An Updated Overview on Nanonutraceuticals: Focus on Nanoprebiotics and Nanoprobiotics
Abstract
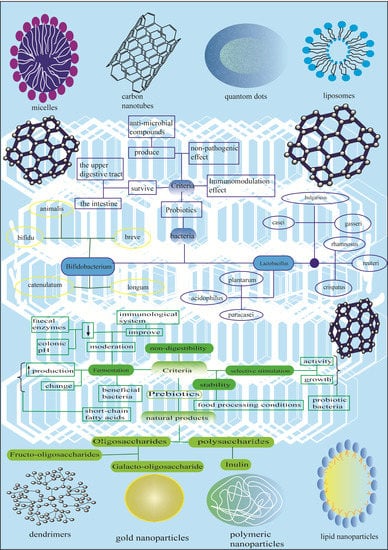
1. Nanonutraceuticals
1.1. Nutraceuticals
1.2. From Nanopharmaceuticals to Nanonutraceuticals
1.2.1. Characteristics of Nanoparticles and General Classification
1.2.2. Emerging Area of Applications
2. Focus on Nanotechnologies Applied to Prebiotics, Probiotics, and Synbiotics
2.1. An Overview on Prebiotics, Probiotics, and Synbiotics
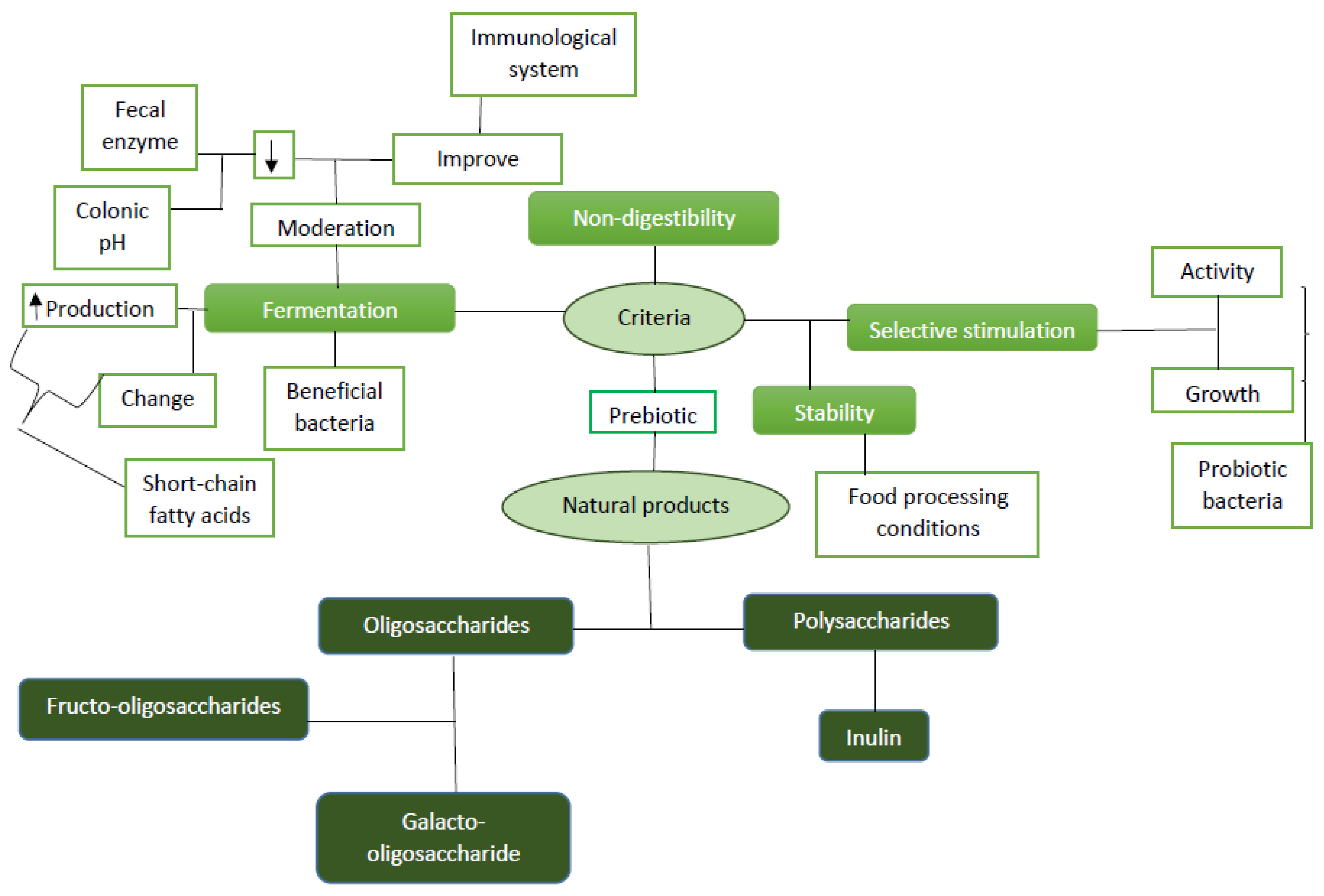
2.1.1. Prebiotics
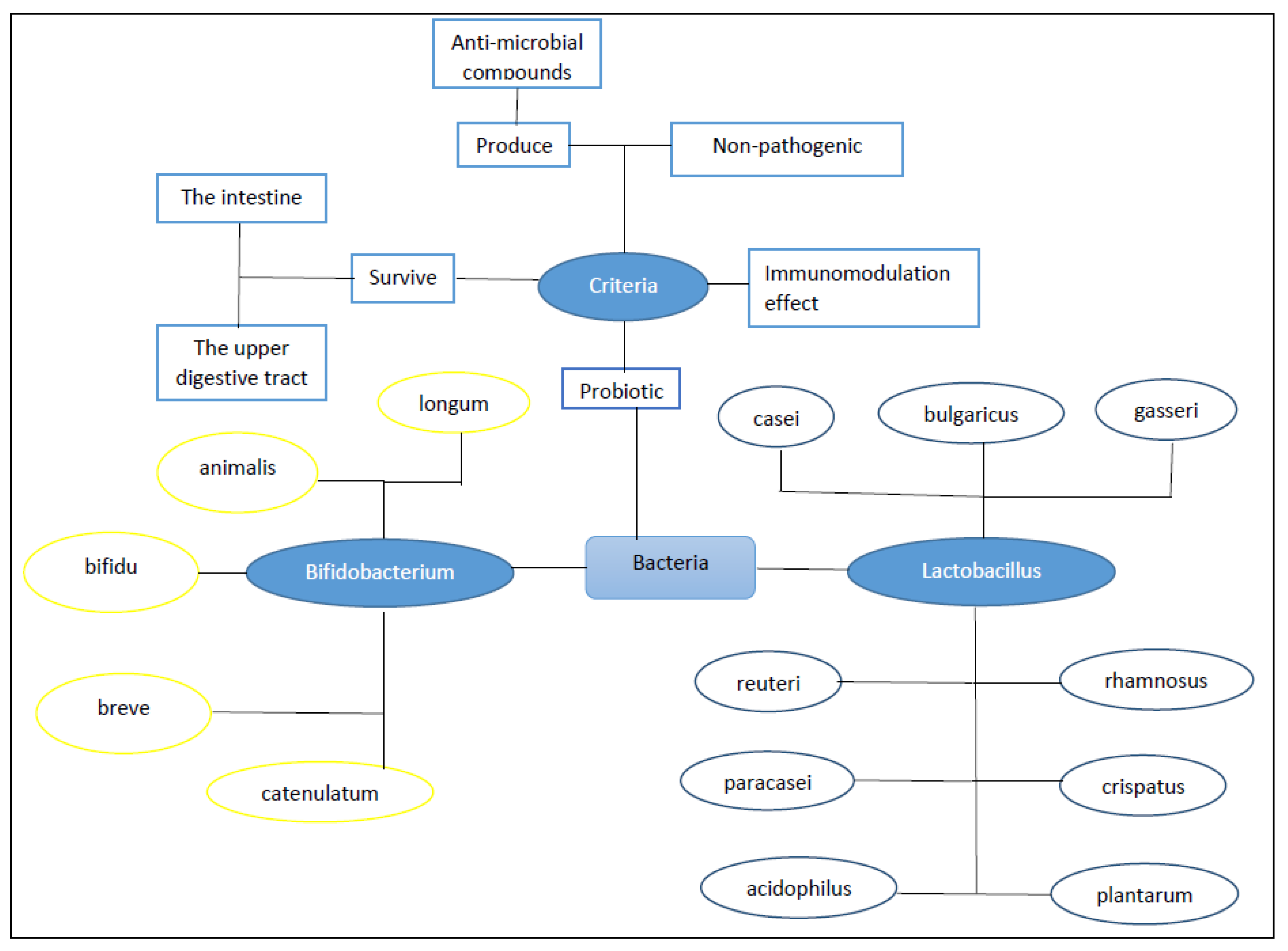
2.1.2. Probiotics
2.1.3. Synbiotics
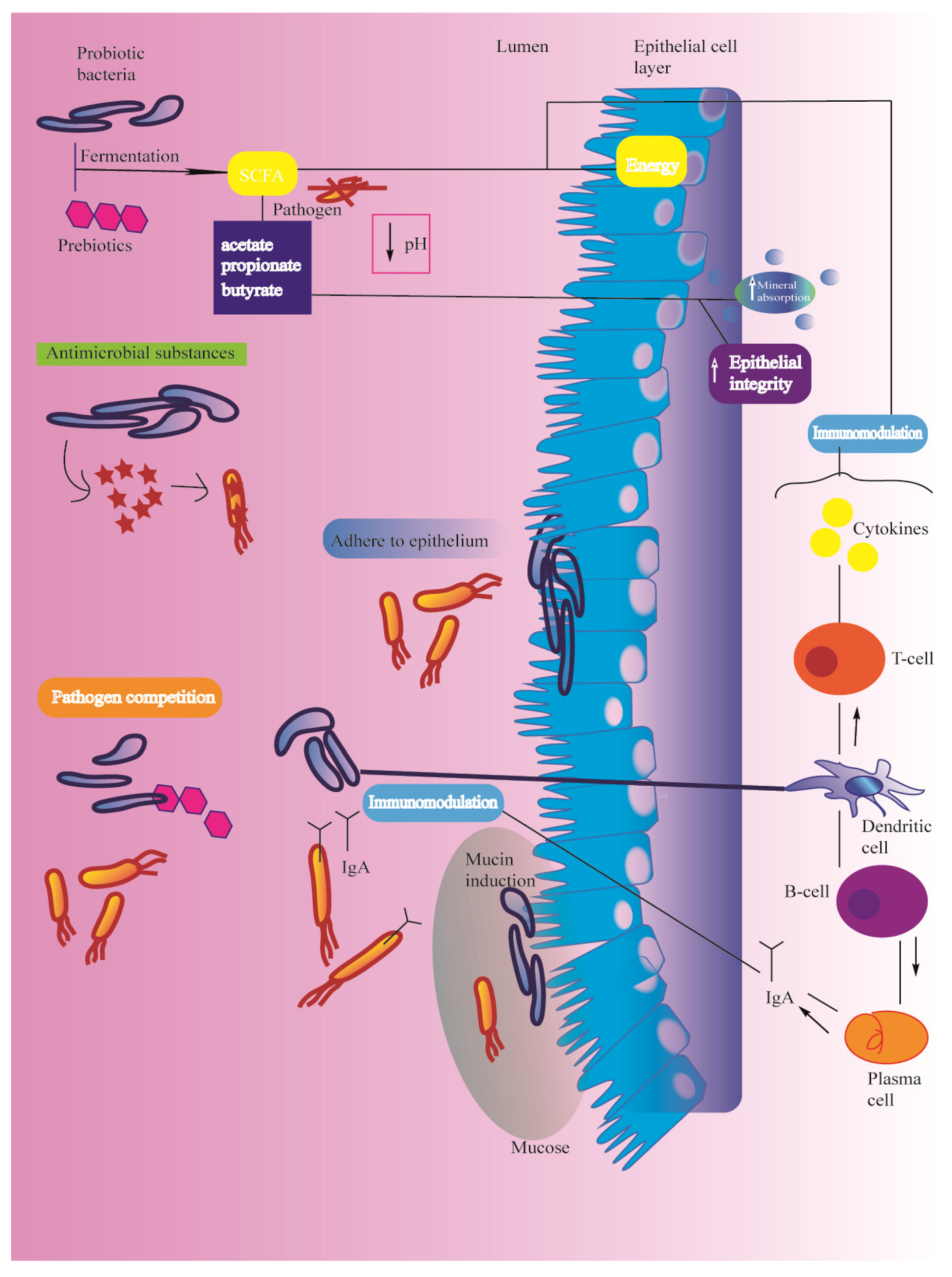
2.1.4. Health Promoting Effect of Prebiotics, Probiotics, and Synbiotics
2.2. Nano-Prebiotics, Nano-Probiotics, and Nano-Synbiotics
3. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Santini, A.; Novellino, E. Nutraceuticals: Beyond the diet before the drugs. Curr. Bioact. Comp. 2014, 10, 1–12. [Google Scholar] [CrossRef]
- Santini, A.; Novellino, E. To Nutraceuticals and back: Rethinking a concept. Foods 2017, 6, 74. [Google Scholar] [CrossRef] [PubMed]
- Abenavoli, L.; Izzo, A.A.; Milić, N.; Cicala, C.; Santini, A.; Capasso, R. Milk thistle (Silybum marianum): A concise overview on its chemistry, pharmacological, and nutraceutical uses in liver diseases. Phytother. Res. 2018, 32, 2202–2213. [Google Scholar] [CrossRef] [PubMed]
- Durazzo, A. Extractable and Non-extractable polyphenols: An overview. In Non-Extractable Polyphenols and Carotenoids: Importance in Human Nutrition and Health; Saura-Calixto, F., Pérez-Jiménez, J., Eds.; Royal Society of Chemistry: London, UK, 2018; pp. 1–37. [Google Scholar]
- Santini, A.; Novellino, E. Nutraceuticals-shedding light on the grey area between pharmaceuticals and food. Expert Rev. Clin. Pharmacol. 2018, 11, 545–547. [Google Scholar] [CrossRef] [PubMed]
- Durazzo, A.; Lucarini, M. A current shot and re-thinking of antioxidant research strategy. Braz. J. Anal. Chem. 2018, 5, 9–11. [Google Scholar] [CrossRef]
- Santini, A.; Cammarata, S.M.; Capone, G.; Ianaro, A.; Tenore, G.C.; Pani, L.; Novellino, E. Nutraceuticals: Opening the debate for a regulatory framework. Br. J. Clin. Pharmacol. 2018, 84, 659–672. [Google Scholar] [CrossRef]
- Daliu, P.; Santini, A.; Novellino, E. A decade of nutraceutical patents: Where are we now in 2018? Expert Opin. Ther. Pat. 2018, 28, 875–882. [Google Scholar] [CrossRef]
- Durazzo, A.; D’Addezio, L.; Camilli, E.; Piccinelli, R.; Turrini, A.; Marletta, L.; Marconi, S.; Lucarini, M.; Lisciani, S.; Gabrielli, P.; et al. From plant compounds to botanicals and back: A current snapshot. Molecules 2018, 23, 1844. [Google Scholar] [CrossRef]
- Santini, A.; Tenore, G.C.; Novellino, E. Nutraceuticals: A paradigm of proactive medicine. Eur. J. Pharm. Sci. 2017, 96, 53–61. [Google Scholar] [CrossRef]
- De Jong, W.H.; Borm, P.J.A. Drug delivery and nanoparticles: Applications and hazards. Int. J. Nanomed. 2008, 3, 133–149. [Google Scholar] [CrossRef]
- Jeevanandam, J.; Barhoum, A.; Chan, Y.S.; Dufresne, A.; Danquah, M.K. Review on nanoparticles and nanostructured materials: History, sources, toxicity and regulations. Beilstein. J. Nanotechnol. 2018, 9, 1050–1074. [Google Scholar] [CrossRef] [PubMed]
- Auffan, M.; Rose, J.; Bottero, J.Y.; Lowry, G.V.; Jolivet, J.P.; Wiesner, M.R. Towards a definition of inorganic nanoparticles from an environmental, health and safety perspective. Nat. Nanotechnol. 2009, 4, 634–641. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, Q.; Scotter, M.; Blackburn, J.; Ross, B.; Boxall, A.; Castle, L.; Aitken, R.; Watkins, R. Applications and implications of nanotechnologies for the food sector. Food Addit. Contam. Part A Chem. Anal. Control Expo. Risk Assess. 2008, 25, 241–258. [Google Scholar] [CrossRef] [PubMed]
- Ljubimova, J.Y.; Holler, E. Biocompatible nanopolymers: The next generation of breast cancer treatment? Nanomedicine 2012, 7, 1467–1470. [Google Scholar] [CrossRef]
- Peters, R.J.B.; Bouwmeester, H.; Gottardo, S.; Amenta, V.; Arena, M.; Brandho, P.; Marvin, H.J.P.; Mech, A.; Moniz, F.B.; Pesudo, L.Q.; et al. Nanomaterials for products and application in agriculture, feed and food. Trends Food Sci. Technol. 2016, 54, 155–164. [Google Scholar] [CrossRef]
- Dudefoi, W.; Villares, A.; Peyron, S.; Moreau, C.; Ropers, M.-H.; Gontard, N.; Cathala, B. Nanoscience and nanotechnologies for biobased materials, packaging and food applications: New opportunities and concerns. Innov. Food Sci. Emerg. Technol. 2018, 46, 107–121. [Google Scholar] [CrossRef]
- He, X.; Deng, H.; Hwang, H.-M. The current application of nanotechnology in food and agriculture. J. Food Drug Anal. 2019, 27, 1–21. [Google Scholar] [CrossRef]
- Das, G.; Patra, J.K.; Paramithiotis, S.; Shin, H.S. The sustainability challenge of food and environmental nanotechnology: Current status and imminent perceptions. Int. J. Environ. Res. Public Health 2019, 16, 4848. [Google Scholar] [CrossRef]
- Farokhzad, O.C.; Langer, R. Nanomedicine: Developing smarter therapeutic and diagnostic modalities. Adv. Drug Deliv. Rev. 2006, 58, 1456–1459. [Google Scholar] [CrossRef]
- Davis, M.E.; Chen, Z.G.; Shin, D.M. Nanoparticle therapeutics: An emerging treatment modality for cancer. Nat. Rev. Drug Discov. 2008, 7, 771–782. [Google Scholar] [CrossRef]
- Norouzi, M.; Amerian, M.; Amerian, M.; Atyabi, F. Clinical applications of nanomedicine in cancer therapy. Drug Discov. Today 2019. [Google Scholar] [CrossRef] [PubMed]
- Teleanu, D.M.; Chircov, C.; Grumezescu, A.M.; Teleanu, R.I. Neuronanomedicine: An Up-to-Date Overview. Pharmaceutics 2019, 11, 101. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-López, E.; Guerra, M.; Dias-Ferreira, J.; Lopez-Machado, A.; Ettcheto, M.; Cano, A.; Espina, M.; Camins, A.; Garcia, M.L.; Souto, E.B. Current Applications of Nanoemulsions in Cancer Therapeutics. Nanomaterials 2019, 9, 821. [Google Scholar] [CrossRef] [PubMed]
- Andreani, T.; Severino, P.; de Hollanda, L.M.; Vazzana, M.; Souto, S.B.; Santini, A.; Silva, A.M.; Souto, E.B. Cancer therapies: Applications, nanomedicines and nanotoxicology. In Nanostructures for Cancer Therapy; Ficai, A., Grumezescu, A.M., Eds.; Elsevier: Amsterdam, The Netherlands, 2017; Chapter 9; pp. 241–260. [Google Scholar] [CrossRef]
- Do Ceu Texeira, M.; Santini, A.; Souto, E.B. Nanocancer therapies: Drug delivery formulation and nanotoxicology. In Nanostructures for Antimicrobial Therapy—Micro and Nano Technologies; Multi-Volume SET I-V: Nanostructures in Therapeutic Medicine Series; Elsevier: Amsterdam, The Netherlands, 2017; Chapter 8; pp. 203–222. [Google Scholar] [CrossRef]
- Petros, R.A.; DeSimone, J.M. Strategies in the design of nanoparticles for therapeutic applications. Nat. Rev. Drug Discov. 2010, 9, 615–627. [Google Scholar] [CrossRef] [PubMed]
- Doktorovova, S.; Kovacevic, A.B.; Garcia, M.L.; Souto, E.B. Preclinical safety of solid lipid nanoparticles and nanostructured lipid carriers: Current evidence from in vitro and in vivo evaluation. Eur. J. Pharm. Biopharm. 2016, 108, 235–252. [Google Scholar] [CrossRef] [PubMed]
- Souto, E.B.; Muller, R.H. Lipid nanoparticles: Effect on bioavailability and pharmacokinetic changes. In Drug Delivery; Springer: Berlin/Heidelberg, Germany, 2010. [Google Scholar] [CrossRef]
- Martins, S.; Silva, A.C.; Ferreira, D.C.; Souto, E.B. Improving oral absorption of Salmon calcitonin by trimyristin lipid nanoparticles. J. Biomed. Nanotechnol. 2009, 5, 76–83. [Google Scholar] [CrossRef]
- Muller, R.H.; Runge, S.; Ravelli, V.; Mehnert, W.; Thunemann, A.F.; Souto, E.B. Oral bioavailability of cyclosporine: Solid lipid nanoparticles (SLN) versus drug nanocrystals. Int. J. Pharm. 2006, 317, 82–89. [Google Scholar] [CrossRef]
