Influence of POR*28 Polymorphisms on CYP3A5*3-Associated Variations in Tacrolimus Blood Levels at an Early Stage after Liver Transplantation
Abstract
1. Introduction
2. Results
2.1. Patients’ Characteristics
2.2. Demographics of Genetic Polymorphisms
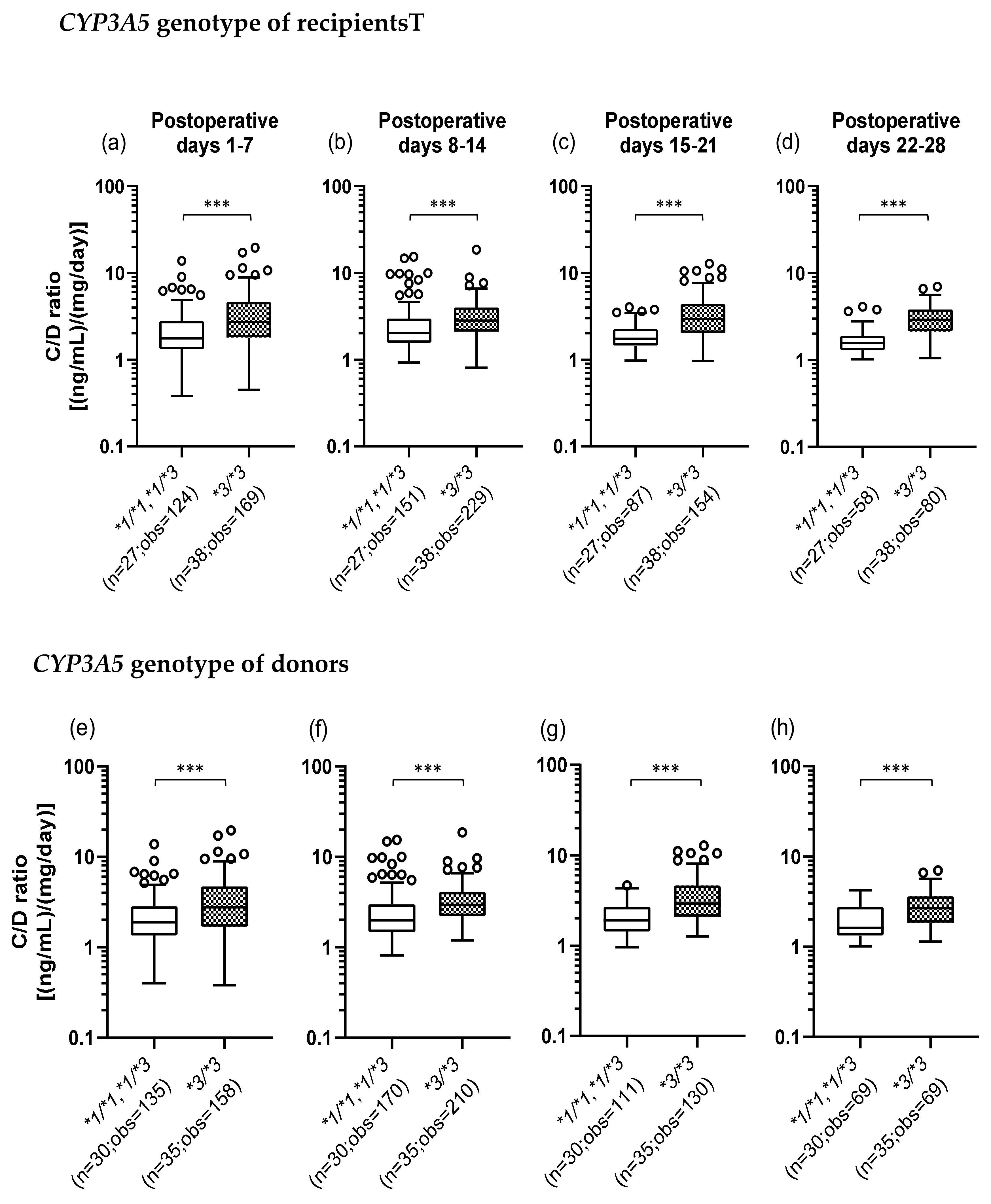
2.3. Influence of the Recipient’s or Donor’s CYP3A5 Polymorphism on the TAC C/D Ratio during the First Month Following Liver Transplantation
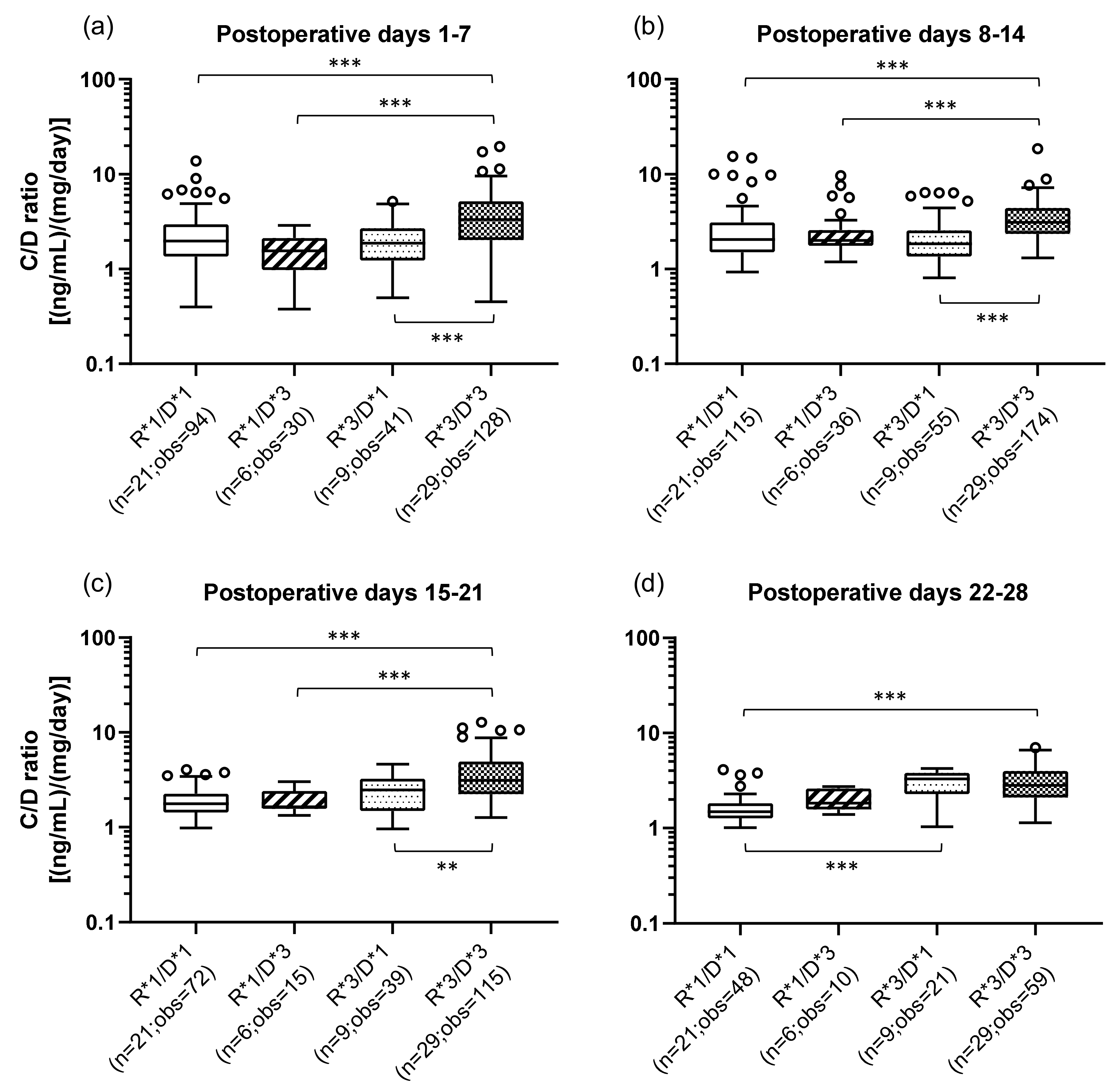
2.4. Influence of the Combination of the Recipient’s and Donor’s CYP3A5 Polymorphisms on the TAC C/D Ratio during the First Month Following Liver Transplantation
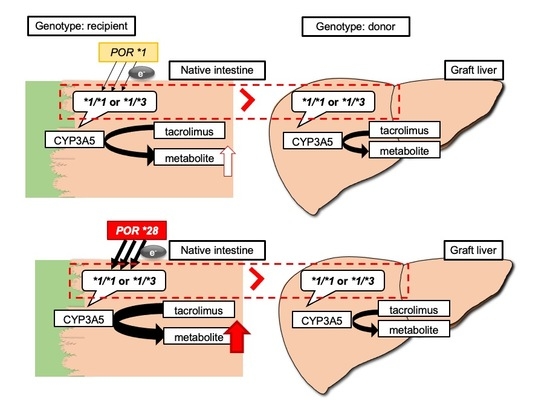
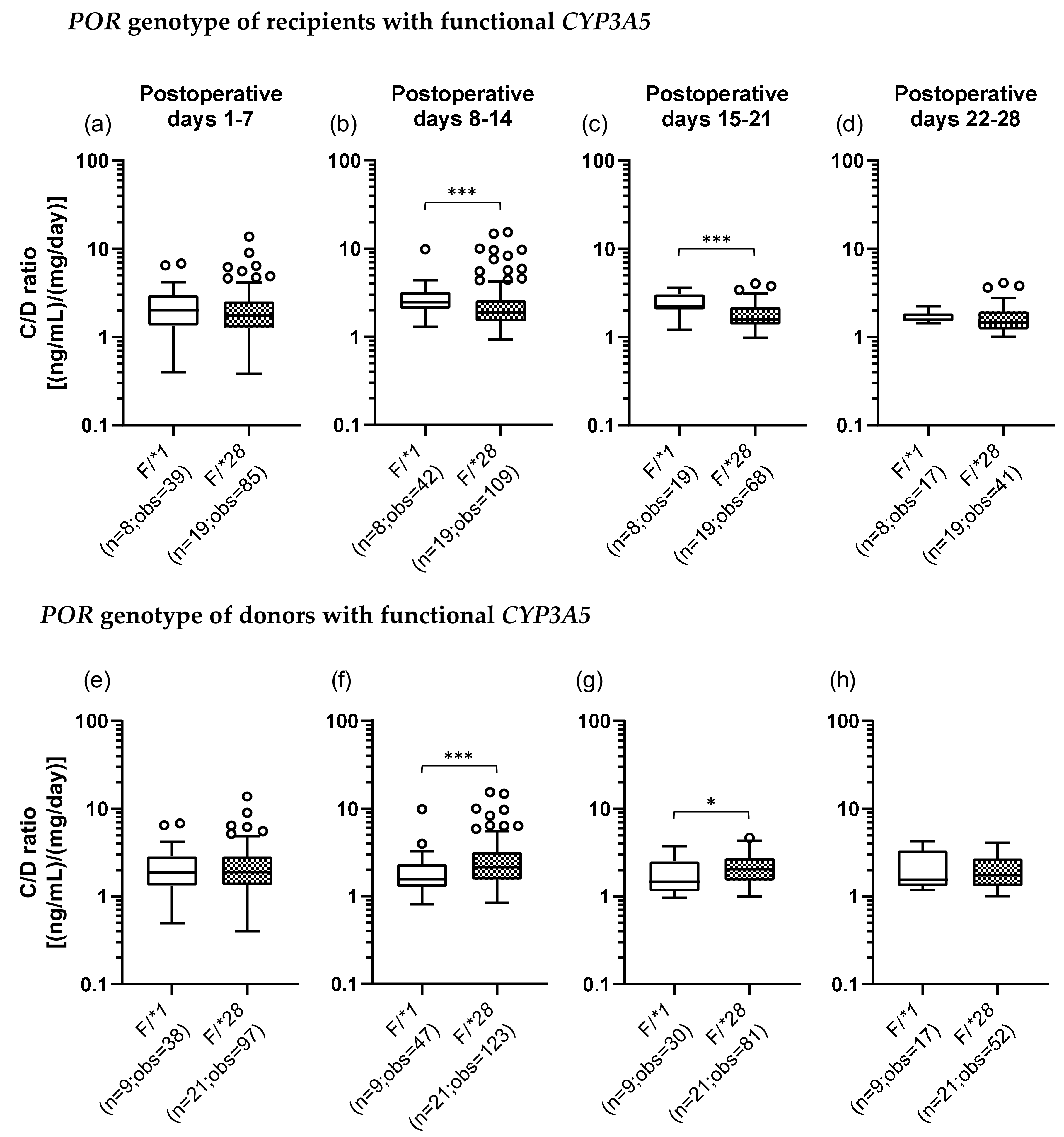
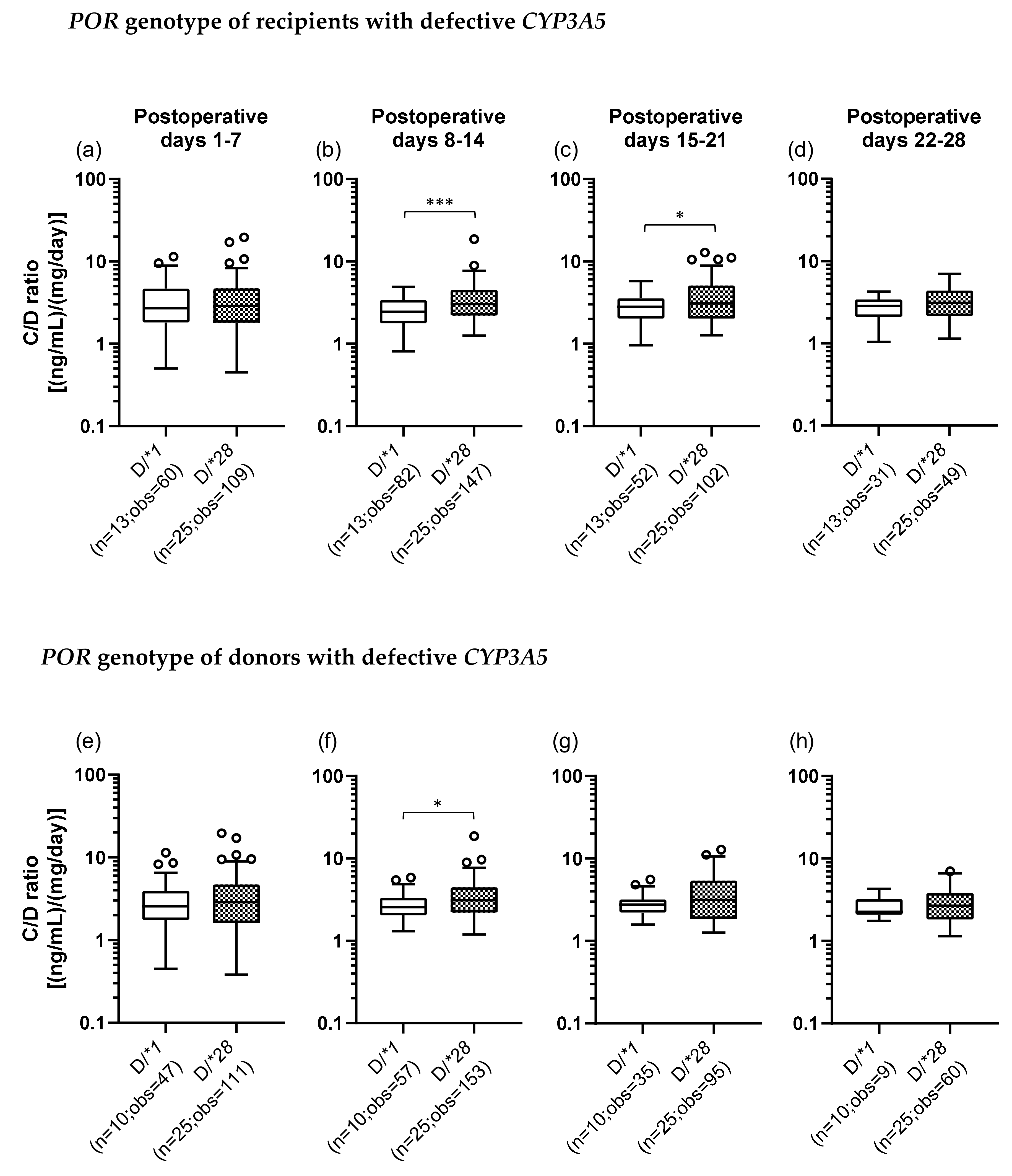
2.5. Impact of Recipient’s or Donor’s POR*28 Genotype on the TAC C/D Ratio Requirement of a CYP3A5 Expressor or Non-Expressor during the First Month Following LIVER transplantation
2.6. Examination of Factors Affecting the TAC C/D Ratio Using Multiple Regression Analysis
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. DNA Extraction and Genotyping of the CYP3A5*3 and POR*28 Polymorphisms
4.3. TAC Trough Concentration Measurement and Immunosuppression Protocol
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kahan, B.D.; Keown, P.; Levy, G.A.; Johnston, A. Therapeutic drug monitoring of immunosuppressant drugs in clinical practice. Clin. Ther. 2002, 24, 330–350. [Google Scholar] [CrossRef]
- Brunet, M.; van Gelder, T.; Asberg, A.; Haufroid, V.; Hesselink, D.A.; Langman, L.; Lemaitre, F.; Marquet, P.; Seger, C.; Shipkova, M.; et al. Therapeutic Drug Monitoring of Tacrolimus-Personalized Therapy: Second Consensus Report. Ther. Drug Monit. 2019, 41, 261–307. [Google Scholar] [CrossRef] [PubMed]
- Staatz, C.E.; Tett, S.E. Clinical pharmacokinetics and pharmacodynamics of tacrolimus in solid organ transplantation. Clin. Pharm. 2004, 43, 623–653. [Google Scholar] [CrossRef] [PubMed]
- Masuda, S.; Inui, K. An up-date review on individualized dosage adjustment of calcineurin inhibitors in organ transplant patients. Pharmacol. Ther. 2006, 112, 184–198. [Google Scholar] [CrossRef]
- Wilkinson, G.R. Drug metabolism and variability among patients in drug response. N. Engl. J. Med. 2005, 352, 2211–2221. [Google Scholar] [CrossRef]
- de Jonge, H.; de Loor, H.; Verbeke, K.; Vanrenterghem, Y.; Kuypers, D.R. In vivo CYP3A4 activity, CYP3A5 genotype, and hematocrit predict tacrolimus dose requirements and clearance in renal transplant patients. Clin. Pharmacol. Ther. 2012, 92, 366–375. [Google Scholar] [CrossRef]
- Hesselink, D.A.; van Schaik, R.H.; van der Heiden, I.P.; van der Werf, M.; Gregoor, P.J.; Lindemans, J.; Weimar, W.; van Gelder, T. Genetic polymorphisms of the CYP3A4, CYP3A5, and MDR-1 genes and pharmacokinetics of the calcineurin inhibitors cyclosporine and tacrolimus. Clin. Pharmacol. Ther. 2003, 74, 245–254. [Google Scholar] [CrossRef]
