Different Treatments in Patients with Temporomandibular Joint Disorders: A Comparative Randomized Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Inclusion Criteria
2.3. Treatments
2.4. Pain and Mouth Opening Measurements
2.5. Statistics
3. Results
3.1. Patient Description
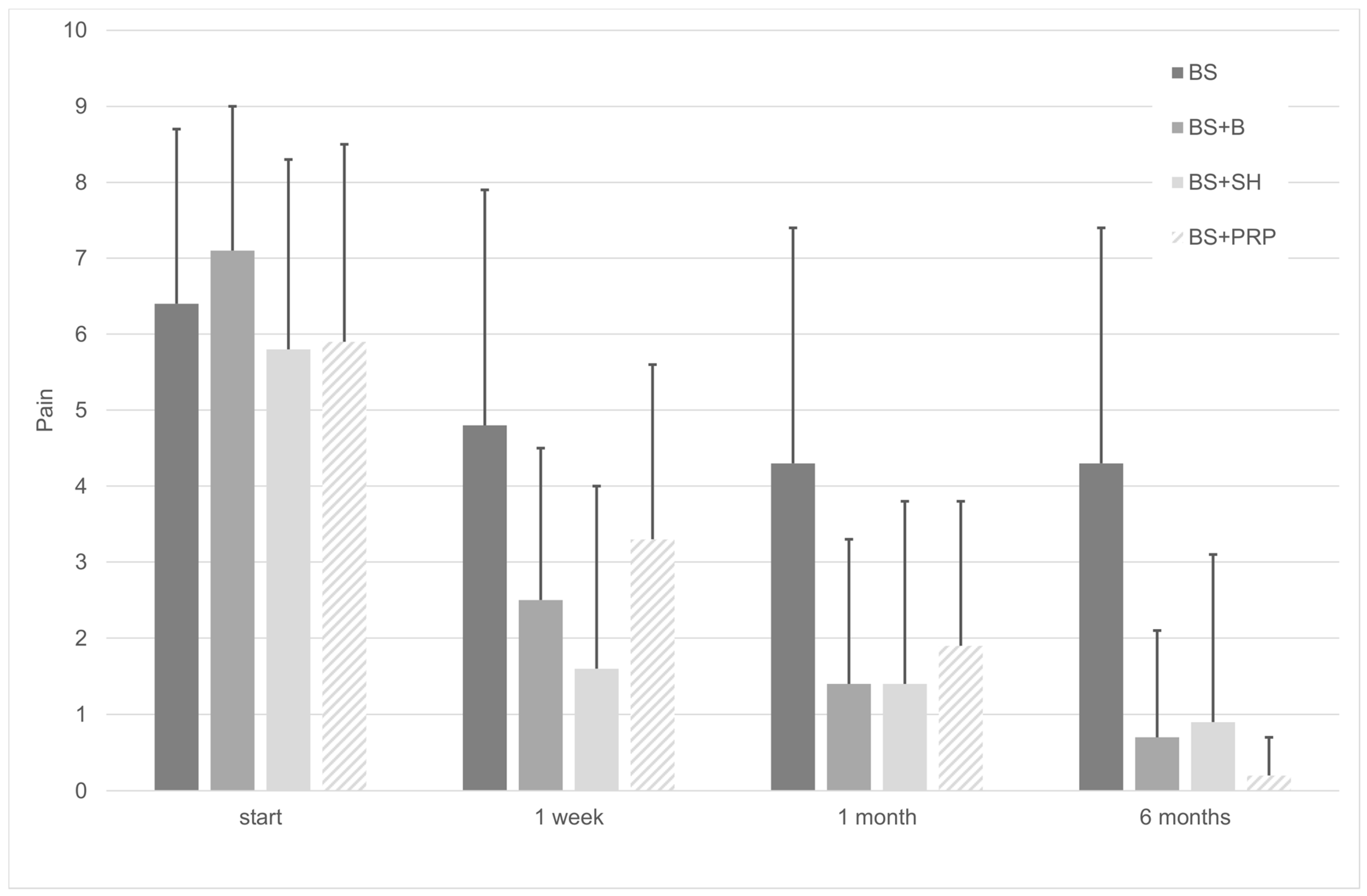
3.2. Treatments Reduce Pain
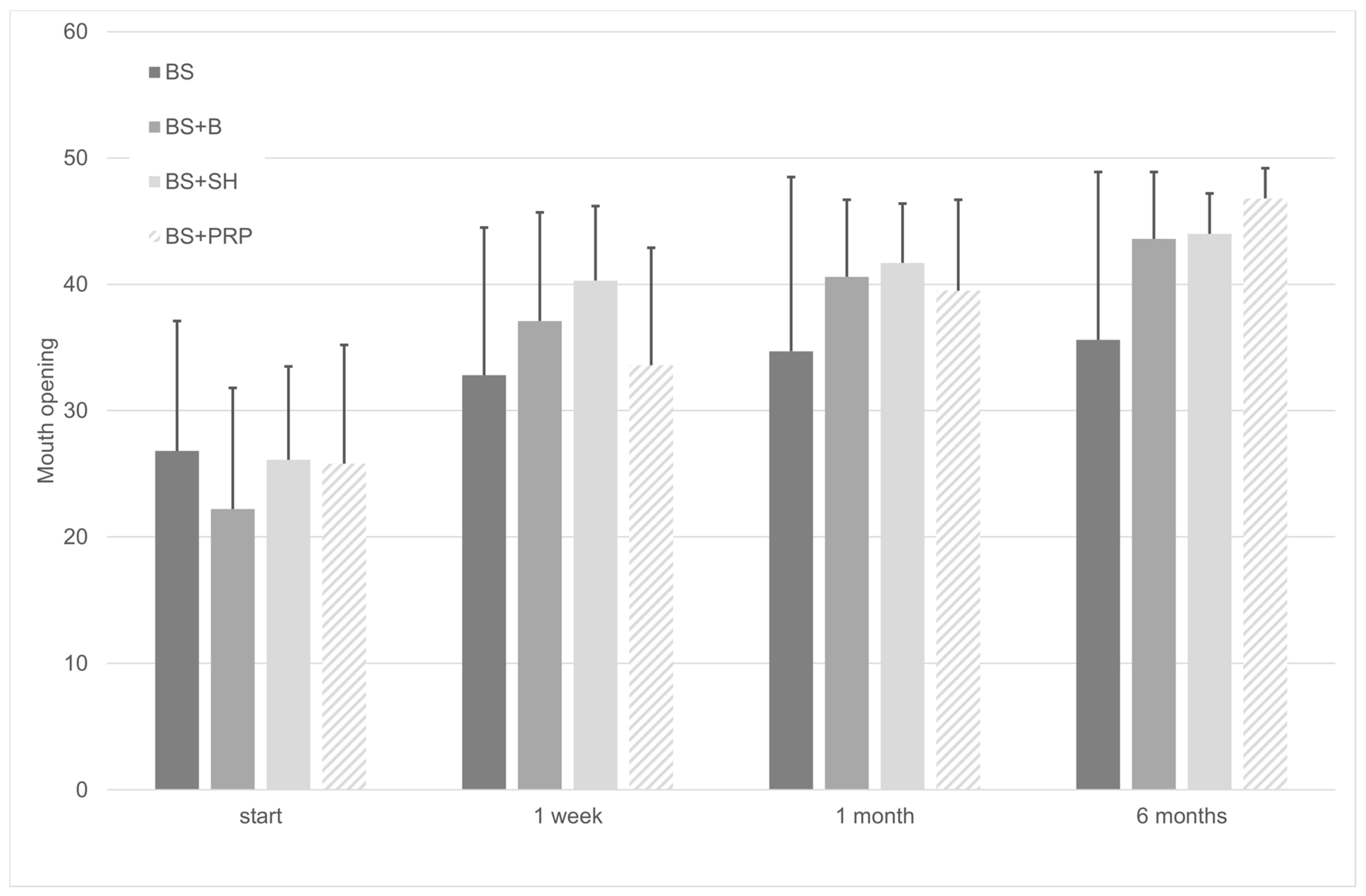
3.3. Treatments Increase Mouth Opening
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- LeResche, L.; Mancl, L.; Sherman, J.J.; Gandara, B.; Dworkin, S.F. Changes in temporomandibular pain and other symptoms across the menstrual cycle. Pain 2003, 106, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Poveda, R.; Fernández, J.M.D.; Bazán, S.H.; Soriano, Y.J.; Margaix, M.; Sarrión, G. A review of temporomandibular joint disease (TMJD). Part II: Clinical and radiological semiology. Morbidity processes. Med. Oral Patol. Oral Cir. Bucal 2008, 13. [Google Scholar] [CrossRef]
- Liu, H.X.; Liang, Q.J.; Xiao, P.; Jiao, H.X.; Gao, Y.; Ahmetjiang, A. The effectiveness of cognitive-behavioural therapy for temporomandibular disorders: A systematic review. J. Oral Rehabil. 2011, 39, 55–62. [Google Scholar] [CrossRef]
- Nadershah, M. Prevalence of Temporomandibular Joint Disorders in Adults in Jeddah, Kingdom of Saudi Arabia: A Cross-sectional Study. J. Contemp. Dent. Pract. 2019, 20, 1009–1013. [Google Scholar] [CrossRef]
- Ali, H.M. Diagnostic Criteria for Temporomandibular Joint Disorders. Physiotherapy 2002, 88, 421–426. [Google Scholar]
- Wänman, A.; Marklund, S. Treatment outcome of supervised exercise, home exercise and bite splint therapy, respectively, in patients with symptomatic disc displacement with reduction: A randomised clinical trial. J. Oral Rehabil. 2019, 47, 143–149. [Google Scholar] [CrossRef] [PubMed]
- La Touche, R.; Fernández-De-Las-Peñas, C.; Fernández-Carnero, J.; Escalante, K.; Angulo-Díaz-Parreño, S.; Paris-Alemany, A.; Cleland, J.A. The effects of manual therapy and exercise directed at the cervical spine on pain and pressure pain sensitivity in patients with myofascial temporomandibular disorders. J. Oral Rehabil. 2009, 36, 644–652. [Google Scholar] [CrossRef] [PubMed]
