Prediabetes Is Associated with Increased Prevalence of Sleep-Disordered Breathing
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Approval
2.2. Design of the Study and Report of the Study Individuals
2.3. Diagnosis of Prediabetes
2.4. Nighttime Respiratory Function Assessment
2.5. Excessive Daytime Sleepiness Assessment
2.6. Covariates Assessment
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lecube, A.; Simó, R.; Pallayova, M.; Punjabi, N.M.; López-Cano, C.; Turino, C.; Hernández, C.; Barbé, F. Pulmonary Function and Sleep Breathing: Two New Targets for Type 2 Diabetes Care. Endocr. Rev. 2017, 38, 550–573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lecube, A.; Sampol, G.; Hernández, C.; Romero, O.; Ciudin, A.; Simó, R. Characterization of Sleep Breathing Pattern in Patients with Type 2 Diabetes: Sweet Sleep Study. PLoS ONE 2015, 10, e0119073. [Google Scholar] [CrossRef] [PubMed]
- Lecube, A.; Romero, O.; Sampol, G.; Mestre, O.; Ciudin, A.; Sánchez, E.; Hernández, C.; Caixàs, A.; Vigil, L.; Simó, R. Sleep biosignature of Type 2 diabetes: A case-control study. Diabet. Med. 2016, 34, 79–85. [Google Scholar] [CrossRef] [Green Version]
- Lecube, A.; Sánchez, E.; Gómez-Peralta, F.; Abreu, C.; Valls, J.; Mestre, O.; Romero, O.; Martinez, M.D.; Sampol, G.; CIudin, A.; et al. Global Assessment of the Impact of Type 2 Diabetes on Sleep through Specific Questionnaires. A Case-Control Study. PLoS ONE 2016, 11, e0157579. [Google Scholar] [CrossRef] [Green Version]
- Lecube, A.; Sampol, G.; Lloberes, P.; Romero, O.; Mesa, J.; Hernandez, C.; Simo, R. Diabetes is an independent risk factor for severe nocturnal hypoxemia in obese patients. A case-control study. PLoS ONE 2009, 4, e4692. [Google Scholar] [CrossRef]
- Gutiérrez-Carrasquilla, L.; López-Cano, C.; Sánchez, E.; Barbé, F.; Dalmases, M.; Hernández, M.; Campos, A.; Gaeta, A.M.; Carmona, P.; Hernández, C.; et al. Effect of Glucose Improvement on Nocturnal Sleep Breathing Parameters in Patients with Type 2 Diabetes: The Candy Dreams Study. J. Clin. Med. 2020, 9, 1022. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reutrakul, S.; Mokhlesi, B. Obstructive sleep apnea and diabetes: A state of the art review. Chest 2017, 152, 1070–1086. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.; Lin, B.M.; Stampfer, M.J.; Tworoger, S.S.; Hu, F.B.; Redline, S. A population-based study of the bidirectional association between obstructive sleep apnea and type 2 diabetes in three prospective U.S. cohorts. Diabetes Care 2018, 41, 2111–2119. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention. National Diabetes Statistics Report; Centers for Disease Control and Prevention, US Department of Health and Human Services: Atlanta, GA, USA, 2020.
