Nafamostat Mesylate Improved Survival Outcomes of Sepsis Patients Who Underwent Blood Purification: A Nationwide Registry Study in Japan
Abstract
1. Introduction
2. Materials and Methods
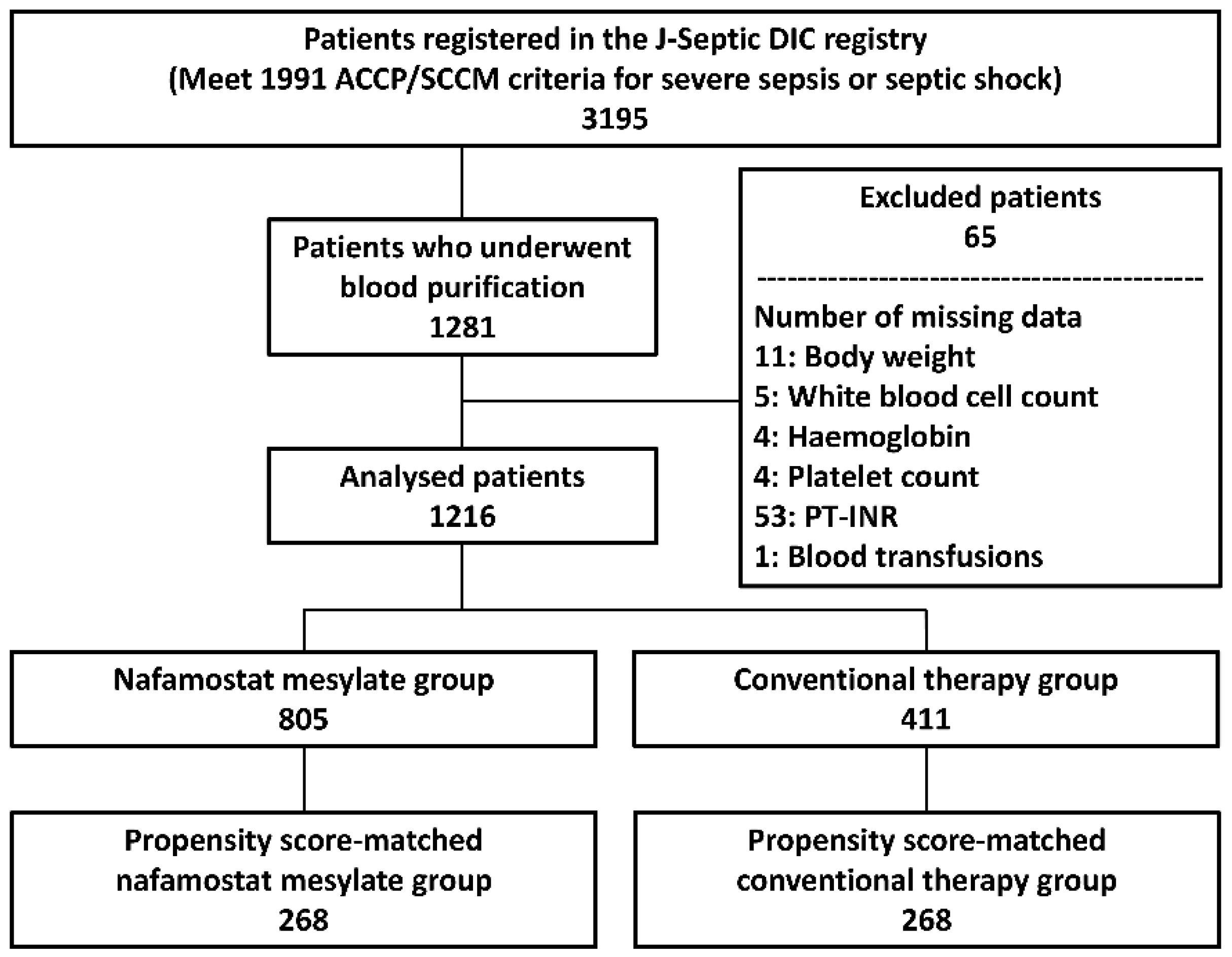
2.1. Study Design, Setting, and Population
2.2. Analyzed Data
2.3. Outcome Measures
2.4. Statistical Analysis
3. Results
3.1. ICU and Patient Characteristics
3.2. Comparing Propensity Score-Matched Nafamostat Mesylate and Conventional Therapy Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rudd, K.E.; Johnson, S.C.; Agesa, K.M.; Shackelford, K.A.; Tsoi, D.; Kievlan, D.R.; Colombara, D.V.; Ikuta, K.S.; Kissoon, N.; Finfer, S.; et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet 2020, 395, 200–211. [Google Scholar] [CrossRef]
- Bateman, R.M.; Sharpe, M.D.; Singer, M.; Ellis, C.G. The effect of sepsis on the erythrocyte. Int. J. Mol. Sci. 2017, 18, 1932. [Google Scholar] [CrossRef] [PubMed]
- Perner, A.; Gordon, A.C.; Angus, D.C.; Lamontagne, F.; Machado, F.; Russell, J.A.; Timsit, J.F.; Marshall, J.C.; Myburgh, J.; Shankar-Hari, M.; et al. The intensive care medicine research agenda on septic shock. Intensive Care Med. 2017, 43, 1294–1305. [Google Scholar] [CrossRef] [PubMed]
- Cecconi, M.; Evans, L.; Levy, M.; Rhodes, A. Sepsis and septic shock. Lancet 2018, 392, 75–87. [Google Scholar] [CrossRef]
- Putzu, A.; Schorer, R.; Lopez-Delgado, J.C.; Cassina, T.; Landoni, G. Blood purification and mortality in sepsis and septic shock: A systematic review and meta-analysis of randomized trials. Anesthesiology 2019, 131, 580–593. [Google Scholar] [CrossRef] [PubMed]
- Gando, S. Disseminated intravascular coagulation is a frequent complication of systemic inflammatory response syndrome. Thromb. Haemost. 1996, 75, 224–228. [Google Scholar] [CrossRef]
- Okamoto, K.; Tamura, T.; Sawatsubashi, Y. Sepsis and disseminated intravascular coagulation. J. Intensive Care 2016, 4, 23. [Google Scholar] [CrossRef]
- Levi, M.; Van Der Poll, T. Endothelial injury in sepsis. Intensive Care Med. 2013, 39, 1839–1842. [Google Scholar] [CrossRef]
- Yatabe, T.; Inoue, S.; Sakamoto, S.; Sumi, Y.; Nishida, O.; Hayashida, K.; Hara, Y.; Fukuda, T.; Matsushima, A.; Matsuda, A.; et al. The anticoagulant treatment for sepsis induced disseminated intravascular coagulation; network meta-analysis. Thromb. Res. 2018, 171, 136–142. [Google Scholar] [CrossRef]
- Umemura, Y.; Yamakawa, K.; Ogura, H.; Yuhara, H.; Fujimi, S. Efficacy and safety of anticoagulant therapy in three specific populations with sepsis: A meta-analysis of randomized controlled trials. J. Thromb. Haemost. 2016, 14, 518–530. [Google Scholar] [CrossRef]