- Sindelar, B.J.; Herring, S.W.; Alonzo, T.A. The effects of intraoral splints on the masticatory system of pigs. J. Oral Rehabil. 2003, 30, 823–831. [Google Scholar] [CrossRef] [PubMed]
- Shaefer, J.R.; Holland, N.; Whelan, J.; Velly, A.M. Pain and Temporomandibular Disorders. Dent. Clin. N. Am. 2013, 57, 233–262. [Google Scholar] [CrossRef]
- Greene, C.S.; Menchel, H.F. The Use of Oral Appliances in the Management of Temporomandibular Disorders. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 265–277. [Google Scholar] [CrossRef]
- Ramfjord, S.; Ash, M.M. Reflections on the Michigan occlusal splint. J. Oral Rehabil. 1994, 21, 491–500. [Google Scholar] [CrossRef]
- Marzook, H.A.; Razek, A.A.A.; Yousef, E.A.; Attia, A.A.M. Intra-articular injection of a mixture of hyaluronic acid and corticosteroid versus arthrocentesis in TMJ internal derangement. J. Stomatol. Oral Maxillofac. Surg. 2020, 121, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Alstergren, P.; Appelgren, A.; Appelgren, B.; Kopp, S.; Lundeberg, T.; Theodorsson, E. The effect on joint fluid concentration of neuropeptide Y by intra-articular injection of glucocorticoid in temporomandibular joint arthritis. Acta Odontol. Scand. 1996, 54. [Google Scholar] [CrossRef] [PubMed]
- Kopp, S.; Akerman, S.; Nilner, M. Short-term effects of intra-articular sodium hyaluronate, glucocorticoid, and saline injections on rheumatoid arthritis of the temporomandibular joint. J. Craniomandib. Disord. Facial Oral Pain 1991, 5, 231–238. [Google Scholar]
- Wenneberg, B.; Kopp, S.; Gröndahl, H.G. Long-term effect of intra-articular injections of a glucocorticosteroid into the TMJ: A clinical and radiographic 8-year follow-up. J. Craniomandib. Disord. Facial Oral Pain 1991, 5, 11–18. [Google Scholar]
