Bioactivity and Antibacterial Behaviors of Nanostructured Lithium-Doped Hydroxyapatite for Bone Scaffold Application
Abstract
1. Introduction
2. Results
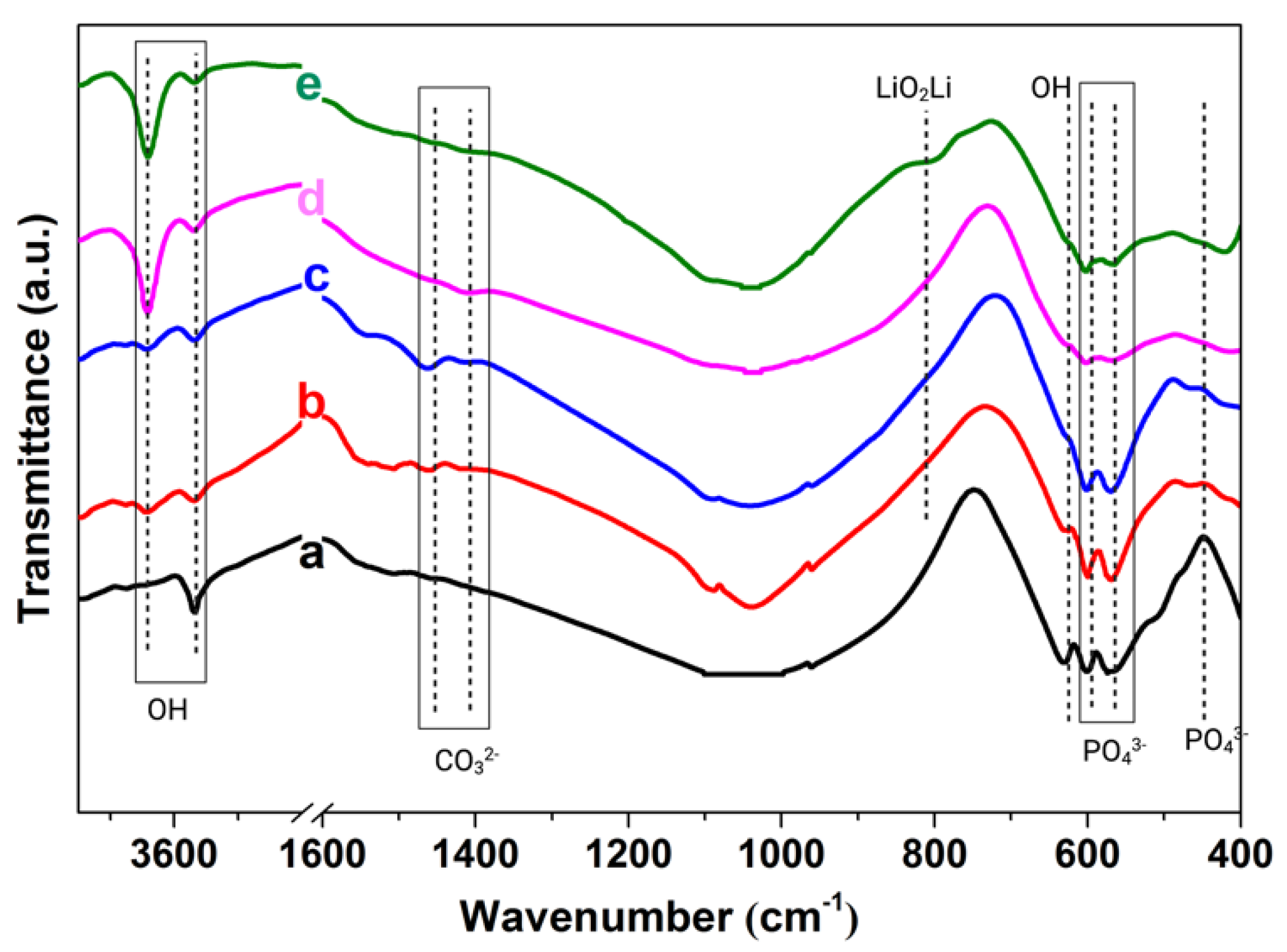
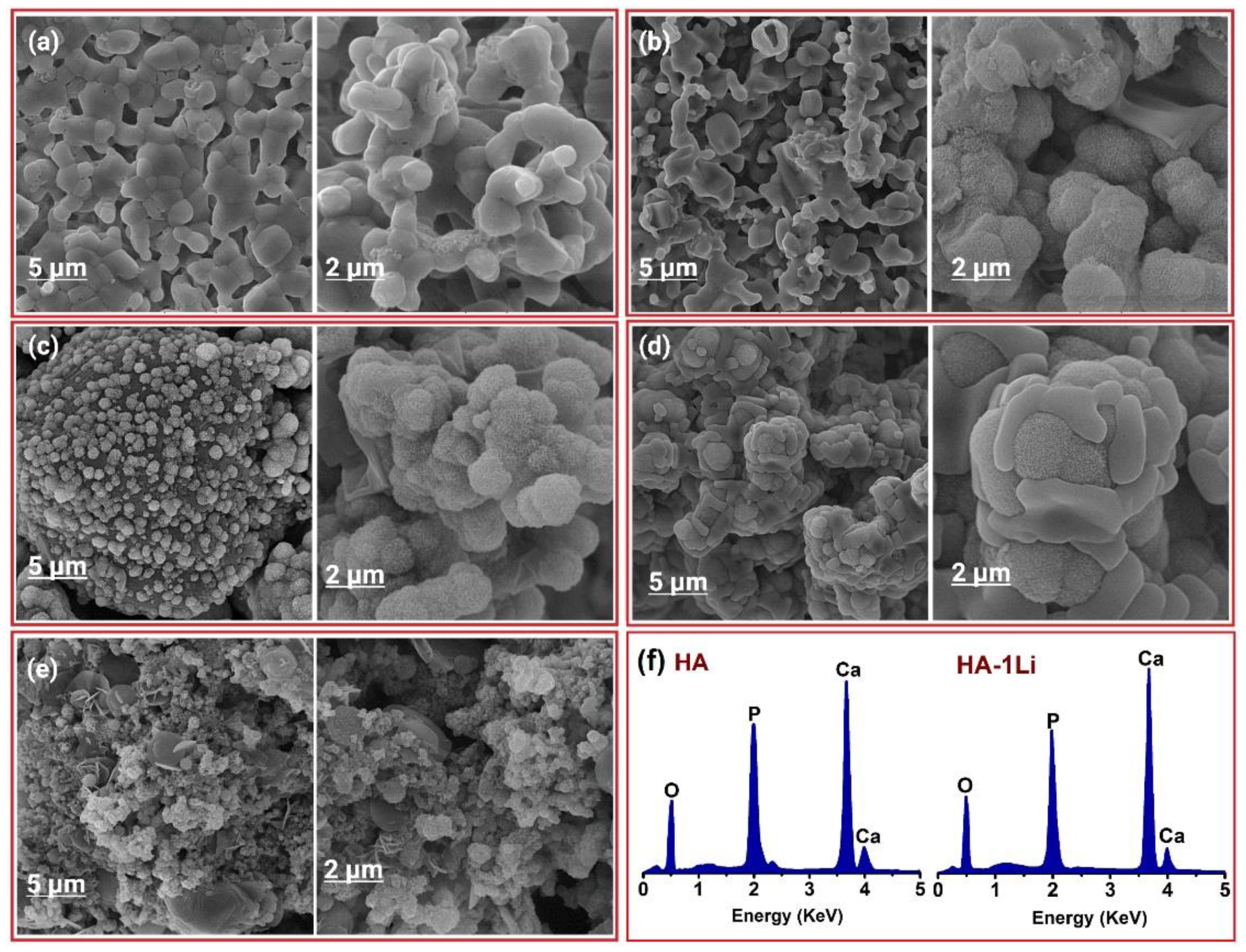
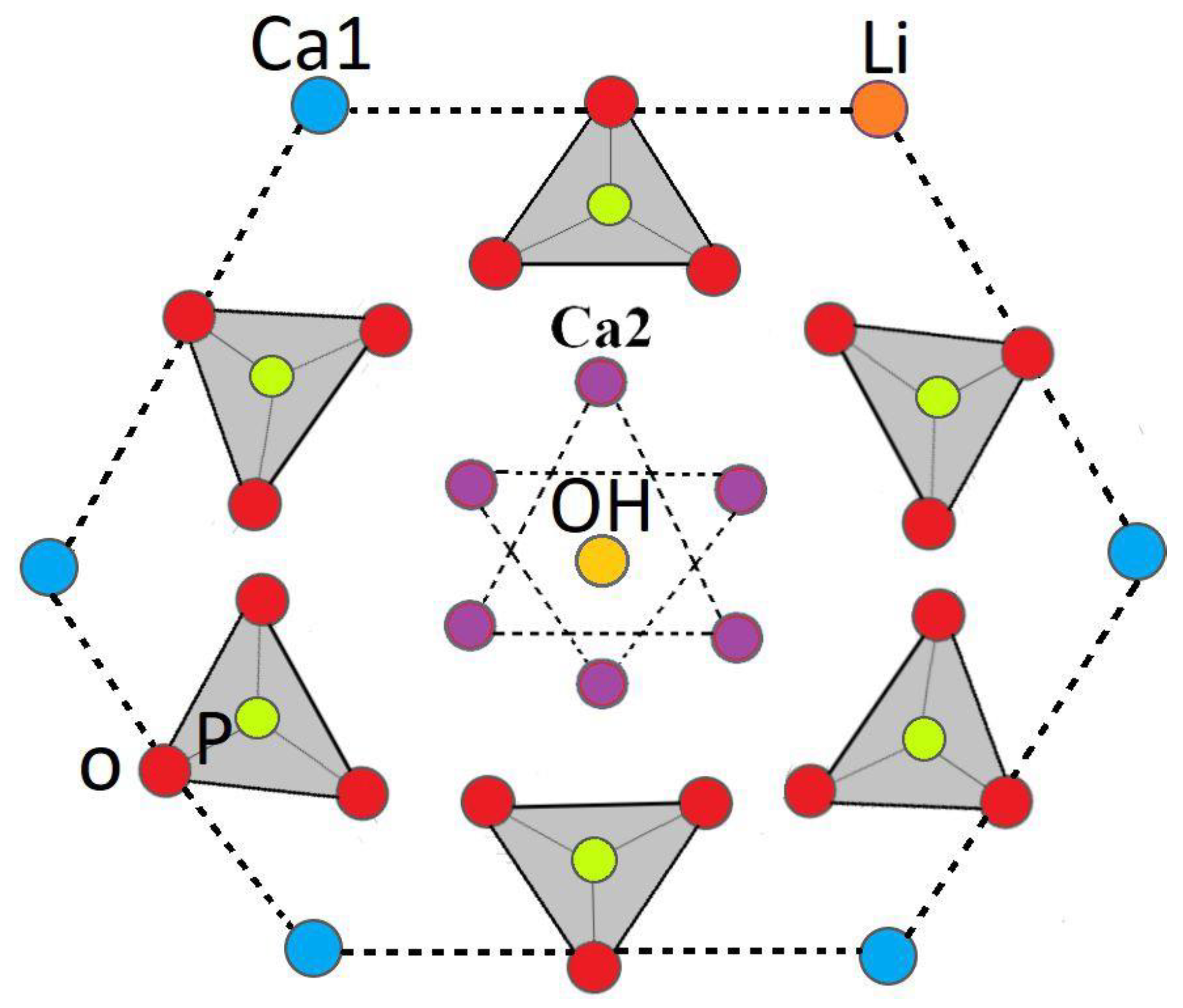
2.1. Characterization
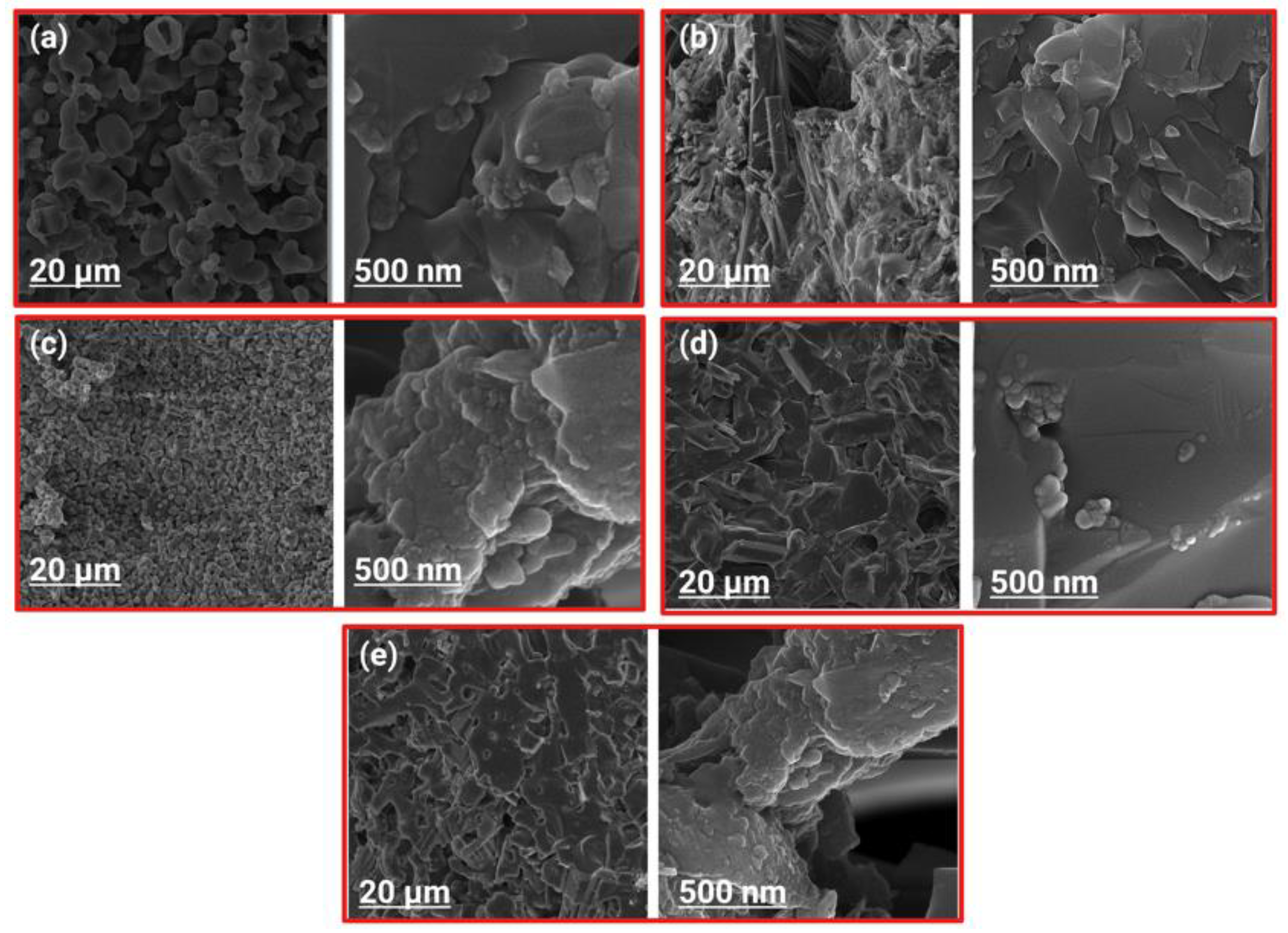
2.2. Bioactivity Behavior
Apatite Growth Ability
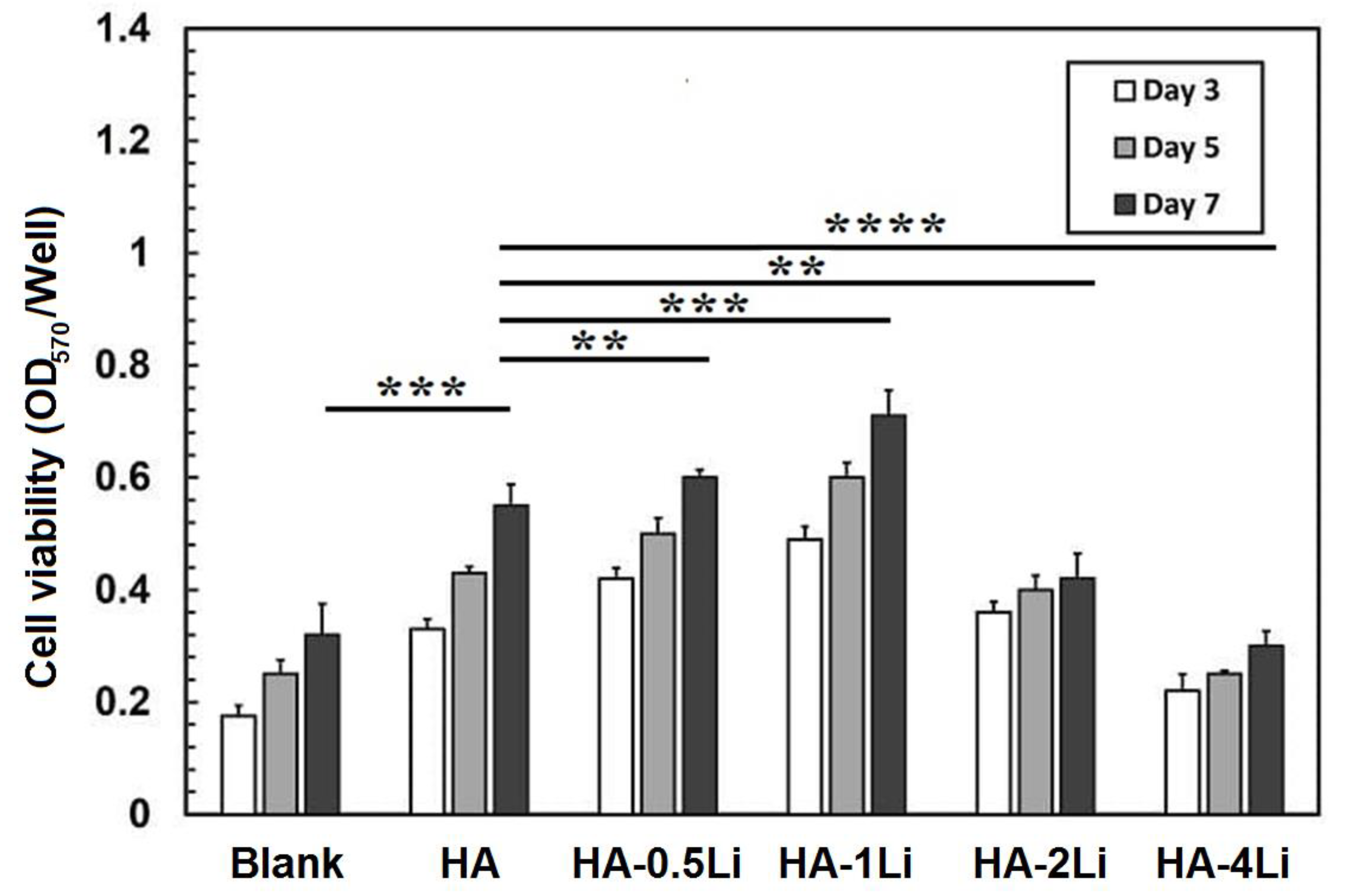
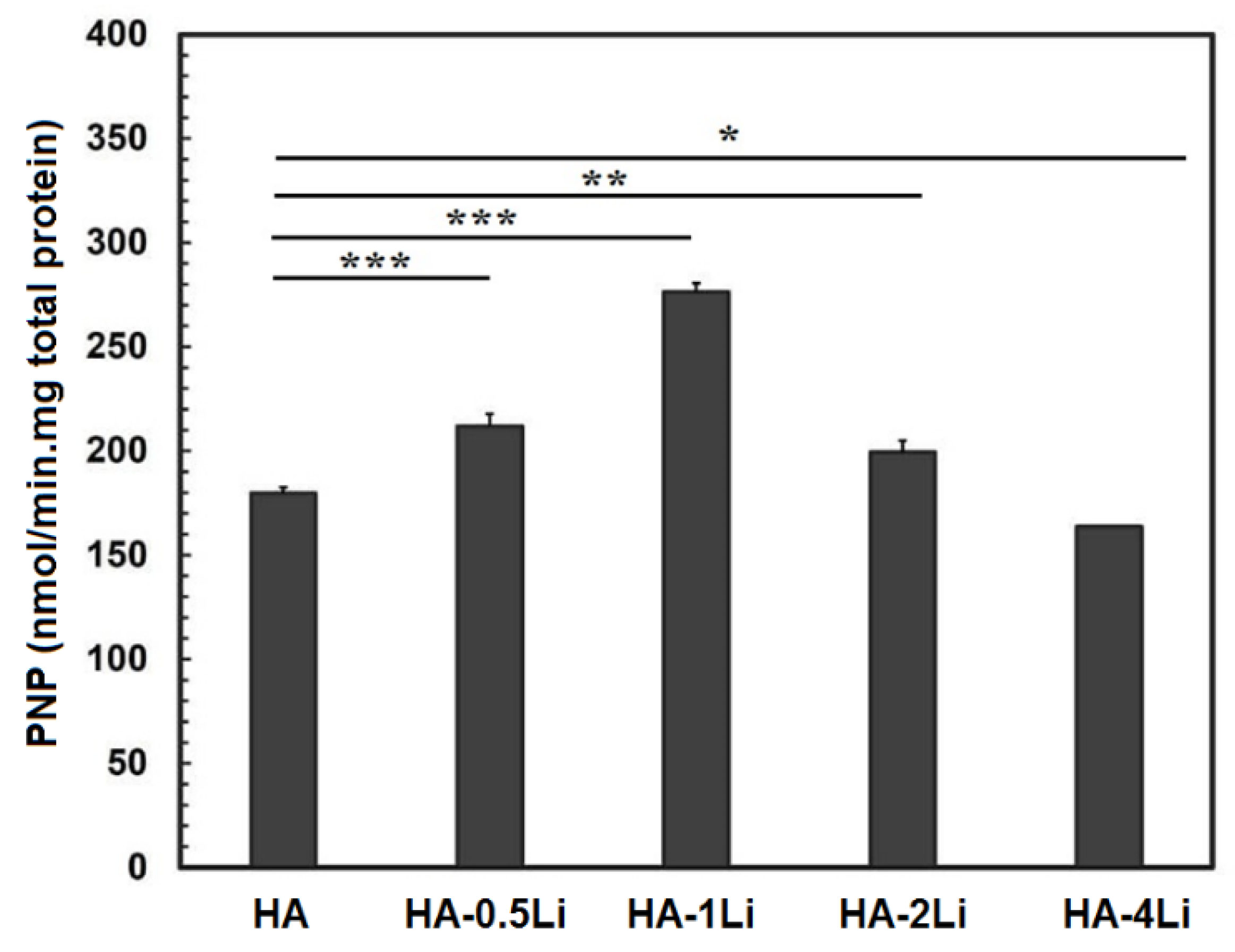
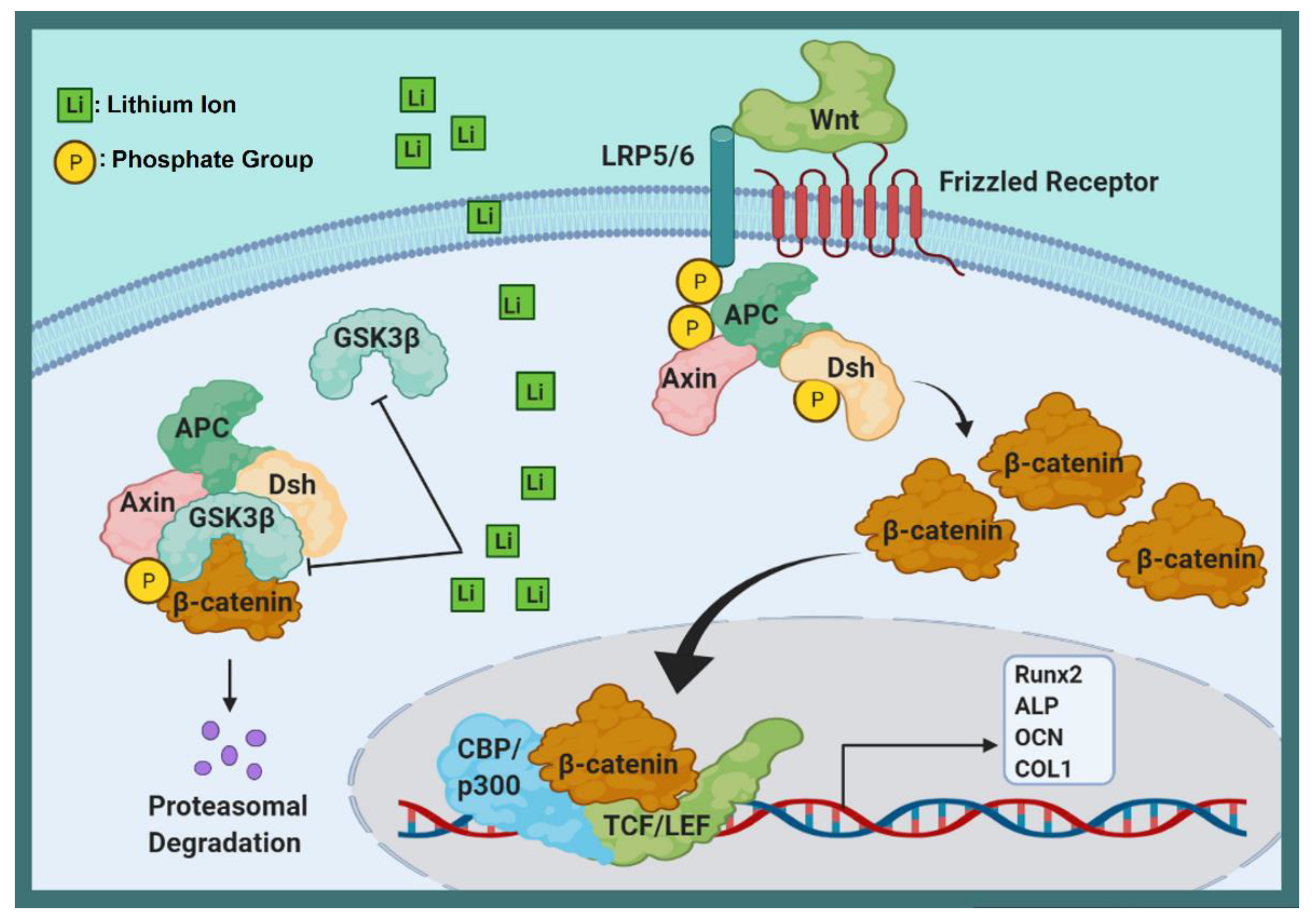
2.3. Biological Behavior
2.3.1. Cellular Behavior
2.3.2. Antibacterial Behavior
3. Discussion
4. Materials and Methods
4.1. Material Preparation
4.2. Characterization
4.3. Bioactivity Behavior
Apatite Growth Ability
4.4. Biological Behavior
4.4.1. Cellular Behavior
4.4.2. Antibacterial Behavior
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kahaie Khosrowshahi, A.; Khoshfetrat, A.B.; Khosrowshahi, Y.B.; Maleki-Ghaleh, H. Cobalt content modulates characteristics and osteogenic properties of cobalt-containing hydroxyapatite in in-vitro milieu. Mater. Today Commun. 2021, 27, 102392. [Google Scholar] [CrossRef]
- Mbarki, M.; Sharrock, P.; Fiallo, M.; ElFeki, H. Hydroxyapatite bioceramic with large porosity. Mater. Sci. Eng. C 2017, 76, 985–990. [Google Scholar] [CrossRef]
- Maleki-Ghaleh, H.; Khalil-Allafi, J.; Keikhosravani, P.; Etminanfar, M.R.; Behnamian, Y. Effect of Nano-zirconia on Microstructure and Biological Behavior of Hydroxyapatite-Based Bone Scaffolds. J. Mater. Eng. Perform. 2020, 29, 4412–4420. [Google Scholar] [CrossRef]
- Zhou, H.; Lee, J. Nanoscale hydroxyapatite particles for bone tissue engineering. Acta Biomater. 2011, 7, 2769–2781. [Google Scholar] [CrossRef]
- Evis, Z.; Webster, T.J. Nanosize hydroxyapatite: Doping with various ions. Adv. Appl. Ceram. 2011, 110, 311–321. [Google Scholar] [CrossRef]
- Maleki-Ghaleh, H.; Khalil-Allafi, J.; Horandghadim, N.; Keikhosravani, P.; Hosseini, M.G. Structural characterization, mechanical, and electrochemical studies of hydroxyapatite-titanium composite coating fabricated using electrophoretic deposition and reaction bonding process. J. Biomed. Mater. Res. Part B Appl. Biomater. 2020, 108, 2119–2130. [Google Scholar] [CrossRef]
- Šupová, M. Substituted hydroxyapatites for biomedical applications: A review. Ceram. Int. 2015, 41, 9203–9231. [Google Scholar] [CrossRef]
- Badran, H.; Yahia, I.S.; Hamdy, M.S.; Awwad, N.S. Lithium-doped hydroxyapatite nano-composites: Synthesis, characterization, gamma attenuation coefficient and dielectric properties. Radiat. Phys. Chem. 2017, 130, 85–91. [Google Scholar] [CrossRef]
- Kalita, S.J.; Bhatt, H.A. Nanocrystalline hydroxyapatite doped with magnesium and zinc: Synthesis and characterization. Mater. Sci. Eng. C 2007, 27, 837–848. [Google Scholar] [CrossRef]
