Effect of Crocus sativus (Saffron) Intake on Top of Standard Treatment, on Disease Outcomes and Comorbidities in Patients with Rheumatic Diseases: Synthesis without Meta-Analysis (SWiM) and Level of Adherence to the CONSORT Statement for Randomized Controlled Trials Delivering Herbal Medicine Interventions
Abstract
1. Introduction
2. Materials and Methods
2.1. Systematic Review Protocol and PIO
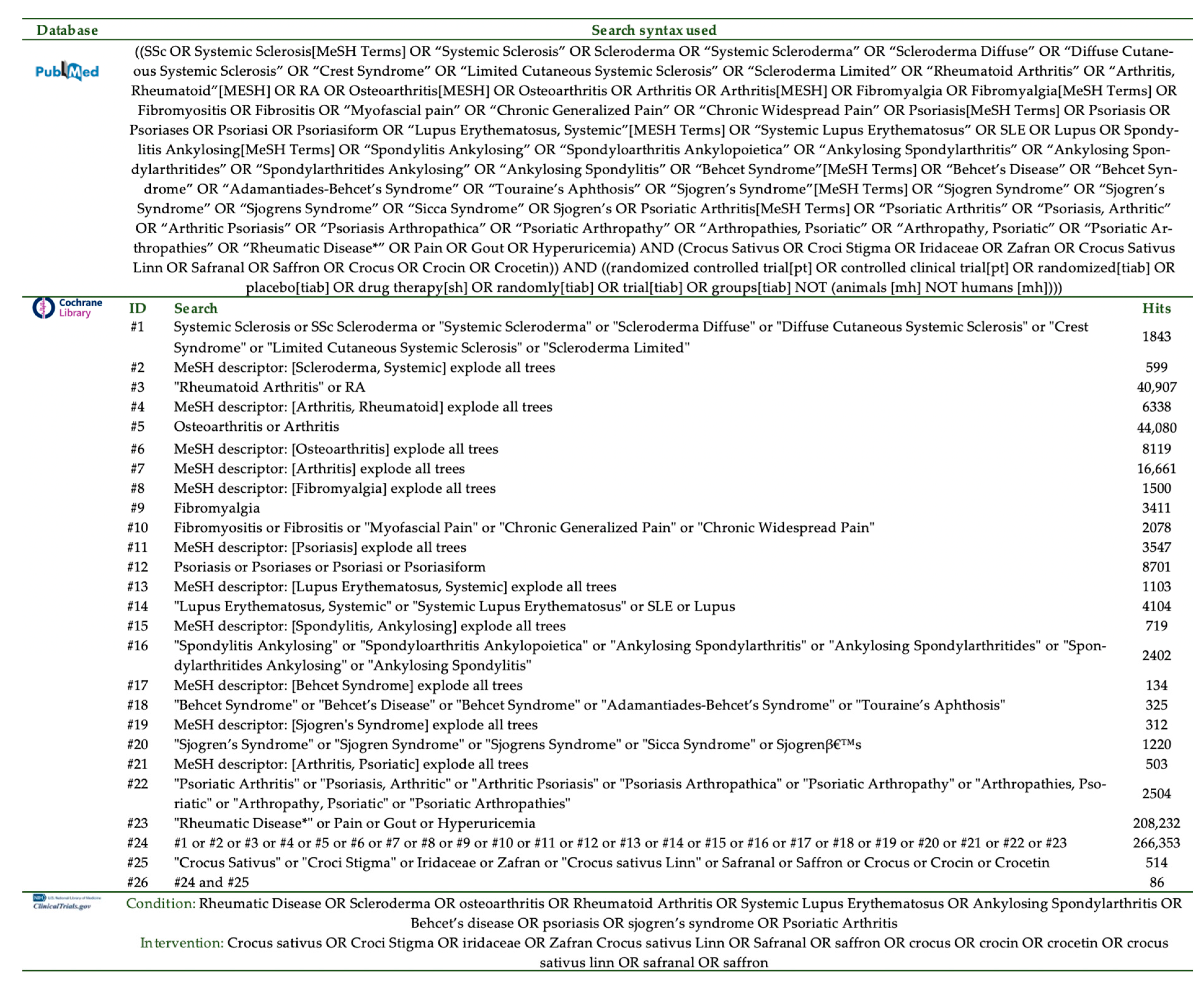
2.2. Search Strategy and Algorithm
2.3. Inclusion and Exclusion Criteria
2.4. Outcomes of Interest
2.5. Risk of Bias
2.6. Data Extraction
2.7. Data Synthesis
3. Results
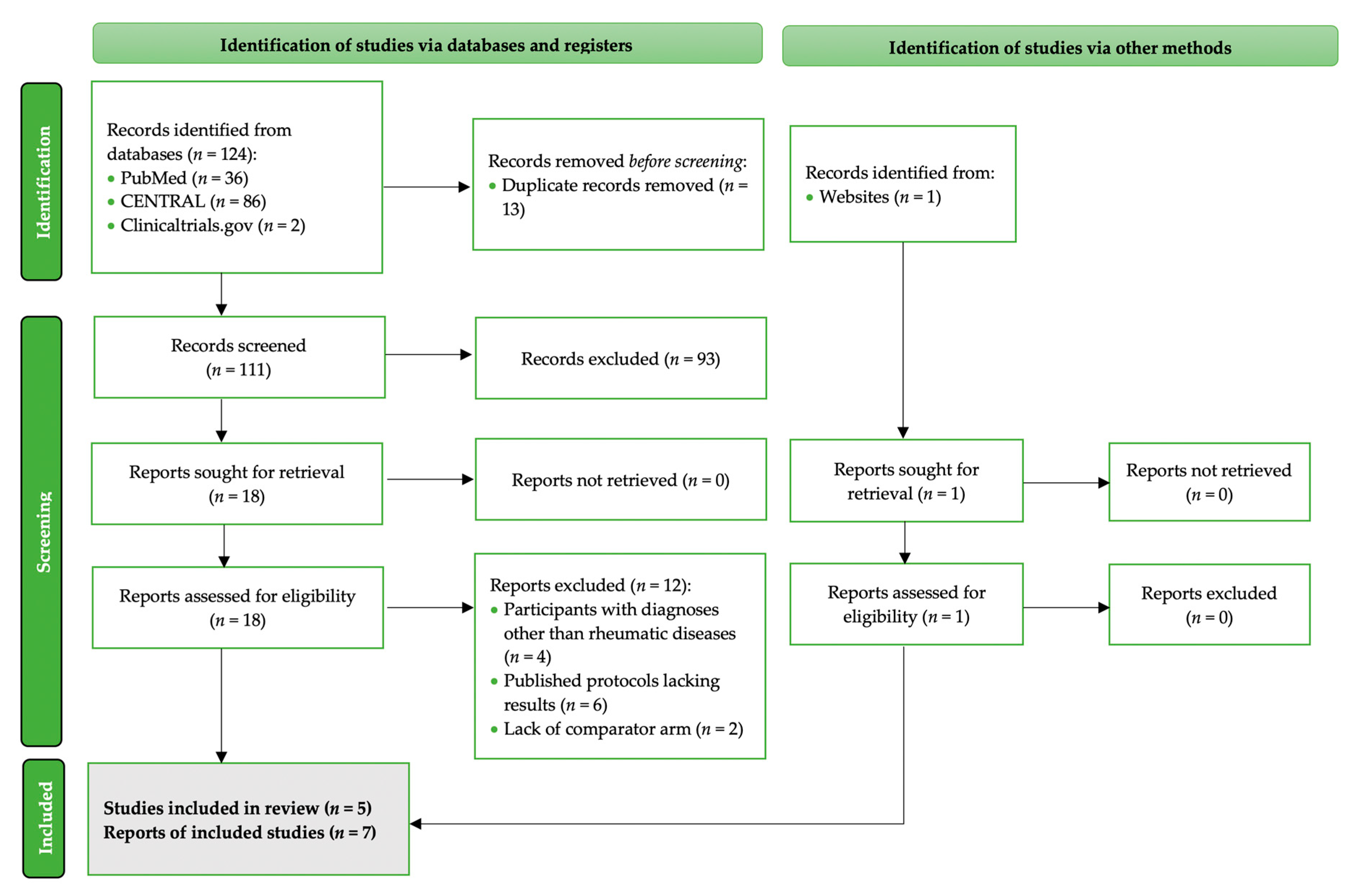
3.1. Search Results
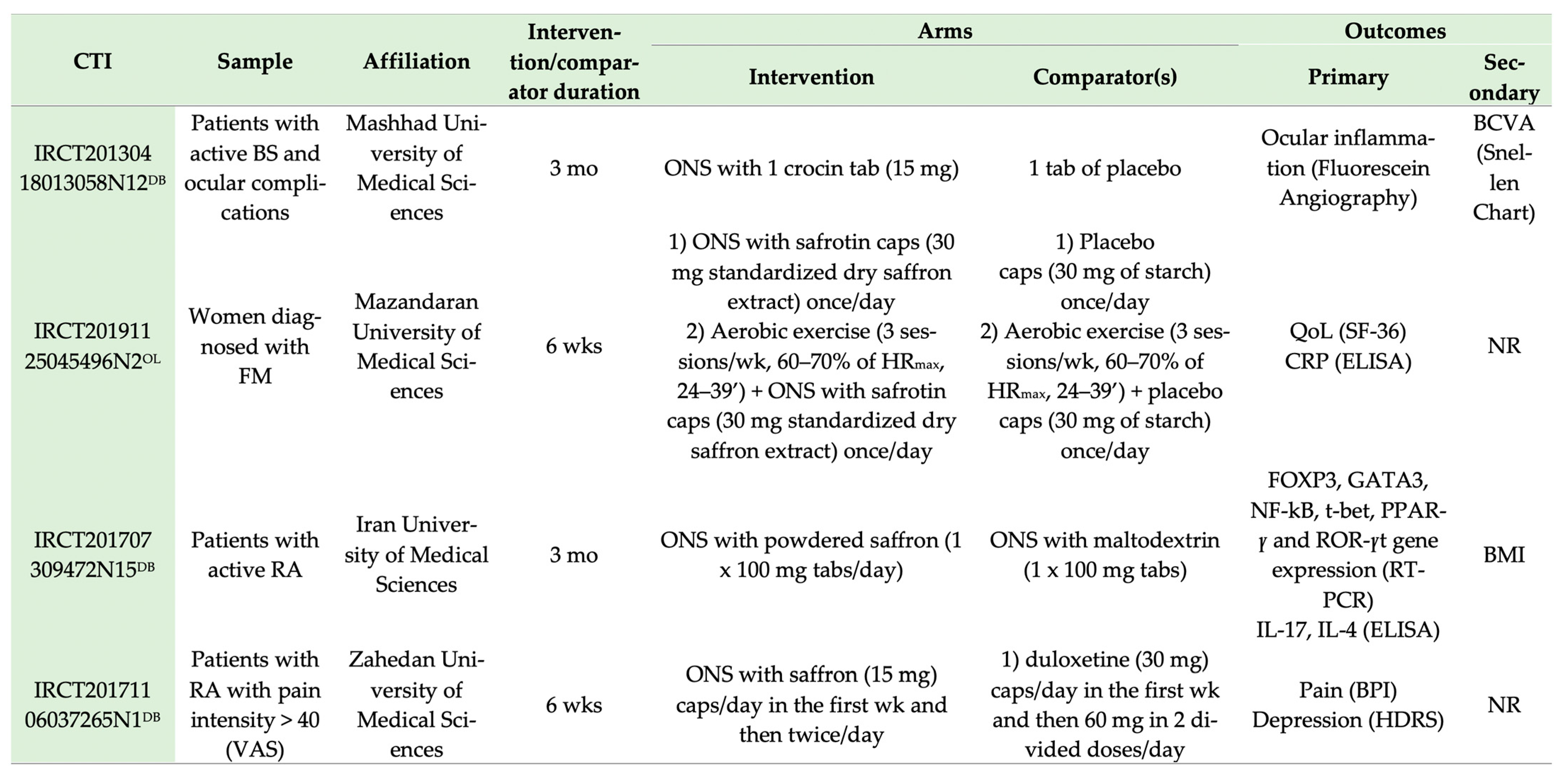
3.2. Characteristics of RCTs with Saffron Interventions in Patients with Rheumatic Diseases
3.2.1. RD Diagnoses
3.2.2. Trial Design and Origin
3.2.3. Intervention and Comparator Particularities
3.2.4. Sample Size
3.3. Outcomes Assessed in the Included Interventions
3.3.1. Sensation of Pain
3.3.2. Immune Response
3.3.3. Inflammation
3.3.4. Health Assessment, Depression and Fatigue
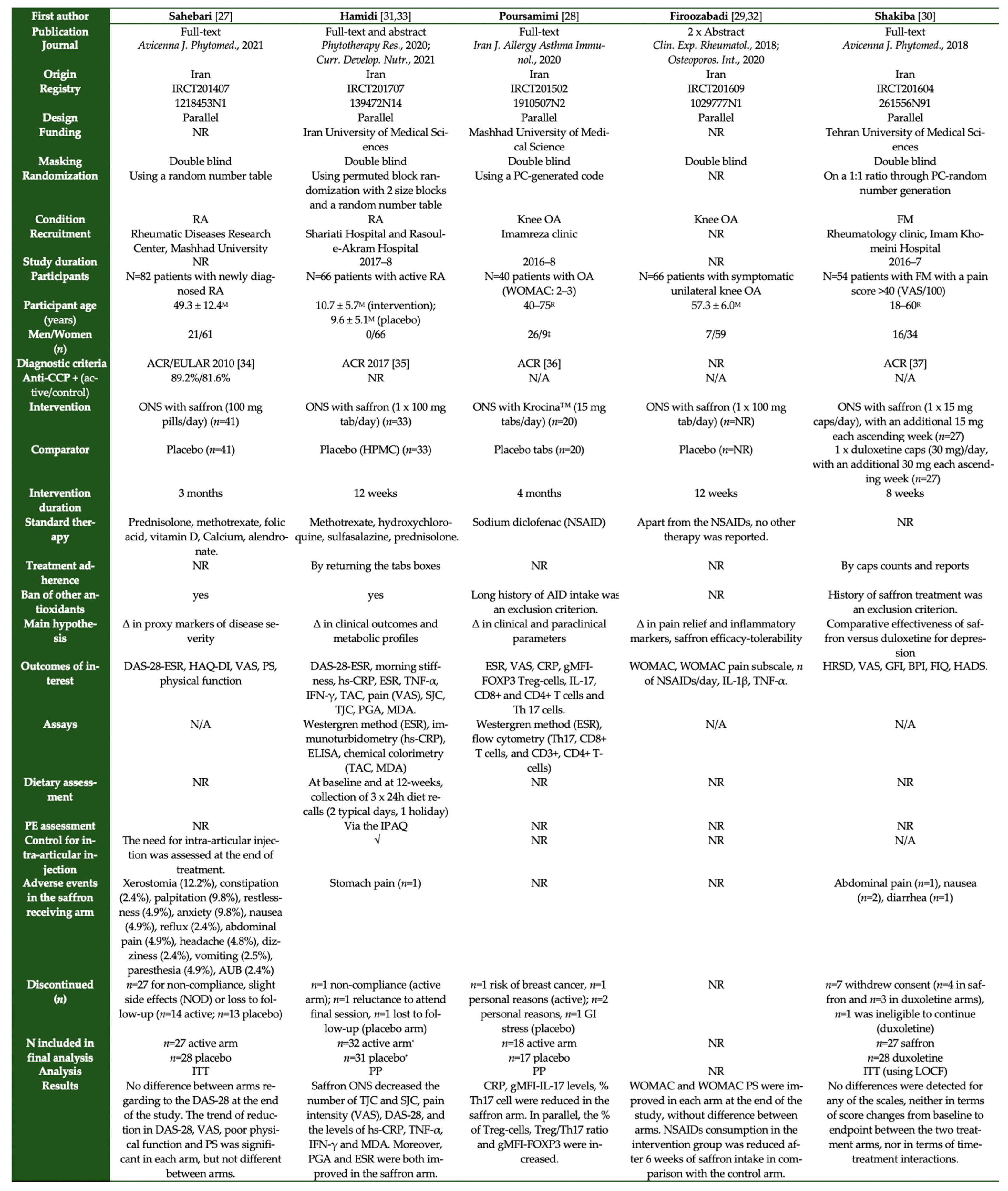
3.3.5. Antioxidant Status
3.3.6. Disease-Specific Scores
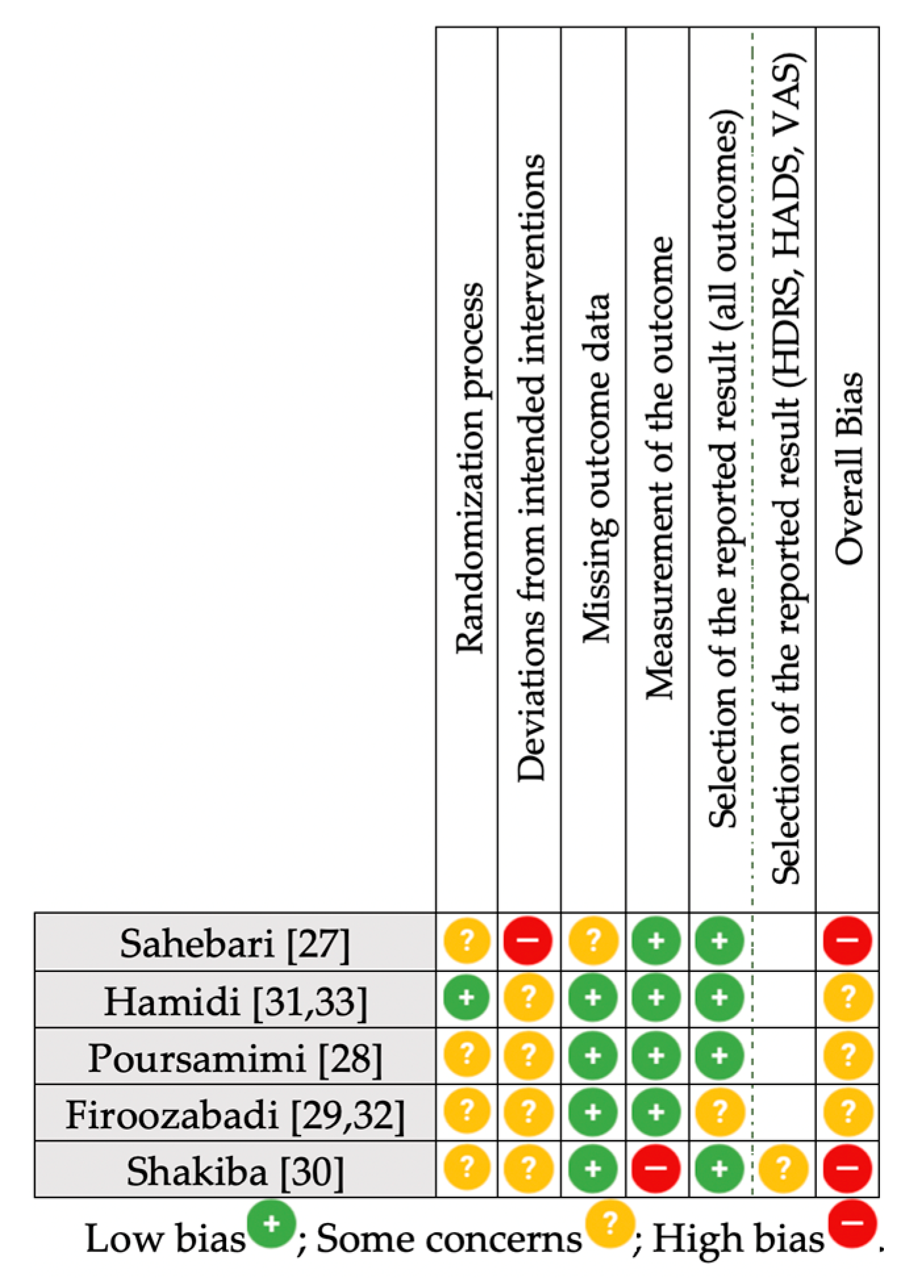
3.4. Risk of Bias Summary
3.5. Other Bias
3.5.1. Treatment Adherence
3.5.2. Dietary Intake and Exercise Patterns
3.6. Adherence to the CONSORT Statement for RCTs with Herbal Medicine
3.7. Results
3.8. Adverse Events
3.9. Synthesis without Meta-Analysis (SWiM)
4. Discussion
4.1. Methodological Limitations of the Included Trials
4.1.1. Assessment of Treatment Adherence Rate
4.1.2. Possible Cross-Treatment Effect
4.1.3. Differentiation between OA and RA
4.1.4. Effect of Lifestyle on RD Outcomes
4.1.5. Standardization of the Herbal Intervention and Reporting Quality of Formula Elaborations
4.1.6. Intervention Duration
4.1.7. Country of Origin
4.2. Ongoing Trials
4.3. Limitations of the Present Qualitative Synthesis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Safiri, S.; Kolahi, A.-A.; Cross, M.; Hill, C.; Smith, E.; Carson-Chahhoud, K.; Mansournia, M.A.; Almasi-Hashiani, A.; Ashrafi-Asgarabad, A.; Kaufman, J.; et al. Prevalence, Deaths, and Disability-Adjusted Life Years Due to Musculoskeletal Disorders for 195 Countries and Territories 1990–2017. Arthritis Rheumatol. 2021, 73, 702–714. [Google Scholar] [CrossRef]
- Simões, D.; Araújo, F.A.; Monjardino, T.; Severo, M.; Cruz, I.; Carmona, L.; Lucas, R. The population impact of rheumatic and musculoskeletal diseases in relation to other non-communicable disorders: Comparing two estimation approaches. Rheumatol. Int. 2018, 38, 905–915. [Google Scholar] [CrossRef] [PubMed]
- Ernst, E. Herbal medicine in the treatment of rheumatic diseases. Rheum. Dis. Clin. North Am. 2011, 37, 95–102. [Google Scholar] [CrossRef]
- Kolasinski, S.L. Herbal medicine for rheumatic diseases: Promises kept? Curr. Rheumatol. Rep. 2012, 14, 617–623. [Google Scholar] [CrossRef]
- Mauricio Marquez, A.; Evans, C.; Boltson, K.; Kesselman, M. Systematic Review Nutritional interventions and supplementation for rheumatoid arthritis patients: A systematic review for clinical application, Part 3: Fruits and Herbs. Curr. Rheumatol. Res. 2020, 1, 39–48. [Google Scholar]
- Letarouilly, J.-G.; Sanchez, P.; Nguyen, Y.; Sigaux, J.; Czernichow, S.; Flipo, R.-M.; Sellam, J.; Daïen, C. Efficacy of Spice Supplementation in Rheumatoid Arthritis: A Systematic Literature Review. Nutrients 2020, 12, 3800. [Google Scholar] [CrossRef]