- Polderman, K.H.; Girbes, A.R.J. Drug intervention trials in sepsis: Divergent results. Lancet 2004, 363, 1721–1723. [Google Scholar] [CrossRef]
- Uchino, S.; Bellomo, R.; Morimatsu, H.; Morgera, S.; Schetz, M.; Tan, I.; Bouman, C.; Macedo, E.; Gibney, N.; Tolwani, A.; et al. Continuous renal replacement therapy: A worldwide practice survey: The Beginning and Ending Supportive Therapy for the Kidney (B.E.S.T. Kidney) Investigators. Intensive Care Med. 2007, 33, 1563–1570. [Google Scholar] [CrossRef] [PubMed]
- Arimura, T.; Abe, M.; Shiga, H.; Katayama, H.; Kaizu, K.; Oda, S. Clinical study of blood purification therapy in critical care in Japan: Results from the survey research of the Japan Society for Blood Purification in Critical Care in 2013. J. Artif. Organs 2017, 20, 244–251. [Google Scholar] [CrossRef]
- Suzuki, K.; Wada, H.; Matsumoto, T.; Ikejiri, M.; Ohishi, K.; Yamashita, Y.; Imai, H.; Iba, T.; Katayama, N. Usefulness of the APTT waveform for the diagnosis of DIC and prediction of the outcome or bleeding risk. Thromb. J. 2019, 17, 12. [Google Scholar] [CrossRef] [PubMed]
- Doi, K.; Ikeda, M.; Hayase, N.; Moriya, K.; Morimura, N.; COVID-UTH Study Group. Nafamostat mesylate treatment in combination with favipiravir for patients critically ill with Covid-19: A case series. Crit. Care 2020, 24, 392. [Google Scholar] [CrossRef] [PubMed]
- Sadahiro, T.; Yuzawa, H.; Kimura, T.; Oguchi, M.; Morito, T.; Mizushima, S.; Hirose, Y. Current practices in acute blood purification therapy in Japan and topics for further study. Contrib. Nephrol. 2018, 196, 209–214. [Google Scholar]
- Makino, S.; Egi, M.; Kita, H.; Miyatake, Y.; Kubota, K.; Mizobuchi, S. Comparison of nafamostat mesilate and unfractionated heparin as anticoagulants during continuous renal replacement therapy. Int. J. Artif. Organs 2016, 39, 16–21. [Google Scholar] [CrossRef]
- Lee, Y.K.; Lee, H.W.; Choi, K.H.; Kim, B.S. Ability of nafamostat mesilate to prolong filter patency during continuous renal replacement therapy in patients at high risk of bleeding: A randomized controlled study. PLoS ONE 2014, 9, e108737. [Google Scholar] [CrossRef]
- Hayakawa, M.; Yamakawa, K.; Saito, S.; Uchino, S.; Kudo, D.; Iizuka, Y.; Sanui, M.; Takimoto, K.; Mayumi, T. Data descriptor: Nationwide registry of sepsis patients in Japan focused on disseminated intravascular coagulation 2011–2013. Sci. Data 2018, 5, 1–6. [Google Scholar] [CrossRef]