- Yatongchai, C.; Wren, A.W.; Curran, D.J.; Hornez, J.-C.; Mark R, T. Comparison of the Weibull characteristics of hydroxyapatite and strontium doped hydroxyapatite. J. Mech. Behav. Biomed. Mater. 2013, 21, 95–108. [Google Scholar] [CrossRef] [PubMed]
- Kulanthaivel, S.; Mishra, U.; Agarwal, T.; Giri, S.; Pal, K.; Pramanik, K.; Banerjee, I. Improving the osteogenic and angiogenic properties of synthetic hydroxyapatite by dual doping of bivalent cobalt and magnesium ion. Ceram. Int. 2015, 41, 11323–11333. [Google Scholar] [CrossRef]
- Khalili, V.; Khalil-Allafi, J.; Maleki-Ghaleh, H.; Paulsen, A.; Frenzel, J.; Eggeler, G. The influence of Si as reactive bonding agent in the electrophoretic coatings of HA–Si–MWCNTs on NiTi alloys. J. Mater. Eng. Perform. 2016, 25, 390–400. [Google Scholar] [CrossRef]
- Uysal, I.; Severcan, F.; Tezcaner, A.; Evis, Z. Co-doping of hydroxyapatite with zinc and fluoride improves mechanical and biological properties of hydroxyapatite. Prog. Nat. Sci. Mater. Int. 2014, 24, 340–349. [Google Scholar] [CrossRef]
- Mardziah, C.; Sopyan, I.; Ramesh, S. Strontium-doped hydroxyapatite nanopowder via sol-gel method: Effect of strontium concentration and calcination temperature on phase behavior. Trends Biomater. Artif. Organs 2009, 23, 105–113. [Google Scholar]
- Suchanek, W.; Yashima, M.; Kakihana, M.; Yoshimura, M. Hydroxyapatite ceramics with selected sintering additives. Biomaterials 1997, 18, 923–933. [Google Scholar] [CrossRef]
- LeGeros, R.Z. Properties of osteoconductive biomaterials: Calcium phosphates. Clin. Orthop. Relat. Res. 2002, 395, 81–98. [Google Scholar] [CrossRef]
- Bose, S.; Fielding, G.; Tarafder, S.; Bandyopadhyay, A. Understanding of dopant-induced osteogenesis and angiogenesis in calcium phosphate ceramics. Trends Biotechnol. 2013, 31, 594–605. [Google Scholar] [CrossRef]
- Li, L.; Peng, X.; Qin, Y.; Wang, R.; Tang, J.; Cui, X.; Wang, T.; Liu, W.; Pan, H.; Li, B. Acceleration of bone regeneration by activating Wnt/β-catenin signalling pathway via lithium released from lithium chloride/calcium phosphate cement in osteoporosis. Sci. Rep. 2017, 7, 45204. [Google Scholar] [CrossRef]
- Kaygili, O.; Keser, S.; Ates, T.; Yakuphanoglu, F. Synthesis and characterization of lithium calcium phosphate ceramics. Ceram. Int. 2013, 39, 7779–7785. [Google Scholar] [CrossRef]
- Bose, S.; Fielding, G.; Tarafder, S.; Bandyopadhyay, A. Trace element doping in calcium phosphate ceramics to understand osteogenesis and angiogenesis. Trends Biotechnol. 2013, 31. [Google Scholar] [CrossRef]
- Trampuz, A.; Widmer, A.F. Infections associated with orthopedic implants. Curr. Opin. Infect. Dis. 2006, 19, 349–356. [Google Scholar] [CrossRef]
- Jabłońska, J.; Onyszko, M.; Konopacki, M.; Augustyniak, A.; Rakoczy, R.; Mijowska, E. Fabrication of Paper Sheets Coatings Based on Chitosan/Bacterial Nanocellulose/ZnO with Enhanced Antibacterial and Mechanical Properties. Int. J. Mol. Sci. 2021, 22, 7383. [Google Scholar] [CrossRef]
