Osteosarcopenic Obesity: Current Knowledge, Revised Identification Criteria and Treatment Principles
Abstract
:1. Introduction
2. Literature Search Methods
- osteosarcopenic obesity
- definitions and cutoffs for sarcopenia, obesity and visceral fat
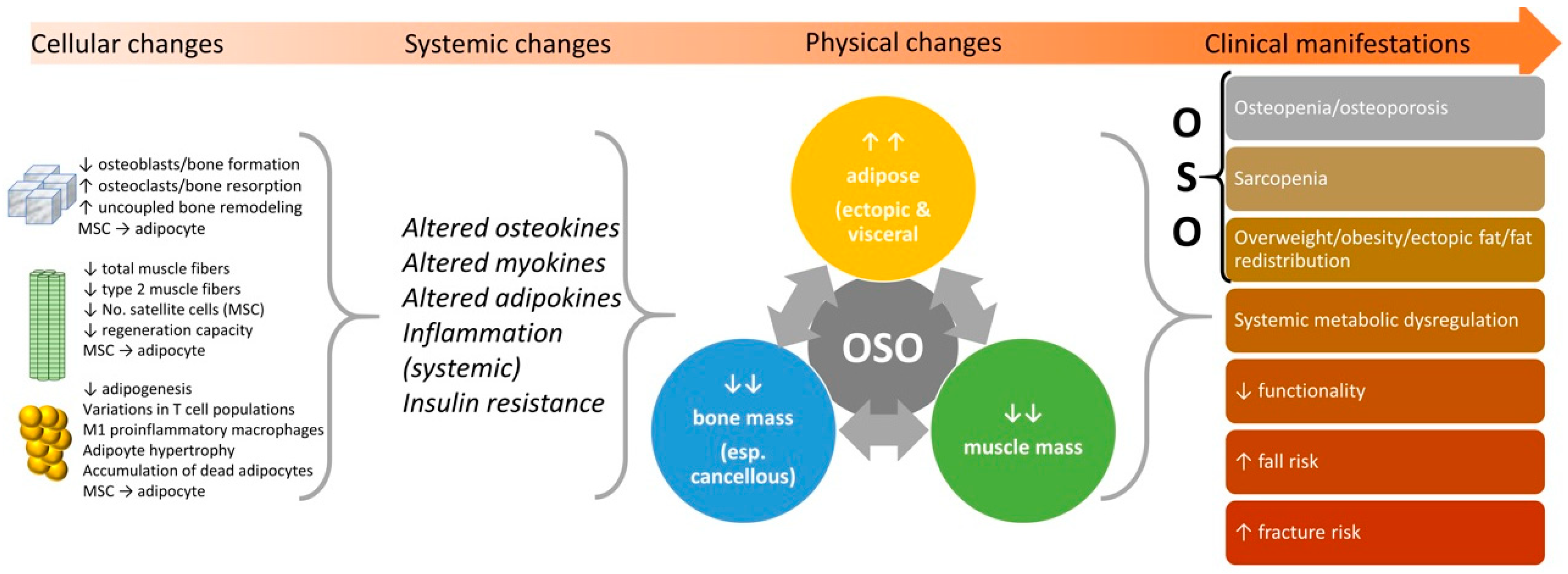
3. State of the Current Knowledge
4. Persisting Difficulties in the Identification of OSO and Its Components
4.1. Bone and Muscle Tissues
4.2. Obesity Classification and Adipose Tissue
5. Updated OSO and Ectopic Fat Identification
6. Future Refinements for OSO Diagnosis and Treatment
6.1. Bone
6.2. Muscle
6.3. Serum Markers of OSO
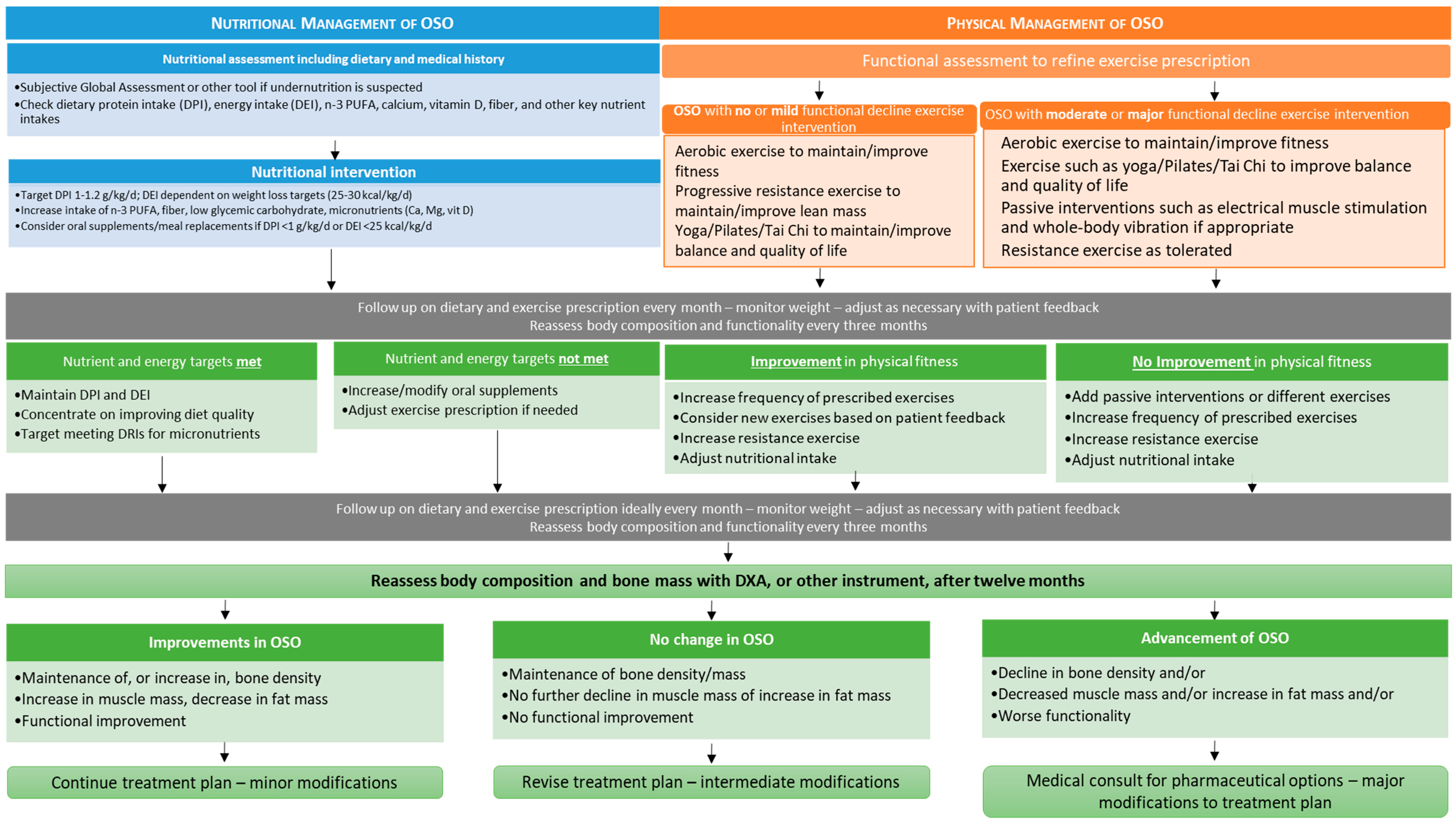
7. Nutritional and Physical Activity Considerations for OSO
7.1. Nutrition
7.2. Physical Activity
8. Summary
Author Contributions
Funding
Conflicts of Interest
References
- Ilich, J.Z.; Kelly, O.J.; Inglis, J.E.; Panton, L.B.; Duque, G.; Ormsbee, M.J. Interrelationship among muscle, fat, and bone: Connecting the dots on cellular, hormonal, and whole body levels. Ageing Res. Rev. 2014, 15, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Ilich, J.Z.; Kelly, O.J.; Inglis, J.E. Osteosarcopenic obesity syndrome: What is it and how can it be identified and diagnosed? Curr. Gerontol. Geriatr. Res. 2016, 2016, 7325973. [Google Scholar] [CrossRef] [PubMed]
- JafariNasabian, P.; Inglis, J.E.; Kelly, O.J.; Ilich, J.Z. Osteosarcopenic obesity in women: Impact, prevalence, and management challenges. Int. J. Women Health 2017, 9, 33–42. [Google Scholar] [CrossRef]
- Reginster, J.Y.; Beaudart, C.; Buckinx, F.; Bruyere, O. Osteoporosis and sarcopenia: Two diseases or one? Curr. Opin. Clin. Nutr. Metab. Care 2016, 19, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Kaji, H. Linkage between muscle and bone: Common catabolic signals resulting in osteoporosis and sarcopenia. Curr. Opin. Clin. Nutr. Metab. Care 2013, 16, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Stenholm, S.; Harris, T.B.; Rantanen, T.; Visser, M.; Kritchevsky, S.B.; Ferrucci, L. Sarcopenic obesity: Definition, cause and consequences. Curr. Opin. Clin. Nutr. Metab. Care 2008, 11, 693–700. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.M. Sarcopenia and sarcopenic obesity. Korean J. Intern. Med. 2016, 31, 1054–1060. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zamboni, M.; Mazzali, G.; Fantin, F.; Rossi, A.; Di Francesco, V. Sarcopenic obesity: A new category of obesity in the elderly. Nutr. Metab. Cardiovasc. Dis. 2008, 18, 388–395. [Google Scholar] [CrossRef]
- Vaidya, R. Obesity, sarcopenia and postmenopausal osteoporosis: An interlinked triad. J. Midlife Health 2014, 5, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Migliaccio, S.; Greco, E.A.; Aversa, A.; Lenzi, A. Age-associated (cardio) metabolic diseases and cross-talk between adipose tissue and skeleton: Endocrine aspects. Horm. Mol. Biol. Clin. Investig. 2014, 20, 25–38. [Google Scholar] [CrossRef] [PubMed]
- Ilich, J.Z.; Inglis, J.E.; Kelly, O.J.; McGee, D.L. Osteosarcopenic obesity is associated with reduced handgrip strength, walking abilities, and balance in postmenopausal women. Osteoporos. Int. 2015, 26, 2587–2595. [Google Scholar] [CrossRef]
- Szlejf, C.; Parra-Rodriguez, L.; Rosas-Carrasco, O. Osteosarcopenic obesity: Prevalence and relation with frailty and physical performance in middle-aged and older women. J. Am. Med. Dir. Assoc. 2017, 18, 733. [Google Scholar] [CrossRef]
- Angel, A. Pathophysiologic changes in obesity. Can. Med. Assoc. J. 1978, 119, 1401–1406. [Google Scholar] [PubMed]
- Deschenes, M.R. Effects of aging on muscle fibre type and size. Sports Med. 2004, 34, 809–824. [Google Scholar] [CrossRef]