- Bone, R.C.; Balk, R.A.; Cerra, F.B.; Dellinger, R.P.; Fein, A.M.; Knaus, W.A.; Schein, R.M.H.; Sibbald, W.J. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 1992, 101, 1644–1655. [Google Scholar] [CrossRef]
- Austin, P.C. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun. Stat. Simul. Comput. 2009, 38, 1228–1234. [Google Scholar] [CrossRef]
- Choi, J.Y.; Kang, Y.J.; Jang, H.M.; Jung, H.Y.; Cho, J.H.; Park, S.H.; Kim, Y.L.; Kim, C.D. Nafamostat mesilate as an anticoagulant during continuous renal replacement therapy in patients with high bleeding risk a randomized clinical trial. Medicine 2015, 94, e2392. [Google Scholar] [PubMed]
- Hoffmann, J.N.; Vollmar, B.; Laschke, M.W.; Inthorn, D.; Kaneider, N.C.; Dunzendorfer, S.; Wiedermann, C.J.; Römisch, J.; Schildberg, F.W.; Menger, M.D. Adverse effect of heparin on antithrombin action during endotoxemia: Microhemodynamic and cellular mechanisms. Thromb. Haemost. 2002, 88, 242–252. [Google Scholar] [PubMed]
- Kang, Y.; Moon, S.J.; Kang, H. The effects of nafamostat mesilate on a bleeding risk as an anticoagulant during use as a continuous renal replacement therapy: Systematic review. J. Health Tech. Assess. 2018, 6, 133–141. [Google Scholar]
- Aoyama, T.; Ino, Y.; Ozeki, M.; Oda, M.; Sato, T.; Koshiyama, Y.; Suzuki, S.; Fujita, M. Pharmacological studies of FUT-175, nafamstat mesilate, I. Inhibition of protease activity in in vitro and in vivo experiments. Jpn. J. Pharm. 1984, 35, 203–227. [Google Scholar]
- Asakura, H. Classifying types of disseminated intravascular coagulation: Clinical and animal models. J. Intensive Care 2014, 2, 20. [Google Scholar] [CrossRef]
- Tsujimoto, H.; Tsujimoto, Y.; Nakata, Y.; Fujii, T.; Takahashi, S.; Akazawa, M.; Kataoka, Y. Pharmacological interventions for preventing clotting of extracorporeal circuits during continuous renal replacement therapy. Cochrane Database Syst. Rev. 2020, 3, CD012467. [Google Scholar] [CrossRef]
- Mochizuki, K.; Mori, K.; Kamijo, H.; Ichikawa, M.; Nitta, K.; Imamura, H. Beneficial effect modification on survival outcome of sepsis between ART-123 and polymyxin B-immobilised haemoperfusion: A nationwide Japanese registry study. Ann. Intensive Care 2020, 10, 57. [Google Scholar] [CrossRef]
- Lee, B.K.; Lessler, J.; Stuart, E.A. Improving propensity score weighting using machine learning. Stat. Med. 2010, 29, 337–346. [Google Scholar]