- Moghanian, A.; Firoozi, S.; Tahriri, M. Synthesis and in vitro studies of sol-gel derived lithium substituted 58S bioactive glass. Ceram. Int. 2017, 43, 12835–12843. [Google Scholar] [CrossRef]
- Rao, Y.; Wang, W.; Tan, F.; Cai, Y.; Lu, J.; Qiao, X. Sol–gel preparation and antibacterial properties of Li-doped MgO nanoplates. Ceram. Int. 2014, 40, 14397–14403. [Google Scholar] [CrossRef]
- Li, Y.; Liao, C.; Tjong, S.C. Recent Advances in Zinc Oxide Nanostructures with Antimicrobial Activities. Int. J. Mol. Sci. 2020, 21, 8836. [Google Scholar] [CrossRef] [PubMed]
- Kavitha, R.; Subha, B.; Shanmugam, S.; Ravichandran, K. Synthesis and invitro characterisation of lithium doped bioactive glass through quick alkali Sol-Gel method. Int. J. Innov. Res. Sci. Eng. 2014, 2, 2347–3207. [Google Scholar]
- Suryanarayana, C. Mechanical alloying and milling. Prog. Mater. Sci. 2001, 46, 1–184. [Google Scholar] [CrossRef]
- Bulina, N.V.; Chaikina, M.V.; Prosanov, I.Y.; Dudina, D.V.; Solovyov, L.A. Fast synthesis of La-substituted apatite by the dry mechanochemical method and analysis of its structure. J. Solid State Chem. 2017, 252, 93–99. [Google Scholar] [CrossRef]
- Fathi, M.; Zahrani, E.M. Mechanical alloying synthesis and bioactivity evaluation of nanocrystalline fluoridated hydroxyapatite. J. Cryst. Growth 2009, 311, 1392–1403. [Google Scholar] [CrossRef]
- Maleki-Ghaleh, H.; Khalili, V.; Khalil-Allafi, J.; Javidi, M. Hydroxyapatite coating on NiTi shape memory alloy by electrophoretic deposition process. Surf. Coat. Technol. 2012, 208, 57–63. [Google Scholar] [CrossRef]
- Vahabzadeh, S.; Hack, V.K.; Bose, S. Lithium-doped β-tricalcium phosphate: Effects on physical, mechanical and in vitro osteoblast cell–material interactions. J. Biomed. Mater. Res. Part B Appl. Biomater. 2017, 105, 391–399. [Google Scholar] [CrossRef]
- Karimi, M.; Hesaraki, S.; Alizadeh, M.; Kazemzadeh, A. Synthesis of calcium phosphate nanoparticles in deep-eutectic choline chloride–urea medium: Investigating the role of synthesis temperature on phase characteristics and physical properties. Ceram. Int. 2016, 42, 2780–2788. [Google Scholar] [CrossRef]
- Wang, X.; Andrews, L. Infrared spectra, structure and bonding in the LiO2, LiO2Li, LiO and Li2O molecules in solid neon. Mol. Phys. 2009, 107, 739–748. [Google Scholar] [CrossRef]
- Guo, H.; Wang, C.; Wang, J.; He, Y. Lithium-incorporated deproteinized bovine bone substitute improves osteogenesis in critical-sized bone defect repair. J. Biomater. Appl. 2018, 32, 1421–1434. [Google Scholar] [CrossRef] [PubMed]
- Baghaban Eslaminejad, M.; Talkhabi, M.; Zeynali, B. Effect of Lithium chloride on proliferation and bone differentiation of rat marrow-derived mesenchymal stem cells in culture. Iran. J. Basic Med Sci. 2008, 11, 143–151. [Google Scholar]
- Tang, L.; Chen, Y.; Pei, F.; Zhang, H. Lithium chloride modulates adipogenesis and osteogenesis of human bone marrow-derived mesenchymal stem cells. Cell. Physiol. Biochem. 2015, 37, 143–152. [Google Scholar] [CrossRef]