- Severino, P.; Pinho, S.C.; Souto, E.B.; Santana, M.H. Polymorphism, crystallinity and hydrophilic-lipophilic balance of stearic acid and stearic acid-capric/caprylic triglyceride matrices for production of stable nanoparticles. Colloids Surf. B Biointerfaces 2011, 86, 125–130. [Google Scholar] [CrossRef]
- Andreani, T.; Fangueiro, J.F.; Severino, P.; Souza, A.L.R.; Martins-Gomes, C.; Fernandes, P.M.V.; Calpena, A.C.; Gremiao, M.P.; Souto, E.B.; Silva, A.M. The Influence of Polysaccharide Coating on the Physicochemical Parameters and Cytotoxicity of Silica Nanoparticles for Hydrophilic Biomolecules Delivery. Nanomaterials 2019, 9, 1081. [Google Scholar] [CrossRef]
- Ferreira da Silva, C.; Severino, P.; Martins, F.; Santana, M.H.; Souto, E.B. Didanosine-loaded chitosan microspheres optimized by surface-response methodology: A modified “Maximum Likelihood Classification” approach formulation for reverse transcriptase inhibitors. Biomed. Pharmacother. 2015, 70, 46–52. [Google Scholar] [CrossRef]
- Severino, P.; Da Silva, C.F.; Dalla Costa, T.C.; Silva, H.; Chaud, M.V.; Santana, M.H.; Souto, E.B. In vivo absorption of didanosine formulated in pellets composed of chitosan microspheres. In Vivo 2014, 28, 1045–1050. [Google Scholar] [PubMed]
- Severino, P.; de Oliveira, G.G.G.; Ferraz, H.G.; Souto, E.B.; Santana, M.H.A. Preparation of gastro-resistant pellets containing chitosan microspheres for improvement of oral didanosine bioavailability. J. Pharm. Anal. 2012, 2, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Severino, P.; Souto, E.B.; Pinho, S.C.; Santana, M.H. Hydrophilic coating of mitotane-loaded lipid nanoparticles: Preliminary studies for mucosal adhesion. Pharm. Dev. Technol. 2013, 18, 577–581. [Google Scholar] [CrossRef] [PubMed]
- Severino, P.; Chaud, M.V.; Shimojo, A.; Antonini, D.; Lancelloti, M.; Santana, M.H.; Souto, E.B. Sodium alginate-cross-linked polymyxin B sulphate-loaded solid lipid nanoparticles: Antibiotic resistance tests and HaCat and NIH/3T3 cell viability studies. Colloids Surf. B Biointerfaces 2015, 129, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Severino, P.; da Silva, C.F.; Andrade, L.N.; de Lima Oliveira, D.; Campos, J.; Souto, E.B. Alginate Nanoparticles for Drug Delivery and Targeting. Curr. Pharm. Des. 2019, 25, 1312–1334. [Google Scholar] [CrossRef]
- Sarei, F.; Mohammadpour Dounighi, N.; Zolfagharian, H.; Khaki, P.; Moradi Bidhendi, S. Alginate Nanoparticles as a Promising Adjuvant and Vaccine Delivery System. Indian J. Pharm. Sci. 2013, 75, 442–449. [Google Scholar] [CrossRef]
- Havel, H.A. Where are the nanodrugs? An industry perspective on development of drug products containing nanomaterials. AAPS J. 2016, 18, 1351–1353. [Google Scholar] [CrossRef]
- Feng, J.; Markwalter, C.E.; Tian, C.; Armstrong, M.; Prud’homme, R.K. Translational formulation of nanoparticle therapeutics from laboratory discovery to clinical scale. J. Transl. Med. 2019, 17, 200. [Google Scholar] [CrossRef]
- Öztürk-Atar, K.; Eroğlu, H.; Gürsoy, R.N.; Çaliş, S. Current advances in nanopharmaceuticals. J. Nanosci. Nanotechnol. 2019, 19, 3686–3705. [Google Scholar] [CrossRef]
- Souto, E.B.; Silva, G.F.; Dias-Ferreira, J.; Zielinska, A.; Ventura, F.; Durazzo, A.; Lucarini, M.; Novellino, E.; Santini, A. Nanopharmaceutics: Part I-Clinical Trials Legislation and Good Manufacturing Practices (GMP) of Nanotherapeutics in the EU. Pharmaceutics 2020, 12, 146. [Google Scholar] [CrossRef]
- Agarwal, V.; Bajpai, M.; Sharma, A. Patented and Approval Scenario of Nanopharmaceuticals with Relevancy to Biomedical Application, Manufacturing Procedure and Safety Aspects. Recent. Pat. Drug Deliv. Formul. 2018, 12, 40–52. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.P.; Wang, D.; Li, Z. Grand challenges in nanomedicine. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 106, 110302. [Google Scholar] [CrossRef] [PubMed]
- Daliu, P.; Santini, A.; Novellino, E. From pharmaceuticals to nutraceuticals: Bridging disease prevention and management. Expert Rev. Clin. Pharmacol. 2019, 12, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Durazzo, A.; Lucarini, M.; Souto, E.B.; Cicala, C.; Caiazzo, E.; Izzo, A.A.; Novellino, E.; Santini, A. Polyphenols: A concise overview on the chemistry, occurrence and human health. Phyt. Res. 2019, 33, 2221–2243. [Google Scholar] [CrossRef] [PubMed]
- Durazzo, A.; Lucarini, M. Extractable and Non-extractable antioxidants. Molecules 2019, 24, 1933. [Google Scholar] [CrossRef] [PubMed]
- Durazzo, A.; Lucarini, M. Editorial: The State of Science and Innovation of Bioactive Research and Applications, Health, and Diseases. Front. Nutr. 2019, 6, 178. [Google Scholar] [CrossRef]
- Watkins, R.; Wu, L.; Zhang, C.; Davis, R.M.; Xu, B. Natural product-based nanomedicine: Recent advances and issues. Int. J. Nanomed. 2015, 10, 6055–6074. [Google Scholar]
- Pimentel-Moral, S.; Teixeira, M.C.; Fernandes, A.R.; Arráez-Román, D.; Martínez-Férez, A.; Segura-Carretero, A.; Souto, E.B. Lipid nanocarriers for the loading of polyphenols—A comprehensive review. Adv. Colloid Interface Sci. 2018, 260, 85–94. [Google Scholar] [CrossRef]
- Singh, B. Nanonutraceuticals, 1st ed.; CRC Press: Boca Raton, FL, USA, 2018; 326p. [Google Scholar]
- Menditto, E.; Guerriero, F.; Orlando, V.; Crola, C.; Di Somma, C.; Illario, M.; Morisky, D.; Colao, A. Self-Assessment of Adherence to Medication: A Case Study in Campania Region Community-Dwelling Population. J Aging Res. 2015, 2015, 682503. [Google Scholar] [CrossRef]
- Putignano, D.; Bruzzese, D.; Orlando, V.; Fiorentino, D.; Tettamanti, A.; Menditto, E. Differences in drug use between men and women: An Italian cross sectional study. BMC Women’s Health 2017, 17, 73. [Google Scholar] [CrossRef]
- Menditto, E.; Cahir, C.; Aza-Pascual-Salcedo, M.; Bruzzese, D.; Poblador-Plou, B.; Malo, S.; Costa, E.; González-Rubio, F.; Gimeno-Miguel, A.; Orlando, V.; et al. Adherence to chronic medication in older populations: Application of a common protocol among three European cohorts. Patient Prefer. Adherence 2018, 12, 1975–1987. [Google Scholar] [CrossRef] [PubMed]
- Iolascon, G.; Gimigliano, F.; Moretti, A.; Riccio, I.; Di Gennaro, M.; Illario, M.; Monetti, V.M.; Orlando, V.; Menditto, E. Rates and reasons for lack of persistence with anti-osteoporotic drugs: Analysis of the Campania region database. Clin. Cases Miner. Bone Metab. 2016, 13, 126–129. [Google Scholar] [CrossRef] [PubMed]
- Scala, D.; Menditto, E.; Armellino, M.F.; Manguso, F.; Monetti, V.M.; Orlando, V.; Antonino, A.; Makoul, G.; De Palma, M. Italian translation and cultural adaptation of the communication assessment tool in an outpatient surgical clinic. BMC Health Serv. Res. 2016, 16, 163. [Google Scholar] [CrossRef] [PubMed]
- Wiwanitkit, V. Delivery of nutraceuticals using nanotechnology. Int. J. Pharm. Investig. 2012, 2, 218. [Google Scholar] [CrossRef] [PubMed]
- Bernela, M.; Kaur, P.; Ahuja, M.; Thakur, R. Nano-based Delivery System for Nutraceuticals: The Potential Future. In Advances in Animal Biotechnology and Its Applications; Gahlawat, S., Duhan, J., Salar, R., Siwach, P., Kumar, S., Kaur, P., Eds.; Springer: Singapore, 2018. [Google Scholar]
- Aditya, N.P.; Espinosa, Y.G.; Norton, I.T. Encapsulation systems for the delivery of hydrophilic nutraceuticals: Food application. Biotechnol. Adv. 2017, 35, 450–457. [Google Scholar] [CrossRef]
- Thammarutwasik, P.; Hongpattarakere, T.; Chantachum, S.; Kijroongrojana, K.; Itharat, A.; Reanmongkol, W.; Tewtrakul, S.; Ooraikul, B. Prebiotics—A Review. Songklanakarin J. Sci. Technol. 2009, 31, 401–408. [Google Scholar]
- Patel, S.; Goyal, A. The current trends and future perspectives of prebiotics research: A review. Biotech 2012, 2, 115–125. [Google Scholar] [CrossRef]
