Abstract
Osteoarthritis (OA) is considered one of the most common joint disorders worldwide and its prevalence is constantly increasing due to the global longevity and changes in eating habits and lifestyle. In this context, the role of gut microbiota (GM) in the pathogenesis of OA is still unclear. Perturbation of GM biodiversity and function, defined as ‘gut dysbiosis’, might be involved in the development of inflammaging, one of the main risk factors of OA development. It is well known that physical exercise could play a key role in the prevention and treatment of several chronic diseases including OA, and it is recommended by several guidelines as a first line intervention. Several studies have shown that physical exercise could modulate GM composition, boosting intestinal mucosal immunity, increasing the Bacteroidetes–Firmicutes ratio, modifying the bile acid profile, and improving the production of short chain fatty acids. Moreover, it has been shown that low intensity exercise might reduce the risk of gastrointestinal diseases, confirming the hypothesis of a strict correlation between skeletal muscle and GM. However, up to date, there is still a lack of clinical trials focusing on this research field. Therefore, in this narrative, we aimed to summarize the state-of-the-art of the literature regarding the correlation between these conditions, supporting the hypothesis of a ‘gut–joint axis’ and highlighting the role of physical exercise combined with adequate diet and probiotic supplements in rebalancing microbial dysbiosis.
1. Introduction
Osteoarthritis (OA) is the most common musculoskeletal disease, characterized by progressive articular cartilage loss, formation of osteophytes, subchondral bone remodeling, and chronic joint inflammation []. OA mainly targets the hip and knee joints, although other skeletal sites (i.e., hands, feet, spine) might be affected by this condition []. In particular, knee OA has a prevalence of 3.8% and an incidence of 12% in the elderly population and occurs with joint pain and peri-articular muscle weakness with a subsequent loss of function, increased disability, and reduction of health-related quality of life [,]. Indeed, an early diagnosis of OA is crucial to set up a prompt, effective, and patient-oriented treatment in order to prevent the age-related degenerative progression of this pathological condition []. The etiology of OA still remains unknown, but several risk factors have been identified such as age, sex, obesity, diet, physical inactivity, abnormal loading of the joints, metabolic syndrome, and inflammaging []. These two latter conditions are key components of OA onset and evolution, and recently the microbial dysbiosis induced by quantitative and qualitative alterations of the gut microbiota (GM) has been shown to sustain a chronic systemic low-grade inflammation, boosting the main pathophysiological mechanisms underpinning OA [].
The GM colonizes the entire gastrointestinal tract in a variable way and represents a real ecosystem, weighing about 1.5 kg, and is composed of more than 1014 bacteria and more than 1000 species as well as fungi, viruses, phages, parasites, and archea []. The most representative bacterial phyla of healthy GM are Bacteroidetes and Firmicutes, followed by Actinobacteria, Fusobacteria, and Proteobacteria, whereas the most representative genera are Bacteroides, Faecalibacterium, and Bifidobacterium []. GM has several functions such as nutrient absorption, maintenance of metabolic homeostasis, protection from infections, and development of systemic and mucosal immunity [,]. Modifications in the GM composition and metabolic activity might alter the immune response and host metabolism, leading to a constant low-grade inflammation status with consequent development of musculoskeletal impairment and frailty [,]. Furthermore, an expert consensus of the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases has recently hypothesized that GM is a major hidden risk factor for OA [].
Several studies [,,] have hypothesized the linkage between GM and osteoarthritis, taking into account the potential correlations between serum levels of bacterial metabolites and joint degeneration, however, at present, no systematic reviews have clearly described this topic.
Moreover, it has been recently hypothesized that physical exercise could also play a key role in modifying GM composition [] and at the same time, it could reduce the risk of gastrointestinal diseases [] such as inflammatory bowel disease, considering the emergent well-studied relationship between muscle function and GM [,,,].
In this narrative review, we aimed to show the state-of-the-art about the previously hypothesized correlations between GM alterations and OA in order to highlight new potential therapeutic directions and types of intervention in the ‘gut–joint axis’ modulation.
2. Inflammaging
The association between OA and low-grade systemic and local inflammation is well known [,]; indeed, OA etiopathogenic mechanisms might include epigenetic alterations, mitochondrial dysfunction, cellular senescence, and an age-related increased production of proinflammatory mediators, resulting in a pro-inflammatory state, referred to as ‘inflammaging’ [,].
The presence of physiological TGF-β signaling is mandatory for the maintenance of correct architecture and functioning of the articular cartilage []. The binding of TGF-β to its type II receptor leads to the recruitment and phosphorylation of a type I receptor. In more detail, TGF-β could signal both via the canonical type I receptor ALK5 (TGFBR1) or via the ALK1 (ACVRL1) receptor in chondrocytes [,], and a positive correlation between the ALK1 expression levels and MMP13 expression in human OA cartilage has been previously demonstrated []. Therefore, an adequate balance between ALK5 and ALK1 is mandatory to maintain cartilage homeostasis and the loss of ALK5 signaling could result in the loss of cartilage integrity []. Indeed, the ALK1/ALK5 ratio was demonstrated to be significantly increased in old C57Bl/6 mice compared to the young ones, leading TGF-β signaling via the Smad1/5/8 route and chondrocyte differentiation into cells with an autolytic phenotype []. Furthermore, the chronic systemic inflammation in the geriatric population is sustained by pro-inflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-a), whose serum levels commonly increase with age and are strongly correlated with the risk of OA progression [,].
