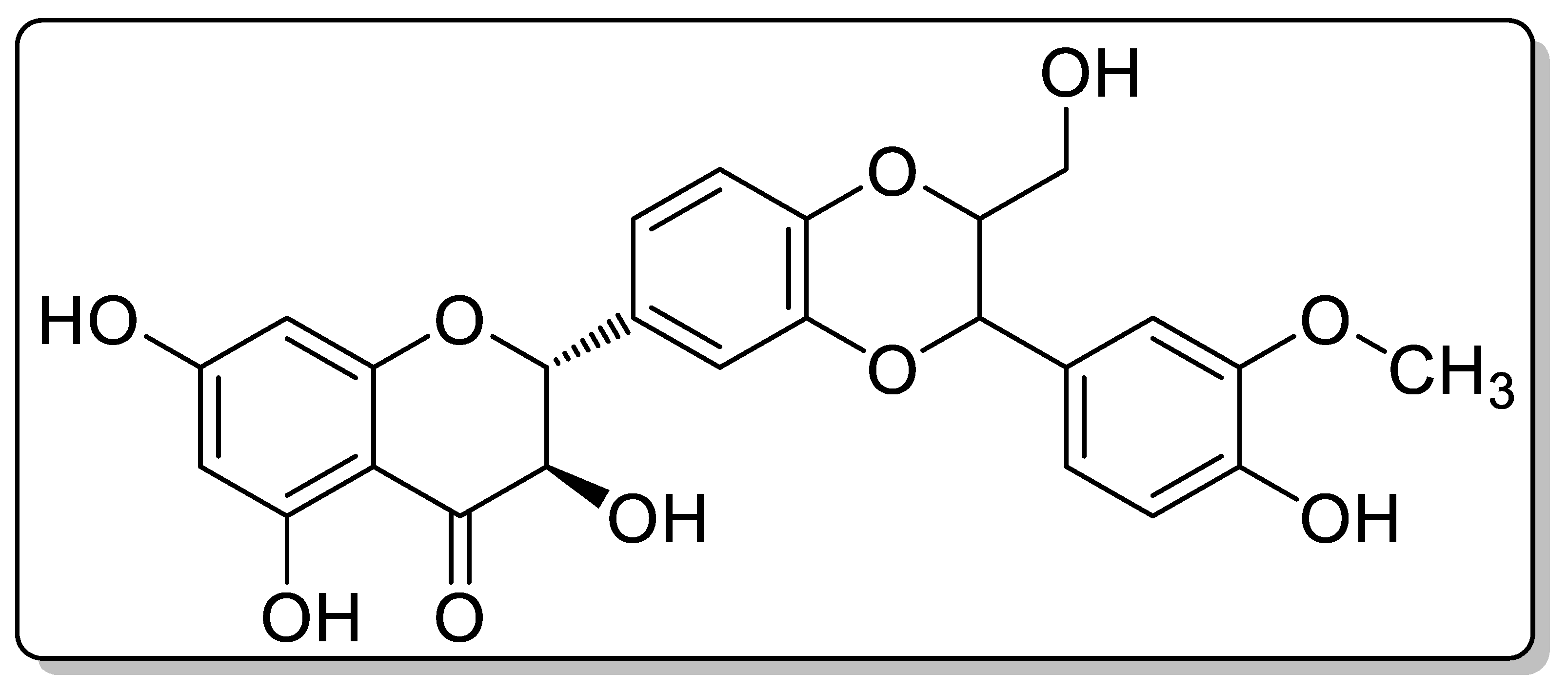
Preparation, Characterization and Evaluation of Flavonolignan Silymarin Effervescent Floating Matrix Tablets for Enhanced Oral Bioavailability
Abstract
1. Introduction
2. Results
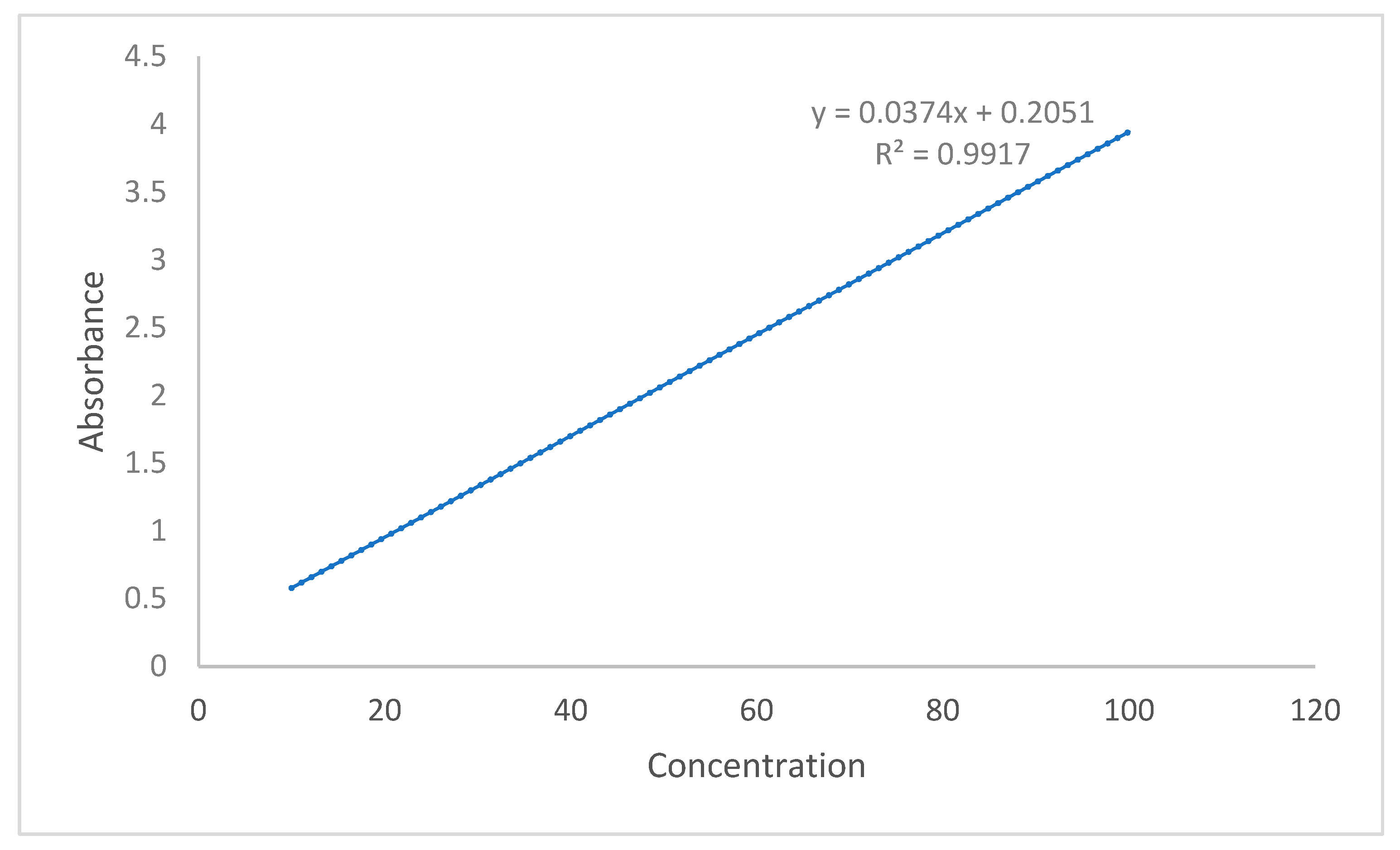
2.1. Pre-Compression Parameters
2.2. Post-Compression Parameters
2.3. Buoyancy Studies
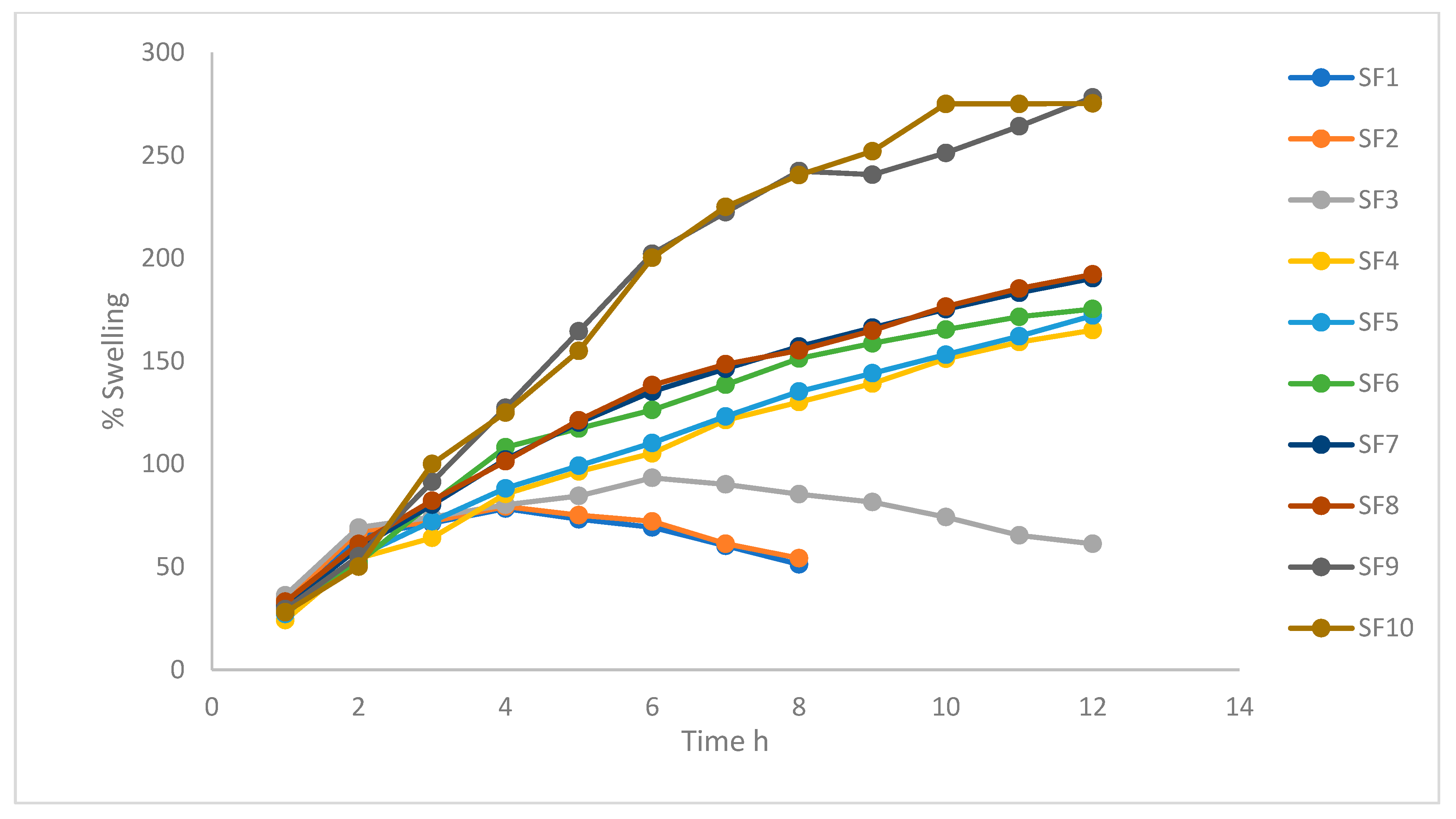
2.4. Swelling Index
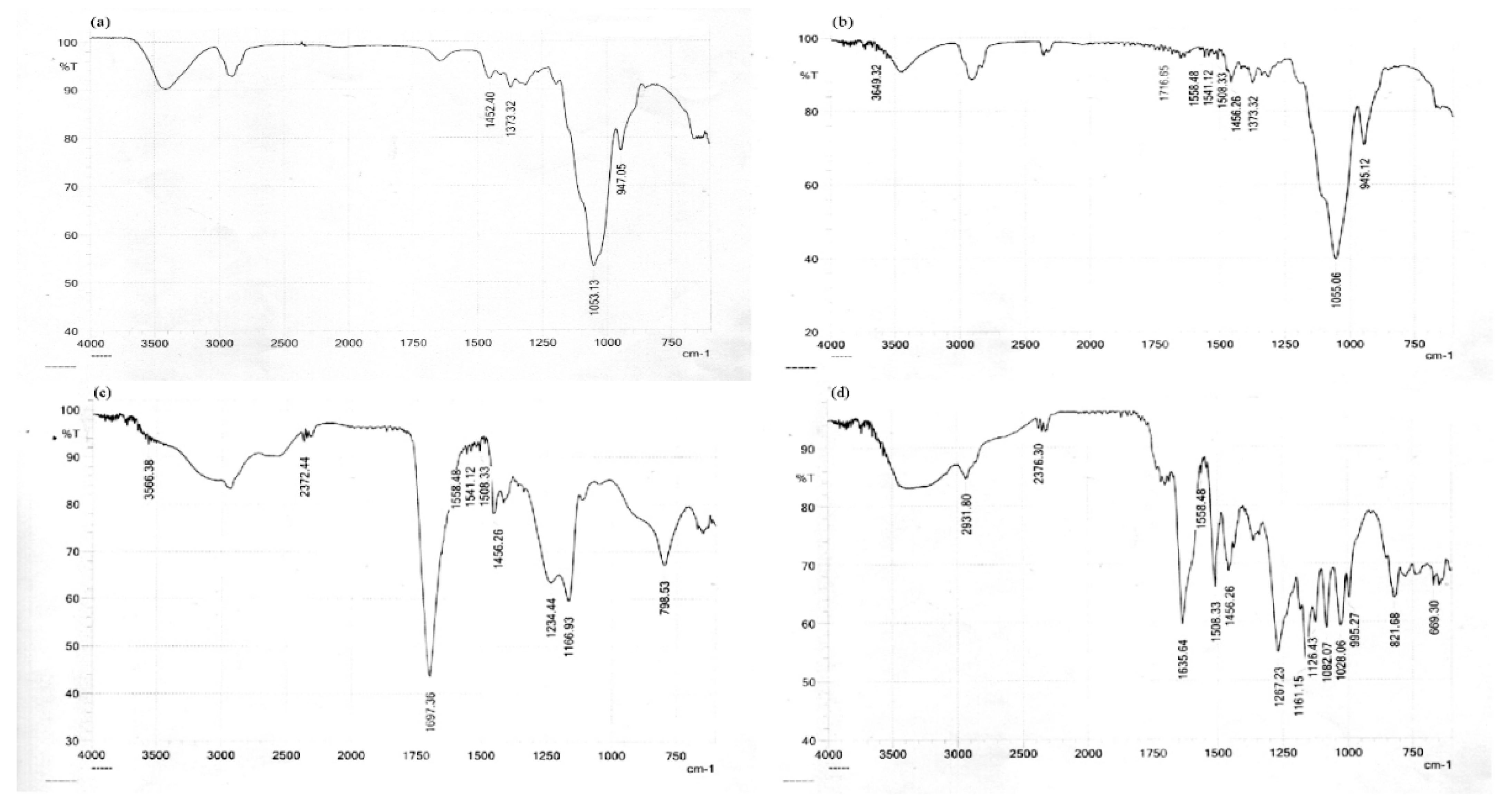
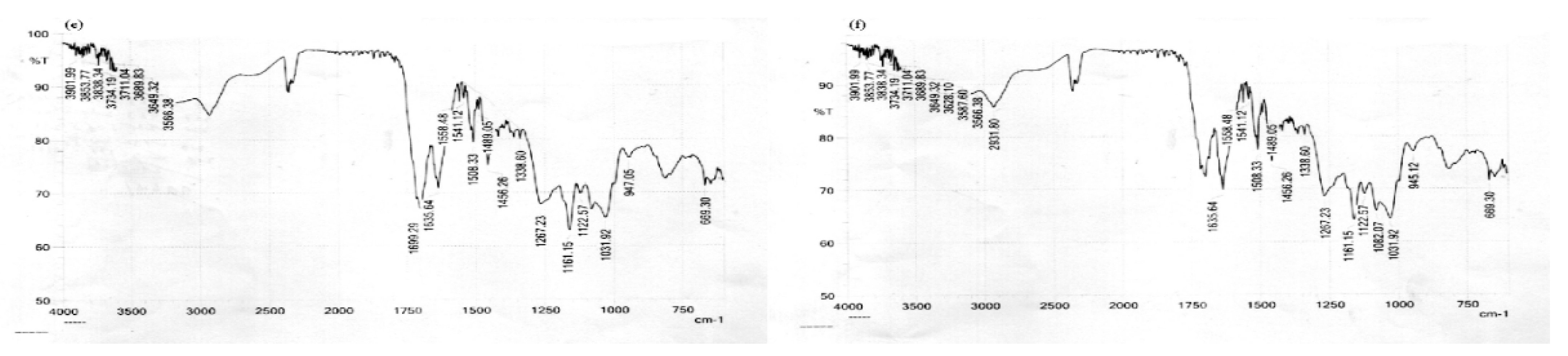
2.5. FTIR
2.6. Differential Scanning Calorimetry (DSC)
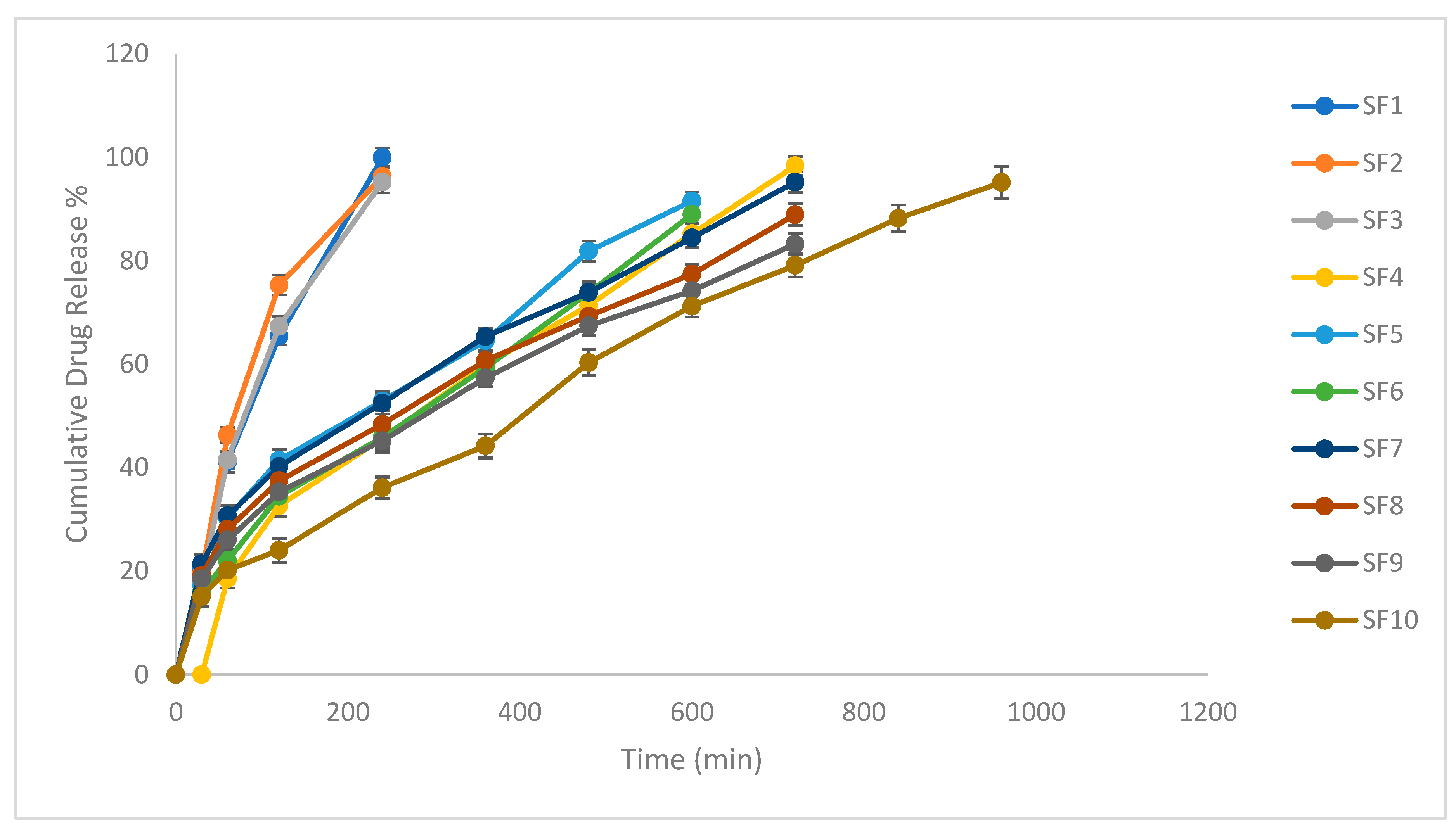
2.7. In Vitro Drug Release
2.8. In Vitro Release Kinetics
2.9. Ultrasonic Floating Behavior Study
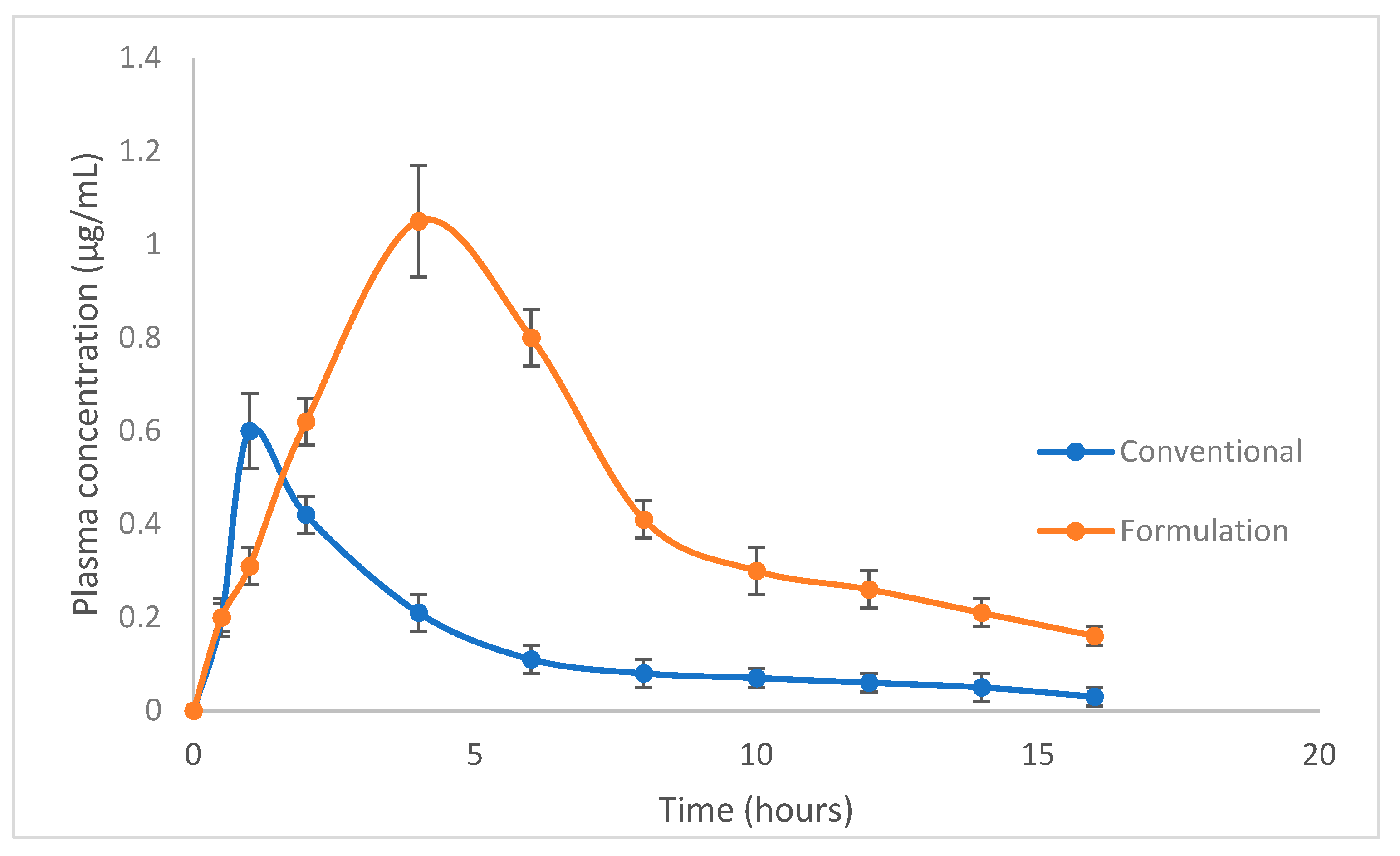
2.10. In Vivo Pharmacokinetic Studies
2.11. Stability Study
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Preparation of Floating Tablets of Silymarin
4.3. Pre-Compression Parameters
4.3.1. Fourier Transform Infrared Spectroscopy
4.3.2. Differential Scanning Calorimeter (DSC)
4.3.3. Micromeritics of the Powder Mixture
4.3.4. Angle of Repose
4.3.5. Bulk and Tapped Densities
4.3.6. Compressibility Index/Carr’s Index
4.3.7. Hausner Ratio
4.4. Post-Compression Parameters
4.4.1. Weight Variation Test
4.4.2. Content Uniformity
4.4.3. Diameter, Thickness and Hardness
4.4.4. Friability (F)
4.4.5. In Vitro Dissolution Study
4.5. Floating Tablet Specific Evaluation
4.5.1. Buoyancy Properties of the Tablets
4.5.2. Swelling Behavior of Tablets
4.5.3. Kinetic Analysis of the Release of the Drug
4.6. In Vivo Floating Behavior of the Silymarin Tablet
4.7. Study of the Pharmacokinetic Parameters of Silymarin
4.8. Pharmacokinetic Parameters
4.9. Stability Studies
4.10. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sornsuvit, C.; Hongwiset, D.; Yotsawimonwat, S.; Toonkum, M.; Thongsawat, S.; Taesotikul, W. The Bioavailability and Pharmacokinetics of Silymarin SMEDDS Formulation Study in Healthy Thai Volunteers. Evid. Based Complement. Altern. Med. 2018, 2018, 1507834. [Google Scholar] [CrossRef]
- Bijak, M. Silybin, a Major Bioactive Component of Milk Thistle (Silybum marianum L. Gaernt.)—Chemistry, Bioavailability, and Metabolism. Molecules 2017, 22, 1942. [Google Scholar] [CrossRef] [PubMed]
- Kesharwani, S.S.; Jain, V.; Dey, S.; Sharma, S.; Mallya, P.; Kumar, V.A. An overview of advanced formulation and nanotechnology-based approaches for solubility and bioavailability enhancement of silymarin. J. Drug Deliv. Sci. Technol. 2020, 60, 102021. [Google Scholar] [CrossRef]
