Identification of Marker Compounds and In Vitro Toxicity Evaluation of Two Portuguese Asphodelus Leaf Extracts
Abstract
1. Introduction
2. Results and Discussion
2.1. Drug-Extract Ratio
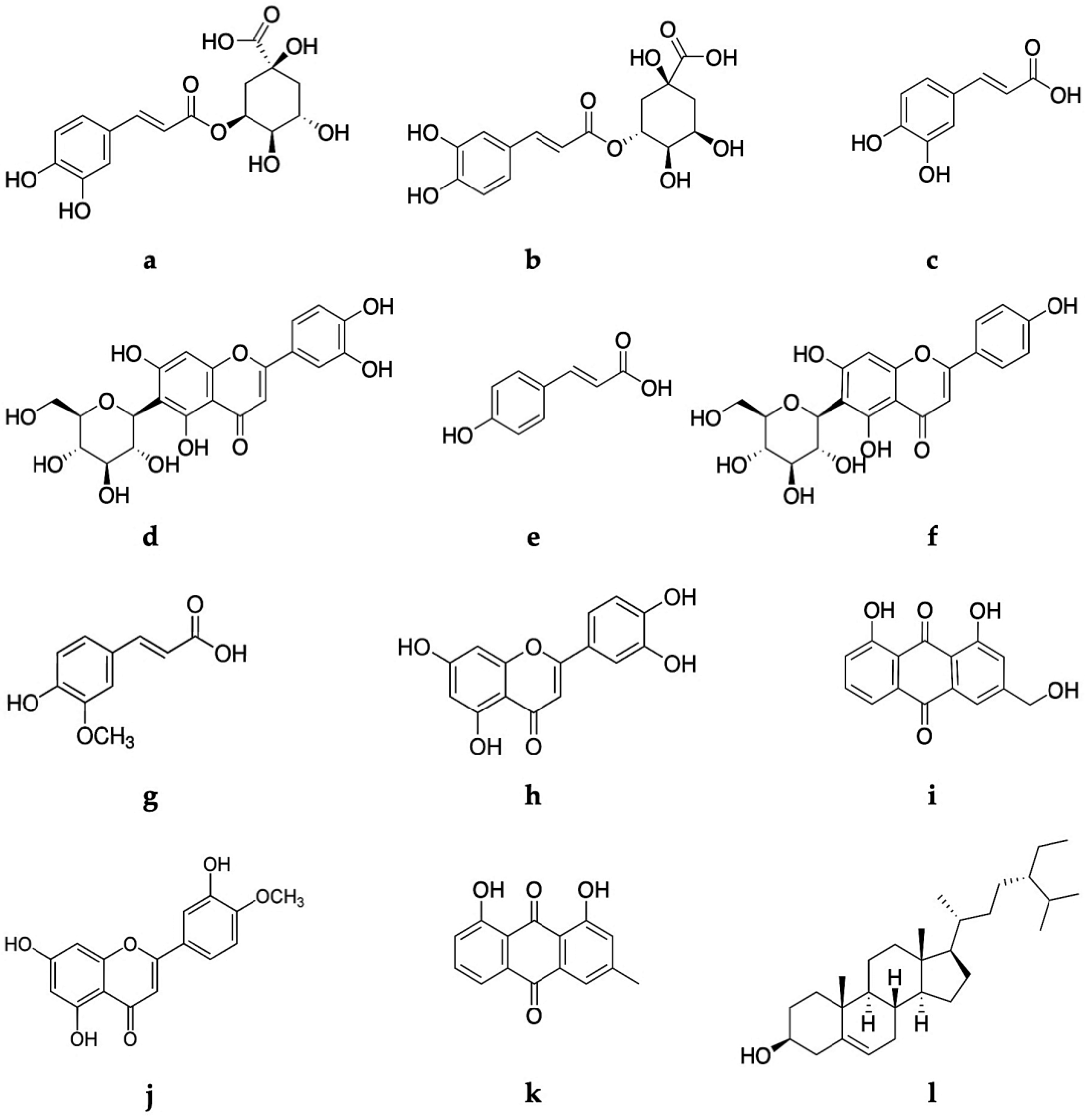
2.2. Phytochemical Analysis
2.3. Determination of In Vitro Antioxidant Potential
2.4. Assessment of the Antibacterial Potential
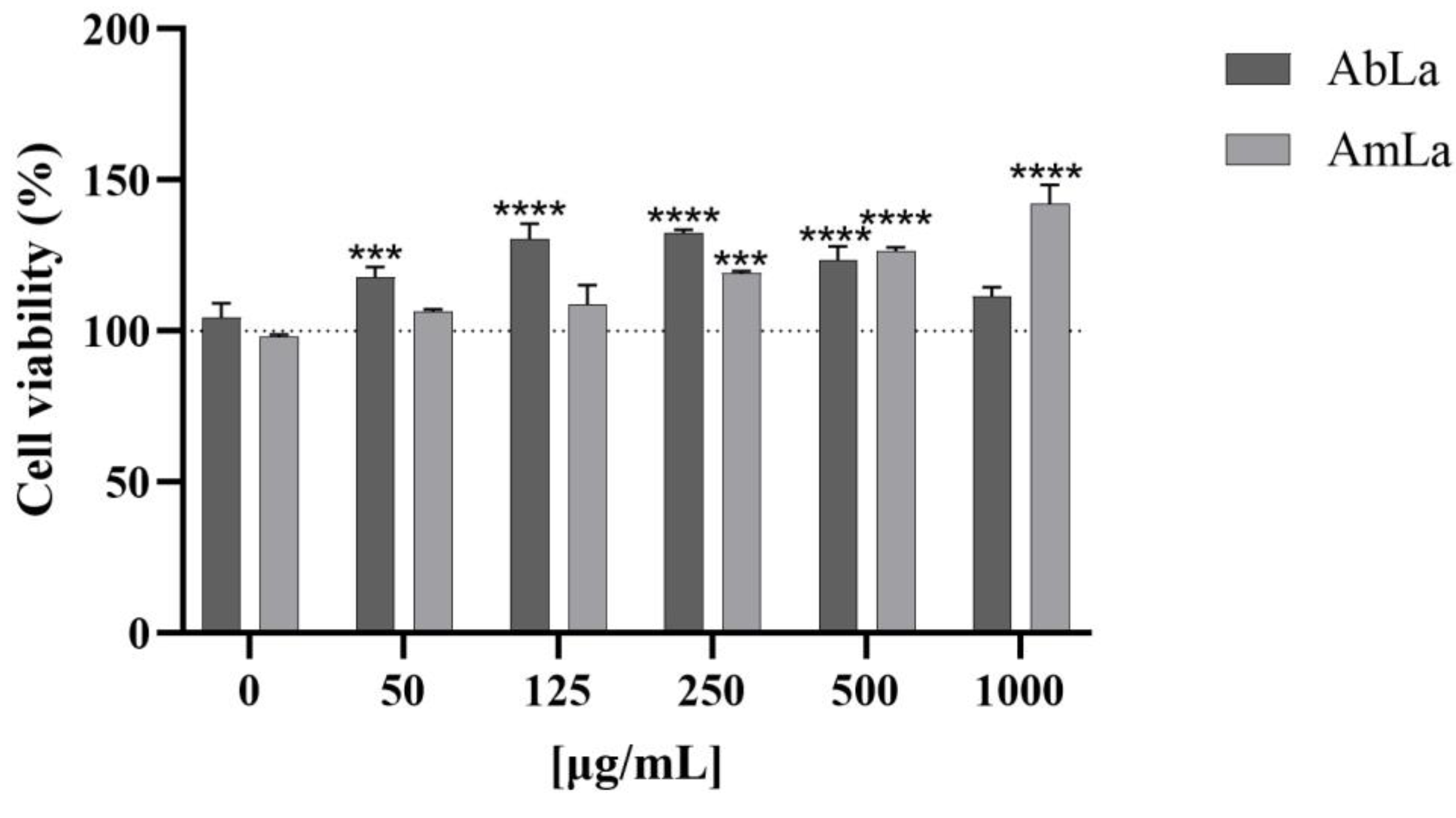
2.5. Pre-Clinical Safety Assessment
3. Materials and Methods
3.1. Chemical and Biological Reagents
3.2. Plant Materials
3.3. Preparation of Extract
3.4. Chromatographic Conditions
3.5. Quantification Assays for Determination of the Main Classes of Secondary Metabolites
3.6. In Vitro Antimicrobial Activity
3.7. In Vitro Antioxidant Activity
3.8. In Vitro Genotoxicity/Mutagenicity Evaluation by Ames Test
3.9. In Vitro Cytotoxicity Evaluation by MTT Assay
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Sivakumar, D.; Chen, L.; Sultanbawa, Y. A Comprehensive Review on Beneficial Dietary Phytochemicals in Common Traditional Southern African Leafy Vegetables. Food Sci. Nutr. 2018, 6, 714–727. [Google Scholar] [CrossRef] [PubMed]
- Peksel, A.; Imamoglu, S.; Altas Kiymaz, N.; Orhan, N. Antioxidant and Radical Scavenging Activities of Asphodelus Aestivus Brot. Extracts. Int. J. Food Prop. 2013, 16, 1339–1350. [Google Scholar] [CrossRef]
- Paura, B.; Di Marzio, P. Making a Virtue of Necessity: The Use of Wild Edible Plant Species (Also Toxic) in Bread Making in Times of Famine According to Giovanni Targioni Tozzetti (1766). Biology 2022, 11, 285. [Google Scholar] [CrossRef] [PubMed]
- Malmir, M.; Serrano, R.; Caniça, M.; Silva-Lima, B.; Silva, O. A Comprehensive Review on the Medicinal Plants from the Genus Asphodelus. Plants 2018, 7, 20. [Google Scholar] [CrossRef]
- Díaz Linfante, Z. Asphodelus L. In Flora Iberica; Talavera, S., Andrés, C., Arista, M., Piedra, M.P.F., Rico, E., Crespo, M.B., Quintanar, A., Herrero, A., Aedo, C., Eds.; Real Jardin Botänico, Consejo Superior de Investigaciones Científicas C.S.I.C.: Madrid, Spain, 2013; ISBN 276-308-152. [Google Scholar]
- Hammouda, F.M.; Rizk, A.M.; Ghaleb, H.; Abdel-Gawad, M.M. Chemical and Pharmacological Studies of Asphodelus microcarpus. Planta Med. 1972, 22, 188–195. [Google Scholar] [CrossRef]
- Di Petrillo, A.; Fais, A.; Pintus, F.; Santos-Buelga, C.; González-Paramás, A.M.; Piras, V.; Orrù, G.; Mameli, A.; Tramontano, E.; Frau, A. Broad-Range Potential of Asphodelus microcarpus Leaves Extract for Drug Development. BMC Microbiol. 2017, 17, 159. [Google Scholar] [CrossRef]