A direct correlation between aging and gut dysbiosis has been previously demonstrated and is mainly characterized by an increase of pro-inflammatory anaerobes species and a consistent decrease in anti-inflammatory species such as Faecalibacterium prauznitzii []. As evidence of these hypotheses, it was later shown how longevity was inversely correlated with the alpha diversity of GM [,]. Finally, a typical feature of the aging process is the so-called “leaky gut syndrome”, an increased intestinal permeability leading to the translocation of microbial products through the intestinal tight junctions, resulting in endotoxemia and consequently in a pro-inflammatory status [].
A possible link between gut dysbiosis and OA might be suggested by the correlation between the serum levels of bacterial metabolites and joint degeneration []. This correlation has been described in rodent models and humans affected by OA and is characterized by increased levels of circulatory inflammatory markers including bacterially produced lipopolysaccharides (LPS) [,], suggesting that microbiome-derived proinflammatory metabolites could play a putative role in OA pathogenesis. Moreover, it has recently been shown that the subchondral dysbiosis resulting from the bacterial translocation from GM to the joint, might support the development of OA []. Therefore, considering gut dysbiosis and the leaky gut syndrome as cofactors in the development of inflammaging and consequently of OA [], it is likely to hypothesize the existence of a ‘gut–joint axis’ [,,,].
3. Obesity and Metabolic Syndrome
Diet is one of the major environmental factors contributing to the inter-individual differences in physiologic GM microbiota composition [,]. Nutrients are fundamental not only for human health, but also for the well-being of the trillions of microbes that compose the GM []. It has been demonstrated that a high-fat diet was associated with a reduction of Bacteroidetes and an overgrowth of opportunistic pathogens, promoting leaky gut syndrome, and enhancing systemic inflammation and insulin resistance []. In contrast, the production of short-chain fatty acids (SCFAs) by healthy gut bacteria such as Faecalibacterium, Succinivibrio, and Butyricimonas are able to induce an increase of glucose uptake and insulin sensitivity []. Similarly, mice models have shown that SCFAs might have a key role in maintaining bone homeostasis, downregulating the pro-inflammatory stimuli sustained by regulatory T-cells and inhibiting bone resorption through a direct inhibition of osteoclast activity [].
It is important to underline the role of an adequate diet and the use of dietary supplements in the ‘active aging’ population [,]. Indeed, these two interventions combined with vitamin D and amino acid supplementation and physical exercise could prevent several sequelae of the aging process including sarcopenia, as shown by several studies in the literature [,,,,,,]. Finally, it has been demonstrated that there is a strong correlation between the adherence to a Mediterranean diet and a lower risk of OA manifestation, mediated by the well-known anti-inflammatory activity of fibers []. Taken together, these findings suggest that a rich in fiber nutritional approach like the Mediterranean diet combined with an adequate intake of micronutrients and physical exercise might be a cornerstone to maintain good health status, particularly in older people.
The excess of adipose tissue is the result of a multifactorial process including genetic and environmental factors with an imbalance between energy intake and expenditure, which might lead to an increased risk of developing metabolic syndrome, characterized by hyperglycemia, hypertriglyceridemia, dyslipidemia, and hypertension []. Recent studies have focused on the association between body mass index (BMI) and GM composition [,]. In particular, Gao et al. [] investigated the fecal microbiome composition, profiled via 16S rRNA gene sequencing, on 551 participants categorized as underweight, normal, overweight, and obese, based on their BMI. The authors showed that the bacterial community of the underweight group had a significantly higher alpha diversity than other groups and, if stratified by gender, the alpha diversity across the BMI was maintained in females. Moreover, an enrichment of Fusobacteria was observed in the fecal microbiota of obese males and an abundance of Actinobacteria in obese females. Finally, the butyrate-acetoacetate CoA-transferase was enriched in obese subjects, resulting in an excess of energy accumulation. These findings are in line with previous data in the literature showing a correlation between the development of obesity-associated OA and gut dysbiosis [,] in animal models, acting through an interaction with the innate immune system at both systemic and local levels []. Lipotoxicity is a typical feature of the metabolic syndrome that might promote the production of proinflammatory cytokines with the consequent recruitment of mast cells, macrophages, and dendritic cells in the adipose tissue, inducing a chronic low-grade inflammatory status [].
Thus, considering these proinflammatory effects, obesity is considered one of the main risk factors of OA [], and it seems to also negatively influence muscle mass and function in older people [,]. In animal models, a high-fat/high-sucrose diet is able to promote knee joint damage, with an increase of the intestinal permeability and a consequent increase of serum levels of LPS, supporting the hypothesis of a linkage between gut dysbiosis, metabolic inflammation, and OA [].
4. Gut Microbiota Modulation as Treatment of Osteoarthritis
The rebalancing of GM could have positive effects on the treatment of dysbiosis-related diseases; in particular, GM modulation might be obtained through specific diets, probiotics (live organisms), and prebiotics (indigestible and non-absorbable substances) supplementation [,,]. Probiotics such as Bifidobacterium and Lactobacillus exert their role by promoting gut health through the regulation of pH levels and the colonization resistance [,,]. On the other hand, prebiotics are able to stimulate the activity and growth of several bacteria in the gastrointestinal tract, promoting the fermenting process involved in the generation of SCFAs, which are considered key regulatory metabolites of gut wellness [,,].