- Hua, S. Advances in oral drug delivery for regional targeting in the gastrointestinal tract-influence of physiological, pathophysiologi-cal and pharmaceutical factors. Front. Pharmacol. 2020, 11, 524. [Google Scholar] [CrossRef] [PubMed]
- De Souza, M.P.C.; Sábio, R.M.; de Cassia Ribeiro, T.; dos Santos, A.M.; Meneguin, A.B.; Chorilli, M. Highlighting the impact of chitosan on the development of gastroretentive drug delivery systems. Int. J. Biol. Macromol. 2020, 159, 804–822. [Google Scholar] [CrossRef] [PubMed]
- Simons, F.J.; Wagner, K.G. Modeling, design and manufacture of innovative floating gastroretentive drug delivery systems based on hot-melt extruded tubes. Eur. J. Pharm. Biopharm. 2019, 137, 196–208. [Google Scholar] [CrossRef]
- Vrettos, N.-N.; Roberts, C.J.; Zhu, Z. Gastroretentive Technologies in Tandem with Controlled-Release Strategies: A Potent Answer to Oral Drug Bioavailability and Patient Compliance Implications. Pharmaceutics 2021, 13, 1591. [Google Scholar] [CrossRef]
- Zhang, P.; Shadambikar, G.; Almutairi, M.; Bandari, S.; Repka, M.A. Approaches for developing acyclovir gastro-retentive formulations using hot melt extrusion technology. J. Drug Deliv. Sci. Technol. 2020, 60, 102002. [Google Scholar] [CrossRef]
- Zhang, X.; Sun, X.; Lv, T.; Weng, L.; Chi, M.; Shi, J.; Zhang, S. Preparation of PI porous fiber membrane for recover-ing oil-paper insulation structure. Journal of materials science. Mater. Electron. 2020, 31, 13344–13351. [Google Scholar] [CrossRef]
- Reddy, P.; Manichandrika; Madhurima, K.; Fatima, N.; Aliya, A.; Siddiqui, K.; Begum, N. Formulation and evaluation of pantoprazole floating tablets. Int. J. Adv. Res. Med. Pharm. Sci. 2018, 3, 38. [Google Scholar] [CrossRef]
- Fang, D.; Pan, H.; Cui, M.; Qiao, S.; Li, X.; Wang, T.; Meng, Q.; Xu, L.; Pan, W. Fabrication of three-dimensional-printed ofloxacin gastric floating sustained-release tablets with different structures. J. Drug Deliv. Sci. Technol. 2022, 67, 102992. [Google Scholar] [CrossRef]
- Sinka, D.; Doma, E.; Szendi, N.; Páll, J.; Kósa, D.; Pető, Á.; Fehér, P.; Ujhelyi, Z.; Fenyvesi, F.; Váradi, J.; et al. Formulation, Characterization and Permeability Studies of Fenugreek (Trigonella foenum-graecum) Containing Self-Emulsifying Drug Delivery System (SEDDS). Molecules 2022, 27, 2846. [Google Scholar] [CrossRef]
- Rahamathulla, M.; Saisivam, S.; Gangadharappa, H. Development of valsartan floating matrix tablets using low density poly-propylene foam powder: In vitro and in vivo evaluation. AAPS PharmSciTech 2019, 20, 35. [Google Scholar] [CrossRef]
