960–976. [Google Scholar] [CrossRef]
- Zhang, Z.; Yao, L.; Yang, J.; Wang, Z.; Du, G. PI3K/Akt and HIF1 signaling pathway in hypoxiaischemia (Review). Mol. Med. Rep. 2018, 18, 3547–3554. [Google Scholar] [CrossRef]
- Yang, X.M.; Wang, Y.S.; Zhang, J.; Li, Y.; Xu, J.F.; Zhu, J.; Zhao, W.; Chu, D.K.; Wiedemann, P. Role of PI3K/Akt and MEK/ERK in mediating hypoxia-induced expression of HIF-1alpha and VEGF in laser-induced rat choroidal neovascularization. Investig. Ophthalmol. Vis. Sci. 2009, 50, 1873–1879. [Google Scholar] [CrossRef] [PubMed]
- Karar, J.; Cerniglia, G.J.; Lindsten, T.; Koumenis, C.; Maity, A. Dual PI3K/mTOR inhibitor NVP-BEZ235 suppresses hypoxia-inducible factor (HIF)-1alpha expression by blocking protein translation and increases cell death under hypoxia. Cancer Biol. Ther. 2012, 13, 1102–1111. [Google Scholar] [CrossRef] [PubMed]
- Chu, H.; Jia, B.; Qiu, X.; Pan, J.; Sun, X.; Wang, Z.; Zhao, J. Investigation of proliferation and migration of tongue squamous cell carcinoma promoted by three chemokines, MIP-3alpha, MIP-1beta, and IP-10. Onco Targets Ther. 2017, 10, 4193–4203. [Google Scholar] [CrossRef] [PubMed]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chou, M.-H.; Chuang, H.-C.; Lin, Y.-T.; Tsai, M.-H.; Kao, Y.-H.; Lin, I.-C.; Huang, T.-L.; Fang, F.-M.; Chien, C.-Y. Targeting mTOR-CCL20 Signaling May Improve Response to Docetaxel in Head and Neck Squamous Cell Carcinoma. Int. J. Mol. Sci. 2021, 22, 3046. https://doi.org/10.3390/ijms22063046
Chou M-H, Chuang H-C, Lin Y-T, Tsai M-H, Kao Y-H, Lin I-C, Huang T-L, Fang F-M, Chien C-Y. Targeting mTOR-CCL20 Signaling May Improve Response to Docetaxel in Head and Neck Squamous Cell Carcinoma. International Journal of Molecular Sciences. 2021; 22(6):3046. https://doi.org/10.3390/ijms22063046
Chicago/Turabian StyleChou, Ming-Huei, Hui-Ching Chuang, Yu-Tsai Lin, Ming-Hsien Tsai, Ying-Hsien Kao, I-Chun Lin, Tai-Lin Huang, Fu-Min Fang, and Chih-Yen Chien. 2021. "Targeting mTOR-CCL20 Signaling May Improve Response to Docetaxel in Head and Neck Squamous Cell Carcinoma" International Journal of Molecular Sciences 22, no. 6: 3046. https://doi.org/10.3390/ijms22063046
APA StyleChou, M.-H., Chuang, H.-C., Lin, Y.-T., Tsai, M.-H., Kao, Y.-H., Lin, I.-C., Huang, T.-L., Fang, F.-M., & Chien, C.-Y. (2021). Targeting mTOR-CCL20 Signaling May Improve Response to Docetaxel in Head and Neck Squamous Cell Carcinoma. International Journal of Molecular Sciences, 22(6), 3046. https://doi.org/10.3390/ijms22063046