In this context, it was hypothesized that GM modulation is able to modify the onset and the progression of OA. Previous studies have shown that the administration of probiotics significantly decreased the expression of pro-inflammatory cytokines in rat knee cartilage during monoiodoacetate-induced OA []. Korotkyi et al. described the beneficial effects of a probiotic diet on the expression of prostaglandin endoperoxide synthase-2 (PTGS2) and transforming growth factor beta-1 (TGFb1), suggesting a potential perspective to improve the standard treatment of OA []. Furthermore, prebiotic supplementation in combination with aerobic exercise could prevent knee joint damage, otherwise observed in an obesity-induced OA rat model []; in this study, the authors highlighted that the integrity of the knee joint obtained in the prebiotic diet and physical activity group was associated with the maintenance of GM homeostasis and the prevention of endotoxemia.
The main linking factor between GM and OA seems to be represented by the common chronic low-grade inflammation, supporting a new OA phenotype, indicated as the ‘metabolic OA’ []. However, it has been hypothesized that the microbial community shifts induced by antibiotics, a germ-free environment, or high-fat might have a key role in the development of OA, suggesting that active microbiome modulation could be an effective therapeutic option to counter joint degeneration in OA []. Finally, it has been suggested that dietary supplements and nutraceuticals might exert their positive effects on health status in the elderly [] through quantitative and qualitative modifications of the GM [].
Although previous studies have investigated the gut–joint axis in animal models, clinical studies in humans are lacking and future perspectives should focus on a more detailed understanding of the in vivo effects of probiotic and/or prebiotic administration in OA patients.
5. Physical Exercise and Gut Microbiota
Physical exercise plays a fundamental role in the prevention and treatment of several chronic diseases including OA []; and it is recommended by several guidelines as a first line intervention in the management of this condition [,,]. Pathogenic mechanisms of the ‘gut–joint axis’ and the potential therapeutic role of physical exercise combined with diet and probiotics are depicted by Figure 1.
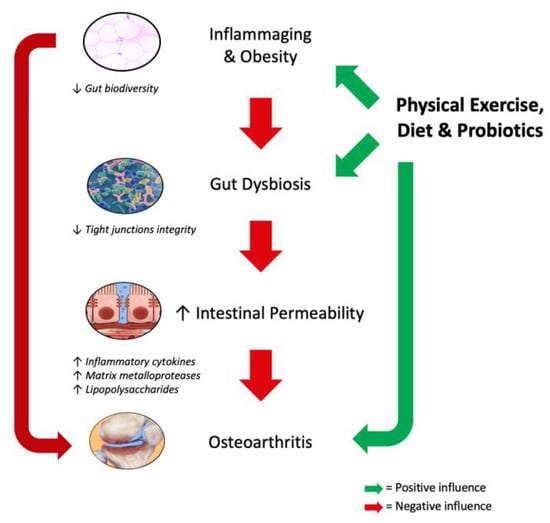
Figure 1.
Pathogenic mechanisms of the ‘gut–joint axis’ and the potential role of physical exercise combined with diet and probiotics.
Recently, several studies have shown that physical exercise could modulate GM composition [,,], boost intestinal mucosal immunity [], increase the Bacteroidetes–Firmicutes ratio [,], modify the bile acid profile [], and improve the production of short chain fatty acids such as n-butyrate, acetate, and propionate [,]. In more detail, it has to be noted that acetate and propionate are carried in the bloodstream to several organs as substrates for local energy metabolism (i.e., gluconeogenesis) [].
It has been previously shown that low intensity exercise might reduce the risk of gastrointestinal diseases (i.e., colon cancer, diverticulosis, and inflammatory bowel disease), taking into account the strict correlation between skeletal muscle and GM [,,,,,]. In more detail, physical activity might modify the transient stool time and the contact time between the pathogens and the gastrointestinal mucus layer, resulting in the gastrointestinal tract modifications above-mentioned [].
How can the GM be modified in patients undergoing intense physical activity? At present, the question remains unanswered. However, it has been demonstrated that GM can control oxidative stress and inflammatory responses, improving metabolism and energy expenditure []. It is important to underline that this is a two-way relationship, as shown by the key role of exercise in reducing inflammatory infiltrate and protecting the morphology and integrity of the intestinal tract, independently from the diet [].
Does exercise have a role in contrasting inflammaging independently of an adequate diet? Evans et al. showed that physical activity seems to prevent diet-induced obesity through a GM modulation that results in a microbial composition similar to lean mice []. Moreover, it was recently demonstrated that cardiorespiratory fitness, independent from diet, was correlated with increased GM diversity in healthy humans []. At the same time, exercise might prevent obesity, also changing the percentage of major bacterial phyla in obese-induced mice through high fat feeding, as shown by the inverse correlation between the Bacteroidetes–Firmicutes ratio and the total distance run [].
All these data were confirmed by a recent study performed by Campbell et al. that demonstrated the presence of bacteria related to Faecalibacterium prausnitzii in mice undergoing a physical exercise protocol []. These bacteria commonly protect the digestive tract through butyrate production and lowering the oxygen tension in the lumen, boosting a flavin/thiol electron shuttle. Furthermore, it has been demonstrated that fit individuals showed a gut microbial profile enriched in Clostridiales, Roseburia, Lachnospiraceae, and Erysipelotrichaceae bacteria, which are all butyrate-producers and considered as indicators of gut health [].
However, up to now, despite these evidences, the conundrum between physical exercise and probiotic interventions in the modulation of GM is far from being understood in detail. Moreover, few studies including the ones previously cited, took into account specific parameters of physical function. Román et al. [] have recently shown in a randomized trial that the administration of a probiotic blend to cirrhotic patients could enhance the physical performance, according to the timed up and go test (TUG); indeed, patients treated with probiotics showed an improvement in TUG (p = 0.015) and gait speed (p = 0.02), and a trend toward a lower incidence of falls at the follow-up (p = 0.10). Table 1 describes all the studies that have investigated the correlation between physical exercise and GM.

