Dietary Management of Eosinophilic Esophagitis: Tailoring the Approach
Abstract
:1. Introduction
2. Literature Search
3. Therapeutic Endpoints in EoE
4. Rationale for Avoidance Strategies in EoE: Food Is the Trigger
5. Balancing Pros and Cons of Dietary Management
6. Tailoring the Diet to the Patient and Available Resources
7. Diets
7.1. Elemental Diet
7.2. Empiric Elimination Diets
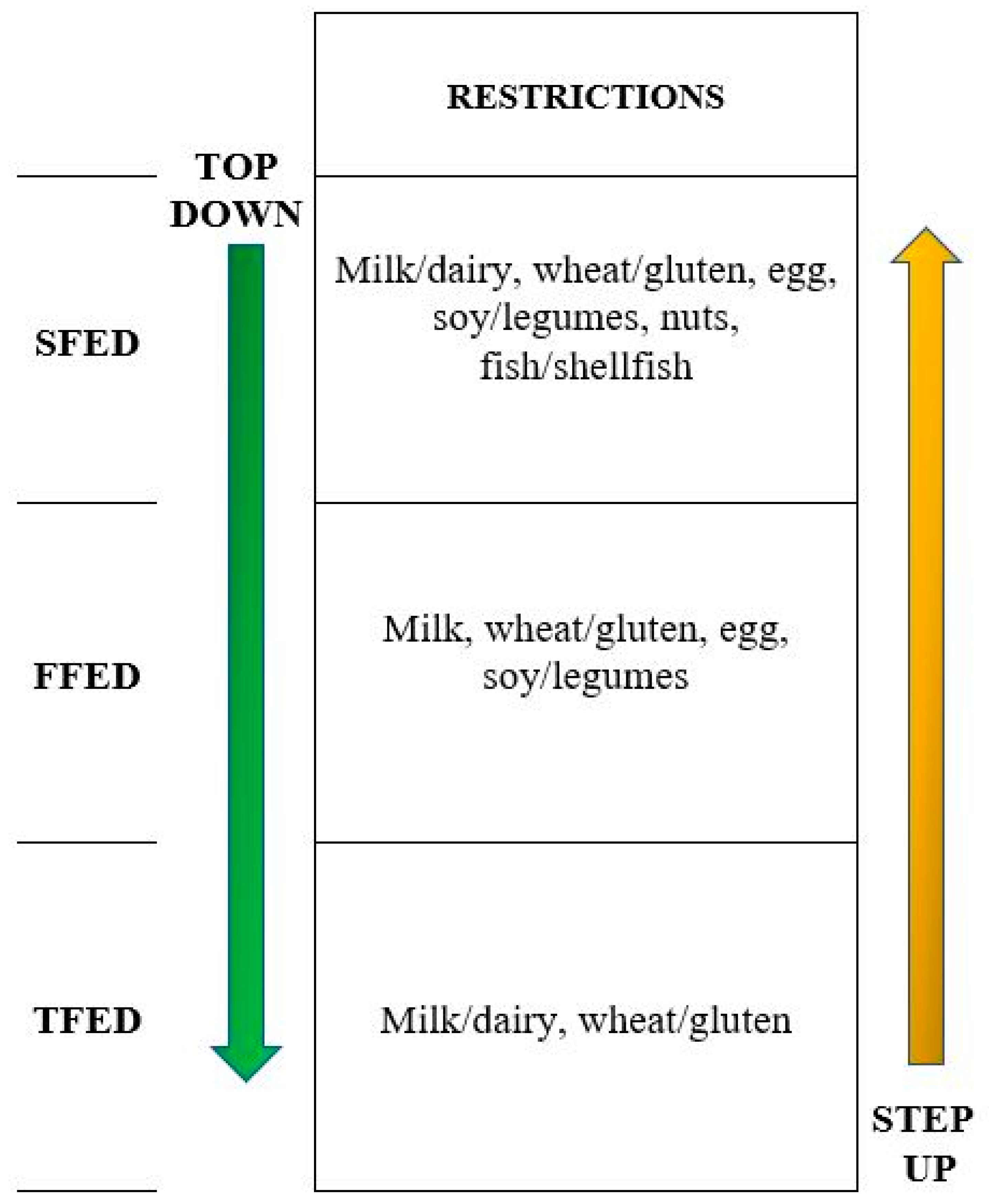
7.2.1. SFED: The “Classic” Top-Down Approach
7.2.2. Four-FoodElimination Diet
7.2.3. The Step-Up Approach
7.2.4. One-Food Elimination Diets
7.3. Target Elimination Diet
8. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liacouras, C.A.; Furuta, G.T.; Hirano, I.; Atkins, D.; Attwood, S.E.; Bonis, P.A.; Burks, A.W.; Chehade, M.; Collins, M.H.; Dellon, E.S.; et al. Eosinophilic esophagitis: Updated consensus recommendations for children and adults. J. Allergy Clin. Immunol. 2011, 128, 3–20.e6. [Google Scholar] [CrossRef] [Green Version]
- Dellon, E.S.; Liacouras, C.A.; Molina-Infante, J.; Furuta, G.T.; Spergel, J.M.; Zevit, N.; Spechler, S.J.; Attwood, S.E.; Straumann, A.; Aceves, S.S.; et al. Updated International Consensus Diagnostic Criteria for Eosinophilic Esophagitis: Proceedings of the AGREE Conference. Gastroenterology 2018, 155, 1022–1033.e10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Visaggi, P.; Savarino, E.; Sciume, G.; Di Chio, T.; Bronzini, F.; Tolone, S.; Frazzoni, M.; Pugno, C.; Ghisa, M.; Bertani, L.; et al. Eosinophilic esophagitis: Clinical, endoscopic, histologic and therapeutic differences and similarities between children and adults. Ther. Adv. Gastroenterol. 2021, 14, 1756284820980860. [Google Scholar] [CrossRef] [PubMed]
- Arias, A.; Perezmartinez, I.; Tenías, J.M.; Lucendo, A.J. Systematic review with meta-analysis: The incidence and prevalence of eosinophilic oesophagitis in children and adults in population-based studies. Aliment. Pharmacol. Ther. 2015, 43, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Arias, Á.; Lucendo, A.J. Epidemiology and risk factors for eosinophilic esophagitis: Lessons for clinicians. Expert Rev. Gastroenterol. Hepatol. 2020, 14, 1069–1082. [Google Scholar] [CrossRef]
- Kinoshita, Y.; Ishimura, N.; Oshima, N.; Ishihara, S. Systematic review: Eosinophilic esophagitis in Asian countries. World J. Gastroenterol. 2015, 21, 8433–8440. [Google Scholar] [CrossRef] [PubMed]
- Mukkada, V.; Falk, G.W.; Eichinger, C.S.; King, D.; Todorova, L.; Shaheen, N.J. Health-Related Quality of Life and Costs Associated with Eosinophilic Esophagitis: A Systematic Review. Clin. Gastroenterol. Hepatol. 2018, 16, 495–503.e8. [Google Scholar] [CrossRef] [Green Version]
- Dellon, E.S.; Hirano, I. Epidemiology and Natural History of Eosinophilic Esophagitis. Gastroenterology 2018, 154, 319–332.e3. [Google Scholar] [CrossRef] [PubMed]
- Sciumé, G.D.; Visaggi, P.; Sostilio, A.; Tarducci, L.; Pugno, C.; Frazzoni, M.; Ricchiuti, A.; Bellini, M.; Giannini, E.G.; Marchi, S.; et al. Eosinophilic esophagitis: Novel concepts regarding pathogenesis and clinical manifestations. Minerva Gastroenterol. Dietol. 2021. [Google Scholar] [CrossRef]
- Rothenberg, M.E.; Spergel, J.M.; Sherrill, J.D.; Annaiah, K.; Martin, L.J.; Cianferoni, A.; Gober, L.; Kim, C.; Glessner, J.; Frackelton, E.; et al. Common variants at 5q22 associate with pediatric eosinophilic esophagitis. Nat. Genet. 2010, 42, 289–291. [Google Scholar] [CrossRef]