- Martyniak, K.; Masternak, M.M. Changes in adipose tissue cellular composition during obesity and aging as a cause of metabolic dysregulation. Exp. Gerontol. 2017, 94, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Miljkovic, N.; Lim, J.Y.; Miljkovic, I.; Frontera, W.R. Aging of skeletal muscle fibers. Ann. Rehabil. Med. 2015, 39, 155–162. [Google Scholar] [CrossRef]
- Sikaris, K.A. The clinical biochemistry of obesity. Clin. Biochem. Rev. 2004, 25, 165–181. [Google Scholar] [PubMed]
- Ormsbee, M.J.; Prado, C.M.; Ilich, J.Z.; Purcell, S.; Siervo, M.; Folsom, A.; Panton, L. Osteosarcopenic obesity: The role of bone, muscle, and fat on health. J. Cachexia Sarcopenia Muscle 2014, 5, 183–192. [Google Scholar] [CrossRef]
- Hita-Contreras, F.; Martinez-Amat, A.; Cruz-Diaz, D.; Perez-Lopez, F.R. Osteosarcopenic obesity and fall prevention strategies. Maturitas 2015, 80, 126–132. [Google Scholar] [CrossRef]
- Kim, J.; Lee, Y.; Kye, S.; Chung, Y.S.; Kim, J.H.; Chon, D.; Lee, K.E. Diet quality and osteosarcopenic obesity in community-dwelling adults 50 years and older. Maturitas 2017, 104, 73–79. [Google Scholar] [CrossRef]
- Kim, J.; Lee, Y.; Kye, S.; Chung, Y.S.; Lee, O. Association of serum vitamin D with osteosarcopenic obesity: Korea national health and nutrition examination survey 2008–2010. J. Cachexia Sarcopenia Muscle 2017, 8, 259–266. [Google Scholar] [CrossRef]
- Mo, D.; Hsieh, P.; Yu, H.; Zhou, L.; Gong, J.; Xu, L.; Liu, P.; Chen, G.; Chen, Z.; Deng, Q. Osteosarcopenic obesity and its relationship with dyslipidemia in women from different ethnic groups of china. Arch. Osteoporos. 2018, 13, 65. [Google Scholar] [CrossRef] [PubMed]
- Perna, S.; Spadaccini, D.; Nichetti, M.; Avanzato, I.; Faliva, M.A.; Rondanelli, M. Osteosarcopenic visceral obesity and osteosarcopenic subcutaneous obesity, two new phenotypes of sarcopenia: Prevalence, metabolic profile, and risk factors. J. Aging Res. 2018, 2018, 6147426. [Google Scholar] [CrossRef] [PubMed]
- Buehring, B.; Hansen, K.E.; Lewis, B.L.; Cummings, S.R.; Lane, N.E.; Binkley, N.; Ensrud, K.E.; Cawthon, P.M.; Osteoporotic Fractures in Men Study Research Group. Dysmobility syndrome independently increases fracture risk in the osteoporotic fractures in men (MrOS) prospective cohort study. J. Bone Miner. Res. 2018, 33, 1622–1629. [Google Scholar] [CrossRef] [PubMed]
- Takayama, M.; Azuma, K.; Shimizu-Hirota, R.; Makino, K.; Seino, T.; Yoshida, T.; Kashiwagi, K.; Hirose, H.; Inoue, N.; Iwao, Y. Sarcopenic obesity is associated with osteopenia among japanese elderly women: A cross-sectional study from comprehensive health checkups. Health Eval. Promot. 2018, 45, 573–578. [Google Scholar] [CrossRef]
- Park, S.; Na, W.; Sohn, C. Relationship between osteosarcopenic obesity and dietary inflammatory index in postmenopausal Korean women: 2009 to 2011 Korea national health and nutrition examination surveys. J. Clin. Biochem. Nutr. 2018, 63, 211–216. [Google Scholar] [CrossRef]
- Stefanaki, C.; Pervanidou, P.; Boschiero, D.; Chrousos, G.P. Chronic stress and body composition disorders: Implications for health and disease. Hormones (Athens) 2018, 17, 33–43. [Google Scholar] [CrossRef]
- Stefanaki, C.; Peppa, M.; Boschiero, D.; Chrousos, G.P. Healthy overweight/obese youth: Early osteosarcopenic obesity features. Eur. J. Clin. Investig. 2016, 46, 767–778. [Google Scholar] [CrossRef]
- Hong, W.; Cheng, Q.; Zhu, X.; Zhu, H.; Li, H.; Zhang, X.; Zheng, S.; Du, Y.; Tang, W.; Xue, S.; et al. Prevalence of sarcopenia and its relationship with sites of fragility fractures in elderly Chinese men and women. PLoS ONE 2015, 10, e0138102. [Google Scholar] [CrossRef]
- Chung, J.H.; Hwang, H.J.; Shin, H.Y.; Han, C.H. Association between sarcopenic obesity and bone mineral density in middle-aged and elderly Korean. Ann. Nutr. Metab. 2016, 68, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Scott, D.; Chandrasekara, S.D.; Laslett, L.L.; Cicuttini, F.; Ebeling, P.R.; Jones, G. Associations of sarcopenic obesity and dynapenic obesity with bone mineral density and incident fractures over 5–10 years in community-dwelling older adults. Calcif. Tissue Int. 2016, 99, 30–42. [Google Scholar] [CrossRef]
