An Undergraduate Interprofessional Experience with Self-Learning Methodology in Simulation Environment (MAES©): A Qualitative Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Settings
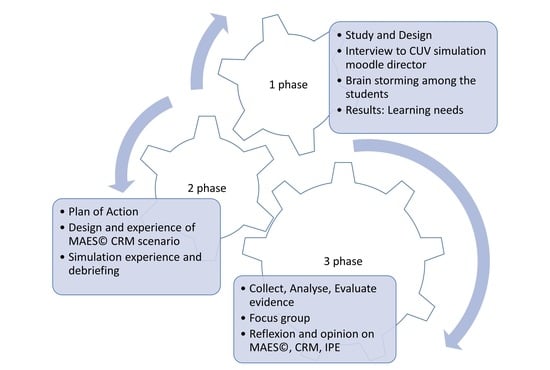
2.2. Design
2.3. Participants
2.4. Procedure
2.4.1. First Phase
2.4.2. Second Phase
2.4.3. Third Phase
2.5. Data Analysis
3. Results
3.1. Study and Design: Investigate and Set Learning Needs
3.1.1. Expert Interview
“They are future professionals that will share many objectives and a great deal of knowledge: patients’ care, patients’ safety, health education, prevention etc. (…).” (I)
“Thinking about how long nurses and doctors live together after their graduation, in their work sites, I cannot believe how poor their relationship is during university. They barely see each other (…).” (I)
“Universities focus on developing nurses and doctor students’ critical thinking, their ability to face difficult situations, and improving their patients’ care (…).” (I)
“If we clearly know what our common educational objective is, something is wrong when we use IPE only for some very punctual and specific training (…).” (I)
“We use IPE training to develop and train only specific techniques in a more theoretical way. This does not allow us to develop and train non-technical skills. They work together in the same room, but they do not solve the case together (…).” (I)
“We observed the medical students use nursing students only to realise that technique alone cannot solve the problem, while nursing students referred to doctors only to ask prescriptions. This does not allow us to develop and train non-technical skills, whereas clinical simulation is more appropriate and could help students to experience more realistic scenarios (…).” (I)
“The students need to live experiences; they cannot base their training only on theory. Simulation can definitely help professors, tutors, and facilitators to deliver knowledge (…).” (I)
“With SBL, students solve a case given by an expert and the relationships between nurses, and medical students may be limited to the simulation and the learning objectives decided by the facilitator. With MAES©, the experience could be amplified as the students not only solve the scenario, but also decide what they want to learn and then design it (…).” (I)
“With MAES simulation, the medical students focus on their competences and the nurses on theirs, but for the first session, the homework and the structured debriefing could guarantee shared opportunities and the peer work could break barriers that students from different degrees usually have (…).” (I)
“How students can manage a crisis could be the best theme to work on (…).” (I)
“In my opinion, CRM helps to share knowledge but it does not focus on how well you perform techniques or on who is the best in the team. It lets us focus on how students face a crisis together, as a team, something that we have less of an opportunity to train for in separate nursing and medical universities (…).” (I)
3.1.2. Students’ Learning Needs and Baseline Learning Objectives
3.2. Action: IPE Planning and Simulating with MAES©
- Group 1: design scenario, look for information to answer baseline learning needs during the exposition phase in the debriefing (one student nurse, one student doctor)
- Group 2: perform simulation and participate in debriefing (one student nurse, two student doctors)
- Group 3: observe and participate to the debriefing (four student nurses, four student doctors)
- Doctor 1: Emergency doctor who needed to manage the airway, even if she was not an expert. An authoritarian leader unopen to accepting others’ ideas and possessing a short temper.
- Doctor 2: Anesthetic doctor, expert in managing (obstructed?) airways. She could not give suggestions because she wanted to be the center of the situation and she had to try to take over the airway management from the ED doctor.
- Nurse: She needed to react to what she saw as she would have done in a real situation.
