Comparative Analysis of Three Machine-Learning Techniques and Conventional Techniques for Predicting Sepsis-Induced Coagulopathy Progression
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Setting
2.2. Data Collection
2.3. Definitions
2.4. Outcomes
2.5. Statistical Analysis
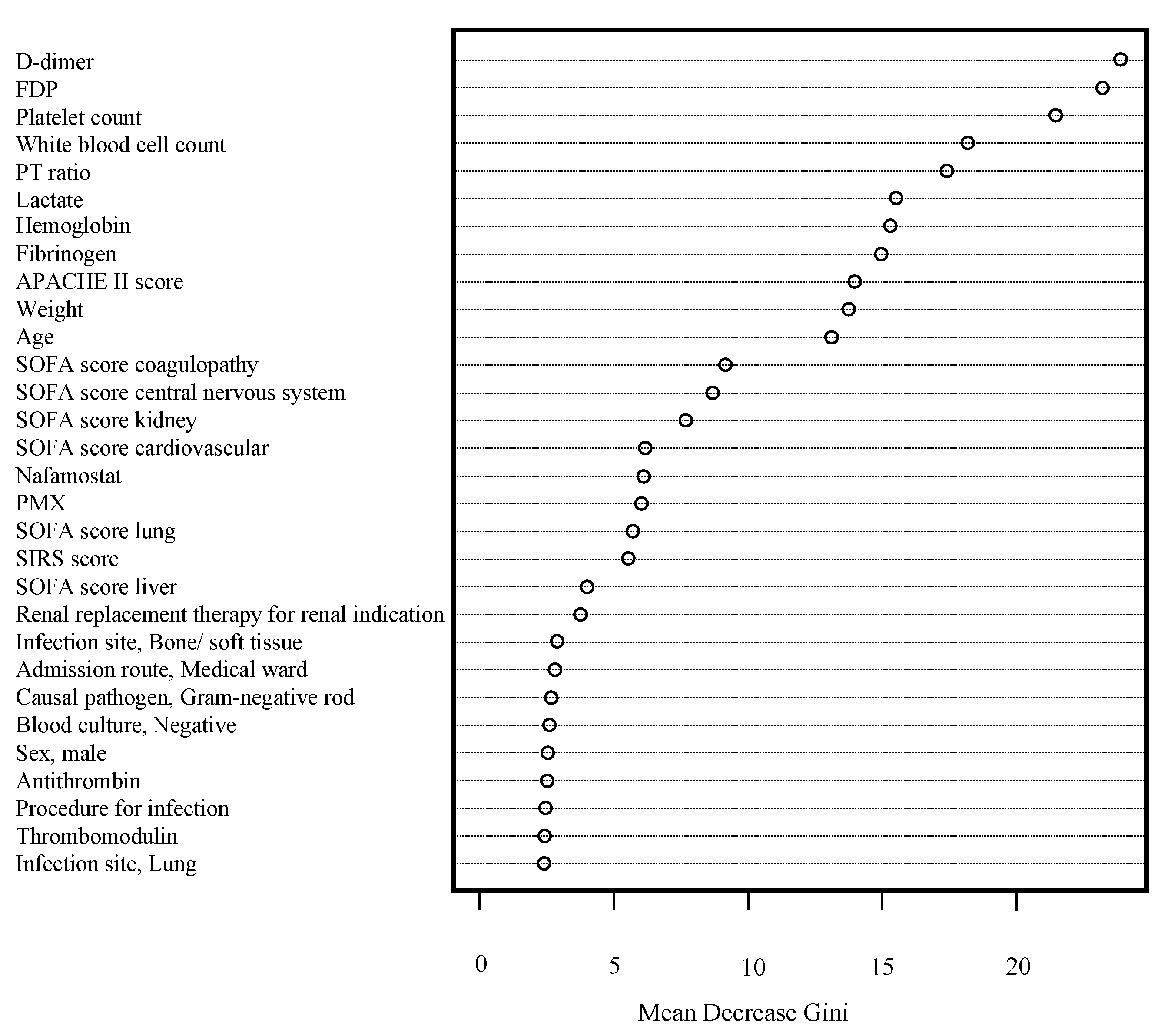
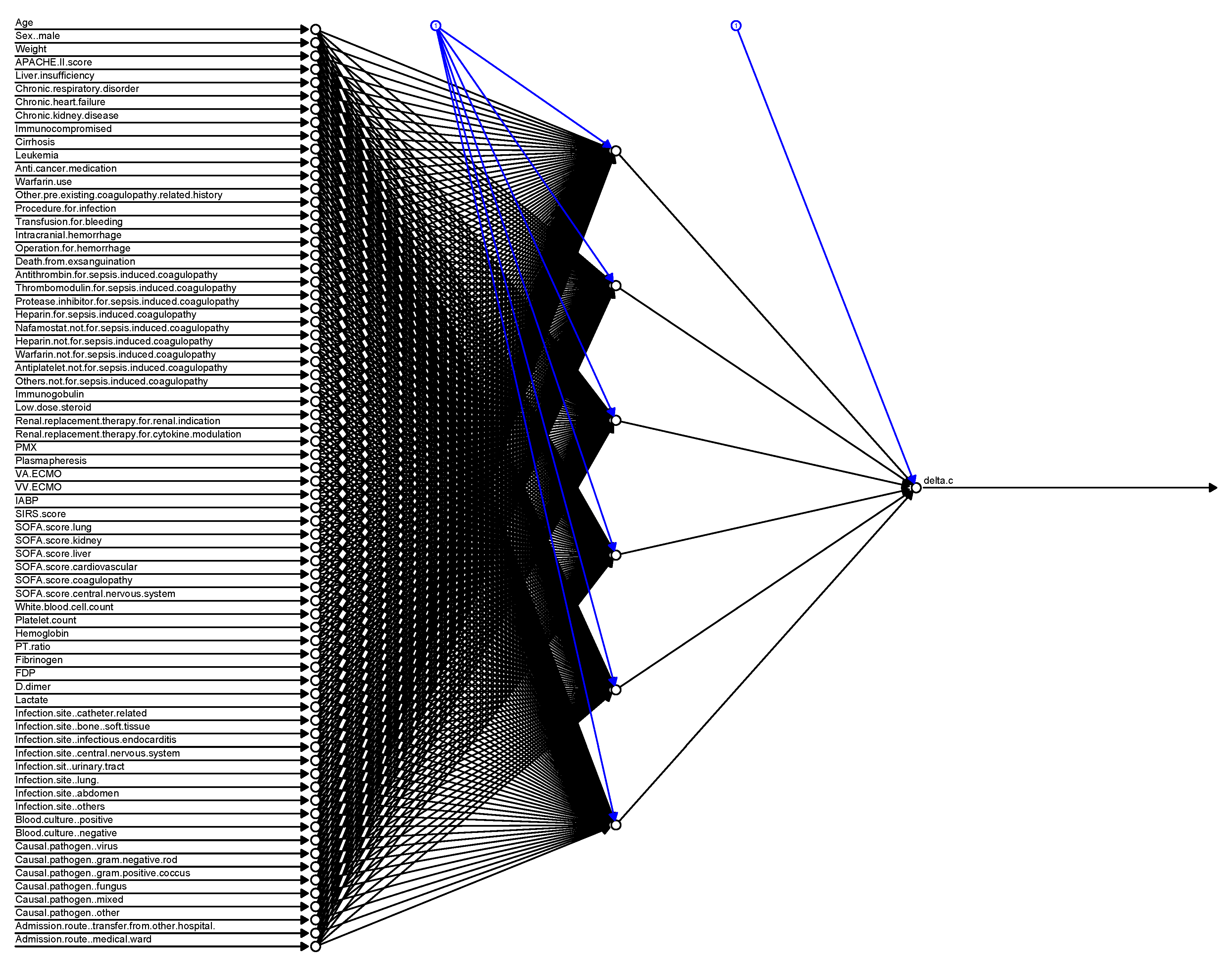
3. Results
3.1. Study Population and Included Covariates
3.1.1. Prediction Accuracy with Conventional and Machine-Learning Approaches
3.1.2. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). J. Am. Med. Assoc. 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Dhainaut, J.F.; Yan, S.B.; Joyce, D.E.; Pettilä, V.; Basson, B.; Brandt, J.T.; Sundin, D.P.; Levi, M. Treatment effects of drotrecogin alfa (activated) in patients with severe sepsis with or without overt disseminated intravascular coagulation. J. Thromb. Haemost. 2004, 2, 1924–1933. [Google Scholar] [CrossRef] [PubMed]
- Moore, H.B.; Winfield, R.D.; Aibiki, M.; Neal, M.D. Is coagulopathy an appropriate therapeutic target during critical illness such as trauma or sepsis? Shock 2017, 48, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Gando, S.; Levi, M.; Toh, C.H. Disseminated intravascular coagulation. Nat. Rev. Dis. Primers 2016, 2, 16037. [Google Scholar] [CrossRef] [PubMed]
- Lyons, P.G.; Micek, S.T.; Hampton, N.; Kollef, M.H. Sepsis-associated coagulopathy severity predicts hospital mortality. Crit. Care Med. 2018, 46, 736–742. [Google Scholar] [CrossRef]
- Attia, Z.I.; Noseworthy, P.A.; Lopez-Jimenez, F.; Asirvatham, S.J.; Deshmukh, A.J.; Gersh, B.J.; Carter, R.E.; Yao, X.; Rabinstein, A.A.; Erickson, B.J.; et al. An artificial intelligence-enabled ECG algorithm for the identification of patients with atrial fibrillation during sinus rhythm: A retrospective analysis of outcome prediction. Lancet 2019, 394, 861–867. [Google Scholar] [CrossRef]
- Hayakawa, M.; Yamakawa, K.; Saito, S.; Uchino, S.; Kudo, D.; Iizuka, Y.; Sanui, M.; Takimoto, K.; Mayumi, T. Nationwide registry of sepsis patients in Japan focused on disseminated intravascular coagulation 2011–2013. Sci. Data 2018, 5, 180243. [Google Scholar] [CrossRef]
