Effect of Chitosan Dispersion and Microparticles on Older Streptococcus mutans Biofilms
Abstract
:1. Introduction
2. Results
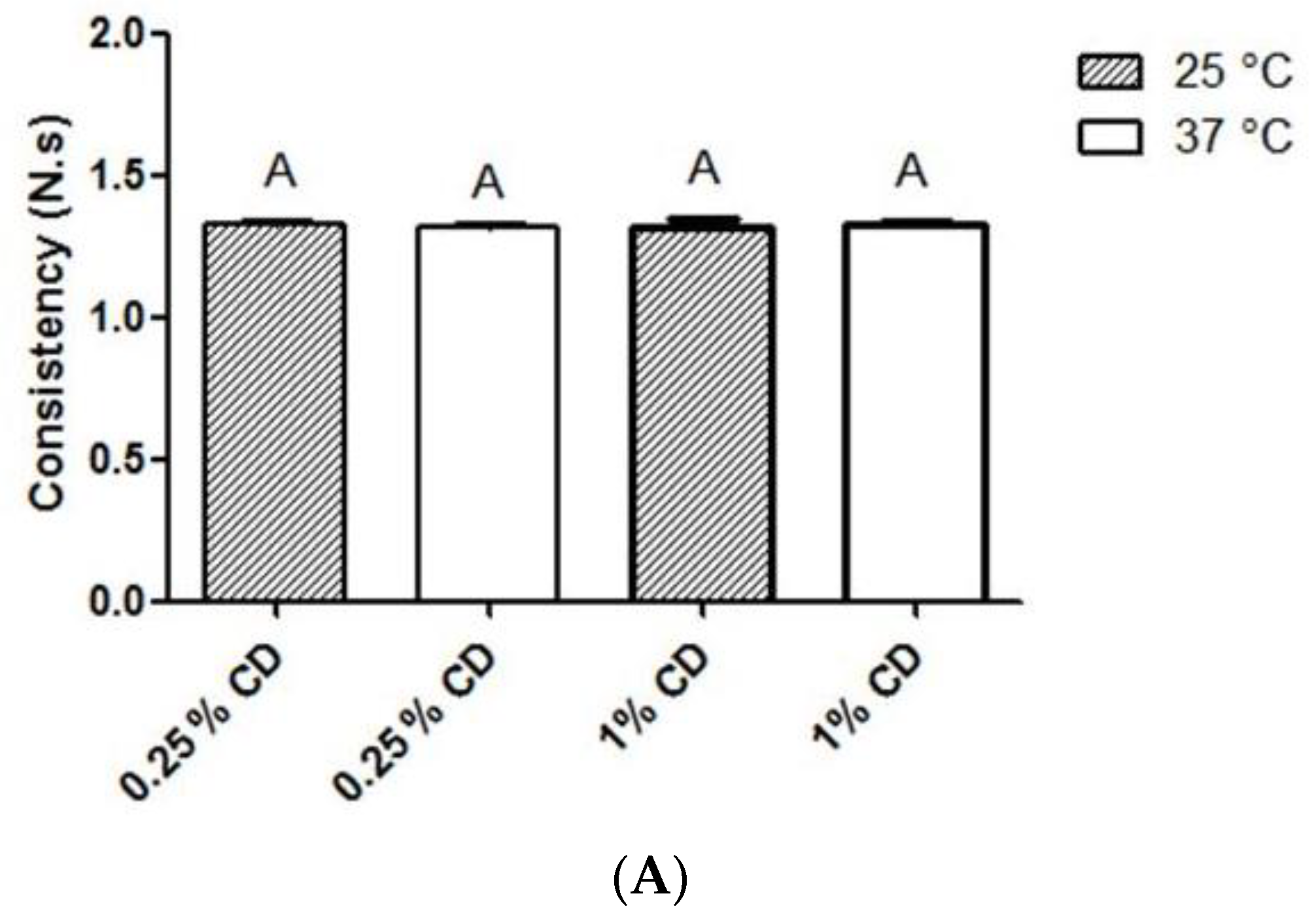
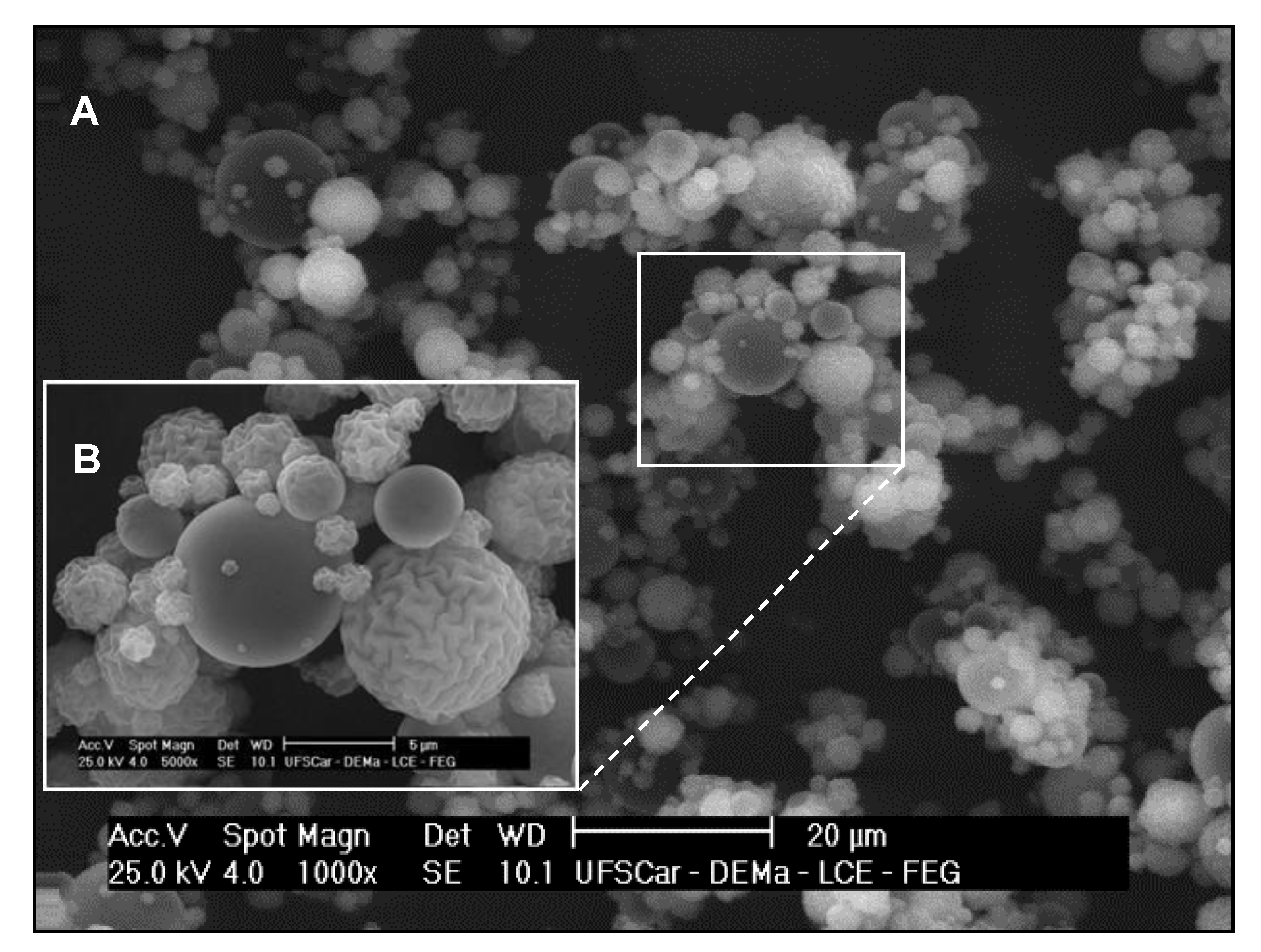
2.1. Physicochemical Properties of Chitosan Dispersion and Microparticles
2.2. Determination of Minimum Inhibitory (MIC) and Bactericidal Concentrations (MBC)
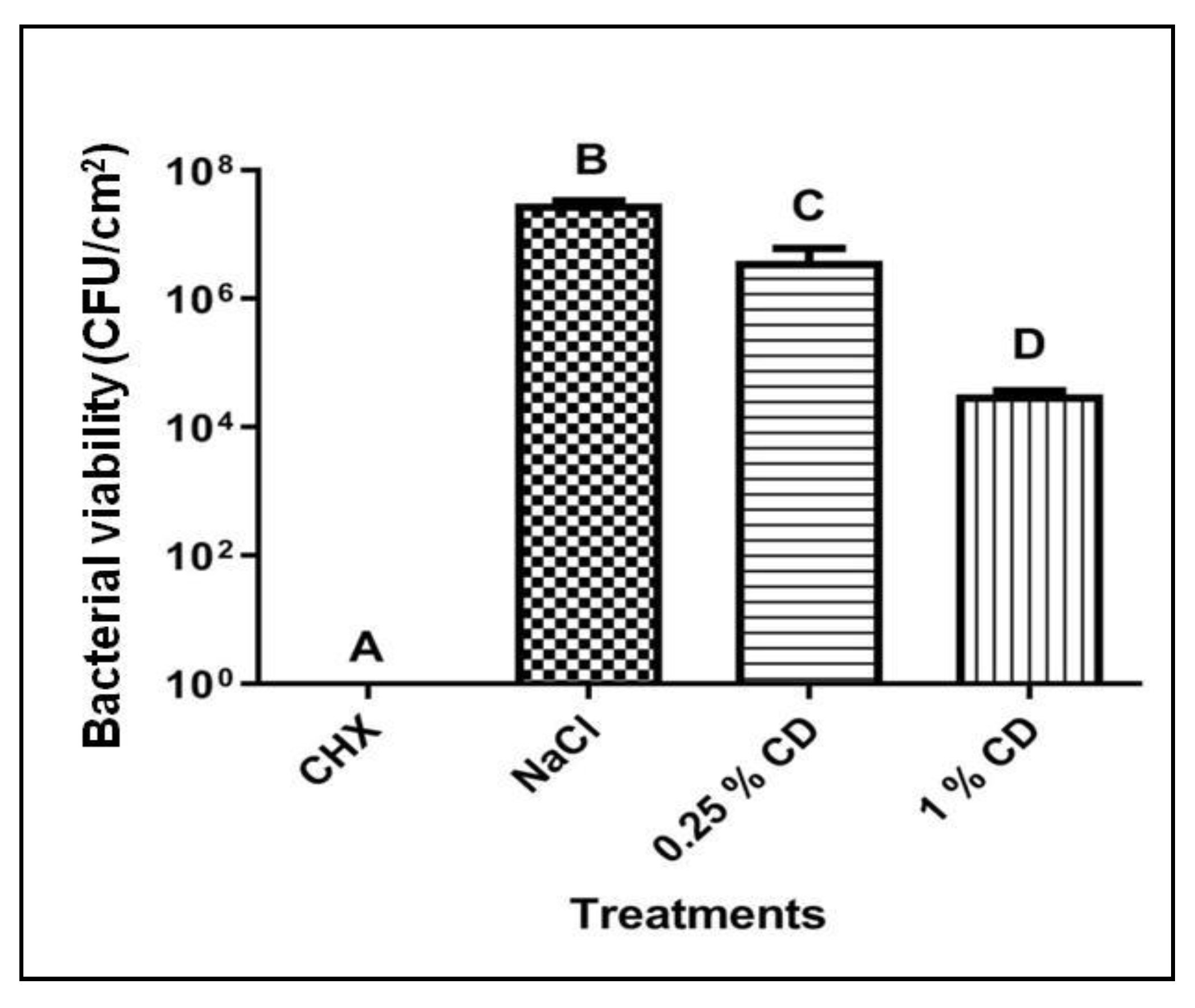
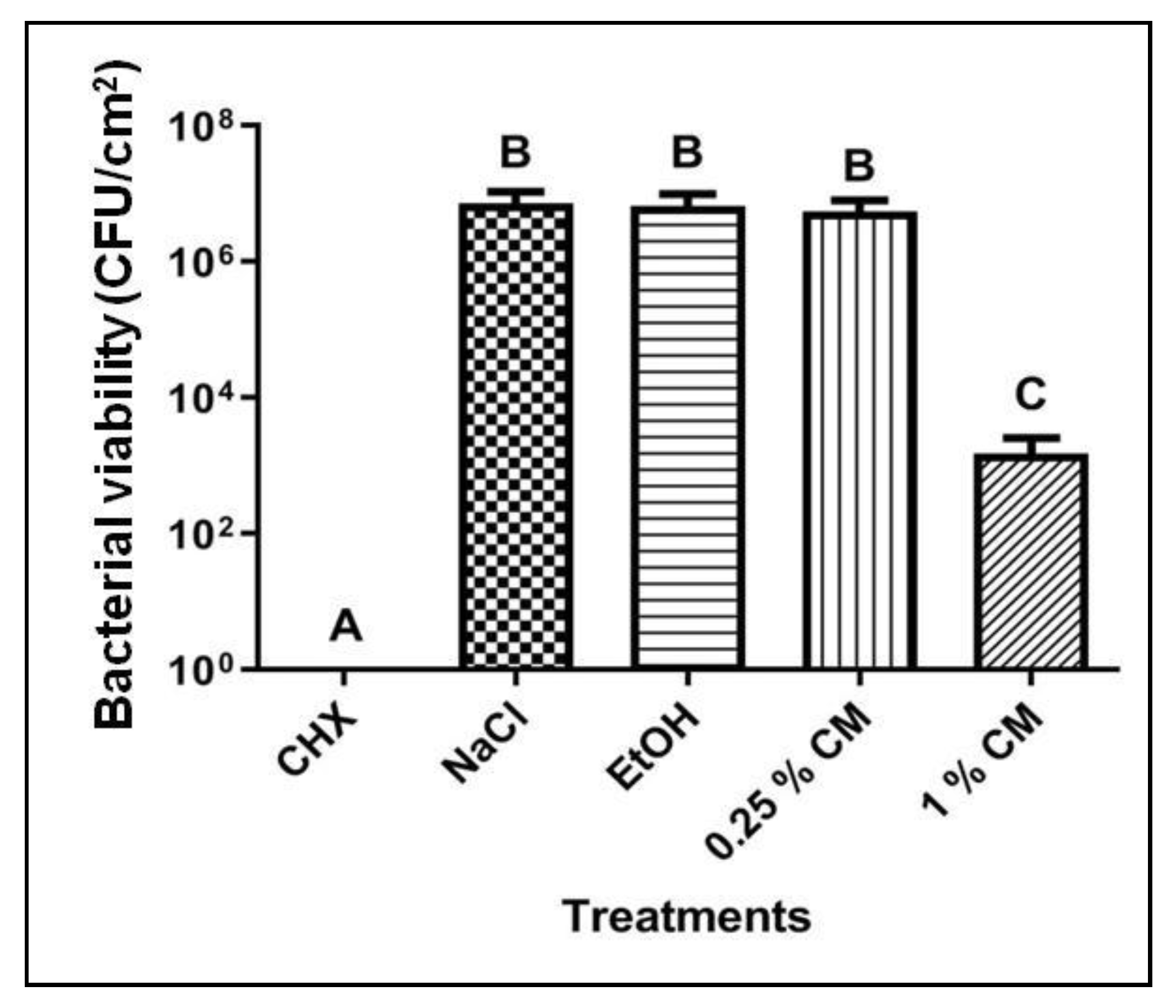
2.3. Biofilm Assay
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Chitosan Dispersion and Chitosan Microparticles: Preparation and Evaluation of Physicochemical Properties
4.3. Determination of Minimum Inhibitory and Bactericidal Concentrations
4.4. Biofilm Assay
4.5. Statistical Analysis
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kuang, X.; Chen, V.; Xu, X. Novel approaches to the control of oral microbial biofilms. Biomed. Res. Int. 2018, 2018, 6498932. [Google Scholar] [CrossRef] [PubMed]
- Sahariah, P.; Másson, M. Antimicrobial chitosan and chitosan derivatives: A review of the structure-activity relationship. Biomacromolecules 2017, 18, 3846–3868. [Google Scholar] [CrossRef] [PubMed]
- Szymańska, E.; Winnicka, K. Stability of chitosan — a challenge for pharmaceutical and biomedical applications. Mar. Drugs 2015, 13, 1819–1846. [Google Scholar] [CrossRef] [PubMed]
- Bellich, B.; D’Agostino, I.; Semeraro, S.; Gamini, A.; Cesàro, A. “The good, the bad and the ugly” of chitosans. Mar. Drugs 2016, 14. [Google Scholar] [CrossRef]