3.3. Evaluation: Perception of IPE with MAES© and CRM Experience Outcome
3.3.1. Category 1: MAES
“I liked the fact that I had to decide for myself about what I had to learn based on what I want, my interests, and how I wanted to spend my knowledge on my work. In other words, we were moved by our intrinsic motivation, and it made us more enthusiastic (…).” (GF3)
“Knowing our student-colleagues were the ones who were performing the simulation motivated us even more to design a simulation case that had the best realistic elements possible (…).” (GF1)
“I think MAES is more practical and dynamic than a normal classroom. I found it even more dynamic than the clinical simulation I used to do (…).” (GF6)
“This MAES experience induced us to work, investigate, share, and learn using a very dynamic approach that made our jobs less heavy than a normal class (…).” (GF2, GF3, GF11)
“Analyse together, during the debriefing, what went well and what could have better helped us to focus and better understand the scenario and the subject. The exposition phase, at the end of the debriefing, also helped to better fix the ideas and answer our own questions. It was the best way to close the learning circle (…).” (GF1, GF12)
“I think the problem is homework and how at the beginning it is difficult to fit it into our already busy timetable. Although, I have to say, the group-work is motivating and the perception that we were really working for our own knowledge helped me to find an alternative solution for organisation (…).” (GF4)
3.3.2. Category 2: IPE
“In the future we will work together, and it is important to have experience together in university, but these experiences are rare. I can count three or maybe four times during my time in university. Many times, we (nursing students) have simulation on the same day as medical students and even with the same subject. Nevertheless, the university does not place us together. I think we are missing opportunities (…).” (GF7, GF9)
“I think at the beginning, it is difficult, and we could be a bit shy or have preconceived notions towards our colleagues from a different career (…).” (GF1, GF2, GF4)
“I do not think the problems with IPE are many, and even if they are, I think the positive aspects are more important. IPE allows us to see and touch a different view and a different way of working, even if it is with the same objective: patient care. It also improves teamwork and communication (…).” (GF2, GF5, GF10)
“Working alongside our future doctor colleagues helped us to put ourselves in their position and better understand their work and decisions. MAES and its self-learning method unified with its collaborative learning characteristic accentuated teamwork, helped communication, and raised our mutual respect (…).” (GF8)
“Working with MAES during IPE made me meet someone with similar interests (patients’ care and patients’ safety) but at the same time made my group face the work from two different points of view. This enriched my experience (…).” (GF1, GF2)
“MAES structured debriefing helped us to gain a better understanding of the situation from both points of view (nurse and doctor). It also helped to improve our empathy towards our colleagues (…).” (GF7)
3.3.3. Category 3: CRM
“With CRM we can see and train many non-technical skills that help us in the future to reduce risks for both the patients and the healthcare professionals (…).” (GF4)
“CRM helped us to better understand decision-making and how we should face a crisis in our team, and I think it is very useful when thinking of my professional future (…).” (GF3)
“Communication, empathy, teamwork, leadership…they are all aspects that we can train and learn with CRM for our future jobs. It has been a great opportunity to do so with IPE since it was even more realistic (…).” (GF6)
4. Discussion
5. Conclusions
5.1. Limitations
5.2. Implications for Educational Practice
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Interview to the University expert | ||
| What is your name? | ||
| What is your role in the university | ||
| Have you got any clinical simulation experience? | ||
| Have you got any Interprofessional education experience? | ||
| Do you interact with both nursing and medical degrees? | ||
