Airway Proficiency and Efficiency Amongst Anesthesia Providers and Respiratory Therapists: A Comparison Study
Abstract
1. Introduction
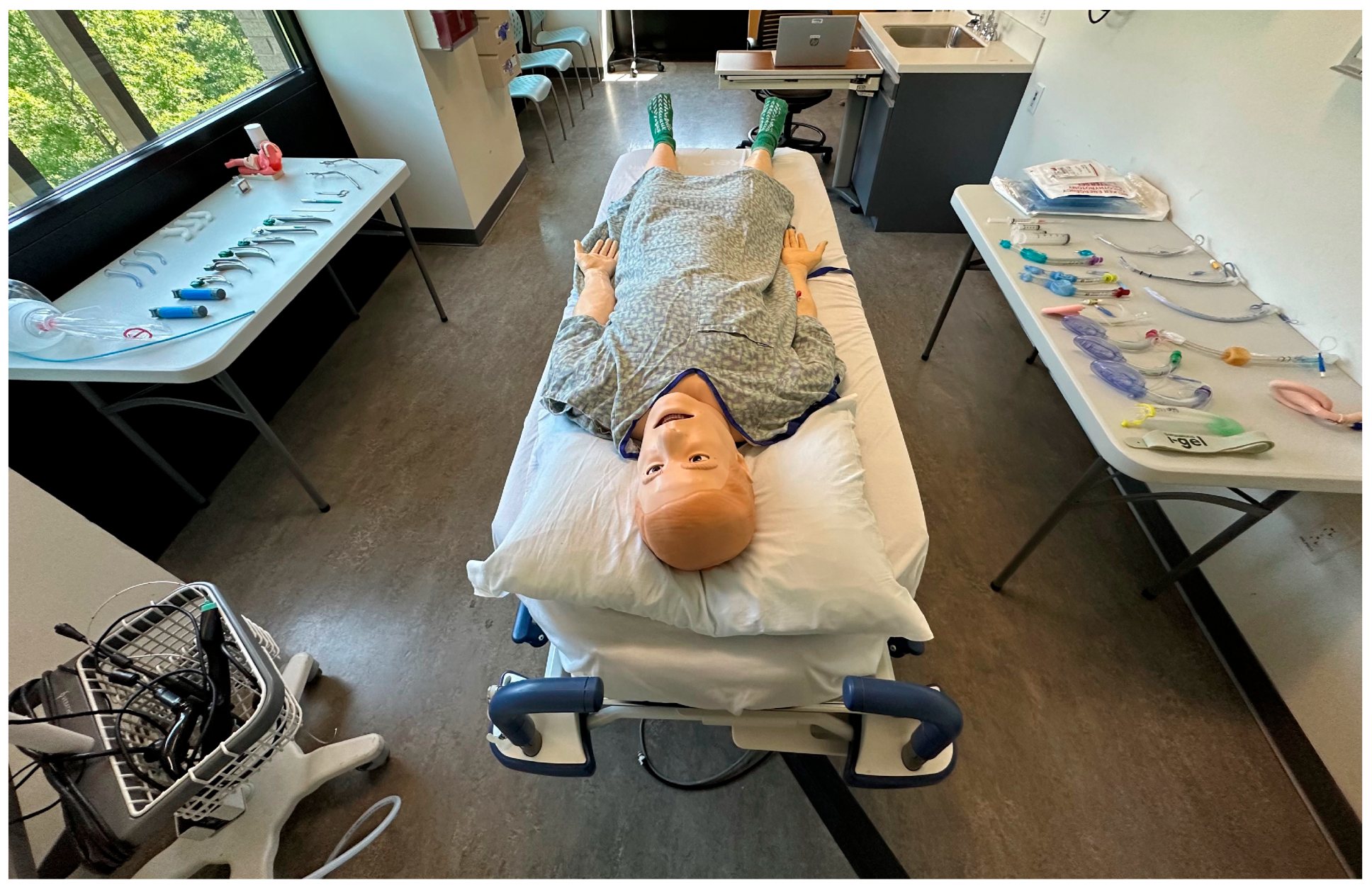
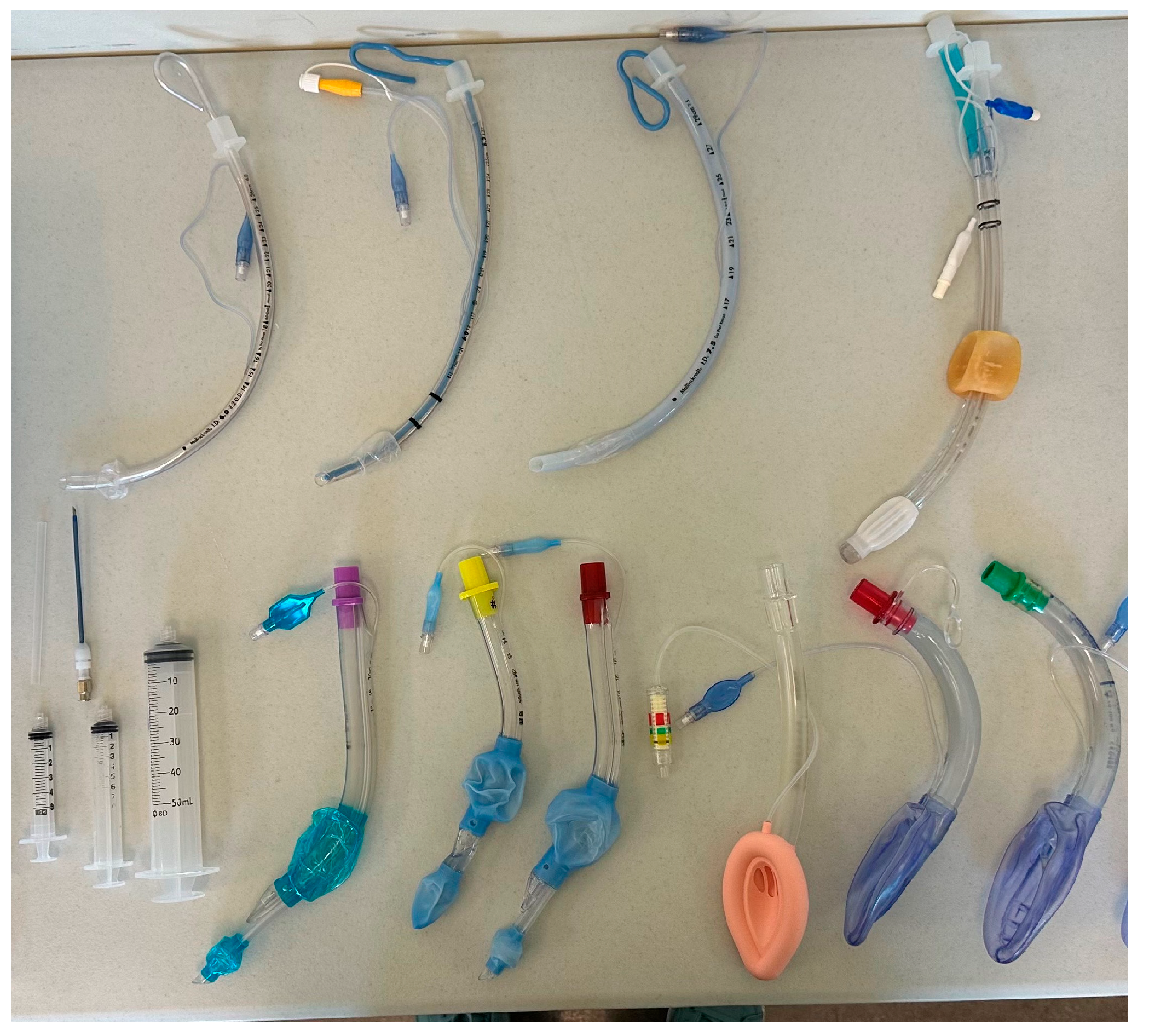
2. Materials and Methods
2.1. Study Population
2.2. Study Design
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CRNAs | Certified Registered Nurse Anesthetists |
| Aas | Anesthesiology Assistants |
| DAA | Difficult Airway Algorithm |
| DL | Direct Laryngoscopy |
| LMA | Laryngeal Mask Airway |
| VL | Video Laryngoscopy |
| ROM | Range of Motion |
References
- Kennedy, C.C.; Cannon, E.K.; Warner, D.O.; Cook, D.A. Advanced airway management simulation training in medical education. Crit. Care Med. 2014, 42, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.D.; Mhyre, J.M.; Shanks, A.M.; Tremper, K.K.; Kheterpal, S. 3423 emergency tracheal intubations at a university hospital: Airway outcomes and complications. Anesthesiology 2011, 114, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Brindley, P.G.; Beed, M.; Law, J.A.; Hung, O.; Levitan, R.; Murphy, M.F.; Duggan, L.V. Airway management outside the operating room: How to better prepare. Can. J. Anesth. 2017, 64, 530–539. [Google Scholar] [CrossRef] [PubMed]
- Royal College of Anaesthetists. 4th National Audit Project (NAP 4) of the Royal College of Anaesthetists and the Difficult Airway Society: Major Complications of Airway Management in the UK. Available online: www.rcoa.ac.uk/nap4 (accessed on 2 July 2025).