- Haufroid, V.; Mourad, M.; Van Kerckhove, V.; Wawrzyniak, J.; De Meyer, M.; Eddour, D.C.; Malaise, J.; Lison, D.; Squifflet, J.P.; Wallemacq, P. The effect of CYP3A5 and MDR1 (ABCB1) polymorphisms on cyclosporine and tacrolimus dose requirements and trough blood levels in stable renal transplant patients. Pharmacogenetics 2004, 14, 147–154. [Google Scholar] [CrossRef]
- Press, R.R.; Ploeger, B.A.; den Hartigh, J.; van der Straaten, T.; van Pelt, J.; Danhof, M.; de Fijter, J.W.; Guchelaar, H.J. Explaining variability in tacrolimus pharmacokinetics to optimize early exposure in adult kidney transplant recipients. Ther. Drug Monit. 2009, 31, 187–197. [Google Scholar] [CrossRef]
- Ruiz, J.; Herrero, M.J.; Boso, V.; Megias, J.E.; Hervas, D.; Poveda, J.L.; Escriva, J.; Pastor, A.; Sole, A.; Alino, S.F. Impact of Single Nucleotide Polymorphisms (SNPs) on Immunosuppressive Therapy in Lung Transplantation. Int. J. Mol. Sci. 2015, 16, 20168–20182. [Google Scholar] [CrossRef]
- Yang, T.H.; Chen, Y.K.; Xue, F.; Han, L.Z.; Shen, C.H.; Zhou, T.; Luo, Y.; Zhang, J.J.; Xia, Q. Influence of CYP3A5 genotypes on tacrolimus dose requirement: Age and its pharmacological interaction with ABCB1 genetics in the Chinese paediatric liver transplantation. Int. J. Clin. Pract. 2015, 183, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Picard, N.; Bergan, S.; Marquet, P.; van Gelder, T.; Wallemacq, P.; Hesselink, D.A.; Haufroid, V. Pharmacogenetic Biomarkers Predictive of the Pharmacokinetics and Pharmacodynamics of Immunosuppressive Drugs. Ther. Drug Monit. 2016, 38, S57–S69. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, M.E.; Schladt, D.P.; Guan, W.; Wu, B.; van Setten, J.; Keating, B.J.; Ikle, D.; Remmel, R.P.; Dorr, C.R.; Mannon, R.B.; et al. Tacrolimus troughs and genetic determinants of metabolism in kidney transplant recipients: A comparison of four ancestry groups. Am. J. Transplant. 2019, 19, 2795–2804. [Google Scholar] [CrossRef] [PubMed]
- Kuehl, P.; Zhang, J.; Lin, Y.; Lamba, J.; Assem, M.; Schuetz, J.; Watkins, P.B.; Daly, A.; Wrighton, S.A.; Hall, S.D.; et al. Sequence diversity in CYP3A promoters and characterization of the genetic basis of polymorphic CYP3A5 expression. Nat. Genet. 2001, 27, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Lamba, J.K.; Lin, Y.S.; Schuetz, E.G.; Thummel, K.E. Genetic contribution to variable human CYP3A-mediated metabolism. Adv. Drug Deliv. Rev. 2002, 54, 1271–1294. [Google Scholar] [CrossRef]
- Hart, S.N.; Zhong, X.B. P450 oxidoreductase: Genetic polymorphisms and implications for drug metabolism and toxicity. Expert Opin. Drug Metab. Toxicol. 2008, 4, 439–452. [Google Scholar] [CrossRef]
- Fluck, C.E.; Tajima, T.; Pandey, A.V.; Arlt, W.; Okuhara, K.; Verge, C.F.; Jabs, E.W.; Mendonca, B.B.; Fujieda, K.; Miller, W.L. Mutant P450 oxidoreductase causes disordered steroidogenesis with and without Antley-Bixler syndrome. Nat. Genet. 2004, 36, 228–230. [Google Scholar] [CrossRef]