Table 1.
Main studies included in the present narrative review that have investigated the correlation between physical exercise and gut microbiota (GM).
6. Conclusions
This narrative review showed how several studies supported the hypothesis of a ‘gut–joint axis’ and in this context, physical exercise interventions combined with different nutritional approaches might play a key role in rebalancing microbial dysbiosis and could be considered as adjuvant treatments in dysbiosis-associated diseases.
However, these findings remain anecdotal and data on quantitative and qualitative microbiome composition in OA patients are still lacking and more research efforts are needed to understand the shared pathways and synergies between exercise, diet, and probiotics in GM modulation. Thus, to address these issues, future research should focus on several aspects: (1) a detailed assessment of the correlation between GM, prebiotics/probiotics, and nutraceuticals to create effective therapeutic interventions to counteract OA pathogenesis and progression; (2) investigate new potential biomarkers related to inflammaging and gut dysbiosis (i.e., inflammatory cytokines, matrix metalloproteases, and LPS) that are able to predict OA onset and monitor therapeutic intervention efficacy; and (3) to investigate how new cutting edge GM therapeutic interventions might impact host biology and might protect from OA onset.
Author Contributions
Conceptualization, A.d.S., R.d.S., F.S., and M.I.; Literature research, A.d.S., R.d.S., V.P., and L.M.; Writing Original Draft Preparation, A.d.S. and R.d.S.; Writing Review & Editing, F.S. and M.I.; Supervision, C.C. and A.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cross, M.; Smith, E.; Hoy, D.; Nolte, S.; Ackerman, I.; Fransen, M.; Bridgett, L.; Williams, S.; Guillemin, F.; Hill, C.L.; et al. The global burden of hip and knee osteoarthritis: Estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 2014, 73, 1323–1330. [Google Scholar] [CrossRef]
- McDonough, C.M.; Jette, A.M. The contribution of osteoarthritis to functional limitations and disability. Clin. Geriatr. Med. 2010, 26, 387–399. [Google Scholar] [CrossRef]
- McAlindon, T.E.; Cooper, C.; Kirwan, J.R.; Dieppe, P.A. Determinants of disability in osteoarthritis of the knee. Ann. Rheum. Dis. 1993, 52, 258–262. [Google Scholar] [CrossRef]
- Iolascon, G.; Gimigliano, F.; Moretti, A.; de Sire, A.; Migliore, A.; Brandi, M.L.; Piscitelli, P. Early osteoarthritis: How to define, diagnose, and manage. A systematic review. Eur. Geriatr. Med. 2017, 8, 383–396. [Google Scholar] [CrossRef]
- Malfait, A.M. Osteoarthritis year in review 2015: Biology. Osteoarthr. Cartil. 2016, 24, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xiao, W.; Luo, W.; Zeng, C.; Deng, Z.; Ren, W.; Wu, G.; Lei, G. Alterations of amino acid metabolism in osteoarthritis: Its implications for nutrition and health. Amino Acids 2016, 48, 907–914. [Google Scholar] [CrossRef] [PubMed]
- Biver, E.; Berenbaum, F.; Valdes, A.M.; de Carvalho, I.A.; Bindels, L.B.; Brandi, M.L.; Calder, P.C.; Castronovo, V.; Cavalier, E.; Cherubini, A.; et al. Gut microbiota and osteoarthritis management: An expert consensus of the European society for clinical and economic aspects of osteoporosis, osteoarthritis and musculoskeletal diseases (ESCEO). Ageing Res. Rev. 2019, 55, 100946. [Google Scholar] [CrossRef] [PubMed]
- Sommer, F.; Bäckhed, F. The gut microbiota-masters of host development and physiology. Nat. Rev. Microbiol. 2013, 11, 227–238. [Google Scholar] [CrossRef] [PubMed]
- Arumugam, M.; Raes, J.; Pelletier, E.; Le Paslier, D.; Yamada, T.; Mende, D.R.; Fernandes, G.R.; Tap, J.; Bruls, T.; Batto, J.M.; et al. Enterotypes of the human gut microbiome. Nature 2011, 473, 174–180. [Google Scholar] [CrossRef]
- Kamada, N.; Seo, S.U.; Chen, G.Y.; Nunez, G. Role of the gut microbiota in immunity and inflammatory disease. Nat. Rev. Immunol. 2011, 13, 321–335. [Google Scholar] [CrossRef]
- De Sire, R.; Talocco, C.; Petito, V.; Lopetuso, L.R.; Graziani, C.; Gasbarrini, A.; Scaldaferri, F. Microbiota and inflammatory bowel disease: An update. Recenti Prog. Med. 2018, 109, 570–573. [Google Scholar] [PubMed]
- Li, Y.; Luo, W.; Deng, Z.; Lei, G. Diet-Intestinal Microbiota Axis in Osteoarthritis: A Possible Role. Mediat. Inflamm. 2016. [Google Scholar] [CrossRef] [PubMed]
