Striking Back against Fungal Infections: The Utilization of Nanosystems for Antifungal Strategies
Abstract
1. Fungal Infection
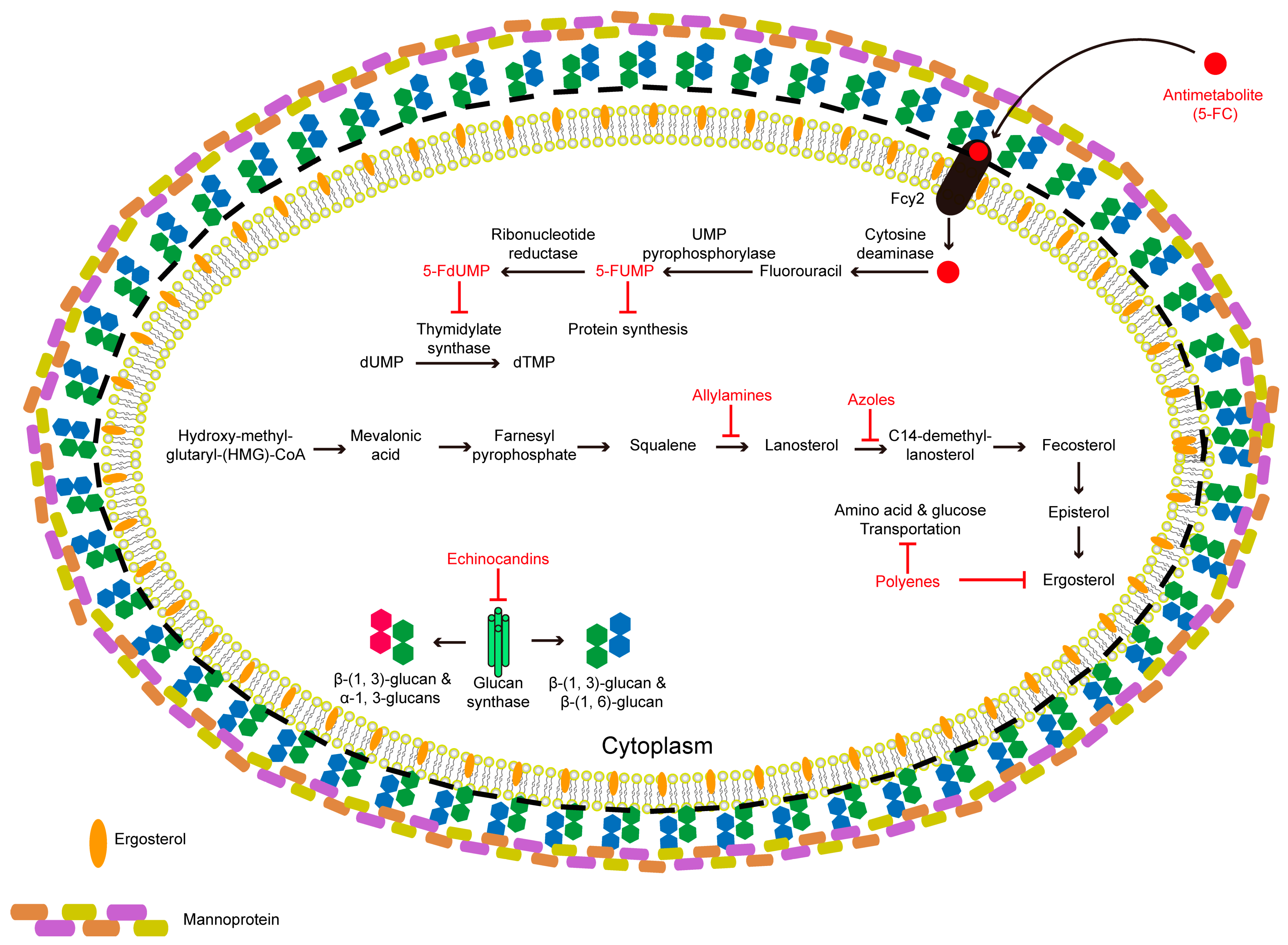
2. Conventional Treatments for Candidiasis, Cryptococcosis, and Aspergillosis
3. Unsatisfactory Properties of Currently Used Antifungal Drugs
4. Nanotechnology-Based Therapies for Fungal Infections
5. Metallic Nanoparticles
6. Mesoporous Silica Nanoparticles
7. Polymeric Nanoparticles
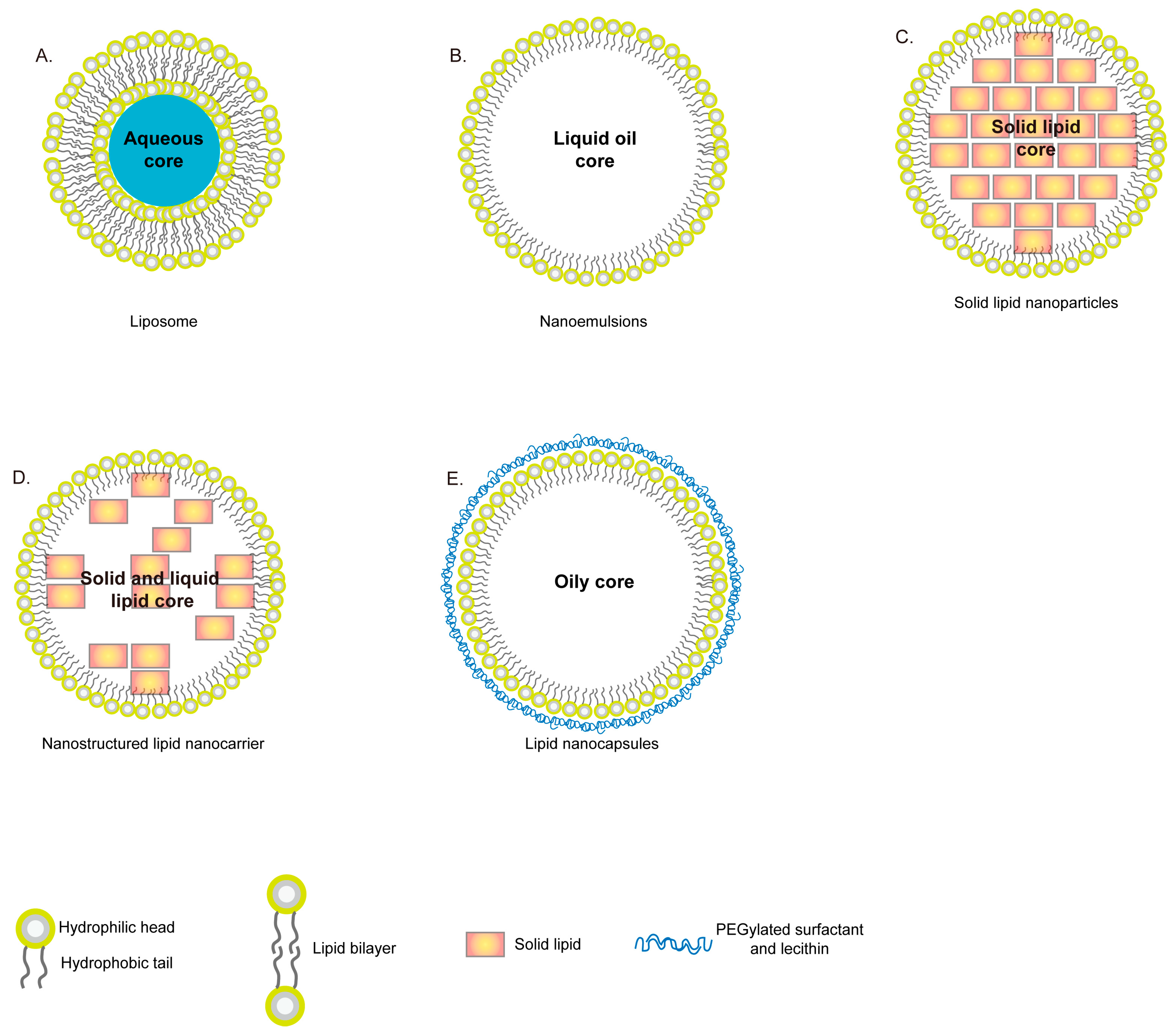
8. Lipid Based Nanoparticles
9. Conclusions and Perspectives
Funding
Conflicts of Interest
References
- One Health: Fungal Pathogens of Humans, Animals, and Plants: Report on an American Academy of Microbiology Colloquium held in Washington, DC, on 18 October 2017; American Society for Microbiology: Washington, DC, USA, 2019. [CrossRef]
- Brown, G.D.; Denning, D.W.; Gow, N.A.; Levitz, S.M.; Netea, M.G.; White, T.C. Hidden killers: Human fungal infections. Sci. Transl. Med. 2012, 4, 165rv113. [Google Scholar] [CrossRef] [PubMed]
- Brown, G.D.; Denning, D.W.; Levitz, S.M. Tackling human fungal infections. Science 2012, 336, 647. [Google Scholar] [CrossRef]
- Kohler, J.R.; Hube, B.; Puccia, R.; Casadevall, A.; Perfect, J.R. Fungi that Infect Humans. Microbiol. Spectr. 2017, 5, 813–843. [Google Scholar] [CrossRef]
- Denning, D.W.; Kneale, M.; Sobel, J.D.; Rautemaa-Richardson, R. Global burden of recurrent vulvovaginal candidiasis: A systematic review. Lancet Infect. Dis. 2018, 18, e339–e347. [Google Scholar] [CrossRef]
- Singh, M.; Paul, N.; Singh, S.; Nayak, G.R. Asthma and Fungus: Role in Allergic Bronchopulmonary Aspergillosis (ABPA) and Other Conditions. Indian J. Pediatr. 2018, 85, 899–904. [Google Scholar] [CrossRef]
- Carevic, M.; Singh, A.; Rieber, N.; Eickmeier, O.; Griese, M.; Hector, A.; Hartl, D. CXCR4+ granulocytes reflect fungal cystic fibrosis lung disease. Eur. Respir. J. 2015, 46, 395–404. [Google Scholar] [CrossRef]
- Chotirmall, S.H.; McElvaney, N.G. Fungi in the cystic fibrosis lung: Bystanders or pathogens? Int. J. Biochem. Cell Biol. 2014, 52, 161–173. [Google Scholar] [CrossRef]
- Denning, D.W.; Chakrabarti, A. Pulmonary and sinus fungal diseases in non-immunocompromised patients. Lancet Infect. Dis. 2017, 17, e357–e366. [Google Scholar] [CrossRef]
- Tyler, M.A.; Lam, K.; Marino, M.J.; Yao, W.C.; Schmale, I.; Citardi, M.J.; Luong, A.U. Revisiting the controversy: The role of fungi in chronic rhinosinusitis. Int. Forum Allergy Rhinol. 2021. [Google Scholar] [CrossRef] [PubMed]
- McCarty, T.P.; Pappas, P.G. Invasive Candidiasis. Infect. Dis. Clin. N. Am. 2016, 30, 103–124. [Google Scholar] [CrossRef]
- Pappas, P.G.; Rex, J.H.; Lee, J.; Hamill, R.J.; Larsen, R.A.; Powderly, W.; Kauffman, C.A.; Hyslop, N.; Mangino, J.E.; Chapman, S.; et al. A prospective observational study of candidemia: Epidemiology, therapy, and influences on mortality in hospitalized adult and pediatric patients. Clin. Infect. Dis. 2003, 37, 634–643. [Google Scholar] [CrossRef] [PubMed]
- Kullberg, B.J.; Arendrup, M.C. Invasive Candidiasis. N. Engl. J. Med. 2015, 373, 1445–1456. [Google Scholar] [CrossRef] [PubMed]
- Wisplinghoff, H.; Bischoff, T.; Tallent, S.M.; Seifert, H.; Wenzel, R.P.; Edmond, M.B. Nosocomial bloodstream infections in US hospitals: Analysis of 24,179 cases from a prospective nationwide surveillance study. Clin. Infect. Dis. 2004, 39, 309–317. [Google Scholar] [CrossRef]
- Spivak, E.S.; Hanson, K.E. Candida auris: An Emerging Fungal Pathogen. J. Clin. Microbiol. 2018, 56, e01588-17. [Google Scholar] [CrossRef] [PubMed]
- Chowdhary, A.; Sharma, C.; Meis, J.F. Candida auris: A rapidly emerging cause of hospital-acquired multidrug-resistant fungal infections globally. PLoS Pathog. 2017, 13, e1006290. [Google Scholar] [CrossRef] [PubMed]
- Lockhart, S.R.; Etienne, K.A.; Vallabhaneni, S.; Farooqi, J.; Chowdhary, A.; Govender, N.P.; Colombo, A.L.; Calvo, B.; Cuomo, C.A.; Desjardins, C.A.; et al. Simultaneous Emergence of Multidrug-Resistant Candida auris on 3 Continents Confirmed by Whole-Genome Sequencing and Epidemiological Analyses. Clin. Infect. Dis. 2017, 64, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Clancy, C.J.; Nguyen, M.H. Emergence of Candida auris: An International Call to Arms. Clin. Infect. Dis. 2017, 64, 141–143. [Google Scholar] [CrossRef]
- Chan, J.F.; Lau, S.K.; Yuen, K.Y.; Woo, P.C. Talaromyces (Penicillium) marneffei infection in non-HIV-infected patients. Emerg. Microbes Infect. 2016, 5, e19. [Google Scholar] [CrossRef]
- Latge, J.P.; Chamilos, G. Aspergillus fumigatus and Aspergillosis in 2019. Clin. Microbiol. Rev. 2019, 33, e00140-18. [Google Scholar] [CrossRef]
- Pappas, P.G. Invasive candidiasis. Infect. Dis. Clin. N. Am. 2006, 20, 485–506. [Google Scholar] [CrossRef]
- Binder, U.; Maurer, E.; Lass-Florl, C. Mucormycosis—From the pathogens to the disease. Clin. Microbiol. Infect. 2014, 20, 60–66. [Google Scholar] [CrossRef]
- Saha, D.C.; Goldman, D.L.; Shao, X.; Casadevall, A.; Husain, S.; Limaye, A.P.; Lyon, M.; Somani, J.; Pursell, K.; Pruett, T.L.; et al. Serologic evidence for reactivation of cryptococcosis in solid-organ transplant recipients. Clin. Vaccine Immunol. 2007, 14, 1550–1554. [Google Scholar] [CrossRef] [PubMed]
- Springer, D.J.; Billmyre, R.B.; Filler, E.E.; Voelz, K.; Pursall, R.; Mieczkowski, P.A.; Larsen, R.A.; Dietrich, F.S.; May, R.C.; Filler, S.G.; et al. Cryptococcus gattii VGIII isolates causing infections in HIV/AIDS patients in Southern California: Identification of the local environmental source as arboreal. PLoS Pathog. 2014, 10, e1004285. [Google Scholar] [CrossRef] [PubMed]
- Litvintseva, A.P.; Carbone, I.; Rossouw, J.; Thakur, R.; Govender, N.P.; Mitchell, T.G. Evidence that the human pathogenic fungus Cryptococcus neoformans var. grubii may have evolved in Africa. PLoS ONE 2011, 6, e19688. [Google Scholar] [CrossRef]
- Baddley, J.W.; Schain, D.C.; Gupte, A.A.; Lodhi, S.A.; Kayler, L.K.; Frade, J.P.; Lockhart, S.R.; Chiller, T.; Bynon, J.S., Jr.; Bower, W.A. Transmission of Cryptococcus neoformans by Organ Transplantation. Clin. Infect. Dis. 2011, 52, e94–e98. [Google Scholar] [CrossRef]
- Garcia-Hermoso, D.; Janbon, G.; Dromer, F. Epidemiological evidence for dormant Cryptococcus neoformans infection. J. Clin. Microbiol. 1999, 37, 3204–3209. [Google Scholar] [CrossRef]
- Stephen, C.; Lester, S.; Black, W.; Fyfe, M.; Raverty, S. Multispecies outbreak of cryptococcosis on southern Vancouver Island, British Columbia. Can. Vet. J. 2002, 43, 792–794. [Google Scholar] [PubMed]
- Kidd, S.E.; Hagen, F.; Tscharke, R.L.; Huynh, M.; Bartlett, K.H.; Fyfe, M.; Macdougall, L.; Boekhout, T.; Kwon-Chung, K.J.; Meyer, W. A rare genotype of Cryptococcus gattii caused the cryptococcosis outbreak on Vancouver Island (British Columbia, Canada). Proc. Natl. Acad. Sci. USA 2004, 101, 17258–17263. [Google Scholar] [CrossRef]
- Kidd, S.E.; Guo, H.; Bartlett, K.H.; Xu, J.; Kronstad, J.W. Comparative gene genealogies indicate that two clonal lineages of Cryptococcus gattii in British Columbia resemble strains from other geographical areas. Eukaryot Cell 2005, 4, 1629–1638. [Google Scholar] [CrossRef]
- Byrnes, E.J., 3rd; Bildfell, R.J.; Dearing, P.L.; Valentine, B.A.; Heitman, J. Cryptococcus gattii with bimorphic colony types in a dog in western Oregon: Additional evidence for expansion of the Vancouver Island outbreak. J. Vet. Diagn. Invest. 2009, 21, 133–136. [Google Scholar] [CrossRef]
- Byrnes, E.J., 3rd; Bildfell, R.J.; Frank, S.A.; Mitchell, T.G.; Marr, K.A.; Heitman, J. Molecular evidence that the range of the Vancouver Island outbreak of Cryptococcus gattii infection has expanded into the Pacific Northwest in the United States. J. Infect. Dis. 2009, 199, 1081–1086. [Google Scholar] [CrossRef]
- Byrnes, E.J.; Heitman, J. Cryptococcus gattii outbreak expands into the Northwestern United States with fatal consequences. F1000 Biol. Rep. 2009, 1, 62. [Google Scholar] [CrossRef]
- Byrnes, E.J., 3rd; Li, W.; Lewit, Y.; Perfect, J.R.; Carter, D.A.; Cox, G.M.; Heitman, J. First reported case of Cryptococcus gattii in the Southeastern USA: Implications for travel-associated acquisition of an emerging pathogen. PLoS ONE 2009, 4, e5851. [Google Scholar] [CrossRef]
- Datta, K.; Bartlett, K.H.; Baer, R.; Byrnes, E.; Galanis, E.; Heitman, J.; Hoang, L.; Leslie, M.J.; MacDougall, L.; Magill, S.S.; et al. Spread of Cryptococcus gattii into Pacific Northwest region of the United States. Emerg. Infect. Dis. 2009, 15, 1185–1191. [Google Scholar] [CrossRef]
- Engelthaler, D.M.; Casadevall, A. On the Emergence of Cryptococcus gattii in the Pacific Northwest: Ballast Tanks, Tsunamis, and Black Swans. mBio 2019, 10, e02193-19. [Google Scholar] [CrossRef] [PubMed]
- Chowdhary, A.; Rhandhawa, H.S.; Prakash, A.; Meis, J.F. Environmental prevalence of Cryptococcus neoformans and Cryptococcus gattii in India: An update. Crit. Rev. Microbiol. 2012, 38, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Steenbergen, J.N.; Shuman, H.A.; Casadevall, A. Cryptococcus neoformans interactions with amoebae suggest an explanation for its virulence and intracellular pathogenic strategy in macrophages. Proc. Natl. Acad. Sci. USA 2001, 98, 15245–15250. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Croudace, J.E.; Lammas, D.A.; May, R.C. Expulsion of live pathogenic yeast by macrophages. Curr. Biol. 2006, 16, 2156–2160. [Google Scholar] [CrossRef]
- Alvarez, M.; Casadevall, A. Phagosome extrusion and host-cell survival after Cryptococcus neoformans phagocytosis by macrophages. Curr. Biol. 2006, 16, 2161–2165. [Google Scholar] [CrossRef]
- Bloom, A.L.M.; Jin, R.M.; Leipheimer, J.; Bard, J.E.; Yergeau, D.; Wohlfert, E.A.; Panepinto, J.C. Thermotolerance in the pathogen Cryptococcus neoformans is linked to antigen masking via mRNA decay-dependent reprogramming. Nat. Commun. 2019, 10, 4950. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Casadevall, A. Decreased susceptibility of melanized Cryptococcus neoformans to UV light. Appl. Environ. Microbiol. 1994, 60, 3864–3866. [Google Scholar] [CrossRef] [PubMed]
- May, R.C.; Stone, N.R.; Wiesner, D.L.; Bicanic, T.; Nielsen, K. Cryptococcus: From environmental saprophyte to global pathogen. Nat. Rev. Microbiol. 2016, 14, 106–117. [Google Scholar] [CrossRef] [PubMed]
- Rajasingham, R.; Rhein, J.; Klammer, K.; Musubire, A.; Nabeta, H.; Akampurira, A.; Mossel, E.C.; Williams, D.A.; Boxrud, D.J.; Crabtree, M.B.; et al. Epidemiology of meningitis in an HIV-infected Ugandan cohort. Am. J. Trop. Med. Hyg. 2015, 92, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Jarvis, J.N.; Meintjes, G.; Williams, A.; Brown, Y.; Crede, T.; Harrison, T.S. Adult meningitis in a setting of high HIV and TB prevalence: Findings from 4961 suspected cases. BMC Infect. Dis. 2010, 10, 67. [Google Scholar] [CrossRef] [PubMed]
- Honda, H.; Warren, D.K. Central nervous system infections: Meningitis and brain abscess. Infect. Dis. Clin. N. Am. 2009, 23, 609–623. [Google Scholar] [CrossRef]
