Extraction, Purification, Structural Characteristics, Biological Activities and Pharmacological Applications of Acemannan, a Polysaccharide from Aloe vera: A Review
Abstract
1. Introduction
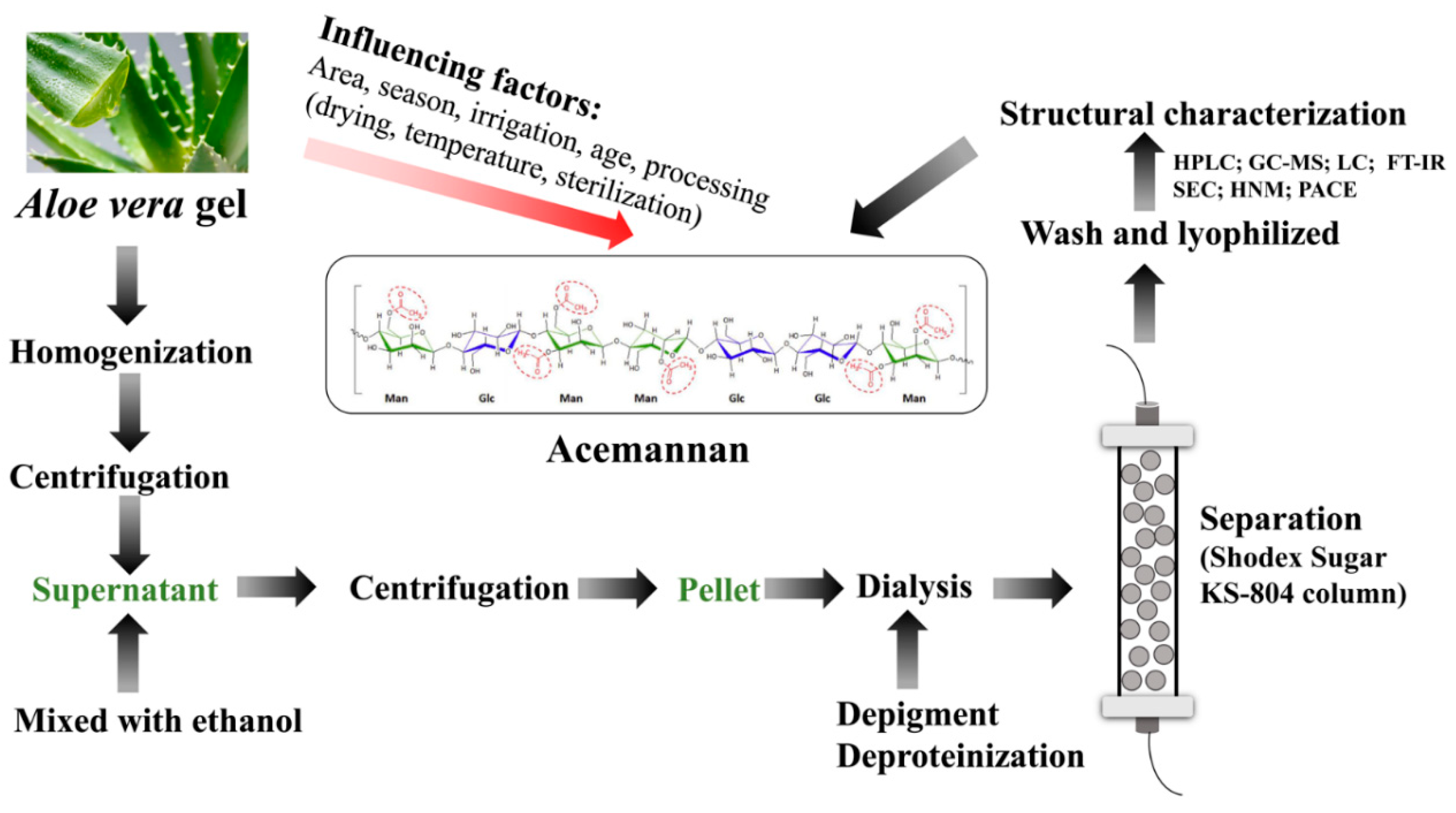
2. Extraction, Separation and Purification of Acemannan
2.1. Factors Affecting Acemannan Production and Structure
2.2. Exaction of Acemannan
2.3. Separation and Purification of Acemannan
2.4. Structural Characterization Method and Characteristics of Acemannan
3. Biological Activities of Acemannan
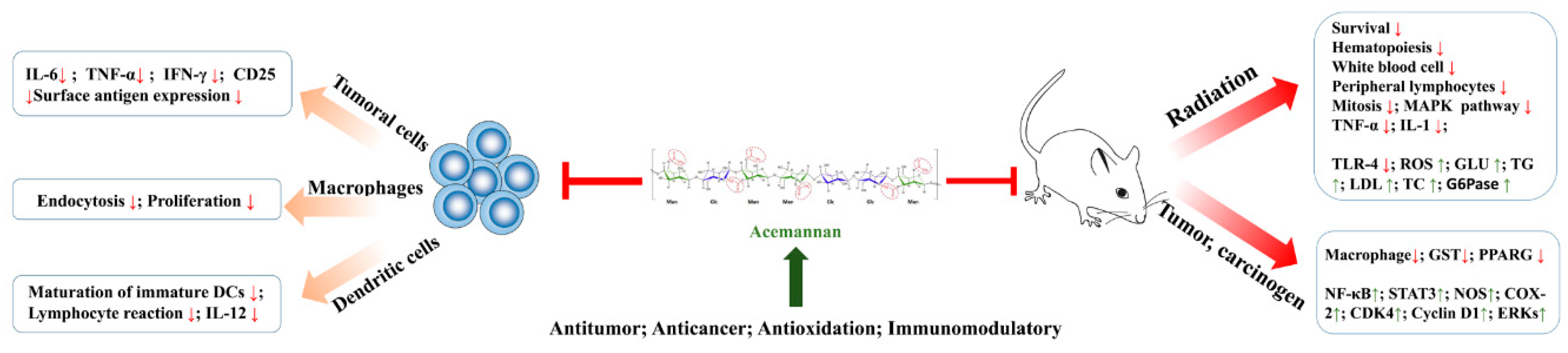
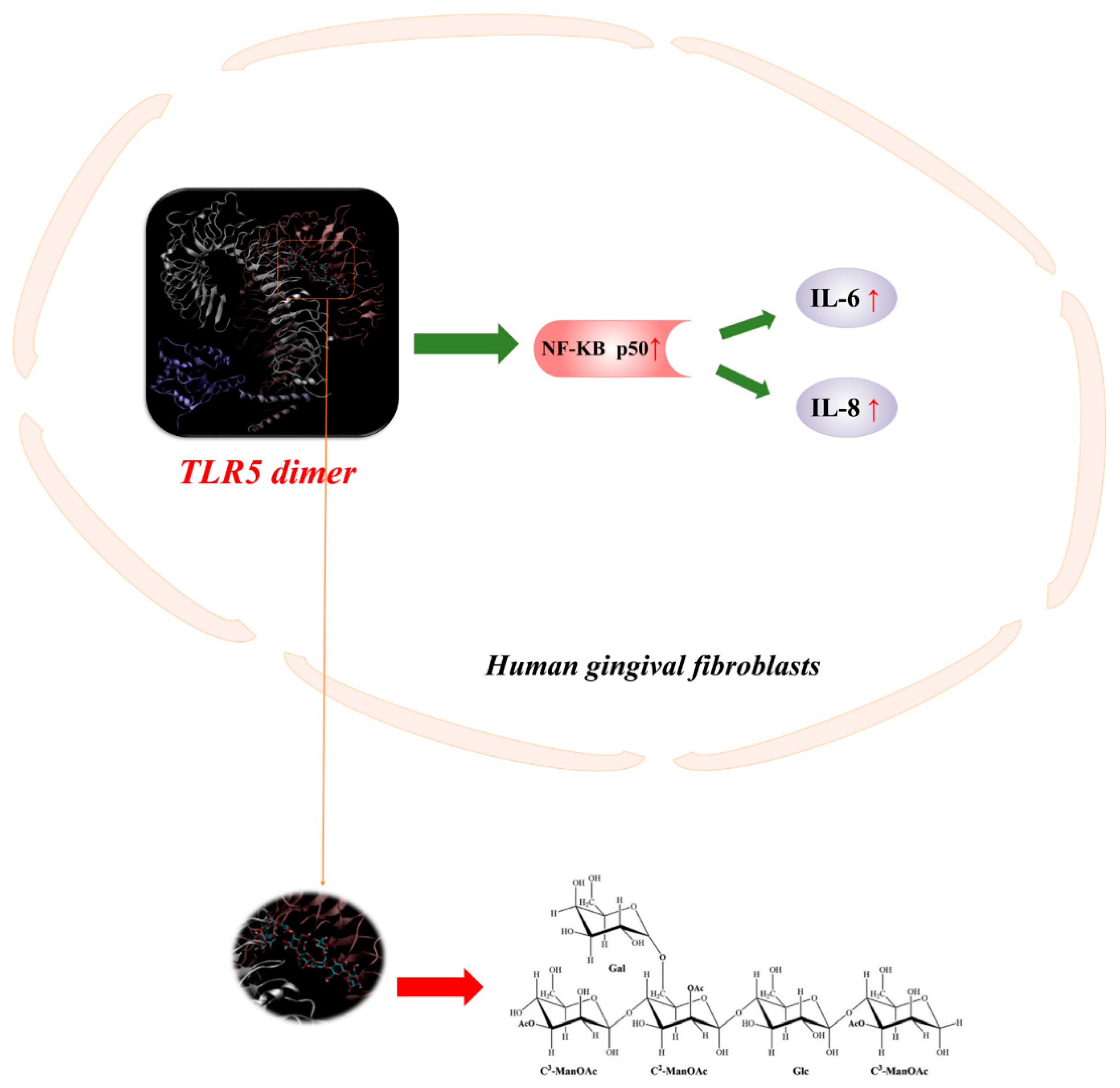
3.1. Immunomodulation Activity
3.2. Anti-Cancer Activity
3.3. Antioxidant Activity
3.4. Gastric and Intestinal Activity
3.5. Neuroprotective Activities
3.6. Hepatoprotective Effect
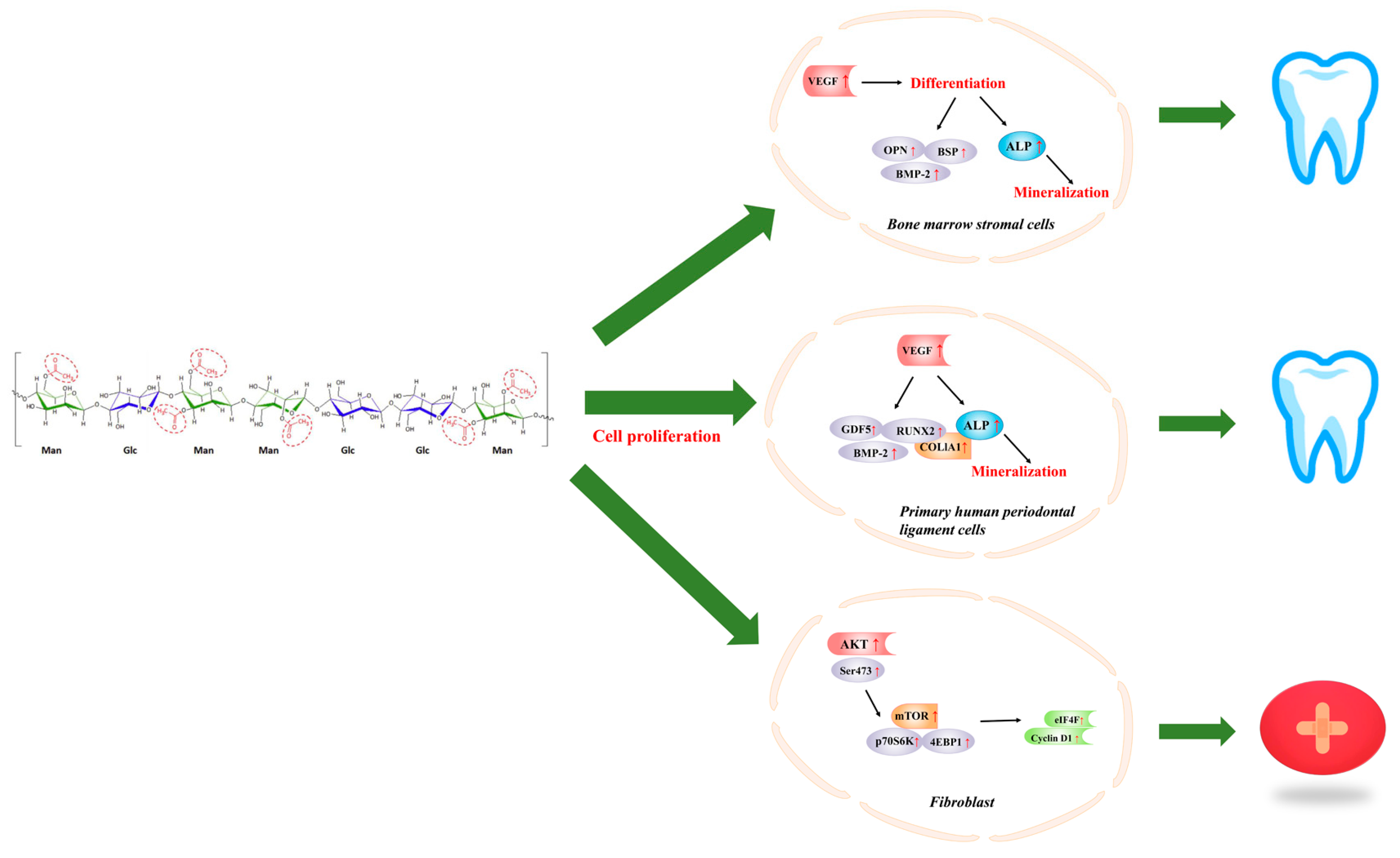
4. Acemannan in Dentistry
5. Acemannan in Wound Healing
6. Structure-Activity Relationship
7. Applications of Acemannan
8. Conclusions and Future Prospects
Author Contributions
Funding
Conflicts of Interest
References
- Li, Y.; Xu, F.; Zheng, M.; Xi, X.; Cui, X.; Han, C. Maca polysaccharides: A review of compositions, isolation, therapeutics and prospects. Int. J. Biol. Macromol. 2018, 111, 894–902. [Google Scholar] [CrossRef]
- Luiz, C.; da Rocha Neto, A.C.; Franco, P.O.; Di Piero, R.M. Emulsions of essential oils and aloe polysaccharides: Antimicrobial activity and resistance inducer potential against Xanthomonas fragariae. Trop. Plant Pathol. 2017, 42, 370–381. [Google Scholar] [CrossRef]
- Nazeam, J.A.; Gad, H.A.; Esmat, A.; El-Hefnawy, H.M.; Singab, A.-N.B. Aloe arborescens Polysaccharides: In Vitro Immunomodulation and Potential Cytotoxic Activity. J. Med. Food 2017, 20, 491–501. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.-H.; Jin, M.-L.; Morris, G.A.; Zha, X.-Q.; Chen, H.-Q.; Yi, Y.; Li, J.-E.; Wang, Z.-J.; Gao, J.; Nie, S.-P.; et al. Advances on Bioactive Polysaccharides from Medicinal Plants. Crit. Rev. Food Sci. Nutr. 2016, 56, S60–S84. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Yuan, Q.; Saeeduddin, M.; Ou, S.; Zeng, X.; Ye, H. Recent advances in tea polysaccharides: Extraction, purification, physicochemical characterization and bioactivities. Carbohydr. Polym. 2016, 153, 663–678. [Google Scholar] [CrossRef] [PubMed]
- Marhefka, J.N.; Kameneva, M.V. Natural Drag-Reducing Polymers: Discovery, Characterization and Potential Clinical Applications. Fluids 2016, 1, 6. [Google Scholar] [CrossRef]
- Jettanacheawchankit, S.; Sasithanasate, S.; Sangvanich, P.; Banlunara, W.; Thunyakitpisal, P. Acemannan Stimulates Gingival Fibroblast Proliferation; Expressions of Keratinocyte Growth Factor-1, Vascular Endothelial Growth Factor, and Type I Collagen; and Wound Healing. J. Pharmacol. Sci. 2009, 109, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Sinha, V.R.; Kumria, R. Polysaccharides in colon-specific drug delivery. Int. J. Pharm. 2001, 224, 19–38. [Google Scholar] [CrossRef]
- Rahman, S.; Carter, P.; Bhattarai, N. Aloe vera for Tissue Engineering Applications. J. Funct. Biomater. 2017, 8, 6. [Google Scholar] [CrossRef] [PubMed]
- Eshun, K.; He, Q. Aloe vera: A valuable ingredient for the food, pharmaceutical and cosmetic industries—A review. Crit. Rev. Food Sci. Nutr. 2004, 44, 91–96. [Google Scholar] [CrossRef]
- Reynolds, T.; Dweck, A.C. Aloe vera leaf gel: A review update. J. Ethnopharmacol. 1999, 68, 3–37. [Google Scholar] [CrossRef]
- Strickland, F.A. Immune regulation by polysaccharides: Implications for skin cancer. J. Photochem. Photobiol. B-Biol. 2001, 63, 132–140. [Google Scholar] [CrossRef]
- Harlev, E.; Nevo, E.; Lansky, E.P.; Ofir, R.; Bishayee, A. Anticancer Potential of Aloes: Antioxidant, Antiproliferative, and Immunostimulatory Attributes. Planta Med. 2012, 78, 843–852. [Google Scholar] [CrossRef]
- Chokboribal, J.; Tachaboonyakiat, W.; Sangvanich, P.; Ruangpornvisuti, V.; Jettanacheawchankit, S.; Thunyakitpisal, P. Deacetylation affects the physical properties and bioactivity of acemannan, an extracted polysaccharide from Aloe vera. Carbohydr. Polym. 2015, 133, 556–566. [Google Scholar] [CrossRef]
- Sierra-Garcia, G.D.; Castro-Rios, R.; Gonzalez-Horta, A.; Lara-Arias, J.; Chavez-Montes, A. Acemannan, an Extracted Polysaccharide from Aloe vera: A Literature Review. Nat. Prod. Commun. 2014, 9, 1217–1221. [Google Scholar] [CrossRef] [PubMed]
