Napyradiomycin A4 and Its Relate Compounds, a New Anti-PRV Agent and Their Antibacterial Activities, from Streptomyces kebangsaanensis WS-68302
Abstract
1. Introduction
2. Results and Discussion
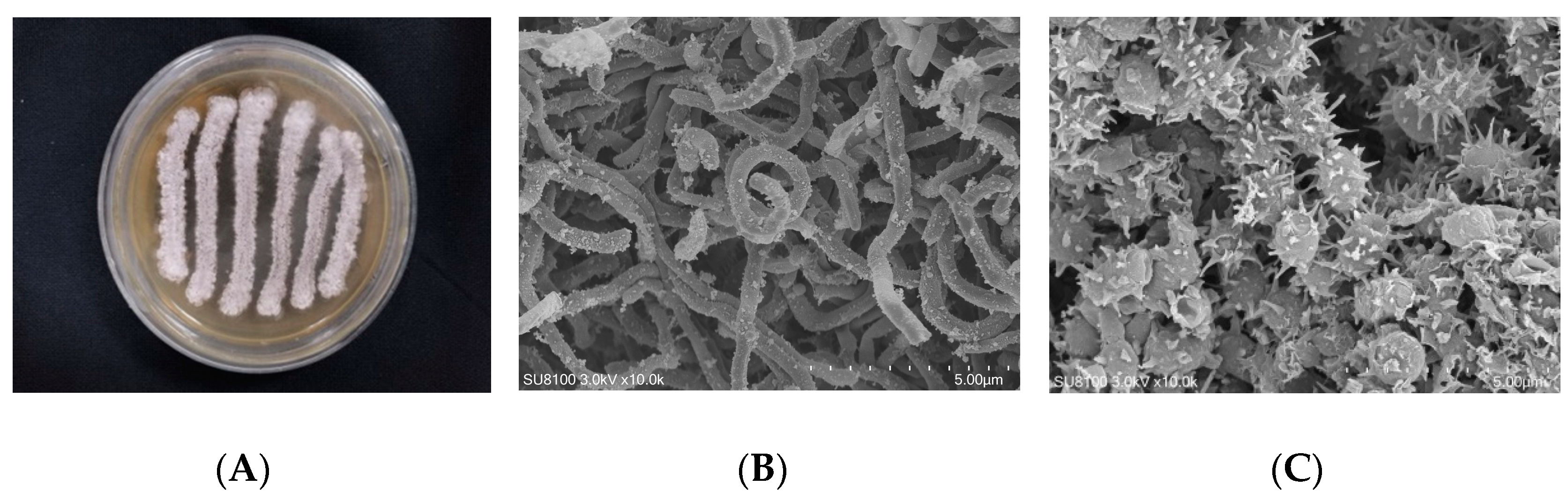
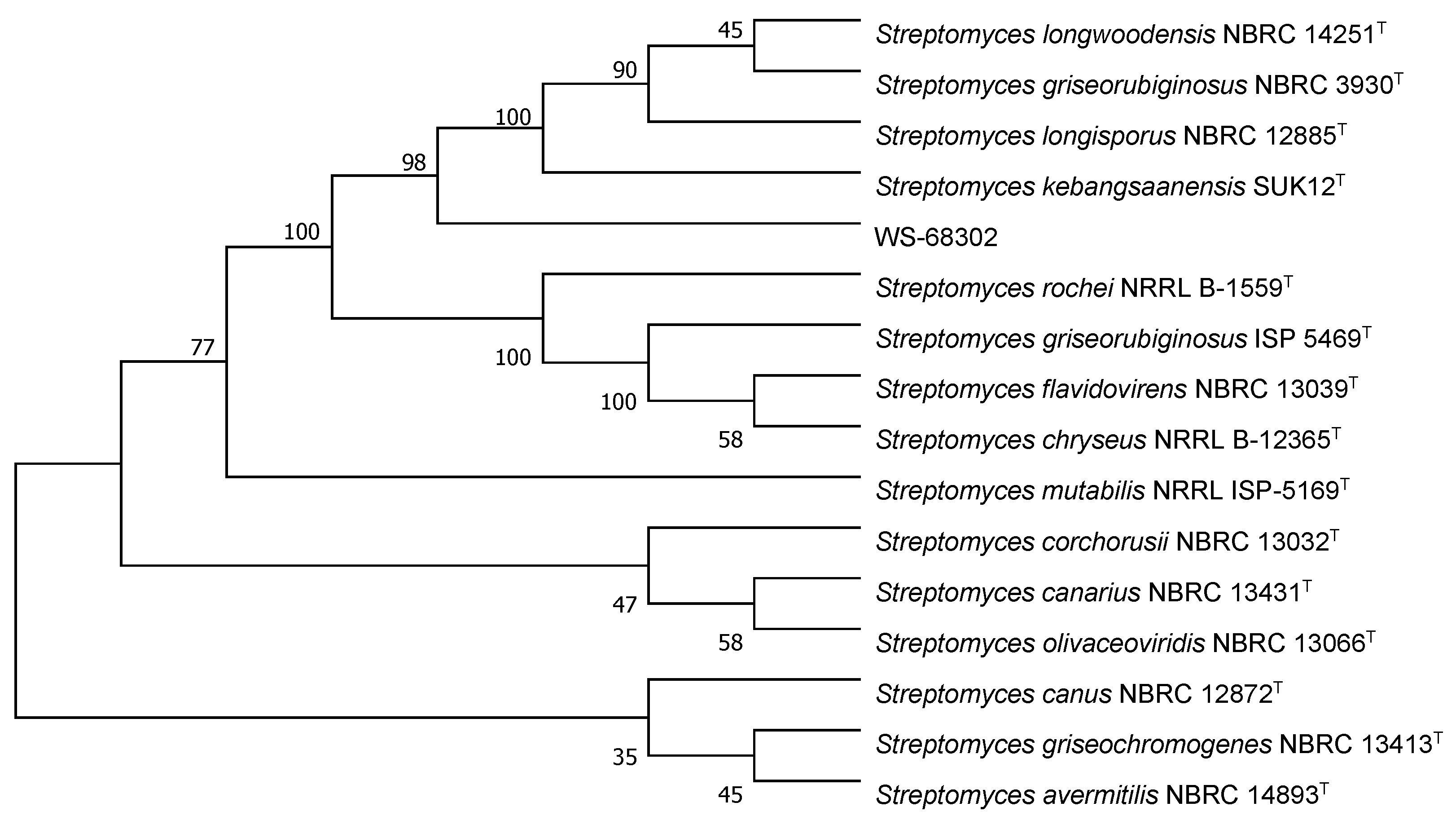
2.1. Taxonomy of Strain WS-68302
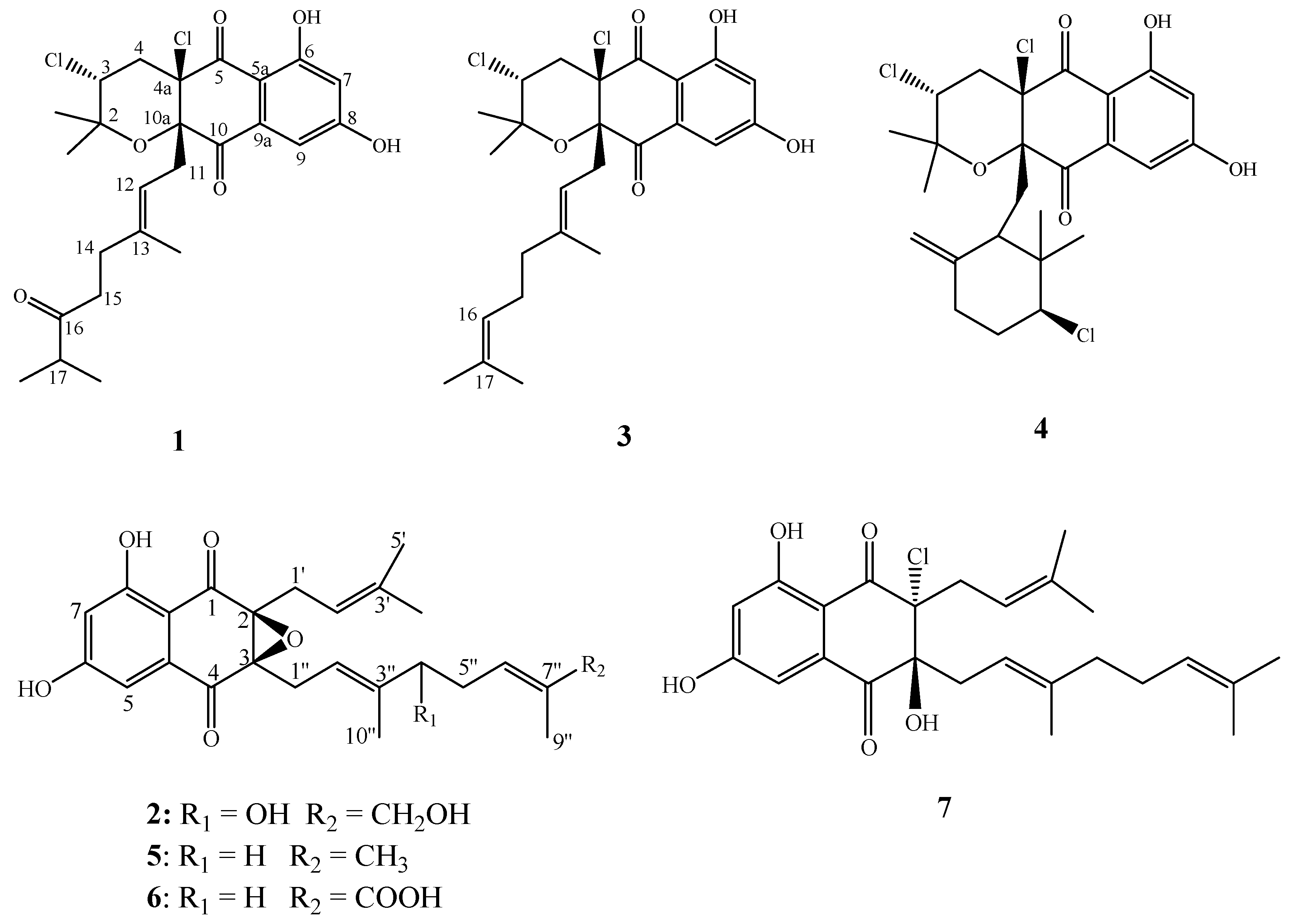
2.2. Structural Elucidation
2.3. Biological Activities
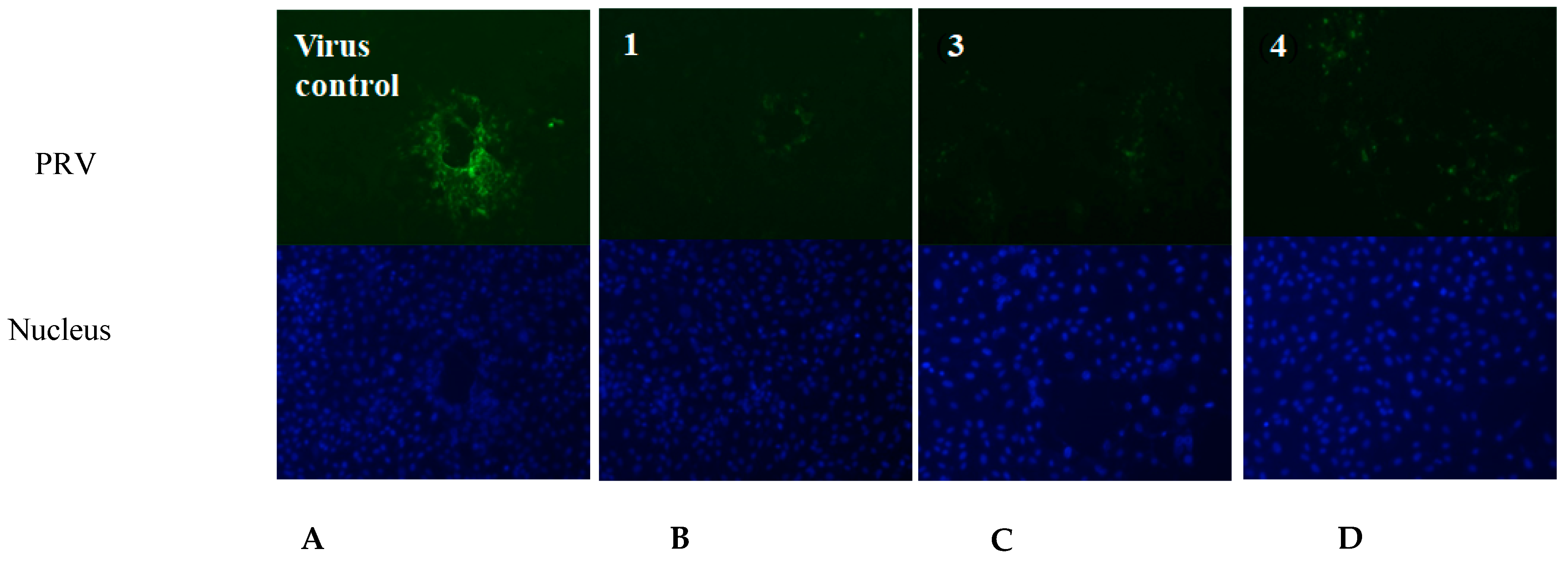
2.3.1. Antiviral Activities of 1–7 against PRV In Vitro
2.3.2. Indirect Immunofluorescence Assay
2.3.3. Antibacterial Activities
3. Conclusions
4. Experimental Section
4.1. General Experimental Procedures
4.2. Isolation of Strain and Morphological Identification
4.3. Fermentation
4.4. Extraction and Isolation
4.5. Antiviral and Antibacterial Assays
4.5.1. Antiviral Assays
Cells, Virus and Reagents
Chemicals, Antibodies and Reagents
Cell Proliferation
Cell Bioability Assay
Indirect Immunofluorescence Assay
4.5.2. Antibacterial Assays
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Ma, W.J.; Lager, K.M.; Richt, J.A.; Stoffregen, W.C.; Zhou, F.H.; Yoon, K.J. Development of real-time polymerase chain reaction assays for rapid detection and differentiation of wild-type pseudorabies and gene-deleted vaccine viruses. J. Vet. Diagn. Investig. 2008, 20, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.H.; Tong, W.Z.; Song, X.; Jia, R.Y.; Li, L.X.; Zou, Y.F.; He, C.L.; Liang, X.X.; Lv, C.; Jing, B. Antiviral effect of resveratrol in piglets infected with virulent pseudorabies virus. Viruses 2018, 10, 457. [Google Scholar] [CrossRef] [PubMed]