- Mortensen, K.L.; Johansen, H.K.; Fuursted, K.; Knudsen, J.D.; Gahrn-Hansen, B.; Jensen, R.H.; Howard, S.J.; Arendrup, M.C. A prospective survey of Aspergillus spp. in respiratory tract samples: Prevalence, clinical impact and antifungal susceptibility. Eur. J. Clin. Microbiol. Infect. Dis. 2011, 30, 1355–1363. [Google Scholar] [CrossRef]
- Nguyen, L.D.; Viscogliosi, E.; Delhaes, L. The lung mycobiome: An emerging field of the human respiratory microbiome. Front. Microbiol. 2015, 6, 89. [Google Scholar] [CrossRef]
- Maiz, L.; Vendrell, M.; Olveira, C.; Giron, R.; Nieto, R.; Martinez-Garcia, M.A. Prevalence and factors associated with isolation of Aspergillus and Candida from sputum in patients with non-cystic fibrosis bronchiectasis. Respiration 2015, 89, 396–403. [Google Scholar] [CrossRef]
- Pashley, C.H.; Fairs, A.; Morley, J.P.; Tailor, S.; Agbetile, J.; Bafadhel, M.; Brightling, C.E.; Wardlaw, A.J. Routine processing procedures for isolating filamentous fungi from respiratory sputum samples may underestimate fungal prevalence. Med. Mycol. 2012, 50, 433–438. [Google Scholar] [CrossRef]
- Denning, D.W.; Park, S.; Lass-Florl, C.; Fraczek, M.G.; Kirwan, M.; Gore, R.; Smith, J.; Bueid, A.; Moore, C.B.; Bowyer, P.; et al. High-frequency triazole resistance found In nonculturable Aspergillus fumigatus from lungs of patients with chronic fungal disease. Clin. Infect. Dis. 2011, 52, 1123–1129. [Google Scholar] [CrossRef]
- Perfect, J.R.; Cox, G.M.; Lee, J.Y.; Kauffman, C.A.; de Repentigny, L.; Chapman, S.W.; Morrison, V.A.; Pappas, P.; Hiemenz, J.W.; Stevens, D.A.; et al. The impact of culture isolation of Aspergillus species: A hospital-based survey of Aspergillosis. Clin. Infect. Dis. 2001, 33, 1824–1833. [Google Scholar] [CrossRef]
- Abdel Hameed, A.A.; Yasser, I.H.; Khoder, I.M. Indoor air quality during renovation actions: A case study. J. Environ. Monit. 2004, 6, 740–744. [Google Scholar] [CrossRef]
- Mahieu, L.M.; De Dooy, J.J.; Van Laer, F.A.; Jansens, H.; Ieven, M.M. A prospective study on factors influencing aspergillus spore load in the air during renovation works in a neonatal intensive care unit. J. Hosp. Infect. 2000, 45, 191–197. [Google Scholar] [CrossRef]
- Pini, G.; Faggi, E.; Donato, R.; Sacco, C.; Fanci, R. Invasive pulmonary aspergillosis in neutropenic patients and the influence of hospital renovation. Mycoses 2008, 51, 117–122. [Google Scholar] [CrossRef]
- Van de Veerdonk, F.L.; Gresnigt, M.S.; Romani, L.; Netea, M.G.; Latge, J.P. Aspergillus fumigatus morphology and dynamic host interactions. Nat. Rev. Microbiol. 2017, 15, 661–674. [Google Scholar] [CrossRef]
- Gago, S.; Overton, N.L.D.; Ben-Ghazzi, N.; Novak-Frazer, L.; Read, N.D.; Denning, D.W.; Bowyer, P. Lung colonization by Aspergillus fumigatus is controlled by ZNF77. Nat. Commun. 2018, 9, 3835. [Google Scholar] [CrossRef] [PubMed]
- Pouliot, M.; Jeanmart, S. Pan Assay Interference Compounds (PAINS) and Other Promiscuous Compounds in Antifungal Research. J. Med. Chem. 2016, 59, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, R.S.; Robbins, N.; Cowen, L.E. Regulatory circuitry governing fungal development, drug resistance, and disease. Microbiol. Mol. Biol. Rev. 2011, 75, 213–267. [Google Scholar] [CrossRef] [PubMed]
- Vincent, B.M.; Lancaster, A.K.; Scherz-Shouval, R.; Whitesell, L.; Lindquist, S. Fitness trade-offs restrict the evolution of resistance to amphotericin B. PLoS Biol. 2013, 11, e1001692. [Google Scholar] [CrossRef]
- Revie, N.M.; Iyer, K.R.; Robbins, N.; Cowen, L.E. Antifungal drug resistance: Evolution, mechanisms and impact. Curr. Opin. Microbiol. 2018, 45, 70–76. [Google Scholar] [CrossRef]
- O’Meara, T.R.; Alspaugh, J.A. The Cryptococcus neoformans capsule: A sword and a shield. Clin. Microbiol. Rev. 2012, 25, 387–408. [Google Scholar] [CrossRef] [PubMed]
- Gow, N.A.R.; Latge, J.P.; Munro, C.A. The Fungal Cell Wall: Structure, Biosynthesis, and Function. Microbiol. Spectr. 2017, 5, 267–292. [Google Scholar] [CrossRef]
- Bowman, S.M.; Free, S.J. The structure and synthesis of the fungal cell wall. Bioessays 2006, 28, 799–808. [Google Scholar] [CrossRef]
- Latge, J.P.; Beauvais, A.; Chamilos, G. The Cell Wall of the Human Fungal Pathogen Aspergillus fumigatus: Biosynthesis, Organization, Immune Response, and Virulence. Annu. Rev. Microbiol. 2017, 71, 99–116. [Google Scholar] [CrossRef]
- Douglas, L.M.; Konopka, J.B. Fungal membrane organization: The eisosome concept. Annu. Rev. Microbiol. 2014, 68, 377–393. [Google Scholar] [CrossRef]
- Klemptner, R.L.; Sherwood, J.S.; Tugizimana, F.; Dubery, I.A.; Piater, L.A. Ergosterol, an orphan fungal microbe-associated molecular pattern (MAMP). Mol. Plant. Pathol. 2014, 15, 747–761. [Google Scholar] [CrossRef]
- Sheehan, D.J.; Hitchcock, C.A.; Sibley, C.M. Current and emerging azole antifungal agents. Clin. Microbiol. Rev. 1999, 12, 40–79. [Google Scholar] [CrossRef] [PubMed]
- Carrillo-Munoz, A.J.; Giusiano, G.; Ezkurra, P.A.; Quindos, G. Antifungal agents: Mode of action in yeast cells. Rev. Esp. Quimioter. 2006, 19, 130–139. [Google Scholar]
- Dellenbach, P.; Thomas, J.L.; Guerin, V.; Ochsenbein, E.; Contet-Audonneau, N. Topical treatment of vaginal candidosis with sertaconazole and econazole sustained-release suppositories. Int. J. Gynaecol. Obstet. 2000, 71, S47–S52. [Google Scholar] [CrossRef]
- Benfield, P.; Clissold, S.P. Sulconazole. A review of its antimicrobial activity and therapeutic use in superficial dermatomycoses. Drugs 1988, 35, 143–153. [Google Scholar] [CrossRef]
- Clissold, S.P.; Heel, R.C. Tioconazole. A review of its antimicrobial activity and therapeutic use in superficial mycoses. Drugs 1986, 31, 29–51. [Google Scholar] [CrossRef]
- Lake-Bakaar, G.; Scheuer, P.J.; Sherlock, S. Hepatic reactions associated with ketoconazole in the United Kingdom. Br. Med. J. Clin. Res. Ed. 1987, 294, 419–422. [Google Scholar] [CrossRef]
- Stricker, B.H.; Blok, A.P.; Bronkhorst, F.B.; Van Parys, G.E.; Desmet, V.J. Ketoconazole-associated hepatic injury. A clinicopathological study of 55 cases. J. Hepatol. 1986, 3, 399–406. [Google Scholar] [CrossRef]
- Pont, A.; Goldman, E.S.; Sugar, A.M.; Siiteri, P.K.; Stevens, D.A. Ketoconazole-induced increase in estradiol-testosterone ratio. Probable explanation for gynecomastia. Arch. Intern. Med. 1985, 145, 1429–1431. [Google Scholar] [CrossRef]
- Ellepola, A.N.; Samaranayake, L.P. Oral candidal infections and antimycotics. Crit. Rev. Oral. Biol. Med. 2000, 11, 172–198. [Google Scholar] [CrossRef]
- Munoz, P.; Moreno, S.; Berenguer, J.; Bernaldo de Quiros, J.C.; Bouza, E. Fluconazole-related hepatotoxicity in patients with acquired immunodeficiency syndrome. Arch. Intern. Med. 1991, 151, 1020–1021. [Google Scholar] [CrossRef]
- Gayam, V.; Khalid, M.; Dahal, S.; Garlapati, P.; Gill, A. Hyperacute liver injury following intravenous fluconazole: A rare case of dose-independent hepatotoxicity. J. Family Med. Prim. Care 2018, 7, 451–454. [Google Scholar] [CrossRef]
- Moon, W.J.; Scheller, E.L.; Suneja, A.; Livermore, J.A.; Malani, A.N.; Moudgal, V.; Kerr, L.E.; Ferguson, E.; Vandenberg, D.M. Plasma fluoride level as a predictor of voriconazole-induced periostitis in patients with skeletal pain. Clin. Infect. Dis. 2014, 59, 1237–1245. [Google Scholar] [CrossRef] [PubMed]
- Tarlock, K.; Johnson, D.; Cornell, C.; Parnell, S.; Meshinchi, S.; Baker, K.S.; Englund, J.A. Elevated fluoride levels and periostitis in pediatric hematopoietic stem cell transplant recipients receiving long-term voriconazole. Pediatr. Blood Cancer 2015, 62, 918–920. [Google Scholar] [CrossRef]
- Elewski, B.E.; Rich, P.; Pollak, R.; Pariser, D.M.; Watanabe, S.; Senda, H.; Ieda, C.; Smith, K.; Pillai, R.; Ramakrishna, T.; et al. Efinaconazole 10% solution in the treatment of toenail onychomycosis: Two phase III multicenter, randomized, double-blind studies. J. Am. Acad. Dermatol. 2013, 68, 600–608. [Google Scholar] [CrossRef]
- McCormack, P.L. Isavuconazonium: First global approval. Drugs 2015, 75, 817–822. [Google Scholar] [CrossRef] [PubMed]
- Young, G.A.; Bosly, A.; Gibbs, D.L.; Durrant, S. A double-blind comparison of fluconazole and nystatin in the prevention of candidiasis in patients with leukaemia. Antifungal Prophylaxis Study Group. Eur. J. Cancer 1999, 35, 1208–1213. [Google Scholar] [CrossRef]
- Lalitha, P.; Vijaykumar, R.; Prajna, N.V.; Fothergill, A.W. In vitro natamycin susceptibility of ocular isolates of Fusarium and Aspergillus species: Comparison of commercially formulated natamycin eye drops to pharmaceutical-grade powder. J. Clin. Microbiol. 2008, 46, 3477–3478. [Google Scholar] [CrossRef]
- Te Welscher, Y.M.; van Leeuwen, M.R.; de Kruijff, B.; Dijksterhuis, J.; Breukink, E. Polyene antibiotic that inhibits membrane transport proteins. Proc. Natl. Acad. Sci. USA 2012, 109, 11156–11159. [Google Scholar] [CrossRef] [PubMed]
- Muller, G.G.; Kara-Jose, N.; de Castro, R.S. Antifungals in eye infections: Drugs and routes of administration. Rev. Bras. Oftalmol. 2013, 72, 132–141. [Google Scholar]
- De la Torre, P.; Meyer, D.K.; Reboli, A.C. Anidulafungin: A novel echinocandin for candida infections. Future Microbiol. 2008, 3, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Vazquez, J.A.; Sobel, J.D. Anidulafungin: A novel echinocandin. Clin. Infect. Dis. 2006, 43, 215–222. [Google Scholar] [CrossRef]
- Keating, G.M.; Figgitt, D.P. Caspofungin—A review of its use in oesophageal candidiasis, invasive candidiasis and invasive aspergillosis. Drugs 2003, 63, 2235–2263. [Google Scholar] [CrossRef]
- Kofla, G.; Ruhnke, M. Pharmacology and metabolism of anidulafungin, caspofungin and micafungin in the treatment of invasive candidosis: Review of the literature. Eur. J. Med. Res. 2011, 16, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Singal, A. Butenafine and superficial mycoses: Current status. Expert. Opin. Drug. Metab. Toxicol. 2008, 4, 999–1005. [Google Scholar] [CrossRef]
- Gupta, A.K.; Stec, N.; Summerbell, R.C.; Shear, N.H.; Piguet, V.; Tosti, A.; Piraccini, B.M. Onychomycosis: A review. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 1972–1990. [Google Scholar] [CrossRef]
- Lipner, S.R.; Scher, R.K. Onychomycosis: Treatment and prevention of recurrence. J. Am. Acad. Dermatol. 2019, 80, 853–867. [Google Scholar] [CrossRef] [PubMed]
- Monk, J.P.; Brogden, R.N. Naftifine. A review of its antimicrobial activity and therapeutic use in superficial dermatomycoses. Drugs 1991, 42, 659–672. [Google Scholar] [CrossRef] [PubMed]
- Matsumori, N.; Sawada, Y.; Murata, M. Mycosamine orientation of amphotericin B controlling interaction with ergosterol: Sterol-dependent activity of conformation-restricted derivatives with an amino-carbonyl bridge. J. Am. Chem. Soc. 2005, 127, 10667–10675. [Google Scholar] [CrossRef] [PubMed]
- Bruheim, P.; Borgos, S.E.; Tsan, P.; Sletta, H.; Ellingsen, T.E.; Lancelin, J.M.; Zotchev, S.B. Chemical diversity of polyene macrolides produced by Streptomyces noursei ATCC 11455 and recombinant strain ERD44 with genetically altered polyketide synthase NysC. Antimicrob. Agents Chemother. 2004, 48, 4120–4129. [Google Scholar] [CrossRef]