- Pisano, S.; Pozzi, M.; Catone, G.; Scrinzi, G.; Clementi, E.; Coppola, G.; Milone, A.; Bravaccio, C.; Santosh, P.; Masi, G. Putative mechanisms of action and clinical use of lithium in children and adolescents: A critical review. Curr. Neuropharmacol. 2019, 17, 318–341. [Google Scholar] [CrossRef]
- Sinha, D.; Wang, Z.; Ruchalski, K.L.; Levine, J.S.; Krishnan, S.; Lieberthal, W.; Schwartz, J.H.; Borkan, S.C. Lithium activates the Wnt and phosphatidylinositol 3-kinase Akt signaling pathways to promote cell survival in the absence of soluble survival factors. Am. J. Physiol.-Ren. Physiol. 2005, 288, F703–F713. [Google Scholar] [CrossRef]
- Rao, A.; Kremenevskaja, N.; Resch, J.; Brabant, G. Lithium stimulates proliferation in cultured thyrocytes by activating Wnt/β-catenin signalling. Eur. J. Endocrinol. 2005, 153, 929–938. [Google Scholar] [CrossRef]
- Vallée, A.; Vallée, J.-N.; Lecarpentier, Y. Parkinson’s Disease: Potential Actions of Lithium by Targeting the WNT/β-Catenin Pathway, Oxidative Stress, Inflammation and Glutamatergic Pathway. Cells 2021, 10, 230. [Google Scholar] [CrossRef]
- Fanovich, M.; Lopez, J.P. Influence of temperature and additives on the microstructure and sintering behaviour of hydroxyapatites with different Ca/P ratios. J. Mater. Sci. Mater. Med. 1998, 9, 53–60. [Google Scholar] [CrossRef]
- Bodhak, S.; Bose, S.; Bandyopadhyay, A. Influence of MgO, SrO, and ZnO dopants on electro-thermal polarization behavior and in vitro biological properties of hydroxyapatite ceramics. J. Am. Ceram. Soc. 2011, 94, 1281–1288. [Google Scholar] [CrossRef]
- Wang, Y.; Yang, X.; Gu, Z.; Qin, H.; Li, L.; Liu, J.; Yu, X. In vitro study on the degradation of lithium-doped hydroxyapatite for bone tissue engineering scaffold. Mater. Sci. Eng. C 2016, 66, 185–192. [Google Scholar] [CrossRef]
- Ahmed, W.; Zhai, Z.; Gao, C. Adaptive antibacterial biomaterial surfaces and their applications. Mater. Today Bio. 2019, 2, 100017. [Google Scholar] [CrossRef]
- Cacciotti, I. Handbook of Bioceramics and Biocomposites; Springer: Berlin, Germany, 2014; pp. 1–68. [Google Scholar]
- Brückner, R.; Tylkowski, M.; Hupa, L.; Brauer, D.S. Controlling the ion release from mixed alkali bioactive glasses by varying modifier ionic radii and molar volume. J. Mater. Chem. B 2016, 4, 3121–3134. [Google Scholar] [CrossRef] [PubMed]
- Fanovich, M.; Castro, M.; Lopez, J.P. Improvement of the microstructure and microhardness of hydroxyapatite ceramics by addition of lithium. Mater. Lett. 1998, 33, 269–272. [Google Scholar] [CrossRef]
- Lee, J.-A.; Lee, H.-C.; Heo, Y.-W.; Lee, J.-H.; Kim, J.-J. Effect of Li doping on sintering characteristics and microstructural behavior of yttria-stabilized zirconia. Ceram. Int. 2016, 42, 17339–17346. [Google Scholar] [CrossRef]
