Impact of COVID-19 on the Destiny of Bariatric Patients
Abstract
:1. Introduction
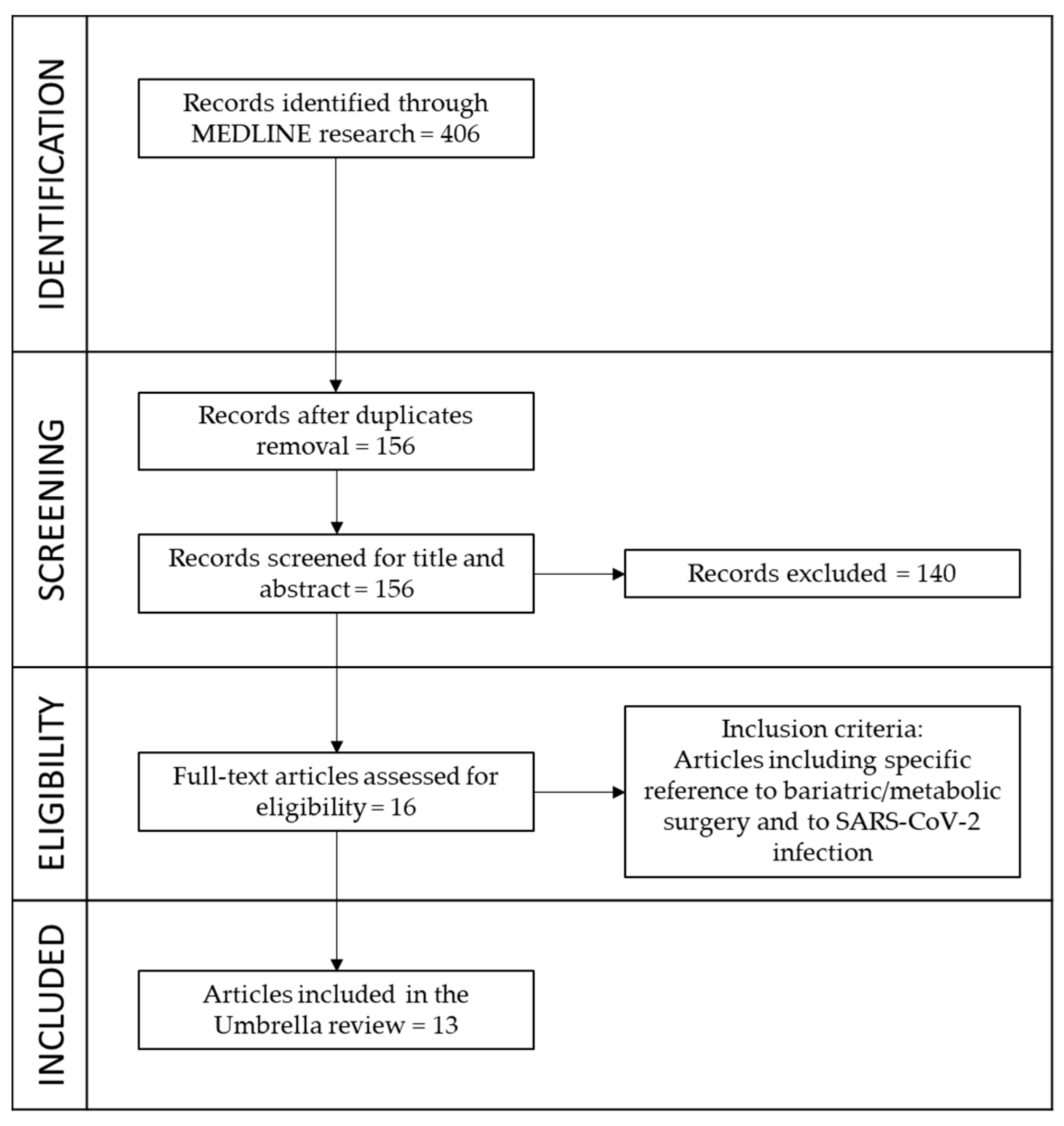
2. Materials and Methods
3. Results
- -
- Five reviews are focused on strategies and management of candidates for bariatric surgery and how to restart from this pandemic;
- -
- One review dealt with cost analysis of bariatric surgery during the pandemic;
- -
- Three reviews highlighted the association between obesity, infectious disease, and COVID-19;
- -
- Three reviews reported that bariatric and metabolic surgeries are protective procedures for severe clinical outcomes of SARS-CoV-2 infection; and
- -
- One review is focused on the nutritional management of bariatric patients during the stop of bariatric surgery due to COVID-19.