| What do you think about the relation that exist between nursing and medical students during their years in university, on a formation point of view? | ||
| What is the main lack you have noticed during nursing and medical students simulation, thinking of no-interprofessional experiences? | ||
| How can we help both students to think and learn in a more cooperative way? | ||
| Do you know MAES©? | ||
| Do you think MAES© can help interprofessional training? Can you motivate your answer? | ||
| What do you think could be an appropriate case scenario to work with interprofessional MAES©? | ||
| No. Item | Guide Questions/Description | Reported on Page |
| Domain 1: | 1 | |
| Research team and reflexivity | ||
| Personal Characteristics | 1 | |
| 1. Inter viewer/facilitator | Which author/s conducted the interview or focus group? | |
| 2. Credentials | What were the researcher’s credentials? E.g. PhD, MD | 1 |
| 3. Occupation | What was their occupation at the time of the study? | 1, 5 |
| 4. Gender | Was the researcher male or female? | 5 |
| 5. Experience and training | What experience or training did the researcher have? | 5 |
| Relationship with participants | 5 | |
| 6. Relationship established | Was a relationship established prior to study commencement? | 4 |
| 7. Participant knowledge of the interviewer | What did the participants know about the researcher? e.g., personal goals, reasons for doing the research | 4, 5 |
| 8. Interviewer characteristics | What characteristics were reported about the inter viewer/facilitator? e.g., Bias, assumptions, reasons and interests in the research topic | 4, 5 |
| Domain 2: study design | 3–6 | |
| Theoretical framework | 1–3 | |
| 9. Methodological orientation and Theory | What methodological orientation was stated to underpin the study? e.g., grounded theory, discourse analysis, ethnography, phenomenology, content analysis | 1, 3 |
| Participant selection | 4 | |
| 10. Sampling | How were participants selected? e.g., purposive, convenience, consecutive, snowball | 4 |
| 11. Method of approach | How were participants approached? e.g., face-to-face, telephone, mail, email | 3, 4 |
| 12. Sample size | How many participants were in the study? | 4 |
| 13. Nonparticipation | How many people refused to participate or dropped out? Reasons? | N/A |
| Setting | ||
| 14. Setting of data collection | Where was the data collected? e.g., home, clinic, workplace | 3 |
| 15. Presence of non-participants | Was anyone else present besides the participants and researchers? | N/A |
| 16. Description of sample | What are the important characteristics of the sample? e.g., demographic data, date | 4 |
| Data collection | 17. Interview guide Were questions, prompts, guides provided by the authors? Was it pilot tested? | 13, 18, 19 |
| 18. Repeat interviews | Were repeat interviews carried out? If yes, how many? | N/A |
| 19. Audio/visual recording | Did the research use audio or visual recording to collect the data? | 6 |
| 20. Field notes | Were field notes made during and/or after the interview or focus group? | 6 |
| 21. Duration | What was the duration of the inter views or focus group? | 4 |
| 22. Data saturation | Was data saturation discussed? | 6 |
| 23. Transcripts returned | Were transcripts returned to participants for comment and/or correction? | 6 |
| Domain 3: analysis and findings | ||
| Data analysis | ||
| 24. Number of data coders | How many data coders coded the data? | N/A |
| 25. Description of the coding tree | Did authors provide a description of the coding tree? | N/A |
| 26. Derivation of themes | Were themes identified in advance or derived from the data? | 6 |
| 27. Software | What software, if applicable, was used to manage the data? | 6 |
| 28. Participant checking | Did participants provide feedback on the findings? | N/A |
| Reporting | ||
| 29. Quotations presented | Were participant quotations presented to illustrate the themes/findings? Was each quotation identified? e.g., participant number | 6–11 |
| 30. Data and findings consistent | Was there consistency between the data presented and the findings? | 6–11 |
| 31. Clarity of major themes | Were major themes clearly presented in the findings? | 6–11 |