- Alshaarawy, O.; Teppala, S.; Shankar, A. Markers of Sleep-Disordered Breathing and Prediabetes in US Adults. Int. J. Endocrinol. 2012, 2012, 902324. [Google Scholar] [CrossRef]
- Betriu, À.; Farràs, C.; Abajo, M.; Martinez-Alonso, M.; Arroyo, D.; Barbé, F.; Buti, M.; Lecube, A.; Portero, M.; Purroy, F.; et al. Randomised intervention study to assess the prevalence of subclinical vascular disease and hidden kidney disease and its impact on morbidity and mortality: The ILERVAS project. Nefrología 2016, 36, 389–396. [Google Scholar] [CrossRef] [Green Version]
- Bermúdez-López, M.; Martínez-Alonso, M.; Castro-Boqué, E.; Betriu, À.; Cambray, S.; Farràs, C.; Barbe, F.; Pamplona, R.; Lecube, A.; Mauricio, D.; et al. Subclinical atheromatosis localization and burden in a low-to-moderate cardiovascular risk population: The ILERVAS study. Rev. Esp. Cardiol. 2021, 74, 1042–1053. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. Classification and diagnosis of diabetes. Sec. 2. In standards of medical care in diabetes—2017. Diabetes Care 2017, 40, S11–S24. [Google Scholar]
- Lenters-Westra, E.; Slingerland, R.J. Three of 7 hemoglobin A1c point-of care instruments do not meet generally accepted analytical performance criteria. Clin. Chem. 2014, 60, 1062–1072. [Google Scholar] [CrossRef] [PubMed]
- Erman, M.K.; Stewart, D.; Einhorn, D.; Gordon, N.; Casal, E. Validation of the ApneaLinkTM for the screening of sleep apnea: A novel and simple single-channel recording device. J. Clin. Sleep Med. 2007, 3, 387–392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kapur, V.K.; Auckley, D.H.; Chowdhuri, S.; Kuhlmann, D.C.; Mehra, R.; Ramar, K.; Harrod, C.G. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: An American Academy of Sleep Medicine clinical practice guideline. J. Clin. Sleep Med. 2017, 13, 479–504. [Google Scholar] [CrossRef]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef] [Green Version]
- Shaw, J.E.; Punjabi, N.M.; Wilding, J.P.; Alberti, K.G.; Zimmet, P.Z. International Diabetes Federation Taskforce on Epidemiology and Prevention. Sleep-disordered breathing and type 2 diabetes: A report from the International Diabetes Federation Taskforce on Epidemiology and Prevention. Diabetes Res. Clin. Pract. 2008, 81, 2–12. [Google Scholar] [CrossRef]
- Fredheim, J.M.; Rollheim, J.; Omland, T.; Hofsø, D.; Røislien, J.; Vegsgaard, K.; Hjelmesæth, J. Type 2 diabetes and pre-diabetes are associated with obstructive sleep apnea in extremely obese subjects: A cross-sectional study. Cardiovasc. Diabetol. 2011, 25, 10–84. [Google Scholar] [CrossRef] [Green Version]