- Çalış, I.; Birincioǧlu, S.S.; Kırmızıbekmez, H.; Pfeiffer, B.; Heilmann, J. Secondary Metabolites from Asphodelus aestivus. Z. Für Naturforsch. B 2006, 61, 1304–1310. [Google Scholar] [CrossRef]
- Faidi, K.; Hammami, S.; Ben Salem, A.; El Mokni, R.; Garrab, M.; Mastouri, M.; Gorcii, M.; Trabelsi Ayedi, M.; Taglialatela-Scafati, O.; Mighri, Z. Polyphenol Derivatives from Bioactive Butanol Phase of the Tunisian Narrow-Leaved Asphodel (Asphodelus Tenuifolius Cav., Asphodelaceae). J. Med. Plants Res. 2014, 8, 550–557. [Google Scholar] [CrossRef]
- Raynaud Par, J.; Abdel-Gawad, M.M. Contribution à l’étude Chimiotaxinomique Du Genre Asphodelus (Liliaceae); Lyon Linnéenne Society: Lyon, France, 1974. [Google Scholar]
- Reynaud, J.; Flament, M.M.; Lussignol, M.; Becchi, M. Flavonoid Content of Asphodelus ramosus (Liliaceae). Can. J. Bot. 1997, 75, 2105–2107. [Google Scholar] [CrossRef]
- Williams, C.A. Biosystematics of the Monocotyledoneae—Flavonoid Patterns in Leaves of the Liliaceae. Biochem. Syst. Ecol. 1975, 3, 229–244. [Google Scholar] [CrossRef]
- Van Rheede van Oudtshoorn, M.C.B. Chemotaxonomic Investigations in Asphodeleae and Aloineae (Liliaceae). Phytochemistry 1964, 3, 383–390. [Google Scholar] [CrossRef]
- Hammouda, F.M.; Rizk, A.M.; El-Nasr, M.M.S.; Asr, E.-N. Anthraquinones of Certain Egyptian Asphodelus Species. Z. Für Naturforsch. C 1974, 29, 351–354. [Google Scholar] [CrossRef]
- El-Ghaly, E.-S. Phytochemical and Biological Activities of Asphodelus Microcarpus Leaves. J. Pharmacogn. Phytochem. 2017, 6, 259–264. [Google Scholar]
- Abd El-Fattah, H. Chemistry of Asphodelus fistulosus. Int. J. Pharmacogn. 1997, 35, 274–277. [Google Scholar] [CrossRef]
- Al-Kayali, R.; Kitaz, A.; Haroun, M. Antibacterial Activity of Asphodelin lutea and Asphodelus microcarpus Against Methicillin Resistant Staphylococcus aureus Isolates. Int. J. Pharmacogn. Phytochem. Res. 2016, 8, 1964–1968. [Google Scholar]
- Vaghasiya, Y.; Chanda, S.V. Screening of Methanol and Acetone Extracts of Fourteen Indian Medicinal Plants for Antimicrobial Activity. Turk. J. Biol. 2007, 31, 243–248. [Google Scholar]
- Peksel, A. Evaluation of Antioxidant and Antifungal Potential of Asphodelus aestivus Brot. Growing in Turkey. J. Med. Plants Res. 2012, 6, 253–265. [Google Scholar] [CrossRef]
- Ali-Shtayeh, M.S.; Abu Ghdeib, S.I. Antifungal Activity of Plant Extracts against Dermatophytes. Mycoses 1999, 42, 665–672. [Google Scholar] [CrossRef]
