Effect of Print Orientation and Thermal Aging on the Flexural Strength of Zirconia-Reinforced Three-Dimensional-Printed Restorative Resin Materials
Abstract
1. Introduction
2. Results
2.1. Three-Point-Bending Test
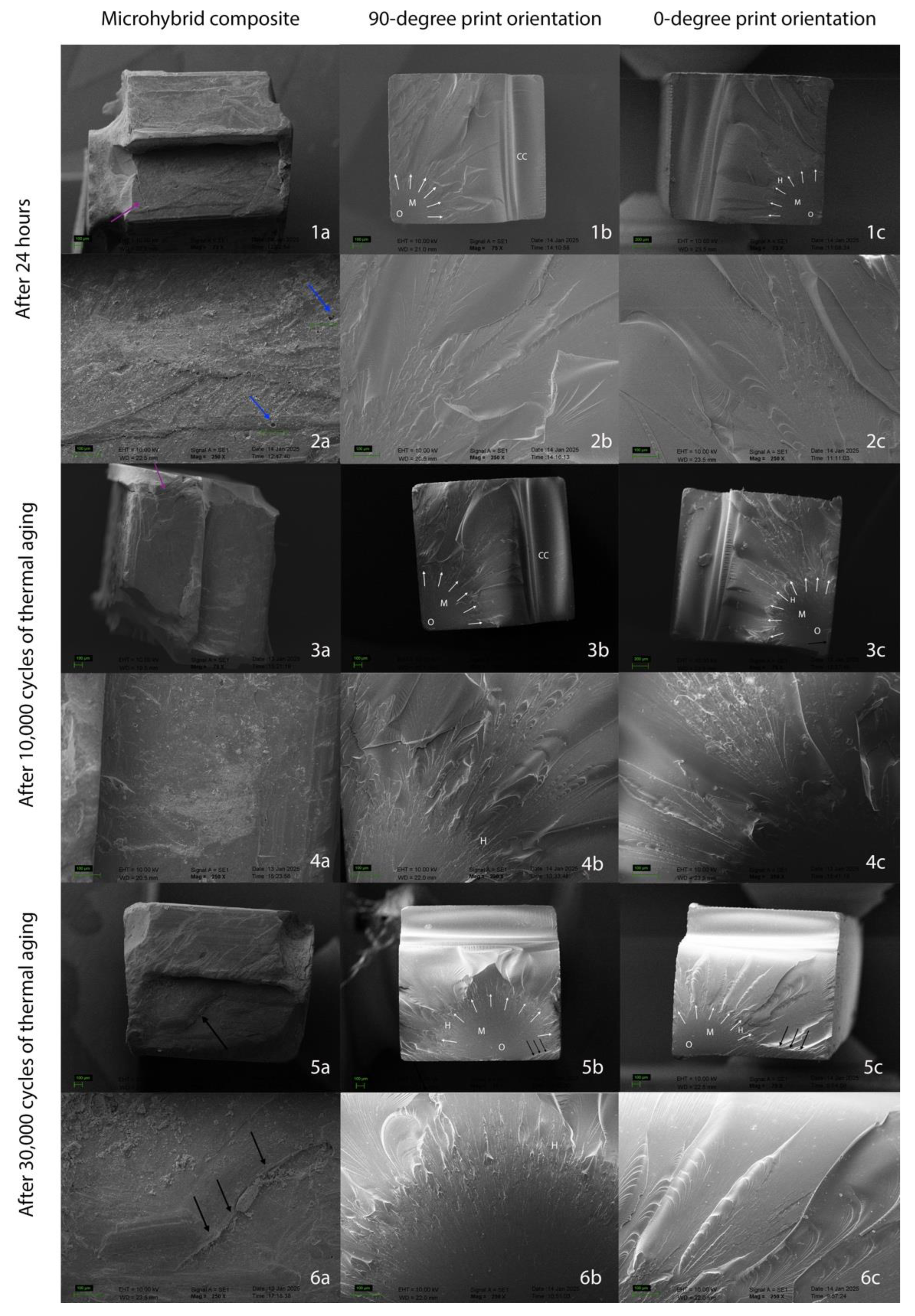
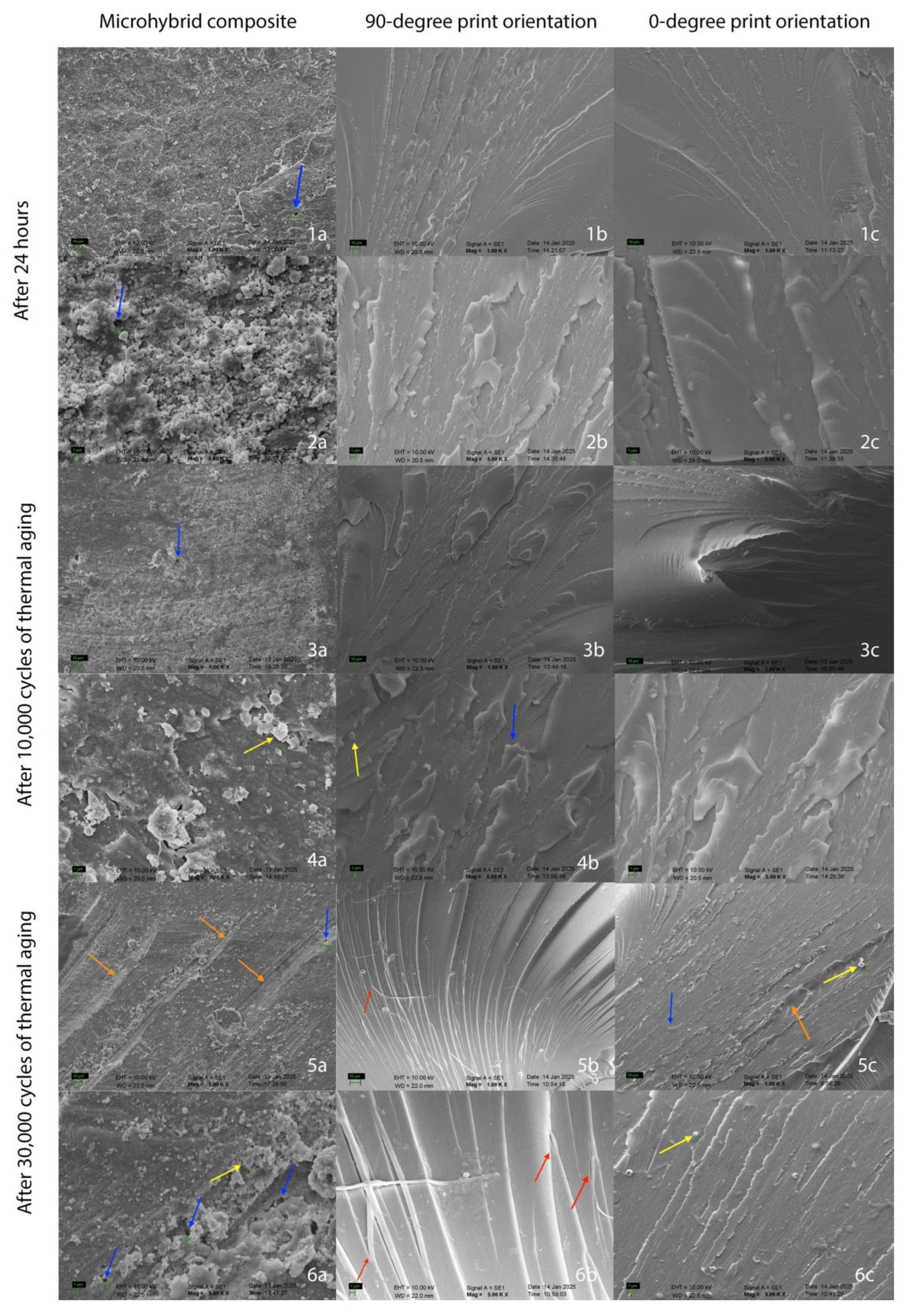
2.2. Scanning Electron Microscope (SEM) Analysis
3. Discussion
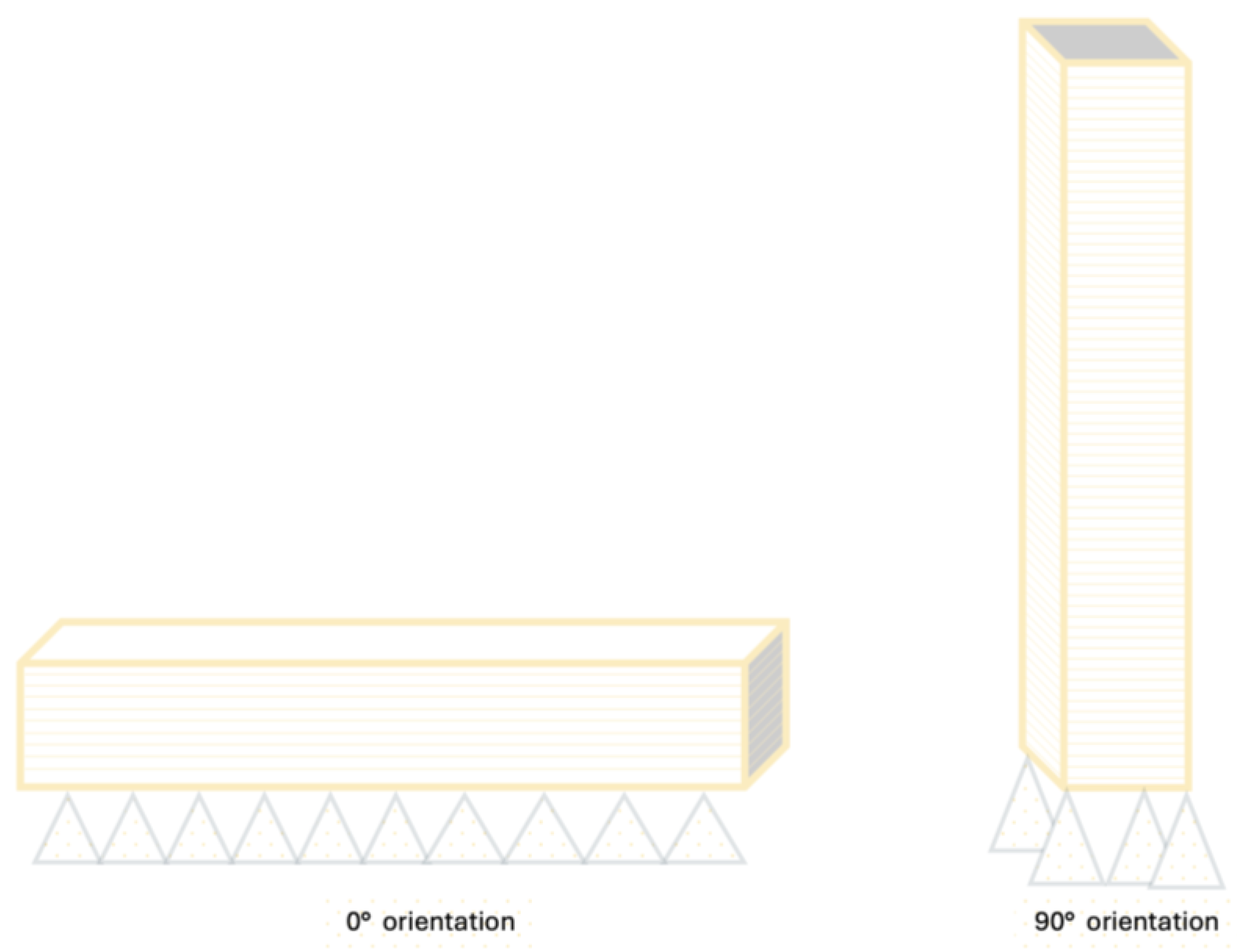
4. Materials and Methods
Sample Preparation and Artificial Aging
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| FS | Flexural strength |
| FM | Flexural modulus |
| 3D | Three-dimensional |
| PMMA | Polymethyl methacrylate |
| DLP | Digital light processing |
| SEM | Scanning electron microscopy |
| CAD-CAM | Computer-aided design and computer-aided manufacturing |
| SM | Subtractive manufacturing |
| AM | Additive manufacturing |
| ISO | The International Organization for Standardization |
| MPa | Megapascal |
| GPa | Gigapascal |
| PEEK | Polyether ether ketone |
| SLA | Stereolithography |
| UDMA | Urethane dimethacrylate |
| BIS-EMA | Bisphenol a polyethylene glycol diether dimethacrylate |
| BIS-GMA | Bisphenol a-glycidyl methacrylate |
| STL | Standard tessellation language |
References
- Barazanchi, A.; Li, K.C.; Al-Amleh, B.; Lyons, K.; Waddell, J.N. Additive Technology: Update on Current Materials and Applications in Dentistry. J. Prosthodont. 2017, 26, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Alghauli, M.A.; Alqutaibi, A.Y. 3D-printed intracoronal restorations, occlusal and laminate veneers: Clinical relevance, properties, and behavior compared to milled restorations; a systematic review and meta-analysis. J. Esthet. Restor. Dent. 2024, 36, 1153–1170. [Google Scholar] [CrossRef] [PubMed]
- Warrier, D.; Jayalakshmi, D. A Review On Temporary Restorative Materials. Int. J. Pharma Sci. Res. 2016, 7, 315–319. Available online: https://scholar.google.com/scholar?hl=tr&as_sdt=0%2C5&q=3.%09Warrier+D%3B+Jayalakshmi+D.+A+Review+On+Temporary+Restorative+Materials.+International+Journal+of+Pharma+Sciences+and+Re-search.+2016%3B7%287%29%3A315-319.+&btnG= (accessed on 5 January 2025).