- Huang, N.; Pandey, A.V.; Agrawal, V.; Reardon, W.; Lapunzina, P.D.; Mowat, D.; Jabs, E.W.; Van Vliet, G.; Sack, J.; Fluck, C.E.; et al. Diversity and function of mutations in p450 oxidoreductase in patients with Antley-Bixler syndrome and disordered steroidogenesis. Am. J. Hum. Genet. 2005, 76, 729–749. [Google Scholar] [CrossRef]
- Huang, N.; Agrawal, V.; Giacomini, K.M.; Miller, W.L. Genetics of P450 oxidoreductase: Sequence variation in 842 individuals of four ethnicities and activities of 15 missense mutations. Proc. Natl. Acad. Sci. USA 2008, 105, 1733–1738. [Google Scholar] [CrossRef]
- Fluck, C.E.; Nicolo, C.; Pandey, A.V. Clinical, structural and functional implications of mutations and polymorphisms in human NADPH P450 oxidoreductase. Fundam. Clin. Pharmacol. 2007, 21, 399–410. [Google Scholar] [CrossRef]
- de Jonge, H.; Metalidis, C.; Naesens, M.; Lambrechts, D.; Kuypers, D.R. The P450 oxidoreductase *28 SNP is associated with low initial tacrolimus exposure and increased dose requirements in CYP3A5-expressing renal recipients. Pharmacogenomics 2011, 12, 1281–1291. [Google Scholar] [CrossRef] [PubMed]
- Elens, L.; Hesselink, D.A.; Bouamar, R.; Budde, K.; de Fijter, J.W.; De Meyer, M.; Mourad, M.; Kuypers, D.R.; Haufroid, V.; van Gelder, T.; et al. Impact of POR*28 on the pharmacokinetics of tacrolimus and cyclosporine A in renal transplant patients. Ther. Drug Monit. 2014, 36, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Lunde, I.; Bremer, S.; Midtvedt, K.; Mohebi, B.; Dahl, M.; Bergan, S.; Asberg, A.; Christensen, H. The influence of CYP3A, PPARA, and POR genetic variants on the pharmacokinetics of tacrolimus and cyclosporine in renal transplant recipients. Eur. J. Clin. Pharmacol. 2014, 70, 685–693. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.J.; Liu, S.B.; Xue, L.; Ding, X.L.; Zhang, H.; Miao, L.Y. The genetic polymorphisms of POR*28 and CYP3A5*3 significantly influence the pharmacokinetics of tacrolimus in Chinese renal transplant recipients. Int. J. Clin. Pharmacol. Ther. 2015, 53, 728–736. [Google Scholar] [CrossRef] [PubMed]
- Almeida-Paulo, G.N.; Dapia Garcia, I.; Lubomirov, R.; Borobia, A.M.; Alonso-Sanchez, N.L.; Espinosa, L.; Carcas-Sansuan, A.J. Weight of ABCB1 and POR genes on oral tacrolimus exposure in CYP3A5 nonexpressor pediatric patients with stable kidney transplant. Pharm. J. 2018, 18, 180–186. [Google Scholar] [CrossRef] [PubMed]
- 1000-Genomes-Project-Consortium; Auton, A.; Brooks, L.D.; Durbin, R.M.; Garrison, E.P.; Kang, H.M.; Korbel, J.O.; Marchini, J.L.; McCarthy, S.; McVean, G.A. A global reference for human genetic variation. Nature 2015, 526, 68–74. [Google Scholar]