- de Sire, R.; Rizzatti, G.; Ingravalle, F.; Pizzoferrato, M.; Petito, V.; Lopetuso, L.; Graziani, C.; de Sire, A.; Mentella, M.C.; Mele, M.C.; et al. Skeletal muscle-gut axis: Emerging mechanisms of sarcopenia for intestinal and extra intestinal diseases. Minerva Gastroenterol. Dietol. 2018, 64, 1351–1362. [Google Scholar] [CrossRef]
- Berthelot, J.-M.; Sellam, J.; Maugars, Y.; Berenbaum, F. Cartilage-gut-microbiome axis: A new paradigm for novel therapeutic opportunities in osteoarthritis. RMD Open 2019, 2, e001037. [Google Scholar] [CrossRef] [PubMed]
- Szychlinska, M.A.; Di Rosa, M.; Castorina, A.; Mobasheri, A.; Musumeci, G. A correlation between intestinal microbiota dysbiosis and osteoarthritis. Heliyon 2019, 1, e01134. [Google Scholar] [CrossRef] [PubMed]
- Favazzo, L.J.; Hendesi, H.; Villani, D.A.; Soniwala, S.; Dar, Q.A.; Schott, E.M.; Gill, S.R.; Zuscik, M.J. The gut microbiome-joint connection: Implications in osteoarthritis. Curr. Opin. Rheumatol. 2020, 1, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Monda, V.; Villano, I.; Messina, A.; Valenzano, A.; Esposito, T.; Moscatelli, F.; Viggiano, A.; Cibelli, G.; Chieffi, S.; Monda, M.; et al. Exercise modifies the gut microbiota with positive health effects. Oxid. Med. Cell. Longev. 2017. [Google Scholar] [CrossRef]
- Peters, H.P.; De Vries, W.R.; Vanberge-Henegouwen, G.P.; Akkermans, L.M. Potential benefits and hazards of physical activity and exercise on the gastrointestinal tract. Gut 2001, 48, 435–439. [Google Scholar] [CrossRef]
- Pizzoferrato, M.; de Sire, R.; Ingravalle, F.; Mentella, M.C.; Petito, V.; Martone, A.M.; Landi, F.; Miggiano, G.A.; Mele, M.C.; Lopetuso, L.R.; et al. Characterization of Sarcopenia in an IBD Population Attending an Italian Gastroenterology Tertiary Center. Nutrients 2019, 24, 2281. [Google Scholar] [CrossRef]
- Ticinesi, A.; Nouvenne, A.; Cerundolo, N.; Catania, P.; Prati, B.; Tana, C.; Meschi, T. Gut Microbiota, Muscle Mass and Function in Aging: A Focus on Physical Frailty and Sarcopenia. Nutrients 2019, 17, 1633. [Google Scholar] [CrossRef] [PubMed]
- Picca, A.; Ponziani, F.R.; Calvani, R.; Marini, F.; Biancolillo, A.; Coelho-Júnior, H.J.; Gervasoni, J.; Primiano, A.; Putignani, L.; Del Chierico, F.; et al. Gut Microbial, Inflammatory and Metabolic Signatures in Older People with Physical Frailty and Sarcopenia: Results from the BIOSPHERE Study. Nutrients 2019, 26, 65. [Google Scholar] [CrossRef] [PubMed]
- Attur, M.; Krasnokutsky, S.; Statnikov, A.; Samuels, J.; Li, Z.; Friese, O.; Le Graverand-Gastineau, M.P.H.; Rybak, L.; Kraus, V.B.; Jordan, J.M.; et al. Low-grade inflammation in symptomatic knee osteoarthritis: Prognostic value of inflammatory plasma lipids and peripheral blood leukocyte biomarkers. Arthritis Rheumatol. 2015, 67, 2905–2915. [Google Scholar] [CrossRef] [PubMed]
- Scanzello, C.R.; Loeser, R.F. Inflammatory activity in symptomatic knee osteoarthritis: Not all inflammation is local. Arthritis Rheumatol. 2015, 67, 2797–2800. [Google Scholar] [CrossRef] [PubMed]
- Greene, M.A.; Loeser, R.F. Aging-related inflammation in osteoarthritis. Osteoarthr. Cartil. 2015, 23, 1966–1971. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, C.; Bonafè, M.; Valensin, S.; Olivieri, F.; De Luca, M.; Ottaviani, E.; De Benedictis, G. Inflamm-aging: An evolutionary perspective on immunosenescence. Ann. N. Y. Acad. Sci. 2000, 908, 244–254. [Google Scholar] [CrossRef]
- Davidson, E.B.; Van Caam, A.P.; Vitters, E.L.; Bennink, M.B.; Thijssen, E.; Van Den Berg, W.B.; Koenders, M.I.; Van Lent, P.L.; Van De Loo, F.A.; Van Der Kraan, P.M. TGF-â is a potent inducer of nerve growth factor in articular cartilage via the ALK5-Smad2/3 pathway. Potential role in OA related pain? Osteoarthr. Cartil. 2015, 23, 478–486. [Google Scholar] [CrossRef]
- Davidson, E.N.; Remst, D.F.; Vitters, E.L.; van Beuningen, H.M.; Blom, A.B.; Goumans, M.J.; van den Berg, W.B.; van der Kraan, P.M. Increase in ALK1/ALK5 ratio as a cause for elevated MMP-13 expression in osteoarthritis in humans and mice. J. Immunol. 2009, 182, 7937–7945. [Google Scholar] [CrossRef]
- Finnson, K.W.; Parker, W.L.; ten Dijke, P.; Thorikay, M.; Philip, A. ALK1 opposes ALK5/Smad3 signaling and expression of extracellular matrix components in human chondrocytes. J. Bone Miner. Res. 2008, 23, 896–906. [Google Scholar] [CrossRef]