- Ardila, N.; Daigle, F.; Heuzey, M.-C.; Ajji, A. Effect of chitosan physical form on its antibacterial activity against pathogenic bacteria. J. Food. Sci. 2017, 82, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Chávez de Paz, L.E.; Resin, A.; Howard, K.A.; Sutherland, D.S.; Wejse, P.L. Antimicrobial effect of chitosan nanoparticles on Streptococcus mutans biofilms. Appl. Environ. Microbiol. 2011, 77, 3892–3895. [Google Scholar] [CrossRef]
- Sreekumar, S.; Goycoolea, F.M.; Moerschbacher, B.M.; Rivera-Rodriguez, G.R. Parameters influencing the size of chitosan-TPP nano- and microparticles. Sci. Rep. 2018, 8, 4695. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Wang, Q.; Wang, W.; Wu, J. Preparation, characterization and drug-release behaviors of crosslinked chitosan/attapulgite hybrid microspheres by a facile spray-drying technique. J. Biomater. Nanobiotechnol. 2011, 2, 250–257. [Google Scholar] [CrossRef]
- Marsh, P.D.; Head, D.A.; Devine, D.A. Ecological approaches to oral biofilms: Control without killing. Caries Res. 2015, 49 (Suppl. 1), 46–54. [Google Scholar] [CrossRef]
- Xiao, J.; Koo, H. Structural organization and dynamics of exopolysaccharide matrix and microcolonies formation by Streptococcus mutans in biofilms. J. Appl. Microbiol. 2010, 108, 2103–2113. [Google Scholar]