- Ramadan, W.; Dewasmes, G.; Petitjean, M.; Wiernsperger, N.; Delanaud, S.; Geloen, A.; Libert, J.P. Sleep apnea is induced by a high-fat diet and reversed and prevented by metformin in non-obese rats. Obesity 2007, 15, 1409–1418. [Google Scholar] [CrossRef]
- Balkau, B.; Vol, S.; Loko, S.; Andriamboavonjy, T.; Lantieri, O.; Gusto, G.; Meslier, N. Epidemiologic Study on the Insulin Resistance Syndrome Study Group. High baseline insulin levels associated with 6-year incident observed sleep apnea. Diabetes Care 2010, 33, 1044–1049. [Google Scholar] [CrossRef] [Green Version]
- Vgontzas, A.N.; Legro, R.S.; Bixler, E.O.; Grayev, A.; Kales, A.; Chrousos, G.P. Polycystic ovary syndrome is associated with obstructive sleep apnea and daytime sleepiness: Role of insulin resistance. J. Clin. Endocrinol. Metab. 2001, 86, 517–520. [Google Scholar] [PubMed]
- Yki-Järvinen, H.; Westerbacka, J. Vascular actions of insulin in obesity. Int. J. Obes. Relat. Metab. Disord. 2000, 24 (Suppl. 2), S25–S28. [Google Scholar] [CrossRef] [Green Version]
- Osman, A.M.; Carter, S.G.; Carberry, J.C.; Eckert, D.J. Obstructive sleep apnea: Current perspectives. Nat. Sci. Sleep 2018, 10, 21–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jahn, C.; Gouveris, H.; Matthias, C. Systemic inflammation in patients with compromised upper airway anatomy and primary snoring or mild obstructive sleep apnea. Eur. Arch. Oto-Rhino-Laryngol. 2016, 273, 3429–3433. [Google Scholar] [CrossRef]
- Levy, P.; Bonsignore, M.R.; Eckel, J. Sleep, sleep-disordered breathing and metabolic consequences. Eur. Respir. J. 2009, 34, 243–260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coopmans, C.; Zhou, T.L.; Henry, R.M.; Heijman, J.; Schaper, N.C.; Koster, A.; Schram, M.T.; van der Kallen, C.J.; Wesselius, A.; Engelsman, R.J.D.; et al. Both Prediabetes and Type 2 Diabetes Are Associated with Lower Heart Rate Variability: The Maastricht Study. Diabetes Care 2020, 43, 1126–1133. [Google Scholar] [CrossRef]
- Bassi, M.; Furuya, W.; Zoccal, D.B.; Menani, J.V.; Colombari, D.; Mulkey, D.; Colombari, E. Facilitation of breathing by leptin effects in the central nervous system. J. Physiol. 2016, 594, 1617–1625. [Google Scholar] [CrossRef] [Green Version]
- Bradley, T.D.; Floras, J.S. Obstructive sleep apnea and its cardiovascular consequences. Lancet 2009, 373, 82–93. [Google Scholar] [CrossRef]
- Xie, C.; Zhu, R.; Tian, Y.; Wang, K. Association of obstructive sleep apnoea with the risk of vascular outcomes and all-cause mortality: A meta-analysis. BMJ Open 2017, 7, e013983. [Google Scholar] [CrossRef] [Green Version]
- Sánchez, E.; Betriu, À.; López-Cano, C.; Hernández, M.; Fernández, E.; Purroy, F.; Bermúdez-López, M.; Farràs-Sallés, C.; Barril, S.; Pamplona, R.; et al. Characteristics of atheromatosis in the prediabetes stage: A cross-sectional investigation of the ILERVAS project. Cardiovasc. Diabetol. 2019, 18, 154. [Google Scholar] [CrossRef] [Green Version]