- Al-Sheraji, S.H.; Ismail, A.; Manap, M.Y.; Mustafa, S.; Yusof, R.M.; Hassan, F.A. Prebiotics as functional foods: A review. J. Funct. Foods 2013, 5, 1542–1553. [Google Scholar] [CrossRef]
- Bindels, L.B.; Delzenne, N.M.; Cani, P.D.; Walter, J. Towards a more comprehensive concept for prebiotics. Nat. Rev. Gastroenterol. Hepatol. 2015, 12, 303–310. [Google Scholar] [CrossRef]
- Hutkins, R.W.; Krumbeck, J.A.; Bindels, L.B.; Cani, P.D.; Fahey, G., Jr.; Goh, Y.J.; Hamaker, B.; Martens, E.C.; Mills, D.A.; Rastal, R.A.; et al. Prebiotics: Why definitions matter. Curr. Opin. Biotechnol. 2016, 37, 1–7. [Google Scholar] [CrossRef]
- Monteagudo-Mera, A.; Rastall, R.A.; Gibson, G.R.; Charalampopoulos, D.; Chatzifragkou, A. Adhesion mechanisms mediated by probiotics and prebiotics and their potential impact on human health. Appl. Microbiol. Biotechnol. 2019, 103, 6463–6472. [Google Scholar] [CrossRef] [PubMed]
- Pandey, K.R.; Naik, S.R.; Vakil, B.V. Probiotics, prebiotics and synbiotics—A review. J. Food Sci. Technol. 2015, 52, 7577–7587. [Google Scholar] [CrossRef] [PubMed]
- Khangwal, I.; Shukla, P. Potential prebiotics and their transmission mechanisms: Recent approaches. J. Food Drug Anal. 2019, 27, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Davani-Davari, D.; Negahdaripour, M.; Karimzadeh, I.; Seifan, M.; Mohkam, M.; Masoumi, J.S.; Berenjian, A.; Ghasemi, Y. Prebiotics: Definition, Types, Sources, Mechanisms, and Clinical Applications. Foods 2019, 8, 92. [Google Scholar] [CrossRef]
- FAO. Guidelines for the Evaluation of Probiotics in Food; Report of a Joint FAO/WHO Working Group on Drafting Guidelines for the Evaluation of Probiotics in Food; FAO: London, ON, Canada, 2002. [Google Scholar]
- Food and Agriculture Organization. FAO Technical Meeting on Prebiotics: Food Quality and Standards Service (AGNS); FAO Technical Meeting Report; FAO: Rome, Italy, 2007. [Google Scholar]
- Chung, W.S.F.; Walker, A.W.; Louis, P.; Parkhill, J.; Vermeiren, J.; Bosscher, D.; Duncan, S.H.; Flint, H.J. Modulation of the human gut microbiota by dietary fibres occurs at the species level. BMC Biol. 2016, 14, 3. [Google Scholar] [CrossRef] [PubMed]
- Scavuzzi, B.M.; Henrique, F.C.; Miglioranza, L.H.S.; Simão, A.N.C.; Dichi, I. Impact of prebiotics, probiotics and synbiotics on components of the metabolic syndrome. Ann. Nutr. Disord. Ther. 2014, 1, 1009. [Google Scholar]
- Ustundag, G.H.; Altuntas, H.; Soysal, Y.D.; Kokturk, F. The effects of synbiotic Bifidobacterium lactis B94 plus Inulin addition on standard triple therapy of Helicobacter pylori eradication in children. Can. J. Gastroenterol. Hepatol. 2017, 2017, 8130596. [Google Scholar] [CrossRef]
- Roškar, I.; Švigelj, K.; Štempelj, M.; Volfand, J.; Štabuc, B.; Malovrh, Š.; Rogelj, I. Effects of a probiotic product containing Bifidobacterium animalis subsp. animalis IM386 and Lactobacillus plantarum MP2026 in lactose intolerant individuals: Randomized, placebo-controlled clinical trial. J. Funct. Foods 2017, 35, 1–8. [Google Scholar] [CrossRef]
- Brahe, L.K.; Le Chatelier, E.; Prifti, E.; Pons, N.; Kennedy, S.; Blædel, T.; Håkansson, J.; Dalsgaard, T.K.; Hansen, T.; Pedersen, O. Dietary modulation of the gut microbiota—A randomised controlled trial in obese postmenopausal women. Br. J. Nutr. 2015, 114, 406–417. [Google Scholar] [CrossRef]
- Ivey, K.L.; Hodgson, J.M.; Kerr, D.A.; Thompson, P.L.; Stojceski, B.; Prince, R.L. The effect of yoghurt and its probiotics on blood pressure and serum lipid profile; a randomised controlled trial. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Hariri, M.; Salehi, R.; Feizi, A.; Mirlohi, M.; Ghiasvand, R.; Habibi, N. A randomized, double-blind, placebo-controlled, clinical trial on probiotic soy milk and soy milk: Effects on epigenetics and oxidative stress in patients with type II diabetes. Genes Nutr. 2015, 10, 52. [Google Scholar] [CrossRef] [PubMed]
- Tonucci, L.B.; Olbrich Dos Santos, K.M.; Licursi de Oliveira, L.; Rocha Ribeiro, S.M.; Duarte Martino, H.S. Clinical application of probiotics in type 2 diabetes mellitus: Arandomized, double-blind, placebo-controlled study. Clin. Nutr. 2015, 36, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Mohamadshahi, M.; Veissi, M.; Haidari, F.; Javid, A.Z.; Mohammadi, F.; Shirbeigi, E. Effects of probiotic yogurt consumption on lipid profile in type 2 diabetic patients: A randomized controlled clinical trial. J. Res. Med. Sci. 2014, 19, 531–536. [Google Scholar] [PubMed]
- Champagne, C.P.; Ross, R.P.; Saarela, M.; Hansen, K.F.; Charalampopoulos, D. Recommendations for the viability assessment of probiotics as concentrated cultures and in food matrices. Int. J. Food Microbiol. 2011, 149, 185–193. [Google Scholar] [CrossRef]
- Homayoni Rad, A.; Mehrabany, E.V.; Alipoor, B.; Mehrabany, L.V.; Javadi, M. Do probiotics act more efficiently in foods than in supplements? Nutrition 2012, 28, 733–736. [Google Scholar] [CrossRef]
- Markowiak, P.; Slizewska, K. Effects of Probiotics, Prebiotics, and Synbiotics on Human Health. Nutrients 2017, 9, 1021. [Google Scholar] [CrossRef]
- Sarkar, A.; Mandal, S. Bifidobacteria—Insight into clinical outcomes and mechanisms of its probiotic action. Microbiol. Res. 2016, 192, 159–171. [Google Scholar] [CrossRef]
- Turroni, F.; Duranti, S.; Milani, C.; Lugli, A.G.; van Sinderen, D.; Ventura, M. Bifidobacterium bifidum: A Key Member of the Early Human Gut Microbiota. Microorganisms 2019, 7, 544. [Google Scholar] [CrossRef]
- Plaza-Diaz, J.; Ruiz-Ojeda, F.J.; Gil-Campos, M.; Gil, A. Mechanisms of Action of Probiotics. Adv. Nutr. 2019, 10, S49–S66. [Google Scholar] [CrossRef]
- Lee, C.W.; Chen, H.J.; Chien, Y.H.; Hsia, S.M.; Chen, J.H.; Shih, C.K. Synbiotic Combination of Djulis (Chenopodium formosanum) and Lactobacillus acidophilus Inhibits Colon Carcinogenesis in Rats. Nutrients 2019, 12, 103. [Google Scholar] [CrossRef]
- Navaei, M.; Haghighat, S.; Janani, L.; Vafa, S.; Saneei Totmaj, A.; Raji Lahiji, M.; Emamat, H.; Salehi, Z.; Amirinejad, A.; Izad, M.; et al. The Effects of Synbiotic Supplementation on Antioxidant Capacity and Arm Volumes in Survivors of Breast Cancer-Related Lymphedema. Nutr. Cancer 2020, 72, 62–73. [Google Scholar] [CrossRef] [PubMed]
- Le, B.; Ngoc, A.P.T.; Yang, S.H. Synbiotic fermented soymilk with Weissella cibaria FB069 and xylooligosaccharides prevents proliferation in human colon cancer cells. J. Appl. Microbiol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Faraki, A.; Noori, N.; Gandomi, H.; Banuree, S.A.H.; Rahmani, F. Effect of Auricularia auricula aqueous extract on survival of Lactobacillus acidophilus La-5 and Bifidobacterium bifidum Bb-12 and on sensorial and functional properties of synbiotic yogurt. Food Sci. Nutr. 2020, 8, 1254–1263. [Google Scholar] [CrossRef] [PubMed]
- Athiyyah, A.; Widjaja, N.; Fitri, P.; Setiowati, A.; Darma, A.; Ranuh, R.; Sudarmo, S. Effects of a multispecies synbiotic on intestinal mucosa immune responses. Iran. J. Microbiol. 2019, 11. [Google Scholar] [CrossRef]
- Morshedi, M.; Saghafi-Asl, M.; Hosseinifard, E.-S. The potential therapeutic effects of the gut microbiome manipulation by synbiotic containing-Lactobacillus plantarum on neuropsychological performance of diabetic rats. J. Transl. Med. 2020, 18, 1–14. [Google Scholar] [CrossRef]
- Ghafouri, A.; Zarrati, M.; Shidfar, F.; Heydari, I.; Shokouhi Shoormasti, R.; Eslami, O. Effect of synbiotic bread containing lactic acid on glycemic indicators, biomarkers of antioxidant status and inflammation in patients with type 2 diabetes: A randomized controlled trial. Diabetol. Metab. Syndr. 2019, 11, 103. [Google Scholar] [CrossRef]