| 32. Clarity of minor themes | Is there a description of diverse cases or discussion of minor themes? | 6–11 |
| MAES simulation | |
| MAES clinical simulation title: CRM | |
| Team planning the simulation: RN-TEAM | |
| Information provided to the simulator group prior to the simulation | |
| Debriefing | Clinical history & situation |
| Learning goals & discussion points | Situation |
| 1. What is CRM? | 25 y.o. female patient who attended Emergency Department with 3 days history abdominal pain (RLQ), nausea and temperature. No vomit, no diarrhoea. In ED they performed XR, Bloods and CT scan before deciding she needed urgent appendicectomy. |
| 2. Existing protocols | |
| 3. People involved? | |
| 4. Who is teamleader? | |
| Technical & non technical skills | Background |
| Allergic to paracetamol. Smoker. | |
| 1. Technique to solve a CRM (check list) | Assessment |
| FC 126, TA 87/52, FR 33, Sats 95%, Temp 39º. Patient with vomit, strong abdominal pain (8/10), GCS 13, pale, diaphoretic. | |
| Recommendation | |
| Assessment and secure airway to transfer her to theatre. | |
| Clinical happenings (Evolution of the clinical situation during the simulation) | ||
| ||
| Interventions (Activities and interventions that the simulator team is expected to perform) | ||
| Intervention 1: Conflict resolution | ||
| YES | NO | |
| Activity 1: Allow team members to express their feelings | ||
| Activity 2: Use different communication technique (reflexion, active listening, open questions) | ||
| Activity 3: Help members to identify problems and possible solutions | ||
| Activity 4: Facilitate problems solution | ||
| Activity 5: Help members to actively solve problems | ||
| Intervention 2: Intubation and airway management | ||
| YES | NO | |
| Activity 1: Wash hands | ||
| Activity 2: Select correctly oropharyngeal/nasopharyngeal airway | ||
| Activity 3: Correct patient’s position and preoxygenation | ||
| Activity 4: Aspiration of patient’s airway | ||
| Activity 5: Insert airway management tool and verify correct position | ||
| Resources | ||
 | Mannequin and Actors | |
| Instruction for the actors: Doctor 1: Emergency doctor who needed to manage airway, even if she was not an expert. Authoritarian leader, not opened to accept others’ ideas. Easy to get angry Doctor 2: Anesthetic doctor, expert in managing difficult airway. She could not give suggestions because she wanted to be the center of the situation and she had to try to take over the airway management from the ED doctor. Nurse: She needed to react to what she saw as she would have done in a real situation | ||
 | Materials | |
| Resus trolley, airway trolley, difficult airway trolley, monitor, cannulation materials, medication for definitive airway management | ||
| SCIENTIFIC EVIDENCES | ||
| Themes | Reference | |
| 1-2-3 | https://www.google.com/search?client=safari&rls=en&q=Simulaci%C3%B3n+cl%C3%ADnica+y+segurdad+en+urgencia (accessed on 3 February 2022) https://litfl.com/crisis-resource-management-crm/s+y+emergencias%3A+Emergency+Crisis+Resource+Management+(E-CRM)&ie=UTF-8&oe=UTF-8 (accessed on 3 February 2022) | |
| 4 | https://eds.p.ebscohost.com/eds/pdfviewer/pdfviewer?vid=0&sid=9ebca4d3-2d7c-479f-9903-716870e29339%40redis (accessed on 3 February 2022) | |
| Check List | https://www.fcchi.org.ar/wp-content/uploads/2020/02/Checklist-IOT-UTIA-HIBAfeb2020.pdf?fbclid=IwAR1oR575sOaUzLnwgNCENF47niua6iQ1N7GFsmxa-uARd5qg4zEYM9wXU (accessed on 3 February 2022) | |
| Focus Group |
|---|
| What is your name? |
| Have you got any clinical simulation experience? |
| Have you got any Interprofessional education experience? |
| What do you think about teamwork? |
| What do you think about the relation that exist between nursing and medical students on a formation point of view? |
| What do you think about the possibility to work with a doctor/nurse teammate? |
| Did you know MAES©? |
| Do you think MAES© can help interprofessional training? Can you motivate your answer? |
References
- Medicine, I. To Err Is Human: Building a Safer Health System; Institute of Medicine: Washington, DC, USA, 1999; ISBN 978-0-309-26174-6. Available online: https://nap.nationalacademies.org/catalog/9728/to-err-is-human-building-a-safer-health-system (accessed on 30 April 2022).
