Urothelial Cell Carcinoma of the Renal Pelvis Misdiagnosed as Ureteropelvic Junction Obstruction: A Case Report
Abstract
:1. Introduction
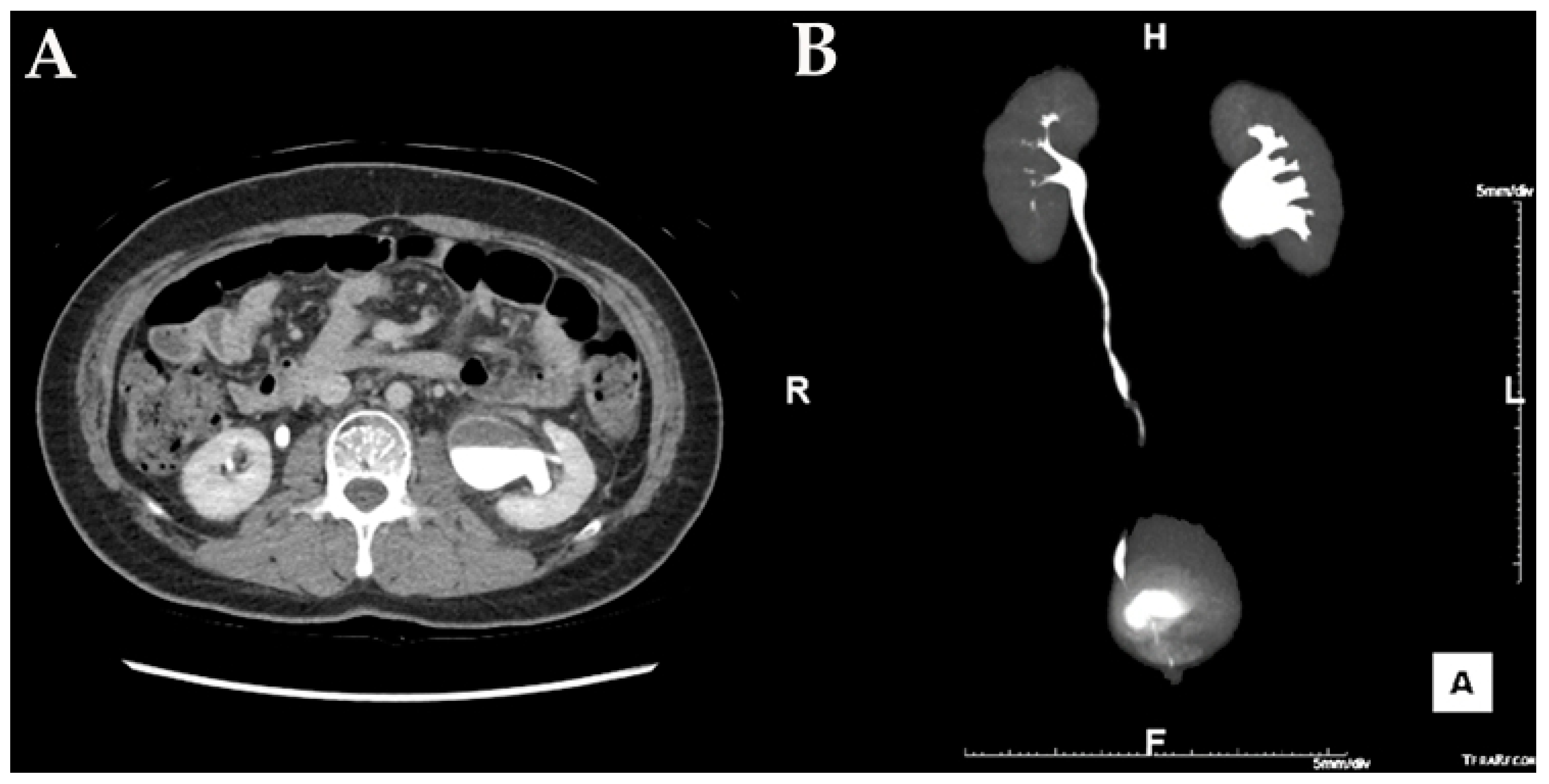
2. Case Report
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Saginala, K.; Barsouk, A.; Aluru, J.S.; Rawla, P.; Padala, S.A.; Barsouk, A. Epidemiology of bladder cancer. Med. Sci. 2020, 8, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tawfiek, E.R.; Bagley, D.H. Upper-tract transitional cell carcinoma. Urology 1997, 50, 321–329. [Google Scholar] [CrossRef]
- Rouprêt, M.; Zigeuner, R.; Palou, J.; Boehle, A.; Kaasinen, E.; Sylvester, R.; Babjuk, M.; Oosterlinck, W. European guidelines for the diagnosis and management of upper urinary tract urothelial cell carcinomas: 2011 update. Eur. Urol. 2011, 59, 584–594. [Google Scholar] [CrossRef] [PubMed]
- Goel, A.; Singh, D. Transitional cell cancer of ureter misdiagnosed as pelviureteric junction obstruction: Pitfalls of standard diagnostic tools. Indian J. Cancer 2008, 45, 184–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Margulis, V.; Shariat, S.F.; Matin, S.F.; Kamat, A.M.; Zigeuner, R.; Kikuchi, E.; Lotan, Y.; Weizer, A.; Raman, J.D.; Wood, G.G.; et al. Outcomes of radical nephroureterectomy: A series from the Upper Tract Urothelial Carcinoma Collaboration. Cancer 2009, 115, 1224–1233. [Google Scholar] [CrossRef] [PubMed]
- Shariat, S.F.; Favaretto, R.L.; Gupta, A.; Fritsche, H.-M.; Matsumoto, K.; Kassouf, W.; Walton, T.J.; Tritschler, S.; Baba, S.; Matsushita, K.; et al. Gender differences in radical nephroureterectomy for upper tract urothelial carcinoma. World J. Urol. 2011, 29, 481–486. [Google Scholar] [CrossRef]
- Green, D.A.; Rink, M.; Xylinas, E.; Matin, S.F.; Stenzl, A.; Roupret, M.; Karakiewicz, P.I.; Scherr, D.S.; Shariat, S.F. Urothelial carcinoma of the bladder and the upper tract: Disparate twins. J. Urol. 2013, 189, 1214–1221. [Google Scholar] [CrossRef] [PubMed]
- Colin, P.; Koenig, P.; Ouzzane, A.; Berthon, N.; Villers, A.; Biserte, J.; Roupret, M. Environmental factors involved in carcinogenesis of urothelial cell carcinomas of the upper urinary tract. BJU Int. 2009, 104, 1436–1440. [Google Scholar] [CrossRef]
- McLaughlin, J.K.; Silverman, D.T.; Hsing, A.W.; Ross, R.K.; Schoenberg, J.B.; Yu, M.C.; Stemhagen, A.; Lynch, C.F.; Blot, W.J.; Fraumeni, J.F.J. Cigarette smoking and cancers of the renal pelvis and ureter. Cancer Res. 1992, 52, 254–257. [Google Scholar]
- Crivelli, J.J.; Xylinas, E.; Kluth, L.A.; Rieken, M.; Rink, M.; Shariat, S.F. Effect of smoking on outcomes of urothelial carcinoma: A systematic review of the literature. Eur. Urol. 2014, 65, 742–754. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.J.; Chuang, Y.C.; You, S.L.; Lin, T.M.; Wu, H.Y. A retrospective study on malignant neoplasms of bladder, lung and liver in blackfoot disease endemic area in Taiwan. Br. J. Cancer 1986, 53, 399–405. [Google Scholar] [CrossRef]