- Gómez-Bravo, M.A.; Salcedo, M.; Fondevila, C.; Suarez, F.; Castellote, J.; Rufian, S.; Pons, J.A.; Alamo, J.M.; Millán, O.; Brunet, M. Impact of donor and recipient CYP3A5 and ABCB1 genetic polymorphisms on tacrolimus dosage requirements and rejection in Caucasian Spanish liver transplant patients. J. Clin. Pharmacol. 2013, 53, 1146–1154. [Google Scholar] [CrossRef]
- Goto, M.; Masuda, S.; Kiuchi, T.; Ogura, Y.; Oike, F.; Okuda, M.; Tanaka, K.; Inui, K. CYP3A5*1-carrying graft liver reduces the concentration/oral dose ratio of tacrolimus in recipients of living-donor liver transplantation. Pharmacogenetics 2004, 14, 471–478. [Google Scholar] [CrossRef]
- Uesugi, M.; Masuda, S.; Katsura, T.; Oike, F.; Takada, Y.; Inui, K.-I. Effect of intestinal CYP3A5 on postoperative tacrolimus trough levels in living-donor liver transplant recipients. Pharm. Genom. 2006, 16, 119–127. [Google Scholar] [CrossRef]
- Uesugi, M.; Kikuchi, M.; Shinke, H.; Omura, T.; Yonezawa, A.; Matsubara, K.; Fujimoto, Y.; Okamoto, S.; Kaido, T.; Uemoto, S.; et al. Impact of cytochrome P450 3A5 polymorphism in graft livers on the frequency of acute cellular rejection in living-donor liver transplantation. Pharm. Genom. 2014, 24, 356–366. [Google Scholar] [CrossRef]
- Ji, E.; Choi, L.; Suh, K.-S.; Cho, J.-Y.; Han, N.; Oh, J.M. Combinational effect of intestinal and hepatic CYP3A5 genotypes on tacrolimus pharmacokinetics in recipients of living donor liver transplantation. Transplantation 2012, 94, 866–872. [Google Scholar] [CrossRef] [PubMed]
- Wolbold, R.; Klein, K.; Burk, O.; Nussler, A.K.; Neuhaus, P.; Eichelbaum, M.; Schwab, M.; Zanger, U.M. Sex is a major determinant of CYP3A4 expression in human liver. Hepatology 2003, 38, 978–988. [Google Scholar] [CrossRef] [PubMed]
- Lamba, V.; Panetta, J.C.; Strom, S.; Schuetz, E.G. Genetic predictors of interindividual variability in hepatic CYP3A4 expression. J. Pharmacol. Exp. Ther. 2010, 332, 1088–1099. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Zhang, B.; Molony, C.; Chudin, E.; Hao, K.; Zhu, J.; Gaedigk, A.; Suver, C.; Zhong, H.; Leeder, J.S.; et al. Systematic genetic and genomic analysis of cytochrome P450 enzyme activities in human liver. Genome Res. 2010, 20, 1020–1036. [Google Scholar] [CrossRef]
- Paine, M.F.; Ludington, S.S.; Chen, M.L.; Stewart, P.W.; Huang, S.M.; Watkins, P.B. Do men and women differ in proximal small intestinal CYP3A or P-glycoprotein expression? Drug Metab. Dispos. Biol. Fate Chem. 2005, 33, 426–433. [Google Scholar] [CrossRef]
- Cotreau, M.M.; von Moltke, L.L.; Greenblatt, D.J. The influence of age and sex on the clearance of cytochrome P450 3A substrates. Clin. Pharm. 2005, 44, 33–60. [Google Scholar] [CrossRef]
- Herrlinger, C.; Klotz, U. Drug metabolism and drug interactions in the elderly. Best Pract. Res. Clin. Gastroenterol. 2001, 15, 897–918. [Google Scholar] [CrossRef]
- Anderson, B.J.; Holford, N.H. Mechanism-based concepts of size and maturity in pharmacokinetics. Ann. Rev. Pharmacol. Toxicol. 2008, 48, 303–332. [Google Scholar] [CrossRef]