- Klein, M.I.; Hwang, G.; Santos, P.H.S.; Campanella, O.H.; Koo, H. Streptococcus mutans-derived extracellular matrix in cariogenic oral biofilms. Front. Cell. Infect. Microbiol. 2015, 5, 10. [Google Scholar] [CrossRef] [PubMed]
- Flemming, H.-C.; Wingender, J.; Szewzyk, U.; Steinberg, P.; Rice, S.A.; Kjelleberg, S. Biofilms: An emergent form of bacterial life. Nat. Rev. Microbiol. 2016, 14, 563–575. [Google Scholar] [CrossRef] [PubMed]
- Kostakioti, M.; Hadjifrangiskou, M.; Hultgren, S.J. Bacterial biofilms: Development, dispersal, and therapeutic strategies in the dawn of the postantibiotic era. Cold Spring Harb. Perspect. Med. 2013, 3, a010306. [Google Scholar] [CrossRef]
- Costa, E.M.; Silva, S.; Pina, C.; Tavaria, F.K.; Pintado, M.M. Evaluation and insights into chitosan antimicrobial activity against anaerobic oral pathogens. Anaerobe 2012, 18, 305–309. [Google Scholar] [CrossRef] [PubMed]
- Costa, E.M.; Silva, S.; Tavaria, F.K.; Pintado, M.M. Study of the effects of chitosan upon Streptococcus mutans adherence and biofilm formation. Anaerobe 2013, 20, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Leme, A.F.P.; Koo, H.; Bellato, C.M.; Bedi, G.; Cury, J.A. The role of sucrose in cariogenic dental biofilm formation—new insight. J. Dent. Res. 2006, 85, 878–887. [Google Scholar] [CrossRef] [PubMed]
- Krzyściak, W.; Jurczak, A.; Piątkowski, J. The role of human oral microbiome in dental biofilm formation. In Microbial Biofilms—Importance and Applications; Dhanasekaran, D., Thajuddin, N., Eds.; IntechOpen: London, UK, 2016; pp. 329–382. [Google Scholar]