- Bhalang, K.; Thunyakitpisal, P.; Rungsirisatean, N. Acemannan, a Polysaccharide Extracted from Aloe vera, Is Effective in the Treatment of Oral Aphthous Ulceration. J. Altern. Complement. Med. 2013, 19, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Djeraba, A.; Quere, P. In vivo macrophage activation in chickens with Acemannan, a complex carbohydrate extracted from Aloe vera. Int. J. Immunopharmacol. 2000, 22, 365–372. [Google Scholar] [CrossRef]
- Lobo, R.; Prabhu, K.S.; Shirwaikar, A.; Ballal, M.; Balachandran, C.; Shirwaikar, A. A HPTLC densitometric method for the determination of aloeverose in Aloe vera gel. Fitoterapia 2010, 81, 231–233. [Google Scholar] [CrossRef]
- Songsiripradubboon, S.; Banlunara, W.; Sangvanich, P.; Trairatvorakul, C.; Thunyakitpisal, P. Clinical, radiographic, and histologic analysis of the effects of acemannan used in direct pulp capping of human primary teeth: Short-term outcomes. Odontology 2016, 104, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez Rodriguez, E.; Darias Martin, J.; Diaz Romero, C. Aloe vera as a functional ingredient in foods. Crit. Rev. Food Sci. Nutr. 2010, 50, 305–326. [Google Scholar] [CrossRef]
- Ni, Y.; Turner, D.; Yates, K.M.; Tizard, I. Isolation and characterization of structural components of Aloe vera L. leaf pulp. Int. Immunopharmacol. 2004, 4, 1745–1755. [Google Scholar] [CrossRef] [PubMed]
- Femenia, A.; Sanchez, E.S.; Simal, S.; Rossello, C. Compositional features of polysaccharides from Aloe vera (Aloe barbadensis Miller) plant tissues. Carbohydr. Polym. 1999, 39, 109–117. [Google Scholar] [CrossRef]
- Femenia, A.; Garcia-Pascual, P.; Simal, S.; Rossello, C. Effects of heat treatment and dehydration on bioactive polysaccharide acemannan and cell wall polymers from Aloe barbadensis Miller. Carbohyd. Polym. 2003, 51, 397–405. [Google Scholar] [CrossRef]
- Lucini, L.; Pellizzoni, M.; Molinari, G.P. Anthraquinones and beta-polysaccharides content and distribution in Aloe plants grown under different light intensities. Biochem. Syst. Ecol. 2013, 51, 264–268. [Google Scholar] [CrossRef]
- Minjares-Fuentes, R.; Medina-Torres, L.; Francisco Gonzalez-Laredo, R.; Manuel Rodriguez-Gonzalez, V.; Eim, V.; Femenia, A. Influence of water deficit on the main polysaccharides and the rheological properties of Aloe vera (Aloe barbadensis Miller) mucilage. Ind. Crops Prod. 2017, 109, 644–653. [Google Scholar] [CrossRef]
- Jiang, C.-Q.; Quan, L.-T.; Shi, F.; Yang, N.; Wang, C.-H.; Yin, X.-M.; Zheng, Q.-S. Distribution of Mineral Nutrients and Active Ingredients in Aloe vera Irrigated with Diluted Seawater. Pedosphere 2014, 24, 722–730. [Google Scholar] [CrossRef]
- Ray, A.; Aswatha, S.M. An analysis of the influence of growth periods on physical appearance, and acemannan and elemental distribution of Aloe vera L. gel. Ind. Crops Prod. 2013, 48, 36–42. [Google Scholar] [CrossRef]
- Minjares-Fuentes, R.; Rodriguez-Gonzalez, V.M.; Gonzalez-Laredo, R.F.; Eim, V.; Gonzalez-Centeno, M.R.; Femenia, A. Effect of different drying procedures on the bioactive polysaccharide acemannan from Aloe vera (Aloe barbadensis Miller). Carbohydr. Polym. 2017, 168, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Sriariyakul, W.; Swasdisevi, T.; Devahastin, S.; Soponronnarit, S. Drying of Aloe vera puree using hot air in combination with far-infrared radiation and high-voltage electric field: Drying kinetics, energy consumption and product quality evaluation. Food Bioprod. Process. 2016, 100, 391–400. [Google Scholar] [CrossRef]
- Rodriguez-Gonzalez, V.M.; Femenia, A.; Gonzalez-Laredo, R.F.; Rocha-Guzman, N.E.; Gallegos-Infante, J.A.; Candelas-Cadillo, M.G.; Ramirez-Baca, P.; Simal, S.; Rossello, C. Effects of pasteurization on bioactive polysaccharide acemannan and cell wall polymers from Aloe barbadensis Miller. Carbohydr. Polym. 2011, 86, 1675–1683. [Google Scholar] [CrossRef]
- Manna, S.; McAnalley, B.H. Determination of the position of the O-acetyl group in a beta-(1-->4)-mannan (acemannan) from Aloe barbardensis Miller. Carbohydr. Res. 1993, 241, 317–319. [Google Scholar] [CrossRef]