- Pawar, H.A.; Dhavale, R. Development and evaluation of gastroretentive floating tablets of an antidepressant drug by thermo-plastic granulation technique. Beni Suef Univ. J. Basic Appl. Sci. 2014, 3, 122–132. [Google Scholar]
- Diós, P.; Nagy, S.; Pál, S.; Pernecker, T.; Kocsis, B.; Budán, F.; Horváth, I.; Szigeti, K.; Bölcskei, K.; Máthé, D.; et al. Preformulation studies and optimization of sodium alginate based floating drug delivery system for eradication of Helicobacter pylori. Eur. J. Pharm. Biopharm. 2015, 96, 196–206. [Google Scholar] [CrossRef] [PubMed]
- Pawar, H.A.; Gharat, P.R.; Dhavale, R.V.; Joshi, P.R.; Rakshit, P.P. Development and Evaluation of Gastroretentive Floating Tablets of an Antihypertensive Drug Using Hydrogenated Cottonseed Oil. ISRN Pharm. 2013, 2013, 137238. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Li, J.; Xiao, M.; Wang, D.; Qu, Y.; Zou, L.; Zheng, C.; Zhang, J. Oral colon-targeted mucoadhesive micelles with enzyme-responsive controlled release of curcumin for ulcerative colitis therapy. Chin. Chem. Lett. 2022, 33, 4924–4929. [Google Scholar] [CrossRef]
- Essa, E.A.; Elkotb, F.E.; Eldin, E.E.Z.; El Maghraby, G.M. Development and evaluation of glibenclamide floating tablet with optimum release. J. Drug Deliv. Sci. Technol. 2015, 27, 28–36. [Google Scholar] [CrossRef]
- Zhou, M.; Tang, T.; Qin, D.; Cheng, H.; Wang, X.; Chen, J.; Wågberg, T.; Hu, G. Hematite nanoparticle decorated MIL-100 for the highly selective and sensitive electrochemical detection of trace-level paraquat in milk and honey. Sensors Actuators B: Chem. 2023, 376, 132931. [Google Scholar] [CrossRef]
- Shriram, R.G.; Moin, A.; Alotaibi, H.F.; Khafagy, E.S.; Al Saqr, A.; Abu Lila, A.S.; Charyulu, R.N. Phytosomes as a Plausible Nano-Delivery System for Enhanced Oral Bioavailability and Improved Hepatoprotective Activity of Silymarin. Pharmaceuticals 2022, 15, 790. [Google Scholar] [CrossRef]
- Sharma, A.; Puri, V.; Kakkar, V.; Singh, I. Formulation and Evaluation of Silymarin-Loaded Chitosan-Montmorilloite Microbeads for the Potential Treatment of Gastric Ulcers. J. Funct. Biomater. 2018, 9, 52. [Google Scholar] [CrossRef]
- Suhail, M.; Wu, P.-C.; Minhas, M. Using carbomer-based hydrogels for control the release rate of diclofenac sodium: Prepara-tion and in vitro evaluation. Pharmaceuticals 2020, 13, 399. [Google Scholar] [CrossRef]
- El-Masry, S.M.; Helmy, S.A. Hydrogel-based matrices for controlled drug delivery of etamsylate: Prediction of in-vivo plasma profiles. Saudi Pharm. J. 2020, 28, 1704–1718. [Google Scholar] [CrossRef]