- Hong, N.; Kim, C.O.; Youm, Y.; Kim, H.C.; Rhee, Y. Low peak jump power is associated with elevated odds of dysmobility syndrome in community-dwelling elderly individuals: The Korean urban rural elderly (KURE) study. Osteoporos. Int. 2018, 29, 1427–1436. [Google Scholar] [CrossRef]
- Looker, A.C. Dysmobility syndrome and mortality risk in US men and women age 50 years and older. Osteoporos. Int. 2015, 26, 93–102. [Google Scholar] [CrossRef]
- Zhu, K.; Hunter, M.; James, A.; Lim, E.M.; Cooke, B.R.; Walsh, J.P. Discordance between fat mass index and body mass index is associated with reduced bone mineral density in women but not in men: The busselton healthy ageing study. Osteoporos. Int. 2017, 28, 259–268. [Google Scholar] [CrossRef] [PubMed]
- Jeng, C.; Zhao, L.-J.; Wu, K.; Zhou, Y.; Chen, T.; Deng, H.-W. Race and socioeconomic effect on sarcopenia and sarcopenic obesity in the Louisiana osteoporosis study (LOS). JCSM Clin. Rep. 2018, 3, 2. [Google Scholar] [CrossRef]
- Weaver, C.M. Diet, gut microbiome, and bone health. Curr. Osteoporos. Rep. 2015, 13, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.C.; Greenbaum, J.; Shen, H.; Deng, H.W. Association between gut microbiota and bone health: Potential mechanisms and prospective. J. Clin. Endocrinol. Metab. 2017, 102, 3635–3646. [Google Scholar] [CrossRef] [PubMed]
- Ticinesi, A.; Lauretani, F.; Milani, C.; Nouvenne, A.; Tana, C.; Del Rio, D.; Maggio, M.; Ventura, M.; Meschi, T. Aging gut microbiota at the cross-road between nutrition, physical frailty, and sarcopenia: Is there a gut-muscle axis? Nutrients 2017, 9, 1303. [Google Scholar] [CrossRef] [PubMed]
- Baothman, O.A.; Zamzami, M.A.; Taher, I.; Abubaker, J.; Abu-Farha, M. The role of gut microbiota in the development of obesity and diabetes. Lipids Health Dis. 2016, 15, 108. [Google Scholar] [CrossRef] [PubMed]
- Inglis, J.E.; Ilich, J.Z. The microbiome and osteosarcopenic obesity in older individuals in long-term care facilities. Curr. Osteoporos. Rep. 2015, 13, 358–362. [Google Scholar] [CrossRef] [PubMed]
- Carsote, M.; Albu, S.E.; Gherigian, A.; Valea, A. Particular types of non-age related sarcopenia: Osteosarcopenic obesity and malignancy—Associated muscle waste (a mini-review). Arch. Balk. Med. Union 2016, 51, 369–372. [Google Scholar]
- Hawkins, K.L.; Zhang, L.; Ng, D.K.; Althoff, K.N.; Palella, F.J., Jr.; Kingsley, L.A.; Jacobson, L.P.; Margolick, J.B.; Lake, J.E.; Brown, T.T.; et al. Abdominal obesity, sarcopenia, and osteoporosis are associated with frailty in men living with and without HIV. AIDS 2018, 32, 1257–1266. [Google Scholar] [CrossRef]
- Yatsyshyn, R.; Stoika, I. AB0358 phenotypes of secondary sarcopenia in patients with rheumatoid arthritis. Ann. Rheum. Dis. 2018, 77, 1351. [Google Scholar]
- Fui, M.N.T.; Grossmann, M. Hypogonadism from androgen deprivation therapy in identical twins. Lancet 2016, 388, 2653. [Google Scholar] [CrossRef]
- Cosman, F.; de Beur, S.J.; LeBoff, M.S.; Lewiecki, E.M.; Tanner, B.; Randall, S.; Lindsay, R. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos. Int. 2014, 25, 2359–2381. [Google Scholar] [CrossRef]
- Siris, E.S.; Adler, R.; Bilezikian, J.; Bolognese, M.; Dawson-Hughes, B.; Favus, M.J.; Harris, S.T.; Jan de Beur, S.M.; Khosla, S.; Lane, N.E.; et al. The clinical diagnosis of osteoporosis: A position statement from the national bone health alliance working group. Osteoporos. Int. 2014, 25, 1439–1443. [Google Scholar] [CrossRef]
- Centre for Metabolic Bone Diseases University of Sheffield UK. FRAX® fracture risk assessment tool. Available online: https://www.sheffield.ac.uk/FRAX/index.aspx (accessed on 14 February 2019).