- Singer, M.; Deutschman, C.S.; Seymour, C.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Nakamura, Y.; Hara, S.; Hatomoto, H.; Yamasaki, S.; Nakano, T.; Miyazaki, M.; Matsumoto, N.; Irie, Y.; Ishikura, H. Adsorption Of nafamostat mesilate on AN69ST membranes: A single-center retrospective and in vitro study. Ther. Apher Dial. 2017, 21, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Hirayama, T.; Nosaka, N.; Okawa, Y.; Ushio, S.; Kitamura, Y.; Sendo, T.; Ugawa, T.; Nakao, A. AN69ST membranes adsorb nafamostat mesylate and affect the management of anticoagulant therapy: A retrospective study. J. Intensive Care 2017, 5, 46. [Google Scholar] [CrossRef] [PubMed]
- Sergi, C.; Shen, F.; Lim, D.W.; Liu, W.; Zhang, M.; Chiu, B.; Anand, V.; Sun, Z. Cardiovascular dysfunction in sepsis at the dawn of emerging mediators. Biomed. Pharm. 2017, 95, 153–160. [Google Scholar] [CrossRef] [PubMed]

| Overall (n = 1216) | Nafamostat Mesylate (n = 805) | Conventional Therapy (n = 411) | Standardized Difference | |
|---|---|---|---|---|
| Characteristics of ICU | 0.113 | |||
| General ICU, n (%) | 698 (57.4) | 447 (55.5) | 251 (61.1) | |
| Emergency ICU, n (%) | 518 (42.6) | 358 (44.5) | 160 (38.9) | |
| Management Policy of the ICU | 0.474 | |||
| Closed Policy, n (%) | 605 (49.8) | 447 (55.5) | 158 (38.4) | |
| Open Policy, n (%) | 381 (31.3) | 255 (31.7) | 126 (30.7) | |
| Other, n (%) | 230 (18.9) | 103 (12.8) | 127 (30.9) | |
| Number of Beds in the ICU | 12 (8, 16) | 12 (8, 14) | 11 (7, 18) | 0.045 |
| Admission Route to the ICU | 0.067 | |||
| Emergency Department, n (%) | 465 (38.2) | 299 (37.1) | 166 (40.4) | |
| Other Hospital, n (%) | 315 (25.9) | 213 (26.5) | 102 (24.8) | |
| Ward, n (%) | 436 (35.9) | 293 (36.4) | 143 (34.8) | |
| Age, (Years) | 70 (61, 78) | 70 (62, 78) | 70 (60, 79) | 0.066 |
| Male Sex, n (%) | 750 (61.7) | 510 (63.4) | 240 (58.4) | 0.102 |
| Body Weight, (Kg) | 56.1 (48.0, 65.4) | 56.3 (48.0, 66.0) | 56.1 (48.0, 65.0) | 0.064 |
| Pre-Existing Organ Insufficiency or Immunosuppression Based on APACHE II Score | ||||
| Liver, n (%) | 69 (5.7) | 47 (5.8) | 22 (5.4) | 0.021 |
| Respiratory, n (%) | 33 (2.7) | 19 (2.4) | 14 (3.4) | 0.063 |
| Cardiovascular, n (%) | 76 (6.3) | 52 (6.5) | 24 (5.8) | 0.026 |
| Renal, n (%) | 194 (16.0) | 141 (17.5) | 53 (12.9) | 0.129 |
| Immunocompromised, n (%) | 209 (17.2) | 138 (17.1) | 71 (17.3) | 0.003 |
| Pre-Existing Hemostatic Disorder | ||||
| Cirrhosis, n (%) | 60 (4.9) | 39 (4.8) | 21 (5.1) | 0.012 |
| Hematologic Malignancy, n (%) | 40 (3.3) | 29 (3.6) | 11 (2.7) | 0.053 |
| Chemotherapy, n (%) | 63 (5.2) | 44 (5.5) | 19 (4.6) | 0.039 |
| Warfarin Intake, n (%) | 68 (5.6) | 40 (5.0) | 28 (6.8) | 0.078 |
| Other, n (%) | 31 (2.5) | 15 (1.9) | 16 (3.9) | 0.122 |
| APACHE II Score | 25 (19, 31) | 27 (21, 32) | 22 (17, 28) | 0.352 |