- Di Petrillo, A.; González-Paramás, A.M.; Era, B.; Medda, R.; Pintus, F.; Santos-Buelga, C.; Fais, A. Tyrosinase Inhibition and Antioxidant Properties of Asphodelus microcarpus Extracts. BMC Complement. Altern. Med. 2016, 16, 453. [Google Scholar] [CrossRef]
- Al-Laith, A.A.; Alkhuzai, J.; Freije, A. Assessment of Antioxidant Activities of Three Wild Medicinal Plants from Bahrain. Arab. J. Chem. 2019, 12, 2365–2371. [Google Scholar] [CrossRef]
- Mayouf, N.; Charef, N.; Saoudi, S.; Baghiani, A.; Khennouf, S.; Arrar, L. Antioxidant and Anti-Inflammatory Effect of Asphodelus microcarpus Methanolic Extracts. J. Ethnopharmacol. 2019, 239, 111914. [Google Scholar] [CrossRef] [PubMed]
- Al Groshi, A.; Nahar, L.; Andrew, E.; Auzi, A.; Sarker, S.D.; Ismail, F.M.D. Cytotoxicity of Asphodelus aestivus against Two Human Cancer Cell Lines. Nat. Prod. Chem. Res. 2017, 5, 61. [Google Scholar]
- Malmir, M.; Serrano, R.; Lima, K.; Duarte, M.P.; Moreira da Silva, I.; Silva Lima, B.; Caniça, M.; Silva, O. Monographic Quality Parameters and Genotoxicity Assessment of Asphodelus Bento-Rainhae and Asphodelus Macrocarpus Root Tubers as Herbal Medicines. Plants 2022, 11, 3173. [Google Scholar] [CrossRef] [PubMed]
- Kitaz, A. Comparison of the Total Phenol, Flavonoid Contents and Antioxidant Activity of Methanolic Roots Extracts of Asphodelus microcarpus and Asphodeline lutea Growing in Syria. Int. J. Pharmacogn. Phytochem. Res. 2017, 9, 159–164. [Google Scholar] [CrossRef]
- Chimona, C.; Karioti, A.; Skaltsa, H.; Rhizopoulou, S. Occurrence of Secondary Metabolites in Tepals of Asphodelus Ramosus L. Plant Biosyst.-Int. J. Deal. All Asp. Plant Biol. 2013, 148, 31–34. [Google Scholar] [CrossRef]
- Abdel-Gawad, M.M.; Hasan, A.; Raynaud Par, J. Estude de l’insaponifiable et Des Acides Gras Des Tuberculus d’ Asphodelus albus. Fitoterapia 1976, 47, 111–112. [Google Scholar]
- Rizk, A.M.; Hammouda, F.M. Phytochemical Studies of Asphodelus microcarpus (Lipids and Carbohydrates). Planta Med. 1970, 18, 168–172. [Google Scholar] [CrossRef]
- Abdel-Mogib, M.; Basaif, S. Two New Naphthalene and Anthraquinone Derivatives from Asphodelus tenuifolius. Pharmazie 2002, 57, 286–287. [Google Scholar]
- Fell, K.R.; Hammouda, F.M.; Rizk, A.M. The Constituents of the Seeds of Asphodelus microcarpus Viviani and A. Fistulosus L. J. Pharm. Pharmacol. 1968, 20, 646–649. [Google Scholar] [CrossRef]
- Apaydin, E.; Arabaci, G. Antioxidant Capacity and Phenolic Compounds with HPLC of Asphodelus Ramosus and Comparison of the Results with Allium Cepa L. and Allium Porrum L. Extracts. Turk. J. Agric. Nat. Sci. 2017, 4, 499–505. [Google Scholar]