- Peppa, M.; Stefanaki, C.; Papaefstathiou, A.; Boschiero, D.; Dimitriadis, G.; Chrousos, G.P. Bioimpedance analysis vs. Dexa as a screening tool for osteosarcopenia in lean, overweight and obese caucasian postmenopausal females. Hormones (Athens) 2017, 16, 181–193. [Google Scholar] [PubMed]
- Chen, H.; Zhou, X.; Fujita, H.; Onozuka, M.; Kubo, K.Y. Age-related changes in trabecular and cortical bone microstructure. Int. J. Endocrinol. 2013, 2013, 213234. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, R.N.; Koehler, K.M.; Gallagher, D.; Romero, L.; Heymsfield, S.B.; Ross, R.R.; Garry, P.J.; Lindeman, R.D. Epidemiology of sarcopenia among the elderly in new mexico. Am. J. Epidemiol. 1998, 147, 755–763. [Google Scholar] [CrossRef]
- Shepherd, J.A.; Ng, B.K.; Sommer, M.J.; Heymsfield, S.B. Body composition by DXA. Bone 2017, 104, 101–105. [Google Scholar] [CrossRef]
- Baumgartner, R.N. Body composition in healthy aging. Ann. N. Y. Acad. Sci. 2000, 904, 437–448. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Heber, D. Sarcopenic obesity in the elderly and strategies for weight management. Nutr. Rev. 2012, 70, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Schutz, Y.; Kyle, U.U.; Pichard, C. Fat-free mass index and fat mass index percentiles in Caucasians aged 18–98 y. Int. J. Obes. Relat. Metab. Disord. 2002, 26, 953–960. [Google Scholar] [CrossRef] [Green Version]
- Stoklossa, C.A.J.; Sharma, A.M.; Forhan, M.; Siervo, M.; Padwal, R.S.; Prado, C.M. Prevalence of sarcopenic obesity in adults with class II/III obesity using different diagnostic criteria. J. Nutr. Metab. 2017, 2017, 7307618. [Google Scholar]
- Domiciano, D.S.; Figueiredo, C.P.; Lopes, J.B.; Caparbo, V.F.; Takayama, L.; Menezes, P.R.; Bonfa, E.; Pereira, R.M. Discriminating sarcopenia in community-dwelling older women with high frequency of overweight/obesity: The Sao Paulo ageing & health study (SPAH). Osteoporos. Int. 2013, 24, 595–603. [Google Scholar] [PubMed]
- Newman, A.B.; Kupelian, V.; Visser, M.; Simonsick, E.; Goodpaster, B.; Nevitt, M.; Kritchevsky, S.B.; Tylavsky, F.A.; Rubin, S.M.; Harris, T.B.; et al. Sarcopenia: Alternative definitions and associations with lower extremity function. J. Am. Geriatr. Soc. 2003, 51, 1602–1609. [Google Scholar] [CrossRef]
- Studenski, S.A.; Peters, K.W.; Alley, D.E.; Cawthon, P.M.; McLean, R.R.; Harris, T.B.; Ferrucci, L.; Guralnik, J.M.; Fragala, M.S.; Kenny, A.M.; et al. The FNIH sarcopenia project: Rationale, study description, conference recommendations, and final estimates. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2014, 69, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Ilich, J.Z. Another impairment in older age: What does osteosarcopenic obesity syndrome mean for middle-aged and older women? J. Am. Med. Dir. Assoc. 2017, 18, 648–650. [Google Scholar] [CrossRef] [PubMed]
- JafariNasabian, P.; Inglis, J.E.; Reilly, W.; Kelly, O.J.; Ilich, J.Z. Aging human body: Changes in bone, muscle and body fat with consequent changes in nutrient intake. J. Endocrinol. 2017, 234, R37–R51. [Google Scholar] [CrossRef] [PubMed]
- Coutinho, T.; Goel, K.; Correa de Sa, D.; Kragelund, C.; Kanaya, A.M.; Zeller, M.; Park, J.S.; Kober, L.; Torp-Pedersen, C.; Cottin, Y.; et al. Central obesity and survival in subjects with coronary artery disease: A systematic review of the literature and collaborative analysis with individual subject data. J. Am. Coll. Cardiol. 2011, 57, 1877–1886. [Google Scholar] [CrossRef] [PubMed]
- Shahar, E. The association of body mass index with health outcomes: Causal, inconsistent, or confounded? Am. J. Epidemiol. 2009, 170, 957–958. [Google Scholar] [CrossRef] [PubMed]
- Blackburn, H.; Jacobs, D., Jr. Commentary: Origins and evolution of body mass index (BMI): Continuing saga. Int. J. Epidemiol. 2014, 43, 665–669. [Google Scholar] [CrossRef] [PubMed]
- Santos, V.R.d.; Christofaro, D.G.D.; Gomes, I.C.; Agostinete, R.R.; Freitas Júnior, I.F.; Gobbo, L.A. Factors associated with sarcopenia in subjects aged 80 years and over. Rev. Nutr. 2015, 28, 319–326. [Google Scholar] [CrossRef] [Green Version]
- Coin, A.; Sergi, G.; Beninca, P.; Lupoli, L.; Cinti, G.; Ferrara, L.; Benedetti, G.; Tomasi, G.; Pisent, C.; Enzi, G. Bone mineral density and body composition in underweight and normal elderly subjects. Osteoporos. Int. 2000, 11, 1043–1050. [Google Scholar] [CrossRef] [PubMed]
- Hedges, W.P.; Bukhari, M. Increasing body fat mass reverses bone loss in osteopenia as detected by dual-energy x-ray absorptiometry scans. Eur. J. Rheumatol. 2016, 3, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Tatsumi, Y.; Higashiyama, A.; Kubota, Y.; Sugiyama, D.; Nishida, Y.; Hirata, T.; Kadota, A.; Nishimura, K.; Imano, H.; Miyamatsu, N.; et al. Underweight young women without later weight gain are at high risk for osteopenia after midlife: The kobe study. J. Epidemiol. 2016, 26, 572–578. [Google Scholar] [CrossRef] [PubMed]
- Rietman, M.L.; van der, A.D.; van Oostrom, S.H.; Picavet, H.S.J.; Dolle, M.E.T.; van Steeg, H.; Verschuren, W.M.M.; Spijkerman, A.M.W. The association between BMI and different frailty domains: A u-shaped curve. J. Nutr. Health Aging 2018, 22, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Boutin, E.; Natella, P.A.; Schott, A.M.; Bastuji-Garin, S.; David, J.P.; Paillaud, E.; Rolland, Y.; Canoui-Poitrine, F. Interrelations between body mass index, frailty, and clinical adverse events in older community-dwelling women: The epidos cohort study. Clin. Nutr. 2018, 37, 1638–1644. [Google Scholar] [CrossRef] [PubMed]