- van der Kraan, P.; Matta, C.; Mobasheri, A. Age-Related Alterations in Signaling Pathways in Articular Chondrocytes: Implications for the Pathogenesis and Progression of Osteoarthritis—A Mini-Review. Gerontology 2017, 63, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Livshits, G.; Zhai, G.; Hart, D.J.; Kato, B.S.; Wang, H.; Williams, F.M.; Spector, T.D. Interleukin-6 is a significant predictor of radiographic knee osteoarthritis: The Chingford study. Arthritis Rheum. 2009, 60, 2037–2045. [Google Scholar] [CrossRef] [PubMed]
- Singh, T.; Newman, A.B. Inflammatory markers in population studies of aging. Ageing Res. Rev. 2011, 10, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Santoro, A.; Ostan, R.; Candela, M.; Biagi, E.; Brigidi, P.; Capri, M.; Franceschi, C. Gut microbiota changes in the extreme decades of human life: A focus on centenarians. Cell. Mol. Life Sci. 2018, 75, 129–148. [Google Scholar] [CrossRef]
- Biagi, E.; Nylund, L.; Candela, M.; Ostan, R.; Bucci, L.; Pini, E.; Nikkïla, J.; Monti, D.; Satokari, R.; Franceschi, C.; et al. Through ageing, and beyond: Gut microbiota and inflammatory status in seniors and centenarians. PLoS ONE 2010, 5, e10667. [Google Scholar] [CrossRef]
- Kong, F.; Hua, Y.; Zeng, B.; Ning, R.; Li, Y.; Zhao, J. Gut microbiota signatures of longevity. Curr. Biol. 2016, 26, R832–R833. [Google Scholar] [CrossRef] [PubMed]
- Graziani, C.; Talocco, C.; De Sire, R.; Petito, V.; Lopetuso, L.R.; Gervasoni, J.; Persichilli, S.; Franceschi, F.; Ojetti, V.; Gasbarrini, A.; et al. Intestinal permeability in physiological and pathological conditions: Major determinants and assessment modalities. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 795–810. [Google Scholar] [PubMed]
- Collins, K.H.; Paul, H.A.; Reimer, R.A.; Seerattan, R.A.; Hart, D.A.; Herzog, W. Relationship between inflammation, the gut microbiota, and metabolic osteoarthritis development: Studies in a rat model. Osteoarthr. Cartil. 2015, 11, 1989–1998. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.Y.; Stabler, T.; Pei, F.X.; Kraus, V.B. Both systemic and local lipopolysaccharide (LPS) burden are associated with knee OA severity and inflammation. Osteoarthr. Cartil. 2016, 10, 1769–1775. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, C.; Garagnani, P.; Parini, P.; Giuliani, C.; Santoro, A. Inflammaging: A new immune-metabolic viewpoint for age-related diseases. Nat. Rev. Endocrinol. 2018, 14, 576–590. [Google Scholar] [CrossRef] [PubMed]
- Milani, C.; Ferrario, C.; Turroni, F.; Duranti, S.; Mangifesta, M.; van Sinderen, D.; Ventura, M. The human gut microbiota and its interactive connections to diet. J. Hum. Nutr. Diet. 2016, 29, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Rinninella, E.; Raoul, P.; Cintoni, M.; Franceschi, F.; Miggiano, G.A.D.; Gasbarrini, A.; Mele, M.C. What is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms 2019, 1, 14. [Google Scholar] [CrossRef] [PubMed]
- Gentile, C.L.; Weir, T.L. The gut microbiota at the intersection of diet and human health. Science 2018, 16, 776–780. [Google Scholar] [CrossRef] [PubMed]
- Murphy, E.A.; Velazquez, K.T.; Herbert, K.M. Influence of high-fat diet on gut microbiota: A driving force for chronic disease risk. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Ticinesi, A.; Lauretani, F.; Milani, C.; Nouvenne, A.; Tana, C.; Del Rio, D.; Maggio, M.; Ventura, M.; Meschi, T. Aging Gut Microbiota at the Cross-Road between Nutrition, Physical Frailty, and Sarcopenia: Is There a Gut-Muscle Axis? Nutrients 2017, 30, 1303. [Google Scholar] [CrossRef] [PubMed]
- Lucas, S.; Omata, Y.; Hofmann, J.; Böttcher, M.; Iljazovic, A.; Sarter, K.; Albrecht, O.; Schulz, O.; Krishnacoumar, B.; Krönke, G.; et al. Short-chain fatty acids regulate systemic bone mass and protect from pathological bone loss. Nat. Commun. 2018, 4, 55. [Google Scholar] [CrossRef] [PubMed]
- Iolascon, G.; Gimigliano, R.; Bianco, M.; De Sire, A.; Moretti, A.; Giusti, A.; Malavolta, N.; Migliaccio, S.; Migliore, A.; Napoli, N.; et al. Are Dietary Supplements and Nutraceuticals Effective for Musculoskeletal Health and Cognitive Function? A Scoping Review. J. Nutr. Health Aging 2017, 21, 527–538. [Google Scholar] [CrossRef] [PubMed]
- Landi, F.; Calvani, R.; Tosato, M.; Martone, A.M.; Ortolani, E.; Savera, G.; D’Angelo, E.; Sisto, A.; Marzetti, E. Protein Intake and Muscle Health in Old Age: From Biological Plausibility to Clinical Evidence. Nutrients 2016, 14, 295. [Google Scholar] [CrossRef]