- Grammatikopoulou, M.; Gkiouras, K.; Theodoridis, X.; Asteriou, E.; Forbes, A.; Bogdanos, D. Oral Adjuvant Curcumin Therapy for Attaining Clinical Remission in Ulcerative Colitis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2018, 10, 1737. [Google Scholar] [CrossRef] [PubMed]
- Singletary, K. Saffron: Potential Health Benefits. Nutr. Today 2020, 55, 294–303. [Google Scholar] [CrossRef]
- Asbaghi, O.; Sadeghian, M.; Sadeghi, O.; Rigi, S.; Tan, S.C.; Shokri, A.; Mousavi, S.M. Effects of saffron (Crocus sativus L.) supplementation on inflammatory biomarkers: A systematic review and meta-analysis. Phyther. Res. 2021, 35, 20–32. [Google Scholar] [CrossRef] [PubMed]
- Amin, B.; Hosseinzadeh, H. Analgesic and Anti-Inflammatory Effects of Crocus sativus L. (Saffron). In Bioactive Nutraceuticals and Dietary Supplements in Neurological and Brain Disease: Prevention and Therapy; Watson, R.R., Preedy, V.R., Eds.; Academic Press: Cambridge, MA, USA, 2015; pp. 319–324. [Google Scholar]
- Sohaei, S.; Hadi, A.; Karimi, E.; Arab, A. Saffron supplementation effects on glycemic indices: A systematic review and meta-analysis of randomized controlled clinical trials. Int. J. Food Prop. 2020, 23, 1386–1401. [Google Scholar] [CrossRef]
- Marx, W.; Lane, M.; Rocks, T.; Ruusunen, A.; Loughman, A.; Lopresti, A.; Marshall, S.; Berk, M.; Jacka, F.; Dean, O.M. Effect of saffron supplementation on symptoms of depression and anxiety: A systematic review and meta-analysis. Nutr. Rev. 2019, 77, 557–571. [Google Scholar] [CrossRef] [PubMed]
- Ayati, Z.; Yang, G.; Ayati, M.H.; Emami, S.A.; Chang, D. Saffron for mild cognitive impairment and dementia: A systematic review and meta-analysis of randomised clinical trials. BMC Complement. Med. Ther. 2020, 20, 1–10. [Google Scholar] [CrossRef]
- Zare, M.; Bazrafshan, A.; Afshar, R.M.; Mazloomi, S.M. Saffron (adjunct) for people with schizophrenia who have antipsychotic-induced metabolic syndrome. Cochrane Database Syst. Rev. 2018, 2018. [Google Scholar] [CrossRef]
- Setayesh, L.; Ashtary-Larky, D.; Clark, C.C.T.; Kelishadi, M.R.; Khalili, P.; Bagheri, R.; Asbaghi, O.; Suzuki, K. The Effect of Saffron Supplementation on Blood Pressure in Adults: A Systematic Review and Dose-Response Meta-Analysis of Randomized Controlled Trials. Nutrients 2021, 13, 2736. [Google Scholar] [CrossRef]
- Kunle, O.F.; Egharevba, H.O.; Ahmadu, P.O. Standardization of herbal medicines—A review. Int. J. Biodivers. Conserv. 2012, 4, 101–112. [Google Scholar] [CrossRef]
- Gagnier, J.J.; Boon, H.; Rochon, P.; Moher, D.; Barnes, J.; Bombardier, C. Reporting randomized, controlled trials of herbal interventions: An elaborated CONSORT statement. Ann. Intern. Med. 2006, 144, 364–367. [Google Scholar] [CrossRef] [PubMed]
- Gagnier, J.J.; Oltean, H.; Van Tulder, M.W.; Berman, B.M.; Bombardier, C.; Robbins, C.B. Herbal Medicine for Low Back Pain: A Cochrane Review. Spine 2016, 41, 116–133. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372. [Google Scholar] [CrossRef]
- Campbell, M.; McKenzie, J.E.; Sowden, A.; Katikireddi, S.V.; Brennan, S.E.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J.; et al. Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ 2020, 368, I6890. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Andrade, O.; Gomez, D.; Santos-Moreno, P.; Saavedra-Martinez, G. AB0378 Osteoarthritis is the Most Frequent Cause of Rheumathoid Arthritis Misdiagnosis in a Colombian Specialized Center. Ann. Rheum. Dis. 2015, 74. [Google Scholar] [CrossRef]