- Oliveros, E.; Somers, V.K.; Sochor, O.; Goel, K.; Lopez-Jimenez, F. The concept of normal weight obesity. Prog. Cardiovasc. Dis. 2014, 56, 426–433. [Google Scholar] [CrossRef]
- Kelly, T.L.; Wilson, K.E.; Heymsfield, S.B. Dual energy x-ray absorptiometry body composition reference values from nhanes. PLoS ONE 2009, 4, e7038. [Google Scholar] [CrossRef] [PubMed]
- Kyle, U.G.; Schutz, Y.; Dupertuis, Y.M.; Pichard, C. Body composition interpretation: Contributions of the fat-free mass index and the body fat mass index. Nutrition 2003, 19, 597–604. [Google Scholar] [CrossRef]
- Dufour, A.B.; Hannan, M.T.; Murabito, J.M.; Kiel, D.P.; McLean, R.R. Sarcopenia definitions considering body size and fat mass are associated with mobility limitations: The framingham study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2013, 68, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Ho-Pham, L.T.; Campbell, L.V.; Nguyen, T.V. More on body fat cutoff points. Mayo Clin. Proc. 2011, 86, 584. [Google Scholar] [CrossRef]
- American Council on Exercise. Percent body fat norms for men and women. Available online: https://www.acefitness.org/education-and-resources/lifestyle/tools-calculators/percent-body-fat-calculator (accessed on 9 February 2019).
- American College of Sports Medicine. ACSM’s Health-Related Physical Fitness Assessment Manual, 5th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2017; p. 208. [Google Scholar]
- Imboden, M.T.; Welch, W.A.; Swartz, A.M.; Montoye, A.H.; Finch, H.W.; Harber, M.P.; Kaminsky, L.A. Reference standards for body fat measures using GE dual energy x-ray absorptiometry in Caucasian adults. PLoS ONE 2017, 12, e0175110. [Google Scholar] [CrossRef] [PubMed]
- Hunter, G.R.; Gower, B.A.; Kane, B.L. Age related shift in visceral fat. Int. J. Body Compos. Res. 2010, 8, 103–108. [Google Scholar]
- Ilich, J.Z.; Kelly, O.J. Letter to the editor: Re: Comments referring to the article “comprehensive nutritional status in sarco-osteoporotic older fallers”. J. Nutr. Health Aging 2016, 20, 231–232. [Google Scholar] [CrossRef] [PubMed]
- Rosen, C.J.; Bouxsein, M.L. Mechanisms of disease: Is osteoporosis the obesity of bone? Nat. Clin. Pract. Rheumatol. 2006, 2, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Ilich, J.Z.; Kelly, O.J.; Kim, Y.; Spicer, M.T. Low-grade chronic inflammation perpetuated by modern diet as a promoter of obesity and osteoporosis. Arh. Hig. Rada. Toksikol. 2014, 65, 139–148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, U. Abdominal obesity: A marker of ectopic fat accumulation. J. Clin. Investig. 2015, 125, 1790–1792. [Google Scholar] [CrossRef] [PubMed]
- Janssen, I.; Heymsfield, S.B.; Allison, D.B.; Kotler, D.P.; Ross, R. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous, and visceral fat. Am. J. Clin. Nutr. 2002, 75, 683–688. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C., Jr.; et al. Diagnosis and management of the metabolic syndrome: An American heart association/national heart, lung, and blood institute scientific statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.M.M.; Zimmet, P.Z. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus. Provisional report of a who consultation. Diabetic Medicine 1998, 15, 539–553. [Google Scholar] [CrossRef]
- Camhi, S.M.; Bray, G.A.; Bouchard, C.; Greenway, F.L.; Johnson, W.D.; Newton, R.L.; Ravussin, E.; Ryan, D.H.; Smith, S.R.; Katzmarzyk, P.T. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: Sex and race differences. Obesity 2011, 19, 402–408. [Google Scholar] [CrossRef] [PubMed]
- De Blasio, F.; Rutten, E.P.; Wouters, E.F.; Scalfi, L.; De Blasio, F.; Akkermans, M.A.; Spruit, M.A.; Franssen, F.M. Preliminary study on the assessment of visceral adipose tissue using dual-energy x-ray absorptiometry in chronic obstructive pulmonary disease. Multidiscip. Respir. Med. 2016, 11, 33. [Google Scholar] [CrossRef]
- Okosun, I.S.; Seale, J.P.; Lyn, R. Commingling effect of gynoid and android fat patterns on cardiometabolic dysregulation in normal weight American adults. Nutr. Diabetes 2015, 5, e155. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.; Zhu, F.; Zhao, X.; Ma, X.; Zhu, S. Central fat accumulation associated with metabolic risks beyond total fat in normal BMI Chinese adults. Ann. Nutr. Metab. 2014, 64, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Miazgowski, T.; Dziwura-Ogonowska, J.; Safranow, K.; Iskierska, K.; Widecka, K. Changes in adiponectin level and fat distribution in patients with type 2 diabetes. Eur. J. Clin. Investig. 2014, 44, 192–199. [Google Scholar] [CrossRef]
- Samsell, L.; Regier, M.; Walton, C.; Cottrell, L. Importance of android/gynoid fat ratio in predicting metabolic and cardiovascular disease risk in normal weight as well as overweight and obese children. J. Obes. 2014, 2014, 846578. [Google Scholar] [CrossRef]
- Micklesfield, L.K.; Goedecke, J.H.; Punyanitya, M.; Wilson, K.E.; Kelly, T.L. Dual-energy x-ray performs as well as clinical computed tomography for the measurement of visceral fat. Obesity 2012, 20, 1109–1114. [Google Scholar] [CrossRef]