- Litosh, V.A.; Rochman, M.; Rymer, J.K.; Porollo, A.; Kottyan, L.C.; Rothenberg, M.E. Calpain-14 and its association with eosinophilic esophagitis. J. Allergy Clin. Immunol. 2017, 139, 1762–1771.e7. [Google Scholar] [CrossRef] [PubMed]
- Reed, C.C.; Iglesia, E.G.; Commins, S.P.; Dellon, E.S. Seasonal exacerbation of eosinophilic esophagitis histologic activity in adults and children implicates role of aeroal-lergens. Ann. Allergy Asthma Immunol. 2019, 122, 296–301. [Google Scholar] [CrossRef]
- Ram, G.; Lee, J.; Ott, M.; Brown-Whitehorn, T.F.; Cianferoni, A.; Shuker, M.; Wang, M.-L.; Verma, R.; Liacouras, C.A.; Spergel, J.M. Seasonal exacerbation of esophageal eosinophilia in children with eosinophilic esophagitis and allergic rhinitis. Ann. Allergy, Asthma Immunol. 2015, 115, 224–228.e1. [Google Scholar] [CrossRef] [PubMed]
- Hill, D.A.; Grundmeier, R.W.; Ramos, M.; Spergel, J.M. Eosinophilic Esophagitis Is a Late Manifestation of the Allergic March. J. Allergy Clin. Immunol. Pract. 2018, 6, 1528–1533. [Google Scholar] [CrossRef] [PubMed]
- Richter, J.E. Esophageal dilation in eosinophilic esophagitis. Best Pract. Res. Clin. Gastroenterol. 2015, 29, 815–828. [Google Scholar] [CrossRef] [PubMed]
- Visaggi, M.P.; Ibraheim, H.; Wong, T.; Jafari, J.; Dunn, J.; Zeki, S. OWE-031 Oesophageal aperistalsis is under investigated in those without achalasia or reflux. Gut 2018, 67, A210. [Google Scholar]
- Savarino, E.; Gemignani, L.; Zentilin, P.; De Bortoli, N.; Malesci, A.; Mastracci, L.; Fiocca, R.; Savarino, V. Achalasia With Dense Eosinophilic Infiltrate Responds to Steroid Therapy. Clin. Gastroenterol. Hepatol. 2011, 9, 1104–1106. [Google Scholar] [CrossRef]
- Ghisa, M.; Laserra, G.; Marabotto, E.; Ziola, S.; Tolone, S.; De Bortoli, N.; Frazzoni, M.; Mauro, A.; Penagini, R.; Savarino, V.; et al. Achalasia and Obstructive Motor Disorders Are Not Uncommon in Patients with Eosinophilic Esophagitis. Clin. Gastroenterol. Hepatol. 2020. [Google Scholar] [CrossRef]
- Savarino, E.V.; Tolone, S.; Bartolo, O.; de Cassan, C.; Caccaro, R.; Galeazzi, F.; Nicoletti, L.; Salvador, R.; Martinato, M.; Costantini, M.; et al. The GerdQ questionnaire and high resolution manometry support the hypothesis that proton pump inhibi-tor-responsive oesophageal eosinophilia is a GERD-related phenomenon. Aliment. Pharmacol. Ther. 2016, 44, 522–530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dellon, E.S.; Cotton, C.C.; Gebhart, J.H.; Higgins, L.L.; Beitia, R.; Woosley, J.T.; Shaheen, N.J. Accuracy of the Eosinophilic Esophagitis Endoscopic Reference Score in Diagnosis and Determining Response to Treatment. Clin. Gastroenterol. Hepatol. 2016, 14, 31–39. [Google Scholar] [CrossRef] [Green Version]
- Lucendo, A.J.; Molina-Infante, J.; Arias, Á.; von Arnim, U.; Bredenoord, A.J.; Bussmann, C.; Amil Dias, J.; Bove, M.; González-Cervera, J.; Larsson, H.; et al. Guidelines on eosinophilic esophagitis: Evidence-based statements and recommendations for diagnosis and man-agement in children and adults. United Eur. Gastroenterol. J. 2017, 5, 335–358. [Google Scholar] [CrossRef] [Green Version]