| SOFA Score | 12 (9, 14) | 12 (9, 14) | 11 (8, 13) | 0.318 |
| SIRS Score | 3 (2, 4) | 3 (2, 4) | 3 (3, 4) | 0.115 |
| White Blood Cell Count, ×103 | 10.3 (3.5, 17.7) | 10.1 (3.6, 17.1) | 11.3 (3.4, 19.2) | 0.072 |
| Hemoglobin, G/Dl | 10.3 (8.7, 12.2) | 10.4 (8.7, 12.2) | 10.3 (8.7, 12.2) | 0.032 |
| Platelet Count, ×103 | 103 (54, 170) | 100 (53, 165) | 111 (59, 178) | 0.110 |
| Prothrombin Time International Normalized Ratio | 1.42 (1.22, 1.76) | 1.41 (1.22, 1.76) | 1.42 (1.22, 1.73) | 0.027 |
| Blood Culture | 0.141 | |||
| Not Taken, n (%) | 61 (5.0) | 34 (4.2) | 27 (6.6) | |
| Positive, n (%) | 558 (45.9) | 385 (47.8) | 173 (42.1) | |
| Negative, n (%) | 597 (49.1) | 386 (48.0) | 211 (51.3) | |
| Microorganisms | 0.168 | |||
| Unknown, n (%) | 267 (22.0) | 169 (21.0) | 98 (23.8) | |
| Virus, n (%) | 8 (0.7) | 6 (0.7) | 2 (0.5) | |
| Gram-Negative Rod, n (%) | 436 (35.9) | 291 (36.1) | 145 (35.3) | |
| Gram-Positive Coccus, n (%) | 286 (23.5) | 202 (25.1) | 84 (20.4) | |
| Fungus, n (%) | 18 (1.5) | 12 (1.5) | 6 (1.5) | |
| Mixed Infection, n (%) | 183 (15.0) | 117 (14.5) | 66 (16.1) | |
| Other, n (%) | 18 (1.5) | 8 (1.0) | 10 (2.4) | |
| Primary Source of Infection | 0.218 | |||
| Unknown, n (%) | 87 (7.2) | 55 (6.8) | 32 (7.8) | |
| Catheter-Related Bloodstream Infection, n (%) | 17 (1.4) | 13 (1.6) | 4 (1.0) | |
| Bone, Soft Tissue, n (%) | 138 (11.3) | 97 (12.0) | 41 (10.0) | |
| Cardiovascular System, n (%) | 29 (2.4) | 22 (2.7) | 7 (1.7) | |
| Central Nervous System, n (%) | 15 (1.2) | 14 (1.7) | 1 (0.2) | |
| Urinary Tract, n (%) | 138 (11.3) | 94 (11.7) | 44 (10.7) | |
| Lung, Thoracic Cavity, n (%) | 239 (19.7) | 161 (20.0) | 78 (19.0) | |
| Abdomen, n (%) | 530 (43.6) | 333 (41.4) | 197 (47.9) | |
| Other, n (%) | 23 (1.9) | 16 (2.0) | 7 (1.7) | |
| Specific Treatment | ||||
| Surgical Intervention, n (%) | 640 (52.6) | 410 (50.9) | 230 (56.0) | 0.101 |
| Mechanical Ventilator, n (%) | 1038 (85.4) | 696 (86.5) | 342 (83.2) | 0.091 |
| Vasopressor, n (%) | 1109 (91.2) | 743 (92.3) | 366 (89.1) | 0.112 |
| Immunoglobulins, n (%) | 505 (41.5) | 376 (46.7) | 129 (31.4) | 0.318 |
| Low-Dose Steroids, n (%) | 447 (36.8) | 315 (39.1) | 132 (32.1) | 0.147 |
| Veno-Arterial ECMO, n (%) | 17 (1.4) | 9 (1.1) | 8 (1.9) | 0.067 |
| Veno-Venous ECMO, n (%) | 30 (2.5) | 21 (2.6) | 9 (2.2) | 0.027 |
| Intra-Aortic Balloon Pumping, n (%) | 9 (0.7) | 4 (0.5) | 5 (1.2) | 0.078 |
| Red Blood Cell Transfusion, Units | 3 (0, 6) | 4 (0, 6) | 2 (0, 6) | 0.167 |