- Bi, X.; Seabolt, L.; Shibao, C.; Buchowski, M.; Kang, H.; Keil, C.D.; Tyree, R.; Silver, H.J. DXA-measured visceral adipose tissue predicts impaired glucose tolerance and metabolic syndrome in obese Caucasian and African-American women. Eur. J. Clin. Nutr. 2015, 69, 329–336. [Google Scholar] [CrossRef]
- Schousboe, J.T.; Langsetmo, L.; Schwartz, A.V.; Taylor, B.C.; Vo, T.N.; Kats, A.M.; Barrett-Connor, E.; Orwoll, E.S.; Marshall, L.M.; Miljkovic, I.; et al. Comparison of associations of DXA and CT visceral adipose tissue measures with insulin resistance, lipid levels, and inflammatory markers. J. Clin. Densitom. 2017, 20, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Murray, T.E.; Williams, D.; Lee, M.J. Osteoporosis, obesity, and sarcopenia on abdominal CT: A review of epidemiology, diagnostic criteria, and management strategies for the reporting radiologist. Abdom. Radiol. 2017, 42, 2376–2386. [Google Scholar] [CrossRef] [PubMed]
- Farr, J.N.; Drake, M.T.; Amin, S.; Melton, L.J.; McCready, L.K.; Khosla, S. In vivo assessment of bone quality in postmenopausal women with type 2 diabetes. J. Bone Miner. Res. 2014, 29, 787–795. [Google Scholar] [CrossRef] [PubMed]
- Randall, C.; Bridges, D.; Guerri, R.; Nogues, X.; Puig, L.; Torres, E.; Mellibovsky, L.; Hoffseth, K.; Stalbaum, T.; Srikanth, A.; et al. Applications of a new handheld reference point indentation instrument measuring bone material strength. J. Med. Device 2013, 7, 410051–410056. [Google Scholar] [CrossRef]
- Malgo, F.; Hamdy, N.A.; Papapoulos, S.E.; Appelman-Dijkstra, N.M. Bone material strength as measured by microindentation in vivo is decreased in patients with fragility fractures independently of bone mineral density. J. Clin. Endocrinol. Metab. 2015, 100, 2039–2045. [Google Scholar] [CrossRef]
- Liu, Y.; Tang, G.-y.; Tang, R.-b.; Peng, Y.-f.; Li, W. Assessment of bone marrow changes in postmenopausal women with varying bone densities: Magnetic resonance spectroscopy and diffusion magnetic resonance imaging. Chin. Med. J. 2010, 123, 1524–1527. [Google Scholar] [PubMed]
- Paccou, J.; Hardouin, P.; Cotten, A.; Penel, G.; Cortet, B. The role of bone marrow fat in skeletal health: Usefulness and perspectives for clinicians. J. Clin. Endocrinol. Metab. 2015, 100, 3613–3621. [Google Scholar] [CrossRef]
- Tang, G.Y.; Lv, Z.W.; Tang, R.B.; Liu, Y.; Peng, Y.F.; Li, W.; Cheng, Y.S. Evaluation of MR spectroscopy and diffusion-weighted MRI in detecting bone marrow changes in postmenopausal women with osteoporosis. Clin. Radiol. 2010, 65, 377–381. [Google Scholar] [CrossRef]
- Paccou, J.; Penel, G.; Chauveau, C.; Cortet, B.; Hardouin, P. Marrow adiposity and bone: Review of clinical implications. Bone 2019, 118, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Bredella, M.A.; Fazeli, P.K.; Daley, S.M.; Miller, K.K.; Rosen, C.J.; Klibanski, A.; Torriani, M. Marrow fat composition in anorexia nervosa. Bone 2014, 66, 199–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanrahan, C.J.; Shah, L.M. MRI of spinal bone marrow: Part 2, T1-weighted imaging-based differential diagnosis. AJR Am. J. Roentgenol. 2011, 197, 1309–1321. [Google Scholar] [CrossRef] [PubMed]
- Barbosa-Silva, M.C.; Barros, A.J.; Wang, J.; Heymsfield, S.B.; Pierson, R.N., Jr. Bioelectrical impedance analysis: Population reference values for phase angle by age and sex. Am. J. Clin. Nutr. 2005, 82, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Brooks, N.; Layne, J.E.; Gordon, P.L.; Roubenoff, R.; Nelson, M.E.; Castaneda-Sceppa, C. Strength training improves muscle quality and insulin sensitivity in hispanic older adults with type 2 diabetes. Int. J. Med. Sci. 2006, 4, 19–27. [Google Scholar] [CrossRef]
- Wood, R.J.; Gregory, S.; Maneen, J.; Sullivan, R.; Richard, J.; Sawyer, J.; Matthews, T.D.; Headley, S.A.E. Weight loss and muscle quality in older men with metabolic syndrome. FASEB J. 2011, 25, 982. [Google Scholar]
- Looijaard, W.G.; Dekker, I.M.; Stapel, S.N.; Girbes, A.R.; Twisk, J.W.; Oudemans-van Straaten, H.M.; Weijs, P.J. Skeletal muscle quality as assessed by CT-derived skeletal muscle density is associated with 6-month mortality in mechanically ventilated critically ill patients. Crit. Care 2016, 20, 386. [Google Scholar] [CrossRef] [PubMed]
- Aubrey, J.; Esfandiari, N.; Baracos, V.E.; Buteau, F.A.; Frenette, J.; Putman, C.T.; Mazurak, V.C. Measurement of skeletal muscle radiation attenuation and basis of its biological variation. Acta Physiol. 2014, 210, 489–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mourtzakis, M.; Wischmeyer, P. Bedside ultrasound measurement of skeletal muscle. Curr. Opin. Clin. Nutr. Metab. Care 2014, 17, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Qin, X.; Fei, B. Measuring myofiber orientations from high-frequency ultrasound images using multiscale decompositions. Phys. Med. Biol. 2014, 59, 3907–3924. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Yamada, Y.; Fukumoto, Y.; Ishihara, T.; Yokoyama, K.; Yoshida, T.; Miyake, M.; Yamagata, E.; Kimura, M. Echo intensity obtained from ultrasonography images reflecting muscle strength in elderly men. Clin. Interv. Aging 2013, 8, 993–998. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bellamy, L.M.; Joanisse, S.; Grubb, A.; Mitchell, C.J.; McKay, B.R.; Phillips, S.M.; Baker, S.; Parise, G. The acute satellite cell response and skeletal muscle hypertrophy following resistance training. PLoS ONE 2014, 9, e109739. [Google Scholar] [CrossRef]