- Seidel, A.; Belli, R.; Breidebach, N.; Wichmann, M.; Matta, R.E. The occlusal wear of ceramic fixed dental prostheses: 3-Year results in a randomized controlled clinical trial with split-mouth design. J. Dent. 2020, 103, 103500. [Google Scholar] [CrossRef]
- Atria, P.J.; Bordin, D.; Marti, F.; Nayak, V.V.; Conejo, J.; Benalcázar Jalkh, E.; Witek, L.; Sampaio, C.S. 3D-printed resins for provisional dental restorations: Comparison of mechanical and biological properties. J. Esthet. Restor. Dent. 2022, 34, 804–815. [Google Scholar] [CrossRef]
- AlGhamdi, M.A.; Alatiyyah, F.M.; Dawood, Z.H.A.; Alshaikhnasser, F.Y.; Almedarham, R.F.; Alboryh, S.Y.; Elakel, A.; Akhtar, S.; Khan, S.Q.; Gad, M.M. Flexural strength of 3D-printed nanocomposite provisional resins: Impact of SiO(2) and ZrO(2) nanoparticles and printing orientations in vitro. J. Prosthodont. 2024, 1–11. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M. Factors affecting flexural strength of 3D-printed resins: A systematic review. J. Prosthodont. 2023, 32, 96–110. [Google Scholar] [CrossRef]
- Nguyen, J.; Ruse, D.; Phan, A.; Sadoun, M. High-temperature-pressure polymerized resin-infiltrated ceramic networks. J. Dent. Res. 2014, 93, 62–67. [Google Scholar] [CrossRef]
- Yilmaz, E.Ç.; Sadeler, R. A literature review on chewing simulation and wear mechanisms of dental biomaterials. J. Bio-Tribo-Corros. 2021, 7, 91. [Google Scholar] [CrossRef]
- Mudhaffer, S.; Haider, J.; Satterthwaite, J.; Silikas, N. Effects of print orientation and artificial aging on the flexural strength and flexural modulus of 3D printed restorative resin materials. J. Prosthet. Dent. 2024, 133, 1345–1357. [Google Scholar] [CrossRef]
- Unkovskiy, A.; Bui, P.H.; Schille, C.; Geis-Gerstorfer, J.; Huettig, F.; Spintzyk, S. Objects build orientation, positioning, and curing influence dimensional accuracy and flexural properties of stereolithographically printed resin. Dent. Mater. 2018, 34, e324–e333. [Google Scholar] [CrossRef] [PubMed]