4. Discussion
4.1. Obesity Pandemic
4.2. Double Pandemic: Obesity and COVID-19
4.3. Benefits of Bariatric Surgery in General and Respect to SARS-CoV-2 Infection
4.4. Economic Aspects
4.5. How to Restart
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kwok, S.; Adam, S.; Ho, J.H.; Iqbal, Z.; Turkington, P.; Razvi, S.; Le Roux, C.W.; Soran, H.; Syed, A.A. Obesity: A critical risk factor in the COVID-19 pandemic. Clin. Obes. 2020, 10, e12403. [Google Scholar] [CrossRef] [PubMed]
- Marinari, G.M.; Anselmino, M.; Tascini, C.; Bernante, P.; Foletto, M.; Gentileschi, P.; Morino, M.; Olmi, S.; Toppino, M.; Silecchia, G. Bariatric and metabolic surgery during COVID-19 outbreak phase 2 in Italy: Why, when and how to restart. Surg. Obes. Relat. Dis. 2020, 16, 1614–1618. [Google Scholar] [CrossRef]
- Aminian, A.; Tu, C. Association of Bariatric Surgery with Clinical Outcomes of SARS-CoV-2 Infection: A Systematic Review and Meta-analysis in the Initial Phase of COVID-19 Pandemic. Obes. Surg. 2021, 31, 2419–2425. [Google Scholar] [CrossRef]
- Zakka, K.; Chidambaram, S.; Mansour, S.; Mahawar, K.; Salminen, P.; Almino, R.; Schauer, P.; Kinross, J.; Purkayastha, S.; PanSurg Collaborative. SARS-CoV-2 and Obesity: “CoVesity”—A Pandemic within a Pandemic. Obes. Surg. 2021, 31, 1745–1754. [Google Scholar] [CrossRef] [PubMed]
- De Lorenzo, A.; Siclari, M.; Gratteri, S.; Romano, L.; Gualtieri, P.; Marchetti, M.; Merra, G.; Colica, C. Developing and cross-validation of new equations to estimate fat mass in Italian population. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 2513–2524. [Google Scholar] [CrossRef] [PubMed]
- De Lorenzo, A.; Romano, L.; Di Renzo, L.; Di Lorenzo, N.; Cenname, G.; Gualtieri, P. Obesity: A preventable, treatable, but relapsing disease. Nutrition 2020, 71, 110615. [Google Scholar] [CrossRef]
- Aminian, A.; Tu, C.; Milinovich, A.; Wolski, K.E.; Kattan, M.W.; Nissen, S.E. Association of Weight Loss Achieved Through Metabolic Surgery with Risk and Severity of COVID-19 Infection. JAMA Surg. 2022, 157, 221–230. [Google Scholar] [CrossRef]
- Pugliese, G.; Liccardi, A.; Graziadio, C.; Barrea, L.; Muscogiuri, G.; Colao, A. Obesity and infectious diseases: Pathophysiology and epidemiology of a double pandemic condition. Int. J. Obes. 2022, 46, 449–465. [Google Scholar] [CrossRef]
- S.I.C.OB. Indagine Conoscitiva Sulla Riduzione Dell’attività di Chirurgia Bariatrica COVID-19 Correlata. Available online: https://www.sicob.org/09_covid/chirurgia.html (accessed on 26 November 2022).