- Madni, A.; Ekwal, M.; Ahmad, S.; Din, I.; Hussain, Z.; Muhammad Ranjha, N.; Imran Khan, M.; Akhlaq, M.; Ahmad Mahmood, M.; Zafar, H. FTIR Drug-Polymer Interactions Studies of Perindopril Erbumine. J. Chem. Soc. Pak. 2014, 36, 1064–1070. [Google Scholar]
- Pramod, K.; Suneesh, C.V.; Shanavas, S.; Ansari, S.H.; Ali, J. Unveiling the compatibility of eugenol with formulation excipients by systematic drug-excipient compatibility studies. J. Anal. Sci. Technol. 2015, 6, 34. [Google Scholar] [CrossRef]
- Narendar, D.; Arjun, N.; Someshwar, K.; Madhusudan Rao, Y. Quality by design approach for development and optimization of Quetiapine Fumarate effervescent floating ma-trix tablets for improved oral bioavailability. J. Pharm. Investig. 2016, 46, 253–263. [Google Scholar] [CrossRef]
- Aly, U.F.; Mansour, H.F. Novel Pharmaceutical gels containing glyccerihizic acid ammonium salt for chronic wounds. Br. J. Pharm. Res. 2014, 4, 654–668. [Google Scholar] [CrossRef]
- Chandak, A.R.; Verma, P.R.P. Design and Development of Hydroxypropyl Methycellulose (HPMC) Based Polymeric Films of Methotrexate: Physicochemical and Pharmacokinetic Evaluations. YAKUGAKU ZASSHI 2008, 128, 1057–1066. [Google Scholar] [CrossRef] [PubMed]
- Imran, M.; Shah, M.R.; Ullah, F.; Ullah, S.; Elhissi, A.M.; Nawaz, W.; Ahmad, F.; Sadiq, A.; Ali, I. Sugar-based novel niosomal nanocarrier system for enhanced oral bioavailability of levofloxacin. Drug Deliv. 2016, 23, 3653–3664. [Google Scholar] [CrossRef] [PubMed]
- Rahim, H.; Khan, M.A.; Sadiq, A.; Khan, S.; Chishti, K.A.; Rahman, I.U. Comparative studies of binding potential of Prunus armeniaca and Prunus domestica gums in tablets formulations. Pak. J. Pharm. Sci. 2015, 28, 909–915. [Google Scholar] [PubMed]
- El-Nahas, A.E.; Allam, A.N.; El-Kamel, A.H. Mucoadhesive buccal tablets containing silymarin Eudragit-loaded nanoparticles: Formulation, characterisation and ex vivo permeation. J. Microencapsul. 2017, 34, 463–474. [Google Scholar] [CrossRef]
- Rahim, H.; Sadiq, A.; Khan, S.; Chishti, K.A.; Amin, F.; Khan, M.A.; Abbas, S. Isolation and preliminary evaluation of Mulva Neglecta mucilage: A novel tablet binder. Pak. J. Pharm. Sci. 2016, 52, 201–210. [Google Scholar] [CrossRef]
- Sahibzada, M.U.; Sadiq, A.; Khan, S.; Faidah, H.S.; Naseemullah; Khurram, M.; Amin, M.U.; Haseeb, A. Fabrication, characterization and in vitro evaluation of silibinin nanoparticles: An attempt to enhance its oral bioavailability. Drug Des. Dev. Ther. 2017, 11, 1453–1464. [Google Scholar] [CrossRef] [PubMed]