- Moser, A.M.; Spindelboeck, W.; Halwachs, B.; Strohmaier, H.; Kump, P.; Gorkiewicz, G.; Hogenauer, C. Effects of an oral synbiotic on the gastrointestinal immune system and microbiota in patients with diarrhea-predominant irritable bowel syndrome. Eur. J. Nutr. 2019, 58, 2767–2778. [Google Scholar] [CrossRef]
- Pistol, G.C.; Marin, D.E.; Dragomir, C.; Taranu, I. Synbiotic combination of prebiotic grape pomace extract and probiotic Lactobacillus sp. reduced important intestinal inflammatory markers and in-depth signalling mediators in lipopolysaccharide-treated Caco-2 cells. Br. J. Nutr. 2018, 121, 291–305. [Google Scholar] [CrossRef]
- Sengupta, S.; Koley, H.; Dutta, S.; Bhowal, J. Hepatoprotective effects of synbiotic soy yogurt on mice fed a high-cholesterol diet. Nutrition 2019, 63, 36–44. [Google Scholar] [CrossRef]
- Hill, C.; Guarner, F.; Reid, G.; Gibson, G.R.; Merenstein, D.J.; Pot, B.; Morelli, L.; Canani, R.B.; Flint, H.J.; Salminen, S.; et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 506–514. [Google Scholar] [CrossRef]
- Brandi, J.; Di Carlo, C.; Manfredi, M.; Federici, F.; Bazaj, A.; Rizzi, E.; Cornaglia, G.; Manna, L.; Marengo, E.; Cecconi, D. Investigating the Proteomic Profile of HT-29 Colon Cancer Cells after Lactobacillus kefiri SGL 13 Exposure Using the SWATH Method. J. Am. Soc. Mass Spectrom. 2019, 30, 1690–1699. [Google Scholar] [CrossRef] [PubMed]
- Ragul, K.; Kandasamy, S.; Devi, P.B.; Shetty, P.H. Evaluation of functional properties of potential probiotic isolates from fermented brine pickle. Food Chem. 2020, 311, 126057. [Google Scholar] [CrossRef] [PubMed]
- Ayyash, M.; Abu-Jdayil, B.; Itsaranuwat, P.; Galiwango, E.; Tamiello-Rosa, C.; Abdullah, H.; Esposito, G.; Hunashal, Y.; Obaid, R.S.; Hamed, F. Characterization, bioactivities, and rheological properties of exopolysaccharide produced by novel probiotic Lactobacillus plantarum C70 isolated from camel milk. Int. J. Biol. Macromol. 2020, 144, 938–946. [Google Scholar] [CrossRef] [PubMed]
- Rahbar Saadat, Y.; Yari Khosroushahi, A.; Movassaghpour, A.A.; Talebi, M.; Pourghassem Gargari, B. Modulatory role of exopolysaccharides of Kluyveromyces marxianus and Pichia kudriavzevii as probiotic yeasts from dairy products in human colon cancer cells. J. Funct. Foods 2020, 64, 103675. [Google Scholar] [CrossRef]
- Justino, P.F.C.; Franco, A.X.; Pontier-Bres, R.; Monteiro, C.E.S.; Barbosa, A.L.R.; Souza, M.H.L.P.; Czerucka, D.; Soares, P.M.G. Modulation of 5-fluorouracil activation of toll-like/MyD88/NF-κB/MAPK pathway by Saccharomyces boulardii CNCM I-745 probiotic. Cytokine 2020, 125, 154791. [Google Scholar] [CrossRef] [PubMed]
- Ghanavati, R.; Asadollahi, P.; Shapourabadi, M.B.; Razavi, S.; Talebi, M.; Rohani, M. Inhibitory effects of Lactobacilli cocktail on HT-29 colon carcinoma cells growth and modulation of the Notch and Wnt/β-catenin signaling pathways. Microb. Pathog. 2020, 139, 103829. [Google Scholar] [CrossRef]
- Rupasinghe, H.P.V.; Parmar, I.; Neir, S.V. Biotransformation of Cranberry Proanthocyanidins to Probiotic Metabolites by Lactobacillus rhamnosus Enhances Their Anticancer Activity in HepG2 Cells in Vitro. Oxid. Med. Cell. Longev. 2019, 2019, 4750795. [Google Scholar] [CrossRef]
- Nozari, S.; Faridvand, Y.; Etesami, A.; Ahmad Khan Beiki, M.; Miresmaeili Mazrakhondi, S.A.; Abdolalizadeh, J. Potential anticancer effects of cell wall protein fractions from Lactobacillus paracasei on human intestinal Caco-2 cell line. Lett. Appl. Microbiol. 2019, 69, 148–154. [Google Scholar] [CrossRef]
- Chandel, D.; Sharma, M.; Chawla, V.; Sachdeva, N.; Shukla, G. Isolation, characterization and identification of antigenotoxic and anticancerous indigenous probiotics and their prophylactic potential in experimental colon carcinogenesis. Sci. Rep. 2019, 9, 14769. [Google Scholar] [CrossRef]
- Lin, P.-Y.; Li, S.-C.; Lin, H.-P.; Shih, C.-K. Germinated brown rice combined with Lactobacillus acidophilus and Bifidobacterium animalis subsp. lactis inhibits colorectal carcinogenesis in rats. Food Sci. Nutr. 2019, 7, 216–224. [Google Scholar] [CrossRef]
- Karimi Ardestani, S.; Tafvizi, F.; Tajabadi Ebrahimi, M. Heat-killed probiotic bacteria induce apoptosis of HT-29 human colon adenocarcinoma cell line via the regulation of Bax/Bcl2 and caspases pathway. Hum. Exp. Toxicol. 2019, 38, 1069–1081. [Google Scholar] [CrossRef] [PubMed]
- He, L.; Yang, H.; Tang, J.; Liu, Z.; Chen, Y.; Lu, B.; He, H.; Tang, S.; Sun, Y.; Liu, F.; et al. Intestinal probiotics E. coli Nissle 1917 as a targeted vehicle for delivery of p53 and Tum-5 to solid tumors for cancer therapy. J. Biol. Eng. 2019, 13, 58. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Sheng, J.; Wang, M.; Luo, H.; Zhu, J.; Zhang, B.; Liu, Z.; Yang, X. Combination Therapy of TGF-beta Blockade and Commensal-derived Probiotics Provides Enhanced Antitumor Immune Response and Tumor Suppression. Theranostics 2019, 9, 4115–4129. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.C.; Tsai, C.-C.; Hsieh, C.C.; Lan, A.; Huang, C.C.; Leu, S.F. Multispecies probiotics combination prevents ovalbumin-induced airway hyperreactivity in mice. Allergol. Immunopathol. 2018, 46, 354–360. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, S.; Mitsunaga, F. Anti-Allergic Effect of Para-Probiotics from Non-Viable Acetic Acid Bacteria in Ovalbumin-Sensitized Mice. Food Nutr. Sci. 2018, 9, 1376–1385. [Google Scholar] [CrossRef]
- Koh, W.Y.; Utra, U.; Ahmad, R.; Rather, I.A.; Park, Y.-H. Evaluation of probiotic potential and anti-hyperglycemic properties of a novel Lactobacillus strain isolated from water kefir grains. Food Sci. Biotechnol. 2018, 27, 1369–1376. [Google Scholar] [CrossRef]
- Yadav, R.; Dey, D.K.; Vij, R.; Meena, S.; Kapila, R.; Kapila, S. Evaluation of anti-diabetic attributes of Lactobacillus rhamnosus MTCC: 5957, Lactobacillus rhamnosus MTCC: 5897 and Lactobacillus fermentum MTCC: 5898 in streptozotocin induced diabetic rats. Microb. Pathog. 2018, 125, 454–462. [Google Scholar] [CrossRef]
- Miraghajani, M.; Zaghian, N.; dehkohneh, A.; Mirlohi, M.; Ghiasvand, R. Probiotic Soy Milk Consumption and Renal Function among Type 2 Diabetic Patients with Nephropathy: A Randomized Controlled Clinical Trial. Probiotics Antimicrob. Proteins 2019, 11, 124–132. [Google Scholar] [CrossRef]
- Choi, W.J.; Dong, H.J.; Jeong, H.U.; Jung, H.H.; Kim, Y.-H.; Kim, T.H. Antiobesity Effects of Lactobacillus plantarum LMT1-48 Accompanied by Inhibition of Enterobacter cloacae in the Intestine of Diet-Induced Obese Mice. J. Med. Food 2019, 22, 560–566. [Google Scholar] [CrossRef]
- Legrand, R.; Lucas, N.; Dominique, M.; Azhar, S.; Deroissart, C.; Le Solliec, M.-A.; Rondeaux, J.; Nobis, S.; Guérin, C.; Léon, F.; et al. Commensal Hafnia alvei strain reduces food intake and fat mass in obese mice-a new potential probiotic for appetite and body weight management. Int. J. Obes. 2020. [Google Scholar] [CrossRef]
- Kang, D.; Su, M.; Duan, Y.; Huang, Y. Eurotium cristatum, a potential probiotic fungus from Fuzhuan brick tea, alleviated obesity in mice by modulating gut microbiota. Food Funct. 2019, 10, 5032–5045. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.H.; Ho, C.Y.; Chen, C.T.; Hsu, H.F.; Lin, Y.H. Probiotic BSH Activity and Anti-Obesity Potential of Lactobacillus plantarum Strain TCI378 Isolated from Korean Kimchi. Prev. Nutr. Food Sci. 2019, 24, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Hsu, T.C.; Yi, P.J.; Lee, T.Y.; Liu, J.R. Probiotic characteristics and zearalenone-removal ability of a Bacillus licheniformis strain. PLoS ONE 2018, 13, e0194866. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zeng, Y.; Wang, S.; Liu, H.; Zhang, D.; Zhang, W.; Wang, Y.; Ji, H. Swine-Derived Probiotic Lactobacillus plantarum Inhibits Growth and Adhesion of Enterotoxigenic Escherichia coli and Mediates Host Defense. Front. Microbiol. 2018, 9, 1364. [Google Scholar] [CrossRef] [PubMed]