- Executive Council of ASMBS. Safer through surgery: American Society for Metabolic and Bariatric Surgery statement regarding metabolic and bariatric surgery during the COVID-19 pandemic. Surg. Obes. Relat. Dis. 2020, 16, 981–982. [Google Scholar] [CrossRef]
- Rubino, F.; Cohen, R.V.; Mingrone, G.; le Roux, C.W.; Mechanick, J.I.; Arterburn, D.E.; Vidal, J.; Alberti, G.; Amiel, S.A.; Batterham, R.L.; et al. Bariatric and metabolic surgery during and after the COVID-19 pandemic: DSS recommendations for management of surgical candidates and postoperative patients and prioritisation of access to surgery. Lancet Diabetes Endocrinol. 2020, 8, 640–648. [Google Scholar] [CrossRef]
- Erol, V.; Sümer, A.; Savaş, O.A.; Pekşen, Ç.; Gülay, H.; Aktimur, R.; Özmen, M.M. Recommendations for bariatric and metabolic surgical operations during the COVID-19 pandemic in Turkey. Turk. J. Surg. 2020, 36, 132–136. [Google Scholar] [CrossRef]
- Sánchez Santos, R.; Garcia Ruiz de Gordejuela, A.; Breton Lesmes, I.; Lecube Torelló, A.; Moizé Arcone, V.; Arroyo Martin, J.J.; Fernandez Alsina, E.; Martín Antona, E.; Rubio Herrera, M.Á.; Sabench Pereferrer, F.; et al. Obesity and SARS-CoV-2: Considerations on bariatric surgery and recommendations for the start of surgical activity. Cirugía Española 2021, 99, 4–10. [Google Scholar] [CrossRef]
- De Amicis, R.; Cancello, R.; Capodaglio, P.; Gobbi, M.; Brunani, A.; Gilardini, L.; Castelnuovo, G.; Molinari, E.; Barbieri, V.; Mambrini, S.P.; et al. Patients with Severe Obesity during the COVID-19 Pandemic: How to Maintain an Adequate Multidisciplinary Nutritional Rehabilitation Program? Obes. Facts 2021, 14, 205–213. [Google Scholar] [CrossRef]
- Gupta, R.; Gupta, J.; Ammar, H. Impact of COVID-19 on the outcomes of gastrointestinal surgery. Clin. J. Gastroenterol. 2021, 14, 932–946. [Google Scholar] [CrossRef]
- Liu, D.; Cheng, Q.; Suh, H.R.; Magdy, M.; Loi, K. Role of bariatric surgery in a COVID-19 era: A review of economic costs. Surg. Obes. Relat. Dis. 2021, 17, 2091–2096. [Google Scholar] [CrossRef]
- Dickey, J.; Davtyan, C.; Davtyan, D.; Taegtmeyer, H. Homeostasis Disrupted and Restored—A Fresh Look at the Mechanism and Treatment of Obesity During COVID-19. Front. Cardiovasc. Med. 2021, 8, 721956. [Google Scholar] [CrossRef]
- Italian Ministry of Health. Available online: https://www.salute.gov.it/portale/nuovocoronavirus/dettaglioContenutiNuovoCoronavirus.jsp?lingua=italiano&id=5338&area=nuovoCoronavirus&menu=vuoto (accessed on 26 November 2022).