- Salinas, P.; Salinas, C.; Contreras, R.A.; Zuniga, G.E.; Dupree, P.; Cardemil, L. Water deficit and abscisic acid treatments increase the expression of a glucomannan mannosyltransferase gene (GMMT) in Aloe vera Burm. F. Phytochemistry 2018, 159, 90–101. [Google Scholar] [CrossRef] [PubMed]
- Thunyakitpisal, P.; Ruangpornvisuti, V.; Kengkwasing, P.; Chokboribal, J.; Sangvanich, P. Acemannan increases NF-kappa B/DNA binding and IL-6/-8 expression by selectively binding Toll-like receptor-5 in human gingival fibroblasts. Carbohydr. Polym. 2017, 161, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Gulia, A.; Sharma, H.K.; Sarkar, B.C.; Upadhyay, A.; Shitandi, A. Changes in physico-chemical and functional properties during convective drying of aloe vera (Aloe barbadensis) leaves. Food Bioprod. Process. 2010, 88, 161–164. [Google Scholar] [CrossRef]
- Lim, Z.X.; Cheong, K.Y. Effects of drying temperature and ethanol concentration on bipolar switching characteristics of natural Aloe vera-based memory devices. Phys. Chem. Chem. Phys. 2015, 17, 26833–26853. [Google Scholar] [CrossRef] [PubMed]
- Mary, S.A.; Dev, V.R.G. Electrospun herbal nanofibrous wound dressings for skin tissue engineering. J. Text. Inst. 2015, 106, 886–895. [Google Scholar] [CrossRef]
- Im, S.A.; Oh, S.T.; Song, S.; Kim, M.R.; Kim, D.S.; Woo, S.S.; Jo, T.H.; Park, Y.I.; Lee, C.K. Identification of optimal molecular size of modified Aloe polysaccharides with maximum immunomodulatory activity. Int. Immunopharmacol. 2005, 5, 271–279. [Google Scholar] [CrossRef]
- Chang, X.-L.; Xu, H.; Wang, J.-J.; Wang, W.-H.; Feng, Y.-M. Research on Water Soluble Polysaccharides Separated from Skin Juice, Gel Juice and Flower of Aloe ferox Miller. Food Sci. Technol. Res. 2013, 19, 901–907. [Google Scholar] [CrossRef][Green Version]
- Chang, X.L.; Feng, Y.M.; Wang, W.H. Comparison of the polysaccharides isolated from skin juice, gel juice and flower of Aloe arborescens tissues. J. Taiwan Inst. Chem. Eng. 2011, 42, 13–19. [Google Scholar] [CrossRef]
- Chang, X.L.; Chen, B.Y.; Feng, Y.M. Water-soluble polysaccharides isolated from skin juice, gel juice and flower of Aloe vera Miller. J. Taiwan Inst. Chem. Eng. 2011, 42, 197–203. [Google Scholar] [CrossRef]
- Xing, J.-M.; Li, F.-F. Separation and purification of aloe polysaccharides by a combination of membrane ultrafiltration and aqueous two-phase extraction. Appl. Biochem. Biotechnol. 2009, 158, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K.; Lee, M.K.; Yun, Y.P.; Kim, Y.; Kim, J.S.; Kim, Y.S.; Kim, K.; Han, S.S.; Lee, C.K. Acemannan purified from Aloe vera induces phenotypic and functional maturation of immature dendritic cells. Int. Immunopharmacol. 2001, 1, 1275–1284. [Google Scholar] [CrossRef]
- Chumpol, J.; Siri, S. Electrospun cellulose acetate membrane for size separating and antibacterial screening of crude polysaccharides. IET Nanobiotechnol. 2016, 10, 405–410. [Google Scholar] [CrossRef] [PubMed]
- Leung, M.Y.; Liu, C.; Zhu, L.F.; Hui, Y.Z.; Yu, B.; Fung, K.P. Chemical and biological characterization of a polysaccharide biological response modifier from Aloe vera L. var. chinensis (Haw.) Berg. Glycobiology 2004, 14, 501–510. [Google Scholar] [CrossRef]
- Shi, X.-D.; Nie, S.-P.; Yin, J.-Y.; Que, Z.-Q.; Zhang, L.-J.; Huang, X.-J. Polysaccharide from leaf skin of Aloe barbadensis Miller: Part I. Extraction, fractionation, physicochemical properties and structural characterization. Food Hydrocolloid 2017, 73, 176–183. [Google Scholar] [CrossRef]
- Boonyagul, S.; Banlunara, W.; Sangvanich, P.; Thunyakitpisal, P. Effect of acemannan, an extracted polysaccharide from Aloe vera, on BMSCs proliferation, differentiation, extracellular matrix synthesis, mineralization, and bone formation in a tooth extraction model. Odontology 2014, 102, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.-D.; Yin, J.-Y.; Huang, X.-J.; Que, Z.-Q.; Nie, S.-P. Structural and conformational characterization of linear O-acetyl-glucomannan purified from gel of Aloe barbadensis Miller. Int. J. Biol. Macromol. 2018, 120, 2373–2380. [Google Scholar] [CrossRef] [PubMed]
- Salinas, C.; Handford, M.; Pauly, M.; Dupree, P.; Cardemil, L. Structural Modifications of Fructans in Aloe barbadensis Miller (Aloe vera) Grown under Water Stress. PLoS ONE 2016, 11, e0159819. [Google Scholar] [CrossRef]