- Laserna-Mendieta, E.J.; Casabona, S.; Savarino, E.; Perelló, A.; Pérez-Martínez, I.; Guagnozzi, D.; Barrio, J.; Guardiola, A.; Asensio, T.; de la Riva, S.; et al. Efficacy of Therapy for Eosinophilic Esophagitis in Real-World Practice. Clin. Gastroenterol. Hepatol. 2020, 18, 2903–2911.e4. [Google Scholar] [CrossRef]
- Laserna-Mendieta, E.J.; Casabona, S.; Guagnozzi, D.; Savarino, E.; Perelló, A.; Guardiola-Arévalo, A.; Barrio, J.; Pérez-Martínez, I.; Krarup, A.L.; Alcedo, J.; et al. Efficacy of proton pump inhibitor therapy for eosinophilic oesophagitis in 630 patients: Results from the EoE connect registry. Aliment. Pharmacol. Ther. 2020, 52, 798–807. [Google Scholar] [CrossRef] [PubMed]
- Chehade, M.; Brown, S. Elimination diets for eosinophilic esophagitis: Making the best choice. Expert Rev. Clin. Immunol. 2020, 16, 679–687. [Google Scholar] [CrossRef]
- Dellon, E.S.; Gupta, S.K. A Conceptual Approach to Understanding Treatment Response in Eosinophilic Esophagitis. Clin. Gastroenterol. Hepatol. 2019, 17, 2149–2160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Safroneeva, E.; Straumann, A.; Coslovsky, M.; Zwahlen, M.; Kuehni, C.E.; Panczak, R.; Haas, N.A.; Alexander, J.A.; Dellon, E.S.; Gonsalves, N.; et al. Symptoms Have Modest Accuracy in Detecting Endoscopic and Histologic Remission in Adults WithEosino-philic Esophagitis. Gastroenterology 2016, 150, 581–590.e4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Safroneeva, E.; Straumann, A.; Schoepfer, A.M. Latest Insights on the Relationship between Symptoms and Biologic Findings in Adults with Eosinophilic Esophagitis. Gastrointest. Endosc. Clin. N. Am. 2018, 28, 35–45. [Google Scholar] [CrossRef]
- Eke, R.; Li, T.; White, A.; Tariq, T.; Markowitz, J.; Lenov, A. Systematic review of histological remission criteria in eosinophilic esophagitis. JGH Open 2018, 2, 158–165. [Google Scholar] [CrossRef]
- Warners, M.J.; Hindryckx, P.; Levesque, B.G.; Parker, C.E.; Shackelton, L.M.; Khanna, R.; Sandborn, W.J.; D’Haens, G.R.; Feagan, B.G.; Bredenoord, A.J.; et al. Systematic Review: Disease Activity Indices in Eosinophilic Esophagitis. Am. J. Gastroenterol. 2017, 112, 1658–1669. [Google Scholar] [CrossRef] [PubMed]
- Schoepfer, A.; Blanchard, C.; Dawson, H.; Lucendo, A.; Mauro, A.; Ribi, C.; Safroneeva, E.; Savarino, E.V.; Penagini, R. Eosinophilic esophagitis: Latest insights from diagnosis to therapy. Ann. N. Y. Acad. Sci. 2018, 1434, 84–93. [Google Scholar] [CrossRef] [PubMed]
- De Bortoli, N.; Penagini, R.; Savarino, E.; Marchi, S. Eosinophilic esophagitis: Update in diagnosis and management. Position paper by the Italian Society of Gastro-enterology and Gastrointestinal Endoscopy (SIGE). Dig. Liver Dis. 2017, 49, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Hirano, I.; Moy, N.; Heckman, M.G.; Thomas, C.S.; Gonsalves, N.; Achem, S.R. Endoscopic assessment of the oesophageal features of eosinophilic oesophagitis: Validation of a novel classification and grading system. Gut 2013, 62, 489–495. [Google Scholar] [CrossRef]
- Lucendo, A.J. Nutritional approach to eosinophilic esophagitis: Which diet and when. Minerva Gastroenterol. Dietol. 2020. [Google Scholar] [CrossRef]
- Kelly, K.J.; Lazenby, A.J.; Rowe, P.C.; Yardley, J.H.; Perman, J.A.; Sampson, H.A. Eosinophilic esophagitis attributed to gastroesophageal reflux: Improvement with an amino acid-based formula. Gastroenterology 1995, 109, 1503–1512. [Google Scholar] [CrossRef]