- Rocha-Ramírez, M.L.; Hernández-Ochoa, B.; Gómez-Manzo, S.; Marcial-Quino, J.; Cárdenas-Rodríguez, N.; Centeno-Leija, S.; García-Garibay, M. Evaluation of Immunomodulatory Activities of the Heat-Killed Probiotic Strain Lactobacillus casei IMAU60214 on Macrophages in Vitro. Microorganisms 2020, 8, 79. [Google Scholar] [CrossRef]
- Beller, A.; Kruglov, A.; Durek, P.; von Goetze, V.; Hoffmann, U.; Maier, R.; Heiking, K.; Siegmund, B.; Heinz, G.; Mashreghi, M.F.; et al. P104 Anaeroplasma, a potential anti-inflammatory probiotic for the treatment of chronic intestinal inflammation. Ann. Rheum. Dis. 2019, 78, A45–A46. [Google Scholar] [CrossRef]
- Coqueiro, A.Y.; Raizel, R.; Bonvini, A.; Tirapegui, J.; Rogero, M.M. Probiotics for inflammatory bowel diseases: A promising adjuvant treatment. Int. J. Food Sci. Nutr. 2019, 70, 20–29. [Google Scholar] [CrossRef]
- Machado Prado, M.R.; Boller, C. Anti-inflammatory effects of probiotics. In Discovery and Development of Anti-Inflammatory Agents from Natural Products; Brahmachari, G., Ed.; Elsevier: Amsterdam, The Netherlands, 2019; Chapter 9; pp. 259–282. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, L.; Hong, G.; Huang, C.; Qian, W.; Bai, T.; Song, J.; Song, Y.; Hou, X. Probiotic mixtures with aerobic constituent promoted the recovery of multi-barriers in DSS-induced chronic colitis. Life Sci. 2020, 240, 117089. [Google Scholar] [CrossRef]
- Zhang, Z.; Lv, J.; Pan, L.; Zhang, Y. Roles and applications of probiotic Lactobacillus strains. Appl. Microbiol. Biotechnol. 2018, 102, 8135–8143. [Google Scholar] [CrossRef]
- Lee, J.-E.; Lee, J.; Kim, J.H.; Cho, N.; Lee, S.H.; Park, S.B.; Koh, B.; Kang, D.; Kim, S.; Yoo, H.M. Characterization of the Anti-Cancer Activity of the Probiotic Bacterium Lactobacillus fermentum Using 2D vs. 3D Culture in Colorectal Cancer Cells. Biomolecules 2019, 9, 557. [Google Scholar] [CrossRef]
- Fornai, M.; Pellegrini, C.; Benvenuti, L.; Tirotta, E.; Gentile, D.; Natale, G.; Ryskalin, L.; Colucci, R.; Piccoli, E.; Ghelardi, E.; et al. Protective effects of the combination Bifidobacterium longum plus lactoferrin against NSAID-induced enteropathy. Nutrition 2020, 70, 110583. [Google Scholar] [CrossRef] [PubMed]
- Ben Othman, M.; Sakamoto, K. Effect of inactivated Bifidobacterium longum intake on obese diabetes model mice (TSOD). Food Res. Int. 2020, 129, 108792. [Google Scholar] [CrossRef] [PubMed]
- Talani, G.; Biggio, F.; Mostallino, M.C.; Locci, V.; Porcedda, C.; Boi, L.; Saolini, E.; Piras, R.; Sanna, E.; Biggio, G. Treatment with gut bifidobacteria improves hippocampal plasticity and cognitive behavior in adult healthy rats. Neuropharmacology 2020, 165, 107909. [Google Scholar] [CrossRef] [PubMed]
- Khangwal, I.; Shukla, P. Prospecting prebiotics, innovative evaluation methods, and their health applications: A review. Biotech 2019, 9, 187. [Google Scholar] [CrossRef] [PubMed]
- Korcz, E.; Kerényi, Z.; Varga, L. Dietary fibers, prebiotics, and exopolysaccharides produced by lactic acid bacteria: Potential health benefits with special regard to cholesterol-lowering effects. Food. Funct. 2018, 9, 3057–3068. [Google Scholar] [CrossRef]
- Shehata, M.; El-sahn, M.A.; El-Sohaimy, S.A.; Youssef, M.M. Role and Mechanisms Lowering Cholesterol by Dietary of Probiotics and Prebiotics: A Review. J. Appl. Sci. 2019, 19, 737–746. [Google Scholar] [CrossRef][Green Version]
- Zhu, W.; Zhou, S.; Liu, J.; McLean, R.J.C.; Chu, W. Prebiotic, immuno-stimulating and gut microbiota-modulating effects of Lycium barbarum polysaccharide. Biomed. Pharmacother. 2020, 121, 109591. [Google Scholar] [CrossRef]
- Cerdó, T.; García-Santos, A.J.; G. Bermúdez, M.; Campoy, C. The Role of Probiotics and Prebiotics in the Prevention and Treatment of Obesity. Nutrients 2019, 11, 635. [Google Scholar] [CrossRef]
- Vyas, N.; Nair, S.; Rao, M.; Miraj, S.S. Chapter 29—Childhood Obesity and Diabetes: Role of Probiotics and Prebiotics. In Global Perspectives on Childhood Obesity, 2nd ed.; Bagchi, D., Ed.; Academic Press: Cambridge, MA, USA, 2019. [Google Scholar]
- Laurell, A.; Sjöberg, K. Prebiotics and synbiotics in ulcerative colitis. Scand. J. Gastroenterol. 2017, 52, 477–485. [Google Scholar] [CrossRef]
- Rani, A.; Baruah, R.; Goyal, A. Prebiotic Chondroitin Sulfate Disaccharide Isolated from Chicken Keel Bone Exhibiting Anticancer Potential against Human Colon Cancer Cells. Nutr. Cancer 2019, 71, 825–839. [Google Scholar] [CrossRef]
- Wen, Y.; Wen, P.; Hu, T.G.; Linhardt, R.J.; Zong, M.H.; Wu, H.; Chen, Z.Y. Encapsulation of phycocyanin by prebiotics and polysaccharides-based electrospun fibers and improved colon cancer prevention effects. Int. J. Biol. Macromol. 2020, 149, 672–681. [Google Scholar] [CrossRef] [PubMed]
- Ohara, T.; Mori, T. Antiproliferative Effects of Short-chain Fatty Acids on Human Colorectal Cancer Cells via Gene Expression Inhibition. Anticancer Res. 2019, 39, 4659–4666. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Xie, M.; Yang, F.; Liu, J. Antioxidant activity of high purity blueberry anthocyanins and the effects on human intestinal microbiota. LWT 2020, 117, 108621. [Google Scholar] [CrossRef]
- Li, E.; Yang, S.; Zou, Y.; Cheng, W.; Li, B.; Hu, T.; Li, Q.; Wang, W.; Liao, S.; Pang, D. Purification, Characterization, Prebiotic Preparations and Antioxidant Activity of Oligosaccharides from Mulberries. Molecules 2019, 24, 2329. [Google Scholar] [CrossRef]
- Weinborn, V.; Valenzuela, C.; Olivares, M.; Arredondo, M.; Weill, R.; Pizarro, F. Prebiotics increase heme iron bioavailability and do not affect non-heme iron bioavailability in humans. Food. Funct. 2017, 8, 1994–1999. [Google Scholar] [CrossRef] [PubMed]
- Aliasgharzadeh, A.; Khalili, M.; Mirtaheri, E.; Pourghassem Gargari, B.; Tavakoli, F.; Abbasalizad Farhangi, M.; Babaei, H.; Dehghan, P. A Combination of Prebiotic Inulin and Oligofructose Improve Some of Cardiovascular Disease Risk Factors in Women with Type 2 Diabetes: A Randomized Controlled Clinical Trial. Adv. Pharm. Bull. 2015, 5, 507–514. [Google Scholar] [CrossRef]
- Da Silva Sabo, S.; Converti, A.; Todorov, S.D.; Domínguez, J.M.; de Souza Oliveira, R.P. Effect of inulin on growth and bacteriocin production by Lactobacillus plantarum in stationary and shaken cultures. Int. J. Food Sci. Technol. 2015, 50, 864–870. [Google Scholar] [CrossRef]
- Ramos, C.I.; Armani, R.G.; Canziani, M.E.F.; Dalboni, M.A.; Dolenga, C.J.R.; Nakao, L.S.; Campbell, K.L.; Cuppari, L. Effect of prebiotic (fructooligosaccharide) on uremic toxins of chronic kidney disease patients: A randomized controlled trial. Nephrol. Dial. Transpl. 2018, 34, 1876–1884. [Google Scholar] [CrossRef]
- Flesch, A.G.; Poziomyck, A.K.; Damin, D.C. The therapeutic use of symbiotics. Arq. Bras. Cir. Dig. 2014, 27, 206–209. [Google Scholar] [CrossRef]
- Bonfrate, L.; Palo, D.M.; Celano, G.; Albert, A.; Vitellio, P.; De Angelis, M.; Gobbetti, M.; Portincasa, P. Effects of Bifidobacterium longum BB536 and Lactobacillus rhamnosus HN001 in IBS patients. Eur. J. Clin. Investig. 2020, 50, e13201. [Google Scholar] [CrossRef]
- Mohan, A.; Hadi, J.; Gutierrez-Maddox, N.; Li, Y.; Leung, I.K.H.; Gao, Y.; Shu, Q.; Quek, S.Y. Sensory, Microbiological and Physicochemical Characterisation of Functional Manuka Honey Yogurts Containing Probiotic Lactobacillus reuteri DPC16. Foods 2020, 9, 106. [Google Scholar] [CrossRef] [PubMed]
- Li, P.H.; Lu, W.C.; Chan, Y.J.; Zhao, Y.P.; Nie, X.B.; Jiang, C.X.; Ji, Y.X. Feasibility of Using Seaweed (Gracilaria coronopifolia) Synbiotic as a Bioactive Material for Intestinal Health. Foods 2019, 8, 623. [Google Scholar] [CrossRef] [PubMed]