- Rubio Herrera, M.A.; Bretón Lesmes, I. Obesity in the COVID era: A global health challenge. Endocrinol. Diabetes Nutr. 2021, 68, 123–129. [Google Scholar] [CrossRef]
- Stefan, N.; Birkenfeld, A.L.; Schulze, M.B.; Ludwig, D.S. Obesity and impaired metabolic health in patients with COVID-19. Nat. Rev. Endocrinol. 2020, 16, 341–342. [Google Scholar] [CrossRef] [Green Version]
- Popkin, B.M.; Du, S.; Green, W.D.; Beck, M.A.; Algaith, T.; Herbst, C.H.; Alsukait, R.F.; Alluhidan, M.; Alazemi, N.; Shekar, M. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes. Rev. 2020, 21, e13128. [Google Scholar] [CrossRef]
- Albashir, A.A.D. The potential impacts of obesity on COVID-19. Clin. Med. 2020, 20, e109–e113. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Leggeri, C.; Cinelli, G.; Tarsitano, M.G.; Caparello, G.; Carrano, E.; et al. COVID-19: Is there a role for immunonutrition in the obese patient? J. Transl. Med. 2020, 18, 415. [Google Scholar] [CrossRef] [PubMed]
- De Lorenzo, A.; Soldati, L.; Sarlo, F.; Calvani, M.; Di Lorenzo, N.; Di Renzo, L. New obesity classification criteria as a tool for bariatric surgery indication. World J. Gastroenterol. 2016, 22, 681–703. [Google Scholar] [CrossRef] [PubMed]
- Ammori, B.J.; Skarulis, M.C.; Soran, H.; Syed, A.A.; Eledrisi, M.; Malik, R.A. Medical and surgical management of obesity and diabetes: What’s new? Diabet. Med. 2020, 37, 203–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarno, G.; Calabrese, P.; Schiavo, L.; Izzo, F.; Pilone, V. What are risk factors for COVID-19 vaccine breakthrough infections in patients with previous history of bariatric surgery? EXCLI J. 2022, 21, 786–790. [Google Scholar] [CrossRef] [PubMed]
- Hany, M.; Torensma, B.; Abouelnasr, A.A.; Zidan, A.; Ibrahim, M.; Agayby, A.S.S.; Hesham, M.; Elsheredy, A.; Abu-Sheasha, G.A. Impact of bariatric surgery on the effectiveness of serological response after COVID-19 vaccination. Langenbeck’s Arch. Surg. 2022, 407, 2337–2346. [Google Scholar] [CrossRef]
- Carrano, F.M.; Peev, M.P.; Saunders, J.K.; Melis, M.; Tognoni, V.; Di Lorenzo, N. The Role of Minimally Invasive and Endoscopic Technologies in Morbid Obesity Treatment: Review and Critical Appraisal of the Current Clinical Practice. Obes. Surg. 2020, 30, 736–752. [Google Scholar] [CrossRef]
- Sudlow, A.; le Roux, C.W.; Pournaras, D.J. The metabolic benefits of social ine bariatric operations: What procedure to choose? Endocr. Connect. 2020, 9, R28–R35. [Google Scholar] [CrossRef] [Green Version]
- Petrakis, D.; Margină, D.; Tsarouhas, K.; Tekos, F.; Stan, M.; Nikitovic, D.; Kouretas, D.; Spandidos, D.A.; Tsatsakis, A. Obesity—A risk factor for increased COVID-19 prevalence, severity and lethality (Review). Mol. Med. Rep. 2020, 22, 9–19. [Google Scholar] [CrossRef]
- Fezeu, L.; Julia, C.; Henegar, A.; Bitu, J.; Hu, F.B.; Grobbee, D.E.; Kengne, A.P.; Hercberg, S.; Czernichow, S. Obesity is associated with a higher risk of intensive care unit admission and death in influenza A (H1N1) patients: A systematic review and meta-analysis. Obes. Rev. 2011, 12, 653–659. [Google Scholar] [CrossRef]
- Yang, J.; Hu, J.; Zhu, C. Obesity aggravates COVID-19: A systematic review and meta-analysis. J. Med. Virol. 2021, 93, 257–261. [Google Scholar] [CrossRef]
- Caci, G.; Albini, A.; Malerba, M.; Noonan, D.M.; Pochetti, P.; Polosa, R. COVID-19 and obesity: Dangerous liaisons. J. Clin. Med. 2020, 9, 2511. [Google Scholar] [CrossRef]
- Ritter, A.; Kreis, N.N.; Louwen, F.; Yuan, J. Obesity and COVID-19: Molecular Mechanisms Linking Both Pandemics. Int. J. Mol. Sci. 2020, 21, 5793. [Google Scholar] [CrossRef]