- Sugawara, Y.; Makuuchi, M.; Kaneko, J.; Ohkubo, T.; Imamura, H.; Kawarasaki, H. Correlation between optimal tacrolimus doses and the graft weight in living donor liver transplantation. Clin. Transplant. 2002, 16, 102–106. [Google Scholar] [CrossRef]
- Fukatsu, S.; Yano, I.; Igarashi, T.; Hashida, T.; Takayanagi, K.; Saito, H.; Uemoto, S.; Kiuchi, T.; Tanaka, K.; Inui, K.; et al. Population pharmacokinetics of tacrolimus in adult recipients receiving living-donor liver transplantation. Eur. J. Clin. Pharmacol. 2001, 57, 479–484. [Google Scholar]
- Kuypers, D.R.; de Loor, H.; Naesens, M.; Coopmans, T.; de Jonge, H. Combined effects of CYP3A5*1, POR*28, and CYP3A4*22 single nucleotide polymorphisms on early concentration-controlled tacrolimus exposure in de-novo renal recipients. Pharm. Genom. 2014, 24, 597–606. [Google Scholar] [CrossRef] [PubMed]
- Phupradit, A.; Vadcharavivad, S.; Ingsathit, A.; Kantachuvesiri, S.; Areepium, N.; Sra-Ium, S.; Auamnoy, T.; Sukasem, C.; Sumethkul, V.; Kitiyakara, C. Impact of POR and CYP3A5 Polymorphisms on Trough Concentration to Dose Ratio of Tacrolimus in the Early Post-operative Period Following Kidney Transplantation. Ther. Drug Monit. 2018, 40, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Lesche, D.; Sigurdardottir, V.; Setoud, R.; Oberhansli, M.; Carrel, T.; Fiedler, G.M.; Largiader, C.R.; Mohacsi, P.; Sistonen, J. CYP3A5*3 and POR*28 genetic variants influence the required dose of tacrolimus in heart transplant recipients. Ther. Drug Monit. 2014, 36, 710–715. [Google Scholar] [CrossRef]
- Fu, R.; Tajima, S.; Suetsugu, K.; Watanabe, H.; Egashira, N.; Masuda, S. Biomarkers for individualized dosage adjustments in immunosuppressive therapy using calcineurin inhibitors after organ transplantation. Acta Pharm. Sin. 2019, 40, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Cederbaum, A.I. Molecular mechanisms of the microsomal mixed function oxidases and biological and pathological implications. Redox Biol. 2015, 4, 60–73. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, K. Metabolism of tacrolimus (FK506) and recent topics in clinical pharmacokinetics. Drug Metab. Pharm. 2007, 22, 328–335. [Google Scholar] [CrossRef] [PubMed]
- Gomes, A.M.; Winter, S.; Klein, K.; Turpeinen, M.; Schaeffeler, E.; Schwab, M.; Zanger, U.M. Pharmacogenomics of human liver cytochrome P450 oxidoreductase: Multifactorial analysis and impact on microsomal drug oxidation. Pharmacogenomics 2009, 10, 579–599. [Google Scholar] [CrossRef]
- Agrawal, V.; Choi, J.H.; Giacomini, K.M.; Miller, W.L. Substrate-specific modulation of CYP3A4 activity by genetic variants of cytochrome P450 oxidoreductase. Pharm. Genom. 2010, 20, 611–618. [Google Scholar] [CrossRef]
- Oneda, B.; Crettol, S.; Jaquenoud Sirot, E.; Bochud, M.; Ansermot, N.; Eap, C.B. The P450 oxidoreductase genotype is associated with CYP3A activity in vivo as measured by the midazolam phenotyping test. Pharm. Genom. 2009, 19, 877–883. [Google Scholar] [CrossRef]