- Sarwar, A.; Aziz, T.; Al-Dalali, S.; Zhao, X.; Zhang, J.; ud Din, J.; Chen, C.; Cao, Y.; Yang, Z. Physicochemical and Microbiological Properties of Synbiotic Yogurt Made with Probiotic Yeast Saccharomyces boulardii in Combination with Inulin. Foods 2019, 8, 468. [Google Scholar] [CrossRef] [PubMed]
- Karimi, M.; Yazdi, F.T.; Mortazavi, S.A.; Shahabi-Ghahfarrokhi, I.; Chamani, J. Development of active antimicrobial poly (l-glutamic) acid-poly (l-lysine) packaging material to protect probiotic bacterium. Polym. Test. 2020, 83, 106338. [Google Scholar] [CrossRef]
- Aziz Mousavi, S.M.A.; Mirhosseini, S.A.; Rastegar Shariat Panahi, M.; Mahmoodzadeh Hosseini, H. Characterization of Biosynthesized Silver Nanoparticles Using Lactobacillus rhamnosus GG and its in Vitro Assessment against Colorectal Cancer Cells. Probiotics Antimicrob. Proteins 2019. [Google Scholar] [CrossRef]
- Kouhkan, M.; Ahangar, P.; Babaganjeh, L.; Allahyari-Devin, M. Biosynthesis of copper oxide nanoparticles using Lactobacillus casei subsp. casei and its anticancer and antibacterial activities. Curr. Nanosci. 2019, 15. [Google Scholar] [CrossRef]
- Xu, C.; Qiao, L.; Guo, Y.; Ma, L.; Cheng, Y. Preparation, characteristics and antioxidant activity of polysaccharides and proteins-capped selenium nanoparticles synthesized by Lactobacillus casei ATCC 393. Carbohydr. Polym. 2018, 195, 576–585. [Google Scholar] [CrossRef]
- Xu, C.; Guo, Y.; Qiao, L.; Ma, L.; Cheng, Y.; Roman, A. Biogenic Synthesis of Novel Functionalized Selenium Nanoparticles by Lactobacillus casei ATCC 393 and Its Protective Effects on Intestinal Barrier Dysfunction Caused by Enterotoxigenic Escherichia coli K88. Front. Microbiol. 2018, 9, 1129. [Google Scholar] [CrossRef]
- Lee, H.A.; Kim, H.; Lee, K.W.; Park, K.Y. Dead Nano-Sized Lactobacillus plantarum Inhibits Azoxymethane/Dextran Sulfate Sodium-Induced Colon Cancer in Balb/c Mice. J. Med. Food 2015, 18, 1400–1405. [Google Scholar] [CrossRef]
- Markus, J.; Mathiyalagan, R.; Kim, Y.J.; Abbai, R.; Singh, P.; Ahn, S.; Perez, Z.E.J.; Hurh, J.; Yang, D.C. Intracellular synthesis of gold nanoparticles with antioxidant activity by probiotic Lactobacillus kimchicus DCY51(T) isolated from Korean kimchi. Enzym. Microb. Technol. 2016, 95, 85–93. [Google Scholar] [CrossRef]
- Jimenez-Sanchez, M.; Perez-Morales, R.; Goycoolea, F.M.; Mueller, M.; Praznik, W.; Loeppert, R.; Bermudez-Morales, V.; Zavala-Padilla, G.; Ayala, M.; Olvera, C. Self-assembled high molecular weight inulin nanoparticles: Enzymatic synthesis, physicochemical and biological properties. Carbohydr. Polym. 2019, 215, 160–169. [Google Scholar] [CrossRef]
- Kim, W.; Han, G.; Hong, L.; Kang, S.-K.; Shokouhimehr, M.; Choi, Y.-J.; Cho, C. Novel production of natural bacteriocin via internalization of dextran nanoparticles into probiotics. Biomaterials 2019, 218, 119360. [Google Scholar] [CrossRef] [PubMed]
- Cui, L.H.; Yan, C.G.; Li, H.S.; Kim, W.S.; Hong, L.; Kang, S.K.; Choi, Y.J.; Cho, C.S. A New Method of Producing a Natural Antibacterial Peptide by Encapsulated Probiotics Internalized with Inulin Nanoparticles as Prebiotics. J. Microbiol. Biotechnol. 2018, 28, 510–519. [Google Scholar] [CrossRef] [PubMed]
- Hong, L.; Kim, W.S.; Lee, S.M.; Kang, S.K.; Choi, Y.J.; Cho, C.S. Pullulan Nanoparticles as Prebiotics Enhance the Antibacterial Properties of Lactobacillus plantarum through the Induction of Mild Stress in Probiotics. Front. Microbiol. 2019, 10, 142. [Google Scholar] [CrossRef]
- Kaur, K.; Rath, G. Formulation and evaluation of UV protective synbiotic skin care topical formulation. J. Cosmet. Laser Ther. Off. Publ. Eur. Soc. Laser Dermatol. 2019, 21, 332–342. [Google Scholar] [CrossRef] [PubMed]
- Krithika, B.; Preetha, R. Formulation of protein based inulin incorporated synbiotic nanoemulsion for enhanced stability of probiotic. Mat. Res. Express 2019, 6, 114003. [Google Scholar] [CrossRef]
- Atia, A.; Gomaa, A.; Fliss, I.; Beyssac, E.; Garrait, G.; Subirade, M. A prebiotic matrix for encapsulation of probiotics: Physicochemical and microbiological study. J. Microencapsul. 2016, 33, 89–101. [Google Scholar] [CrossRef]
- Caneus, D. Nanotechnology and its Partnership with Synbiotics. J. Nanomed. Res. 2017, 6, 142. [Google Scholar] [CrossRef][Green Version]
- Pathak, K.; Akhtar, N. Nanoprobiotics: Progress and Issues. In Nanonutraceuticals, 1st ed.; Singh., B., Ed.; CRC Press: Boca Raton, FL, USA, 2018; Chapter 9; 326p. [Google Scholar]
- Rajendran, K.; Sen, S.; Latha, P. Nanotechnology in probiotics and prebiotics. In Nanotechnology in Nutraceuticals: Production to Consumption, 1st ed.; Sen, S., Pathak, Y., Eds.; CRC Press: Oxfordshire, UK; Taylor & Francis Group: Oxfordshire, UK; Abingdon-on-Thames: Oxfordshire, UK, 2016; Chapter 9. [Google Scholar]
- Kazmierczak, R.; Choe, E.; Sinclair, J.; Eisenstark, A. Direct attachment of nanoparticle cargo to Salmonella typhimurium membranes designed for combination bacteriotherapy against tumors. Methods Mol. Biol. 2015, 1225, 151–163. [Google Scholar] [CrossRef]
- Hu, Q.; Wu, M.; Fang, C.; Cheng, C.; Zhao, M.; Fang, W.; Chu, P.K.; Ping, Y.; Tang, G. Engineering Nanoparticle-Coated Bacteria as Oral DNA Vaccines for Cancer Immunotherapy. Nano Lett. 2015, 15, 2732–2739. [Google Scholar] [CrossRef]
- Feher, F.; Pinter, E.; Helyes, Z.; Szolcsanyi, J. Nano-size particles of probiotics for preventing and treating neuroinflammation. ARVO Annual Meeting. Investig. Ophthalmol. Vis. Sci. 2012, 53, 331. [Google Scholar]
- Kim, W.S.; Lee, J.Y.; Singh, B.; Maharjan, S.; Hong, L.; Lee, S.M.; Cui, L.H.; Lee, K.J.; Kim, G.; Yun, C.H.; et al. A new way of producing pediocin in Pediococcus acidilactici through intracellular stimulation by internalized inulin nanoparticles. Sci. Rep. 2018, 8, 5878. [Google Scholar] [CrossRef] [PubMed]
- Song, Q.; Zheng, C.; Jia, J.; Zhao, H.; Feng, Q.; Zhang, H.; Wang, L.; Zhang, Z.; Zhang, Y. A Probiotic Spore-Based Oral Autonomous Nanoparticles Generator for Cancer Therapy. Adv. Mater. 2019, 31, e1903793. [Google Scholar] [CrossRef] [PubMed]
- Fung, W.Y.; Yuen, K.H.; Liong, M.T. Agrowaste-based nanofibers as a probiotic encapsulant: Fabrication and characterization. J. Agric. Food Chem. 2011, 59, 8140–8147. [Google Scholar] [CrossRef] [PubMed]
- Nagy, Z.K.; Wagner, I.; Suhajda, A.; Tobak, T.; Harsztos, A.H.; Vigh, T.; Soti, P.L.; Pataki, K.; Molnar, K.; Marosi, G. Nanofibrous solid dosage form of living bacteria prepared by electrospinning. Express Polym. Lett. 2014, 8, 352–361. [Google Scholar] [CrossRef]
- Zupancic, S.; Škrlec, K.; Kocbek, P.; Kristl, J.; Berlec, A. Effects of electrospinning on the viability of ten species of lactic acid bacteria in poly(ethylene oxide) nanofibers. Pharmaceutics 2019, 11, 483. [Google Scholar] [CrossRef]
- Wang, A.; Xu, C.; Zhang, C.; Gan, Y.; Wang, B. Experimental Investigation of the Properties of Electrospun Nanofibers for Potential Medical Application. J. Nanomater. 2015, 2015, 418932. [Google Scholar] [CrossRef]
- Xue, J.; Xie, J.; Liu, W.; Xia, Y. Electrospun Nanofibers: New Concepts, Materials, and Applications. Acc. Chem. Res. 2017, 50, 1976–1987. [Google Scholar] [CrossRef]
- Shahriar, S.M.; Mondal, J.; Hasan, M.N.; Revuri, V.; Lee, D.Y.; Lee, Y.K. Electrospinning Nanofibers for Therapeutics Delivery. Nanomaterials 2019, 9, 532. [Google Scholar] [CrossRef]
- Torres-Martínez, E.T.; Cornejo Bravo, J.M.; Serrano Medina, A.; Pérez González, G.L.; Villarreal Gómez, L.J. A summary of electrospun nanofibers as drug delivery system: Drugs loaded and biopolymers used as matrices. Curr. Drug Deliv. 2018, 15, 1360–1374. [Google Scholar] [CrossRef]