- Frazzoni, M.; Penagini, R.; Frazzoni, L.; De Bortoli, N.; Mauro, A.; Tolone, S.; Bertani, H.; Conigliaro, R.; Savarino, E.V. Mo1135—Role of Reflux in the Pathogenesis of Eosinophilic Esophagitis—Comprehensive Appraisal with Off- and On-Ppi Impedance-Ph Monitoring. Am. J. Gastroenterol. 2019, 156. [Google Scholar] [CrossRef]
- Kagalwalla, A.F.; Sentongo, T.A.; Ritz, S.; Hess, T.; Nelson, S.P.; Emerick, K.M.; Melin–Aldana, H.; Li, B. Effect of Six-Food Elimination Diet on Clinical and Histologic Outcomes in Eosinophilic Esophagitis. Clin. Gastroenterol. Hepatol. 2006, 4, 1097–1102. [Google Scholar] [CrossRef]
- Henderson, C.J.; Abonia, J.P.; King, E.C.; Putnam, P.E.; Collins, M.H.; Franciosi, J.P.; Rothenberg, M.E. Comparative dietary therapy effectiveness in remission of pediatric eosinophilic esophagitis. J. Allergy Clin. Immunol. 2012, 129, 1570–1578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lucendo, A.J.; Arias, Á.; González-Cervera, J.; Yagüe-Compadre, J.L.; Guagnozzi, D.; Angueira, T.; Jiménez-Contreras, S.; González-Castillo, S.; Rodríguez-Domíngez, B.; De Rezende, L.C.; et al. Empiric 6-food elimination diet induced and maintained prolonged remission in patients with adult eosinophilic esophagitis: A prospective study on the food cause of the disease. J. Allergy Clin. Immunol. 2013, 131, 797–804. [Google Scholar] [CrossRef]
- Gonsalves, N.; Yang, G.Y.; Doerfler, B.; Ritz, S.; Ditto, A.M.; Hirano, I. Elimination diet effectively treats eosinophilic esophagitis in adults; food reintroduction identifies causative factors. Gastroenterology 2012, 142, 1451–1459.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cianferoni, A.; Shuker, M.; Brown-Whitehorn, T.; Hunter, H.; Venter, C.; Spergel, J.M. Food avoidance strategies in eosinophilic oesophagitis. Clin. Exp. Allergy 2019, 49, 269–284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, D.A.; Spergel, J.M. The Immunologic Mechanisms of Eosinophilic Esophagitis. Curr. Allergy Asthma Rep. 2016, 16, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Simon, D.; Cianferoni, A.; Spergel, J.M.; Aceves, S.; Holbreich, M.; Venter, C.; Rothenberg, M.E.; Terreehorst, I.; Muraro, A.; Lucendo, A.J.; et al. Eosinophilic esophagitis is characterized by a non-IgE-mediated food hypersensitivity. Allergy 2016, 71, 611–620. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Molina-Infante, J.; Lucendo, A.J. Dietary therapy for eosinophilic esophagitis. J. Allergy Clin. Immunol. 2018, 142, 41–47. [Google Scholar] [CrossRef] [Green Version]
- Arias, Á.; González-Cervera, J.; Tenias, J.M.; Lucendo, A.J. Efficacy of dietary interventions for inducing histologic remission in patients with eosinophilic esophagitis: A system-atic review and meta-analysis. Gastroenterology 2014, 146, 1639–1648. [Google Scholar] [CrossRef] [PubMed]
- Molina-Infante, J.; Arias, Á.; Alcedo, J.; Garcia-Romero, R.; Casabona-Frances, S.; Prieto-Garcia, A.; Modolell, I.; Gonzalez-Cordero, P.L.; Perez-Martinez, I.; Martin-Lorente, J.L.; et al. Step-up empiric elimination diet for pediatric and adult eosinophilic esophagitis: The 2-4-6 study. J. Allergy Clin. Immunol. 2018, 141, 1365–1372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colson, D.; Kalach, N.; Soulaines, P.; Vannerom, Y.; Campeotto, F.; Talbotec, C.; Chatenoud, L.; Hankard, R.; Dupont, C. The Impact of Dietary Therapy on Clinical and Biologic Parameters of Pediatric Patients with Eosinophilic Esophagitis. J. Allergy Clin. Immunol. Pract. 2014, 2, 587–593. [Google Scholar] [CrossRef]