- Anderson, T.M.; Clay, M.C.; Cioffi, A.G.; Diaz, K.A.; Hisao, G.S.; Tuttle, M.D.; Nieuwkoop, A.J.; Comellas, G.; Maryum, N.; Wang, S.; et al. Amphotericin forms an extramembranous and fungicidal sterol sponge. Nat. Chem. Biol. 2014, 10, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Denning, D.W. Echinocandin antifungal drugs. Lancet 2003, 362, 1142–1151. [Google Scholar] [CrossRef]
- Simitsopoulou, M.; Peshkova, P.; Tasina, E.; Katragkou, A.; Kyrpitzi, D.; Velegraki, A.; Walsh, T.J.; Roilides, E. Species-specific and drug-specific differences in susceptibility of Candida biofilms to echinocandins: Characterization of less common bloodstream isolates. Antimicrob. Agents Chemother. 2013, 57, 2562–2570. [Google Scholar] [CrossRef]
- Ryder, N.S. Squalene epoxidase as a target for the allylamines. Biochem. Soc. Trans. 1991, 19, 774–777. [Google Scholar] [CrossRef]
- Mohr, J.; Johnson, M.; Cooper, T.; Lewis, J.S.; Ostrosky-Zeichner, L. Current Options in Antifungal Pharmacotherapy. Pharmacother. Pharmacotherapy 2008, 28, 614–645. [Google Scholar] [CrossRef]
- Mohd-Assaad, N.; McDonald, B.A.; Croll, D. Multilocus resistance evolution to azole fungicides in fungal plant pathogen populations. Mol. Ecol. 2016, 25, 6124–6142. [Google Scholar] [CrossRef] [PubMed]
- Roemer, T.; Krysan, D.J. Antifungal drug development: Challenges, unmet clinical needs, and new approaches. Cold Spring Harb. Perspect. Med. 2014, 4, 4148–4153. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekar, P. Management of invasive fungal infections: A role for polyenes. J. Antimicrob. Chemother. 2011, 66, 457–465. [Google Scholar] [CrossRef] [PubMed]
- Crawford, F.; Hollis, S. Topical treatments for fungal infections of the skin and nails of the foot. Cochrane Database Syst Rev. 2007, 3, CD001434. [Google Scholar] [CrossRef]
- Reboutier, D.; Piednoël, M.; Boisnard, S.; Conti, A.; Chevalier, V.; Florent, M.; Gibot-Leclerc, S.; Da Silva, B.; Chastin, C.; Fallague, K.; et al. Combination of different molecular mechanisms leading to fluconazole resistance in a Candida lusitaniae clinical isolate. Diagn. Microbiol. Infect. Dis. 2009, 63, 188–193. [Google Scholar] [CrossRef]
- Florent, M.; Noël, T.; Ruprich-Robert, G.; Da Silva, B.; Fitton-Ouhabi, V.; Chastin, C.; Papon, N.; Chapeland-Leclerc, F. Nonsense and missense mutations in FCY2 and FCY1 genes are responsible for flucytosine resistance and flucytosine-fluconazole cross-resistance in clinical isolates of Candida lusitaniae. Antimicrob. Agents Chemother. 2009, 53, 2982–2990. [Google Scholar] [CrossRef]
- Vermes, A.; Guchelaar, H.J.; Dankert, J. Flucytosine: A review of its pharmacology, clinical indications, pharmacokinetics, toxicity and drug interactions. J. Antimicrob. Chemother. 2000, 46, 171–179. [Google Scholar] [CrossRef]
- Hope, W.W.; Tabernero, L.; Denning, D.W.; Anderson, M.J. Molecular mechanisms of primary resistance to flucytosine in Candida albicans. Antimicrob. Agents Chemother. 2004, 48, 4377–4386. [Google Scholar] [CrossRef]
- Chen, S.C.; Meyer, W.; Sorrell, T.C. Cryptococcus gattii infections. Clin. Microbiol. Rev. 2014, 27, 980–1024. [Google Scholar] [CrossRef] [PubMed]
- Felton, T.; Troke, P.F.; Hope, W.W. Tissue penetration of antifungal agents. Clin. Microbiol. Rev. 2014, 27, 68–88. [Google Scholar] [CrossRef]
- Shahid, S.K. Newer patents in antimycotic therapy. Pharm. Pat. Anal. 2016, 5, 115–134. [Google Scholar] [CrossRef]
- Vandeputte, P.; Ferrari, S.; Coste, A.T. Antifungal resistance and new strategies to control fungal infections. Int. J. Microbiol. 2012, 2012, 713687. [Google Scholar] [CrossRef]
- Mohammadi, G.; Shakeri, A.; Fattahi, A.; Mohammadi, P.; Mikaeili, A.; Aliabadi, A.; Adibkia, K. Preparation, Physicochemical Characterization and Anti-fungal Evaluation of Nystatin-Loaded PLGA-Glucosamine Nanoparticles. Pharm. Res. 2017, 34, 301–309. [Google Scholar] [CrossRef] [PubMed]
- Niemirowicz, K.; Durnas, B.; Tokajuk, G.; Gluszek, K.; Wilczewska, A.Z.; Misztalewska, I.; Mystkowska, J.; Michalak, G.; Sodo, A.; Watek, M.; et al. Magnetic nanoparticles as a drug delivery system that enhance fungicidal activity of polyene antibiotics. Nanomedicine 2016, 12, 2395–2404. [Google Scholar] [CrossRef] [PubMed]
- Das, B.; Khan, M.I.; Jayabalan, R.; Behera, S.K.; Yun, S.I.; Tripathy, S.K.; Mishra, A. Understanding the Antifungal Mechanism of Ag@ZnO Core-shell Nanocomposites against Candida krusei. Sci. Rep. 2016, 6, 36403. [Google Scholar] [CrossRef] [PubMed]
- Chidambaram, M.; Manavalan, R.; Kathiresan, K. Nanotherapeutics to overcome conventional cancer chemotherapy limitations. J. Pharm. Pharm. Sci. 2011, 14, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Farokhzad, O.C. Nanotechnology for drug delivery: The perfect partnership. Expert. Opin. Drug. Deliv. 2008, 5, 927–929. [Google Scholar] [CrossRef]
- Peer, D.; Karp, J.M.; Hong, S.; Farokhzad, O.C.; Margalit, R.; Langer, R. Nanocarriers as an emerging platform for cancer therapy. Nat. Nanotechnol. 2007, 2, 751–760. [Google Scholar] [CrossRef]
- Power, S.; Slattery, M.M.; Lee, M.J. Nanotechnology and its relationship to interventional radiology. Part II: Drug Delivery, Thermotherapy, and Vascular Intervention. Cardiovasc. Intervent. Radiol. 2011, 34, 676–690. [Google Scholar] [CrossRef]
- Dos Santos Ramos, M.A.; Da Silva, P.B.; Sposito, L.; De Toledo, L.G.; Bonifacio, B.V.; Rodero, C.F.; Dos Santos, K.C.; Chorilli, M.; Bauab, T.M. Nanotechnology-based drug delivery systems for control of microbial biofilms: A review. Int. J. Nanomedicine. 2018, 13, 1179–1213. [Google Scholar] [CrossRef]
- Ghosh, P.; Han, G.; De, M.; Kim, C.K.; Rotello, V.M. Gold nanoparticles in delivery applications. Adv. Drug Deliv. Rev. 2008, 60, 1307–1315. [Google Scholar] [CrossRef]
- More, M.P.; Ganguly, P.R.; Pandey, A.P.; Dandekar, P.P.; Jain, R.D.; Patil, P.O.; Deshmukh, P.K. Development of surface engineered mesoporous alumina nanoparticles: Drug release aspects and cytotoxicity assessment. Iet. Nanobiotechnol. 2017, 11, 661–668. [Google Scholar] [CrossRef]
- Mathur, M.; Devi, V.K. Potential of novel drug delivery systems in the management of topical candidiasis. J. Drug Target. 2017, 25, 685–703. [Google Scholar] [CrossRef] [PubMed]
- Weir, E.; Lawlor, A.; Whelan, A.; Regan, F. The use of nanoparticles in anti-microbial materials and their characterization. Analyst 2008, 133, 835–845. [Google Scholar] [CrossRef]
- Wani, I.A.; Ahmad, T.; Manzoor, N. Size and shape dependant antifungal activity of gold nanoparticles: A case study of Candida. Colloids Surf. B Biointerfaces 2013, 101, 162–170. [Google Scholar] [CrossRef]
- Choi, H.; Lee, D.G. Lycopene induces apoptosis in Candida albicans through reactive oxygen species production and mitochondrial dysfunction. Biochimie 2015, 115, 108–115. [Google Scholar] [CrossRef]
- Shaikh, S.; Nazam, N.; Rizvi, S.M.D.; Ahmad, K.; Baig, M.H.; Lee, E.J.; Choi, I. Mechanistic Insights into the Antimicrobial Actions of Metallic Nanoparticles and Their Implications for Multidrug Resistance. Int. J. Mol. Sci. 2019, 20, 2468. [Google Scholar] [CrossRef] [PubMed]
- Jebali, A.; Hajjar, F.H.E.; Hekmatimoghaddam, S.; Kazemi, B.; De La Fuente, J.M.; Rashidi, M. Triangular gold nanoparticles conjugated with peptide ligands: A new class of inhibitor for Candida albicans secreted aspartyl proteinase. Biochem. Pharmacol. 2014, 90, 349–355. [Google Scholar] [CrossRef]
- Rahimi, H.; Roudbarmohammadi, S.; Delavari, H.H.; Roudbary, M. Antifungal effects of indolicidin-conjugated gold nanoparticles against fluconazole-resistant strains of Candida albicans isolated from patients with burn infection. Int. J. Nanomed. 2019, 14, 5323–5338. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, T.; Wani, I.A.; Lone, I.H.; Ganguly, A.; Manzoor, N.; Ahmad, A.; Ahmed, J.; Al-Shihri, A.S. Antifungal activity of gold nanoparticles prepared by solvothermal method. Mater. Res. Bull. 2013, 48, 12–20. [Google Scholar] [CrossRef]
- Baygar, T.; Sarac, N.; Ugur, A.; Karaca, I.R. Antimicrobial characteristics and biocompatibility of the surgical sutures coated with biosynthesized silver nanoparticles. Bioorg. Chem. 2019, 86, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Wang, Y.Y.; Huang, J.; Chen, C.Y.; Wang, Z.X.; Xie, H. Silver nanoparticles: Synthesis, medical applications and biosafety. Theranostics 2020, 10, 8996–9031. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, A.; Wei, Y.; Syed, F.; Tahir, K.; Taj, R.; Khan, A.U.; Hameed, M.U.; Yuan, Q. Amphotericin B-conjugated biogenic silver nanoparticles as an innovative strategy for fungal infections. Microb. Pathog. 2016, 99, 271–281. [Google Scholar] [CrossRef]
- Al Aboody, M.S. Silver/silver chloride (Ag/AgCl) nanoparticles synthesized from Azadirachta indica lalex and its antibiofilm activity against fluconazole resistant Candida tropicalis. Artif. Cells Nanomed. Biotechnol. 2019, 47, 2107–2113. [Google Scholar] [CrossRef]
- Selvaraj, M.; Pandurangan, P.; Ramasami, N.; Rajendran, S.B.; Sangilimuthu, S.N.; Perumal, P. Highly potential antifungal activity of quantum-sized silver nanoparticles against Candida albicans. Appl. Biochem. Biotechnol. 2014, 173, 55–66. [Google Scholar] [CrossRef]
- Ronavari, A.; Igaz, N.; Gopisetty, M.K.; Szerencses, B.; Kovacs, D.; Papp, C.; Vagvolgyi, C.; Boros, I.M.; Konya, Z.; Kiricsi, M.; et al. Biosynthesized silver and gold nanoparticles are potent antimycotics against opportunistic pathogenic yeasts and dermatophytes. Int. J. Nanomed. 2018, 13, 695–703. [Google Scholar] [CrossRef]
- Jesmin, R.; Chanda, A. Restricting mycotoxins without killing the producers: A new paradigm in nano-fungal interactions. Appl. Microbiol. Biotechnol. 2020, 104, 2803–2813. [Google Scholar] [CrossRef]
- Khalil, N.M.; Abd El-Ghany, M.N.; Rodriguez-Couto, S. Antifungal and anti-mycotoxin efficacy of biogenic silver nanoparticles produced by Fusarium chlamydosporum and Penicillium chrysogenum at non-cytotoxic doses. Chemosphere 2019, 218, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Ammar, H.A.; El-Desouky, T.A. Green synthesis of nanosilver particles by Aspergillus terreus HA1N and Penicillium expansum HA2N and its antifungal activity against mycotoxigenic fungi. J. Appl. Microbiol. 2016, 121, 89–100. [Google Scholar] [CrossRef] [PubMed]
- Sirelkhatim, A.; Mahmud, S.; Seeni, A.; Kaus, N.H.M.; Ann, L.C.; Bakhori, S.K.M.; Hasan, H.; Mohamad, D. Review on Zinc Oxide Nanoparticles: Antibacterial Activity and Toxicity Mechanism. Nanomicrob. Lett. 2015, 7, 219–242. [Google Scholar] [CrossRef]
- Sun, Q.; Li, J.; Le, T. Zinc Oxide Nanoparticle as a Novel Class of Antifungal Agents: Current Advances and Future Perspectives. J. Agric. Food Chem. 2018, 66, 11209–11220. [Google Scholar] [CrossRef] [PubMed]
- Singh, S. Zinc oxide nanoparticles impacts: Cytotoxicity, genotoxicity, developmental toxicity, and neurotoxicity. Toxicol. Mech. Methods 2019, 29, 300–311. [Google Scholar] [CrossRef]