- Simoes, J.; Nunes, F.M.; Domingues, P.; Coimbra, M.A.; Domingues, M.R. Mass spectrometry characterization of an Aloe vera mannan presenting immunostimulatory activity. Carbohydr. Polym. 2012, 90, 229–236. [Google Scholar] [CrossRef]
- Davis, B.; Goux, W.J. Single-Laboratory Validation of an NMR Method for the Determination of Aloe vera Polysaccharide in Pharmaceutical Formulations. J. AOAC Int. 2009, 92, 1607–1616. [Google Scholar]
- Kiran, P.; Rao, P.S. Development and characterization of reconstituted hydrogel from Aloe vera (Aloe barbadensis Miller) powder. J. Food Meas. Charact. 2016, 10, 411–424. [Google Scholar] [CrossRef]
- Zhang, Y.; Bao, Z.; Ye, X.; Xie, Z.; He, K.; Mergens, B.; Li, W.; Yatcilla, M.; Zheng, Q. Chemical Investigation of Major Constituents in Aloe vera Leaves and Several Commercial Aloe Juice Powders. J. AOAC Int. 2018, 101, 1741–1751. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Kumar, R. Role of acemannan O-acetyl group in murine radioprotection. Carbohydr. Polym. 2019, 207, 460–470. [Google Scholar] [CrossRef]
- Talmadge, J.; Chavez, J.; Jacobs, L.; Munger, C.; Chinnah, T.; Chow, J.T.; Williamson, D.; Yates, K. Fractionation of Aloe vera L. inner gel, purification and molecular profiling of activity. Int. Immunopharmacol. 2004, 4, 1757–1773. [Google Scholar] [CrossRef] [PubMed]
- Yagi, A.; Hamada, K.; Mihashi, K.; Harada, N.; Nishioka, I. Structure determination of polysaccharides in Aloe saponaria (Hill.) Haw. (Liliaceae). J. Pharm. Sci. 1984, 73, 62–65. [Google Scholar] [CrossRef] [PubMed]
- Radjabi-Nassab, F.; Ramiliarison, C.; Monneret, C.; Vilkas, E. Further studies of the glucomannan from Aloe vahombe (liliaceae). II. Partial hydrolyses and NMR 13C studies. Biochimie 1984, 66, 563–567. [Google Scholar] [CrossRef]
- Vilkas, E.; Radjabi-Nassab, F. The glucomannan system from Aloe vahombe (liliaceae). III. Comparative studies on the glucomannan components isolated from the leaves. Biochimie 1986, 68, 1123–1127. [Google Scholar] [CrossRef]
- Steenkamp, V.; Stewart, M.J. Medicinal applications and toxicological activities of Aloe products. Pharm. Biol. 2007, 45, 411–420. [Google Scholar] [CrossRef]
- Shi, X.-D.; Yin, J.-Y.; Zhang, L.-J.; Li, O.-Y.; Huang, X.-J.; Nie, S.-P. Studies on polysaccharides from leaf skin of Aloe barbadensis Miller: Part II. Structural characteristics and molecular properties of two lower molecular weight fractions. Food Hydrocolloid. 2019, 86, 50–61. [Google Scholar] [CrossRef]
- Tai-Nin Chow, J.; Williamson, D.A.; Yates, K.M.; Goux, W.J. Chemical characterization of the immunomodulating polysaccharide of Aloe vera L. Carbohydr. Res. 2005, 340, 1131–1142. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Tiku, A.B. Immunomodulatory potential of acemannan (polysaccharide from Aloe vera) against radiation induced mortality in Swiss albino mice. Food Agric. Immunol. 2016, 27, 72–86. [Google Scholar] [CrossRef]
- Paz Quezada, M.; Salinas, C.; Gotteland, M.; Cardemil, L. Acemannan and Fructans from Aloe vera (Aloe barbadensis Miller) Plants as Novel Prebiotics. J. Agric. Food Chem. 2017, 65, 10029–10039. [Google Scholar] [CrossRef] [PubMed]
- Christaki, E.V.; Florou-Paneri, P.C. Aloe vera: A plant for many uses. J. Food Agric. Environ. 2010, 8, 245–249. [Google Scholar]
- Womble, D.; Helderman, J.H. Enhancement of allo-responsiveness of human lymphocytes by acemannan (Carrisyn). Int. J. Immunopharmacol. 1988, 10, 967–974. [Google Scholar] [CrossRef]
- Tsang, M.S.; Cheng, S.W.; Zhu, J.; Atli, K.; Chan, B.C.; Liu, D.; Chan, H.Y.; Sun, X.; Chu, I.M.; Hon, K.L.; et al. Anti-Inflammatory Activities of Pentaherbs formula and Its Influence on Gut Microbiota in Allergic Asthma. Molecules 2018, 23, 2776. [Google Scholar] [CrossRef]
- Cesta, M.F. Normal structure, function, and histology of the spleen. Toxicol Pathol. 2006, 34, 455–465. [Google Scholar] [CrossRef]
- Egger, S.F.; Brown, G.S.; Kelsey, L.S.; Yates, K.M.; Rosenberg, L.J.; Talmadge, J.E. Studies on optimal dose and administration schedule of a hematopoietic stimulatory beta-(1,4)-linked mannan. Int. J. Immunopharmacol. 1996, 18, 113–126. [Google Scholar] [CrossRef]
- Guilliams, M.; Ginhoux, F.; Jakubzick, C.; Naik, S.H.; Onai, N.; Schraml, B.U.; Segura, E.; Tussiwand, R.; Yona, S. Dendritic cells, monocytes and macrophages: A unified nomenclature based on ontogeny. Nat. Rev. Immunol. 2014, 14, 571–578. [Google Scholar] [CrossRef]