- Hayakawa, M.; Saito, S.; Uchino, S.; Yamakawa, K.; Kudo, D.; Iizuka, Y.; Sanui, M.; Takimoto, K.; Mayumi, T.; Azuhata, T.; et al. Characteristics, treatments, and outcomes of severe sepsis of 3195 ICU-treated adult patients throughout Japan during 2011–2013. J. Intensive Care 2016, 4, 44. [Google Scholar] [CrossRef] [Green Version]
- Knaus, W.A.; Draper, E.A.; Wagner, D.P.; Zimmerman, J.E. APACHE II: A severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef]
- Vincent, J.L.; De Mendonça, A.; Cantraine, F.; Moreno, R.; Takala, J.; Suter, P.M.; Sprung, C.L.; Colardyn, F.; Blecher, S. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: Results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit. Care Med. 1998, 26, 1793–1800. [Google Scholar] [CrossRef]
- Bone, R.C.; Balk, R.A.; Cerra, F.B.; Dellinger, R.P.; Fein, A.M.; Knaus, W.A.; Schein, R.M.H.; Sibbald, W.J. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. Chest 1992, 101, 1644–1655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, F.B., Jr.; Toh, C.H.; Hoots, W.K.; Wada, H.; Levi, M. Scientific Subcommittee on Disseminated Intravascular Coagulation (DIC) of the International Society on Thrombosis and Haemostasis (ISTH). Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb. Haemost. 2001, 86, 1327–1330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gando, S.; Saitoh, D.; Ogura, H.; Mayumi, T.; Koseki, K.; Ikeda, T.; Ishikura, H.; Iba, T.; Ueyama, M.; Eguchi, Y.; et al. Japanese Association for Acute Medicine Disseminated Intravascular Coagulation (JAAM DIC) Study Group. Natural history of disseminated intravascular coagulation diagnosed based on the newly established diagnostic criteria for critically ill patients: Results of a multicenter, prospective survey. Crit. Care Med. 2008, 36, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Akaike, H. A new look at the statistical model identification. IEEE. Trans. Automat. Control 1974, 19, 716–723. [Google Scholar] [CrossRef]