- Hesselink, D.A.; Ngyuen, H.; Wabbijn, M.; Gregoor, P.J.; Steyerberg, E.W.; van Riemsdijk, I.C.; Weimar, W.; van Gelder, T. Tacrolimus dose requirement in renal transplant recipients is significantly higher when used in combination with corticosteroids. Br. J. Clin. Pharmacol. 2003, 56, 327–330. [Google Scholar] [CrossRef]
- Fukuda, M.; Suetsugu, K.; Tajima, S.; Katsube, Y.; Watanabe, H.; Harada, N.; Yoshizumi, T.; Egashira, N.; Mori, M.; Masuda, S. Neutrophil Gelatinase-Associated Lipocalin Is Not Associated with Tacrolimus-Induced Acute Kidney Injury in Liver Transplant Patients Who Received Mycophenolate Mofetil with Delayed Introduction of Tacrolimus. Int. J. Mol. Sci. 2019, 20, 3103. [Google Scholar] [CrossRef] [PubMed]
| Recipients (n = 65) | Donors (n = 65) | |
|---|---|---|
| Preoperative data | ||
| Sex (male/female) | 28/37 (43.1/56.9) | 43/22 (66.2/33.8) |
| Age (years) | 59 (51–65) | 39 (33–48) |
| Body weight (kg) | 61.5 (54.0–67.9) | |
| Scr (mg/dL) | 0.68 (0.52–0.90) | |
| BUN (mg/dL) | 14 (10–19) | |
| eGFR (mL/min/1.73 m2) | 78 (58–97) | |
| AST (U/L) | 47 (31–74) | |
| ALT (U/L) | 24 (17–38) | |
| γ-GTP (U/L) | 36 (25–81) | |
| T-Bil (mg/dL) | 2.5 (1.6–5.0) | |
| Alb (g/dL) | 2.7 (2.4–3.0) | |
| Graft data | ||
| GV (g) | 490 (439–556) | |
| GRWR (%) | 0.82 (0.69–0.91) | |
| Primary disease | ||
| Alcoholic liver disease | 16 (24.6) | |
| Primary biliary cholangitis | 13 (20.0) | |
| Hepatitis C | 10 (15.4) | |
| Hepatitis B | 7 (10.8) | |
| Hepatocellular carcinoma | 6 (9.2) | |
| Non-alcoholic steatohepatitis | 5 (7.7) | |
| Autoimmune hepatitis | 2 (3.1) | |
| Wilson’s disease | 1 (1.5) | |
| Others | 5 (7.7) | |
| ABO blood group match | ||
| Identical | 34 (52.3) | |
| Compatible | 11 (16.9) | |
| Incompatible | 20 (30.8) |
| Category | n (%) | Recipient’s CYP3A5 Genotype | Donor’s CYP3A5 Genotype |
|---|---|---|---|
| R*1/D*1 | 21 (32.3) | *1/*1, *1/*3 | *1/*1, *1/*3 |
| R*1/D*3 | 6 (9.2) | *1/*1, *1/*3 | *3/*3 |
| R*3/D*1 | 9 (13.8) | *3/*3 | *1/*1, *1/*3 |
| R*3/D*3 | 29 (44.6) | *3/*3 | *3/*3 |
| A) Categorization of the recipients by CYP3A5 and POR genotypes | |||
|---|---|---|---|
| Category | n (%) | Recipient’s CYP3A5 Genotype | Recipient’s POR Genotype |
| F/*1 | 8 (12.3) | *1/*1, *1/*3 | *1/*1 |
| F/*28 | 19 (29.2) | *1/*1, *1/*3 | *1/*28, *28/*28 |
| D/*1 | 13 (20.0) | *3/*3 | *1/*1 |
| D/*28 | 25 (38.5) | *3/*3 | *1/*28, *28/*28 |
| B)Categorization of the donors by CYP3A5 and POR genotypes | |||
| Category | n (%) | Donor’s CYP3A5 Genotype | Donor’s POR Genotype |
| F/*1 | 9 (13.8) | *1/*1, *1/*3 | *1/*1 |
| F/*28 | 21 (32.3) | *1/*1, *1/*3 | *1/*28, *28/*28 |
| D/*1 | 10 (15.4) | *3/*3 | *1/*1 |
| D/*28 | 25 (38.5) | *3/*3 | *1/*28, *28/*28 |
| All Patients (65) | Pod 1–7 | Pod 8–14 | Pod 15–21 | Pod 22–28 | ||||
|---|---|---|---|---|---|---|---|---|