- Eddine, L.S.; Segni, L.R.O. In Vitro Assays of the Antibacterial and Antioxidant Properties of Extracts from Asphodelus tenuifolius Cav and Its Main Constituents: A Comparative Study. Int. J. Pharm. Clin. Res. 2015, 7, 119–125. [Google Scholar]
- Malmir, M.; Serrano, R.; Silva, O. Anthraquinones as Potential Antimicrobial Agents—A Review. In Antimicrobial Research: Novel Bioknowledge and Educational Programs; Mendez-Vilas, A., Ed.; Formatex: Badajoz, Spain, 2017; pp. 55–61. [Google Scholar]
- Li, T.; Lu, Y.; Zhang, H.; Wang, L.; Beier, R.C.; Jin, Y.; Wang, W.; Li, H.; Hou, X. Antibacterial Activity and Membrane-Targeting Mechanism of Aloe-Emodin Against Staphylococcus epidermidis. Front. Microbiol. 2021, 12, 621866. [Google Scholar] [CrossRef]
- Oskay, M.; Aktaş, K.; Sari, D.; Azeri, C. A Comparative Study of Antimicrobial Activity Using Well and Disk Diffusion Method on Asphodelus aestivus (Liliaceae). Ekoloji 2007, 16, 62–65. [Google Scholar]
- Al-Qudah, M.M.A. Antibacterial Effect of Asphodelus Fistulosus Aqueous and Ethanolic Crude Extracts on Gram Positive and Gram-Negative Bacteria. Braz. J. Biol. 2022, 84, 1–9. [Google Scholar] [CrossRef]
- Khalfaoui, A.; Noumi, E.; Belaabed, S.; Aouadi, K.; Lamjed, B.; Adnan, M.; Defant, A.; Kadri, A.; Snoussi, M.; Khan, M.A.; et al. LC-ESI/MS-Phytochemical Profiling with Antioxidant, Antibacterial, Antifungal, Antiviral and In Silico Pharmacological Properties of Algerian Asphodelus tenuifolius (Cav.) Organic Extracts. Antioxidants 2021, 10, 628. [Google Scholar] [CrossRef]
- Alhage, J.; Elbitar, H. In Vitro Screening for Antioxidant and Antimicrobial Properties of Three Lebanese Medicinal Plants Crude Extracts. Pharmacogn. Res. 2019, 11, 127. [Google Scholar] [CrossRef]
- Abuhamdah, S. Phytochemical Investigations and Antibacterial Activity of Selected Medicinal Plants from Jordan. Eur. J. Med. Plants 2013, 3, 394–404. [Google Scholar] [CrossRef]
- Shin, K.Y.; Won, B.Y.; Ha, H.J.; Yun, Y.S.; Lee, H.G. Genotoxicity Studies on the Root Extract of Polygala Tenuifolia Willdenow. Regul. Toxicol. Pharmacol. 2015, 71, 365–370. [Google Scholar] [CrossRef]
- Kelber, O.; Wegener, T.; Steinhoff, B.; Staiger, C.; Wiesner, J.; Knöss, W.; Kraft, K. Assessment of Genotoxicity of Herbal Medicinal Products: Application of the “Bracketing and Matrixing” Concept Using the Example of Valerianae Radix (Valerian Root). Phytomedicine 2014, 21, 1124–1129. [Google Scholar] [CrossRef]