- Goel, A.; Aggarwal, B.B. Curcumin, the golden spice from Indian saffron, is a chemosensitizer and radiosensitizer for tumors and chemoprotector and radioprotector for normal organs. Nutr. Cancer 2010, 62, 919–930. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.; Elbers, R.; Blencowe, N.; Boutron, I.; Cates, C.; Cheng, H.-Y.; Corbett, M.; Eldridge, S.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. Br. Med. J. 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Thomson, H.J.; Thomas, S. The effect direction plot: Visual display of non-standardised effects across multiple outcome domains. Res. Synth. Methods 2013, 4, 95. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, J.E.; Brennan, S.E. Synthesizing and presenting findings using other methods. In Cochrane Handbook for Systematic Reviews of Interventions; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2019; pp. 321–347. [Google Scholar]
- Sahebari, M.; Heidari, H.; Nabavi, S.; Khodashahi, M.; Rezaieyazdi, Z.; Dadgarmoghaddam, M.; Hosseinzaheh, H.; Abbasi, S.; Hashemzadeh, K. A double-blind placebo-controlled randomized trial of oral saffron in the treatment of rheumatoid arthritis. Avicenna J. Phytomed. 2021, 11, 332. [Google Scholar] [CrossRef] [PubMed]
- Poursamimi, J.; Shariati-Sarabi, Z.; Tavakkol-Afshari, J.; Mohajeri, S.A.; Ghoryani, M.; Mohammadi, M. Immunoregulatory Effects of KrocinaTM, a Herbal Medicine Made of Crocin, on Osteoarthritis Patients: A Successful Clinical Trial in Iran. Iran. J. Allergy Asthma Immunol. 2020, 19, 253–263. [Google Scholar] [CrossRef]
- Firoozabadi, M.; Abdolahi, N.; Mirfeyzi, S. P976. Anti-inflammatory effect of saffron in knee osteoarthritis: A double blind clinical trial. Osteoporos. Int. 2020, 31, S488. [Google Scholar]
- Shakiba, M.; Moazen-Zadeh, E.; Noorbala, A.A.; Jafarinia, M.; Divsalar, P.; Kashani, L.; Shahmansouri, N.; Tafakhori, A.; Bayat, H.; Akhondzadeh, S. Saffron (Crocus sativus) versus duloxetine for treatment of patients with fibromyalgia: A randomized double-blind clinical trial. Avicenna J. Phytomed. 2018, 8, 513–523. [Google Scholar] [CrossRef]
- Aryaeian, N.; Hamidi, Z.; Shirani, F.; Hadidi, M.; Abolghasemi, J.; Moradi, N.; Fallah, S. The Effect of Saffron Supplement on Clinical Outcomes, Inflammatory and Oxidative Markers in Patients With Active Rheumatoid Arthritis. Curr. Dev. Nutr. 2021, 5, 1118. [Google Scholar] [CrossRef]
- Firoozabadi, M.; Aghei, M.; Mirfeizi, S.Z.; Roshandel, G.R.; Abdol Ahi, N. PT3:026 The effectiveness of saffron pill in treatment of osteoarthritis: A randomized, double-blind controlled trial. Clin. Exp. Rheumatol. 2018, 36, S62. [Google Scholar]
- Hamidi, Z.; Aryaeian, N.; Abolghasemi, J.; Shirani, F.; Hadidi, M.; Fallah, S.; Moradi, N. The effect of saffron supplement on clinical outcomes and metabolic profiles in patients with active rheumatoid arthritis: A randomized, double-blind, placebo-controlled clinical trial. Phyther. Res. 2020, 34, 1650–1658. [Google Scholar] [CrossRef] [PubMed]
- Aletaha, D.; Neogi, T.; Silman, A.J.; Funovits, J.; Felson, D.T.; Bingham, C.O.; Birnbaum, N.S.; Burmester, G.R.; Bykerk, V.P.; Cohen, M.D.; et al. Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. ARTHRITIS Rheum. 2010, 62, 2569–2581. [Google Scholar] [CrossRef] [PubMed]
- Mil, A.V.D.H.-V.; Zink, A. What is rheumatoid arthritis? Considering consequences of changed classification criteria. Ann. Rheum. Dis. 2017, 76, 315–317. [Google Scholar] [CrossRef]