| Fresh Frozen Plasma Transfusion, Units | 0 (0, 10) | 0 (0, 10) | 0 (0, 8) | 0.073 |
| Platelet Concentration Transfusion, Units | 0 (0, 20) | 0 (0, 20) | 0 (0, 15) | 0.193 |
| Therapeutic Interventions For DIC | ||||
| Antithrombin, n (%) | 560 (46.1) | 386 (48.0) | 174 (42.3) | 0.113 |
| Thrombomodulin Alpha, n (%) | 484 (39.8) | 361 (44.8) | 123 (29.9) | 0.312 |
| Protease Inhibitors, n (%) | 214 (17.6) | 125 (15.5) | 89 (21.7) | 0.158 |
| Heparinoids, n (%) | 70 (5.8) | 48 (6.0) | 22 (5.4) | 0.026 |
| Anti-Thrombotic Drugs for Other Than DIC | ||||
| Heparin, n (%) | 175 (14.4) | 74 (9.2) | 101 (14.4) | 0.420 |
| Warfarin, n (%) | 13 (1.1) | 6 (0.7) | 7 (1.7) | 0.087 |
| Anti-Platelet Drugs, n (%) | 26 (2.1) | 4 (0.5) | 22 (5.4) | 0.291 |
| Other, n (%) | 8 (0.7) | 4 (0.5) | 4 (1.0) | 0.056 |
| Blood Purification Treatments | ||||
| RRT, n (%) | 842 (69.2) | 640 (79.5) | 202 (49.1) | 0.668 |
| RRT For Non-Renal Indications, n (%) | 254 (20.9) | 180 (22.4) | 74 (18.0) | 0.109 |
| PMX-HP, n (%) | 663 (54.5) | 425 (52.8) | 238 (57.9) | 0.103 |
| Plasma Exchange, n (%) | 28 (2.3) | 15 (1.9) | 13 (3.2) | 0.083 |
| Concomitant Treatment with Thrombomodulin Alpha And PMX-HP, n (%) | 285 (23.4) | 216 (26.8) | 69 (16.8) | 0.245 |
| Nafamostat Mesylate (n = 268) | Conventional Therapy (n = 268) | Standardized Difference | |
|---|---|---|---|
| Characteristics of the ICU | 0.008 | ||
| General ICU, n (%) | 166 (61.9) | 165 (61.6) | |
| Emergency ICU, n (%) | 102 (38.1) | 103 (38.4) | |
| Management Policy of the ICU | 0.037 | ||
| Closed Policy, n (%) | 116 (43.3) | 115 (42.9) | |
| Open Policy, n (%) | 90 (33.6) | 87 (32.5) | |
| Other, n (%) | 62 (23.1) | 66 (24.6) | |
| Number of Beds in the ICU | 12 (8, 16) | 12 (7, 18) | 0.068 |
| Admission Route to the ICU | 0.083 | ||
| Emergency Department, n (%) | 120 (44.8) | 109 (40.7) | |
| Other Hospital, n (%) | 64 (23.9) | 68 (25.4) | |
| Ward, n (%) | 84 (31.3) | 91 (34.0) | |
| Age, (Years) | 70 (61, 78) | 71 (61, 78) | 0.003 |
| Male Sex, n (%) | 174 (64.9) | 165 (61.6) | 0.070 |
| Body Weight, (Kg) | 57.6 (49.8, 67.0) | 55.5 (47.9, 65.0) | 0.070 |
| Pre-Existing Organ Insufficiency or Immunosuppression Based on APACHE II Score | |||
| Liver, n (%) | 15 (5.6) | 12 (4.5) | 0.051 |
| Respiratory, n (%) | 8 (3.0) | 8 (3.0) | 0 |
| Cardiovascular, n (%) | 14 (5.2) | 16 (6.0) | 0.032 |
| Renal, n (%) | 38 (14.2) | 39 (14.6) | 0.011 |
| Immunocompromised, n (%) | 36 (13.4) | 38 (14.2) | 0.022 |
| Pre-Existing Hemostatic Disorder | |||
| Cirrhosis, n (%) | 14 (5.2) | 9 (3.4) | 0.092 |
| Hematologic Malignancy, n (%) | 7 (2.6) | 7 (2.6) | 0 |