- Mortelmans, K.; Zeiger, E. The Ames Salmonella/Microsome Mutagenicity Assay. Mutat. Res.-Fundam. Mol. Mech. Mutagen. 2000, 455, 29–60. [Google Scholar] [CrossRef]
- Maron, D.M.; Ames, B.N. Revised Methods for the Salmonella Mutagenicity Test. Mutat. Res. Environ. Mutagen. Relat. Subj. 1983, 113, 173–215. [Google Scholar] [CrossRef] [PubMed]
- Wagner, H.; Bladt, S. Plant Drug Analysis: A Thin Layer Chromatography Atlas, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 1996. [Google Scholar]
- Scalbert, A.; Monties, B.; Janin, G. Tannins in Wood: Comparison of Different Estimation Methods. J. Agric. Food Chem. 1989, 37, 1324–1329. [Google Scholar] [CrossRef]
- Olivera, D.F.; Viña, S.Z.; Marani, C.M.; Ferreyra, R.M.; Mugridge, A.; Chaves, A.R.; Mascheroni, R.H. Effect of Blanching on the Quality of Brussels Sprouts (Brassica oleracea L. Gemmifera DC) after Frozen Storage. J. Food Eng. 2008, 84, 148–155. [Google Scholar] [CrossRef]
- Chang, C.L.; Lin, C.S. Phytochemical Composition, Antioxidant Activity, and Neuroprotective Effect of Terminalia Chebula retzius Extracts. Evid.-Based Complement. Altern. Med. 2012, 125247. [Google Scholar] [CrossRef]
- Wilfred Vermerris, R.N. Phenolic Compound Biochemistry; Springer: Dordrecht, The Netherlands, 2006; ISBN 978-1-4020-5163-0. [Google Scholar]
- Sakulpanich, A.; Gritsanapan, W. Extraction Method for High Content of Anthraquinones from Cassia Fistula Pods. J. Health Res. 2008, 22, 167–172. [Google Scholar]
- CLSI. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically, Approved Standard, 9th ed.; CLSI document M07-A9; CLSI: Wayne, PA, USA, 2012; Volume 32, ISBN 1-56238-783-9. [Google Scholar]
- Brand-Williams, W.; Cuvelier, M.E.; Berset, C. Use of a Free Radical Method to Evaluate Antioxidant Activity. LWT—Food Sci. Technol. 1995, 28, 25–30. [Google Scholar] [CrossRef]
- Benzie, I.F.F.; Strain, J.J. The Ferric Reducing Ability of Plasma (FRAP) as a Measure of “Antioxidant Power”: The FRAP Assay. Anal. Biochem. 1996, 239, 70–76. [Google Scholar] [CrossRef]
- Bocayuva Tavares, G.D.; Fortes Aiub, C.A.; Felzenszwalb, I.; Carrão Dantas, E.K.; Araújo-Lima, C.F.; Siqueira Júnior, C.L. In Vitro Biochemical Characterization and Genotoxicity Assessment of Sapindus saponaria Seed Extract. J. Ethnopharmacol. 2021, 276, 114170. [Google Scholar] [CrossRef]
- OECD (Organisation for Economic Co-operation and Development). Guideline for Testing of Chemicals: No.471-Bacterial Reverse Mutation Test; OECD: Paris, France, 2020; ISBN 9789264071247. [Google Scholar]