- Gordon, M.; Darbyshire, D.; Baker, P. Non-technical skills training to enhance patient safety: A systematic review. Med. Educ. 2012, 46, 1042–1054. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2923.2012.04343.x (accessed on 30 April 2022). [CrossRef] [PubMed]
- Díaz-Agea, J.L.; Ayensa-Arano, C.; Pujalte-Jesús, M.J.; Cinesi-Gómez, C.; Cánovas-Pallarés, J.M.; Párraga-Ramírez, M.J.; Leal-Costa, C. Improving Interprofessional Team Simulation Learning. One More Step towards the Humanization of Health Care in Emergency Situations. Available online: https://www.signavitae.com/articles/10.22514/sv.2021.223 (accessed on 30 April 2022).
- Reeves, S.; Zwarenstein, M.; Goldman, J.; Barr, H.; Freeth, D.; Koppel, I.; Hammick, M. The effectiveness of interprofessional education: Key findings from a new systematic review. J. Interprof. Care 2010, 24, 230–241. [Google Scholar] [CrossRef] [PubMed]
- Framework for Action on Interprofessional Education & Collaborative Practice. Available online: https://www.who.int/publications-detail-redirect/framework-for-action-on-interprofessional-education-collaborative-practice (accessed on 30 April 2022).
- Al-Qahtani, M.F.; Guraya, S.Y. Measuring the attitudes of healthcare faculty members towards interprofessional education in KSA. J. Taibah Univ. Med. Sci. 2016, 11, 586–593. Available online: https://www.sciencedirect.com/science/article/pii/S1658361216301093 (accessed on 30 April 2022). [CrossRef] [Green Version]
- Reeves, S.; Goldman, J.; Oandasan, I. Key factors in planning and implementing interprofessional education in health care settings. J. Allied Health 2007, 36, 231–235. [Google Scholar] [PubMed]
- Guraya, S.Y.; Barr, H. The effectiveness of interprofessional education in healthcare: A systematic review and meta-analysis. Kaohsiung J. Med. Sci. 2018, 34, 160–165. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1016/j.kjms.2017.12.009 (accessed on 30 April 2022). [CrossRef]
- Freeth, D.; Reeves, S. Learning to work together: Using the presage, process, product (3P) model to highlight decisions and possibilities. J. Interprof. Care 2004, 18, 43–56. [Google Scholar] [CrossRef]
- INACSL Standards of Best Practice: SimulationSM Simulation-Enhanced Interprofessional Education (Sim-IPE). Clin. Simul. Nurs. 2016, 12, S34–S38. Available online: https://www.nursingsimulation.org/article/S1876-1399(16)30132-3/fulltext (accessed on 30 April 2022). [CrossRef] [Green Version]
- O’Rourke, J.; Horsley, T.L.; Doolen, J.; Mariani, B.; Pariseault, C. Integrative Review of Interprofessional Simulation in Nursing Practice. J. Contin. Educ. Nurs. 2018, 49, 91–96. Available online: https://journals.healio.com/doi/10.3928/00220124-20180116-09 (accessed on 30 April 2022). [CrossRef] [Green Version]
- Gaba, D.M.; Fish, K.J.; Howard, S.K.; Burden, A. Crisis Management in Anesthesiology E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2014; 434p, ISBN 978-1-4557-3809-0. [Google Scholar]
- Crew Resource Management—2nd Edition. Available online: https://www.elsevier.com/books/crew-resource-management/kanki/978-0-08-095900-9 (accessed on 30 April 2022).