- Khan, M.F.; Hameedullah, M.; Ansari, A.H.; Ahmad, E.; Lohani, M.B.; Khan, R.H.; Alam, M.M.; Khan, W.; Husain, F.M.; Ahmad, I. Flower-shaped ZnO nanoparticles synthesized by a novel approach at near-room temperatures with antibacterial and antifungal properties. Int. J. Nanomed. 2014, 9, 853–864. [Google Scholar] [CrossRef] [PubMed]
- Siddiqi, K.S.; Ur Rahman, A.; Tajuddin; Husen, A. Properties of Zinc Oxide Nanoparticles and Their Activity against Microbes. Nanoscale Res. Lett. 2018, 13, 141. [Google Scholar] [CrossRef] [PubMed]
- Abedzadeh Hajar, A.; Dakhili, M.; Saghazadeh, M.; Aghaei, S.S.; Nazari, R. Synergistic Antifungal Effect of Fluconazole Combined with ZnO Nanoparticles against Candida albicans Strains from Vaginal Candidiasis. Med Lab. J. 2020, 14, 26–32. [Google Scholar] [CrossRef]
- Hosseini, S.S.; Joshaghani, H.; Shokohi, T.; Ahmadi, A.; Mehrbakhsh, Z. Antifungal Activity of ZnO Nanoparticles and Nystatin and Downregulation of SAP1-3 Genes Expression in Fluconazole-Resistant Candida albicans Isolates from Vulvovaginal Candidiasis. Infect. Drug Resist. 2020, 13, 385–394. [Google Scholar] [CrossRef]
- Wu, W.; Wu, Z.; Yu, T.; Jiang, C.; Kim, W.S. Recent progress on magnetic iron oxide nanoparticles: Synthesis, surface functional strategies and biomedical applications. Sci. Technol. Adv. Mater. 2015, 16, 023501. [Google Scholar] [CrossRef]
- Vangijzegem, T.; Stanicki, D.; Laurent, S. Magnetic iron oxide nanoparticles for drug delivery: Applications and characteristics. Expert. Opin. Drug Deliv. 2019, 16, 69–78. [Google Scholar] [CrossRef]
- Chifiriuc, C.; Grumezescu, V.; Grumezescu, A.M.; Saviuc, C.; Lazar, V.; Andronescu, E. Hybrid magnetite nanoparticles/Rosmarinus officinalis essential oil nanobiosystem with antibiofilm activity. Nanoscale Res. Lett. 2012, 7, 209. [Google Scholar] [CrossRef] [PubMed]
- Chifiriuc, M.C.; Grumezescu, A.M.; Andronescu, E.; Ficai, A.; Cotar, A.I.; Grumezescu, V.; Bezirtzoglou, E.; Lazar, V.; Radulescu, R. Water dispersible magnetite nanoparticles influence the efficacy of antibiotics against planktonic and biofilm embedded Enterococcus faecalis cells. Anaerobe 2013, 22, 14–19. [Google Scholar] [CrossRef]
- Hu, S.; Gu, F.; Chen, M.; Wang, C.W.; Li, J.; Yang, J.; Wang, G.Y.; Zhou, Z.; Yang, Y. A novel method for identifying and distinguishing Cryptococcus neoformans and Cryptococcus gattii by surface-enhanced Raman scattering using positively charged silver nanoparticles. Sci. Rep. 2020, 10, 12480. [Google Scholar] [CrossRef]
- Rodriguez-Torres, M.D.P.; Diaz-Torres, L.A.; Millan-Chiu, B.E.; Garcia-Contreras, R.; Hernandez-Padron, G.; Acosta-Torres, L.S. Antifungal and Cytotoxic Evaluation of Photochemically Synthesized Heparin-Coated Gold and Silver Nanoparticles. Molecules 2020, 25, 2849. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, S.S.; Ghaemi, E.; Noroozi, A.; Niknejad, F. Zinc Oxide Nanoparticles Inhibition of Initial Adhesion and ALS1 and ALS3 Gene Expression in Candida albicans Strains from Urinary Tract Infections. Mycopathologia 2019, 184, 261–271. [Google Scholar] [CrossRef]
- Hoang Thi, T.T.; Cao, V.D.; Nguyen, T.N.Q.; Hoang, D.T.; Ngo, V.C.; Nguyen, D.H. Functionalized mesoporous silica nanoparticles and biomedical applications. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 99, 631–656. [Google Scholar] [CrossRef] [PubMed]
- Asefa, T.; Tao, Z. Biocompatibility of mesoporous silica nanoparticles. Chem. Res. Toxicol. 2012, 25, 2265–2284. [Google Scholar] [CrossRef]
- Frickenstein, A.N.; Hagood, J.M.; Britten, C.N.; Abbott, B.S.; McNally, M.W.; Vopat, C.A.; Patterson, E.G.; MacCuaig, W.M.; Jain, A.; Walters, K.B.; et al. Mesoporous Silica Nanoparticles: Properties and Strategies for Enhancing Clinical Effect. Pharmaceutics 2021, 13, 570. [Google Scholar] [CrossRef] [PubMed]
- Manzano, M.; Vallet-Regi, M. Mesoporous Silica Nanoparticles for Drug Delivery. Adv. Funct. Mater. 2020, 30, 1902634. [Google Scholar] [CrossRef]
- Mendiratta, S.; Hussein, M.; Nasser, H.A.; Ali, A.A.A. Multidisciplinary Role of Mesoporous Silica Nanoparticles in Brain Regeneration and Cancers: From Crossing the Blood-Brain Barrier to Treatment. Part. Part. Syst. Char. 2019, 36, 1900195. [Google Scholar] [CrossRef]
- Qiao, Z.A.; Zhang, L.; Guo, M.Y.; Liu, Y.L.; Huo, Q.S. Synthesis of Mesoporous Silica Nanoparticles via Controlled Hydrolysis and Condensation of Silicon Alkoxide. Chem. Mater. 2009, 21, 3823–3829. [Google Scholar] [CrossRef]
- Mas, N.; Galiana, I.; Hurtado, S.; Mondragon, L.; Bernardos, A.; Sancenon, F.; Marcos, M.D.; Amoros, P.; Abril-Utrillas, N.; Martinez-Manez, R.; et al. Enhanced antifungal efficacy of tebuconazole using gated pH-driven mesoporous nanoparticles. Int. J. Nanomed. 2014, 9, 2597–2605. [Google Scholar] [CrossRef]
- Montazeri, M.; Razzaghi-Abyaneh, M.; Nasrollahi, S.A.; Maibach, H.; Nafisi, S. Enhanced topical econazole antifungal efficacy by amine-functionalized silica nanoparticles. B Mater. Sci. 2019, 43, 13. [Google Scholar] [CrossRef]
- Abdelbar, M.F.; Shams, R.S.; Morsy, O.M.; Hady, M.A.; Shoueir, K.; Abdelmonem, R. Highly ordered functionalized mesoporous silicate nanoparticles reinforced poly (lactic acid) gatekeeper surface for infection treatment. Int. J. Biol. Macromol. 2020, 156, 858–868. [Google Scholar] [CrossRef] [PubMed]
- Diez-Orejas, R.; Casarrubios, L.; Feito, M.J.; Rojo, J.M.; Vallet-Regi, M.; Arcos, D.; Portoles, M.T. Effects of mesoporous SiO2-CaO nanospheres on the murine peritoneal macrophages/Candida albicans interface. Int. Immunopharmacol. 2021, 94, 107457. [Google Scholar] [CrossRef]
- Quiros, J.; Gonzalo, S.; Jalvo, B.; Boltes, K.; Perdigon-Melon, J.A.; Rosal, R. Electrospun cellulose acetate composites containing supported metal nanoparticles for antifungal membranes. Sci. Total. Environ. 2016, 563–564, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Schaffazick, S.R.; Pohlmann, A.R.; Dalla-Costa, T.; Guterres, S.S. Freeze-drying polymeric colloidal suspensions: Nanocapsules, nanospheres and nanodispersion. A comparative study. Eur. J. Pharm. Biopharm. 2003, 56, 501–505. [Google Scholar] [CrossRef]
- Crucho, C.I.C.; Barros, M.T. Polymeric nanoparticles: A study on the preparation variables and characterization methods. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 80, 771–784. [Google Scholar] [CrossRef]
- Guterres, S.S.; Alves, M.P.; Pohlmann, A.R. Polymeric nanoparticles, nanospheres and nanocapsules, for cutaneous applications. Drug Target. Insights 2007, 2, 147–157. [Google Scholar] [CrossRef]
- Kleine-Brueggeney, H.; Zorzi, G.K.; Fecker, T.; El Gueddari, N.E.; Moerschbacher, B.M.; Goycoolea, F.M. A rational approach towards the design of chitosan-based nanoparticles obtained by ionotropic gelation. Colloid Surf. B 2015, 135, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Farrag, Y.; Ide, W.; Montero, B.; Rico, M.; Rodriguez-Llamazares, S.; Barral, L.; Bouza, R. Preparation of starch nanoparticles loaded with quercetin using nanoprecipitation technique. Int. J. Biol. Macromol. 2018, 114, 426–433. [Google Scholar] [CrossRef]
- Sutar, Y.B.; Telvekar, V.N. Chitosan based copolymer-drug conjugate and its protein targeted polyelectrolyte complex nanoparticles to enhance the efficiency and specificity of low potency anticancer agent. Mat. Sci. Eng. C Mater. 2018, 92, 393–406. [Google Scholar] [CrossRef]
- Gharieh, A.; Khoee, S.; Mandavian, A.R. Emulsion and miniemulsion techniques in preparation of polymer nanoparticles with versatile characteristics. Adv. Colloid Interfac. 2019, 269, 152–186. [Google Scholar] [CrossRef]
- Patra, J.K.; Das, G.; Fraceto, L.F.; Campos, E.V.R.; Rodriguez-Torres, M.D.P.; Acosta-Torres, L.S.; Diaz-Torres, L.A.; Grillo, R.; Swamy, M.K.; Sharma, S.; et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnol. 2018, 16, 71. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.; Saeed, K.; Khan, I. Nanoparticles: Properties, applications and toxicities. Arab. J. Chem. 2019, 12, 908–931. [Google Scholar] [CrossRef]
- Kamaly, N.; Xiao, Z.; Valencia, P.M.; Radovic-Moreno, A.F.; Farokhzad, O.C. Targeted polymeric therapeutic nanoparticles: Design, development and clinical translation. Chem. Soc. Rev. 2012, 41, 2971–3010. [Google Scholar] [CrossRef]
- Sakima, V.T.; Barbugli, P.A.; Cerri, P.S.; Chorilli, M.; Carmello, J.C.; Pavarina, A.C.; Mima, E.G.D. Antimicrobial Photodynamic Therapy Mediated by Curcumin-Loaded Polymeric Nanoparticles in a Murine Model of Oral Candidiasis. Molecules 2018, 23, 2075. [Google Scholar] [CrossRef] [PubMed]
- Gondim, B.L.C.; Castellano, L.R.C.; de Castro, R.D.; Machad, G.; Carlo, H.L.; Valenca, A.M.G.; de Carvalho, F.G. Effect of chitosan nanoparticles on the inhibition of Candida spp. biofilm on denture base surface. Arch. Oral Biol. 2018, 94, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Lucena, P.A.; Nascimento, T.L.; Gaeti, M.P.N.; de Avila, R.I.; Mendes, L.P.; Vieira, M.S.; Fabrini, D.; Amaral, A.C.; Lima, E.M. In Vivo Vaginal Fungal Load Reduction after Treatment with Itraconazole-Loaded Polycaprolactone-Nanoparticles. J. Biomed. Nanotechnol. 2018, 14, 1347–1358. [Google Scholar] [CrossRef] [PubMed]
- Amaral, A.C.; Saavedra, P.H.V.; Souza, A.C.O.; de Melo, M.T.; Tedesco, A.C.; Morais, P.C.; Felipe, M.S.S.; Bocca, A.L. Miconazole loaded chitosan-based nanoparticles for local treatment of vulvovaginal candidiasis fungal infections. Colloid Surf. B 2019, 174, 409–415. [Google Scholar] [CrossRef]
- Costa, A.F.; Araujo, D.E.; Cabral, M.S.; Brito, I.T.; Leite, L.B.D.; Pereira, M.; Amaral, A.C. Development, characterization, and in vitro-in vivo evaluation of polymeric nanoparticles containing miconazole and farnesol for treatment of vulvovaginal candidiasis. Med Mycol. 2019, 57, 52–62. [Google Scholar] [CrossRef]
- Melo, C.M.; Cardoso, J.F.; Perassoli, F.B.; Neto, A.S.D.; Pinto, L.M.; Marques, M.B.D.; Mussel, W.D.; Magalhaes, J.T.; Moura, S.A.D.; Araujo, M.G.D.; et al. Amphotericin B-loaded Eudragit RL100 nanoparticles coated with hyaluronic acid for the treatment of vulvovaginal candidiasis. Carbohyd. Polym. 2020, 230, 115608. [Google Scholar] [CrossRef]
- Carraro, T.C.M.M.; Altmeyer, C.; Khalil, N.M.; Mainardes, R.M. Assessment of in vitro antifungal efficacy and in vivo toxicity of Amphotericin B-loaded PLGA and PLGA-PEG blend nanoparticles. J. Mycol. Med. 2017, 27, 519–529. [Google Scholar] [CrossRef] [PubMed]
- Torres-Rego, M.; Glaucia-Silva, F.; Rocha Soares, K.S.; de Souza, L.; Damasceno, I.Z.; Santos-Silva, E.D.; Lacerda, A.F.; Chaves, G.M.; Silva-Junior, A.A.D.; Fernandes-Pedrosa, M.F. Biodegradable cross-linked chitosan nanoparticles improve anti-Candida and anti-biofilm activity of TistH, a peptide identified in the venom gland of the Tityus stigmurus scorpion. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 103, 109830. [Google Scholar] [CrossRef] [PubMed]