- Hannora, A.E.; Ataya, S. Structure and compression strength of hydroxyapatite/titania nanocomposites formed by high energy ball milling. J. Alloy. Compd. 2016, 658, 222–233. [Google Scholar] [CrossRef]
- Kim, H.-M.; Himeno, T.; Kokubo, T.; Nakamura, T. Process and kinetics of bonelike apatite formation on sintered hydroxyapatite in a simulated body fluid. Biomaterials 2005, 26, 4366–4373. [Google Scholar] [CrossRef]
- Basar, B.; Tezcaner, A.; Keskin, D.; Evis, Z. Improvements in microstructural, mechanical, and biocompatibility properties of nano-sized hydroxyapatites doped with yttrium and fluoride. Ceram. Int. 2010, 36, 1633–1643. [Google Scholar] [CrossRef]
- Miguez-Pacheco, V.; Büttner, T.; Maçon, A.; Jones, J.; Fey, T.; De Ligny, D.; Greil, P.; Chevalier, J.; Malchere, A.; Boccaccini, A. Development and characterization of lithium-releasing silicate bioactive glasses and their scaffolds for bone repair. J. Non-Cryst. Solids 2016, 432, 65–72. [Google Scholar] [CrossRef]
- da Silva, J.G.; Babb, R.; Salzlechner, C.; Sharpe, P.T.; Brauer, D.S.; Gentleman, E. Optimisation of lithium-substituted bioactive glasses to tailor cell response for hard tissue repair. J. Mater. Sci. 2017, 52, 8832–8844. [Google Scholar] [CrossRef] [PubMed]
- Maçon, A.L.; Jacquemin, M.; Page, S.J.; Li, S.; Bertazzo, S.; Stevens, M.M.; Hanna, J.V.; Jones, J.R. Lithium-silicate sol–gel bioactive glass and the effect of lithium precursor on structure–property relationships. J. Sol-Gel Sci. Technol. 2017, 81, 84–94. [Google Scholar] [CrossRef] [PubMed]
- Kar, S.; Jasuja, H.; Katti, D.R.; Katti, K.S. Wnt/β-Catenin Signaling Pathway Regulates Osteogenesis for Breast Cancer Bone Metastasis: Experiments in an In Vitro Nanoclay Scaffold Cancer Testbed. ACS Biomater. Sci. Eng. 2020, 6, 2600–2611. [Google Scholar] [CrossRef]
- Baron, R.; Rawadi, G. Targeting the Wnt/β-Catenin Pathway to Regulate Bone Formation in the Adult Skeleton. Endocrinology 2007, 148, 2635–2643. [Google Scholar] [CrossRef]
- Aubin, J.E.; Triffitt, J.T. Chapter 4—Mesenchymal Stem Cells and Osteoblast Differentiation. In Principles of Bone Biology, 2nd ed.; Bilezikian, J.P., Raisz, L.G., Rodan, G.A., Eds.; Academic Press: San Diego, CA, USA, 2002; pp. 59–81. [Google Scholar]
- Lecarpentier, Y.; Claes, V.; Vallée, A.; Hébert, J.-L. Interactions between PPAR Gamma and the Canonical Wnt/Beta-Catenin Pathway in Type 2 Diabetes and Colon Cancer. PPAR Res. 2017, 2017, 5879090. [Google Scholar] [CrossRef]
- Li, H.-X.; Luo, X.; Liu, R.-X.; Yang, Y.-J.; Yang, G.-S. Roles of Wnt/β-catenin signaling in adipogenic differentiation potential of adipose-derived mesenchymal stem cells. Mol. Cell. Endocrinol. 2008, 291, 116–124. [Google Scholar] [CrossRef]
- Sadat-Shojai, M.; Khorasani, M.T.; Dinpanah-Khoshdargi, E.; Jamshidi, A. Synthesis methods for nanosized hydroxyapatite with diverse structures. Acta Biomater. 2013, 9, 7591–7621. [Google Scholar] [CrossRef]