- Stuart, R.W.; Lefkowitz, D.L.; Lincoln, J.A.; Howard, K.; Gelderman, M.P.; Lefkowitz, S.S. Upregulation of phagocytosis and candidicidal activity of macrophages exposed to the immunostimulant acemannan. Int. J. Immunopharmacol. 1997, 19, 75–82. [Google Scholar] [CrossRef]
- Zhang, L.; Tizard, I.R. Activation of a mouse macrophage cell line by acemannan: The major carbohydrate fraction from Aloe vera gel. Immunopharmacology 1996, 35, 119–128. [Google Scholar] [CrossRef]
- Geissmann, F.; Manz, M.G.; Jung, S.; Sieweke, M.H.; Merad, M.; Ley, K. Development of monocytes, macrophages, and dendritic cells. Science 2010, 327, 656–661. [Google Scholar] [CrossRef]
- McLean, M.H.; Andrews, C.; Hanson, M.L.; Baseler, W.A.; Anver, M.R.; Senkevitch, E.; Staniszewska, A.K.; Smith, C.; Davies, L.C.; Hixon, J.; et al. Interleukin-27 Is a Potential Rescue Therapy for Acute Severe Colitis Through Interleukin-10-Dependent, T-Cell-Independent Attenuation of Colonic Mucosal Innate Immune Responses. Inflamm. Bowel Dis. 2017, 23, 1983–1995. [Google Scholar] [CrossRef]
- Axelrad, J.E.; Lichtiger, S.; Yajnik, V. Inflammatory bowel disease and cancer: The role of inflammation, immunosuppression, and cancer treatment. World J. Gastroenterol. 2016, 22, 4794–4801. [Google Scholar] [CrossRef] [PubMed]
- Karaca, K.; Sharma, J.M.; Nordgren, R. Nitric oxide production by chicken macrophages activated by Acemannan, a complex carbohydrate extracted from Aloe vera. Int. J. Immunopharmacol. 1995, 17, 183–188. [Google Scholar] [CrossRef]
- Im, S.-A.; Kim, J.-W.; Kim, H.-S.; Park, C.-S.; Shin, E.; Do, S.-G.; Park, Y.I.; Lee, C.-K. Prevention of azoxymethane/dextran sodium sulfate-induced mouse colon carcinogenesis by processed Aloe vera gel. Int. Immunopharmacol. 2016, 40, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Sampedro, M.C.; Artola, R.L.; Murature, M.; Murature, D.; Ditamo, Y.; Roth, G.A.; Kivatinitz, S. Mannan from Aloe saponaria inhibits tumoral cell activation and proliferation. Int. Immunopharmacol. 2004, 4, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Leung, M.Y.; Koon, J.C.; Zhu, L.F.; Hui, Y.Z.; Yu, B.; Fung, K.P. Macrophage activation by polysaccharide biological response modifier isolated from Aloe vera L. var. chinensis (Haw.) Berg. Int. Immunopharmacol. 2006, 6, 1634–1641. [Google Scholar] [CrossRef]
- Tello, C.G.; Ford, P.; Iacopino, A.M. In vitro evaluation of complex carbohydrate denture adhesive formulations. Quintessence Int. 1998, 29, 585–593. [Google Scholar]
- Bozzi, A.; Perrin, C.; Austin, S.; Vera, F.A. Quality and authenticity of commercial Aloe vera gel powders. Food Chem. 2007, 103, 22–30. [Google Scholar] [CrossRef]
- Salah, F.; El Ghoul, Y.; Mandhi, A.; Majdoub, H.; Jarroux, N.; Sakli, F. Effect of the deacetylation degree on the antibacterial and antibiofilm activity of acemannan from Aloe vera. Ind. Crops Prod. 2017, 103, 13–18. [Google Scholar] [CrossRef]
- Wang, J.; Hu, S.; Nie, S.; Yu, Q.; Xie, M. Reviews on Mechanisms of In Vitro Antioxidant Activity of Polysaccharides. Oxid. Med. Cell. Longev. 2016, 2016, 5692852. [Google Scholar] [CrossRef]
- Cui, Y.; Ye, Q.; Wang, H.; Li, Y.; Yao, W.; Qian, H. Hepatoprotective potential of Aloe vera polysaccharides against chronic alcohol-induced hepatotoxicity in mice. J. Sci. Food Agric. 2014, 94, 1764–1771. [Google Scholar] [CrossRef]
- Kim, H.S.; Lee, B.M. Inhibition of benzo a pyrene-DNA adduct formation by Aloe barbadensis Miller. Carcinogenesis 1997, 18, 771–776. [Google Scholar] [CrossRef] [PubMed]
- Chantarawaratit, P.; Sangvanich, P.; Banlunara, W.; Soontornvipart, K.; Thunyakitpisal, P. Acemannan sponges stimulate alveolar bone, cementum and periodontal ligament regeneration in a canine class II furcation defect model. J. Periodontal Res. 2014, 49, 164–178. [Google Scholar] [CrossRef] [PubMed]
- Jittapiromsak, N.; Sahawat, D.; Banlunara, W.; Sangvanich, P.; Thunyakitpisal, P. Acemannan, an Extracted Product from Aloe vera, Stimulates Dental Pulp Cell Proliferation, Differentiation, Mineralization, and Dentin Formation. Tissue Eng. Part. A 2010, 16, 1997–2006. [Google Scholar] [CrossRef] [PubMed]