- Xu, N.; Gu, J.; Zhu, Y.; Wen, H.; Ren, Q.; Chen, J. Efficacy of intravenous amphotericin B-polybutylcyanoacrylate nanoparticles against cryptococcal meningitis in mice. Int. J. Nanomed. 2011, 6, 905–913. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.X.; Wu, S.; Lin, J.Q.; Cheng, L.T.; Zhou, J.; Xie, J.; Huang, K.X.; Wang, X.Y.; Yu, Y.; Chen, Z.B.; et al. Nanoparticles Targeted against Cryptococcal Pneumonia by Interactions between Chitosan and Its Peptide Ligand. Nano Lett. 2018, 18, 6207–6213. [Google Scholar] [CrossRef]
- Roque, L.; Castro, P.; Molpeceres, J.; Viana, A.S.; Roberto, A.; Reis, C.; Rijo, P.; Tho, I.; Sarmento, B.; Reis, C. Bioadhesive polymeric nanoparticles as strategy to improve the treatment of yeast infections in oral cavity: In-vitro and ex-vivo studies. Eur. Polym. J. 2018, 104, 19–31. [Google Scholar] [CrossRef]
- Calvo, N.L.; Sreekumar, S.; Svetaz, L.A.; Lamas, M.C.; Moerschbacher, B.M.; Leonardi, D. Design and Characterization of Chitosan Nanoformulations for the Delivery of Antifungal Agents. Int. J. Mol. Sci. 2019, 20, 3686. [Google Scholar] [CrossRef] [PubMed]
- Daraee, H.; Etemadi, A.; Kouhi, M.; Alimirzalu, S.; Akbarzadeh, A. Application of liposomes in medicine and drug delivery. Artif. Cell Nanomed. B 2016, 44, 381–391. [Google Scholar] [CrossRef]
- Luo, Y.L.; Liu, Z.B.; Zhang, X.Q.; Huang, J.; Yu, X.; Li, J.W.; Xiong, D.; Sun, X.D.; Zhong, Z.R. Effect of a controlled-release drug delivery system made of oleanolic acid formulated into multivesicular liposomes on hepatocellular carcinoma in vitro and in vivo. Int. J. Nanomed. 2016, 11, 3111–3129. [Google Scholar] [CrossRef]
- Panahi, Y.; Farshbaf, M.; Mohammadhosseini, M.; Mirahadi, M.; Khalilov, R.; Saghfi, S.; Akbarzadeh, A. Recent advances on liposomal nanoparticles: Synthesis, characterization and biomedical applications. Artif. Cells Nanomed. Biotechnol. 2017, 45, 788–799. [Google Scholar] [CrossRef]
- Chorilli, M.; Calixto, G.; Rimerio, T.C.; Scarpa, M.V. Caffeine Encapsulated in Small Unilamellar Liposomes: Characerization and In Vitro Release Profile. J. Disper. Sci. Technol. 2013, 34, 1465–1470. [Google Scholar] [CrossRef]
- Deshpande, P.P.; Biswas, S.; Torchilin, V.P. Current trends in the use of liposomes for tumor targeting. Nanomedicine 2013, 8, 1509–1528. [Google Scholar] [CrossRef] [PubMed]
- Allen, T.M.; Cullis, P.R. Liposomal drug delivery systems: From concept to clinical applications. Adv. Drug Deliv. Rev. 2013, 65, 36–48. [Google Scholar] [CrossRef] [PubMed]
- Zylberberg, C.; Matosevic, S. Pharmaceutical liposomal drug delivery: A review of new delivery systems and a look at the regulatory landscape. Drug Deliv. 2016, 23, 3319–3329. [Google Scholar] [CrossRef] [PubMed]
- Abu Lila, A.S.; Ishida, T. Liposomal Delivery Systems: Design Optimization and Current Applications. Biol. Pharm. Bull. 2017, 40, 1–10. [Google Scholar] [CrossRef]
- Bowden, R.; Chandrasekar, P.; White, M.H.; Li, X.; Pietrelli, L.; Gurwith, M.; van Burik, J.A.; Laverdiere, M.; Safrin, S.; Wingard, J.R. A double-blind, randomized, controlled trial of amphotericin B colloidal dispersion versus amphotericin B for treatment of invasive aspergillosis in immunocompromised patients. Clin. Infect. Dis. 2002, 35, 359–366. [Google Scholar] [CrossRef]
- Walsh, T.J.; Hiemenz, J.W.; Seibel, N.L.; Perfect, J.R.; Horwith, G.; Lee, L.; Silber, J.L.; DiNubile, M.J.; Reboli, A.; Bow, E.; et al. Amphotericin B lipid complex for invasive fungal infections: Analysis of safety and efficacy in 556 cases. Clin. Infect. Dis. 1998, 26, 1383–1396. [Google Scholar] [CrossRef]
- Wang, Q.H.; Fu, C.; Zhao, Z.Z.; Fu, A.L. Targeted Theranostic of Cryptococcal Encephalitis by a Novel Polypyridyl Ruthenium Complex. Mol. Pharmaceut. 2020, 17, 145–154. [Google Scholar] [CrossRef]
- Giongo, J.L.; de Almeida Vaucher, R.; Fausto, V.P.; Quatrin, P.M.; Lopes, L.Q.S.; Santos, R.C.V.; Gundel, A.; Gomes, P.; Steppe, M. Anti-Candida activity assessment of Pelargonium graveolens oil free and nanoemulsion in biofilm formation in hospital medical supplies. Microb. Pathog. 2016, 100, 170–178. [Google Scholar] [CrossRef]
- De Siqueira, L.B.D.; Matos, A.P.D.; Cardoso, V.D.; Villanova, J.C.O.; Guimaraes, B.D.L.R.; dos Santos, E.P.; Vermelho, A.B.; Santos-Oliveira, R.; Ricci, E. Clove oil nanoemulsion showed potent inhibitory effect against Candida spp. Nanotechnology 2019, 30, 425101. [Google Scholar] [CrossRef]
- Adhavan, P.; Kaur, G.; Princy, A.; Murugan, R. Essential oil nanoemulsions of wild patchouli attenuate multi-drug resistant gram-positive, gram-negative and Candida albicans. Ind. Crop. Prod. 2017, 100, 106–116. [Google Scholar] [CrossRef]
- Fernandez Campos, F.; Calpena Campmany, A.C.; Rodriguez Delgado, G.; Lopez Serrano, O.; Clares Naveros, B. Development and characterization of a novel nystatin-loaded nanoemulsion for the buccal treatment of candidosis: Ultrastructural effects and release studies. J. Pharm. Sci. 2012, 101, 3739–3752. [Google Scholar] [CrossRef]
- Fernandez-Campos, F.; Clares Naveros, B.; Lopez Serrano, O.; Alonso Merino, C.; Calpena Campmany, A.C. Evaluation of novel nystatin nanoemulsion for skin candidosis infections. Mycoses 2013, 56, 70–81. [Google Scholar] [CrossRef]
- De Campos, V.E.B.; Cerqueira-Coutinho, C.S.; Capella, F.N.C.; Soares, B.G.; Holandino, C.; Mansur, C.R.E. Development and In Vitro Assessment of Nanoemulsion for Delivery of Ketoconazole Against Candida albicans. J. Nanosci. Nanotechnol. 2017, 17, 4623–4630. [Google Scholar] [CrossRef]
- Hussain, A.; Singh, V.K.; Singh, O.P.; Shafaat, K.; Kumar, S.; Ahmad, F.J. Formulation and optimization of nanoemulsion using antifungal lipid and surfactant for accentuated topical delivery of Amphotericin B. Drug Deliv. 2016, 23, 3101–3110. [Google Scholar] [CrossRef] [PubMed]
- Mahtab, A.; Anwar, M.; Mallick, N.; Naz, Z.; Jain, G.K.; Ahmad, F.J. Transungual Delivery of Ketoconazole Nanoemulgel for the Effective Management of Onychomycosis. AAPS PharmSciTech 2016, 17, 1477–1490. [Google Scholar] [CrossRef] [PubMed]
- Moazeni, M.; Kelidari, H.R.; Saeedi, M.; Morteza-Semnani, K.; Nabili, M.; Gohar, A.A.; Akbari, J.; Lotfali, E.; Nokhodchi, A. Time to overcome fluconazole resistant Candida isolates: Solid lipid nanoparticles as a novel antifungal drug delivery system. Colloids Surf. B Biointerfaces 2016, 142, 400–407. [Google Scholar] [CrossRef]
- Jain, S.; Jain, S.; Khare, P.; Gulbake, A.; Bansal, D.; Jain, S.K. Design and development of solid lipid nanoparticles for topical delivery of an anti-fungal agent. Drug Deliv. 2010, 17, 443–451. [Google Scholar] [CrossRef]
- Ramasamy, T.; Khandasami, U.S.; Ruttala, H.; Shanmugam, S. Development of solid lipid nanoparticles enriched hydrogels for topical delivery of anti-fungal agent. Macromol. Res. 2012, 20, 682–692. [Google Scholar] [CrossRef]
- Cassano, R.; Ferrarelli, T.; Mauro, M.V.; Cavalcanti, P.; Picci, N.; Trombino, S. Preparation, characterization and in vitro activities evaluation of solid lipid nanoparticles based on PEG-40 stearate for antifungal drugs vaginal delivery. Drug Deliv. 2016, 23, 1047–1056. [Google Scholar] [CrossRef] [PubMed]
- Khare, A.; Singh, I.; Pawar, P.; Grover, K. Design and Evaluation of Voriconazole Loaded Solid Lipid Nanoparticles for Ophthalmic Application. J. Drug Deliv. 2016, 2016, 6590361. [Google Scholar] [CrossRef]
- Chaudhari, M.B.; Desai, P.P.; Patel, P.A.; Patravale, V.B. Solid lipid nanoparticles of amphotericin B (AmbiOnp): In vitro and in vivo assessment towards safe and effective oral treatment module. Drug Deliv. Transl. Res. 2016, 6, 354–364. [Google Scholar] [CrossRef]
- Vaghasiya, H.; Kumar, A.; Sawant, K. Development of solid lipid nanoparticles based controlled release system for topical delivery of terbinafine hydrochloride. Eur. J. Pharm. Sci. 2013, 49, 311–322. [Google Scholar] [CrossRef]
- Carbone, C.; Fuochi, V.; Zielinska, A.; Musumeci, T.; Souto, E.B.; Bonaccorso, A.; Puglia, C.; Petronio Petronio, G.; Furneri, P.M. Dual-drugs delivery in solid lipid nanoparticles for the treatment of Candida albicans mycosis. Colloids Surf. B Biointerfaces 2020, 186, 110705. [Google Scholar] [CrossRef]
- Khames, A.; Khaleel, M.A.; El-Badawy, M.F.; El-Nezhawy, A.O.H. Natamycin solid lipid nanoparticles—Sustained ocular delivery system of higher corneal penetration against deep fungal keratitis: Preparation and optimization. Int. J. Nanomed. 2019, 14, 2515–2531. [Google Scholar] [CrossRef] [PubMed]
- Tian, B.; Yan, Q.; Wang, J.; Ding, C.; Sai, S. Enhanced antifungal activity of voriconazole-loaded nanostructured lipid carriers against Candida albicans with a dimorphic switching model. Int. J. Nanomed. 2017, 12, 7131–7141. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kelidari, H.R.; Moazeni, M.; Babaei, R.; Saeedi, M.; Akbari, J.; Parkoohi, P.I.; Nabili, M.; Gohar, A.A.; Morteza-Semnani, K.; Nokhodchi, A. Improved yeast delivery of fluconazole with a nanostructured lipid carrier system. Biomed. Pharmacother. 2017, 89, 83–88. [Google Scholar] [CrossRef]
- Ravani, L.; Esposito, E.; Bories, C.; Moal, V.L.; Loiseau, P.M.; Djabourov, M.; Cortesi, R.; Bouchemal, K. Clotrimazole-loaded nanostructured lipid carrier hydrogels: Thermal analysis and in vitro studies. Int. J. Pharm. 2013, 454, 695–702. [Google Scholar] [CrossRef] [PubMed]
- Mendes, A.I.; Silva, A.C.; Catita, J.A.; Cerqueira, F.; Gabriel, C.; Lopes, C.M. Miconazole-loaded nanostructured lipid carriers (NLC) for local delivery to the oral mucosa: Improving antifungal activity. Colloids Surf. B Biointerfaces 2013, 111, 755–763. [Google Scholar] [CrossRef]
- Passos, J.S.; Martino, L.C.; Dartora, V.F.C.; Araujo, G.L.B.; Ishida, K.; Lopes, L.B. Development, skin targeting and antifungal efficacy of topical lipid nanoparticles containing itraconazole. Eur. J. Pharm. Sci. 2020, 149, 105296. [Google Scholar] [CrossRef]
- Du, W.; Li, H.; Tian, B.; Sai, S.; Gao, Y.; Lan, T.; Meng, Y.; Ding, C. Development of nose-to-brain delivery of ketoconazole by nanostructured lipid carriers against cryptococcal meningoencephalitis in mice. Colloids Surf. B Biointerfaces 2019, 183, 110446. [Google Scholar] [CrossRef]
- Carbone, C.; Teixeira, M.D.C.; Sousa, M.D.C.; Martins-Gomes, C.; Silva, A.M.; Souto, E.M.B.; Musumeci, T. Clotrimazole-Loaded Mediterranean Essential Oils NLC: A Synergic Treatment of Candida Skin Infections. Pharmaceutics 2019, 11, 231. [Google Scholar] [CrossRef]
- Bianchin, M.D.; Borowicz, S.M.; Machado, G.D.M.; Pippie, B.; Guterres, S.S.; Pohlmann, A.R.; Fuentefria, A.M.; Kulkamp-Guerreiro, I.C. Lipid core nanoparticles as a broad strategy to reverse fluconazole resistance in multiple Candida species. Colloid Surface B 2019, 175, 523–529. [Google Scholar] [CrossRef]
- Oliveira, N.K.; Frank, L.A.; Squizani, E.D.; Reuwsaat, J.C.V.; Marques, B.M.; Motta, H.; Garcia, A.W.A.; Kinskovski, U.P.; Barcellos, V.A.; Schrank, A.; et al. New nanotechnological formulation based on amiodarone-loaded lipid core nanocapsules displays anticryptococcal effect. Eur. J. Pharm. Sci. 2021, 162, 105816. [Google Scholar] [CrossRef]
- Wingard, J.R.; Kubilis, P.; Lee, L.; Yee, G.; White, M.; Walshe, L.; Bowden, R.; Anaissie, E.; Hiemenz, J.; Lister, J. Clinical significance of nephrotoxicity in patients treated with amphotericin B for suspected or proven aspergillosis. Clin. Infect. Dis. 1999, 29, 1402–1407. [Google Scholar] [CrossRef] [PubMed]