- Walz, J.M.; Zayaruzny, M.; Heard, S.O. Airway management in critical illness. Chest 2007, 131, 608–620. [Google Scholar] [CrossRef] [PubMed]
- Cook, T.; Behringer, E.C.; Benger, J. Airway management outside the operating room: Hazardous and incompletely studied. Curr. Opin. Anaesthesiol. 2012, 25, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Mort, T.C. Emergency tracheal intubation: Complications associated with repeated laryngoscopic attempts. Anesth. Analg. 2004, 99, 607–613. [Google Scholar] [CrossRef] [PubMed]
- Mort, T.C. Complications of emergency tracheal intubation: Hemodynamic alterations—Part I. J. Intensive Care Med. 2007, 22, 157–165. [Google Scholar] [CrossRef]
- Collins, S.; Coughlin, M.; Daniero, J. Who Should Manage a Patient’s Airway? AMA J. Ethics 2020, 22, 276–282. [Google Scholar] [CrossRef]
- Straker, T. Airway Management: Isn’t that what anesthesiologists do. J. Head Neck Anesth. 2019, 3, 11. [Google Scholar] [CrossRef]
- Baraka, A.; Salem, M.R.; Joseph, N.J. The origin of the “algorithm”. Anesthesiology 1998, 89, 277. [Google Scholar] [CrossRef] [PubMed]
- Practice guidelines for management of the difficult airway. A report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 1993, 78, 597–602. [Google Scholar] [CrossRef]
- Jung, H. A comprehensive review of difficult airway management strategies for patient safety. Anesth. Pain Med. 2023, 18, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Joffe, A.M.; Aziz, M.F.; Posner, K.L.; Duggan, L.V.; Mincer, S.L.; Domino, K.B. Management of difficult tracheal intubation: A closed claims analysis. Anesthesiology 2019, 131, 818–829. [Google Scholar] [CrossRef]
- Sakles, J.C.; Chiu, S.; Mosier, J.; Walker, C.; Stolz, U. The Importance of First Pass Success When Performing Orotracheal Intubation in the Emergency Department. Acad. Emerg. Med. 2013, 20, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- Accreditation Council for Graduate Medical Education (ACGME). Defined Category Minimums: Surgical Critical Care Review Committee for Surgery. 2024. Available online: https://www.acgme.org/globalassets/defined_category_minimum_numbers_surgical_critical_care.pdf (accessed on 2 July 2025).