- Brittle, E.E.; Reynolds, A.E.; Enquist, L.W. Two modes of pseudorabies virus neuroinvasion and lethality in mice. J. Virol. 2004, 78, 12951–12963. [Google Scholar] [CrossRef] [PubMed]
- Pomeranz, L.E.; Reynolds, A.E.; Hengartner, C.J. Molecular biology of pseudorabies virus: Impact on neurovirology and veterinary medicine. Microbiol. Mol. Biol. Rev. 2005, 69, 462–500. [Google Scholar] [CrossRef]
- An, T.Q.; Peng, J.M.; Tian, Z.J.; Zhao, H.Y.; Li, N.; Liu, Y.M.; Chen, J.Z.; Leng, C.L.; Sun, Y.; Chang, D.; et al. Pseudorabies virus variant in Bartha-K61-vaccinated pigs, China, 2012. Emerg. Infect. Dis. 2013, 19, 1749–1755. [Google Scholar] [CrossRef] [PubMed]
- Freuling, C.M.; Muller, T.F.; Mettenleiter, T.C. Vaccines against pseudorabies virus (PrV). Vet. Microbiol. 2017, 206, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Hu, D.F.; Zhang, Z.D.; Lv, L.; Xiao, Y.H.; Qu, Y.J.; Ma, H.Y.; Niu, Y.J.; Wang, G.W.; Liu, S.D. Outbreak of variant pseudorabies virus in Bartha-K61-vaccinated piglets in central Shandong Province, China. J. Vet. Diagn. Investig. 2015, 27, 600–605. [Google Scholar] [CrossRef] [PubMed]
- Hu, R.M.; Zhou, Q.; Song, W.B.; Sun, E.C.; Zhang, M.M.; He, Q.G.; Chen, H.C.; Wu, B.; Liu, Z.F. Novel pseudorabies virus variant with defects in TK, gE and gI protects growing pigs against lethal challenge. Vaccine 2015, 33, 5733–5740. [Google Scholar] [CrossRef]
- Liu, X.; Lv, L.; Jiang, C.L.; Bai, J.; Gao, Y.N.; Ma, Z.H.; Jian, P. A natural product, (S)-10-Hydroxycamptothecin inhibits pseudorabies virus proliferation through DNA damage dependent antiviral innate immunity. Vet. Microbiol. 2022, 265, 109313–109323. [Google Scholar] [CrossRef]