- Olson, J.A.; Adler-Moore, J.P.; Jensen, G.M.; Schwartz, J.; Dignani, M.C.; Proffitt, R.T. Comparison of the physicochemical, antifungal, and toxic properties of two liposomal amphotericin B products. Antimicrob. Agents Chemother. 2008, 52, 259–268. [Google Scholar] [CrossRef] [PubMed]
- Hann, I.M.; Prentice, H.G. Lipid-based amphotericin B: A review of the last 10 years of use. Int. J. Antimicrob. Agents 2001, 17, 161–169. [Google Scholar] [CrossRef]
- Mason, T.G.; Graves, S.M.; Wilking, J.N.; Lin, M.Y. Effective structure factor of osmotically deformed nanoemulsions. J. Phys. Chem. B 2006, 110, 22097–22102. [Google Scholar] [CrossRef] [PubMed]
- Singh, Y.; Meher, J.G.; Raval, K.; Khan, F.A.; Chaurasia, M.; Jain, N.K.; Chourasia, M.K. Nanoemulsion: Concepts, development and applications in drug delivery. J. Control. Release 2017, 252, 28–49. [Google Scholar] [CrossRef]
- Dos Santos, M.K.; Kreutz, T.; Danielli, L.J.; De Marchi, J.G.B.; Pippi, B.; Koester, L.S.; Fuentefria, A.M.; Limberger, R.P. A chitosan hydrogel-thickened nanoemulsion containing Pelargonium graveolens essential oil for treatment of vaginal candidiasis. J. Drug Deliv. Sci. Tecnol. 2020, 56, 101527. [Google Scholar] [CrossRef]
- Gundel, S.D.; Velho, M.C.; Diefenthaler, M.K.; Favarin, F.R.; Copetti, P.M.; Fogaca, A.D.; Klein, B.; Wagner, R.; Gundel, A.; Sagrillo, M.R.; et al. Basil oil-nanoemulsions: Development, cytotoxicity and evaluation of antioxidant and antimicrobial potential. J. Drug Deliv. Sci. Technol. 2018, 46, 378–383. [Google Scholar] [CrossRef]
- Sosa, L.; Clares, B.; Alvarado, H.L.; Bozal, N.; Domenech, O.; Calpena, A.C. Amphotericin B releasing topical nanoemulsion for the treatment of candidiasis and aspergillosis. Nanomedicine 2017, 13, 2303–2312. [Google Scholar] [CrossRef] [PubMed]
- Martins, S.; Sarmento, B.; Ferreira, D.C.; Souto, E.B. Lipid-based colloidal carriers for peptide and protein delivery—Liposomes versus lipid nanoparticles. Int. J. Nanomed. 2007, 2, 595–607. [Google Scholar]
- Battaglia, L.; Gallarate, M. Lipid nanoparticles: State of the art, new preparation methods and challenges in drug delivery. Expert Opin. Drug Deliv. 2012, 9, 497–508. [Google Scholar] [CrossRef]
- Mishra, V.; Bansal, K.K.; Verma, A.; Yadav, N.; Thakur, S.; Sudhakar, K.; Rosenholm, J.M. Solid Lipid Nanoparticles: Emerging Colloidal Nano Drug Delivery Systems. Pharmaceutics 2018, 10, 191. [Google Scholar] [CrossRef] [PubMed]
- Gordillo-Galeano, A.; Mora-Huertas, C.E. Solid lipid nanoparticles and nanostructured lipid carriers: A review emphasizing on particle structure and drug release. Eur. J. Pharm. Biopharm. 2018, 133, 285–308. [Google Scholar] [CrossRef]
- Levy, M.Y.; Polacheck, I.; Barenholz, Y.; Benita, S. Efficacy evaluation of a novel submicron miconazole emulsion in a murine cryptococcosis model. Pharm. Res. 1995, 12, 223–230. [Google Scholar] [CrossRef]
- Muller, R.H.; Shegokar, R.; Keck, C.M. 20 years of lipid nanoparticles (SLN and NLC): Present state of development and industrial applications. Curr. Drug Discov. Technol. 2011, 8, 207–227. [Google Scholar] [CrossRef]
- Muller, R.H.; Mader, K.; Gohla, S. Solid lipid nanoparticles (SLN) for controlled drug delivery—A review of the state of the art. Eur. J. Pharm. Biopharm. 2000, 50, 161–177. [Google Scholar] [CrossRef]
- Furedi, P.; Papay, Z.E.; Kovacs, K.; Kiss, B.D.; Ludanyi, K.; Antal, I.; Klebovich, I. Development and characterization of the voriconazole loaded lipid-based nanoparticles. J. Pharm. Biomed. Anal. 2017, 132, 184–189. [Google Scholar] [CrossRef]
- Patel, P.A.; Patravale, V.B. AmbiOnp: Solid lipid nanoparticles of amphotericin B for oral administration. J. Biomed. Nanotechnol. 2011, 7, 632–639. [Google Scholar] [CrossRef]
- Doktorovova, S.; Souto, E.B.; Silva, A.M. Nanotoxicology applied to solid lipid nanoparticles and nanostructured lipid carriers—A systematic review of in vitro data. Eur. J. Pharm. Biopharm. 2014, 87, 1–18. [Google Scholar] [CrossRef]
- Shah, R.M.; Malherbe, F.; Eldridge, D.; Palombo, E.A.; Harding, I.H. Physicochemical characterization of solid lipid nanoparticles (SLNs) prepared by a novel microemulsion technique. J. Colloid Interface Sci. 2014, 428, 286–294. [Google Scholar] [CrossRef]
- Iqbal, M.A.; Md, S.; Sahni, J.K.; Baboota, S.; Dang, S.; Ali, J. Nanostructured lipid carriers system: Recent advances in drug delivery. J. Drug Target. 2012, 20, 813–830. [Google Scholar] [CrossRef] [PubMed]
- Wong, H.L.; Bendayan, R.; Rauth, A.M.; Li, Y.; Wu, X.Y. Chemotherapy with anticancer drugs encapsulated in solid lipid nanoparticles. Adv. Drug Deliv. Rev. 2007, 59, 491–504. [Google Scholar] [CrossRef] [PubMed]
- Heurtault, B.; Saulnier, P.; Pech, B.; Proust, J.E.; Benoit, J.P. A novel phase inversion-based process for the preparation of lipid nanocarriers. Pharm. Res. 2002, 19, 875–880. [Google Scholar] [CrossRef] [PubMed]
- Heurtault, B.; Saulnier, P.; Pech, B.; Benoit, J.P.; Proust, J.E. Interfacial stability of lipid nanocapsules. Colloid Surf. B 2003, 30, 225–235. [Google Scholar] [CrossRef]
- Hirsjarvi, S.; Bastiat, G.; Saulnier, P.; Benoit, J.P. Evaluation of surface deformability of lipid nanocapsules by drop tensiometer technique, and its experimental assessment by dialysis and tangential flow filtration. Int. J. Pharm. 2012, 434, 460–467. [Google Scholar] [CrossRef]
- Groo, A.C.; Bossiere, M.; Trichard, L.; Legras, P.; Benoit, J.P.; Lagarce, F. In vivo evaluation of paclitaxel-loaded lipid nanocapsules after intravenous and oral administration on resistant tumor. Nanomedicine 2015, 10, 589–601. [Google Scholar] [CrossRef]
- Nguyen, H.T.P.; Munnier, E.; Perse, X.; Vial, F.; Yvergnaux, F.; Perrier, T.; Souce, M.; Chourpa, I. Qualitative and Quantitative Study of the Potential of Lipid Nanocapsules of One Hundred Twenty Nanometers for the Topical Administration of Hydrophobic Molecules. J. Pharm. Sci. 2016, 105, 3191–3198. [Google Scholar] [CrossRef]
- Bapat, P.; Ghadi, R.; Chaudhari, D.; Katiyar, S.S.; Jain, S. Tocophersolan stabilized lipid nanocapsules with high drug loading to improve the permeability and oral bioavailability of curcumin. Int. J. Pharm. 2019, 560, 219–227. [Google Scholar] [CrossRef]
- Eissa, M.M.; El-Moslemany, R.M.; Ramadan, A.A.; Amer, E.I.; El-Azzouni, M.Z.; El-Khordagui, L.K. Miltefosine Lipid Nanocapsules for Single Dose Oral Treatment of Schistosomiasis Mansoni: A Preclinical Study. PLoS ONE 2015, 10, e0141788. [Google Scholar] [CrossRef] [PubMed]
- Courchesne, W.E. Characterization of a novel, broad-based fungicidal activity for the antiarrhythmic drug amiodarone. J. Pharmacol. Exp. Ther. 2002, 300, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Kozubowski, L.; Aboobakar, E.F.; Cardenas, M.E.; Heitman, J. Calcineurin colocalizes with P-bodies and stress granules during thermal stress in Cryptococcus neoformans. Eukaryot Cell 2011, 10, 1396–1402. [Google Scholar] [CrossRef]
- Cruz, M.C.; Fox, D.S.; Heitman, J. Calcineurin is required for hyphal elongation during mating and haploid fruiting in Cryptococcus neoformans. EMBO J. 2001, 20, 1020–1032. [Google Scholar] [CrossRef] [PubMed]
- Gamarra, S.; Rocha, E.M.F.; Zhang, Y.Q.; Park, S.; Rao, R.; Perlin, D.S. Mechanism of the Synergistic Effect of Amiodarone and Fluconazole in Candida albicans. Antimicrob. Agents Chemother. 2010, 54, 1753–1761. [Google Scholar] [CrossRef] [PubMed]
| Diseases | Fungal Species | Conventional Treatments | Common Clinical Features and Symptoms |
|---|---|---|---|
| Dimorphic mycoses | B. dermatitidis | Azoles and polyenes | Cutaneous disease Pulmonary disease Disseminated disease |
| C. immitis | Fever, cough, shortness of breath, chest pains Headaches, weight loss, rashes Lung cavities (commonly occurs in children) | ||
| C. posadasii | |||
| H. capsulatum | Acute pulmonary histoplasmosis Chronic pulmonary histoplasmosis Disseminated histoplasmosis Histoplasmoma African histoplasmosis | ||
| P. brasiliensis | Systemic mycosis, paracoccidioidomycosis | ||
| T. marneffei | Common symptoms include fever, malaise, weight loss, skin and soft tissue lesions, hepatosplenomegaly, lymphadenopathy, cough and dyspnea Less common symptoms include osteoarticular involvement, abdominal pain and diarrhea [19] | ||
| Disseminated cryptococcosis | C. neoformans | Azoles, polyenes and antimetabolites | Cryptococcal meningocephalitis Cryptococcal pneumonia |
| C. gattii | |||
| Aspergillosis | A. fumigatus | Azoles, polyenes, echinocandins | Chronic cavitary tuberculosis Mild, self-limited hemoptysis Chronic necrotizing pulmonary aspergillosis Chronic fibrotic pulmonary aspergillosis Severe asthma Allergic bronchopulmonary aspergillosis (in atopic patients) [20] |
| A. flavus | |||
| A. terreus | |||
| A. nidulans | |||
| A. niger | |||
| A. clavatus | |||
| Candidiasis | C. albicans | Azoles, polyenes, echinocandins | Mucosal Candida infection, including oropharynx, esophagus and vagina Candidemia Acute disseminated candidiasis Infective endocarditis Vertebral osteomyelitis and diskitis Endophthalmitis Meningitis Septic arthritis Tenosynovitis [11,21] |
| C. tropicalis | |||
| C. glabrata | |||
| C. parapsilosis | |||
| C. krusei | |||
| C. auris | |||
| Mucormycosis | Rhizopus spp. | Polyenes and azoles | Tissue necrosis Sinus pain, nasal congestion, fever, soft tissue swelling and headache Blurred vision or loss of vision Cranial neuropathies or cerebral abscesses Cutaneous mucormycosis, skin swelling, necrosis and formation of abscesses [22] |
| Mucor spp. | |||
| Cunninghamella bertholletiae |
| Antifungal Agents | Drugs | Targets | Mechanisms | Administration Routes | Side Effects |
|---|---|---|---|---|---|
| Azoles | Econazole (ECO) | Epidermophyton, Microsporum, Trichophyton | Inhibits the fungal cytochrome P450-dependnent enzyme 14α-lanosterol demethylase encoded by the ERG11 gene that converts lanosterol to ergosterol in the fungal cell membrane; thus, inhibits fungal growth and replication [68,69] | Topical | Well tolerated, but rare cases with local irritation, itching, and burning [70] |
| Sertaconazole (SER) | Epidermophyton, Trichophyton | ||||
| Miconazole (MCZ) | Candida spp., Aspergillus spp., Cryptococcus neoformans, Histoplasma capsulatum, Pseudallescheria boydii, Trichosporon | Topical Intravenous | May cause congenital disease when combined with metronidazole during pregnancy | ||
| Sulconazole (SUL) | Epidermophyton, Microsporum, Trichophyton, Candida spp. | Topical | Redness, irritation, contact dermatitis, and pruritus [71] | ||
| Tioconazole (TIO) | Candida spp. | Topical | Itching, discomfort, rash, erythema, mild burning, and stinging May cause severe local adverse effects [72] | ||
| Ketoconazole (KTC) | Blastomyces, Candida spp., Histoplasma capsulatum | Topical Systemic applicatoin Oral | Hepatotoxicity and liver failure [73,74] Endocrine dysfunction, e.g., gynecomastia [75] | ||