- ICH (International Conference on Harmonization). S2(R1) Guidance on Genotoxicity Testing and Data Interpretation for Pharmaceuticals Intended for Human Use; Step 4 Version of November; ICH: Geneva, Switzerland, 2011. [Google Scholar]
- Santos, J.M.; Camões, S.P.; Filipe, E.; Cipriano, M.; Barcia, R.N.; Filipe, M.; Teixeira, M.; Simões, S.; Gaspar, M.; Mosqueira, D.; et al. Three-Dimensional Spheroid Cell Culture of Umbilical Cord Tissue-Derived Mesenchymal Stromal Cells Leads to Enhanced Paracrine Induction of Wound Healing. Stem Cell Res. Ther. 2015, 6, 90. [Google Scholar] [CrossRef]
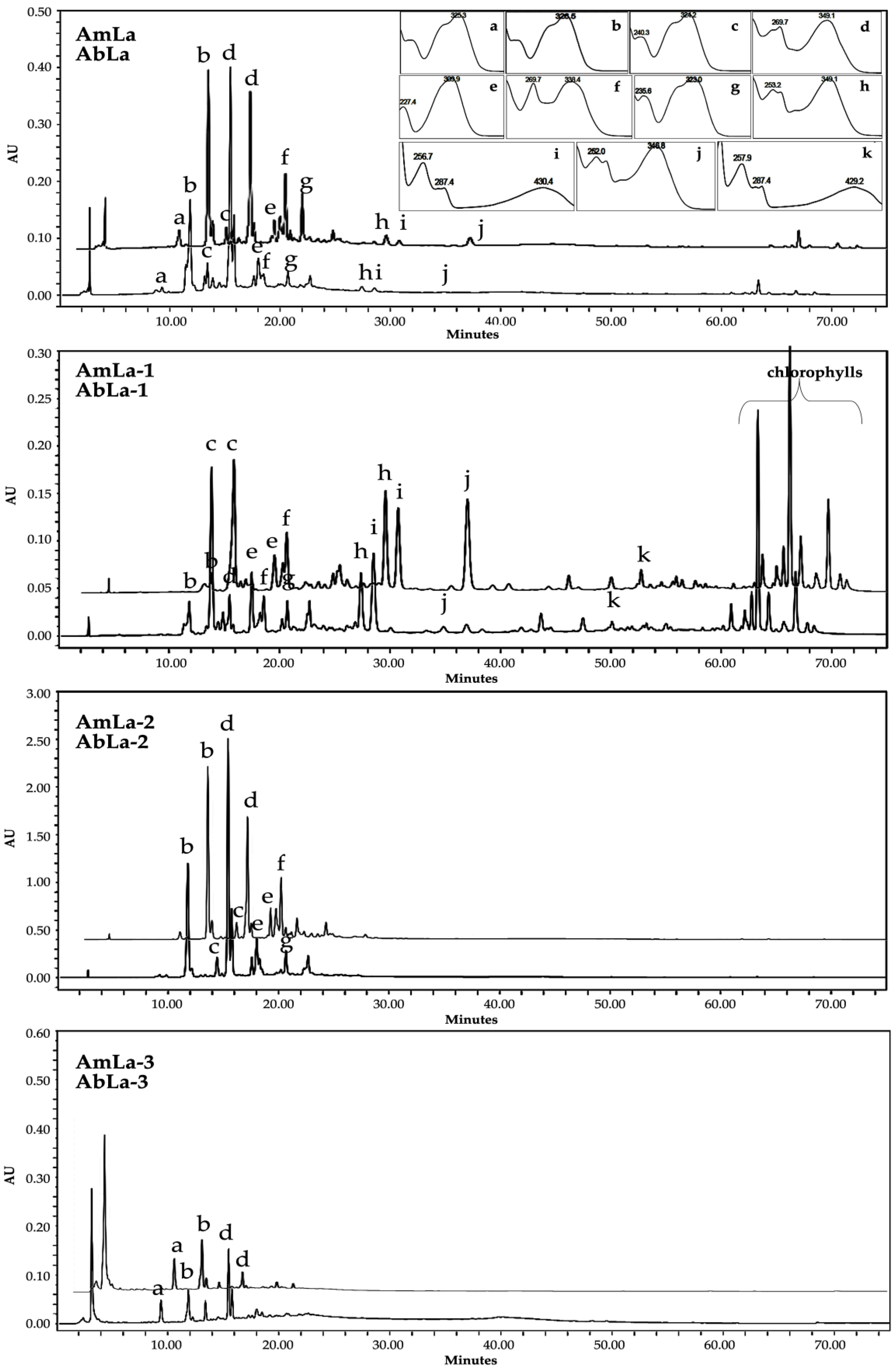
| Peak | tR (min) | λmax (nm) | [M-H]−(m/z) | MS/MS (m/z) | Identified Compound |
|---|---|---|---|---|---|
| a | 9.29 | 325.3 | 353 | 191 (100), 179 (3) | * neochlorogenic acid |
| b | 11.79 | 326.5 | 353 | 191 (100), 179 (67) | chlorogenic acid |
| c | 13.82 | 240.3, 324.2 | 179 | 135 (100) | caffeic acid |
| d | 15.43 | 269.7, 349.1 | 447 | 357 (43), 327 (100), 297 (76) | isoorientin |
| e | 17.46 | 227.4, 309.9 | 163 | 119 (100) | p-coumaric acid |
| f | 18.55 | 269.7, 338.4 | 431 | 341 (23), 311 (72), 283 (100) | isovitexin |
| g | 20.53 | 235.6, 323.0 | 193 | 178 (62), 149 (68), 134 (100) | ferulic acid |
| h | 27.38 | 253.2, 349.1 | 285 | 175 (13), 151 (100), 133 (22) | luteolin |
| i | 28.73 | 256.7, 287.4, 430.4 | 269 | 239 (100) | aloe-emodin |
| j | 34.78 | 252.0, 346.8 | 299 | 284 (100) | diosmetin |
| k | 50.46 | 257.9, 287.4, 429.2 | 253 | 225 (100) | chrysophanol |
| Assays | AbLa | AbLb | AmLa | AmLb |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |
| TPC (mg GAE/g dried extract) (mg GAE/g dried leaf) | 44.16 ± 21.62 9.23 ± 4.52 | 38.83 ± 17.1 8.57 ± 3.78 | 37.15 ± 14.32 12.63 ± 5.38 | 38.28 ± 15.63 6.09 ± 2.49 |
| TFC (mg CAE/g dried extract) (mg CAE/g dried leaf) | * 40.79 ± 4.45 8.16 ± 0.89 | 29.56 ± 1.43 6.53 ± 0.32 | 33.46 ± 0.89 5.32 ± 0.14 | * 35.52 ± 1.51 12.08 ± 0.51 |
| TAC (mg RhE/g dried extract) (mg RhE/g dried leaf) | * 1.16 ± 0.13 0.24 ± 0.05 | 1.07 ± 0.11 0.24 ± 0.04 | 0.55 ± 0.07 0.19 ± 0.02 | 0.81 ± 0.09 0.13 ± 0.01 |
| TCTC (mg CAE/g dried extract) (mg CAE/g dried leaf) | * 180.96 ± 10.98 37.82 ± 2.30 | 149.71 ± 12.98 33.06 ± 2.87 | 132.60 ± 2.73 45.09 ± 0.93 | 142.98 ± 6.71 22.73 ± 1.07 |
| THTC (mg GAE/g dried extract) (mg GAE/g dried leaf) | 67.61 ± 9.22 14.13 ± 1.93 | * 55.16 ± 6.64 12.18 ± 1.47 | 60.53 ± 8.04 20.58 ± 2.74 | 37.03 ± 3.87 5.89 ± 0.62 |