- Riley, G.; Mann, S.; Jesse, R. Angles of repose of cohesive powders. J. Powder Bulk Solids Technol. 1978, 2, 15–18. [Google Scholar]
- Thalberg, K.; Lindholm, D.; Axelsson, A. Comparison of different flowability tests for powders for inhalation. Powder Technol. 2004, 146, 206–213. [Google Scholar] [CrossRef]
- Zhang, X.; Qu, Y.-Y.; Liu, L.; Qiao, Y.-N.; Geng, H.-R.; Lin, Y.; Xu, W.; Cao, J.; Zhao, J.-Y. Homocysteine inhibits pro-insulin receptor cleavage and causes insulin resistance via protein cysteine-homocysteinylation. Cell Rep. 2021, 37, 109821. [Google Scholar] [CrossRef]
- United States Pharmacopeia. General Chapters <1216> Tablet Friability. In 24) USPaNFUN; United States Pharmacopeia: Rockville, MD, USA, 2006. [Google Scholar]
- United States Pharmacopeia. General Chapters <905> Tablet Friability. In 33) USPaNFUN; United States Pharmacopeia: Rockville, MD, USA, 2011. [Google Scholar]
- Acharya, S.; Patra, S.; Pani, N.R. Optimization of HPMC and carbopol concentrations in non-effervescent floating tablet through factorial design. Carbohydr. Polym. 2014, 102, 360–368. [Google Scholar] [CrossRef]
- Raza, A.; Bukhari, N.I.; Karim, S.; Hafiz, M.A.; Hayat, U. Floating tablets of minocycline hydrochloride: Formulation, in-vitro evaluation and optimization. Futur. J. Pharm. Sci. 2017, 3, 131–139. [Google Scholar] [CrossRef]
- Davoudi, E.T.; Noordin, M.I.; Kadivar, A.; Kamalidehghan, B.; Farjam, A.S.; Javar, H.A. Preparation and Characterization of a Gastric Floating Dosage Form of Capecitabine. BioMed. Res. Int. 2013, 2013, 495319. [Google Scholar] [CrossRef]
- Irfan, M.; Akram, A.; Zahoor, A.F.; Qadir, M.I.; Hussain, A.; Abbas, N.; Khan, A.; Arshad, M.S.; Khan, N.I. Formulation parameters affecting floating behaviour and drug release from extended release floating tablets of ranitidine hydrochloride. Lat. Am. J. Pharm. 2016, 35 (Suppl. S1), 1206–1216. [Google Scholar]
- Saab, M.; Samy, W.; Issa, M.; El-Maradny, H. Design and preparation of controlled floating gastroretentive delivery systems for enhanced fexofenadine hydrochlo-ride oral bioavailability. Trop. J. Pharm. Res. 2018, 17, 569–576. [Google Scholar] [CrossRef]
- Sun, S.J.; Deng, P.; Peng, C.E.; Ji, H.Y.; Mao, L.F.; Peng, L.Z. Extraction, Structure and Immunoregulatory Activ-ity of Low Molecular Weight Polysaccharide from Dendrobium officinale. Polymers 2022, 14, 2899. [Google Scholar] [CrossRef]