| Clotrimazole (CLT) | Candida spp., Epidermophyton, Microsporum, Trichophyton | Topical Oral | Gastrointestinal tract toxicity as consumption with oral lozenges Elevation of liver enzymes [76] | ||
| Luliconazole (LUL) | Epidermophyton, Trichophyton | Topical | No significant side effects | ||
| Itraconazole (ITC) | Aspergillus spp., Blastomyces, Histoplasma capsulatum | Systemic application Topical Parenteral | Diarrhea Abdominal pain Hypertriglyceridemia Pancreatitis Liver injury Cardia dysrhythmia | ||
| Posaconazole (POS) | Aspergillus spp., Candida spp. | Systemic application | Fever, diarrhea, nausea, vomiting, headache Hypokalemia, rash Thrombocytopenia, abdominal pain Peripheral neuropathies Hepatocellular damage | ||
| Fluconazole (FLC) | Candida spp., Cryptococcus spp. | Systemic application Topical Oral Parenteral | Liver dysfunction [77,78] Anaphylaxis | ||
| Voriconazole (VRC) | Aspergillus spp., Candida spp., Fusarium spp., Scedosporium spp. | Systemic application | Peripheral neuropathies Pancreatitis Periostitis [79,80] Phototoxic reactions Squamous cell carcinoma | ||
| Efinaconazole (EFI) | Trichophyton | Topical | No significant toxicity reported, but causes embryotoxicity in animal model [81] | ||
| Isavuconazonium (ISA) | Aspergillus spp., Mucor spp. | Systemic application | Headache, nausea, vomiting, diarrhea, elevated liver enzymes [82] | ||
| Polyenes | Amphotericin B (AmB) | Aspergillus spp., Candida spp., Cryptococcus spp. | Directly interacts with cell membrane component and ergosterol, induces the formation of pores, and alters the cell permeability, causing the effusion of cytoplasmic content and fungicidal consequences | Systemic application Topical | Renal failure, electrolyte imbalance, and hepatotoxicity Fever, chills, headache, myalgias, bone marrow, and kidney toxicity |
| Nystatin B (NYT) | Candida spp. | Oral | Mild gastrointestinal symptoms, acute renal failure [83] | ||
| Natamycin (NAT) | Fusarium spp., Aspergillus spp. [84] | Inhibits the amino acid and glucose transportation, leads to ergosterol-specific and reversible inhibition of membrane transport proteins without altering the cell membrane permeability [85] | Topical | No severe side effects have been reported Rare cases reported mild irritation, redness, foreign body sensation, stinging, burning sensation, and tearing [86] | |
| Echinocandins | Anidulafungin (AFG) | Candida spp. [87,88] | Acts as the noncompetitive inhibitor of β-1, 3-D-glucan synthase, which leads to the inhibition of the synthesis of glucan. Thus, it compromises the fungal cell wall stability and synthesis. | Intravenous | No severe side effects have been reported |
| Caspofungin (CFG) | Candida spp., Aspergillus spp. | Intravenous | No severe side effects have been reported Rare cases of chills, fever, phlebitis/thrombophlebitis, tachycardia, nausea, vomiting, rash, abdominal pain, headache, and diarrhea [89] | ||
| Micafungin (MFG) | Candida spp. | Intravenous | Risk of hepatocarcinogenesis Rare cases of vomiting, nausea, diarrhea [89,90] | ||
| Allylamins | Butenafine (BUT) | Epidermophyton, Microsporum, Trichophyton Aspergillus spp. | Acts as the squalene epoxidase inhibitor that inhibits the ergosterol synthesis and causes the fungal cell lysis via altering cell membrane permeability | Topical | Mild burning and/or stinging are common [91] |
| Terbinafine (TRB) | Trichophyton | Topical | Headache Gastrointestinal symptoms Severe neutropenia Thrombocytopenia Liver failure or injury Taste, visual, and smell disturbances Depressive symptoms [92,93] | ||
| Naftifine (NAF) | Trichophyton | Topical | No severe systemic side effects Local irritation and uncommon cases of allergic reaction [94] | ||
| Antimetabolites | 5-flucytosine (5-FC) | Candida spp., Cryptococcus spp. | Interrupts the pyrimidine metabolism and inhibits RNA, DNA, and protein synthesis | Systemic application | Bone marrow suppression Hepatic dysfunction Diarrhea |
| Nanosystems | Active Antifungal Agents | Pathogens | Target Diseases | Antifungal Mechanisms and Outcomes | References |
|---|---|---|---|---|---|
| Triangular gold nanoparticles | Antifungal peptides | Thirty clinical isolates of C. albicans from patients with vaginal candidiasis | Vaginal candidiasis | Antifungal effects were achieved via conjugating nanoparticles with peptide ligands that inhibit secreted aspartyl proteinase 2 (Sap2) in C. albicans | [129] |
| Gold nanoparticles | Indolicidin | Ten fluconazole-resistant clinical isolates of C. albicans in skin lesions | C. albicans caused burn infection | Conjugated indolicidin with gold nanopartilces significantly reduced the expression levels of the ERG11 gene in fluconazole-resistant isolates of C. albicans and iNOS gene in macrophage | [130] |
| Gold nanoparticles | Various size of gold nanopartilces | Three clinical isolates of C. albicans | Anti-fungal growth | 7 nm gold nanoparticles displayed higher antifungal activities than larger ones (15 nm) | [131] |
| Biogenic silver nanoparticles | Amphotericin B (AmB) | C. albicans, C. tropicalis | Anti-fungal growth | Amphotericin B-conjugated silver nanoparticles with more activity in inhibiting C. albicans and C. tropicalis as compared to AmB only | [135] |
| Silver/silver chloride nanopartilces | Latex of Azadirachta indica | Sensitive and resistant strains of C. tropicalis | Inhibited fungal growth and biofilm formation | Latex fabricated silver/silver chloride nanoparticles inhibited fungal growth and biofilm formation | [136] |
| Polyvinylpyrrolidone (PVP)-capped quantum-sized silver nanoparticles (SNPs) | Polyvinylpyrrolidone and silver | C. albicans | Anti-fungal growth | The MIC determined that PVP-capped SNP displayed antifungal effects in 70 ng/mL, which was lower than AmB (500 ng/mL), fluconazole (500 ng/mL), and ketoconazole (8 μg/mL) | [137] |
| Biogenic gold and silver nanoparticles | The high astaxanthin content yeast, Phaffia rhodozyma, is utilized for microbe-assisted nanoparticle synthesis | C. albicans, C. glabrata, C. krusei, C. parapsilosis, C. tropicalis, C. neoformans, M. gypseum, T. mentagrophytes, T. tonsurans | Treat for superficial cutaneous mycosis | Biogenic silver nanoparticles displayed significantly antifungal effects to Cryptococcus, Candida, Microsporum, and Trichophyton dermatophytes, while gold nanoparticles only showed antifungal effects to Cryptococcus | [138] |
| Biogenic silver nanoparticles by F. chlamydosporus (Fusarium-silver nanoparticles) or P. chrysogenum (Penicillium-silver nanoparticles) | Silver nanoparticles | A. flavus, A. ochraceus | Anti-fungal growth and inhibit aflatoxin production | The MIC results for A. flavus were 48, 45, and 50 μg/mL for Fusarium synthesizedsilver nanoparticles (FAgNPs), Penicillium synthesizedsilver nanoparticles (PAgNPs), and itraconazole, respectively. For A. ochraceus, FAgNPs, PAgNPs, and itraconazole displayed MIC values of 51, 47, and 49 μg/mL, respectively. Moreover, FAgNPs and PAgNPs completely inhibit the aflatoxin production by A. flavus and the MIC values were 5.9 and 5.6 μg/mL, respectively, 6.3 and 6.1 μg/mL of the A. ochraceus produced ochratoxin A was inhibited by FAgNPs and PAgNPs, respectively. | [139] |
| Zinc oxide nanoparticles | Fluconazole | C. albicans isolated from vaginal samples | Vulvovaginal candidiasis | Fluconazole conjugated zinc oxide nanoparticles displayed anti-candida growth effects | [146] |
| Zinc oxide nanoparticles | Nystatin | C. albicans isolated from Vulvovaginal Candidiasis | Vulvovaginal candidiasis | Nystatin conjugated zinc oxide nanoparticles anti-candida growth via inhibiting the expression of fungal SAP1-3 genes | [147] |
| Oleic acid and CHCl3 fabricated iron oxide nanoparticles (Fe3O4/oleic acid: CHCl3) | Rosmarinus officinalis essential oil | C. albicans and C. tropicalis | Biofilm formation in the medical apparatus and instruments | The essential oil pulsed iron oxide nanoparticles significantly inhibit fungal adherence of C. albicans and C. tropicalis. Thus, they inhibit the biofilm formation in the medical instruments | [150] |
| Gold and silver nanoparticles | Heparin | C. albicans, C. krusei, C. parapsilosis | Anti-fungal growth | Silver-Heparin conjugated nanoparticles displayed antifungal effects, instead of gold-Heparin conjugated nanoparticles | [153] |
| Zinc oxide nanoparticles | N/A | 125 clinical isolates of C. albicans from patients with urinary tract infections | C. albicans caused urinary Tract Infections | Zinc oxide nanoparticles displayed antifungal effects to 125 clinical isolated C. albicans strains (include 10 fluconazole-resistant strains) via inhibiting the fungal ALS1 and ALS3 gene expression | [154] |
| Nanosystems | Active Antifungal Agents | Pathogens | Target Diseases | Antifungal Mechanisms and Outcomes | References |
|---|---|---|---|---|---|
| pH-sensitive gated mesoporous silica nanoparticles | Tebuconazole | S. cerevisiae | Anti-fungal growth | Tebuconazole loaded mesoporous silica nanoparticles enable sensing of the environmental pH alteration and release the fungal agent for antifungal effects | [161] |
| Hexagonal mesoporous silica nanoparticle with aminopropyl groups | Econazole | C. albicans | Topical fungal infection | Dermal administration of econazole loaded mesoporous silica nanoparticles displayed antifungal effects to C. albicans in vitro and in vivo | [162] |
| Nanoflowers polylactic acid added with mesoporous silica nanoparticles | Levofloxacin | S. aureus, E. coli, C. albicans, A. niger | Anti-fungal growth | The anti-microbial effect of Levofloxacin was enhanced by functionalized mesoporous silica nanoparticles with lactic acid | [163] |
| Nanosystems | Active Antifungal Agents | Pathogens | Target Diseases | Antifungal Mechanisms and Outcomes | References |
|---|---|---|---|---|---|
| Poly-lactic acid and dextran sulfate synthesized polymeric nanoparticles | Curcumin | C. albicans were inoculated in mice tongues | Oral candidiasis | Polymeric nanoparticles improved the hydrophilicity of curcumin and significantly inhibited the colony-forming unit of C. albicans in mouse tongue tissues | [176] |
| Chitosan nanoparticles | N/A | C. albicans C. tropicalis, C. krusei | Anti-biofilm formation | Chitosan nanoparticles displayed significant fungicidal effects in Candida and inhibited its biofilm formation | [177] |
| Polycaprolactone nanoparticles with two forms: nanocapsules (NC) and nanospheres (NS) | Itraconazole | C. albicans were inoculated in mice vagina | Vulvovaginal candidiasis | Only itraconazole loaded NC significantly decreased fungal load in mice vaginal tissue, instead of itraconazole loaded NS | [178] |
| Chitosan-based polymeric nanoparticles | Miconazole | C. albicans were inoculated in mice vagina | Vulvovaginal candidiasis | Miconazole loaded chitosan-based polymeric nanoparticles displayed same therapeutic effects to miconazole; however, nanoparticles only encapsulated one seventh of miconazole concentration | [179] |