- Delaney, A.L.; Arvedson, J.C. Development of swallowing and feeding: Prenatal through first year of life. Dev. Disabil. Res. Rev. 2008, 14, 105–117. [Google Scholar] [CrossRef] [PubMed]
- Lucendo, A.J.; Arias-González, L.; Molina-Infante, J.; Arias, Á. Systematic review: Health-related quality of life in children and adults with eosinophilic oesophagitis-instruments for measurement and determinant factors. Aliment. Pharmacol. Ther. 2017, 46, 401–409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cotton, C.C.; Hiller, S.; Green, D.J.; Wolf, W.A.; Wheeler, S.B.; Shaheen, N.J.; Dellon, E.S. 4 Six-Food Elimination Diet or Topical Steroids for First-Line Treatment of Eosinophilic Esophagitis: A Cost-Utility Analysis. Gastroenterology 2015, 148, S-2. [Google Scholar] [CrossRef]
- Kim, J.; Kwon, J.; Noh, G.; Lee, S.S. The effects of elimination diet on nutritional status in subjects with atopic dermatitis. Nutr. Res. Pract. 2013, 7, 488–494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sova, C.; Feuling, M.B.; Baumler, M.; Gleason, L.; Tam, J.S.; Zafra, H.; Goday, P.S. Systematic Review of Nutrient Intake and Growth in Children with Multiple IgE-Mediated Food Allergies. Nutr. Clin. Pract. 2013, 28, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Groetch, M.; Venter, C.; Skypala, I.; Vlieg-Boerstra, B.; Grimshaw, K.; Durban, R.; Cassin, A.; Henry, M.; Kliewer, K.; Kabbash, L.; et al. Dietary Therapy and Nutrition Management of Eosinophilic Esophagitis: A Work Group Report of the American Academy of Allergy, Asthma, and Immunology. J. Allergy Clin. Immunol. Pract. 2017, 5, 312–324.e29. [Google Scholar] [CrossRef]
- Wolf, W.A.; Huang, K.Z.; Durban, R.; Iqbal, Z.J.; Robey, B.S.; Khalid, F.J.; Dellon, E.S. The Six-Food Elimination Diet for Eosinophilic Esophagitis Increases Grocery Shopping Cost and Complexity. Dysphagia 2016, 31, 765–770. [Google Scholar] [CrossRef] [PubMed]
- Kagalwalla, A.F.; Wechsler, J.B.; Amsden, K.; Schwartz, S.; Makhija, M.; Olive, A.; Davis, C.M.; Manuel-Rubio, M.; Marcus, S.; Shaykin, R.; et al. Efficacy of a 4-Food Elimination Diet for Children with Eosinophilic Esophagitis. Clin. Gastroenterol. Hepatol. 2017, 15, 1698–1707.e7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chehade, M.; Jones, S.M.; Pesek, R.D.; Burks, A.W.; Vickery, B.P.; Wood, R.A.; Leung, D.Y.; Furuta, G.T.; Fleischer, D.M.; Henning, A.K.; et al. Phenotypic Characterization of Eosinophilic Esophagitis in a Large Multicenter Patient Population from the Con-sortium for Food Allergy Research. J. Allergy Clin. Immunol. Pract. 2018, 6, 1534–1544.e5. [Google Scholar] [CrossRef] [PubMed]
- Molina-Infante, J.; Arias, A.; Barrio, J.; Rodríguez-Sánchez, J.; Sanchez-Cazalilla, M.; Lucendo, A.J. Four-food group elimination diet for adult eosinophilic esophagitis: A prospective multicenter study. J. Allergy Clin. Immunol. 2014, 134, 1093–1099.e1. [Google Scholar] [CrossRef]
- Liacouras, C.A.; Spergel, J.M.; Ruchelli, E.; Verma, R.; Mascarenhas, M.; Semeao, E.; Flick, J.; Kelly, J.; Brown–Whitehorn, T.; Mamula, P.; et al. Eosinophilic Esophagitis: A 10-Year Experience in 381 Children. Clin. Gastroenterol. Hepatol. 2005, 3, 1198–1206. [Google Scholar] [CrossRef]