- Segal, N.A.; Williams, G.N.; Davis, M.C.; Wallace, R.B.; Mikesky, A.E. Efficacy of blood flow-restricted, low-load resistance training in women with risk factors for symptomatic knee osteoarthritis. PM R 2015, 7, 376–384. [Google Scholar] [CrossRef] [PubMed]
- Lenchik, L.; Boutin, R.D. Sarcopenia: Beyond muscle atrophy and into the new frontiers of opportunistic imaging, precision medicine, and machine learning. Semin. Musculoskelet. Radiol. 2018, 22, 307–322. [Google Scholar] [CrossRef] [PubMed]
- Tsigos, C.; Stefanaki, C.; Lambrou, G.I.; Boschiero, D.; Chrousos, G.P. Stress and inflammatory biomarkers and symptoms are associated with bioimpedance measures. Eur. J. Clin. Investig. 2015, 45, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.W.; Jo, H.H.; Kim, M.R.; You, Y.O.; Kim, J.H. Association between obesity, metabolic risks and serum osteocalcin level in postmenopausal women. Gynecol. Endocrinol. 2012, 28, 472–477. [Google Scholar] [CrossRef]
- Patti, A.; Gennari, L.; Merlotti, D.; Dotta, F.; Nuti, R. Endocrine actions of osteocalcin. Int. J. Endocrinol. 2013, 2013, 846480. [Google Scholar] [CrossRef]
- JafariNasabian, P.; Inglis, J.E.; Ave, M.P.; Hall, K.J.; Nieto, S.E.; Kelly, O.J.; Ilich, J.Z. Metabolic profile of osteosarcopenic obesity syndrome: Identifying biomarkers for diagnostic criteria. FASEB J. 2017, 31, 151–155. [Google Scholar]
- Ezzat-Zadeh, Z.; Kim, J.S.; Chase, P.B.; Arjmandi, B.H. The cooccurrence of obesity, osteoporosis, and sarcopenia in the ovariectomized rat: A study for modeling osteosarcopenic obesity in rodents. J. Aging Res. 2017, 2017, 1454103. [Google Scholar] [CrossRef]
- Abreu, E.L.; Cheng, A.L.; Kelly, P.J.; Chertoff, K.; Brotto, L.; Griffith, E.; Kinder, G.; Uridge, T.; Zachow, R.; Brotto, M. Skeletal muscle troponin as a novel biomarker to enhance assessment of the impact of strength training on fall prevention in the older adults. Nurs. Res. 2014, 63, 75–82. [Google Scholar] [CrossRef]
- Liu, P.-Y.; Hornbuckle, L.M.; Panton, L.B.; Kim, J.-S.; Ilich, J.Z. Evidence for the association between abdominal fat and cardiovascular risk factors in overweight and obese African American women. J. Am. Coll. Nutr. 2012, 31, 126–132. [Google Scholar] [CrossRef]
- Sanz, Y.; Moya-Perez, A. Microbiota, inflammation and obesity. Adv. Exp. Med. Biol. 2014, 817, 291–317. [Google Scholar] [PubMed]
- Mavros, Y.; Kay, S.; Simpson, K.A.; Baker, M.K.; Wang, Y.; Zhao, R.R.; Meiklejohn, J.; Climstein, M.; O’Sullivan, A.J.; de Vos, N.; et al. Reductions in c-reactive protein in older adults with type 2 diabetes are related to improvements in body composition following a randomized controlled trial of resistance training. J. Cachexia Sarcopenia Muscle 2014, 5, 111–120. [Google Scholar] [CrossRef]
- Schaap, L.A.; Pluijm, S.M.; Deeg, D.J.; Harris, T.B.; Kritchevsky, S.B.; Newman, A.B.; Colbert, L.H.; Pahor, M.; Rubin, S.M.; Tylavsky, F.A.; et al. Higher inflammatory marker levels in older persons: Associations with 5-year change in muscle mass and muscle strength. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 64, 1183–1189. [Google Scholar] [CrossRef] [PubMed]
- Di Renzo, L.; Sarlo, F.; Petramala, L.; Iacopino, L.; Monteleone, G.; Colica, C.; De Lorenzo, A. Association between −308 G/A TNF-α polymorphism and appendicular skeletal muscle mass index as a marker of sarcopenia in normal weight obese syndrome. Dis. Markers 2013, 35, 615–623. [Google Scholar] [CrossRef]
- Orsatti, F.L.; Nahas, E.A.; Nahas-Neto, J.; Orsatti, C.L.; Marocolo, M.; Barbosa-Neto, O.; da Mota, G.R. Low appendicular muscle mass is correlated with femoral neck bone mineral density loss in postmenopausal women. BMC Musculoskelet. Disord. 2011, 12, 225. [Google Scholar] [CrossRef] [PubMed]
- Rom, O.; Kaisari, S.; Aizenbud, D.; Reznick, A.Z. Lifestyle and sarcopenia-etiology, prevention, and treatment. Rambam Maimonides Med. J. 2012, 3, e0024. [Google Scholar] [CrossRef]
- Lawlor, D.A.; Chaturvedi, N. Treatment and prevention of obesity—Are there critical periods for intervention? Int. J. Epidemiol. 2006, 35, 3–9. [Google Scholar] [CrossRef]
- Garcia-Gonzalez, A.I.; Axtle-Serrano, Z.; Lopez-Teros, M.; Szlejf, C.; Martinez-Ruiz, A.; Rosas-Carrasco, O. Clinical interventions in osteosarcopenic obesity: Nutrition, physical and psychological activity. Rev. Med. Inst. Mex. Seguro. Soc. 2018, 56, S82–S93. [Google Scholar]
- Kelly, O.J.; Gilman, J.C.; Kim, Y.; Ilich, J.Z. Micronutrient intake in the etiology, prevention and treatment of osteosarcopenic obesity. Curr. Aging Sci. 2016, 9, 260–278. [Google Scholar] [CrossRef] [PubMed]
- Kelly, O.J.; Gilman, J.C.; Kim, Y.; Ilich, J.Z. Macronutrient intake and distribution in the etiology, prevention and treatment of osteosarcopenic obesity. Curr. Aging Sci. 2017, 10, 83–105. [Google Scholar] [CrossRef] [PubMed]
- Kelly, O.J.; Gilman, J.C.; Ilich, J.Z. Utilizing dietary micronutrient ratios in nutritional research may be more informative than focusing on single nutrients. Nutrients 2018, 10, 107. [Google Scholar] [CrossRef] [PubMed]