- Illingworth, P.; Chelvanayagam, S. Benefits of interprofessional education in health care. Br. J. Nurs. 2007, 16, 121–124. Available online: https://www.magonlinelibrary.com/doi/abs/10.12968/bjon.2007.16.2.22773 (accessed on 30 April 2022). [CrossRef]
- Costello, M.; Prelack, K.; Faller, J.; Huddleston, J.; Adly, S.; Doolin, J. Student experiences of interprofessional simulation: Findings from a qualitative study. J. Interprof. Care 2018, 32, 95–97. [Google Scholar] [CrossRef]
- Cox, M.; Cuff, P.; Brandt, B.; Reeves, S.; Zierler, B. Measuring the impact of interprofessional education on collaborative practice and patient outcomes. J. Interprof. Care 2016, 30, 1–3. [Google Scholar] [CrossRef] [Green Version]
- Alexander, M.; Durham, C.F.; Hooper, J.I.; Jeffries, P.R.; Goldman, N.; “Suzie” Kardong-Edgren, S.; Kesten, K.S.; Spector, N.; Tagliareni, E.; Radtke, B.; et al. NCSBN Simulation Guidelines for Prelicensure Nursing Programs. J. Nurs. Regul. 2015, 6, 39–42. Available online: https://www.journalofnursingregulation.com/article/S2155-8256(15)30783-3/fulltext (accessed on 30 April 2022). [CrossRef]
- Cant, R.P.; Cooper, S.J. Use of simulation-based learning in undergraduate nurse education: An umbrella systematic review. Nurse Educ. Today 2017, 49, 63–71. Available online: https://www.sciencedirect.com/science/article/pii/S0260691716302751 (accessed on 30 April 2022). [CrossRef]
- INACSL Standards of Best Practice: SimulationSM Outcomes and Objectives. Clin. Simul. Nurs. 2016, 12, S13–S15. Available online: https://linkinghub.elsevier.com/retrieve/pii/S187613991630127X (accessed on 30 April 2022). [CrossRef] [Green Version]
- INACSL Standards of Best Practice: SimulationSM Facilitation. Clin. Simul. Nurs. 2016, 12, S16–S20. Available online: https://linkinghub.elsevier.com/retrieve/pii/S1876139916301281 (accessed on 30 April 2022). [CrossRef] [Green Version]
- Díaz, J.L.; Leal, C.; García, J.A.; Hernández, E.; Adánez, M.G.; Sáez, A. Self-Learning Methodology in Simulated Environments (MAES©): Elements and Characteristics. Clin. Simul. Nurs. 2016, 12, 268–274. Available online: https://www.sciencedirect.com/science/article/pii/S1876139916000293 (accessed on 30 April 2022). [CrossRef]
- Agea, J.L.D.; Costa, C.L.; Méndez, J.A.G. Metodología de autoaprendizaje en entornos simulados (MAES©). Evidentia Rev. Enferm. Basada Evid. 2014, 11, 8. Available online: https://dialnet.unirioja.es/servlet/articulo?codigo=4767692 (accessed on 30 April 2022).
- Haigh, J. Expansive learning in the university setting: The case for simulated clinical experience. Nurse Educ. Pract. 2007, 7, 95–102. Available online: https://www.sciencedirect.com/science/article/pii/S1471595306000564 (accessed on 30 April 2022). [CrossRef]
- Renz, S.M.; Boltz, M.P.; Wagner, L.M.; Capezuti, E.A.; Lawrence, T.E. Examining the feasibility and utility of an SBAR protocol in long-term care. Geriatr. Nur. 2013, 34, 295–301. Available online: https://www.sciencedirect.com/science/article/pii/S019745721300133X (accessed on 30 April 2022). [CrossRef] [Green Version]
- Phrampus, P.E.; O’Donnell, J.M. Debriefing Using a Structured and Supported Approach. In The Comprehensive Textbook of Healthcare Simulation; Levine, A.I., DeMaria, S., Schwartz, A.D., Sim, A.J., Eds.; Springer: New York, NY, USA, 2013; pp. 73–84. ISBN 978-1-4614-5993-4. [Google Scholar] [CrossRef]
- Díaz-Agea, J.L.; Jiménez-Rodríguez, D.; García-Méndez, J.A.; Hernández-Sánchez, E.; Sáez-Jiménez, A.; Leal-Costa, C. Patient-Oriented Debriefing: Impact of Real Patients’ Participation during Debriefing. Clin. Simul. Nurs. 2017, 13, 405–413. Available online: https://www.sciencedirect.com/science/article/pii/S1876139916301098 (accessed on 30 April 2022). [CrossRef]
- Franco, I.; Sweeney, R.E.; Marks, J.A.; McLaughlin, C.; Henry, M.; Yaport, M.A.; Arriaga, A.F. Crisis Resource Management and Interdisciplinary Team Training. In Comprehensive Healthcare Simulation: Anesthesiology; Mahoney, B., Minehart, R.D., Pian-Smith, M.C.M., Eds.; Comprehensive Healthcare Simulation; Springer International Publishing: Cham, Switzerland, 2020; pp. 47–60. ISBN 978-3-030-26849-7. [Google Scholar] [CrossRef]
- Carne, B.; Kennedy, M.; Gray, T. Review article: Crisis resource management in emergency medicine. Emerg. Med. Australas. 2012, 24, 7–13. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1742-6723.2011.01495.x (accessed on 30 April 2022). [CrossRef]
- Comprehensive Healthcare Simulation: Emergency Medicine. Available online: https://link.springer.com/book/10.1007/978-3-030-57367-6 (accessed on 30 April 2022).