- Rahim, H.; Sadiq, A.; Khan, S.; Khan, M.A.; Shah, S.M.; Hussain, Z.; Ullah, R.; Shahat, A.A.; Ibrahim, K. Aceclofenac nanocrystals with enhanced in vitro, in vivo performance: Formulation optimization, characterization, analgesic and acute toxicity studies. Drug Des. Dev. Ther. 2017, 2017, 2443–2452. [Google Scholar] [CrossRef]
- Ju, R.T.; NixoN, P.R.; Patel, M.V.; Tong, D.M. Drug Release from Hydrophilic Matrices. 2. A Mathematical Model Based on the Polymer Disentanglement Concentration and the Diffusion Layer. J. Pharm. Sci. 1995, 84, 1464–1477. [Google Scholar] [CrossRef]
- Thulluru, A.; Basha, S.S.; Rao, C.B.; Kumar, C.S.P.; Mahammed, N.; Kumar, K.S. Optimization of HPMC K100M and Sodium Alginate Ratio in Metronidazole Floating Tablets for the Effective Eradication of Helicobacter pylori. Asian J. Pharm. Technol. 2019, 9, 195–203. [Google Scholar] [CrossRef]
- Zeng, Q.; Bie, B.; Guo, Q.; Yuan, Y.; Han, Q.; Han, X.; Chen, M.; Zhang, X.; Yang, Y.; Liu, M.; et al. Hyperpolarized Xe NMR signal advancement by metal-organic framework entrapment in aqueous solution. Proc. Natl. Acad. Sci. USA 2020, 117, 17558–17563. [Google Scholar] [CrossRef]
- Tewari, D.; Durig, T. CusTomizing HPmC to minimize Drug VAriABiliTy. Pharm. Technol. 2016, 40, 24–29. [Google Scholar]
- Hiremath, P.S.; Saha, R.N. Controlled Release Hydrophilic Matrix Tablet Formulations of Isoniazid: Design and In Vitro Studies. AAPS PharmSciTech 2008, 9, 1171–1178. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Chen, H.; Rui, Y.; Yang, F.; Ma, N.; Wu, Z. Floating tablets for controlled release of ofloxacin via compression coating of hydroxypropyl cellulose combined with effervescent agent. Int. J. Pharm. 2015, 489, 210–217. [Google Scholar] [CrossRef]
- Lin, Z.; Zhou, D.; Hoag, S.; Qiu, Y. Influence of Drug Properties and Formulation on In Vitro Drug Release and Biowaiver Regulation of Oral Extended Release Dosage Forms. AAPS J. 2016, 18, 333–345. [Google Scholar] [CrossRef]
- Ramadan, A.A.; Elbakry, A.M.; Sarhan, H.A.; Ali, S.H. Silymarin loaded floating polymer (s) microspheres: Characterization, in-vitro/in-vivo evaluation. Pharm Dev Technol. 2020, 25, 1081–1089. [Google Scholar] [CrossRef] [PubMed]
- Chang, L.-W.; Hou, M.-L.; Tsai, T.-H. Silymarin in Liposomes and Ethosomes: Pharmacokinetics and Tissue Distribution in Free-Moving Rats by High-Performance Liquid Chromatography–Tandem Mass Spectrometry. J. Agric. Food Chem. 2014, 62, 11657–11665. [Google Scholar] [CrossRef] [PubMed]