- Altman, R.; Asch, E.; Bloch, D.; Bole, G.; Borenstein, D.; Brandt, K.; Christy, W.; Cooke, T.D.; Greenwald, R.; Hochberg, M.; et al. Development of criteria for the classification and reporting of osteoarthritis: Classification of osteoarthritis of the knee. Arthritis Rheum. 1986, 29, 1039–1049. [Google Scholar] [CrossRef]
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.-A.; Goldenberg, D.L.; Katz, R.S.; Mease, P.; Russell, A.S.; Russell, I.J.; Winfield, J.B.; Yunus, M.B. The American College of Rheumatology Preliminary Diagnostic Criteria for Fibromyalgia and Measurement of Symptom Severity. Arthritis Care Res. 2010, 62, 600–610. [Google Scholar] [CrossRef]
- Samisaz Pharmaceutical Company KROCINA|Sami Saz. Available online: http://samisaz.com (accessed on 22 November 2021).
- Anderson, J.; Caplan, L.; Yazdany, J.; Robbins, M.L.; Neogi, T.; Michaud, K.; Saag, K.G.; O’dell, J.R.; Kazi, S. Rheumatoid arthritis disease activity measures: American College of Rheumatology recommendations for use in clinical practice. Arthritis Care Res. 2012, 64, 640–647. [Google Scholar] [CrossRef]
- Cleeland, C.S.; Ryan, K.M. Pain assessment: Global use of the Brief Pain Inventory—PubMed. Ann. Acad. Med. Singap. 1994, 23, 129–138. [Google Scholar] [PubMed]
- Theiler, R.; Spielberger, J.; Bischoff, H.A.; Bellamy, N.; Huber, J.; Kroesen, S. Clinical evaluation of the WOMAC 3.0 OA Index in numeric rating scale format using a computerized touch screen version. Osteoarthr. Cartil. 2002, 10, 479–481. [Google Scholar] [CrossRef]
- Wolfe, F.; Michaud, K.; Pincus, T. Development and validation of the health assessment questionnaire II: A revised version of the health assessment questionnaire. Arthritis Rheum. 2004, 50, 3296–3305. [Google Scholar] [CrossRef]
- Pascoe, V.L.; Enamandram, M.; Corey, K.C.; Cheng, C.E.; Javorsky, E.J.; Sung, S.M.; Donahue, K.R.; Kimball, A.B. Using the Physician Global Assessment in a Clinical Setting to Measure and Track Patient Outcomes. JAMA Dermatol. 2015, 151, 375–381. [Google Scholar] [CrossRef]
- Belza, B.L. Comparison of self-reported fatigue in rheumatoid arthritis and controls—PubMed. J. Rheumatol. 1995, 22, 639–643. [Google Scholar]
- Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 62. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.; Becker, J.-C.; Teng, J.; Dougados, M.; Schiff, M.; Smolen, J.; Aletaha, D.; van Riel, P.L.C.M. Validation of the 28-joint Disease Activity Score (DAS28) and European League Against Rheumatism response criteria based on C-reactive protein against disease progression in patients with rheumatoid arthritis, and comparison with the DAS28 based on erythrocyte sedimentation rate. Ann. Rheum. Dis. 2009, 68, 954–960. [Google Scholar] [CrossRef]
- Burckhardt, C.S.; Clark, S.R.; Bennet, R.M. The fibromyalgia impact questionnaire: Development and validation—PubMed. J. Rheumatol. 1991, 18, 728–733. [Google Scholar] [PubMed]
- Ghavidel Parsa, B.; Amir Maafi, A.; Haghdoost, A.; Arabi, Y.; Khojamli, M.; Chatrnour, G.; Bidari, A. The validity and reliability of the Persian version of the Revised Fibromyalgia Impact Questionnaire. Rheumatol. Int. 2014, 34, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sport. Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.; Steer, R.; Brown, G. Beck Depression Inventory, 2nd ed.; Psychological Corporation: San Antonio, TX, USA, 1996. [Google Scholar]
- Husaini, A.M.; Jan, N.; Wani, G.A. Saffron: A potential drug-supplement for severe acute respiratory syndrome coronavirus (COVID) management. Heliyon 2021, 7, e07068. [Google Scholar] [CrossRef]