- Wulff, J.; Rauch, A.; Schmidt, M.B.; Rosentritt, M. Biaxial Flexural Strength of Printed Splint Materials. Materials 2024, 17, 1112. [Google Scholar] [CrossRef]
- Alghauli, M.A.; Alqutaibi, A.Y.; Aljohani, R.; Almuzaini, S.; Saeed, M.H. Influence of different print orientations on properties and behavior of additively manufactured resin dental devices: A systematic review and meta-analysis. J. Prosthet. Dent. 2025, 133, 736.e1–736.e12. [Google Scholar] [CrossRef]
- Väyrynen, V.O.; Tanner, J.; Vallittu, P.K. The anisotropicity of the flexural properties of an occlusal device material processed by stereolithography. J. Prosthet. Dent. 2016, 116, 811–817. [Google Scholar] [CrossRef]
- Morel, L.L.; Almeida, M.V.R.; Santos, K.M.D.; Praseres, M.F.; Gonçalves Girundi, A.L.; Alexandrino, L.D.; da Silva, W.J. Reinforcement of 3D-printed resins for denture base by adding aramid fibers: Effect on mechanical, surface, and optical properties. J. Prosthodont. 2024. [Google Scholar] [CrossRef] [PubMed]
- Salgado, H.; Fialho, J.; Marques, M.; Vaz, M.; Figueiral, M.; Mesquita, P. Mechanical and surface properties of a 3D-printed dental resin reinforced with graphene. Rev. Port. De Estomatol. Med. Dentária E Cir. Maxilofac. 2023, 64, 12–19. [Google Scholar] [CrossRef]
- Almedarham, R.F.; Al Dawood, Z.H.; Alatiyyah, F.M.; Akhtar, S.; Khan, S.Q.; Shetty, A.C.; Gad, M.M. Flexural properties of additive manufactured resin designated for interim fixed dental prosthesis: Effect of nanoparticles, build direction, and artificial aging. Saudi Dent. J. 2024, 36, 1417–1424. [Google Scholar] [CrossRef]
- Scherer, M.D.; Barmak, A.B.; Özcan, M.; Revilla-León, M. Influence of postpolymerization methods and artificial aging procedures on the fracture resistance and flexural strength of a vat-polymerized interim dental material. J. Prosthet. Dent. 2022, 128, 1085–1093. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, A.K.C.; de Freitas, R.F.C.P.; de Carvalho, I.H.G.; de Miranda, L.M.; da Silva, N.R.; de Fátima Dantas de Almeida, L.; Zhang, Y.; Carreiro, A.d.F.P.; Souza, R.O.d.A.e. Flexural strength, surface roughness, micro-CT analysis, and microbiological adhesion of a 3D-printed temporary crown material. Clin. Oral Investig. 2023, 27, 2207–2220. [Google Scholar] [CrossRef]