- Songsiripradubboon, S.; Kladkaew, S.; Trairatvorakul, C.; Sangvanich, P.; Soontornvipart, K.; Banlunara, W.; Thunyakitpisal, P. Stimulation of Dentin Regeneration by Using Acemannan in Teeth with Lipopolysaccharide-induced Pulp Inflammation. J. Endod. 2017, 43, 1097–1103. [Google Scholar] [CrossRef]
- Xing, W.; Guo, W.; Zou, C.-H.; Fu, T.-T.; Li, X.-Y.; Zhu, M.; Qi, J.-H.; Song, J.; Dong, C.-H.; Li, Z.; et al. Acemannan accelerates cell proliferation and skin wound healing through AKT/mTOR signaling pathway. J. Dermatol. Sci. 2015, 79, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Godoy, D.J.D.; Chokboribal, J.; Pauwels, R.; Banlunara, W.; Sangvanich, P.; Jaroenporn, S.; Thunyakitpisal, P. Acemannan increased bone surface, bone volume, and bone density in a calvarial defect model in skeletally-mature rats. J. Dent. Sci. 2018, 13, 334–341. [Google Scholar] [CrossRef]
- Presley, L.L.; Wei, B.; Braun, J.; Borneman, J. Bacteria associated with immunoregulatory cells in mice. Appl. Environ. Microbiol. 2010, 76, 936–941. [Google Scholar] [CrossRef]
- Fernandez, J.; Moreno, F.J.; Olano, A.; Clemente, A.; Villar, C.J.; Lombo, F. A Galacto-Oligosaccharides Preparation Derived from Lactulose Protects against Colorectal Cancer Development in an Animal Model. Front. Microbiol. 2018, 9, 2004. [Google Scholar] [CrossRef]
- Best, T.; Howe, P.; Bryan, J.; Buckley, J.; Scholey, A. Acute effects of a dietary non-starch polysaccharide supplement on cognitive performance in healthy middle-aged adults. Nutr. Neurosci. 2015, 18, 76–86. [Google Scholar] [CrossRef] [PubMed]
- Costa, C.R.; Amorim, B.R.; de Magalhaes, P.; De Luca Canto, G.; Acevedo, A.C.; Guerra, E.N. Effects of Plants on Osteogenic Differentiation and Mineralization of Periodontal Ligament Cells: A Systematic Review. Phytother. Res. 2016, 30, 519–531. [Google Scholar] [CrossRef]
- Jansisyanont, P.; Tiyapongprapan, S.; Chuenchompoonut, V.; Sangvanich, P.; Thunyakitpisal, P. The effect of acemannan sponges in post-extraction socket healing: A randomized trial. J. Oral Maxil. Surg. Med. Pat. 2016, 28, 105–110. [Google Scholar] [CrossRef]
- Singer, A.J.; Clark, R.A. Cutaneous wound healing. N. Engl. J. Med. 1999, 341, 738–746. [Google Scholar] [CrossRef]
- Davis, F.M.; Kimball, A.; denDekker, A.; Joshi, A.D.; Boniakowski, A.E.; Nysz, D.; Allen, R.M.; Obi, A.; Singer, K.; Henke, P.K.; et al. Histone Methylation Directs Myeloid TLR4 Expression and Regulates Wound Healing following Cutaneous Tissue Injury. J. Immunol. 2019, 202, 1777–1785. [Google Scholar] [CrossRef]
- Plemons, J.M.; Rees, T.D.; Binnie, W.H.; Wright, J.M.; Guo, I.; Hall, J.E. Evaluation of Acemannan in the Treatment of Recurrent Aphthous Stomatitis. Wounds 1994, 6, 40–45. [Google Scholar]
- Hamman, J.H. Composition and applications of Aloe vera leaf gel. Molecules 2008, 13, 1599–1616. [Google Scholar] [CrossRef]
- Singab, A.-N.B.; El-Hefnawy, H.M.; Esmat, A.; Gad, H.A.; Nazeam, J.A. A Systemic Review on Aloe arborescens Pharmacological Profile: Biological Activities and Pilot Clinical Trials. Phytother. Res. 2015, 29, 1858–1867. [Google Scholar] [CrossRef]
- Minjares-Fuentes, R.; Femenia, A.; Comas-Serra, F.; Rossello, C.; Rodriguez-Gonzalez, V.M.; Gonzalez-Laredo, R.F.; Gallegos-Infante, J.A.; Medina-Torres, L. Effect of different drying procedures on physicochemical properties and flow behavior of Aloe vera (Aloe barbadensis Miller) gel. LWT-Food Sci. Technol. 2016, 74, 378–386. [Google Scholar] [CrossRef]
- Tummalapalli, M.; Berthet, M.; Verrier, B.; Deopura, B.L.; Alam, M.S.; Gupta, B. Composite wound dressings of pectin and gelatin with aloe vera and curcumin as bioactive agents. Int. J. Biol. Macromol. 2016, 82, 104–113. [Google Scholar] [CrossRef]
- Liang, G.; Chen, C.; Liu, C.; Sun, D. Preparation and properties evaluation of aloe polysaccharide/bacterial cellulose composite membrane as wound dressings. Appl. Chem. Ind. 2017, 46, 1761–1765. [Google Scholar]
- Pinzon, M.I.; Garcia, O.R.; Villa, C.C. The influence of Aloe vera gel incorporation on the physicochemical and mechanical properties of banana starch-chitosan edible films. J. Sci. Food Agric. 2018, 98, 4042–4049. [Google Scholar] [CrossRef] [PubMed]
- Yeren Escobedo-Lozano, A.; Domard, A.; Velazquez, C.A.; Goycoolea, F.M.; Argueelles-Monal, W.M. Physical properties and antibacterial activity of chitosan/acemannan mixed systems. Carbohydr. Polym. 2015, 115, 707–714. [Google Scholar] [CrossRef]