- Thushara, R.M.; Hemshekhar, M.; Paul, M.; Shanmuga Sundaram, M.; Shankar, R.L.; Kemparaju, K.; Girish, K.S. Crocin prevents sesamol-induced oxidative stress and apoptosis in human platelets. J. Thromb. Thrombolysis 2014, 38, 321–330. [Google Scholar] [CrossRef]
- Morvaridzadeh, M.; Agah, S.; Estêvão, M.D.; Hosseini, A.S.; Heydari, H.; Toupchian, O.; Abdollahi, S.; Persad, E.; Abu-Zaid, A.; Rezamand, G.; et al. Effect of saffron supplementation on oxidative stress parameters: A systematic review and meta-analysis of randomized placebo-controlled trials. Food Sci. Nutr. 2021, 9, 5819. [Google Scholar] [CrossRef]
- Tóth, B.; Hegyi, P.; Lantos, T.; Szakács, Z.; Kerémi, B.; Varga, G.; Tenk, J.; Pétervári, E.; Balaskó, M.; Rumbus, Z.; et al. The Efficacy of Saffron in the Treatment of Mild to Moderate Depression: A Meta-analysis. Planta Med. 2018, 85, 24–31. [Google Scholar] [CrossRef]
- Ghaderi, A.; Asbaghi, O.; Reiner, Ž.; Kolahdooz, F.; Amirani, E.; Mirzaei, H.; Banafshe, H.R.; Maleki Dana, P.; Asemi, Z. The effects of saffron (Crocus sativus L.) on mental health parameters and C-reactive protein: A meta-analysis of randomized clinical trials. Complement. Ther. Med. 2020, 48, 102250. [Google Scholar] [CrossRef]
- Christodoulou, E.; Kadoglou, N.P.; Kostomitsopoulos, N.; Valsami, G. Saffron: A natural product with potential pharmaceutical applications. J. Pharm. Pharmacol. 2015, 67, 1634–1649. [Google Scholar] [CrossRef]
- Pachikian, B.D.; Copine, S.; Suchareau, M.; Deldicque, L. Effects of Saffron Extract on Sleep Quality: A Randomized Double-Blind Controlled Clinical Trial. Nutrients 2021, 13, 1473. [Google Scholar] [CrossRef] [PubMed]
- Dai, L.; Chen, L.; Wang, W. Safety and Efficacy of Saffron (Crocus sativus L.) for Treating Mild to Moderate Depression: A Systematic Review and Meta-analysis. J. Nerv. Ment. Dis. 2020, 208, 269–276. [Google Scholar] [CrossRef]
- Khaksarian, M.; Behzadifar, M.; Behzadifar, M.; Alipour, M.; Jahanpanah, F.; Re, T.S.; Firenzuoli, F.; Zerbetto, R.; Bragazzi, N.L. The efficacy of Crocus sativus (Saffron) versus placebo and Fluoxetine in treating depression: A systematic review and meta-analysis. Psychol. Res. Behav. Manag. 2019, 12, 305. [Google Scholar] [CrossRef] [PubMed]
- Azimi, P.; Abrishami, R. Comparison of the Effects of Crocus Sativus and Mefenamic Acid on Primary Dysmenorrhea. J. Pharm. Care 2016, 4, 75–78. [Google Scholar]
- Kubo, I.; Kinst-Hori, I. Flavonols from saffron flower: Tyrosinase inhibitory activity and inhibition mechanism. J. Agric. Food Chem. 1999, 47, 4121–4125. [Google Scholar] [CrossRef]
- Hosseini, A.; Razavi, B.M.; Hosseinzadeh, H. Saffron (Crocus sativus) petal as a new pharmacological target: A review. Iran. J. Basic Med. Sci. 2018, 21, 1091–1099. [Google Scholar] [CrossRef] [PubMed]
- Bani, S.; Pandey, A.; Agnihotri, V.K.; Pathania, V.; Singh, B. Selective Th2 upregulation by crocus sativus: A neutraceutical spice. Evid. Based Complement. Altern. Med. 2010, 2011, 639862. [Google Scholar] [CrossRef]
- Chen, B.; Hou, Z.H.; Dong, Z.; Li, C.D. Crocetin downregulates the proinflammatory cytokines in methylcholanthrene-induced rodent tumor model and inhibits COX-2 expression in cervical cancer Cells. Biomed Res. Int. 2015, 2015. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ding, J.; Su, J.; Zhang, L.; Ma, J. Crocetin Activates Foxp3 Through TIPE2 in Asthma-Associated Treg Cells. Cell. Physiol. Biochem. 2015, 37, 2425–2433. [Google Scholar] [CrossRef]