- López-Cano, C.; Rius, F.; Sánchez, E.; Gaeta, A.M.; Betriu, À.; Fernández, E.; Yeramian, A.; Hernández, M.; Bueno, M.; Gutiérrez-Carrasquilla, L.; et al. The influence of sleep apnea syndrome and intermittent hypoxia in carotid adventitial vasa vasorum. PLoS ONE. 2019, 14, e0211742. [Google Scholar]
- Gilardini, L.; Lombardi, C.; Redaelli, G.; Vallone, L.; Faini, A.; Mattaliano, P.; Parati, G.; Invitti, C. Glucose tolerance and weight loss in obese women with obstructive sleep apnea. PLoS ONE. 2013, 8, e61382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reutrakul, S.; Sumritsopak, R.; Saetung, S.; Chanprasertyothin, S.; Anothaisintawee, T. The relationship between sleep and glucagon-like peptide 1 in patients with abnormal glucose tolerance. J. Sleep Res. 2017, 26, 756–763. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsumoto, T.; Harada, N.; Azuma, M.; Chihara, Y.; Murase, K.; Tachikawa, R.; Minami, T.; Hamada, S.; Tanizawa, K.; Inouchi, M.; et al. Plasma Incretin Levels and Dipeptidyl Peptidase- 4 Activity in Patients with Obstructive Sleep Apnea. Ann. Am. Thorac. Soc. 2016, 13, 1378–1387. [Google Scholar] [CrossRef] [PubMed]
- Blackman, A.; on behalf of the SCALE Study Group; Foster, G.D.; Zammit, G.; Rosenberg, R.; Aronne, L.; Wadden, T.; Claudius, B.; Jensen, C.B.; Mignot, E. Effect of liraglutide 3.0 mg in individuals with obesity and moderate or severe obstructive sleep apnea: The SCALE Sleep Apnea randomized clinical trial. Int. J. Obes. 2016, 40, 1310–1319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, Y.; Sun, Q.; Bai, X.Y.; Zhou, Y.F.; Zhou, Q.L.; Zhang, M. Effect of dapagliflozin on obstructive sleep apnea in patients with type 2 diabetes: A preliminary study. Nutr. Diabetes 2019, 9, 32. [Google Scholar] [CrossRef]
- Iyegha, I.D.; Chieh, A.Y.; Bryant, B.M.; Li, L. Associations between poor sleep and glucose intolerance in prediabetes. Psychoneuroendocrinology 2019, 110, 104444. [Google Scholar] [CrossRef]
- Renko, A.K.; Hiltunen, L.; Laakso, M.; Rajala, U.; Keinänen-Kiukaanniemi, S. The relationship of glucose tolerance to sleep disorders and daytime sleepiness. Diabetes Res. Clin. Pract. 2005, 67, 84–91. [Google Scholar] [CrossRef]
| Prediabetes (n = 311) | Control Group (n = 655) | p | |
|---|---|---|---|
| Age (years) | 59 (54;63) | 56 (52;61) | <0.001 |
| Women, n (%) | 180 (57.8) | 316 (48.2) | 0.004 |
| HbA1c (mmol/mol) | 40 (39;42) | 36 (33;37) | <0.001 |
| HbA1c (%) | 5.8 (5.8;6.0) | 5.4 (5.2;5.5) | <0.001 |
| Hypertension, n (%) | 147 (47.2) | 240 (36.6) | 0.001 |