- Alshamrani, A.; Alhotan, A.; Kelly, E.; Ellakwa, A. Mechanical and Biocompatibility Properties of 3D-Printed Dental Resin Reinforced with Glass Silica and Zirconia Nanoparticles: In Vitro Study. Polymers 2023, 15, 2523. [Google Scholar] [CrossRef]
- Alshamrani, A.; Alhotan, A.; Owais, A.; Ellakwa, A. The Clinical Potential of 3D-Printed Crowns Reinforced with Zirconia and Glass Silica Microfillers. J. Funct. Biomater. 2023, 14, 267. [Google Scholar] [CrossRef]
- Alshaikh, A.A.; Khattar, A.; Almindil, I.A.; Alsaif, M.H.; Akhtar, S.; Khan, S.Q.; Gad, M.M. 3D-Printed Nanocomposite Denture-Base Resins: Effect of ZrO(2) Nanoparticles on the Mechanical and Surface Properties In Vitro. Nanomaterials 2022, 12, 2451. [Google Scholar] [CrossRef] [PubMed]
- Aati, S.; Akram, Z.; Ngo, H.; Fawzy, A.S. Development of 3D printed resin reinforced with modified ZrO2 nanoparticles for long-term provisional dental restorations. Dent. Mater. 2021, 37, e360–e374. [Google Scholar] [CrossRef]
- Simeon, P.; Unkovskiy, A.; Saadat Sarmadi, B.; Nicic, R.; Koch, P.J.; Beuer, F.; Schmidt, F. Wear resistance and flexural properties of low force SLA- and DLP-printed splint materials in different printing orientations: An in vitro study. J. Mech. Behav. Biomed. Mater. 2024, 152, 106458. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.H.; Lin, Y.M.; Lai, Y.L.; Lee, S.Y. Mechanical properties, accuracy, and cytotoxicity of UV-polymerized 3D printing resins composed of Bis-EMA, UDMA, and TEGDMA. J. Prosthet. Dent. 2020, 123, 349–354. [Google Scholar] [CrossRef]
- Masouras, K.; Silikas, N.; Watts, D.C. Correlation of filler content and elastic properties of resin-composites. Dent. Mater. 2008, 24, 932–939. [Google Scholar] [CrossRef] [PubMed]