- Salian, V.S.; Wright, J.A.; Vedell, P.T.; Nair, S.; Li, C.; Kandimalla, M.; Tang, X.; Carmona Porquera, E.M.; Kalari, K.R.; Kandimalla, K.K. COVID-19 Transmission, Current Treatment, and Future Therapeutic Strategies. Mol. Pharm. 2021, 18, 754–771. [Google Scholar] [CrossRef]
- Piche, M.E.; Auclair, A.; Harvey, J.; Marceau, S.; Poirier, P. How to choose and use bariatric surgery in 2015. Can. J. Cardiol. 2015, 31, 153–166. [Google Scholar] [CrossRef]
- De Lorenzo, A.; Cenname, G.; Marchetti, M.; Gualtieri, P.; Dri, M.; Carrano, E.; Pivari, F.; Esposito, E.; Picchioni, O.; Moia, A.; et al. Social inequalities and nutritional disparities: The link between obesity and COVID-19. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 320–339. [Google Scholar] [CrossRef]
- Ho, J.S.Y.; Fernando, D.I.; Chan, M.Y.; Sia, C.H. Obesity in COVID-19: A Systematic Review and Meta-analysis. Ann. Acad. Med. Singap. 2020, 49, 996–1008. [Google Scholar] [CrossRef]
- Carenzo, L.; Costantini, E.; Greco, M.; Barra, F.L.; Rendiniello, V.; Mainetti, M.; Bui, R.; Zanella, A.; Grasselli, G.; Lagioia, M.; et al. Hospital surge capacity in a tertiary emergency referral centre during the COVID-19 outbreak in Italy. Anaesthesia 2020, 75, 928–934. [Google Scholar] [CrossRef] [Green Version]
- Specchia, M.L.; Veneziano, M.A.; Cadeddu, C.; Ferriero, A.M.; Mancuso, A.; Ianuale, C.; Parente, P.; Capri, S.; Ricciardi, W. Economic impact of adult obesity on health systems: A systematic review. Eur. J. Public Health 2015, 25, 255–262. [Google Scholar] [CrossRef] [Green Version]
- Xia, Q.; Campbell, J.A.; Ahmad, H.; Si, L.; de Graaff, B.; Palmer, A.J. Bariatric surgery is a cost-saving treatment for obesity—A comprehensive meta-analysis and updated systematic review of health economic evaluations of bariatric surgery. Obes. Rev. 2020, 21, e12932. [Google Scholar] [CrossRef]
- Alsumali, A.; Al-Hawag, A.; Samnaliev, M.; Eguale, T. Systematic assessment of analytic decision models for the cost-effectiveness of bariatric surgery for morbid obesity. Surg. Obes. Relat. Dis. 2018, 14, 1041–1059. [Google Scholar] [CrossRef]
- Lucchese, M.; Borisenko, O.; Mantovani, L.G.; Cortesi, P.A.; Cesana, G.; Adam, D.; Burdukova, E.; Lukyanov, V.; Di Lorenzo, N. Cost-Utility Analysis of Bariatric Surgery in Italy: Results of Decision-Analytic Modelling. Obes. Facts 2017, 10, 261–272. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Eisenberg, D.; Azagury, D.; Rogers, A.; Campos, G.M. American Society for Metabolic and Bariatric Surgery position statement on long-term survival benefit after metabolic and bariatric surgery. Surg. Obes. Relat. Dis. 2016, 12, 453–459. [Google Scholar] [CrossRef] [PubMed]
- Arezzo, A.; Francis, N.; Mintz, Y.; Adamina, M.; Antoniou, S.A.; Bouvy, N.; Copaescu, C.; de Manzini, N.; Di Lorenzo, N.; Morales-Conde, S.; et al. EAES Recommendations for Recovery Plan in Minimally Invasive Surgery Amid COVID-19 Pandemic. Surg. Endosc. 2021, 35, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Balibrea, J.M.; Badia, J.M.; Rubio Pérez, I.; Martín Antona, E.; Álvarez Peña, E.; García Botella, S.; Álvarez Gallego, M.; Martín Pérez, E.; Martínez Cortijo, S.; Pascual Miguelañez, I.; et al. Surgical Management of Patients with COVID-19 Infection. Recommendations of the Spanish Association of Surgeons. Cirugía Española 2020, 98, 251–259. [Google Scholar] [CrossRef]