- Shinkar, D.M.; Dhake, A.S.; Setty, C.M. Drug delivery from the oral cavity: A focus on mucoadhesive buccal drug delivery systems. PDA J. Pharm. Sci. Technol. 2012, 66, 466–500. [Google Scholar] [CrossRef] [PubMed]
- Stewart, P.S.; Costerton, J.W. Antibiotic resistance of bacteria in biofilms. Lancet 2001, 358, 135–138. [Google Scholar] [CrossRef]
- Younes, I.; Rinaudo, M. Chitin and chitosan preparation from marine sources. Structure, properties and applications. Mar. Drugs 2015, 13, 1133–1174. [Google Scholar] [CrossRef] [PubMed]
- Kockisch, S.; Rees, G.D.; Young, S.A.; Tsibouklis, J.; Smart, J.D. A direct-staining method to evaluate the mucoadhesion of polymers from aqueous dispersion. J. Control. Release 2001, 77, 1–6. [Google Scholar] [CrossRef]
- Pellá, M.C.G.; Lima-Tenório, M.K.; Tenório-Neto, E.T.; Guilherme, M.R.; Muniz, E.C.; Rubira, A.F. Chitosan-based hydrogels: From preparation to biomedical applications. Carbohydr. Polym. 2018, 196, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Raafat, D.; von Bargen, K.; Haas, A.; Sahl, H.-G. Insights into the mode of action of chitosan as an antibacterial compound. Appl. Environ. Microbiol. 2008, 74, 3764–3773. [Google Scholar] [CrossRef] [PubMed]
- Orgaz, B.; Lobete, M.M.; Puga, C.H.; San Jose, C. Effectiveness of chitosan against mature biofilms formed by food related bacteria. Int. J. Mol. Sci. 2011, 12, 817–828. [Google Scholar] [CrossRef] [PubMed]