- Kagalwalla, A.F.; Amsden, K.; Shah, A.; Ritz, S.; Manuel-Rubio, M.; Dunne, K.; Nelson, S.P.; Wershil, B.K.; Melin-Aldana, H. Cow’s Milk Elimination. J. Pediatr. Gastroenterol. Nutr. 2012, 55, 711–716. [Google Scholar] [CrossRef]
- De Agustin, J.; Sanz, N.; Canals, M.; Alvarez, E.; Morales, J.; Soler, J.; Ollero, J.; Vazquez, J. Successful medical treatment of two patients with eosinophilic oesophagitis. J. Pediatr. Surg. 2002, 37, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Al-Hussaini, A.; Al-Idressi, E.; Al-Zahrani, M. The role of allergy evaluation in children with eosinophilic esophagitis. J. Gastroenterol. 2013, 48, 1205–1212. [Google Scholar] [CrossRef] [PubMed]
- Pascual, J.M.R.; Caballer, B.D.L.H.; Verge, C.R.; Cepeda, S.T.; Ariño, G.R.; López, J.M.R.; Salces, C.C. Allergy assessment in children with eosinophilic esophagitis. J. Investig. Allergol. Clin. Immunol. 2011, 21, 59–65. [Google Scholar]
- Peterson, K.A.; Byrne, K.R.; Vinson, L.A.; Ying, J.; Boynton, K.K.; Fang, J.C.; Gleich, G.J.; Adler, D.G.; Clayton, F. Elemental Diet Induces Histologic Response in Adult Eosinophilic Esophagitis. Am. J. Gastroenterol. 2013, 108, 759–766. [Google Scholar] [CrossRef] [PubMed]
- Warners, M.J.; Vlieg-Boerstra, B.J.; Verheij, J.; Van Rhijn, B.D.; Van Ampting, M.T.J.; Harthoorn, L.F.; De Jonge, W.J.; Smout, A.J.P.M.; Bredenoord, A.J. Elemental diet decreases inflammation and improves symptoms in adult eosinophilic oesophagitis patients. Aliment. Pharmacol. Ther. 2017, 45, 777–787. [Google Scholar] [CrossRef] [Green Version]
- Molina-Infante, J.; Lucendo, A.J. Approaches to diet therapy for eosinophilic esophagitis. Curr. Opin. Gastroenterol. 2020, 36, 359–363. [Google Scholar] [CrossRef]
- Spergel, J.M.; Brown-Whitehorn, T.F.; Cianferoni, A.; Shuker, M.; Wang, M.-L.; Verma, R.; Liacouras, C.A. Identification of causative foods in children with eosinophilic esophagitis treated with an elimination diet. J. Allergy Clin. Immunol. 2012, 130, 461–467.e5. [Google Scholar] [CrossRef]
- Philpott, H.; Nandurkar, S.; Royce, S.G.; Thien, F.; Gibson, P.R. A prospective open clinical trial of a proton pump inhibitor, elimination diet and/or budesonide for eosinophilic oesophagitis. Aliment. Pharmacol. Ther. 2016, 43, 985–993. [Google Scholar] [CrossRef]
- Wolf, W.A.; Jerath, M.R.; Sperry, S.L.W.; Shaheen, N.J.; Dellon, E.S. Dietary Elimination Therapy Is an Effective Option for Adults with Eosinophilic Esophagitis. Clin. Gastroenterol. Hepatol. 2014, 12, 1272–1279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kagalwalla, A.F.; Shah, A.; Li, B.U.; Sentongo, T.A.; Ritz, S.; Manuel-Rubio, M.; Jacques, K.; Wang, D.; Melin-Aldana, H.; Nelson, S.P. Identification of specific foods responsible for inflammation in children with eosinophilic esophagitis success-fully treated with empiric elimination diet. J. Pediatr. Gastroenterol. Nutr. 2011, 53, 145–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Warners, M.; Vlieg-Boerstra, B.; Bredenoord, A. Elimination and elemental diet therapy in eosinophilic oesophagitis. Best Pract. Res. Clin. Gastroenterol. 2015, 29, 793–803. [Google Scholar] [CrossRef]
- Spergel, J.M.; Shuker, M. Nutritional Management of Eosinophilic Esophagitis. Gastrointest. Endosc. Clin. N. Am. 2008, 18, 179–194. [Google Scholar] [CrossRef] [PubMed]