- Ghorani, B.; Tucker, N. Fundamentals of electrospinning as novel delivery for bioactive compounds in food nanotechnology. Food Hydrocoll. 2015, 51, 227–240. [Google Scholar] [CrossRef]
- Franz, B.; Balkundi, S.S.; Dahl, C.; Lvov, Y.M.; Prange, A. Layer-by-layer nano-encapsulation of microbes: Controlled cell surface modification and investigation of substrate uptake in bacteria. Macromol. Biosci. 2010, 11, 164–172. [Google Scholar] [CrossRef] [PubMed]
- Ebrahimnejad, P.; Khavarpour, M.; Khalilid, S. Survival of Lactobacillus Acidophilus as probiotic bacteria using chitosan nanoparticles. IJE Trans. A Basics 2017, 30, 456–463. [Google Scholar]
- Ranjan, S.; Dasgupta, N.; Chakraborty, A.R.; Melvin Samuel, S.; Ramalingam, C.; Shanker, R.; Kumar, A. Nanoscience and nanotechnologies in food industries: Opportunities and research trends. J. Nanopart. Res. 2014, 16, 2464. [Google Scholar] [CrossRef]
- Salmerón, I. Fermented cereal beverages: From probiotic, prebiotic and synbiotic towards Nanoscience designed healthy drinks. Lett. Appl. Microbiol. 2017, 65, 114–124. [Google Scholar] [CrossRef]
- Rezaee, P.; Kasra Kermanshahi, R.; Katouli, M. Prebiotics decrease the antibacterial effect of nano silver and nano TiO2 particles against probiotic bacteria of food. Curr. Nutr. Food Sci. 2014, 10. [Google Scholar] [CrossRef]
- Khan, S.T.; Saleem, S.; Ahamed, M.; Ahmad, J. Survival of probiotic bacteria in the presence of food grade nanoparticles from chocolates: An in vitro and in vivo study. Appl. Microbiol. Biotechnol. 2019, 103, 6689–6700. [Google Scholar] [CrossRef]
- Liu, J.M.; Zhao, N.; Wang, Z.H.; Lv, S.W.; Li, C.Y.; Wang, S. In-Taken Labeling and in Vivo Tracing Foodborne Probiotics via DNA-Encapsulated Persistent Luminescence Nanoprobe Assisted Autofluorescence-Free Bioimaging. J. Agric. Food Chem. 2019, 67, 514–519. [Google Scholar] [CrossRef]
- EFSA Scientific Committee. Scientific Opinion: Guidance on the risk assessment of the application of nanoscience and nanotechnologies in the food and feed chain. EFSA J. 2011, 9, 2140. [Google Scholar] [CrossRef]
- McClements, D.J.; Xiao, H. Is nano safe in foods? Establishing the factors impacting the gastrointestinal fate and toxicity of organic and inorganic food-grade nanoparticles. NPJ Sci. Food 2017, 1, 6. [Google Scholar] [CrossRef]
- Gwinn, M.R.; Vallyathan, V. Nanoparticles: Health Effects—Pros and Cons. Environ. Health Perspect. 2006, 114, 1818–1825. [Google Scholar] [CrossRef] [PubMed]
| Type | Microorganisms/Prebiotics | Activity | Study | References |
|---|---|---|---|---|
| Probiotic | Bacillus and Enterobacter | Anticancer and antioxidant effect | The intracellular cell-free supernatants (CFS) from Bacillus licheniformis KT921419 and the ethyl acetate extracts could control the growth of HT-29, a colon cancer cell line | [100] |
| L. plantarum C70 | Anticancer effect | L. plantarum C70 by releasing the exopolysaccharide caused 73.1% and 88.1% cytotoxic properties against the breast and colon cancers, respectively | [101] | |
| Kluyveromyces marxianus and Pichia kudriavzevii | Anticancer effect | According to analysis of Annexin V/PI and DAPI, an apoptotic induction was observed due to exopolysaccharides released by probiotic yeasts of Kluyveromyces marxianus and Pichia kudriavzevii | [102] | |
| Lactobacilli cocktail | Anticancer effect | HT-29, a human colorectal carcinoma cell line was controlled by Lactobacilli cocktail via the modulation of the Notch and Wnt/β-catenin signaling pathways | [104] | |
| L. rhamnosus | Anticancer effect | The bioconversion of cranberry proanthocyanidins to Lactobacillus rhamnosus could result in the IC50 values of 20.1 and 47.8 μg/mL | [105] | |
| Bifidobacterium infantis, L. acidophilus, Enterococcus faecalis, Bacillus cereus | Anti-inflammatory effect | A mixture of aerobic probiotics improved the functions of various intestinal barriers and the restoration of lucrative intestinal microbiota in the mouse model of DSS-induced chronic colitis, meaning anti-inflammatory properties | [127] | |
| Saccharomyces boulardii CNCM I-745 | Anti-inflammatory effect | The inflammatory response was modulated in mucositis caused by 5-FU (fluorouracil) via the probiotic Saccharomyces boulardii CNCM I-745 through the control of TLR 2 and 4 as well as the reduction of pro-inflammatory and NF-κB cytokines | [103] | |
| L. casei IMAU60214 | Immunomodulatory effect | The use of L. casei IMAU60214 killed by heat increased the activity of M1-like pro-inflammatory phenotype through the TLR2 signaling pathway | [123] | |
| L. plantarum | Antimicrobial effect | L. plantarum ZLP001 impeded the ETEC adhesion and linked with IPEC-J2 cells via the competition and exclusion | [122] | |
| Lactobacillus | Anti-diabetic effect | The lactobacillus strain alleviated the levels of blood sugar and HbA1c in diabetic rats | [115] | |
| L. plantarum LMT1-48 | Anti-obesity effect | The body weight and abdominal fat content were decreased in mouse models fed a modified diet through the administration of L. plantarum LMT1-48 at a density of 106 CFU/mL | [117] | |
| Hafnia alvei | Anti-obesity effect | Fat mass, food intake, and body weights were reduced in the mouse model of obesity and hyperphagia | [118] | |
| Eurotium cristatum | Anti-obesity effect | The administration of Eurotium cristatum showed anti-obesity activity in mice fed a high-fat diet (HFD) through the modulation of gut microbiota | [119] | |
| L. plantarum strain TCI378 | Anti-obesity | The expression of glucose transporter type 4 (GLUT-4) and adipocyte-specific genes perilipin 1 was suppressed by metabolism derivatives from L. plantarum strain TCI378 | [120] | |
| Prebiotic | Galacto-oligosaccharides and phycocyanin | Anticancer effect | The prebiotics co-administered by phycocyanin arrested the cell cycle at the G0/G1 phase, resulting in inhibited growth of HCT116 cells | [141] |
| Chondroitin Sulfate Disaccharide | Anticancer effect | The growth of HT-29, human colon cancer cell line, was controlled by Chondroitin sulfate (CS)-Keel disaccharide (CSD) generated by chondroitin AC lyase, estimating at 80% antiproliferative activity | [140] | |
| Short-chain fatty acids | Antiproliferative effects | The administration of short-chain fatty acids (SCFAs) prevented the expression of genes involved in human colorectal cancer cells | [142] | |
| Blueberry anthocyanins | Antioxidant effect | The density and composition of intestinal microbiota in human models were increased by consumption of high purity blueberry anthocyanins through the increase in the modulatory and prebiotic activities | [143] | |
| Oligosaccharides | Antioxidant effect | The water-soluble oligosaccharide of EMOS-1a showed 1420% proliferation level | [144] | |
| Lycium barbarum polysaccharide | Immunomodulation effect | The administration of polysaccharides derived from Lycium barbarum in mice showed immunomodulatory effects, and enhanced density of beneficial bacteria and gut microbiota | [136] | |
| Synbiotic | Djulis (Chenopodium formosanum) with L. acidophilus | Anticancer effect | The co-administration of Djulis (Chenopodium formosanum Koidz.) and Lactobacillus acidophilus inhibited the growth of rat colon cancer cells through the promotion of apoptosis, proliferation, and inflammation | [80] |
| L. casei, acidophilus, rhamnosus, bulgaricus, Bifidobacterium breve, longum and Streptococcus thermophilus with fructo-oligosaccharides. | Anticancer and antioxidant effect | Ten weeks of low-calorie diet program along with synbiotic supplementation enhanced the activity of superoxide dismutase (SOD) and reduced the serum level of malondialdehyde (MDA) in obese patients suffering from breast cancer-related lymphedema | [89] | |