- Navarra, G.; Komaei, I.; Currò, G.; Angrisani, L.; Bellini, R.; Cerbone, M.R.; Di Lorenzo, N.; De Luca, M.; Foletto, M.; Gentileschi, P.; et al. Bariatric surgery and the COVID-19 pandemic: SICOB recommendations on how to perform surgery during the outbreak and when to resume the activities in phase 2 of lockdown. Updates Surg. 2020, 72, 259–268. [Google Scholar] [CrossRef]
- Jing, X.; Chen, J.; Dong, Y.; Han, D.; Zhao, H.; Wang, X.; Gao, F.; Li, C.; Cui, Z.; Liu, Y.; et al. Related factors of quality of life of type 2 diabetes patients: A systematic review and meta-analysis. Health Qual. Life Outcomes 2018, 16, 189. [Google Scholar] [CrossRef]
- Bornstein, S.R.; Dalan, R.; Hopkins, D.; Mingrone, G.; Boehm, B.O. Endocrine and metabolic link to coronavirus infection. Nat. Rev. Endocrinol. 2020, 16, 297–298. [Google Scholar] [CrossRef]
- Italian Ministry of Health. Available online: http://www.salute.gov.it/portale/nuovocoronavirus/homeNuovoCoronavirus.jsp (accessed on 22 July 2020).
| Author | Title | Type of Paper | Date | Finding |
|---|---|---|---|---|
| Rubino, F.; et al. [11] | Bariatric and metabolic surgery during and after the COVID-19 pandemic: DSS recommendations for management of surgical candidates and postoperative patients and prioritisation of access to surgery | Review | 7 May 2020 | Review by experts of the “Diabetes Surgery Summit consensus conference” providing guidance for the management of patients while surgery is delayed for COVID-19 and for postoperative surveillance. In particular, strategies to prioritise bariatric and metabolic surgery candidates on the basis of the diseases that are most likely to be ameliorated postoperatively. |
| Erol, V.; et al. [12] | Recommendations for bariatric and metabolic surgical operations during the COVID-19 pandemic in Turkey. | Review | 20 May 2020 | The aim of this review was to determine the pre-peri and post-operative periods of bariatric surgical requirements during the COVID-19 pandemic according by the Turkish Society for Metabolic and Bariatric Surgery. |
| Executive Council of American Society for Metabolic and Bariatric Surgery, [10] | Safer through surgery: American Society for Metabolic and Bariatric Surgery statement regarding metabolic and bariatric surgery during the COVID-19 pandemic | Review | 6 June 2020 | Metabolic and bariatric surgery is life-saving and life-changing surgery, and especially during this pandemic COVID-19 emerged as the most recent of many diseases in which underlying obesity worsens the prognosis. |
| Marinari, G.M.; et al. [2] | Bariatric and metabolic surgery during COVID-19 outbreak phase 2 in Italy: why, when and how to restart | Review | 9 June 2020 | Review on the Italian experience for a safe restart of elective laparoscopic bariatric surgery thanks to the deliverance of transparent information to the patients and the introduction of the COVID-19 protocol concerning patients and health-professionals protection. |
| Sanchez Santos, R.; et al. [13] | Obesity and SARS-CoV-2: considerations on bariatric surgery and recommendations for the start of surgical activity. | Review | 18 June 2020 | This document contains the main recommendations for bariatric surgery programs in Spain from the point of view of safety, preparation of the bariatric patient and follow up during the SARS-CoV- pandemic. |
| Kwok, S.; et al. [1] | Obesity: A critical risk factor in the COVID-19 pandemic | Review | 7 August 2020 | Review highlighting potential mechanisms by which obesity may influence adverse outcomes from COVID-19, including chronic inflammation, impairment of respiratory function and pulmonary perfusion, immune dysregulation, metabolic and vascular complications; people with severe obesity must be considered a vulnerable group for COVID-19. |