- Darabighane, B.; Nahashon, S.N. A review on effects of Aloe vera as a feed additive in broiler chicken diets. Ann. Anim. Sci. 2014, 14, 491–500. [Google Scholar]
- Chiodelli, G.; Pellizzoni, M.; Ruzickova, G.; Lucini, L. Effect of Different Aloe Fractions on the Growth of Lactic Acid Bacteria. J. Food Sci. 2017, 82, 219–224. [Google Scholar] [CrossRef] [PubMed]
| Source | Extraction, Fractionation, Purification | Structural Characterization Method | MW (kDa) | Monosaccharide Composition | Structural Feature | Yield | Reference |
|---|---|---|---|---|---|---|---|
| Fresh gel | Water extraction (Homogenization, centrifugation mixed with 3 volumes of ethanol, lyophilization) | LC; FT-IR; SEC; 1H-NMR | 190–220 | Man: Glc: Gal = 57:22:17 | O-(Acetyl-d-Manp)-O-(acetyl-d-Manp)-O-(d-Glap)-O-(acetyl-d-Man) | --- | [14] |
| Fresh gel | Water extraction; separation (Shodex Sugar KS-804 column) | 13C-NMR; SEM 1H-NMR; FT-IR | 150-190 | Man: Glc: Gal = 65:17:17 | Single-branched galactose at C6 of the second acetylated mannose residue | 0.04% | [33] |
| Frozen gel | Ultrafiltration cell membrane (Fractionated by ultrafiltration cell with MW cut-off membrane) | HPLC (BIOSEP SECH400 column); GC (SP2330 glass-capillary column); 1H-NMR; IR | >500 | Man: Glc = 97:3 | Galp-(1→residues link to O-2, O-3, or O-6 of →4)-β-Manp-(1→ residues, with ∽16→4)-β-Manp-(1→ residues between the side chains | 2% | [42] |
| Fresh gel | Water extraction; separation (homogenization, centrifugation, alcohol precipitation, dialysis, lyophilization) | HPLC (Shodex Sugar KS-804 column); GC–MS; 13C-NMR | ≥800 | Man (77.18%); Glc (15.3%); Gal (4.9%); Ara (0.7%); Rha (0.2%); Fuc (0.34%); Xyl (0.7%) | β-(1→4) | 0.2% | [46] |
| Fresh gel (1 year old) | Water extraction (Homogenization, centrifugation with 80% v/v alcohol, ammonium sulfate precipitation, lyophilization) | GC-MS; SEC; 13C-NMR | 1100 | Man: Glc = 15:1 | O-2, O-3, and O-6 of→4)- β-Manp-(1→residues to single α-Galp-(1→side chains | --- | [47] |
| Fresh gel | Water extraction; (Homogenization, centrifugation mixed with 3 volumes of ethanol, wash with ethanol, lyophilization) | HPGPC; FTIR; GLC-MS; TGA | 1020 | Mannose (84.9%): glucose (7.2%); galactose (3.9%) | (1→4)-Linked mannose/glucose 2,3,6-tri-O-acetyl-mannose,2,6-di-O-acetylglucose,6-acetyl-O-glucose, 3,6-di-O-acetyl-glucose | --- | [53] |
| Frozen gel | Water extraction (Homogenization, centrifugation, alcohol precipitation, lyophilization) | GC–MS; Ion-chromatograph; 13C-NMR | 1100 | Man: Glc: Gal: GalA: Fuc: Ara: Xyl = 120:9:6:3:2:2:1 | →4)-β-Manp-(1→ and →4)-β-Glcp-(1→ residues in 15:1 ratio | --- | [60] |
| Fresh gel (3 years old)) | Water extraction (Homogenization, centrifugation, supernatant mixed with 3 volumes of ethanol, pellet) | FACE; FT-IR; SEC | 281 | Man (62.9%); Glc (13.1%); Gal (0.6%) | --- | 1.7% | [61] |
| Frozen gel | Water extraction; (depigmentation, deproteinization) | CR; GC-MS; PACE | --- | Man (86.87%); Glc (0.05%); Gal (12.68%); Ara (0.38%) | β-(1→4) | 0.32% | [62] |
| Source | Target | Dose | Biological Activities | Action or Mechanism | Reference |
|---|---|---|---|---|---|
| Fresh gel | Human gingival fibroblasts | 16 mg/mL | Oral wound healing | Proliferation (+); keratinocyte growth factor-1 (KGF-1) (+); VEGF (+); type I collagen production (+) | [7] |
| Fresh gel | Human gingival fibroblasts | 10 mg/mL | Oral wound healing | IL-6 (+); IL−8 (+); p50/DNA (+); TLR5/NF-κB (+); Binds with TLR5 ectodomain flagellin recognition sites | [33] |
| Freeze-dried gel | Immature dendritic cells (mice) | 100 µg/mL | Immunomodulatory | Induce maturation of immature DCs; mixed lymphocyte reaction; IL-12 (+) | [42] |
| Fresh gel | Bone marrow stromal cell (BMSC) (rat) | 8 mg/mL | Periodontal tissue regeneration | BMSC proliferation (+); vascular endothelial growth factors (VEGF) (+); ALPase activity (+); bone morphogenic protein-2 (BMP-2) (+); bone sialoprotein (BSP) (+); osteopontin(OPN) (+); mineralization (+) | [46] |
| Fresh gel | RAW 264.7 cells (mouse) | 100 µg/mL | Immunomodulatory | IL-6 (+); TNF-α (+); surface antigen expression (+); IFN-γ (+) | [70] |
| Fresh gel | Tumoral cells (murine, human) | 0.6 mg/mL | Antitumor | Spontaneous proliferation (−); CD25 (+) | [76] |