- Dellon, E.S.; Liacouras, C.A. Advances in Clinical Management of Eosinophilic Esophagitis. Gastroenterology 2014, 147, 1238–1254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, A.; Robison, R.; Cai, M.; Singh, A.M. Natural History of Food-Triggered Atopic Dermatitis and Development of Immediate Reactions in Children. J. Allergy Clin. Immunol. Pract. 2016, 4, 229–236.e1. [Google Scholar] [CrossRef] [Green Version]
- Hill, D.A.; Shuker, M.; Cianferoni, A.; Wong, T.; Ruchelli, E.; Spergel, J.M.; Brown-Whitehorn, T.F. The development of IgE-mediated immediate hypersensitivity after the diagnosis of eosinophilic esophagitis to the same food. J. Allergy Clin. Immunol. Pract. 2015, 3, 123–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lucendo, A.J. Meta-Analysis-Based Guidance for Dietary Management in Eosinophilic Esophagitis. Curr. Gastroenterol. Rep. 2015, 17, 464. [Google Scholar] [CrossRef] [PubMed]
- Reed, C.C.; Fan, C.; Koutlas, N.T.; Shaheen, N.J.; Dellon, E.S. Food elimination diets are effective for long-term treatment of adults with eosinophilic oesophagitis. Aliment. Pharmacol. Ther. 2017, 46, 836–844. [Google Scholar] [CrossRef]
- Ooi, C.Y.; Day, A.S.; Jackson, R.; Bohane, T.D.; Tobias, V.; Lemberg, D.A. Eosinophilic esophagitis in children with celiac disease. J. Gastroenterol. Hepatol. 2008, 23, 1144–1148. [Google Scholar] [CrossRef] [PubMed]
- Leslie, C.; Mews, C.; Charles, A.; Ravikumara, M. Celiac Disease and Eosinophilic Esophagitis: A True Association. J. Pediatr. Gastroenterol. Nutr. 2010, 50, 397–399. [Google Scholar] [CrossRef]
- Kliewer, K.; Aceves, S.S.; Atkins, D.; Bonis, P.A.; Chehade, M.; Collins, M.H.; Dellon, E.S.; Fei, L.; Gupta, S.K.; Kagalwalla, A.F.; et al. 817—Efficacy of 1-Food and 4-Food Elimination Diets for Pediatric Eosinophilic Esophagitis in a Randomized Multi-Site Study. Gastroenterology 2019, 156, S-172. [Google Scholar] [CrossRef]
- Hoofien, A.; Dias, J.A.; Malamisura, M.; Rea, F.; Chong, S.; Oudshoorn, J.; Nijenhuis-Hendriks, D.; Otte, S.; Papadopoulou, A.; Romano, C.; et al. Pediatric Eosinophilic Esophagitis: Results of the European Retrospective Pediatric Eosinophilic Esophagitis Reg-istry (RetroPEER). J. Pediatr. Gastroenterol. Nutr. 2019, 68, 552–558. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.; Goodine, S.; Samela, K.; Vance, K.S.; Chatfield, B.; Wang, Z.; Sayej, W.N. Efficacy of Dairy Free Diet and 6-Food Elimination Diet as Initial Therapy for Pediatric Eosinophilic Esophagitis: A Retrospective Single-Center Study. Pediatr. Gastroenterol. Hepatol. Nutr. 2020, 23, 79–88. [Google Scholar] [CrossRef]
- Panel, N.S.E. Guidelines for the Diagnosis and Management of Food Allergy in the United States: Report of the NIAID-Sponsored Expert Panel. J. Allergy Clin. Immunol. 2010, 126, S1–S58. [Google Scholar]
- Heine, R.G.; Verstege, A.; Mehl, A.; Staden, U.; Niggemann, B.; Rolinck-Werninghaus, C. Proposal for a standardized interpretation of the atopy patch test in children with atopic dermatitis and suspected food allergy. Pediatr. Allergy Immunol. 2006, 17, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Spergel, J.M.; Brown-Whitehorn, T.; Beausoleil, J.L.; Shuker, M.; Liacouras, C.A. Predictive values for skin prick test and atopy patch test for eosinophilic esophagitis. J. Allergy Clin. Immunol. 2007, 119, 509–511. [Google Scholar] [CrossRef]