- Panchal, A.R.; Way, D.P.; King, A.M.; Yudkowsky, R.; Terndrup, T.E.; Airway Mastery Collaborative (AMC). Performance Standards of Comprehensive Airway Management for Emergency Medicine Residents. AEM Educ. Train. 2018, 3, 39–49. [Google Scholar] [CrossRef] [PubMed]


| Task | Anesthesia Providers (n = 30) Median Time to Complete (Range) (Seconds) | Respiratory Therapists (n = 32) Median Time to Complete (Range) (Seconds) | p-Value | 95% CI |
|---|---|---|---|---|
| Direct Laryngoscopy, Healthy Patient | 21.4 (12.0–86.1) | 23.2 (13.6–90.4) | 0.1999 | [−6.12, 1.33] |
| Video Laryngoscopy, Healthy Patient | 23.0 (13.4–109.0) | 26.0 (14.4–218.0) | 0.2598 | [−6.68, 2.16] |
| LMA Placement, Healthy Patient | 14.2 (5.6–111.0) | 17.0 (8.8–99.2) | 0.0807 | [−6.47, 0.48] |
| Direct Laryngoscopy, Limited Cervical ROM | 30.9 (16.3–165.0) | 31.1 (17.0–139.0) | 0.8512 | [−6.51, 9.47] |
| Video Laryngoscopy, Pharyngeal Obstruction | 23.7 (9.3–74.2) | 43.3 (17.8–120.0) | 0.0004 | [−27.30, −5.90] |
| LMA Placement, Full Tongue Edema | 15.4 (6.3–47.5) | 16.1 (8.8–274.0) | 0.2628 | [−5.97, 1.91] |
| Task | Anesthesia Providers (n = 30) Number of Attempts Required (%) | Respiratory Therapists (n = 32) Number of Attempts Required (%) | p-Value | 95% CI |
|---|---|---|---|---|
| Direct Laryngoscopy, Healthy Patient | 1 attempt = 29 (96.7%) 2+ attempts = 1 (3.3%) | 1 attempt = 31 (96.9%) 2+ attempts = 1 (3.1%) | 1 | [0.01, 75.89] |
| Video Laryngoscopy, Healthy Patient | 1 attempt = 28 (93.3%) 2+ attempts = 2 (6.7%) | 1 attempt = 28 (87.5%) 2+ attempts = 4 (12.5%) | 0.6724 | [0.26, 23.54] |
| LMA Placement, Healthy Patient | 1 attempt = 28 (93.3%) 2+ attempts = 2 (6.7%) | 1 attempt = 30 (93.8%) 2+ attempts = 2 (6.2%) | 1 | [0.06, 13.70] |
| Direct Laryngoscopy, Limited Cervical ROM | 1 attempt = 28 (93.3%) 2+ attempts = 2 (6.7%) | 1 attempt = 27 (84.4%) 2+ attempts = 5 (15.6%) | 0.4267 | [0.38, 29.00] |
| Video Laryngoscopy, Pharyngeal Obstruction | 1 attempt = 29 (96.7%) 2+ attempts = 1 (3.3%) | 1 attempt = 25 (78.1%) 2+ attempts = 7 (21.9%) | 0.0540 | [0.91, 377.55] |
| LMA Placement, Full Tongue Edema | 1 attempt = 28 (93.3%) 2+ attempts = 2 (6.7%) | 1 attempt = 30 (93.8%) 2+ attempts = 2 (6.2%) | 1 | [0.06, 13.70] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brignull, C.G.; Williams, E.B.; Sprouse, H.A.; Adams, K.J.; Tanner, S.L.; Sykes, J.W.; Moulder, H.; Hand, W.R.; Morgan, R.R., Jr. Airway Proficiency and Efficiency Amongst Anesthesia Providers and Respiratory Therapists: A Comparison Study. J. Clin. Med. 2025, 14, 8059. https://doi.org/10.3390/jcm14228059
Brignull CG, Williams EB, Sprouse HA, Adams KJ, Tanner SL, Sykes JW, Moulder H, Hand WR, Morgan RR Jr. Airway Proficiency and Efficiency Amongst Anesthesia Providers and Respiratory Therapists: A Comparison Study. Journal of Clinical Medicine. 2025; 14(22):8059. https://doi.org/10.3390/jcm14228059
Chicago/Turabian StyleBrignull, Calleigh G., Emily B. Williams, Harper A. Sprouse, Kyle J. Adams, Stephanie L. Tanner, John W. Sykes, Henry Moulder, William R. Hand, and Robert R. Morgan, Jr. 2025. "Airway Proficiency and Efficiency Amongst Anesthesia Providers and Respiratory Therapists: A Comparison Study" Journal of Clinical Medicine 14, no. 22: 8059. https://doi.org/10.3390/jcm14228059
APA StyleBrignull, C. G., Williams, E. B., Sprouse, H. A., Adams, K. J., Tanner, S. L., Sykes, J. W., Moulder, H., Hand, W. R., & Morgan, R. R., Jr. (2025). Airway Proficiency and Efficiency Amongst Anesthesia Providers and Respiratory Therapists: A Comparison Study. Journal of Clinical Medicine, 14(22), 8059. https://doi.org/10.3390/jcm14228059