| Aminian, A.; et al. [3] | Association of Bariatric Surgery with Clinical Outcomes of SARS-CoV-2 Infection: a Systematic Review and Meta-analysis in the Initial Phase of COVID-19 Pandemic. | Systematic Review and Meta-analysis | 30 December 2020 | Prior bariatric surgery is associated with a lower rate of mortality and hospital admission in patients with obesity and infected with SARS-CoV-2. |
| Zakka, K.; et al. [4] | SARS-CoV-2 and Obesity: “CoVesity”—a Pandemic Within a Pandemic | Systematic Review | 22 January 2021 | Overview on the link between obesity, a pandemic in itself, as an independent factor for having a worse outcome among COVID-19 patients; the dual pandemic—CoVesity—will have a detrimental outcome in the short, medium, and long term. |
| De Amicis, R.; et al. [14] | Patients with Severe Obesity during the COVID-19 Pandemic: How to Maintain an Adequate Multidisciplinary Nutritional Rehabilitation Program? | Review | 19 March 2021 | The adoption of new strategies, as telemedicine, is necessary to guarantee a continuous multidisciplinary nutritional program to control the severity of SARS-CoV-2 infection in obese patients. |
| Gupta, R.; et al. [15] | Impact of COVID-19 on the outcomes of gastrointestinal surgery | Review | 29 April 2021 | Review of recent studies reporting the outcomes of various gastrointestinal surgeries in the COVID-19 pandemic era including bariatric surgery; bariatric surgery can be offered to the obese patients if the healthcare resources are present and appropriate measures are taken to prevent perioperative transmission of SARS-CoV-2 infection. |
| Liu, D.; et al. [16] | Role of bariatric surgery in a COVID-19 era: a review of econimic costs | Review | 17 July 2021 | Review on the need to the resumption of bariatric services as quickly as possible because of the significant additional medical and economic benefits that it provides. |
| Dickey, J.; et al. [17] | Homeostasis Disrupted and Restored—A Fresh Look at the Mechanism and Treatment of Obesity During COVID-19 | Review | 27 August 2021 | Weight loss during COVID-19 era decrease morbidity and mortality in obese patients, and bariatric surgery should not be postponed. |
| Pugliese, G.; et al. [8] | Obesity and infectious diseases: pathophysiology andepidemiology of a double pandemic condition | Review | 21 January 2022 | Obesity is related directly to a higher risk of contracting different infectious diseases, as well as experiencinga more severe course of COVID-19 with increased mortality rates. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gualtieri, P.; Marchetti, M.; Renzo, L.D.; De Santis, G.L.; Palma, R.; Colica, C.; Frank, G.; De Lorenzo, A.; Di Lorenzo, N. Impact of COVID-19 on the Destiny of Bariatric Patients. Nutrients 2023, 15, 163. https://doi.org/10.3390/nu15010163
Gualtieri P, Marchetti M, Renzo LD, De Santis GL, Palma R, Colica C, Frank G, De Lorenzo A, Di Lorenzo N. Impact of COVID-19 on the Destiny of Bariatric Patients. Nutrients. 2023; 15(1):163. https://doi.org/10.3390/nu15010163
Chicago/Turabian StyleGualtieri, Paola, Marco Marchetti, Laura Di Renzo, Gemma Lou De Santis, Roselisa Palma, Carmela Colica, Giulia Frank, Antonino De Lorenzo, and Nicola Di Lorenzo. 2023. "Impact of COVID-19 on the Destiny of Bariatric Patients" Nutrients 15, no. 1: 163. https://doi.org/10.3390/nu15010163