- An, Y.H.; Yu, S.J.; Kim, I.S.; Kim, S.H.; Moon, J.M.; Kim, S.L.; Choi, Y.H.; Choi, J.S.; Im, S.G.; Lee, K.E.; et al. Hydrogel Functionalized Janus Membrane for Skin Regeneration. Adv. Healthc. Mater. 2017, 6, 1600795. [Google Scholar] [CrossRef]
- Kimelman, D.; Xu, W. β-Catenin destruction complex: Insights and questions from a structural perspective. Oncogene 2006, 25, 7482–7491. [Google Scholar] [CrossRef]
- Parker, T.W.; Neufeld, K.L. APC controls Wnt-induced β-catenin destruction complex recruitment in human colonocytes. Sci. Rep. 2020, 10, 2957. [Google Scholar] [CrossRef]
- Jeong, W.J.; Ro, E.J.; Choi, K.Y. Interaction between Wnt/β-catenin and RAS-ERK pathways and an anti-cancer strategy via degradations of β-catenin and RAS by targeting the Wnt/β-catenin pathway. NPJ Precis Oncol. 2018, 2, 5. [Google Scholar] [CrossRef] [PubMed]
- Chiarini, F.; Paganelli, F.; Martelli, A.M.; Evangelisti, C. The Role Played by Wnt/β-Catenin Signaling Pathway in Acute Lymphoblastic Leukemia. Int. J. Mol. Sci. 2020, 21, 1098. [Google Scholar] [CrossRef]
- González-Sancho, J.M.; Brennan, K.R.; Castelo-Soccio, L.A.; Brown, A.M.C. Wnt proteins induce dishevelled phosphorylation via an LRP5/6- independent mechanism, irrespective of their ability to stabilize beta-catenin. Mol. Cell Biol. 2004, 24, 4757–4768. [Google Scholar] [CrossRef]
- Nishikawa, K.; Osawa, Y.; Kimura, K. Wnt/β-Catenin Signaling as a Potential Target for the Treatment of Liver Cirrhosis Using Antifibrotic Drugs. Int. J. Mol. Sci. 2018, 19, 3103. [Google Scholar] [CrossRef]
- Khosla, S.; Westendorf, J.J.; Oursler, M.J. Building bone to reverse osteoporosis and repair fractures. J. Clin. Investig. 2008, 118, 421–428. [Google Scholar] [CrossRef] [PubMed]
- Meszaros, K.; Patocs, A. Glucocorticoids Influencing Wnt/β-Catenin Pathway; Multiple Sites, Heterogeneous Effects. Molecules 2020, 25, 1489. [Google Scholar] [CrossRef] [PubMed]
- Hong, G.; He, X.; Shen, Y.; Chen, X.; Yang, F.; Yang, P.; Pang, F.; Han, X.; He, W.; Wei, Q. Chrysosplenetin promotes osteoblastogenesis of bone marrow stromal cells via Wnt/β-catenin pathway and enhances osteogenesis in estrogen deficiency-induced bone loss. Stem. Cell Res. Ther. 2019, 10, 277. [Google Scholar] [CrossRef]
- Wong, S.K.; Chin, K.-Y.; Ima-Nirwana, S. The Skeletal-Protecting Action and Mechanisms of Action for Mood-Stabilizing Drug Lithium Chloride: Current Evidence and Future Potential Research Areas. Front. Pharmacol. 2020, 11. [Google Scholar] [CrossRef]
- Liu, W.; Chen, D.; Jiang, G.; Li, Q.; Wang, Q.; Cheng, M.; He, G.; Zhang, X. A lithium-containing nanoporous coating on entangled titanium scaffold can enhance osseointegration through Wnt/β-catenin pathway. Nanomedicine 2018, 14, 153–164. [Google Scholar] [CrossRef]
- Ma, Y.; Li, Y.; Hao, J.; Ma, B.; Di, T.; Dong, H. Evaluation of the degradation, biocompatibility and osteogenesis behavior of lithium-doped calcium polyphosphate for bone tissue engineering. Biomed. Mater. Eng. 2019, 30, 23–36. [Google Scholar] [CrossRef] [PubMed]