- Khazdair, M.R.; Gholamnezhad, Z.; Rezaee, R.; Boskabady, M.H. A qualitative and quantitative comparison of Crocus sativus and Nigella sativa immunomodulatory effects. Biomed. Pharmacother. 2021, 140, 111774. [Google Scholar] [CrossRef] [PubMed]
- Eliasson, L.; Clifford, S.; Mulick, A.; Jackson, C.; Vrijens, B. How the EMERGE guideline on medication adherence can improve the quality of clinical trials. Br. J. Clin. Pharmacol. 2020, 86, 687–697. [Google Scholar] [CrossRef]
- Zhang, Z.; Peluso, M.J.; Gross, C.P.; Viscoli, C.M.; Kernan, W.N. Adherence reporting in randomized controlled trials. Clin. Trials 2014, 11, 195–204. [Google Scholar] [CrossRef]
- Murali, K.M.; Mullan, J.; Chen, J.H.C.; Roodenrys, S.; Lonergan, M. Medication adherence in randomized controlled trials evaluating cardiovascular or mortality outcomes in dialysis patients: A systematic review. BMC Nephrol. 2017, 18, 1–11. [Google Scholar] [CrossRef]
- Shipton, E.A.; Shipton, E.E. Vitamin D and pain: Vitamin D and its role in the aetiology and maintenance of chronic pain states and associated comorbidities. Pain Res. Treat. 2015, 2015, 904967. [Google Scholar] [CrossRef] [PubMed]
- Habib, A.M.; Nagi, K.; Thillaiappan, N.B.; Sukumaran, V.; Akhtar, S. Vitamin D and Its Potential Interplay With Pain Signaling Pathways. Front. Immunol. 2020, 820. [Google Scholar] [CrossRef]
- Vranou, P.; Gkoutzourelas, A.; Athanatou, D.; Zafiriou, E.; Grammatikopoulou, M.G.; Bogdanos, D.P. Let food be thy medicine: The case of the Mediterranean diet in rheumatoid arthritis. Mediterr. J. Rheumatol. 2020, in press. [Google Scholar] [CrossRef]
- Westerlind, H.; Palmqvist, I.; Saevarsdottir, S.; Alfredsson, L.; Klareskog, L.; Di Giuseppe, D. Is tea consumption associated with reduction of risk of rheumatoid arthritis? A Swedish case-control study. Arthritis Res. Ther. 2021, 23, 209. [Google Scholar] [CrossRef]
- Guagnano, M.T.; D’Angelo, C.; Caniglia, D.; Di Giovanni, P.; Celletti, E.; Sabatini, E.; Speranza, L.; Bucci, M.; Cipollone, F.; Paganelli, R. Improvement of Inflammation and Pain after Three Months’ Exclusion Diet in Rheumatoid Arthritis Patients. Nutrients 2021, 13, 3535. [Google Scholar] [CrossRef]
- Skyvalidas, D.N.; Mavropoulos, A.; Tsiogkas, S.; Dardiotis, E.; Liaskos, C.; Mamuris, Z.; Roussaki-Schulze, A.; Sakkas, L.A.; Zafiriou, E.; Bogdanos, D.P. Curcumin mediates attenuation of pro-inflammatory interferon γ and interleukin 17 cytokine responses in psoriatic disease, strengthening its role as a dietary immunosuppressant. Nutr. Res. 2020, 75, 95–108. [Google Scholar] [CrossRef]
- Nelson, J.; Sjöblom, H.; Gjertsson, I.; Ulven, S.M.; Lindqvist, H.M.; Bärebring, L. Do Interventions with Diet or Dietary Supplements Reduce the Disease Activity Score in Rheumatoid Arthritis? A Systematic Review of Randomized Controlled Trials. Nutrients 2020, 12, 2991. [Google Scholar] [CrossRef] [PubMed]
- Ali, R.; Rooman, M.; Mussarat, S.; Norin, S.; Ali, S.; Adnan, M.; Khan, S.N. A Systematic Review on Comparative Analysis, Toxicology, and Pharmacology of Medicinal Plants Against Haemonchus contortus. Front. Pharmacol. 2021, 12, 807. [Google Scholar] [CrossRef] [PubMed]
- Sachan, A.K.; Vishnoi, G.; Kumar, R. Need of standardization of herbal medicines in Modern era. Int. J. Phytomed. 2016, 8, 300–307. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines on Safety Monitoring of Herbal Medicines in Pharmacovigilance Systems; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Parveen, A.; Parveen, B.; Parveen, R.; Ahmad, S. Challenges and guidelines for clinical trial of herbal drugs. J. Pharm. Bioallied Sci. 2015, 7, 333. [Google Scholar] [CrossRef]