- Randolph, L.D.; Palin, W.M.; Leloup, G.; Leprince, J.G. Filler characteristics of modern dental resin composites and their influence on physico-mechanical properties. Dent. Mater. 2016, 32, 1586–1599. [Google Scholar] [CrossRef]
- Rodríguez, H.A.; Kriven, W.M.; Casanova, H. Development of mechanical properties in dental resin composite: Effect of filler size and filler aggregation state. Mater. Sci. Eng. C 2019, 101, 274–282. [Google Scholar] [CrossRef]
- Calheiros, F.C.; Daronch, M.; Rueggeberg, F.A.; Braga, R.R. Degree of conversion and mechanical properties of a BisGMA: TEGDMA composite as a function of the applied radiant exposure. J. Biomed. Mater. Res. Part B Appl. Biomater. 2008, 84B, 503–509. [Google Scholar] [CrossRef]
- Reymus, M.; Fabritius, R.; Keßler, A.; Hickel, R.; Edelhoff, D.; Stawarczyk, B. Fracture load of 3D-printed fixed dental prostheses compared with milled and conventionally fabricated ones: The impact of resin material, build direction, post-curing, and artificial aging—An in vitro study. Clin. Oral Investig. 2020, 24, 701–710. [Google Scholar] [CrossRef] [PubMed]
- Taormina, G.; Sciancalepore, C.; Messori, M.; Bondioli, F. 3D printing processes for photocurable polymeric materials: Technologies, materials, and future trends. J. Appl. Biomater. Funct. Mater. 2018, 16, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Mayer, J.; Reymus, M.; Mayinger, F.; Edelhoff, D.; Hickel, R.; Stawarczyk, B. Temporary 3D printed fixed dental prosthesis materials: Impact of post printing cleaning methods on degree of conversion as well as surface and mechanical properties. Int. J. Prosthodont. 2021, 34, 10–1160. [Google Scholar] [CrossRef]
- Ferracane, J.; Berge, H.; Condon, J. In vitro aging of dental composites in water—Effect of degree of conversion, filler volume, and filler/matrix coupling. J. Biomed. Mater. Res. 1998, 42, 465–472. [Google Scholar] [CrossRef]