- Tadros, M.I. Controlled-release effervescent floating matrix tablets of ciprofloxacin hydrochloride: Development, optimization and in vitro–in vivo evaluation in healthy human volunteers. Eur. J. Pharm. Biopharm. 2010, 74, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Devi, P.; Rathor, S.; Sharma, P.; Sen, J.; Kaur, H.; Singh, J. Development of novel gastroretentive salbutamol sulfate-loaded sodium alginate-pectin bubble beads prepared by co-axial needle air-injection method and in vivo clinical evaluation by ultrasound studies. Eur. J. Pharm. Sci. 2018, 122, 359–373. [Google Scholar] [CrossRef]




| Formulation | Angle of Repose | Bulk Density (g/mL) | Tapped Density (g/mL) | Carr’s Index (%) | Hausner Ratio |
|---|---|---|---|---|---|
| SF1 | 25 | 0.48 | 0.53 | 10 | 1.11 |
| SF2 | 27 | 0.50 | 0.52 | 11 | 1.12 |
| SF3 | 26 | 0.47 | 0.51 | 09 | 1.11 |
| SF4 | 26 | 0.49 | 0.53 | 09 | 1.10 |
| SF5 | 25 | 0.50 | 0.59 | 10 | 1.10 |
| SF6 | 25 | 0.50 | 0.52 | 10 | 1.10 |
| SF7 | 24 | 0.49 | 0.55 | 10 | 1.10 |
| SF8 | 26 | 0.48 | 0.58 | 10 | 1.11 |
| SF9 | 25 | 0.48 | 0.54 | 11 | 1.11 |
| SF10 | 26 | 0.45 | 0.55 | 12 | 1.14 |
| Formulation | Thickness (mm) | Diameter (mm) | Hardness (N) | Friability (%) | Weight Variation (mg) | Content Uniformity (%) |
|---|---|---|---|---|---|---|
| SF1 | 3.14 | 12 | 48 | 0.32 | 530 | 99.1 |
| SF2 | 3.20 | 12 | 49 | 0.34 | 531 | 98.8 |
| SF3 | 3.19 | 12 | 50 | 0.33 | 529 | 100 |
| SF4 | 3.21 | 12 | 47 | 0.31 | 530 | 98.4 |
| SF5 | 3.26 | 12 | 49 | 0.34 | 532 | 99.2 |
| SF6 | 3.25 | 12 | 45 | 0.30 | 531 | 98.5 |
| SF7 | 3.24 | 12 | 46 | 0.35 | 530 | 99.2 |
| SF8 | 3.22 | 12 | 44 | 0.38 | 528 | 98.7 |
| SF9 | 3.31 | 12 | 45 | 0.37 | 527 | 99.0 |
| SF10 | 3.78 | 12 | 52 | 0.27 | 530 | 99.0 |
| Formulation | Floating Time (Lag) (s) | Floating Time (Total) (h) |
|---|---|---|
| SF1 | 34 | 6 |
| SF2 | 42 | 6 |
| SF3 | 58 | 6 |
| SF4 | 70 | 12 |
| SF5 | 95 | 12 |
| SF6 | 120 | 12 |
| SF7 | 50 | 12 |
| SF8 | 67 | 12 |
| SF9 | 80 | 12 |
| SF10 | 60 | >12 |
| Formulation | First-Order | Zero-Order | Higuchi Model | Korsmayer–Peppas | |
|---|---|---|---|---|---|
| r2 | r2 | r2 | r2 | n | |
| SF10 | 0.587 | 0.979 | 0.977 | 0.986 | 0.65 |
| Parameters | Dose | Tmax | Cmax | AUC0-t | MRT |
|---|---|---|---|---|---|
| mg/kg | h | µg/mL | µg·h/mL | h | |
| Reference | 200 | 1.0 ± 0.08 | 0.6 ± 0.11 | 2.4 ± 0.70 | 5.3 ± 0.91 |
| Formulation | 200 | 4.0 ± 0.12 | 1.1 ± 0.42 | 7.5 ± 1.26 | 8.6 ± 1.15 |
| Stability Conditions | Sampling Interval (Months) | Physical Appearance | Drug Content (%) |
|---|---|---|---|
| 25 ± 2 °C, 60 ± 5% RH | Start | Good | 100.2 ± 0.05 |