- Shekelle, P.G.; Morton, S.C.; Suttorp, M.J.; Buscemi, N.; Friesen, C. Challenges in systematic reviews of complementary and alternative medicine topics. Ann. Intern. Med. 2005, 142, 1042–1047. [Google Scholar] [CrossRef]
- Guo, R.; Canter, P.H.; Ernst, E. A systematic review of randomised clinical trials of individualised herbal medicine in any indication. Postgrad. Med. J. 2007, 83, 637. [Google Scholar] [CrossRef]
- Perry, R.; Leach, V.; Davies, P.; Penfold, C.; Ness, A.; Churchill, R. An overview of systematic reviews of complementary and alternative therapies for fibromyalgia using both AMSTAR and ROBIS as quality assessment tools. Syst. Rev. 2017, 6, 1–23. [Google Scholar] [CrossRef]
- Ernst, E. “First, do no harm” with complementary and alternative medicine. Trends Pharmacol. Sci. 2007, 28, 48–50. [Google Scholar] [CrossRef]
- UNICEF/UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases (TDR). Operational Guidance: Information Needed to Support Clinical Trials of Herbal products; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- Cheng, C.W.; Wu, T.X.; Shang, H.C.; Li, Y.P.; Altman, D.G.; Moher, D.; Bian, Z.X. CONSORT Extension for Chinese Herbal Medicine Formulas 2017: Recommendations, Explanation, and Elaboration (Traditional Chinese Version). Ann. Intern. Med. 2017, 167, W7–W20. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. General Guidelines for Methodologies on Research and Evaluation of Traditional Medicine; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- World Health Organization. Annex 1 WHO Guidelines for Selecting Marker Substances of Herbal Origin for Quality Control of Herbal Medicines; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Li, Y.; Shen, Y.; Yao, C.-L.; Guo, D.-A. Quality assessment of herbal medicines based on chemical fingerprints combined with chemometrics approach: A review. J. Pharm. Biomed. Anal. 2020, 185, 113215. [Google Scholar] [CrossRef]
- Zhang, X.; Aixinjueluo, Q.Y.; Li, S.Y.; Song, L.L.; Lau, C.T.; Tan, R.; Bian, Z.X. Reporting quality of Cochrane systematic reviews with Chinese herbal medicines. Syst. Rev. 2019, 8, 1–11. [Google Scholar] [CrossRef]
- Gamret, A.C.; Price, A.; Fertig, R.M.; Lev-Tov, H.; Nichols, A.J. Complementary and Alternative Medicine Therapies for Psoriasis: A Systematic Review. JAMA Dermatol. 2018, 154, 1330–1337. [Google Scholar] [CrossRef]
- Heitmar, R.; Brown, J.; Kyrou, I. Saffron (Crocus sativus L.) in Ocular Diseases: A Narrative Review of the Existing Evidence from Clinical Studies. Nutrients 2019, 11, 649. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Ke, L.; Li, J.; Zhao, H.; Lu, T.; Mentis, A.F.A.; Wang, Y.; Wang, Z.; Polissiou, M.G.; Tang, L.; et al. Saffron (Crocus sativus L.) and health outcomes: A meta-research review of meta-analyses and an evidence mapping study. Phytomedicine 2021, 91, 153699. [Google Scholar] [CrossRef] [PubMed]
- Mosihuzzaman, M. Herbal Medicine in Healthcare-An Overview. Nat. Prod. Commun. 2012, 7, 807–812. [Google Scholar] [CrossRef]
- Ernst, E.; Pittler, M.H. Alternative therapy bias. Nature 1997, 385, 480. [Google Scholar] [CrossRef]
- CAMbrella—A Pan-European Research Network for Complementary and Alternative Medicine (CAM) Final Report Summary. Available online: https://cordis.europa.eu/project/id/241951/reporting (accessed on 22 November 2021).
 not reported;
not reported;  reported.
reported.
 not reported;
not reported;  reported.
reported.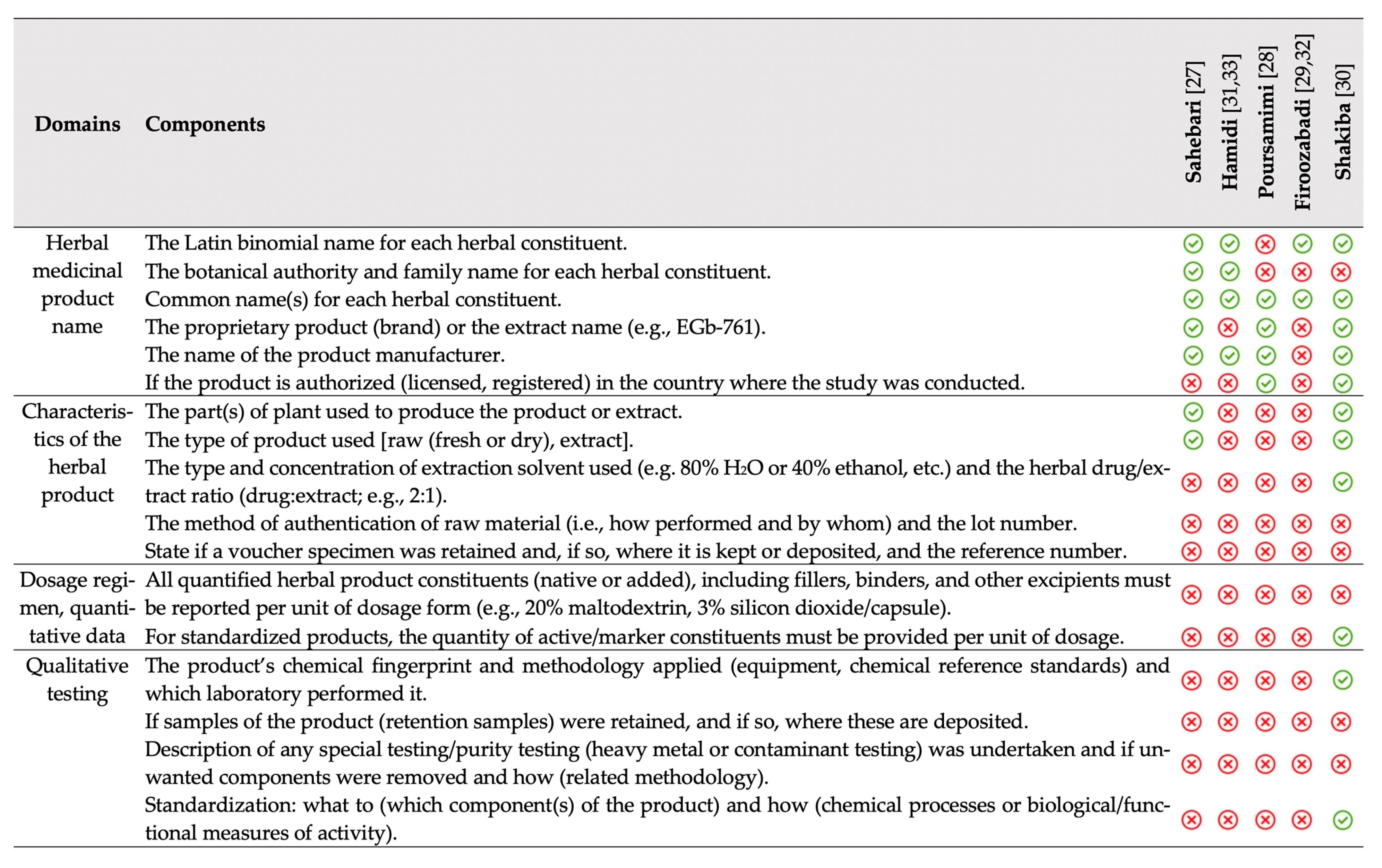
 no change.