| β | p | β | p | Β | p | p | ||
| Recipient sex (male (28) vs. female (37)) | −0.184 | 0.002 | − | − | − | − | − | − |
| Recipient age (years) | 0.156 | 0.002 | 0.095 | 0.018 | 0.100 | 0.043 | − | |
| Recipient BW (kg) | −0.262 | <0.001 | −0.185 | <0.001 | −0.138 | 0.008 | − | − |
| Donor sex (male (43) vs. female (22)) | − | − | − | − | − | − | − | − |
| Donor age (years) | − | − | − | − | − | − | − | − |
| Graft volume (g) | −0.157 | 0.003 | −0.520 | <0.001 | −0.383 | <0.001 | −0.274 | <0.001 |
| Recipient CYP3A5 (f (27) vs. d (38)) | −0.389 | <0.001 | −0.345 | <0.001 | −0.417 | <0.001 | −0.627 | <0.001 |
| Donor CYP3A5 (f (30) vs. d (35)) | − | − | − | − | −0.175 | 0.004 | − | − |
| Recipient POR (*1 (21) vs. *28 (44)) | − | − | − | − | − | − | − | − |
| Donor POR (*1 (19) vs. *28 (46)) | − | − | − | − | − | − | − | − |
| Recipient/ Functional CYP3A5 (27) | Pod 1–7 | Pod 8–14 | Pod 15–21 | Pod 22–28 | ||||
|---|---|---|---|---|---|---|---|---|
| β | p | β | p | Β | p | β | p | |
| Recipient sex (male (11) vs. female (16)) | −0.304 | 0.001 | −0.340 | <0.001 | − | − | −0.440 | 0.001 |
| Recipient age (years) | 0.184 | 0.027 | − | − | 0.641 | <0.001 | 0.941 | <0.001 |
| Recipient BW (kg) | −0.262 | <0.001 | − | − | −0.352 | <0.001 | −0.360 | 0.008 |
| Donor sex (male (19) vs. female (8)) | − | − | − | − | − | − | 0.168 | 0.144 |
| Donor age (years) | − | − | − | − | 0.545 | <0.001 | 1.162 | <0.001 |
| Graft volume (g) | −0.176 | 0.022 | −0.545 | <0.001 | −0.737 | <0.001 | −0.872 | <0.001 |
| Donor CYP3A5 (f (21) vs. d (6)) | − | − | − | − | −0.394 | <0.001 | −0.579 | <0.001 |
| Recipient POR (*1 (8) vs. *28 (19)) | − | − | − | − | 0.390 | <0.001 | − | − |
| Donor POR (*1 (9) vs. *28 (18)) | − | − | − | − | − | − | − | − |
| Donor/ Functional CYP3A5 (30) | Pod 1–7 | Pod 8–14 | Pod 15–21 | Pod 22–28 | ||||
|---|---|---|---|---|---|---|---|---|
| β | p | β | p | β | p | β | p | |
| Recipient sex (male (13) vs. female (17)) | − | − | − | − | − | − | − | − |
| Recipient age (years) | − | − | − | − | 0.312 | <0.001 | 0.187 | 0.074 |
| Recipient BW (kg) | −0.283 | <0.001 | − | − | − | − | − | − |
| Donor sex (male (21) vs. female (9)) | − | − | − | − | − | − | − | − |
| Donor age (years) | 0.310 | <0.001 | − | − | ||||
| Graft volume (g) | −0.178 | 0.032 | −0.617 | <0.001 | −0.730 | <0.001 | −0.301 | 0.006 |
| Recipient CYP3A5 (f (21) vs. d (9)) | − | − | − | − | −0.436 | <0.001 | −0.688 | <0.001 |
| Recipient POR (*1 (11) vs. *28 (19)) | − | − | − | − | − | − | − | − |
| Donor POR (*1 (9) vs. *28 (21)) | − | − | − | − | − | − | − | − |
| Recipient/ Defective CYP3A5 (38) | Pod 1–7 | Pod 8–14 | Pod 15–21 | Pod 22–28 | ||||
|---|---|---|---|---|---|---|---|---|
| β | p | β | p | β | p | β | p | |
| Recipient sex (male (17) vs. female (21)) | −0.198 | 0.009 | −0.205 | <0.001 | − | − | − | − |
| Recipient age (years) | − | − | 0.214 | <0.001 | − | − | − | − |