- Gottschalk, M.; Segura, M.; Xu, J.G. Streptococcus suis infections in humans: The Chinese experience and the situation in North America. Anim. Health Res. Rev. 2007, 8, 29–45. [Google Scholar] [CrossRef]
- Lun, Z.R.; Wang, Q.P.; Chen, X.G.; Li, A.X.; Zhu, X.Q. Streptococcus suis: An emerging zoonotic pathogen. Lancet. Infect. Dis. 2007, 7, 201–209. [Google Scholar] [CrossRef]
- Shimoji, Y. Pathogenicity of Erysipelothrix husiopathiae: Virulence factors and protective immunity. Microbes Infect. 2000, 2, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Josephine Brooke, C.; Riley, T.V. Erysipelothrix rhusiopathiae: Bacteriology, epidemiology and clinical manifestations of an occupational pathogen. J. Med. Microbiol. 1999, 48, 789–799. [Google Scholar] [CrossRef]
- Tacconelli, E.; Carrara, E.; Savoldi, A.; Harbarth, S.; Mendelson, M.; Monnet, D.L. Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect. Dis. 2018, 18, 318–327. [Google Scholar] [CrossRef]
- Shiomi, K.; Iinuma, H.; Hamada, M.; Naganawa, H.; Manabe, M.; Matsuki, C.; Takeuchi, T.; Umezawa, H. Novel antibiotics napyradiomycins. Production, isolation, physicochemical properties and biological activity. J. Antibiot. 1986, 39, 487–493. [Google Scholar] [CrossRef]
- Shiomi, K.; Nakamura, H.; Iinuma, H.; Naganawa, H.; Isshiki, K.; Takeuchi, T.; Umezawa, H. Structures of new antibiotics napyradiomycins. J. Antibiot. 1986, 39, 494–501. [Google Scholar] [CrossRef]