- Rodda, S.J.; McMahon, A.P. Distinct roles for Hedgehog and canonical Wnt signaling in specification, differentiation and maintenance of osteoblast progenitors. Development 2006, 133, 3231–3244. [Google Scholar] [CrossRef]
- Shi, X.; Wang, J.; Lei, Y.; Cong, C.; Tan, D.; Zhou, X. Research progress on the PI3K/AKT signaling pathway in gynecological cancer (Review). Mol. Med. Rep. 2019, 19, 4529–4535. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Kim, N. Regulation of NFATc1 in Osteoclast Differentiation. J. Bone Metab. 2014, 21, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.B.; Kim, J.H.; Kim, K.; Youn, B.U.; Ko, A.; Lee, S.Y.; Kim, N. Akt induces osteoclast differentiation through regulating the GSK3β/NFATc1 signaling cascade. J. Immunol. 2012, 188, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.J.; Yeon, J.T.; Choi, S.W.; Moon, S.H.; Ryu, B.J.; Yu, R.; Park, S.J.; Kim, S.H.; Son, Y.J. Decursin inhibits osteoclastogenesis by downregulating NFATc1 and blocking fusion of pre-osteoclasts. Bone 2015, 81, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Nikaido, H.; Vaara, M. Molecular basis of bacterial outer membrane permeability. Microbiol. Rev. 1985, 49, 1–32. [Google Scholar] [CrossRef]
- Novikova, O.D.; Solovyeva, T.F. Nonspecific porins of the outer membrane of Gram-negative bacteria: Structure and functions. Biochem. (Mosc.) Suppl. Ser. A Membr. Cell Biol. 2009, 3, 3–15. [Google Scholar] [CrossRef]
- Madigan, M.T.; Brock, T.; Martinko, J.; Clark, D.P.; Dunlap, P. Brock Biology of Microorganisms; Pearson/Benjamin Cummings: San Francisco, CA, USA, 2009. [Google Scholar]
- Sizar, O.; Unakal, C.G. Gram Positive Bacteria. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Tian, Q.; Ye, J.; Yuan, W.; Zhang, S.; Shi, L.; Zhong, J.; Ning, G. Highly effective antibacterial activity of lithium-doped magnesium oxide particles synthesized by the microwave-assisted hydrothermal route. Powder Technol. 2020, 371, 130–141. [Google Scholar] [CrossRef]
- Tsao, N.; Kuo, C.-F.; Chiu, C.-C.; Lin, W.-C.; Huang, W.-H.; Chen, L.-Y. Protection against Klebsiella pneumoniae using lithium chloride in an intragastric infection model. Antimicrob. Agents Chemother. 2015, 59, 1525–1533. [Google Scholar] [CrossRef][Green Version]
- Maleki-Ghaleh, H.; Hossein Siadati, M.; Fallah, A.; Zarrabi, A.; Afghah, F.; Koc, B.; Dalir Abdolahinia, E.; Omidi, Y.; Barar, J.; Akbari-Fakhrabadi, A.; et al. Effect of zinc-doped hydroxyapatite/graphene nanocomposite on the physicochemical properties and osteogenesis differentiation of 3D-printed polycaprolactone scaffolds for bone tissue engineering. Chem. Eng. J. 2021, 426, 131321. [Google Scholar] [CrossRef]
- Sun, Y.; Yang, H.; Tao, D. Preparation and characterization of Eu3+-doped fluorapatite nanoparticles by a hydrothermal method. Ceram. Int. 2012, 38, 6937–6941. [Google Scholar] [CrossRef]