- Spergel, J.M.; Andrews, T.; Brown-Whitehorn, T.F.; Beausoleil, J.L.; Liacouras, C.A. Treatment of eosinophilic esophagitis with specific food elimination diet directed by a combination of skin prick and patch tests. Ann. Allergy Asthma Immunol. 2005, 95, 336–343. [Google Scholar] [CrossRef]
- Molina-Infante, J.; Martin-Noguerol, E.; Alvarado-Arenas, M.; Porcel-Carreño, S.L.; Jimenez-Timon, S.; Hernandez-Arbeiza, F.J. Selective elimination diet based on skin testing has suboptimal efficacy for adult eosinophilic esophagitis. J. Allergy Clin. Immunol. 2012, 130, 1200–1202. [Google Scholar] [CrossRef] [PubMed]
- Warners, M.J.; Terreehorst, I.; Van den Wijngaard, R.M.; Akkerdaas, J.; van Esch, B.C.; van Ree, R.; Versteeg, S.A.; Smout, A.J.; Bredenoord, A.J. Abnormal Responses to Local Esophageal Food Allergen Injections in Adult Patients with Eosinophilic Esopha-gitis. Gastroenterology 2018, 154, 57–60.e2. [Google Scholar] [CrossRef] [PubMed]
| Outcome Measures | Histology | Symptoms | Endoscopy | |
|---|---|---|---|---|
| Treatment Response | ||||
| Normalization | <1 eos/hpf a | Decrease >90% in symptoms score * | Resolution of endoscopic findings, EREFS b < 2 | |
| Response | 14 -1 eos/hpf | Decrease 30–90% in symptoms score | Improvement of endoscopic findings, EREFS ≥ 2 | |
| Non-Response | ≥15 eos/hpf | Decrease < 30% in symptoms score | Persistence of endoscopic findings similar to baseline | |
| Type of Diet | Adults, % (95% CI) | Children, % (95% CI) | Overall, % (95% CI) |
|---|---|---|---|
| Elemental | 94.4 | 90.4 (83.5–95.5) | 90.8 (84.7–95.5) |
| SFED | 71.3 (61.7–80) | 72.8 (62.5–82) | 72.1 (65.8–78.1) |
| FFED | 46.2 | 60 | 53.4 (35.7–70.6) |
| TFED | 44 | 40 | 43 |
| Gluten-free | 88.8 (50.5–99.1) | 45.5 (2.6–93.8) | 58.7 (23.1–89.7) |
| Milk-free | 100 | 66.3 (44.7–84.8) | 68.2 (47.8–85.6) |
| Target | 32.2 (17.8–48.7) | 47.9 (36.8–59.1) | 45.5 (35.4–55.7) |
| Advantages of Diets | Disadvantages of Diets |
|---|---|
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Visaggi, P.; Mariani, L.; Pardi, V.; Rosi, E.M.; Pugno, C.; Bellini, M.; Zingone, F.; Ghisa, M.; Marabotto, E.; Giannini, E.G.; et al. Dietary Management of Eosinophilic Esophagitis: Tailoring the Approach. Nutrients 2021, 13, 1630. https://doi.org/10.3390/nu13051630
Visaggi P, Mariani L, Pardi V, Rosi EM, Pugno C, Bellini M, Zingone F, Ghisa M, Marabotto E, Giannini EG, et al. Dietary Management of Eosinophilic Esophagitis: Tailoring the Approach. Nutrients. 2021; 13(5):1630. https://doi.org/10.3390/nu13051630
Chicago/Turabian StyleVisaggi, Pierfrancesco, Lucia Mariani, Veronica Pardi, Emma Maria Rosi, Camilla Pugno, Massimo Bellini, Fabiana Zingone, Matteo Ghisa, Elisa Marabotto, Edoardo G. Giannini, and et al. 2021. "Dietary Management of Eosinophilic Esophagitis: Tailoring the Approach" Nutrients 13, no. 5: 1630. https://doi.org/10.3390/nu13051630
APA StyleVisaggi, P., Mariani, L., Pardi, V., Rosi, E. M., Pugno, C., Bellini, M., Zingone, F., Ghisa, M., Marabotto, E., Giannini, E. G., Savarino, V., Marchi, S., Savarino, E. V., & de Bortoli, N. (2021). Dietary Management of Eosinophilic Esophagitis: Tailoring the Approach. Nutrients, 13(5), 1630. https://doi.org/10.3390/nu13051630