- Courtney-Martin, G.; Ball, R.O.; Pencharz, P.B.; Elango, R. Protein Requirements during Aging. Nutrients 2016, 11, 492. [Google Scholar] [CrossRef]
- Iolascon, G.; Moretti, A.; de Sire, A.; Calafiore, D.; Gimigliano, F. Effectiveness of Calcifediol in Improving Muscle Function in Post-Menopausal Women: A Prospective Cohort Study. Adv. Ther. 2017, 34, 744–752. [Google Scholar] [CrossRef]
- Tessier, A.J.; Chevalier, S. An Update on Protein, Leucine, Omega-3 Fatty Acids, and Vitamin D in the Prevention and Treatment of Sarcopenia and Functional Decline. Nutrients 2018, 16, 1099. [Google Scholar] [CrossRef]
- Iolascon, G.; Moretti, A.; de Sire, A.; Liguori, S.; Toro, G.; Gimigliano, F. Pharmacological therapy of sarcopenia: Past, present and future. Clin. Cases Miner. Bone Metab. 2018, 15, 411–419. [Google Scholar]
- de Sire, A.; Invernizzi, M.; Lippi, L.; Curci, C.; Cisari, C.; Iolascon, G. Nutritional supplementation in hip fracture sarcopenic patients: A narrative review. Clin. Cases Miner. Bone Metab. 2019, 16, 27–30. [Google Scholar]
- Invernizzi, M.; de Sire, A.; D’Andrea, F.; Carrera, D.; Renò, F.; Migliaccio, S.; Iolascon, G.; Cisari, C. Effects of essential amino acid supplementation and rehabilitation on functioning in hip fracture patients: A pilot randomized controlled trial. Aging Clin. Exp. Res. 2019, 10, 1517–1524. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A.; Baricich, A.; Renò, F.; Cisari, C.; Fusco, N.; Invernizzi, M. Myostatin as a potential biomarker to monitor sarcopenia in hip fracture patients undergoing a multidisciplinary rehabilitation and nutritional treatment: A preliminary study. Aging Clin. Exp. Res. 2019, 14, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Koyanagi, A.; Stubbs, B.; Cooper, C.; Guglielmi, G.; Rizzoli, R.; Punzi, L.; Rogoli, D.; Caruso, M.G.; Rotolo, O.; et al. Mediterranean diet and knee osteoarthritis outcomes: A longitudinal cohort study. Clin. Nutr. 2019, 13, 2735–2739. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.; Zimmet, P.; Shaw, J. The metabolic syndrome—A new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- Gao, X.; Zhang, M.; Xue, J.; Huang, J.; Zhuang, R.; Zhou, X.; Zhang, H.; Fu, Q.; Hao, Y. Body Mass Index Differences in the Gut Microbiota Are Gender Specific. Front. Microbiol. 2018, 9, 1250. [Google Scholar] [CrossRef] [PubMed]
- Bai, J.; Hu, Y.; Bruner, D.W. Composition of gut microbiota and its association with body mass index and lifestyle factors in a cohort of 7-18 years old children from the American Gut Project. Pediatr. Obes. 2019, 4, e12480. [Google Scholar] [CrossRef]
- Guss, J.D.; Ziemian, S.N.; Luna, M.; Sandoval, T.N.; Holyoak, D.T.; Guisado, G.G.; Roubert, S.; Callahan, R.L.; Brito, I.L.; van der Meulen, M.C.; et al. The effects of metabolic syndrome, obesity, and the gut microbiome on load-induced osteoarthritis. Osteoarthr. Cartil. 2019, 1, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Ding, W.; Wang, H.L.; Dai, L.L.; Zong, W.H.; Wang, Y.Z.; Bi, J.; Han, W.; Dong, G.J. Gut microbiota and obesity-associated osteoarthritis. Osteoarthr. Cartil. 2019, 9, 1257–1265. [Google Scholar] [CrossRef] [PubMed]
- Boulangé, C.L.; Neves, A.L.; Chilloux, J.; Nicholson, J.K.; Dumas, M.E. Impact of the gut microbiota on inflammation, obesity, and metabolic disease. Genome Med. 2016, 20, 42. [Google Scholar] [CrossRef]
- Visser, M.; Pahor, M.; Taaffe, D.R.; Goodpaster, B.H.; Simonsick, E.M.; Newman, A.B.; Nevitt, M.; Harris, T.B. Relationship of interleukin-6 and tumor necrosis factor-alpha with muscle mass and muscle strength in elderly men and women: The Health ABC Study. J. Gerontol. A Biol. Sci. Med. Sci. 2002, 5, M326–M332. [Google Scholar] [CrossRef] [PubMed]
- Gimigliano, F.; Moretti, A.; de Sire, A.; Calafiore, D.; Iolascon, G. The combination of vitamin D deficiency and overweight affects muscle mass and function in older post-menopausal women. Aging Clin. Exp. Res. 2018, 6, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Hill, C.; Guarner, F.; Reid, G. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 506–514. [Google Scholar] [CrossRef] [PubMed]
- Markowiak, P.; Śliżewska, K. Effects of Probiotics, Prebiotics, and Synbiotics on Human Health. Nutrients 2017, 9, 1021. [Google Scholar] [CrossRef] [PubMed]