| Recipient BW (kg) | − | − | −0.332 | <0.001 | −0.221 | 0.004 | −0.288 | 0.011 |
| Donor sex (male (24) vs. female (14)) | − | − | − | − | − | − | − | − |
| Donor age (years) | − | − | − | − | − | − | −0.258 | 0.022 |
| Graft volume (g) | −0.182 | 0.024 | −0.434 | <0.001 | −0.443 | <0.001 | − | − |
| Donor CYP3A5 (f (9) vs. d (29)) | −0.256 | <0.001 | − | − | − | − | − | − |
| Recipient POR (*1 (13) vs. *28 (25)) | − | − | −0.168 | 0.002 | − | − | − | − |
| Donor POR (*1 (10) vs. *28 (28)) | − | − | − | − | − | − | − | − |
| Donor/ Defective CYP3A5 (35) | Pod 1–7 | Pod 8–14 | Pod 15–21 | Pod 22–28 | ||||
|---|---|---|---|---|---|---|---|---|
| β | p | β | p | β | p | β | p | |
| Recipient sex (male (15) vs. female (20)) | −0.322 | <0.001 | − | − | − | − | − | − |
| Recipient age (years) | − | − | 0.305 | <0.001 | 0.138 | <0.001 | − | − |
| Recipient BW (kg) | − | − | −0.664 | <0.001 | −0.564 | <0.001 | −0.495 | <0.001 |
| Donor sex (male (22) vs. female (13)) | − | − | 0.265 | <0.001 | − | − | − | − |
| Donor age (years) | − | − | − | − | − | − | − | − |
| Graft volume (g) | −0.133 | 0.049 | − | − | − | − | − | − |
| Recipient CYP3A5 (f (6) vs. d (29)) | −0.413 | <0.001 | − | − | −0.289 | <0.001 | −0.309 | 0.004 |
| Recipient POR (*1 (10) vs. *28 (25)) | − | − | −0.050 | 0.352 | −0.098 | 0.152 | −0.155 | 0.133 |
| Donor POR (*1 (10) vs. *28 (25)) | − | − | − | − | − | − | − | − |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakamura, T.; Fukuda, M.; Matsukane, R.; Suetsugu, K.; Harada, N.; Yoshizumi, T.; Egashira, N.; Mori, M.; Masuda, S. Influence of POR*28 Polymorphisms on CYP3A5*3-Associated Variations in Tacrolimus Blood Levels at an Early Stage after Liver Transplantation. Int. J. Mol. Sci. 2020, 21, 2287. https://doi.org/10.3390/ijms21072287
Nakamura T, Fukuda M, Matsukane R, Suetsugu K, Harada N, Yoshizumi T, Egashira N, Mori M, Masuda S. Influence of POR*28 Polymorphisms on CYP3A5*3-Associated Variations in Tacrolimus Blood Levels at an Early Stage after Liver Transplantation. International Journal of Molecular Sciences. 2020; 21(7):2287. https://doi.org/10.3390/ijms21072287
Chicago/Turabian StyleNakamura, Takahiro, Mio Fukuda, Ryosuke Matsukane, Kimitaka Suetsugu, Noboru Harada, Tomoharu Yoshizumi, Nobuaki Egashira, Masaki Mori, and Satohiro Masuda. 2020. "Influence of POR*28 Polymorphisms on CYP3A5*3-Associated Variations in Tacrolimus Blood Levels at an Early Stage after Liver Transplantation" International Journal of Molecular Sciences 21, no. 7: 2287. https://doi.org/10.3390/ijms21072287
APA StyleNakamura, T., Fukuda, M., Matsukane, R., Suetsugu, K., Harada, N., Yoshizumi, T., Egashira, N., Mori, M., & Masuda, S. (2020). Influence of POR*28 Polymorphisms on CYP3A5*3-Associated Variations in Tacrolimus Blood Levels at an Early Stage after Liver Transplantation. International Journal of Molecular Sciences, 21(7), 2287. https://doi.org/10.3390/ijms21072287