- Takeshige, F.; Kawakami, Y.; Hayashi, M.; Ebisu, S. Fatigue behavior of resin composites in aqueous environments. Dent. Mater. 2007, 23, 893–899. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.W.; Kim, J.E.; Choi, Y.J.; Shin, S.H.; Nam, N.E.; Shim, J.S.; Lee, K.-W. Evaluation of the color stability of 3D-printed crown and bridge materials against various sources of discoloration: An in vitro study. Materials 2020, 13, 5359. [Google Scholar] [CrossRef]
- KeßLer, A.; Hickel, R.; Ilie, N. In vitro investigation of the influence of printing direction on the flexural strength, flexural modulus and fractographic analysis of 3D-printed temporary materials. Dent. Mater. J. 2021, 40, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.C.; Lin, L.D.; Chuang, F.H.; Chan, C.P.; Wang, T.M.; Lee, J.J.; Jeng, P.-Y.; Tseng, W.-Y.; Lin, H.-J.; Jeng, J.-H. Carboxylesterase expression in human dental pulp cells: Role in regulation of BisGMA-induced prostanoid production and cytotoxicity. Acta Biomater. 2012, 8, 1380–1387. [Google Scholar] [CrossRef]
- Borella, P.S.; Alvares, L.A.S.; Ribeiro, M.T.H.; Moura, G.F.; Soares, C.J.; Zancopé, K.; Mendonça, G.; Rodrigues, F.P.; das Neves, F.D. Physical and mechanical properties of four 3D-printed resins at two different thick layers: An in vitro comparative study. Dent. Mater. 2023, 39, 686. [Google Scholar] [CrossRef]
- de Castro, E.F.; Nima, G.; Rueggeberg, F.A.; Giannini, M. Effect of build orientation in accuracy, flexural modulus, flexural strength, and microhardness of 3D-Printed resins for provisional restorations. J. Mech. Behav. Biomed. Mater. 2022, 136, 105479. [Google Scholar] [CrossRef]
- Oztürk, S.; Kaya, B.; Şenol, A.; Kahramanoğlu, E.; Atali, P.; Tarçin, B. Comparison Of Flexural Strength And Degree of Conversion of Novel Resin Composites Used in Clinical Practice. Clin. Dent. Res. 2024, 48, 116–124. Available online: https://scholar.google.com/scholar?hl=tr&as_sdt=0%2C5&q=38.%09Oztürk+S%3B+Kaya+B%3B+Şenol+A%3B+Kahramanoğlu+E%3B+Atali+P%3B+Tarçin+B.+Comparison+Of+Flexural+Strength+And+Degree+Of+Conversion+Of+Novel+Resin+Composites+Used+In+Clinical+Practice.+Clinical+Dentistry+And+Research.+2024%3B48%283%29%3A116-124.&btnG= (accessed on 25 January 2025).