| Chemotherapy, n (%) | 13 (4.9) | 12 (4.5) | 0.018 |
| Warfarin Intake, n (%) | 12 (4.5) | 13 (4.9) | 0.018 |
| Other, n (%) | 6 (2.2) | 7 (2.6) | 0.024 |
| APACHE II Score | 25 (18, 30) | 23 (17, 29) | 0.015 |
| SOFA Score | 11 (8, 13) | 11 (8, 13) | 0.011 |
| SIRS Score | 3 (2, 4) | 3 (3, 4) | 0.083 |
| White Blood Cell Count, ×103 | 11.2 (3.4, 18.2) | 12.0 (4.5, 19.5) | 0.090 |
| Hemoglobin, G/Dl | 10.6 (8.9, 12.6) | 10.5 (8.8, 12.5) | 0.002 |
| Platelet Count, ×103 | 118 (65, 175) | 109 (57, 186) | 0.009 |
| Prothrombin Time International Normalize Ratio | 1.40 (1.21, 1.73) | 1.38 (1.20, 1.70) | 0.013 |
| Blood Culture | 0.023 | ||
| Not Taken, n (%) | 14 (5.2) | 14 (5.2) | |
| Positive, n (%) | 114 (42.5) | 117 (43.7) | |
| Negative, n (%) | 140 (52.2) | 137 (51.1) | |
| Microorganisms | 0.090 | ||
| Unknown, n (%) | 66 (24.6) | 62 (23.1) | |
| Virus, n (%) | 0 (0) | 0 (0) | |
| Gram-Negative Rod, n (%) | 106 (39.6) | 101 (37.7) | |
| Gram-Positive Coccus, n (%) | 56 (20.9) | 57 (21.3) | |
| Fungus, n (%) | 3 (1.1) | 4 (1.5) | |
| Mixed Infection, n (%) | 32 (11.9) | 39 (14.6) | |
| Other, n (%) | 5 (1.9) | 5 (1.9) | |
| Primary Source of Infection | 0.087 | ||
| Unknown, n (%) | 24 (9.0) | 24 (9.0) | |
| Catheter-Related Bloodstream Infection, n (%) | 2 (0.7) | 2 (0.7) | |
| Bone, Soft Tissue, n (%) | 29 (10.8) | 28 (10.4) | |
| Cardiovascular System, n (%) | 4 (1.5) | 6 (2.2) | |
| Central Nervous System, n (%) | 1 (0.4) | 1 (0.4) | |
| Urinary Tract, n (%) | 31 (11.6) | 26 (9.7) | |
| Lung, Thoracic Cavity, n (%) | 46 (17.2) | 50 (18.7) | |
| Abdomen, n (%) | 126 (47.0) | 126 (47.0) | |
| Other, n (%) | 5 (1.9) | 5 (1.9) | |
| Specific Treatment | |||
| Surgical Intervention, n (%) | 146 (54.5) | 151 (56.3) | 0.038 |
| Mechanical Ventilator, n (%) | 224 (83.6) | 221 (82.5) | 0.030 |
| Vasopressor, n (%) | 240 (89.6) | 247 (92.2) | 0.091 |
| Immunoglobulins, n (%) | 97 (36.2) | 96 (35.8) | 0.008 |
| Low-Dose Steroids, n (%) | 84 (31.3) | 86 (32.1) | 0.016 |
| Veno-Arterial ECMO, n (%) | 3 (1.1) | 3 (1.1) | 0 |
| Veno-Venous ECMO, n (%) | 5 (1.9) | 6 (2.2) | 0.026 |
| Intra-Aortic Balloon Pumping, n (%) | 2 (0.7) | 1 (0.4) | 0.050 |
| Red Blood Cell Transfusion, Units | 2 (0, 6) | 2 (0, 6) | 0.008 |
| Fresh Frozen Plasma Transfusion, Units | 0 (0, 10) | 0 (0, 8) | 0.014 |
| Platelet Concentration Transfusion, Units | 0 (0, 10) | 0 (0, 15) | 0.053 |
| Therapeutic Interventions For DIC | |||
| Antithrombin, n (%) | 119 (44.4) | 116 (43.3) | 0.023 |
| Thrombomodulin Alpha, n (%) | 99 (36.9) | 90 (33.6) | 0.070 |