- Fenzi, G.; Reuben, A.D.; Agea, J.L.D.; Ruipérez, T.H.; Costa, C.L. Self-learning methodology in simulated environments (MAES©) utilized in hospital settings. Action-research in an Emergency Department in the United Kingdom. Int. Emerg. Nurs. 2022, 61, 101128. Available online: https://www.sciencedirect.com/science/article/pii/S1755599X2100166X (accessed on 30 April 2022). [CrossRef] [PubMed]
- Díaz Agea, J.L.; Megías Nicolás, A.; García Méndez, J.A.; de Gracia Adánez Martínez, M.; Leal Costa, C. Improving simulation performance through Self-Learning Methodology in Simulated Environments (MAES©). Nurse Educ. Today 2019, 76, 62–67. Available online: https://www.sciencedirect.com/science/article/pii/S0260691719301728 (accessed on 30 April 2022). [CrossRef]
- Leal Costa, C.; Megías Nicolás, A.; García Méndez, J.A.; de Gracia Adánez Martínez, M.; Díaz Agea, J.L. Enseñando con metodología de autoaprendizaje en entornos simulados (MAES©). Un estudio cualitativo entre profesores y alumnos de grado en Enfermería. Educ. Médica 2019, 20, 52–58. Available online: https://www.sciencedirect.com/science/article/pii/S1575181318301177 (accessed on 30 April 2022). [CrossRef]
- Peñataro-Pintado, E.; Díaz-Agea, J.L.; Castillo, I.; Leal-Costa, C.; Ramos-Morcillo, A.J.; Ruzafa-Martínez, M.; Rodríguez-Higueras, E. Self-Learning Methodology in Simulated Environments (MAES©) as a Learning Tool in Perioperative Nursing. An Evidence-Based Practice Model for Acquiring Clinical Safety Competencies. Int. J. Environ. Res. Public. Health 2021, 18, 7893. Available online: https://www.mdpi.com/1660-4601/18/15/7893 (accessed on 30 April 2022). [CrossRef]
- Colorafi, K.J.; Evans, B. Qualitative descriptive methods in health science research. HERD Health Environ. Res. Des. J. 2016, 9, 16–25. [Google Scholar] [CrossRef]
- Gordon, M.; Fell, C.W.; Box, H.; Farrell, M.; Stewart, A. Learning health ‘safety’within non-technical skills interprofessional simulation education: A qualitative study. Med. Educ. Online 2017, 22, 1272838. [Google Scholar] [CrossRef] [Green Version]
- Efron, S.E.; Ravid, R. Action Research in Education, Second Edition: A Practical Guide; Guilford Publications: New York, NY, USA, 2019; 297p, ISBN 978-1-4625-4166-9. [Google Scholar]
- Hsieh, H.-F.; Shannon, S.E. Three Approaches to Qualitative Content Analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef]
- Kuckartz, U.; Rädiker, S. (Eds.) Analyzing Focus Group Data. In Analyzing Qualitative Data with MAXQDA: Text, Audio, and Video; Springer International Publishing: Cham, Switzerland, 2019; pp. 201–217. ISBN 978-3-030-15671-8. [Google Scholar] [CrossRef]
- Morrow, R.; Rodriguez, A.; King, N. Colaizzi’s descriptive phenomenological method. Psychologist 2015, 28, 643–644. Available online: https://thepsychologist.bps.org.uk/volume-28/august-2015/learning-lifeworld (accessed on 30 April 2022).