- Shomura, A.; Gomi, S.; Ito, M.; Yoshida, J.; Tanaka, E.; Amano, S.; Watabe, H.; Ohuchi, S.; Itoh, J.; Sezaki, M.; et al. Studies on new antibiotics SF2415. I. Taxonomy, fermentation, isolation, physico-chemical properties and biological activities. J. Antibiot. 1987, 40, 732–739. [Google Scholar] [CrossRef] [PubMed]
- Gomi, S.; Ohuchi, S.; Sasaki, T.; Itoh, J.; Sezaki, M. Studies on new antibiotics SF2415. 2. The structural elucidation. J. Antibiot. 1987, 40, 740–749. [Google Scholar] [CrossRef]
- Fukuda, D.S.; Mynderse, J.S.; Baker, P.J.; Berry, D.M.; Boeck, L.D.; Yao, R.C.; Mertz, F.P.; Nakatsukasa, W.M.; Mabe, J.; Ott, J.; et al. A80915, a new antibiotic complex produced by Streptomyces aculeolatus. Discovery, taxonomy, fermentation, isolation, characterization, and antibacterial evaluation. J. Antibiot. 1990, 43, 623–633. [Google Scholar] [CrossRef] [PubMed]
- Dantzig, A.H.; Minor, P.L.; Garrigus, J.L.; Fukuda, D.S.; Mynderse, J.S. Studies on the mechanism of action of A80915A, a semi-naphthoquinone natural product, as an inhibitor of gastric (H+-K+)-ATPase. Biochem. Pharmacol. 1991, 42, 2019–2026. [Google Scholar] [CrossRef]
- Hori, Y.; Abe, Y.; Shigematsu, N.; Goto, T.; Okuhara, M.; Kohsaka, M. Napyradiomycin A and B1: Non-steroidal estrogen-receptor antagonists produced by a Streptomyces. J. Antibiot. 1993, 46, 1890–1893. [Google Scholar] [CrossRef] [PubMed]
- Farnaes, L.L.L. Novel Analogs and a Protein Target for the Napyradiomycins. Ph.D. Thesis, University of California, San Diego, CA, USA, 2009. [Google Scholar]