- Alderden, J.; Pepper, G.A.; Wilson, A.; Whitney, J.D.; Richardson, S.; Butcher, R.; Jo, Y.; Cummins, M.R. Predicting pressure injury in critical care patients: A machine-learning model. Am. J. Crit. Care 2018, 27, 461–468. [Google Scholar] [CrossRef]
- Ben-Hur, A.; Weston, J. A user’s guide to support vector machines. Methods Mol. Biol. 2010, 609, 223–239. [Google Scholar] [CrossRef] [Green Version]
- Clermont, G. Artificial neural networks as prediction tools in the critically ill. Crit. Care 2005, 9, 153–154. [Google Scholar] [CrossRef] [Green Version]
- Papageorgiou, C.; Jourdi, G.; Adjambri, E.; Walborn, A.; Patel, P.; Fareed, J.; Elalamy, I.; Hoppensteadt, D.; Gerotziafas, G.T. Disseminated intravascular coagulation: An update on pathogenesis, diagnosis, and therapeutic strategies. Clin. Appl. Thromb. Hemost. 2018, 24, 8S–28S. [Google Scholar] [CrossRef] [Green Version]
- Thachil, J. Disseminated intravascular coagulation—New pathophysiological concepts and impact on management. Exp. Rev. Hematol. 2016, 9, 803–814. [Google Scholar] [CrossRef]
- Hayakawa, M.; Yamakawa, K.; Kudo, D.; Ono, K. Optimal antithrombin activity threshold for initiating antithrombin supplementation in patients with sepsis-induced disseminated intravascular coagulation: A multicenter retrospective observational study. Clin. Appl. Thromb. Hemost. 2018, 24, 874–883. [Google Scholar] [CrossRef]
- Opal, S.M.; Kessler, C.M.; Roemisch, J.; Knaub, S. Antithrombin, heparin, and heparan sulfate. Crit. Care Med. 2002, 30, S325–S331. [Google Scholar] [CrossRef] [PubMed]
- Aibiki, M.; Fukuoka, N.; Umakoshi, K.; Ohtsubo, S.; Kikuchi, S. Serum albumin levels anticipate antithrombin III activities before and after antithrombin III agent in critical patients with disseminated intravascular coagulation. Shock 2007, 27, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Seitz, R.; Wolf, M.; Egbring, R.; Havemann, K. The disturbance of hemostasis in septic shock: Role of neutrophil elastase and thrombin, effects of antithrombin III and plasma substitution. Eur. J. Haematol. 1989, 43, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Sie, P.; Letrenne, E.; Caranobe, C.; Genestal, M.; Cathala, B.; Boneu, B. Factor II related antigen and antithrombin III levels as indicators of liver failure in consumption coagulopathy. Thromb. Haemost. 1982, 47, 218–220. [Google Scholar]