| Protease Inhibitors, n (%) | 45 (16.8) | 49 (18.3) | 0.039 |
| Heparinoids, n (%) | 17 (6.3) | 14 (5.2) | 0.048 |
| Anti-Thrombotic Drugs for Other Than DIC | |||
| Heparin, n (%) | 51 (19.0) | 55 (20.5) | 0.037 |
| Warfarin, n (%) | 2 (0.7) | 3 (1.1) | 0.039 |
| Anti-Platelet Drugs, n (%) | 4 (1.5) | 3 (1.1) | 0.033 |
| Other, n (%) | 4 (1.5) | 2 (0.7) | 0.071 |
| Blood Purification Treatments | |||
| RRT, n (%) | 154 (57.5) | 149 (55.6) | 0.038 |
| RRT For Non-Renal Indications, n (%) | 54 (20.1) | 54 (20.1) | 0 |
| PMX-HP, n (%) | 143 (53.4) | 152 (56.7) | 0.068 |
| Plasma Exchange, n (%) | 8 (3.0) | 5 (1.9) | 0.073 |
| Concomitant Treatment with Thrombomodulin Alpha And PMX-HP, n (%) | 59 (22.0) | 55 (20.5) | 0.036 |
| Unmatched | Matched | |||||
|---|---|---|---|---|---|---|
| Nafamostat Mesylate (n = 805) | Conventional Therapy (n = 411) | p-Value | Nafamostat Mesylate (n = 268) | Conventional Therapy (n = 268) | p-Value | |
| Hospital Mortality, n (%) | 343 (42.6) | 158 (38.4) | 0.163 | 79 (29.5) | 108 (40.3) | 0.009 |
| ICU Mortality, n (%) | 226 (28.1) | 95 (23.1) | 0.063 | 49 (18.3) | 72 (26.9) | 0.017 |
| Bleeding Complications, n (%) | 129 (16.0) | 69 (16.8) | 0.733 | 43 (16.0) | 50 (18.7) | 0.425 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamijo, H.; Mochizuki, K.; Nakamura, Y.; Mori, K.; Ichikawa, M.; Nitta, K.; Imamura, H. Nafamostat Mesylate Improved Survival Outcomes of Sepsis Patients Who Underwent Blood Purification: A Nationwide Registry Study in Japan. J. Clin. Med. 2020, 9, 2629. https://doi.org/10.3390/jcm9082629
Kamijo H, Mochizuki K, Nakamura Y, Mori K, Ichikawa M, Nitta K, Imamura H. Nafamostat Mesylate Improved Survival Outcomes of Sepsis Patients Who Underwent Blood Purification: A Nationwide Registry Study in Japan. Journal of Clinical Medicine. 2020; 9(8):2629. https://doi.org/10.3390/jcm9082629
Chicago/Turabian StyleKamijo, Hiroshi, Katsunori Mochizuki, Yuta Nakamura, Kotaro Mori, Michitaro Ichikawa, Kenichi Nitta, and Hiroshi Imamura. 2020. "Nafamostat Mesylate Improved Survival Outcomes of Sepsis Patients Who Underwent Blood Purification: A Nationwide Registry Study in Japan" Journal of Clinical Medicine 9, no. 8: 2629. https://doi.org/10.3390/jcm9082629
APA StyleKamijo, H., Mochizuki, K., Nakamura, Y., Mori, K., Ichikawa, M., Nitta, K., & Imamura, H. (2020). Nafamostat Mesylate Improved Survival Outcomes of Sepsis Patients Who Underwent Blood Purification: A Nationwide Registry Study in Japan. Journal of Clinical Medicine, 9(8), 2629. https://doi.org/10.3390/jcm9082629