- Satokari, R. Modulation of Gut Microbiota for Health by Current and Next-Generation Probiotics. Nutrients 2019, 8, 1921. [Google Scholar] [CrossRef] [PubMed]
- Korotkyi, O.H.; Vovk, A.A.; Dranitsina, A.S.; Falalyeyeva, T.M.; Dvorshchenko, K.O.; Fagoonee, S.; Ostapchenko, L.I. The influence of probiotic diet and chondroitin sulfate administration on Ptgs2, Tgfb1 and Col2a1 expression in rat knee cartilage during monoiodoacetate-induced osteoarthritis. Minerva Med. 2019, 110, 419–424. [Google Scholar] [CrossRef] [PubMed]
- Rios, J.L. Protective effect of prebiotic and exercise intervention on knee health in a rat model of diet-induced obesity. Cartilage 2019, 9, 3893. [Google Scholar] [CrossRef] [PubMed]
- Mazor, M.; Best, T.M.; Cesaro, A.; Lespessailles, E.; Toumi, H. Osteoarthritis biomarker responses and cartilage adaptation to exercise: A review of animal and human models. Scand. J. Med. Sci. Sports 2019, 29, 1072–1082. [Google Scholar] [CrossRef]
- Richmond, J.; Hunter, D.; Irrgang, J.; Jones, M.H.; Levy, B.; Marx, R.; Snyder-Mackler, L.; Watters, W.C.; Haralson, R.H.; Turkelson, C.M.; et al. American Academy of Orthopaedic Surgeons. Treatment of osteoarthritis of the knee (nonarthroplasty). J. Am. Acad. Orthop. Surg. 2009, 17, 591–600. [Google Scholar] [CrossRef]
- Hochberg, M.C.; Altman, R.D.; April, K.T.; Benkhalti, M.; Guyatt, G.; McGowan, J.; Towheed, T.; Welch, V.; Wells, G.; Tugwell, P. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012, 64, 465–474. [Google Scholar] [CrossRef] [PubMed]
- McAlindon, T.E.; Bannuru, R.; Sullivan, M.C.; Arden, N.K.; Berenbaum, F.; Bierma-Zeinstra, S.M.; Hawker, G.A.; Henrotin, Y.; Hunter, D.J.; Kawaguchi, H.; et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr. Cartil. 2014, 22, 363–388. [Google Scholar] [CrossRef] [PubMed]
- Cerda, B.; Perez, M.; Perez-Santiago, J.D.; Tornero-Aguilera, J.F.; Gonzalez-Soltero, R.; Larrosa, M. Gut Microbiota Modification: Another Piece in the Puzzle of the Benefits of Physical Exercise in Health? Front. Physiol. 2016, 7, 51. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.C.; LePard, K.J.; Kwak, J.W.; Stancukas, M.C.; Laskowski, S.; Dougherty, J.; Moulton, L.; Glawe, A.; Wang, Y.; Leone, V.; et al. Exercise prevents weight gain and alters the gut microbiota in a mouse model of high fat diet-induced obesity. PLoS ONE 2014, 26, e92193. [Google Scholar] [CrossRef] [PubMed]
- Morita, E.; Yokoyama, H.; Imai, D.; Takeda, R.; Ota, A.; Kawai, E.; Hisada, T.; Emoto, M.; Suzuki, Y.; Okazaki, K. Aerobic Exercise Training with Brisk Walking Increases Intestinal Bacteroides in Healthy Elderly Women. Nutrients 2019, 4, 868. [Google Scholar] [CrossRef] [PubMed]
- Mach, N.; Fuster-Botella, D. Endurance exercise and gut microbiota: A review. J. Sport Health Sci. 2017, 6, 179–197. [Google Scholar] [CrossRef] [PubMed]
- Hsu, Y.J.; Chiu, C.C.; Li, Y.P.; Huang, W.C.; Huan, Y.T.; Huang, C.C.; Chuang, H.L. Effect of intestinal microbiota on exercise performance in mice. J. Strength Cond. Res. 2015, 29, 552–558. [Google Scholar] [CrossRef] [PubMed]
- Hsu, Y.J.; Chiu, C.C.; Li, Y.P.; Huang, W.C.; Te Huang, Y.; Huang, C.C.; Chuang, H.L. Effects of the gut microbiota on host adiposity are modulated by the short-chain fatty-acid binding G protein-coupled receptor, Gpr41. Proc. Natl. Acad. Sci. USA 2008, 28, 16767–16772. [Google Scholar]
- Bermon, S.; Petriz, B.; Kajėnienė, A.; Prestes, J.; Castell, L.; Franco, O.L. The microbiota: An exercise immunology perspective. Exerc. Immunol. Rev. 2015, 21, 70–79. [Google Scholar] [PubMed]
- Campbell, S.C.; Wisniewski, P.J.; Noji, M.; McGuinness, L.R.; Häggblom, M.M.; Lightfoot, S.A.; Joseph, L.B.; Kerkhof, L.J. The Effect of Diet and Exercise on Intestinal Integrity and Microbial Diversity in Mice. PLoS ONE 2016, 8, e0150502. [Google Scholar] [CrossRef] [PubMed]
- Estaki, M.; Pither, J.; Baumeister, P.; Little, J.P.; Gill, S.K.; Ghosh, S.; Ahmadi-Vand, Z.; Marsden, K.R.; Gibson, D.L. Cardiorespiratory fitness as a predictor of intestinal microbial diversity and distinct metagenomic functions. Microbiome 2016, 8, 42. [Google Scholar] [CrossRef]
- Román, E.; Nieto, J.C.; Gely, C.; Vidal, S.; Pozuelo, M.; Poca, M.; Juárez, C.; Guarner, C.; Manichanh, C.; Soriano, G. Effect of a multistrain probiotic on cognitive function and risk of falls in patients with cirrhosis: A randomized trial. Hepatol. Commun. 2019, 3, 632–645. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).