| Fresh gel | Peritoneal macrophages (mice) | 500 µg/mL | Induced tumor cell cytotoxicity | Endocytosis (+); murine macrophage stimulation | [77] |
| Fresh gel | Lactobacillus, Bifidobacterium, human fecal bacteria | 3 g/L | Prebiotics | Growth (+); butyrate (+); propionate (+); SCFA (+) | [62] |
| Fresh gel | Hepatocytes (rat) | 0.4–250 µg/mL | Antigenotoxic | 3H]B[a]P-DNA adduct formation (−) | [83] |
| Fresh gel | Human periodontal ligament cells | 4 mg/mL | Periodontal tissue regeneration | Cell proliferation (+); RUNX2 (+); GDF5(+); VEGF (+); BMP2 (+); COL1 (+); ALP (+); mineral deposition (+) | [84] |
| Fresh gel | Human periodontal ligament cells, pulpal cells | 1 mg/mL | Periodontal regeneration | BMP2 mRNA (+) and protein (+) | [85] |
| Fresh gel | Human primary dental pulpal cells | --- | Periodontal regeneration | Proliferation (+); alkaline phosphatase (+), type I collagen (+); BMP-2 (+); BMP-4 (+); vascular endothelial growth factor (+); dentin sialo protein expression (+); mineralization (+) | [86] |
| LGM Pharma | Skin primary fibroblasts (mice) | 150 µg/mL | Cell proliferation | Cyclin D1 (+); eukaryotic translation initiation factor-4F (eIF4F) (+); activation of AKT/mTOR | [87] |
| Source | Model | Target | Dose | Administraction | Biological Activities | Action or Mechanism | Reference |
|---|---|---|---|---|---|---|---|
| Fresh gel | --- | Sprague Dawley rats (male) | 2% | External application | Wound healing | Reduced oral wound areas | [7] |
| Dring gel (200:1) | Implanted with sarcoma 180 cell | ICR mice | 1 mg/mouse | Injection | Antitumor | Exhibited macrophage-activating activity | [37] |
| Fresh gel | Tooth extraction model | Sprague–Dawley rats (male) | 32 mg/kg | External application | Accelerating bone formation | Bone mineral density (+); tooth socket healing (+) | [46] |
| Fresh gel | Irradiation at 2.14 Gy/min | Swiss albino mice (male) | 50 mg/kg | Oral gavage | Immunomodulation/radioprotection; antioxidation | Scavenge free radicals; survival (+); mitogenic activity (+); hematopoiesis (+); activation of MAPK | [53] |
| Fresh gel | Radiation-induced mortality | Swiss albino mice (male) | 150 mg/kg | Oral gavage | Immunomodulatory | Survival (+); peripheral lymphocytes (+);TNF-α (+); IL-1 (+) | [61] |
| Fresh gel | Radiation-induced myelosuppression | C57BL/6 mice (female) | 1 mg/mouse | Injection | Hematopoiesis | White blood cell (+); spleen cellularity (+); lymphocytes (+); neutrophils (+); monocytes | [67] |
| Fresh gel | [3H]B[a]P | ICR mice (male) | 50 mg/mouse | Oral gavage | Antigenotoxic | Glutathione-s-transferase (+);[3H]B[a]P-DNA adduct formation (-) | [83] |
| Fresh gel | --- | Mongrel Dogs | --- | Oral gavage | Accelerating bone formation | Induced bone, cementum, and periodontal ligament formation | [84] |
| Fresh gel | Full-thickness skin excisional wound | BALB/c mice (male) | 2 mg/kg | Injection | Wound healing | Accelerated skin wound closure | [87] |
| Fresh gel | --- | SpragueeDawley rats (female) | 8 mg/sponge | External application | Bone regeneration | Integrate new bone with the old bone | [88] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, C.; Cui, Y.; Pi, F.; Cheng, Y.; Guo, Y.; Qian, H. Extraction, Purification, Structural Characteristics, Biological Activities and Pharmacological Applications of Acemannan, a Polysaccharide from Aloe vera: A Review. Molecules 2019, 24, 1554. https://doi.org/10.3390/molecules24081554
Liu C, Cui Y, Pi F, Cheng Y, Guo Y, Qian H. Extraction, Purification, Structural Characteristics, Biological Activities and Pharmacological Applications of Acemannan, a Polysaccharide from Aloe vera: A Review. Molecules. 2019; 24(8):1554. https://doi.org/10.3390/molecules24081554
Chicago/Turabian StyleLiu, Chang, Yan Cui, Fuwei Pi, Yuliang Cheng, Yahui Guo, and He Qian. 2019. "Extraction, Purification, Structural Characteristics, Biological Activities and Pharmacological Applications of Acemannan, a Polysaccharide from Aloe vera: A Review" Molecules 24, no. 8: 1554. https://doi.org/10.3390/molecules24081554
APA StyleLiu, C., Cui, Y., Pi, F., Cheng, Y., Guo, Y., & Qian, H. (2019). Extraction, Purification, Structural Characteristics, Biological Activities and Pharmacological Applications of Acemannan, a Polysaccharide from Aloe vera: A Review. Molecules, 24(8), 1554. https://doi.org/10.3390/molecules24081554