no change.
 no change.
no change.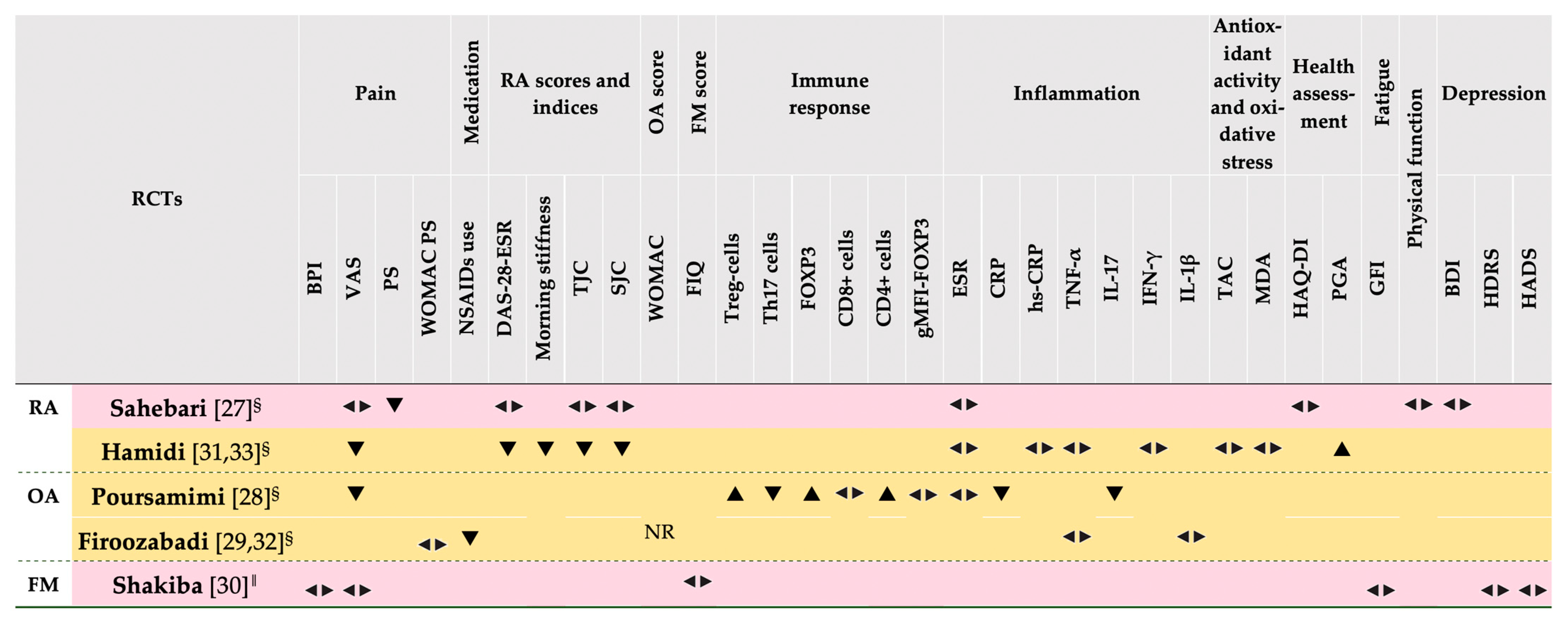
| Population | Patients with any rheumatic disease diagnosis |
| Intervention | Saffron (tabs, sachets, pills, tea, etc.) |
| Comparison | Placebo, or any other intervention |
| Outcomes | Any disease-specific (immediate/intermediate) or comorbidity-related outcome |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsiogkas, S.G.; Grammatikopoulou, M.G.; Gkiouras, K.; Zafiriou, E.; Papadopoulos, I.; Liaskos, C.; Dardiotis, E.; Sakkas, L.I.; Bogdanos, D.P. Effect of Crocus sativus (Saffron) Intake on Top of Standard Treatment, on Disease Outcomes and Comorbidities in Patients with Rheumatic Diseases: Synthesis without Meta-Analysis (SWiM) and Level of Adherence to the CONSORT Statement for Randomized Controlled Trials Delivering Herbal Medicine Interventions. Nutrients 2021, 13, 4274. https://doi.org/10.3390/nu13124274
Tsiogkas SG, Grammatikopoulou MG, Gkiouras K, Zafiriou E, Papadopoulos I, Liaskos C, Dardiotis E, Sakkas LI, Bogdanos DP. Effect of Crocus sativus (Saffron) Intake on Top of Standard Treatment, on Disease Outcomes and Comorbidities in Patients with Rheumatic Diseases: Synthesis without Meta-Analysis (SWiM) and Level of Adherence to the CONSORT Statement for Randomized Controlled Trials Delivering Herbal Medicine Interventions. Nutrients. 2021; 13(12):4274. https://doi.org/10.3390/nu13124274
Chicago/Turabian StyleTsiogkas, Sotirios G., Maria G. Grammatikopoulou, Konstantinos Gkiouras, Efterpi Zafiriou, Iordanis Papadopoulos, Christos Liaskos, Efthimios Dardiotis, Lazaros I. Sakkas, and Dimitrios P. Bogdanos. 2021. "Effect of Crocus sativus (Saffron) Intake on Top of Standard Treatment, on Disease Outcomes and Comorbidities in Patients with Rheumatic Diseases: Synthesis without Meta-Analysis (SWiM) and Level of Adherence to the CONSORT Statement for Randomized Controlled Trials Delivering Herbal Medicine Interventions" Nutrients 13, no. 12: 4274. https://doi.org/10.3390/nu13124274
APA StyleTsiogkas, S. G., Grammatikopoulou, M. G., Gkiouras, K., Zafiriou, E., Papadopoulos, I., Liaskos, C., Dardiotis, E., Sakkas, L. I., & Bogdanos, D. P. (2021). Effect of Crocus sativus (Saffron) Intake on Top of Standard Treatment, on Disease Outcomes and Comorbidities in Patients with Rheumatic Diseases: Synthesis without Meta-Analysis (SWiM) and Level of Adherence to the CONSORT Statement for Randomized Controlled Trials Delivering Herbal Medicine Interventions. Nutrients, 13(12), 4274. https://doi.org/10.3390/nu13124274