- Bjørnland, T.; Gjærum, A.A.; Møystad, A. Osteoarthritis of the temporomandibular joint: An evaluation of the effects and complications of corticosteroid injection compared with injection with sodium hyaluronate. J. Oral Rehabil. 2007, 34, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Kopp, S.; Wenneberg, B. Effects of Occlusal Treatment and Intraarticular Injections on Temporomandibular Joint Pain and Dysfunction. Acta Odontol. Scand. 1981, 39, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Fredriksson, L.; Alstergren, P.; Kopp, S. Tumor Necrosis Factor-α in Temporomandibular Joint Synovial Fluid Predicts Treatment Effects on Pain by Intra-Articular Glucocorticoid Treatment. Mediat. Inflamm. 2006, 2006, 1–7. [Google Scholar] [CrossRef]
- Pei, L.; Li, X.; Liu, Y.; Wang, X.; Ding, H.; Wang, Z.; Zhou, X. Percutaneous intra-articular injections of ropivacaine, and tranexamic acid and removal of the drainage tube one day after total knee arthroplasty as a component of enhanced recovery after surgery: A randomized control trial. J. Orthop. Surg. Res. 2020. [Google Scholar] [CrossRef]
- Yeung, R.W.K.; Chow, R.L.K.; Samman, N.; Chiu, K. Short-term therapeutic outcome of intra-articular high molecular weight hyaluronic acid injection for nonreducing disc displacement of the temporomandibular joint. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2006, 102, 453–461. [Google Scholar] [CrossRef]
- Nardini, L.G.; Masiero, S.; Marioni, G. Conservative treatment of temporomandibular joint osteoarthrosis: Intra-articular injection of sodium hyaluronate. J. Oral Rehabilitation 2005, 32, 729–734. [Google Scholar] [CrossRef] [PubMed]
- Nardini, L.G.; Tito, R.; Staffieri, A.; Beltrame, A. Treatment of patients with arthrosis of the temporomandibular joint by infiltration of sodium hyaluronate: A preliminary study. Eur. Arch. Oto-Rhino-Laryngol. 2002, 259, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Hepguler, S.; Akkoc, Y.S.; Pehlivan, M.; Ozturk, C.; Celebi, G.; Saracoglu, A.; Ozpinar, B. The efficacy of intra-articular sodium hyaluronate in patients with reducing displaced disc of the temporomandibular joint. J. Oral Rehabil. 2002, 29, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Piccotti, F.; Guarda-Nardini, L. Hyaluronic Acid In the Treatment of TMJ Disorders: A Systematic Review of the Literature. CRANIO® 2010, 28, 166–176. [Google Scholar] [CrossRef]