- Cheng, Y.B.; Jensen, P.R.; Fenical, W. Cytotoxic and antimicrobial napyradiomycins from two marine-derived Streptomyces Strains. Eur. J. Organ. Chem. 2013, 2013, 3751–3757. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.C.; Li, S.M.; Li, J.; Chen, Y.C.; Saurav, K.; Zhang, Q.B.; Zhang, H.B.; Zhang, W.J.; Zhang, W.M.; Zhang, S.; et al. Antibacterial and cytotoxic new napyradiomycins from the marine-derived Streptomyces sp. SCSIO 10428. Mar. Drugs 2013, 11, 2113–2125. [Google Scholar] [CrossRef]
- Pereira, F.; Almeida, J.R.; Paulino, M.; Grilo, I.R.; Macedo, H.; Cunha, I.; Sobral, R.G.; Vasconcelos, V.; Gaudêncio, S.P. Antifouling napyradiomycins from marine-derived actinomycetes Streptomyces aculeolatus. Mar. Drugs 2020, 18, 63. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.W.; Kim, G.J.; Kim, H.J.; Nam, J.W.; Kim, J.; Chin, J.W.; Park, J.H.; Choi, H.; Park, K.D. Identification and evaluation of a napyradiomycin as a potent Nrf2 activator: Anti-oxidative and anti-inflammatory activities. Bioorganic Chem. 2020, 105, 104434. [Google Scholar] [CrossRef] [PubMed]
- Sarmin, N.I.M.; Tan, G.Y.A.; Franco, C.M.M.; Edrada-Ebel, R.; Latip, J.; Zin, N.M. Streptomyces kebangsaanensis sp. nov., an endophytic actinomycete isolated from an ethnomedicinal plant, which produces phenazine-1-carboxylic acid. Int. J. Syst. Evol. Micr. 2013, 63, 3733–3738. [Google Scholar] [CrossRef]
- Ohtani, I.; Kusumi, T.; Ishitsuka, M.O.; Kakisawa, H. Absolute configurations of marine diterpenes possessing a xenicane skeleton an application of an advanced Mosher’s method. Tetrahedron Lett. 1989, 30, 3147–3150. [Google Scholar] [CrossRef]
- Takemura, S.; Hirayama, A.; Tokunaga, J.; Kawamura, F.; Inagaki, K.; Hashimoto, K.; Nakata, M. A concise total synthesis of (+)-A80915G, a member of the napyradiomycin family of antibiotics. Tetrahedron Lett. 1999, 40, 7501–7505. [Google Scholar] [CrossRef]