- Asakura, H.; Takahashi, H.; Uchiyama, T.; Eguchi, Y.; Okamoto, K.; Kawasugi, K.; Madoiwa, S.; Wada, H.; DIC subcommittee of the Japanese Society on Thrombosis and Hemostasis. Proposal for new diagnostic criteria for DIC from the Japanese Society on Throm-bosis and Hemostasis. Thromb. J. 2016, 14, 42. [Google Scholar] [CrossRef] [Green Version]
- Vincent, J.L.; Francois, B.; Zabolotskikh, I.; Daga, M.K.; Lascarrou, J.B.; Kirov, M.Y.; Pettilä, V.; Wittebole, X.; Meziani, F.; Mercier, E.; et al. Effect of a recombinant human soluble thrombomodulin on mortality in patients with sepsis-associated coagulopathy. J. Am. Med. Assoc. 2019, 321, 1993–2002. [Google Scholar] [CrossRef] [Green Version]
- Van der Poll, T. Recombinant human soluble thrombomodulin in patients with sepsis-associated coagulopathy: Another negative sepsis trial? J. Am. Med. Assoc. 2019, 321, 1978–1980. [Google Scholar] [CrossRef]
- Yamakawa, K.; Umemura, Y.; Murao, S.; Hayakawia, M.; Fujimi, S. Optimal timing and early intervention with anticoagulant therapy for sepsis-induced disseminated intravascular coagulation. Clin. Appl. Thromb. Hemost. 2019, 25, 1076029619835055. [Google Scholar] [CrossRef] [Green Version]
- Hasegawa, D.; Nishida, O. Individualized recombinant human thrombomodulin (ART-123) administration in sepsis patients based on predicted phenotypes. Crit. Care 2019, 23, 231. [Google Scholar] [CrossRef] [Green Version]

| Patient Characteristics | |
| Age (years), mean (range) | 70.0 (60.0–79.0) |
| Sex, male, N/% | 601/59.1% |
| Weight (kg), mean (range) | 56.0 (48.5–65.4) |
| Pre-Existing Comorbidities | |
| Liver insufficiency, N/% | 49/4.82% |
| Chronic respiratory disorder, N/% | 38/3.74% |
| Chronic heart failure, N/% | 66/6.49% |
| Chronic kidney disease, N/% | 73/7.18% |
| Immunocompromised, N/% | 178/17.5% |
| Infection Site | |
| Catheter related, N/% | 16/1.57% |
| Bone/soft tissue, N/% | 158/15.5% |
| Infectious endocarditis, N/% | 25/2.46% |