- Kelly, O.J.; Gilman, J.C.; Ilich, J.Z. Utilizing dietary nutrient ratios in nutritional research: Expanding the concept of nutrient ratios to macronutrients. Nutrients 2019, 11, 282. [Google Scholar] [CrossRef] [PubMed]
- Burchfield, J.G.; Kebede, M.A.; Meoli, C.C.; Stockli, J.; Whitworth, P.T.; Wright, A.L.; Hoffman, N.J.; Minard, A.Y.; Ma, X.; Krycer, J.R.; et al. High dietary fat and sucrose results in an extensive and time-dependent deterioration in health of multiple physiological systems in mice. J. Biol. Chem. 2018, 293, 5731–5745. [Google Scholar] [CrossRef]
- Genaro Pde, S.; Martini, L.A. Effect of protein intake on bone and muscle mass in the elderly. Nutr. Rev. 2010, 68, 616–623. [Google Scholar] [CrossRef]
- Heaney, R.P.; Layman, D.K. Amount and type of protein influences bone health. Am. J. Clin. Nutr. 2008, 87, 1567S–1570S. [Google Scholar] [CrossRef]
- Wallace, T.C.; Frankenfeld, C.L. Dietary protein intake above the current RDA and bone health: A systematic review and meta-analysis. J. Am. Coll. Nutr. 2017, 36, 481–496. [Google Scholar] [CrossRef] [PubMed]
- Borsheim, E.; Bui, Q.U.; Tissier, S.; Kobayashi, H.; Ferrando, A.A.; Wolfe, R.R. Effect of amino acid supplementation on muscle mass, strength and physical function in elderly. Clin. Nutr. 2008, 27, 189–195. [Google Scholar] [CrossRef]
- Mithal, A.; Bonjour, J.P.; Boonen, S.; Burckhardt, P.; Degens, H.; El Hajj Fuleihan, G.; Josse, R.; Lips, P.; Morales Torres, J.; Rizzoli, R.; et al. Impact of nutrition on muscle mass, strength, and performance in older adults. Osteoporos. Int. 2013, 24, 1555–1566. [Google Scholar] [CrossRef]
- Morley, J.E.; Argiles, J.M.; Evans, W.J.; Bhasin, S.; Cella, D.; Deutz, N.E.; Doehner, W.; Fearon, K.C.; Ferrucci, L.; Hellerstein, M.K.; et al. Nutritional recommendations for the management of sarcopenia. J. Am. Med. Dir. Assoc. 2010, 11, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Morton, R.W.; Murphy, K.T.; McKellar, S.R.; Schoenfeld, B.J.; Henselmans, M.; Helms, E.; Aragon, A.A.; Devries, M.C.; Banfield, L.; Krieger, J.W.; et al. A systematic review, meta-analysis and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults. Br. J. Sports Med. 2018, 52, 376. [Google Scholar]
- Paddon-Jones, D.; Rasmussen, B.B. Dietary protein recommendations and the prevention of sarcopenia. Curr. Opin. Clin. Nutr. Metab. Care 2009, 12, 86–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Du, Y.; Oh, C.; No, J.-k. Osteosarcopenic obesity in elderly: The cascade of bone, muscle, and fat in inflammatory process. Culin. Sci. Hosp. Res. 2017, 23, 173–183. [Google Scholar]
- Cunha, P.M.; Ribeiro, A.S.; Tomeleri, C.M.; Schoenfeld, B.J.; Silva, A.M.; Souza, M.F.; Nascimento, M.A.; Sardinha, L.B.; Cyrino, E.S. The effects of resistance training volume on osteosarcopenic obesity in older women. J. Sports Sci. 2018, 36, 1564–1571. [Google Scholar] [CrossRef] [PubMed]
- Kelly, O.J.; Gilman, J.C. Can unconventional exercise be helpful in the treatment, management and prevention of osteosarcopenic obesity? Curr. Aging Sci. 2017, 10, 106–121. [Google Scholar] [CrossRef] [PubMed]
| Component of OSO | Males | Females | ||
|---|---|---|---|---|
| Bone Mass | 1 | T-score for bone mineral density at the femoral neck, proximal femur or lumbar spine (DXA) ≤ −1.0 SD | 1 | T-score for bone mineral density at the femoral neck, proximal femur or lumbar spine (DXA) ≤ −1.0 SD |
| 2 | Total Bone Mass T-score (BIA-ACC®) ≤ −1.0 SD | 2 | Total Bone Mass T-score (BIA-ACC®) ≤ −1.0 SD | |
| Muscle Mass | 1 | Skeletal Mass Index (DXA, BIA) ≤ 5.45 kg/m2 | 1 | Skeletal Mass Index (DXA, BIA) ≤ 7.26 kg/m2 |
| 2 | ≤20th percentile of Appendicular Lean Mass (DXA, BIA) | 2 | ≤20th percentile of Appendicular Lean Mass (DXA, BIA) | |
| 3 | S-Score (BIA-ACC®) ≤ −1.0 SD | 3 | S-Score (BIA-ACC®) ≤ −1.0 SD | |
| Fat Mass | 1 | Total body fat (DXA, BIA) ≥ 25% | 1 | Total body fat (DXA, BIA) ≥ 32% |
| 2 | Fat Mass Index ≥ 9 kg/m2 | 2 | Fat Mass Index ≥ 13 kg/m2 | |
| Central or Visceral Fat | 1 | Visceral fat (CT, MRI) ≥ 130 cm2 | 1 | Visceral fat (CT, MRI) ≥ 110 cm2 |
| 2 | Visceral/Subcutaneous fat ratio (DXA) > 1 | 2 | Visceral/Subcutaneous fat ratio (DXA) > 1 | |
| 3 | Android/Gynoid fat ratio (DXA) ≤ 1.0 | 3 | Android/Gynoid fat ratio (DXA) ≤ 1.0 | |
| 4 | Intramuscular adipose tissue (IMAT) (BIA-ACC®) > 2.0% | 4 | Intramuscular adipose tissue (IMAT) (BIA-ACC®) > 2.0% | |
| 5 | Waist circumference ≥ 102 cm (40 inches) | 5 | Waist circumference ≥ 88 cm (35 inches) | |
| 6 | Waist–hip ratio > 0.90 | 6 | Waist–hip ratio > 0.85 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kelly, O.J.; Gilman, J.C.; Boschiero, D.; Ilich, J.Z. Osteosarcopenic Obesity: Current Knowledge, Revised Identification Criteria and Treatment Principles. Nutrients 2019, 11, 747. https://doi.org/10.3390/nu11040747
Kelly OJ, Gilman JC, Boschiero D, Ilich JZ. Osteosarcopenic Obesity: Current Knowledge, Revised Identification Criteria and Treatment Principles. Nutrients. 2019; 11(4):747. https://doi.org/10.3390/nu11040747
Chicago/Turabian StyleKelly, Owen J., Jennifer C. Gilman, Dario Boschiero, and Jasminka Z. Ilich. 2019. "Osteosarcopenic Obesity: Current Knowledge, Revised Identification Criteria and Treatment Principles" Nutrients 11, no. 4: 747. https://doi.org/10.3390/nu11040747