- Motohashi, K.; Irie, K.; Toda, T.; Matsuo, Y.; Kasai, H.; Sue, M.; Furihata, K.; Seto, H. Studies on terpenoids produced by actinomycetes. 5-Dimethylallylindole-3-carboxylic acid and A80915G-8″-acid produced by marine-derived Streptomyces sp. MS239. J. Antibiot. 2008, 61, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Henkel, T.; Zeeck, A. Secondary metabolites by chemical screening. 15. Structure and absolute configuration of naphthomevalin, a new dihydro-naphthoquinone antibiotic from Streptomyces sp. J. Antibiot. 1991, 44, 665–669. [Google Scholar] [CrossRef]
- Li, S.F.; Hu, X.X.; Li, L.L.; Hu, X.M.; Wang, J.; Hu, X.W.; Liu, H.Y.; Yu, L.Y.; You, X.F.; Jiang, B.Y.; et al. 1-hydroxy-7-oxolavanducyanin and Δ7″,8″-6″-hydroxynaphthomevalin from Streptomyces sp. CPCC 203577. J. Antibiot. 2020, 73, 324–328. [Google Scholar] [CrossRef] [PubMed]
- Saitou, N.; Nei, M. The neighbor-joining method: A new method for reconstructing phylogenetic trees. Mol. Biol. Evol. 1987, 4, 406–425. [Google Scholar] [PubMed]
- Lu, H.; Lu, W.J.; Zhu, Y.W.; Wang, C.C.; Shi, L.M.; Li, X.D.; Wu, Z.Y.; Wang, G.Y.; Dong, W.; Tan, C.; et al. Auranofin has advantages over first-Line drugs in the treatment of severe Streptococcus suis infections. Antibiotics 2021, 10, 26. [Google Scholar] [CrossRef] [PubMed]

| Position | δC | δH (J in Hz) |
|---|---|---|
| 2 | 78.9, C | |
| 2-CH3 | 29.0, CH3 | 1.50, s |
| 2-CH3 | 22.4, CH3 | 1.18, s |
| 3 | 58.9, CH | 4.42, dd (12.0, 4.0) |
| 4 | 42.8, CH2 | 2.48, dd (14.3, 4.0) |
| 2.43, d (12.0) | ||
| 4a | 79.2, C | |