- Goa, K.L.; Benfield, P. Hyaluronic acid. A review of its pharmacology and use as a surgical aid in ophthalmology, and its therapeutic potential in joint disease and wound healing. Drugs 1994, 47, 536–566. [Google Scholar] [CrossRef]
- Civinini, R.; Macera, A.; Nistri, L.; Redl, B.; Innocenti, M. The use of autologous blood-derived growth factors in bone regeneration. Clin. Cases Miner. Bone Metab. 2011, 8, 25–31. [Google Scholar]
- Del Vecchio, A.; Floravanti, M.; Boccassini, A.; Gaimari, G.; Vestri, A.; Di Paolo, C.; Romeo, U. Evaluation of the efficacy of a new low-level laser therapy home protocol in the treatment of temporomandibular joint disorder-related pain: A randomized, double-blind, placebo-controlled clinical trial. CRANIO® 2019. [Google Scholar] [CrossRef]
- Moldez, M.; Camones, V.; Ramos, G.; Padilla, M.; Enciso, R. Effectiveness of Intra-Articular Injections of Sodium Hyaluronate or Corticosteroids for Intracapsular Temporomandibular Disorders: A Systematic Review and Meta-Analysis. J. Oral Facial Pain Headache 2018, 32, 53–66. [Google Scholar] [CrossRef]
- Giraddi, G.B.; Siddaraju, A.; Kumar, A.; Jain, T. Comparison Between Betamethasone and Sodium Hyaluronate Combination with Betamethasone Alone After Arthrocentesis in the Treatment of Internal Derangement of TMJ—Using Single Puncture Technique: A Preliminary Study. J. Maxillofac. Oral Surg. 2014, 14, 403–409. [Google Scholar] [CrossRef]
- Klasser, G.D.; Greene, C.S. Oral appliances in the management of temporomandibular disorders. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2009, 107, 212–223. [Google Scholar] [CrossRef]
- Gencer, Z.K.; Ozkiris, M.; Okur, A.; Korkmaz, M.; Saydam, L. A comparative study on the impact of intra-articular injections of hyaluronic acid, tenoxicam and betametazon on the relief of temporomandibular joint disorder complaints. J. Craniomaxillofac. Surg. 2014, 42, 1117–1121. [Google Scholar] [CrossRef] [PubMed]