- Daneshkazemi, A.R.; Davari, A.R.; Ataei, E.; Dastjerdi, F.; Hajighasemi, E. Effects of mechanical and thermal load cycling on micro tensile bond strength of clearfil SE bond to superficial dentin. Dent. Res. J. 2013, 10, 202–209. [Google Scholar] [CrossRef]


| 24 h | FS (MPa) Mean ± SD | FM (GPa) Mean ± SD | Deflection (mm) Mean ± SD |
|---|---|---|---|
| 3M Z250 | 147.6 + 16.5 | 4.94 ± 1.36 a | 1.07 ± 0.32 a |
| 90°—3D-printed | 150.7 ± 6.2 | 1.82 ± 0.15 b | 2.78 ± 0.30 b |
| 0°—3D-printed | 140.2 ± 11.8 | 1.80 ± 0.21 b | 2.63 ± 0.37 b |
| p value 1 | 0.125 | <0.001 | <0.001 |
| 10,000 cycles aged | FS (MPa) Mean ± SD | FM (GPa) Mean ± SD | Deflection (mm) Mean ± SD |
| 3M Z250 | 142.3 ± 18.88 a | 4.4 ± 1.45 a | 1.22 ± 0.526 a |
| 90°—3D-printed | 126.1 ± 6.56 b | 1.5 ± 0.16 b | 2.75 ± 0.371 a |
| 0°—3D-printed | 116.4 ± 10.13 b | 1.6 ± 0.12 b | 2.37 ± 0.329 b |
| p value 1 | <0.001 | <0.001 | <0.001 |
| 30,000 cycles aged | FS (MPa) Mean ± SD | FM (GPa) Mean ± SD | Deflection (mm) Mean ± SD |
| 3M Z250 | 115.0 ± 11.8 | 4.07 ± 0.532 a | 0.95 ± 0.13 a |
| 90°—3D-printed | 119.7 ± 9.24 | 1.87 ± 0.842 b | 2.38 ± 0.69 b |
| 0°—3D-printed | 109.4 ± 6.66 | 1.47 ± 0.151 b | 2.50 ± 0.37 b |
| p value 1 | 0.068 | <0.001 | <0.001 |
| 3M Z250 | FS (MPa) Mean ± SD | FM (GPa) Mean ± SD | Deflection (mm) Mean ± SD |
|---|---|---|---|
| 24 h | 147.6 ± 16.5 a | 4.94 ± 1.36 | 1.07 ± 0.315 |
| 10,000 cycles | 142.3 ± 18.9 a | 4.40 ± 1.45 | 1.22 ± 0.526 |
| 30,000 cycles | 115 ± 11.76 b | 4.07 ± 0.53 | 0.95 ± 0.133 |
| p value 1 | <0.001 | 0.274 | 0.266 |
| 90°—3D-printed | FS (MPa) Mean ± SD | FM (GPa) Mean ± SD | Deflection (mm) Mean ± SD |
| 24 h | 150.7 ± 6.2 a | 1.82 ± 0.15 | 2.78 ± 0.30 |
| 10,000 cycles | 126.1 ± 6.6 b | 1.55 ± 0.16 | 2.75 ± 0.37 |
| 30,000 cycles | 119.7 ± 9.2 b | 1.87 ± 0.84 | 2.38 ± 0.69 |
| p value 1 | <0.001 | 0.321 | 0.144 |
| 0°—3D-printed | FS (MPa) Mean ± SD | FM (GPa) Mean ± SD | Deflection (mm) Mean ± SD |
| 24 h | 140.2 ± 8.8 a | 1.80 ± 0.21 a | 2.63 ± 0.37 |