- Edward, K.-L.; Welch, T. The extension of Colaizzi’s method of phenomenological enquiry. Contemp. Nurse 2011, 39, 163–171. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization (WHO). Transforming and Scaling Uphealth Professionals’ Education and Training. 2013. Available online: https://apps.who.int/iris/bitstream/handle/10665/93635/9789241506502_eng.pdf (accessed on 30 April 2022).
- Hernández, E.; Camacho, M.; Leal-Costa, C.; Ruzafa-Martínez, M.; Ramos-Morcillo, A.J.; Cazorla, E.; Díaz-Agea, J.L. Does Multidisciplinary Team Simulation-Based Training Improve Obstetric Emergencies Skills? Healthcare 2021, 9, 170. [Google Scholar] [CrossRef] [PubMed]
- Murray, W.B.; Foster, P.A. Crisis resource management among strangers: Principles of organizing a multidisciplinary group for crisis resource management. J. Clin. Anesth. 2000, 12, 633–638. [Google Scholar] [CrossRef]
- Kotera, Y.; Taylor, E.; Fido, D.; Williams, D.; Tsuda-McCaie, F. Motivation of UK graduate students in education: Self-compassion moderates pathway from extrinsic motivation to intrinsic motivation. Curr. Psychol. 2021. [Google Scholar] [CrossRef]
| Inclusion | Exclusion |
|---|---|
| Last year nursing students (4º year) Last year medical students (6º year) Previous clinical simulation experience | Previous experience with interprofessional training |
| What Do We Know? | What Do We Want to Learn? |
|---|---|
| CRM was born in aviation. | What is CRM? |
| Teamwork and communication are two of the most important concepts in CRM. The qualities that define a team leader. | Is there any existing protocol we can follow to apply CRM? Who are the people and professionals involved in CRM? What are the techniques and concepts related to CRM applied in healthcare? Who is more appropriate to be a team leader in healthcare? |
| Category | Subcategory |
|---|---|
| MAES© | Self-learning & intrinsic motivation |
| MAES© compared with previous experiences | |
| Debriefing | |
| Aspects to improve | |
| IPE | Present situation |
| Positive Aspects | |
| IPE & MAES© | |
| CRM | Link with work situation |
| Positive aspects to train CRM |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fenzi, G.; Díaz-Agea, J.L.; Pethick, D.; Bertolín-Delgado, R.; Hernández-Donoso, N.; Lorente-Corral, L. An Undergraduate Interprofessional Experience with Self-Learning Methodology in Simulation Environment (MAES©): A Qualitative Study. Nurs. Rep. 2022, 12, 446-463. https://doi.org/10.3390/nursrep12030043
Fenzi G, Díaz-Agea JL, Pethick D, Bertolín-Delgado R, Hernández-Donoso N, Lorente-Corral L. An Undergraduate Interprofessional Experience with Self-Learning Methodology in Simulation Environment (MAES©): A Qualitative Study. Nursing Reports. 2022; 12(3):446-463. https://doi.org/10.3390/nursrep12030043
Chicago/Turabian StyleFenzi, Giulio, José Luis Díaz-Agea, David Pethick, Rocío Bertolín-Delgado, Noelia Hernández-Donoso, and Luis Lorente-Corral. 2022. "An Undergraduate Interprofessional Experience with Self-Learning Methodology in Simulation Environment (MAES©): A Qualitative Study" Nursing Reports 12, no. 3: 446-463. https://doi.org/10.3390/nursrep12030043