| TTC (mg OAE/g dried extract) (mg OAE/g dried leaf) | 111.72 ± 22.77 23.35 ± 4.76 | 88.78 ± 23.22 19.60 ± 5.13 | * 165.47 ± 26.54 56.26 ± 9.03 | 125.74 ± 20.72 19.99 ± 3.29 |
| Extracts Code | Assays | |
|---|---|---|
| DPPH (IC50 μg/mL) | FRAP (mmol AA/g Dry Extract) | |
| AbLa | 2000 | 0.337 ± 0.042 |
| AbLb | 2540 | 0.306 ± 0.023 |
| AmLa | 2990 | 0.280 ± 0.046 |
| AmLb | 3070 | 0.271 ± 0.072 |
| AbLa-1 | 2950 | Nd |
| AbLa-2 | 800 | Nd |
| AbLa-3 | 2910 | Nd |
| AmLa-1 | 3009 | Nd |
| AmLa-2 | 1200 | Nd |
| AmLa-3 | 4000 | Nd |
| AA | 83 | Nd |
| Bacteria (Gram +) | MIC (µg/mL) | ||
|---|---|---|---|
| AbLa-1 | AmLa-1 | Aloe-Emodin | |
| S. aureus ATCC 29213 | 500 | 500 | 3.2 |
| S. aureus CQINSA4923 | 62 | 125 | 50 |
| S. aureus INSArefV | 500 | 500 | 1.6 |
| S. aureus INSA936 | 250 | 250 | 12.5 |
| S. aureus INSA896 | 125 | 125 | 3.2 |
| S. saprophyticus INSA842 | 125 | 250 | 100 |
| S. saprophyticus INSA867 | 1000 | 1000 | 25 |
| S. epidermidis INSA796 | 250 | 500 | 1.6 |
| S. epidermidis INSA958 | 250 | 500 | 0.8 |
| S. epidermidis INSA960 | 125 | 125 | 1.6 |
| S. haemolyticus INSA982 | 125 | 125 | 25 |
| S. haemolyticus INSA984 | 125 | 125 | 12.5 |
| AbLa µg/Plate | Number of Revertant Colonies Without Metabolic Activation, Mean (n = 3) ± Standard Deviation (SD) | ||||
|---|---|---|---|---|---|
| TA98 | TA100 | TA102 | TA1535 | TA1537 | |
| 250 | 17 ± 4 | 160 ± 7 | 355 ± 13 | 19 ± 4 | 10 ± 1 |
| 625 | 20 ± 4 | 158 ± 5 | 349 ± 34 | 24 ± 1 | 10 ± 2 |
| 1250 | 17 ± 2 | 182 ± 16 | 429 ± 25 | 20 ± 1 | 7 ± 1 |
| 2500 | 21 ± 2 | 178 ± 8 | 458 ± 16 | 22 ± 2 | 8 ± 2 |
| 3750 | 24 ± 3 | 175 ± 19 | 472 ± 29 | 21 ± 4 | 9 ± 3 |
| 5000 | 24 ± 2 | 175 ± 14 | 485 ± 31 | 18 ± 1 | 13 ± 3 |
| AmLa µg/plate | |||||
| 250 | 17 ± 2 | 186 ± 10 | 357 ± 14 | 22 ± 3 | 9 ± 1 |
| 625 | 20 ± 2 | 155 ± 15 | 365 ± 3 | 20 ± 3 | 9 ± 2 |
| 1250 | 22 ± 5 | 150 ± 5 | 394 ± 8 | 16 ± 1 | 10 ± 5 |
| 2500 | 21 ± 3 | 170 ± 15 | 441 ± 2 | 17 ± 3 | 12 ± 5 |
| 3750 | 24 ± 5 | 168 ± 4 | 454 ± 24 | 17 ± 3 | 8 ± 2 |
| 5000 | 23 ± 3 | 165 ± 20 | 407 ± 28 | 24 ± 2 | 15 ± 1 |
| NC | 19 ± 2 | 156 ± 17 | 320 ± 4 | 21 ± 3 | 7 ± 1 |
| PC | 2-NF | SA | tBHP | SA | 9-AA |
| 488 ± 30 | 1048 ± 43 | 881 ± 26 | 827 ± 13 | 1354 ± 5 | |
| AbLa µg/plate | Number of revertant colonies with metabolic activation, mean (n = 3) ± standard deviation (SD) | ||||
| 500 | Nd | 166 ± 22 | 221 ± 16 | 19 ± 4 | 15 ± 1 |
| 1250 | 63 ± 6 | 164 ± 9 | 248 ± 11 | 15 ± 7 | 16 ± 1 |