| 5 | 194.0, C | |
| 5a | 109.9, C | |
| 6 | 164.8, C | |
| 7 | 109.5, CH | 6.72, br s |
| 8 | 164.4, C | |
| 9 | 108.2, CH | 7.17, br s |
| 9a | 135.4, C | |
| 10 | 195.5, C | |
| 10a | 83.7, C | |
| 11 | 41.2, CH2 | 2.68, br d (8.1) |
| 12 | 115.7, CH | 4.70, t (8.5) |
| 13 | 141.2, C | |
| 13-CH3 | 16.7, CH3 | 1.32, s |
| 14 | 38.0, CH2 | 2.15, m |
| 2.10, m | ||
| 15 | 33.3, CH2 | 1.93, m |
| 1.88, m | ||
| 16 | 215.0, C | |
| 17 | 41.1, CH | 2.53, m |
| 17-CH3 | 18.4, CH3 | 1.06, t (6.4) |
| 17-CH3 | 18.3, CH3 | 1.06, t (6.4) |
| No. | δC | δH (J in Hz) |
|---|---|---|
| 1 | 194.8 s | |
| 2 | 68.0 s | |
| 3 | 67.3 s | |
| 4 | 192.4 s | |
| 4a | 133.8 s | |
| 5 | 108.3 d | 6.89 br s |
| 6 | 164.5 s | |
| 7 | 109.3 d | 6.55 br s |
| 8 | 164.8 s | |
| 8a | 108.7 s | |
| 1′ | 25.4 t | 3.28 dd (15.5, 7.2) |
| 2.36 s | ||
| 2′ | 116.9 d | 5.11 s |
| 3′ | 135.9 s | |
| 4′ | 26.0 q | 1.73 s |
| 5′ | 18.4 q | 1.73 s |
| 1″ | 25.6 t | 2.96 dd (15.5, 7.3) |
| 2.57 dd (15.5, 5.9) | ||
| 2″ | 120.0 d | 5.41 s |
| 3″ | 139.3 s | |
| 4″ | 77.0 d | 4.12 t (6.7) |
| 5″ | 33.1 t | 2.38 m |
| 6″ | 121.7 d | 5.30 s |
| 7″ | 136.8 s | |
| 8″ | 68.8 t | 3.98 m |
| 9″ | 14.1 q | 1.67 s |
| 10″ | 12.3 q | 1.74 s |
| Compounds | IC50 (μM) | CC50 (μM) | TI |
|---|---|---|---|
| 1 | 2.056 ± 0.343 | 30.806 ± 5.565 | 14.98 |
| 2 | - | - | - |
| 3 | 2.208 ± 0.375 | 5.790 ± 0.708 | 2.62 |
| 4 | 13.268 ± 1.109 | 19.630 ± 2.821 | 1.48 |
| 5 | 8.260 ± 0.902 | 16.680 ± 1.122 | 2.05 |
| 6 | 26.470 ± 5.00 | 46.318 ± 7.364 | 1.75 |
| 7 | - | >0.045 | - |
| Ribavirin | 58.032 | >163.9 | >2.82 |
| Code | S. aureus | S. suis | E. rhusiopathiae | E. coli |