- Hopenhayn-Rich, C.; Biggs, M.L.; Smith, A.H. Lung and kidney cancer mortality associated with arsenic in drinking water in Córdoba, Argentina. Int. J. Epidemiol. 1998, 27, 561–569. [Google Scholar] [CrossRef]
- Kurttio, P.; Pukkala, E.; Kahelin, H.; Auvinen, A.; Pekkanen, J. Arsenic concentrations in well water and risk of bladder and kidney cancer in Finland. Environ. Health Perspect. 1999, 107, 705–710. [Google Scholar] [CrossRef]
- Chow, W.-H.; Gridley, G.; Linet, M.S.; Pennello, G.A.; Fraumeni, J.F.J.; Lindblad, P.; Nyren, O.; McLaughlin, J.K.; Adami, H.-O. Risk of urinary tract cancers following kidney or ureter stones. J. Natl. Cancer Inst. 1997, 89, 1453–1457. [Google Scholar] [CrossRef] [PubMed]
- Stewart, G.D.; Bariol, S.V.; Grigor, K.M.; Tolley, D.A.; McNeill, S.A. A comparison of the pathology of transitional cell carcinoma of the bladder and upper urinary tract. BJU Int. 2005, 95, 791–793. [Google Scholar] [CrossRef]
- Vasudeva, P.; Kumar, N.; Kumar, A. Transitional cell carcinoma: A rare development in congenital ureteropelvic junction obstruction kidney. Indian J. Urol. 2016, 32, 79–80. [Google Scholar] [CrossRef] [PubMed]
- Nomikos, M.; Pappas, A.; Kopaka, M.-E.; Tzoulakis, S.; Volonakis, I.; Stavrakakis, G.; Avgenakis, G.; Anezinis, P. Urothelial carcinoma of the urinary bladder in young adults: Presentation, clinical behavior and outcome. Adv. Urol. 2011, 2011, 480738. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wen, Y.-C.; Kuo, J.-Y.; Chen, K.-K.; Lin, A.T.L.; Chang, Y.-H.; Hsu, Y.-S.; Chang, L.S. Urothelial carcinoma of the urinary bladder in young adults—clinical experience at Taipei Veterans General Hospital. J. Chin. Med. Assoc. 2005, 68, 272–275. [Google Scholar] [CrossRef] [Green Version]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, J.-H.; Choi, T.-S.; Lee, D.-G.; Min, G.-E. Urothelial Cell Carcinoma of the Renal Pelvis Misdiagnosed as Ureteropelvic Junction Obstruction: A Case Report. Medicina 2021, 57, 1158. https://doi.org/10.3390/medicina57111158
Choi J-H, Choi T-S, Lee D-G, Min G-E. Urothelial Cell Carcinoma of the Renal Pelvis Misdiagnosed as Ureteropelvic Junction Obstruction: A Case Report. Medicina. 2021; 57(11):1158. https://doi.org/10.3390/medicina57111158
Chicago/Turabian StyleChoi, Jeong-Hyouk, Tae-Soo Choi, Dong-Gi Lee, and Gyeong-Eun Min. 2021. "Urothelial Cell Carcinoma of the Renal Pelvis Misdiagnosed as Ureteropelvic Junction Obstruction: A Case Report" Medicina 57, no. 11: 1158. https://doi.org/10.3390/medicina57111158