| 10,000 cycles | 116.4 ± 10.1 b | 1.65 ± 0.12 a | 2.37 ± 0.33 |
| 30,000 cycles | 109.4 ± 6.7 b | 1.47 ± 0.15 b | 2.50 ± 0.37 |
| p value 1 | <0.001 | <0.001 | 0.291 |
| Material | Manufacturer | Shade | Type | Composition | |
|---|---|---|---|---|---|
| Resin Matrix | Filler | ||||
| Filtek Z250 | 3M ESPE, Germany | A1 | Micro hybrid resin composite | BIS-GMA UDMA BIS-EMA | Zirconia/silica, 0.01–3.5 μm inorganic filler size and 60% filler ratio (volume). |
| Permanent 3D Printing Polymer Resin | Arma Dental, Türkiye | A1 | 3D-Printing Resin | TPO, UDMA, acrylic acid ester, bio-based aliphatic urethane acrylate aliphatic urethane methacrylate | 1% Organo-modified zirconium oxide (30 nm), 5.5% organo-modified silicone Oxide (50 nm) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Özden, Y.E.; Doğu Kaya, B.; Yılmaz Atalı, P.; Ozer, F.; Ozkurt Kayahan, Z. Effect of Print Orientation and Thermal Aging on the Flexural Strength of Zirconia-Reinforced Three-Dimensional-Printed Restorative Resin Materials. Molecules 2025, 30, 2337. https://doi.org/10.3390/molecules30112337
Özden YE, Doğu Kaya B, Yılmaz Atalı P, Ozer F, Ozkurt Kayahan Z. Effect of Print Orientation and Thermal Aging on the Flexural Strength of Zirconia-Reinforced Three-Dimensional-Printed Restorative Resin Materials. Molecules. 2025; 30(11):2337. https://doi.org/10.3390/molecules30112337
Chicago/Turabian StyleÖzden, Yunus Emre, Bengü Doğu Kaya, Pınar Yılmaz Atalı, Fusun Ozer, and Zeynep Ozkurt Kayahan. 2025. "Effect of Print Orientation and Thermal Aging on the Flexural Strength of Zirconia-Reinforced Three-Dimensional-Printed Restorative Resin Materials" Molecules 30, no. 11: 2337. https://doi.org/10.3390/molecules30112337
APA StyleÖzden, Y. E., Doğu Kaya, B., Yılmaz Atalı, P., Ozer, F., & Ozkurt Kayahan, Z. (2025). Effect of Print Orientation and Thermal Aging on the Flexural Strength of Zirconia-Reinforced Three-Dimensional-Printed Restorative Resin Materials. Molecules, 30(11), 2337. https://doi.org/10.3390/molecules30112337