- Varoni, E.; Tarce, M.; Lodi, G.; Carrassi, A. Chlorhexidine (CHX) in dentistry: State of the art. Minerva Stomatol 2012, 61, 399–419. [Google Scholar] [PubMed]
- Lim, J.H.; Song, S.-H.; Park, H.-S.; Lee, J.R.; Lee, S.-M. Spontaneous detachment of Streptococcus mutans biofilm by synergistic effect between zwitterion and sugar alcohol. Sci. Rep. 2017, 7, 8107. [Google Scholar] [CrossRef]
- Ccahuana-Vásquez, R.A.; Cury, J.A. S. mutans biofilm model to evaluate antimicrobial substances and enamel demineralization. Braz. Oral. Res. 2010, 24, 135–141. [Google Scholar] [CrossRef]
- Oliveira, B.F.; Santana, M.H.A.; Ré, M.I. Spray-dried chitosan microspheres cross-linked with d, l-glyceraldehyde as a potential drug delivery system: Preparation and characterization. Braz. J. Chem. Eng. 2005, 22, 353–360. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing: Twenty-Third Informational Supplement; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2013; ISBN 978-1-56238-865-2. [Google Scholar]
- de Queiroz, V.S.; Ccahuana-Vásquez, R.A.; Tedesco, A.F.; Lyra, L.; Cury, J.A.; Schreiber, A.Z. Influence of the culture medium in dose-response effect of the chlorhexidine on Streptococcus mutans biofilms. Scientifica 2016, 2016, 2816812. [Google Scholar] [CrossRef]
- Duarte, S.; Klein, M.I.; Aires, C.P.; Cury, J.A.; Bowen, W.H.; Koo, H. Influences of starch and sucrose on Streptococcus mutans biofilms. Oral Microbiol. Immun. 2008, 23, 206–212. [Google Scholar] [CrossRef]