- Giraddi, G.B.; Siddaraju, A.; Kumar, B.; Singh, C. Internal Derangement of Temporomandibular Joint: An Evaluation of Effect of Corticosteroid Injection Compared with Injection of Sodium Hyaluronate after Arthrocentesis. J. Maxillofac. Oral Surg. 2011, 11, 258–263. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zotti, F.; Albanese, M.; Rodella, L.; Nocini, P.F. Platelet-Rich Plasma in Treatment of Temporomandibular Joint Dysfunctions: Narrative Review. Int. J. Mol. Sci. 2019, 20, 277. [Google Scholar] [CrossRef] [PubMed]
- Hegab, A.; Ali, H.E.; Elmasry, M.; Khallaf, M.G. Platelet-Rich Plasma Injection as an Effective Treatment for Temporomandibular Joint Osteoarthritis. J. Oral Maxillofac. Surg. 2015, 73, 1706–1713. [Google Scholar] [CrossRef]
- Hohmann, E.; Tetsworth, K.; Glatt, V. Is platelet-rich plasma effective for the treatment of knee osteoarthritis? A systematic review and meta-analysis of level 1 and 2 randomized controlled trials. Eur. J. Orthop. Surg. Traumatol. 2020, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Wu, J.-Y.; Deng, D.-L.; He, B.-Y.; Tao, Y.; Niu, Y.-M.; Deng, M.-H. Efficacy of splint therapy for the management of temporomandibular disorders: A meta-analysis. Oncotarget 2016, 7, 84043–84053. [Google Scholar] [CrossRef] [PubMed]
- Vingender, S.; Restár, L.; Csomó, K.B.; Schmidt, P.; Hermann, P.; Vaszilkó, M. Intra-articular steroid and hyaluronic acid treatment of internal derangement of the temporomandibular joint. Orv. Hetil. 2018, 159, 1475–1482. [Google Scholar] [CrossRef] [PubMed]
- Goiato, M.; Da Silva, E.V.F.; De Medeiros, R.; Túrcio, K.; Dos Santos, D. Are intra-articular injections of hyaluronic acid effective for the treatment of temporomandibular disorders? A systematic review. Int. J. Oral Maxillofac. Surg. 2016, 45, 1531–1537. [Google Scholar] [CrossRef]
| Treatment | BS | BS + B | BS + SH | BS + PSP |
|---|---|---|---|---|
| Gender (M/F) | 4/16 (20%/80%) | 4/16 (20%/80%) | 4/16 (20%/80%) | 4/16 (20%/80%) |
| Age ( | 41.3 (17.7) | 40.8 (17.0) | 37.4 (14.1) | 36.7 (13.1) |
| Pain Values | Regression Analysis | ||||||
|---|---|---|---|---|---|---|---|
| Group | Start | 1 Week | 1 Month | 6 Months | p | R2adj | B (IC95%) |
| BS | 6.4 (2.3) | 4.8 (3.1) | 4.3 (3.1) | 4.3 (3.1) | 0.145 * | 0.015 | −0.050 (−0.118, 0.018) |
| BS + B | 7.1 (1.9) | 2.5 (2.0) | 1.4 (1.9) | 0.7 (1.4) | <0.001 | 0.240 | −0.156 (−0.218, −0.094) |