| 2500 | 59 ± 5 | 174 ± 4 | 248 ± 11 | 17 ± 2 | 11 ± 1 |
| 5000 | 52 ± 6 | 178 ± 15 | 254 ± 12 | 15 ± 1 | 16 ± 1 |
| NC | 44 ± 8 | 157 ± 6 | 172 ± 2 | 11 ± 2 | 12 ± 1 |
| PC | 2-AA | BaP | 2-AA | 2-AA | 2-AA |
| 832 ± 35 | 947 ± 148 | 732 ± 12 | 266 ± 1 | 306 ± 50 | |
| Bacteria (Gram +) | Demonstration of Resistance to the Antibiotics | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CXT | CPFX | DAP | ERY | FA | GN | Lzd | OXA | PCN | TEC | TET | VAN | |
| S. aureus ATCC 29,213 | S | MS | ||||||||||
| S. aureus CQINSA4923 | R | R | R | S | R | S | R | R | S | S | S | |
| S. aureus INSArefV | R | R | R | |||||||||
| S. aureus INSA936 | R | |||||||||||
| S. aureus INSA896 | R | R | R | R | ||||||||
| S. saprophyticus INSA842 | R | R | ||||||||||
| S. saprophyticus INSA867 | R | |||||||||||
| S. epidermidis INSA796 | R | R | R | R | ||||||||
| S. epidermidis INSA958 | R | R | ||||||||||
| S. epidermidis INSA960 | R | |||||||||||
| S. haemolyticus INSA982 | R | R | R | |||||||||
| S. haemolyticus INSA984 | R | R | R | |||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malmir, M.; Lima, K.; Póvoas Camões, S.; Manageiro, V.; Duarte, M.P.; Paiva Miranda, J.; Serrano, R.; Moreira da Silva, I.; Silva Lima, B.; Caniça, M.; et al. Identification of Marker Compounds and In Vitro Toxicity Evaluation of Two Portuguese Asphodelus Leaf Extracts. Molecules 2023, 28, 2372. https://doi.org/10.3390/molecules28052372
Malmir M, Lima K, Póvoas Camões S, Manageiro V, Duarte MP, Paiva Miranda J, Serrano R, Moreira da Silva I, Silva Lima B, Caniça M, et al. Identification of Marker Compounds and In Vitro Toxicity Evaluation of Two Portuguese Asphodelus Leaf Extracts. Molecules. 2023; 28(5):2372. https://doi.org/10.3390/molecules28052372
Chicago/Turabian StyleMalmir, Maryam, Katelene Lima, Sérgio Póvoas Camões, Vera Manageiro, Maria Paula Duarte, Joana Paiva Miranda, Rita Serrano, Isabel Moreira da Silva, Beatriz Silva Lima, Manuela Caniça, and et al. 2023. "Identification of Marker Compounds and In Vitro Toxicity Evaluation of Two Portuguese Asphodelus Leaf Extracts" Molecules 28, no. 5: 2372. https://doi.org/10.3390/molecules28052372
APA StyleMalmir, M., Lima, K., Póvoas Camões, S., Manageiro, V., Duarte, M. P., Paiva Miranda, J., Serrano, R., Moreira da Silva, I., Silva Lima, B., Caniça, M., & Silva, O. (2023). Identification of Marker Compounds and In Vitro Toxicity Evaluation of Two Portuguese Asphodelus Leaf Extracts. Molecules, 28(5), 2372. https://doi.org/10.3390/molecules28052372