- Aires, C.P.; Del Bel Cury, A.A.; Tenuta, L.M.A.; Klein, M.I.; Koo, H.; Duarte, S.; Cury, J.A. Effect of starch and sucrose on dental biofilm formation and on root dentine demineralization. Caries Res. 2008, 42, 380–386. [Google Scholar] [CrossRef]
- Herigstad, B.; Hamilton, M.; Heersink, J. How to optimize the drop plate method for enumerating bacteria. J. Microbiol. Meth. 2001, 44, 121–129. [Google Scholar] [CrossRef]
Sample Availability: Samples of the compounds are not available from the authors. |

| Parameter | Value |
|---|---|
| Particle diameter | |
| Mean size (µm) | 5.61 ± 0.57 |
| d10 (µm) | 1.56 ± 0.04 |
| d50 (µm) | 4.15 ± 0.20 |
| d90 (µm) | 10.81 ± 1.19 |
| Span | 2.22 ± 0.19 |
| Zeta potential (mV) | +58.7 ± 3.7 |
| Treatments | Streptococcus mutans UA 159 | |
|---|---|---|
| MIC (µg/mL) | MBC (µg/mL) | |
| CHX | 0.12 ± 0.0 | 0.12 ± 0.0 |
| EtOH | 307,200 ± 0.0 | - |
| CD | 5.2 ± 0.0 | 5.2 ± 0.0 |
| CM | 13.1 ± 0.0 | 13.1 ± 0.0 |
| Treatments | Time after the First Exposure (h) | ||
|---|---|---|---|
| 24 | 48 | 72 | |
| CHX | 7.1 ± 0.0 A | 7.1 ± 0.0 A | 7.4 ± 0.0 B |
| NaCl | 4.4 ± 0.0 C | 4.4 ± 0.1 C | 4.5 ± 0.0 C |
| 0.25% CD | 4.8 ± 0.1 D | 4.5 ± 0.0 C | 4.6 ± 0.1 C |
| 1% CD | 6.9 ± 0.0 A | 5.4 ± 0.2 E | 5.0 ± 0.1 F |
| Treatments | Time after the First Exposure (h) | ||
|---|---|---|---|
| 24 | 48 | 72 | |
| CHX | 6.9 ± 0.0 A, B, C | 7.1 ± 0.1 A, B | 7.3 ± 0.0 A, B |