| Central nervous system, N/% | 22/2.16% |
| Urinary tract, N/% | 128/12.6% |
| Lung, N/% | 230/22.6% |
| Abdomen, N/% | 364/35.8% |
| Others, N/% | 20/1.97% |
| Illness Severity Score on Day 1, Mean (Range) | |
| APACHE II score | 23.0 (17.0–29.0) |
| SIRS score | 3 (2–4) |
| SOFA score, lung | 2 (1–3) |
| SOFA score, kidney | 2 (0–3) |
| SOFA score, liver | 0 (0–1) |
| SOFA score, cardiovascular | 3 (1–4) |
| SOFA score, coagulopathy | 1 (0–2) |
| SOFA score, central nervous system | 1 (0–2) |
| ISTH overt DIC score | 4.0 (3.0–5.0) |
| Laboratory Data on Day 1, Mean (Range) | |
| White blood cell count (×103/μL) | 11.8 (4.70–19.3) |
| Platelet count (×104/μL) | 111 (56.0–180) |
| Hemoglobin (g/dL) | 10.5 (8.9–12.2) |
| PT ratio | 1.36 (1.20–1.62) |
| Fibrinogen (mg/dL) | 386 (263–544) |
| FDP (μg/mL) | 20.0 (11.0–40.0) |
| D-dimer (μg/mL) | 8.90 (4.30–20.80) |
| Lactate (mmol/L) | 2.80 (1.80–5.04) |
| Statistical Analysis | TP | FP | FN | TN | Accuracy |
|---|---|---|---|---|---|
| Logistic Regression | 44 | 33 | 78 | 151 | 63.7% |
| SVM | 40 | 34 | 82 | 150 | 64.4% |
| RF | 38 | 17 | 84 | 167 | 67.0% |
| NN | 46 | 47 | 76 | 137 | 59.8% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hasegawa, D.; Yamakawa, K.; Nishida, K.; Okada, N.; Murao, S.; Nishida, O. Comparative Analysis of Three Machine-Learning Techniques and Conventional Techniques for Predicting Sepsis-Induced Coagulopathy Progression. J. Clin. Med. 2020, 9, 2113. https://doi.org/10.3390/jcm9072113
Hasegawa D, Yamakawa K, Nishida K, Okada N, Murao S, Nishida O. Comparative Analysis of Three Machine-Learning Techniques and Conventional Techniques for Predicting Sepsis-Induced Coagulopathy Progression. Journal of Clinical Medicine. 2020; 9(7):2113. https://doi.org/10.3390/jcm9072113
Chicago/Turabian StyleHasegawa, Daisuke, Kazuma Yamakawa, Kazuki Nishida, Naoki Okada, Shuhei Murao, and Osamu Nishida. 2020. "Comparative Analysis of Three Machine-Learning Techniques and Conventional Techniques for Predicting Sepsis-Induced Coagulopathy Progression" Journal of Clinical Medicine 9, no. 7: 2113. https://doi.org/10.3390/jcm9072113