| Chitosan nanoparticles | Farnesol and miconazole | C. albicans were inoculated in mice vagina | Vulvovaginal candidiasis | Farnesol and miconazole loaded chitosan-nanoparticles not only inhibited fungal growth, but hampered yeast to hyphae transition | [180] |
| Eudragit RL100 nanoparticles coated with hyaluronic acid (EUD nanoparticles /HA) | Amphotericin B (AmB) | C. albicans were inoculated in mice vagina | Vulvovaginal candidiasis | AmB EUD nanoparticles/HA enable to penetrate into the vaginal epithelium via CD44 receptor and eliminated of 100% of the vaginal fungal burden within 24 h | [181] |
| Poly (lactide-co-glycolide) (PLGA) or poly (lactide-co-glycolide)-poly (ethylene glycol) (PLGA-PEG) blend nanoparticles | Amphotericin B (AmB) | C. albicans, C. neoformans | Anti-fungal growth | AmB loaded PLGA-PEG nanoparticles only displayed antifungal effects to C. albicans, not to C. neoformans. Moreover, AmB loaded PLGA-PEG not showed liver and renal damage | [182] |
| Chitosan nanoparticles | Bioactive peptide from Tityus stigmurus scorpion (TistH) | C. albicans, C. parapsilosis, C. tropicalis, C. krusei | Inhibit fungal growth and biofilm formation | TistH-Chitosan nanoparticles inhibited C. albicans, C. parapsilosis, and C. tropicalis, and also reduced the biofilm formation of C. tropicalis, C. krusei, and C. albicans | [183] |
| Polybutylcyanoacrylate nanoparticles (PBCA-NA) | Amphotericin B (AmB) | C. neoformans induced meningoencephalitis in mouse model | Cryptococcal meningoencephalitis | The intravenous administration of AmB-PBCA-NP enabled crossing the blood brain barrier and reduced the colony-forming unit counts of cryptococcal meningoencephalitis mouse model. | [184] |
| Poly (lactic-co-glycolic acid) nanoparticles with fungal chitosan-binding peptide | Itraconazole | C. neoformans | Cryptococcal pneumonia | Polymeric nanoparticle carried cryptococcal chitosan-binding peptide specific recognized and bind to fungal capsules, and thus precisely delivered the itraconazole to clear the C. neoformans from mice lungs | [185] |
| Nanosystems | Active Antifungal Agents | Pathogens | Target Diseases | Antifungal Mechanisms and Outcomes | References |
|---|---|---|---|---|---|
| Sodium cholesteryl sulfate lipid complex with Amphotericin B, as referred to ABCD | Amphotericin B (AmB) | 174 patients with invasive aspergillosis | Invasive aspergillosis | The drug-related toxicity was evaluated via comparing between ABCD and AmB recipients, 53% vs 30% (chills), 27% vs 16% (fever), 1% vs 4% (hypoxia), and 22% vs 24% (toxicity requiring study drug discontinuation). The antifungal efficiency was equivalent between ABCD and AmB | [196] |
| AmB lipid complex (ABLC) | Amphotericin B (AmB) | 556 patients with fungal infection and intolerant of conventional antifungal therapy. | Invasive fungal infection | There were 57% of patients with responses to ABLC, including 42% (55) of 130 cases of aspergillosis, 67% (28) of 42 cases of disseminated candidiasis, 71% (17) of 24 cases of zygomycosis, and 82% (9) of 11 cases of fusariosis | [197] |
| Nanoliposome with RDP (peptide derived from rabies virus glycoprotein for brain-targeting) | Fluorescent polypyridyl ruthenium complex RC-7 | Cryptococcal meningoencephalitis animal model with C. neoformans infection | Cryptococcal meningoencephalitis | RC-7-RDP nanosystem remarkably prolonged the survival days of the meningoencephalitis-bearing mice from 10 days to 24 days. | [198] |
| Nanoemulsions (NE) | Geranium oil (GO) from Pelargonium graveolens | C. albicans, C. tropicalis, C. glabrata, C. krusei | Inhibit fungal growth and biofilm formation | GO loaded nanoemusions inhibited growth and biofilm formation of Candida spp., except C. krusei biofilm formation with strong resistance to GO-NE | [199] |
| Nanoemulsions (NE) | Clove oil (CO) | C. albicans, C. glabrata | Anti-fungal growth | Nanoemulsions enhanced antifungal effects of CO | [200] |
| Nanoemulsions (NE) | Patchouli essential oil (EO) from Pogostemon heyneanus (PH), Pogostemon plectranthoides (PP) | Multi-drug resistant (MDR) strains of S. aureus, S. mutans and C. albicans | Anti-fungal growth | PH-EO nanoemulsion exhibited better anti-bacterial and anti-candida activities than PP-EO nanoemulsion. | [201] |
| Nanoemulsions (NE) | Nystatin | C. albicans | Buccal candidiasis | Nystatin loaded nanoemulsion displayed anti-candida effects | [202] |
| Nanoemulsions (NE) | Nystatin | C. albicans, S. cerevisiae | Skin fungal infection | Nanoemulsion sustained the release of nystatin and the antifungal drug was not absorbed into systemic circulation and sufficiently eliminated dermal C. albicans. Thus, this nanoemulsion system enhanced the nystatin therapy for skin candidiasis | [203] |
| Nanoemulsions (NE) | Ketoconazole with clove oil (CL-KTZ) | C. albicans | Anti-fungal growth | The fungal membrane integrity and growth were decreased in NE-CL-KTZ treated group and the nanoemulsions improved KTZ release more than nine times when compared to KTZ cream | [204] |
| Nanoemulsions (NE) | Amphotericin B (AmB) | C. albicans, A. niger | Skin candidiasis and aspergillosis | NE enhanced AmB to cross the stratum corneum barrier in rat skin and displayed better fungicidal effects than AmB and FungisomeTM (commercial antifungal drug). | [205] |
| Nanoemulsions (NE) with thioglycolic acid as permeation enhancer | Ketoconazole | C. albicans, T. rubrum | Onychomycosis | Ketoconazole-NE contained permeation enhancer that displayed antifungal effects for onychomycosis | [206] |
| Solid lipid nanoparticles | Fluconazole | Fluconazole-resistant strains of C. albicans | Anti-fungal growth | Solid lipid nanoparticle promoted the fluconazole release and enhanced antifungal effects to C. albicans, C. parapsilosis, C. glabrata | [207] |
| Solid lipid nanoparticles (SLN) with hydrogel | Miconazole | C. albicans were inoculated into dermal side of skin in mouse model | Skin candidiasis | This SLN-hydrogel system provided sustained release of miconazole and displayed antifungal effects to C. albicans both in vitro and in vivo | [208] |
| Solid lipid nanoparticles (SLN) with hydrogel | Ketoconazole (KCZ) | C. albicans were inoculated to the skin in mouse model | Skin candidiasis | KCZ-SLN exhibited a sustained drug release over 24 h and inhibited topical fungal infection | [209] |
| Solid lipid nanoparticles (SLN) conjugated with polyoxyethylene-40 stearate (PEG-40 stearate) | Ketoconazole (KCZ) and clorimazole | C. albicans | Vulvovaginal candidiasis | SLN conjugated PEG-40 facilitated the stabilization of antifungal agents and enhanced fungicidal effects | [210] |
| Lipid-based nanoparticles (LNP) | Voriconazole | C. glabrata, A. flavus | Ophthalmic candidiasis and aspergillosis | LNP improved the poor solubility of voriconaole and enhanced its antifungal effects | [211] |
| Solid lipid nanoparticles (SLN) | Amphotericin B (AmB) | C. albicans | Oral candidiasis | SLN improved AmB oral bioavailability and alleviated its toxicity, and it enhanced its antifungal effects both in vivo and in vitro | [212] |
| Solid lipid nanoparticles (SLN) | Terbinafine hydrochloride (TH) | C. albicans | Skin candidiasis | SLN improved the stability and antifungal effects of TH | [213] |
| Solid lipid nanoparticles (SLN) | Clotrimazole (CLZ) and alphalipolic acid (ALA) | C. albicans | Anti-fungal growth | SLN prolonged drug release without any burst effect and facilitated antifungal effects in animal model | [214] |
| Solid lipid nanoparticles (SLN) | Natamycin | C. albicans, A. fumigatus | Fungal keratitis | SLN sustained drug release and increased corneal penetration. SLN-natamycin increased antifungal activity without cytotoxic effects on corneal tissues | [215] |
| Nanostructured lipid carriers (NLC) | Voriconazole | C. albicans | Anti-candidal hyphae formation | NLC sustained drug release, inhibited hyphae formation, and improved antifungal activities in vitro | [216] |
| Nanostructured lipid carriers (NLC) | Fluconazole | Fluconazole-resistant strains of C. albicans, C. glabrata, C. parapsilosis | Anti-fungal growth | NLC sustained drug release and improved fungicidal activities | [217] |
| Nanostructured lipid carriers (NLC) incorporated with poloxamer P407 | Clotrimazole | Candida albicans | Anti-fungal growth | NLC-P407 provided an optimized drug delivery system with suitable viscosity for mucosal application and four fold more antifungal activities than FungizoneTM (commercial antifungal drug) against Candida albicans | [218] |
| Nanostructured lipid carriers (NLC) | Miconazole | Candida albicans | Oral candidiasis | NLC enhanced drug release, improved local delivery of miconazole to the oral mucosa and improved antifungal effects than miconazole alone | [219] |
| Nanostructured lipid carriers (NLC) | Itraconazole | S. brasiliensis, Candida albicans | Skin fungal infection | NLC decreased transepidermal water loss, but improved drug delivery and antifungal activity | [220] |
| Nanostructured lipid carriers (NLC) | Ketoconazole | C. neoformans | Cryptococcal meningoencephalitis | NLC sustained drug release and improved antifungal effects in mouse brain tissues | [221] |
| Nanostructured lipid carriers (NLC) with Mediterranean essential oils | Clotrimazole | Candida albicans, C. krusei, C. parapsilosis | Skin candidiasis | NLC contained Mediterranean essential oils and enhanced membrane permeabilization and antifungal effects for treating topical candidiasis | [222] |
| Lipid nanocapsules (LNC) | Fluconazole | Fluconazole-resistant strains of C. albicans, C. glabrata, C. krusei, C. tropicalis | Anti-fungal growth | NLC provided the high drug carrying and controlled drug release system, enhanced antifungal activity to fluconazole-resistant Candida spp. | [223] |
| Lipid nanocapsules (LNC) | Amiodarone (AMD) and/or fluconazole (FLU) | C. neoformans | Anti-fungal growth | LNC displayed better antifungal effects, whether it was encapsulated with AMD, FLU, or AMD+FLU, than single usage of these two drugs in cryptococcal infected mice | [224] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Du, W.; Gao, Y.; Liu, L.; Sai, S.; Ding, C. Striking Back against Fungal Infections: The Utilization of Nanosystems for Antifungal Strategies. Int. J. Mol. Sci. 2021, 22, 10104. https://doi.org/10.3390/ijms221810104
Du W, Gao Y, Liu L, Sai S, Ding C. Striking Back against Fungal Infections: The Utilization of Nanosystems for Antifungal Strategies. International Journal of Molecular Sciences. 2021; 22(18):10104. https://doi.org/10.3390/ijms221810104
Chicago/Turabian StyleDu, Wei, Yiru Gao, Li Liu, Sixiang Sai, and Chen Ding. 2021. "Striking Back against Fungal Infections: The Utilization of Nanosystems for Antifungal Strategies" International Journal of Molecular Sciences 22, no. 18: 10104. https://doi.org/10.3390/ijms221810104
APA StyleDu, W., Gao, Y., Liu, L., Sai, S., & Ding, C. (2021). Striking Back against Fungal Infections: The Utilization of Nanosystems for Antifungal Strategies. International Journal of Molecular Sciences, 22(18), 10104. https://doi.org/10.3390/ijms221810104