| Three | Good | 99.86 ± 0.07 | |
| Six | Good | 99.52 ± 0.08 | |
| Twelve | Good | 99.21 ± 0.12 | |
| 30 ± 2 °C, 65 ± 5% RH | Start | Good | 100.04 ± 0.03 |
| Three | Good | 99.94 ± 0.04 | |
| Six | Good | 99.65 ± 0.06 | |
| Twelve | Good | 99.36 ± 0.09 | |
| 40 ± 2 °C, 75 ± 5% RH | Start | Good | 100.06 ± 0.07 |
| Three | Good | 99.15 ± 0.14 | |
| Six | Good | 98.86 ± 0.15 |
| Ingredients in mg | Formulation Code | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SF1 | SF2 | SF3 | SF4 | SF5 | SF6 | SF7 | SF8 | SF9 | SF10 | |
| Drug | 200 | 200 | 200 | 200 | 200 | 200 | 200 | 200 | 200 | 200 |
| HPMCK4 | 100 | 150 | 200 | - | - | - | 100 | 100 | 100 | 100 |
| HPMCK15 | - | - | - | 80 | 100 | 120 | 80 | 100 | 120 | 120 |
| Carbopol 934p | - | - | - | - | - | - | - | - | - | 25 |
| NaHCO3 | 70 | 70 | 70 | 70 | 70 | 70 | 70 | 70 | 70 | 70 |
| Magnesium stearate | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 |
| Citric acid | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmad, S.; Khan, J.A.; Kausar, T.N.; Mahnashi, M.H.; Alasiri, A.; Alqahtani, A.A.; Alqahtani, T.S.; Walbi, I.A.; Alshehri, O.M.; Elnoubi, O.A.; et al. Preparation, Characterization and Evaluation of Flavonolignan Silymarin Effervescent Floating Matrix Tablets for Enhanced Oral Bioavailability. Molecules 2023, 28, 2606. https://doi.org/10.3390/molecules28062606
Ahmad S, Khan JA, Kausar TN, Mahnashi MH, Alasiri A, Alqahtani AA, Alqahtani TS, Walbi IA, Alshehri OM, Elnoubi OA, et al. Preparation, Characterization and Evaluation of Flavonolignan Silymarin Effervescent Floating Matrix Tablets for Enhanced Oral Bioavailability. Molecules. 2023; 28(6):2606. https://doi.org/10.3390/molecules28062606
Chicago/Turabian StyleAhmad, Sher, Jamshaid Ali Khan, Tabassum Naheed Kausar, Mater H. Mahnashi, Ali Alasiri, Abdulsalam A. Alqahtani, Thamer S. Alqahtani, Ismail A. Walbi, Osama M. Alshehri, Osman A. Elnoubi, and et al. 2023. "Preparation, Characterization and Evaluation of Flavonolignan Silymarin Effervescent Floating Matrix Tablets for Enhanced Oral Bioavailability" Molecules 28, no. 6: 2606. https://doi.org/10.3390/molecules28062606
APA StyleAhmad, S., Khan, J. A., Kausar, T. N., Mahnashi, M. H., Alasiri, A., Alqahtani, A. A., Alqahtani, T. S., Walbi, I. A., Alshehri, O. M., Elnoubi, O. A., Mahmood, F., & Sadiq, A. (2023). Preparation, Characterization and Evaluation of Flavonolignan Silymarin Effervescent Floating Matrix Tablets for Enhanced Oral Bioavailability. Molecules, 28(6), 2606. https://doi.org/10.3390/molecules28062606