- Goehner, R. Background subtract subroutine for spectral data. Anal. Chem. 1978, 50, 1223–1225. [Google Scholar] [CrossRef]
- Landi, E.; Tampieri, A.; Celotti, G.; Sprio, S. Densification behaviour and mechanisms of synthetic hydroxyapatites. J. Eur. Ceram. Soc. 2000, 20, 2377–2387. [Google Scholar] [CrossRef]
- Kokubo, T.; Takadama, H. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials 2006, 27, 2907–2915. [Google Scholar] [CrossRef] [PubMed]
- Navale, G.R.; Rout, C.S.; Gohil, K.N.; Dharne, M.S.; Late, D.J.; Shinde, S.S. Oxidative and membrane stress-mediated antibacterial activity of WS2 and rGO-WS2 nanosheets. RSC Adv. 2015, 5, 74726–74733. [Google Scholar] [CrossRef]





| Sample | Lattice Parameters (nm) | Unit Cell Volume (nm) | Crystallinity (%) |
|---|---|---|---|
| HA | a = b = 0.9422; c = 0.6886 | 0.5298 | 95 |
| HA-0.5Li | a = b = 0.9415; c = 0.6882 | 0.5287 | 97 |
| HA-1Li | a = b = 0.9411; c = 0.6880 | 0.5281 | 98 |
| HA-2Li | a = b = 0.9417; c = 0.6883 | 0.5290 | 96 |
| HA-4Li | a = b = 0.9420; c = 0.6887 | 0.5297 | 96 |
| Sample | Crystallite Size (nm) | Relative Density (%) |
|---|---|---|
| HA | 88.5 | 90.12 |
| HA-0.5Li | 71.2 | 92.32 |
| HA-1Li | 59.3 | 95.48 |
| HA-2Li | 75.6 | 91.17 |
| HA-4Li | 81.4 | 90.87 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keikhosravani, P.; Maleki-Ghaleh, H.; Kahaie Khosrowshahi, A.; Bodaghi, M.; Dargahi, Z.; Kavanlouei, M.; Khademi-Azandehi, P.; Fallah, A.; Beygi-Khosrowshahi, Y.; Siadati, M.H. Bioactivity and Antibacterial Behaviors of Nanostructured Lithium-Doped Hydroxyapatite for Bone Scaffold Application. Int. J. Mol. Sci. 2021, 22, 9214. https://doi.org/10.3390/ijms22179214
Keikhosravani P, Maleki-Ghaleh H, Kahaie Khosrowshahi A, Bodaghi M, Dargahi Z, Kavanlouei M, Khademi-Azandehi P, Fallah A, Beygi-Khosrowshahi Y, Siadati MH. Bioactivity and Antibacterial Behaviors of Nanostructured Lithium-Doped Hydroxyapatite for Bone Scaffold Application. International Journal of Molecular Sciences. 2021; 22(17):9214. https://doi.org/10.3390/ijms22179214
Chicago/Turabian StyleKeikhosravani, Pardis, Hossein Maleki-Ghaleh, Amir Kahaie Khosrowshahi, Mahdi Bodaghi, Ziba Dargahi, Majid Kavanlouei, Pooriya Khademi-Azandehi, Ali Fallah, Younes Beygi-Khosrowshahi, and M. Hossein Siadati. 2021. "Bioactivity and Antibacterial Behaviors of Nanostructured Lithium-Doped Hydroxyapatite for Bone Scaffold Application" International Journal of Molecular Sciences 22, no. 17: 9214. https://doi.org/10.3390/ijms22179214
APA StyleKeikhosravani, P., Maleki-Ghaleh, H., Kahaie Khosrowshahi, A., Bodaghi, M., Dargahi, Z., Kavanlouei, M., Khademi-Azandehi, P., Fallah, A., Beygi-Khosrowshahi, Y., & Siadati, M. H. (2021). Bioactivity and Antibacterial Behaviors of Nanostructured Lithium-Doped Hydroxyapatite for Bone Scaffold Application. International Journal of Molecular Sciences, 22(17), 9214. https://doi.org/10.3390/ijms22179214