| NaCl | 4.8 ± 0.0 D | 4.8 ± 0.1 D | 4.6 ± 0.0 D |
| EtOH | 5.8 ± 0.4 E, F | 5.4 ± 0.0 F, G | 5.0 ± 0.2 D, G |
| 0.25% CM | 6.5 ± 0.0 C | 6.1 ± 0.4 E | 5.0 ± 0.1 D, G |
| 1% CM | 7.0 ± 0.0 A, B, C | 7.1 ± 0.0 A, B | 7.3 ± 0.0 A |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawakita, E.R.H.; Ré, A.C.S.; Peixoto, M.P.G.; Ferreira, M.P.; Ricomini-Filho, A.P.; Freitas, O.; Aires, C.P. Effect of Chitosan Dispersion and Microparticles on Older Streptococcus mutans Biofilms. Molecules 2019, 24, 1808. https://doi.org/10.3390/molecules24091808
Kawakita ERH, Ré ACS, Peixoto MPG, Ferreira MP, Ricomini-Filho AP, Freitas O, Aires CP. Effect of Chitosan Dispersion and Microparticles on Older Streptococcus mutans Biofilms. Molecules. 2019; 24(9):1808. https://doi.org/10.3390/molecules24091808
Chicago/Turabian StyleKawakita, Erika R. H., Ana Carolina S. Ré, Maria Paula G. Peixoto, Maíra P. Ferreira, Antônio P. Ricomini-Filho, Osvaldo Freitas, and Carolina P. Aires. 2019. "Effect of Chitosan Dispersion and Microparticles on Older Streptococcus mutans Biofilms" Molecules 24, no. 9: 1808. https://doi.org/10.3390/molecules24091808
APA StyleKawakita, E. R. H., Ré, A. C. S., Peixoto, M. P. G., Ferreira, M. P., Ricomini-Filho, A. P., Freitas, O., & Aires, C. P. (2019). Effect of Chitosan Dispersion and Microparticles on Older Streptococcus mutans Biofilms. Molecules, 24(9), 1808. https://doi.org/10.3390/molecules24091808