|---|---|---|---|---|
| 1 | 25 | 100 | 50 | - |
| 2 | - | - | - | - |
| 3 | <0.78 | 3.125 | 50 | - |
| 4 | <0.78 | 6.25 | 50 | - |
| 5 | - | 25 | 25 | - |
| 6 | 50 | 50 | 25 | - |
| 7 | <0.625 | 20 | 40 | - |
| Penicillin G | - | 12.5 | 50 | - |
| Cefpirome Sulfate | <0.78 | <0.78 | <0.78 | 25 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Fang, W.; Wang, K.; Zhang, Z.; Wu, Z.; Shi, L.; Liu, F.; Wan, Z.; Liu, M. Napyradiomycin A4 and Its Relate Compounds, a New Anti-PRV Agent and Their Antibacterial Activities, from Streptomyces kebangsaanensis WS-68302. Molecules 2023, 28, 640. https://doi.org/10.3390/molecules28020640
Zhang Y, Fang W, Wang K, Zhang Z, Wu Z, Shi L, Liu F, Wan Z, Liu M. Napyradiomycin A4 and Its Relate Compounds, a New Anti-PRV Agent and Their Antibacterial Activities, from Streptomyces kebangsaanensis WS-68302. Molecules. 2023; 28(2):640. https://doi.org/10.3390/molecules28020640
Chicago/Turabian StyleZhang, Yani, Wei Fang, Kaimei Wang, Zhigang Zhang, Zhaoyuan Wu, Liqiao Shi, Fang Liu, Zhongyi Wan, and Manli Liu. 2023. "Napyradiomycin A4 and Its Relate Compounds, a New Anti-PRV Agent and Their Antibacterial Activities, from Streptomyces kebangsaanensis WS-68302" Molecules 28, no. 2: 640. https://doi.org/10.3390/molecules28020640
APA StyleZhang, Y., Fang, W., Wang, K., Zhang, Z., Wu, Z., Shi, L., Liu, F., Wan, Z., & Liu, M. (2023). Napyradiomycin A4 and Its Relate Compounds, a New Anti-PRV Agent and Their Antibacterial Activities, from Streptomyces kebangsaanensis WS-68302. Molecules, 28(2), 640. https://doi.org/10.3390/molecules28020640