| BS + SH | 5.8 (2.5) | 1.6 (2.4) | 1.4 (2.4) | 0.9 (2.2) | 0.002 | 0.109 | −0.108 (−0.174, −0.042) |
| BS + PRP | 5.9 (2.6) | 3.3 (2.3) | 1.9 (1.9) | 0.2 (0.5) | <0.001 | 0.343 | −0.172 (−0.224, −0.119) |
| Mouth Opening Values (mm) | Regression Analysis | ||||||
|---|---|---|---|---|---|---|---|
| Group | Start | 1 Week | 1 Month | 6 Months | p | R2adj | B IC95% |
| BS | 26.8 (10.3) | 32.8 (11.7) | 34.7 (13.8) | 35.6 (13.3) | 0.128 | 0.017 | 0.219 (−0.065, 0.503) |
| BS + B | 22.2 (9.6) | 37.1 (8.6) | 40.6 (6.1) | 43.6 (5.3) | <0.001 | 0.219 | 0.546 (0.316, 0.776) |
| BS + SH | 26.1 (7.4) | 40.3 (5.9) | 41.7 (4.7) | 44.0 (3.2) | <0.001 | 0.204 | 0.418 (0.237, 0.598) |
| BS + PRP | 25.8 (9.4) | 33.6 (9.3) | 39.5 (7.2) | 46.8 (2.4) | <0.001 | 0.372 | 0.676 (0.482, 0.871) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Macedo De Sousa, B.; López-Valverde, N.; López-Valverde, A.; Caramelo, F.; Flores Fraile, J.; Herrero Payo, J.; Rodrigues, M.J. Different Treatments in Patients with Temporomandibular Joint Disorders: A Comparative Randomized Study. Medicina 2020, 56, 113. https://doi.org/10.3390/medicina56030113
Macedo De Sousa B, López-Valverde N, López-Valverde A, Caramelo F, Flores Fraile J, Herrero Payo J, Rodrigues MJ. Different Treatments in Patients with Temporomandibular Joint Disorders: A Comparative Randomized Study. Medicina. 2020; 56(3):113. https://doi.org/10.3390/medicina56030113
Chicago/Turabian StyleMacedo De Sousa, Bruno, Nansi López-Valverde, Antonio López-Valverde, Francisco Caramelo, Javier Flores Fraile, Julio Herrero Payo, and María João Rodrigues. 2020. "Different Treatments in Patients with Temporomandibular Joint Disorders: A Comparative Randomized Study" Medicina 56, no. 3: 113. https://doi.org/10.3390/medicina56030113
APA StyleMacedo De Sousa, B., López-Valverde, N., López-Valverde, A., Caramelo, F., Flores Fraile, J., Herrero Payo, J., & Rodrigues, M. J. (2020). Different Treatments in Patients with Temporomandibular Joint Disorders: A Comparative Randomized Study. Medicina, 56(3), 113. https://doi.org/10.3390/medicina56030113