| Weissella cibaria FB069 with xylooligosaccharides | Anticancer effect | The use of synbiotic-fermented soymilk (containing xylooligosaccharides and Weissella cibaria FB069) inhibited the proliferation of HCT116 and Caco-2, colorectal cancer cell lines, through the reduction in the transcription of MD2/TLR4/MyD88/NF-κB | [90] | |
| Auricularia auricula aqueous with L. acidophilus La-5 and Bifidobacterium bifidum Bb-12 | Antioxidant effect | The aqueous extract of Auricularia auricula in the presence of L. acidophilus La-5 and Bifidobacterium bifidum Bb-12 significantly elevated the level of phenolic compounds and the activity of antioxidant properties up to 1057.6 mg of Gallic acid/kg and 115.30 of mg BHT eq/kg following 28-day storage | [91] | |
| L. bulgaricus PXN 39, L. casei subsp. casei PXN 37, Bifidobacterium breve PXN 25, L. rhamnosus PXN 54, B. infantis PXN 27 Lactobacillus acidophilus PXN 35, Streptococcus thermophilus PXN 66 with fructo-oligosaccharides | Immunomodulation effect | The use of multispecies symbiotic showed immunoregulatory effects on the expression levels of CD4 and IgA in mice exposed to lipopolysaccharide (LPS) | [92] | |
| L. plantarum with inulin | Neuropsychological effect | Concomitant administration of inulin and L. plantarum in diabetic rats improved CREB/BDNF/TrkB signaling pathway, serotonin secretion, brain parameters, intestinal microbial composition, and oxidative stress, thus leading to improved memory and learning disorders | [93] | |
| β-glucan, Bacillus coagulans, and inulin, lactic acid | Anti-diabetic effect | Eight weeks of taking daily synbiotic plus lactic acid improved the levels of GSH-Px, SOD and HbA1c in patients with type II diabetes | [94] | |
| Corn starch, maltodextrin, inulin, fructooligosaccharides, potassium chloride, magnesium sulfate, mangan sulfate with L. casei W56, acidophilus W22, paracasei W20, salivarius W24, plantarum W62, Lactococcus lactis W19, Bifidobacterium lactis W51 and W52, and Bifidobacterium bifidum W23 | Improve symptoms of diarrhea-predominant irritable bowel syndrome | Irritable bowel syndrome (IBS) symptoms were improved by synbiotic treatment through an increase in fecal acetate and butyrate, colonic CD4+ T cells, mucosal microbial diversity as well as a decrease in surrogate of intestinal barrier function and fecal zonulin | [95] | |
| Grape pomace extract with lactobacilli | Anti- inflammatory effect | The co-administration of lactobacilli and prebiotic grape pomace caused a downregulation of inflammatory genes, proteins, signaling molecules through the symbiotic effects | [96] | |
| L. acidophilus, L. rhamnosus, B. longum and Bifidobacterium bifidum, Saccharomyces boulardii with fructo-oligosaccharides | Hepatoprotective effects | The administration of synbiotic soy yogurt controlled hypercholesterolemia in mice liver by reducing the levels of low-density lipoprotein cholesterol, triacylglycerols, blood cholesterol, and lipid peroxidation. | [97] |
| Type | Activity | Study | References |
|---|---|---|---|
| Probiotic | Antimicrobial effect | The polylysine-induced poly glutamic acid (PG) films caused protection of probiotics against food-borne pathogens | [154] |
| Anticancer effect | The high levels of synthesized silver/Lactobacillus rhamnosus GG nanoparticles (Ag-LNPs) led to a decline in the rate of HT-29 live cells | [155] | |
| Anticancer and antimicrobial effect | The fabrication of copper oxide nanoparticles (CuO-NPs) using L. casei could control the proliferation of HT-29, a human colon carcinoma cell line, and human gastric carcinoma cell line, as well as could eliminate Pseudomonas aeruginosa and Staphylococcus aureus | [156] | |
| Anticancer and antioxidant effect | The L. casei capped-SeNPS suppressed the cytotoxicity caused by Diquat and oxidative damage, impeded the cell damage and apoptosis induced by H2O2, and induced the apoptosis mediated by the HepG2 cell line | [157] | |
| Anticancer and antioxidant effect | The findings from the administration of L. casei 393-SeNPs were the induction of HepG2 cell line apoptosis, the elevation of oxidative damage caused by Diquat in IECs, and the reduction in gut barrier dysfunction caused by ETEC K88 via the antioxidant functions, the regulation of inflammation, the establishment of gut epithelial barrier integrity, and the balance of gut microflora | [158] | |
| Anticancer effect | Dead nano-scale L. plantarum could impede the proliferation of a colorectal cancer cell line through an increase in the expression level of IgA, an induction of cancer cell cycle arrest and apoptosis, and a suppression of inflammatory response | [159] | |
| Anticancer and antioxidant effect | The synthesis gold nanoparticles (AuNps) having antioxidant activity and low cytotoxicity using L. kimchicus DCY51T strain exhibited the activity of a protective protein capping layer | [160] | |
| Prebiotic | Improve drug delivery | High molecular weight (HMW) inulin nanoparticles were fabricated to achieve drug delivery system, whose concentration of <200 μg/mL had no toxicity for peripheral blood mononuclear cells (PBMCs) | [161] |
| Antimicrobial effect | The probiotics were internalized by phthalyl dextran nanoparticles (PDNs) to construct pediocin, aiming at the alteration of gut microbiome composition, the suppression of pathogenic intestinal infections, and the elevation of beneficial bacteria species | [162] | |
| Antimicrobial effect | The higher pediocin generation following the administration of PIN-internalized probiotics with 0.171 polydispersity index (PDI) with a size of about 203 nm showed the maximum antimicrobial properties | [163] | |
| Synbiotic | Antimicrobial effect | The activity of Listeria monocytogenes and Escherichia coli K99 was inhibited by L. plantarum exposed to phthalylpullulan nanoparticle (PPN) due to production of antimicrobial peptides via intracellular stimulation | [164] |
| The photo protective effect | A cream containing L. rhamnosus plus Selenium nanoparticles could heal the side effects induced by sunburn and showed sun protection factor (SPF) of 29.77 in Wistar rat model | [165] | |
| Improve delivery system | A new formulation of nano-emulsion containing E. faecium plus inulin could increase probiotic bacterial viability and stability | [166] | |
| Improve tolerance of probiotic bacteria | Beads reinforced by inulin (5% w/v) had the highest effect on bacterial protection against bile salts | [167] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Durazzo, A.; Nazhand, A.; Lucarini, M.; Atanasov, A.G.; Souto, E.B.; Novellino, E.; Capasso, R.; Santini, A. An Updated Overview on Nanonutraceuticals: Focus on Nanoprebiotics and Nanoprobiotics. Int. J. Mol. Sci. 2020, 21, 2285. https://doi.org/10.3390/ijms21072285
Durazzo A, Nazhand A, Lucarini M, Atanasov AG, Souto EB, Novellino E, Capasso R, Santini A. An Updated Overview on Nanonutraceuticals: Focus on Nanoprebiotics and Nanoprobiotics. International Journal of Molecular Sciences. 2020; 21(7):2285. https://doi.org/10.3390/ijms21072285
Chicago/Turabian StyleDurazzo, Alessandra, Amirhossein Nazhand, Massimo Lucarini, Atanas G. Atanasov, Eliana B. Souto, Ettore Novellino, Raffaele Capasso, and Antonello Santini. 2020. "An Updated Overview on Nanonutraceuticals: Focus on Nanoprebiotics and Nanoprobiotics" International Journal of Molecular Sciences 21, no. 7: 2285. https://doi.org/10.3390/ijms21072285
APA StyleDurazzo, A., Nazhand, A., Lucarini, M., Atanasov, A. G., Souto, E. B., Novellino, E., Capasso, R., & Santini, A. (2020). An Updated Overview on Nanonutraceuticals: Focus on Nanoprebiotics and Nanoprobiotics. International Journal of Molecular Sciences, 21(7), 2285. https://doi.org/10.3390/ijms21072285