| Systolic blood pressure (mm Hg) | 132 (120;143) | 128 (118;139) | 0.008 |
| Diastolic blood pressure (mm Hg) | 81 (75;88) | 81 (74;87) | 0.569 |
| Obesity, n (%) | 124 (39.8) | 177 (27.0) | <0.001 |
| BMI (Kg/m2) | 29.7 (26.9;33.2) | 27.9 (24.9;31.0) | <0.001 |
| Waist circumference (cm) | 103 (96;110) | 98 (92;106) | <0.001 |
| Neck circumference (cm) | 37.5 (35.0;41.0) | 37.5 (34.5;41.0) | 0.261 |
| Current or former smoker, n (%) | 184 (59.1) | 430 (65.6) | 0.050 |
| Prediabetes (n = 311) | Control Group (n = 655) | p | |
|---|---|---|---|
| Time of evaluation (hs) | 7.2 (6.4;8.0) | 7.2 (6.5;8.0) | 0.684 |
| AHI (events/h) | 12.7 (6.1;24.3) | 9.5 (4.2;19.6) | <0.001 |
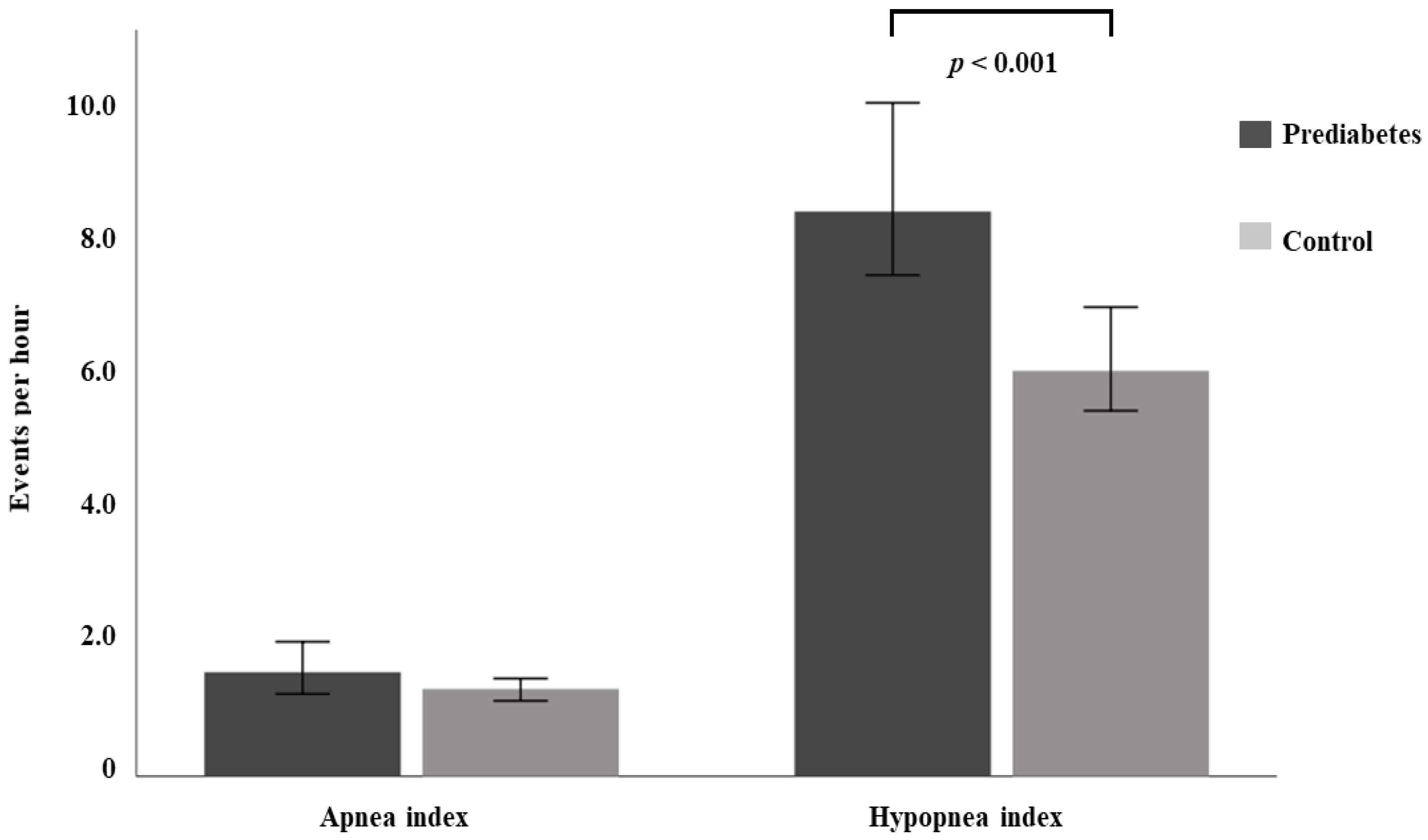
| Apnea index (events/h) | 1.6 (0.4;5.8) | 1.3 (0.4;4.3) | 0.159 |
| Hypopnea index (events/h) | 8.4 (4.0;14.9) | 6.0 (2.7;12.6) | <0.001 |
| OSA, n (%) | 243 (78.1) | 458 (69.9) | 0.007 |
| Mild OSA, n (%) | 108 (34.8) | 227 (34.6) | 0.142 |
| Moderate OSA, n (%) | 76 (24.4) | 138 (21.0) | 0.060 |
| Severe OSA, n (%) | 57 (18.5) | 89 (13.6) | 0.010 |
| Median SpO2 level (%) | 92 (91;93) | 93 (92;94) | <0.001 |
| Minimum SpO2 level (%) | 82 (77;85) | 83 (80;87) | <0.001 |
| CT90 (%) | 14 (4;33) | 6 (1;24) | <0.001 |
| ODI4% (events/h) | 14 (8;27) | 11 (5;21) | 0.001 |
| Epworth Sleepiness Scale score * | 4 (2;5) | 3 (2;5) | 0.740 |
| Prediabetes (n = 311) | Entire Population (n = 966) | |||
|---|---|---|---|---|
| r | p | r | p | |
| AHI (events/h) | 0.093 | 0.099 | 0.131 | <0.001 |
| Apnea index (events/h) | −0.039 | 0.492 | 0.065 | 0.042 |
| Hypopnea index (events/h) | 0.171 | 0.002 | 0.141 | <0.001 |
| Median SpO2 level (%) | −0.166 | 0.003 | −0.204 | <0.001 |
| Minimum SpO2 level (%) | −0.126 | 0.025 | −0.159 | <0.001 |
| CT90 (%) | 0.144 | 0.010 | 0.209 | <0.001 |
| ODI4% (events/h) | 0.123 | 0.028 | 0.150 | <0.001 |
| Epworth Sleepiness Scale score * | 0.009 | 0.884 | −0.035 | 0.322 |
| AHI (Events/h) R2 = 0.12 | B (95% IC) | Standardized Regression Coefficients | p |
|---|---|---|---|
| Age (Years) | 0.36 (0.19 to 0.52) | 0.14 | <0.001 |
| Sex (Male) | 8.29 (6.23 to 10.35) | 0.24 | <0.001 |
| Obesity (BMI ≥ 30 kg/m2) | 8.54 (6.44 to 10.64) | 0.26 | <0.001 |
| Prediabetes (HbA1c 5.7 to 6.4%) | 2.20 (0. 10 to 4.31) | 0.58 | 0.040 |
| Apnea index (events/h) R2 = 0.06 | |||
| Age (Years) | 0.21 (0.13 to 0.30) | 0.17 | <0.001 |
| Sex (Male) | 3.58 (2.55 to 4.62) | 0.20 | <0.001 |
| Obesity (BMI ≥ 30 kg/m2) | 1.73 (0.67 to 2.78) | 0.11 | 0.001 |
| Prediabetes (HbA1c 5.7 to 6.4%) | 0.16 (−0. 90 to 1.22) | 0.00 | 0.765 |
| Hypopnea index (events/h) R2 = 0.12 | |||
| Age (Years) | 0.13 (0.03 to 0.23) | 0.11 | 0.013 |
| Sex (Male) | 3.81 (2.57 to 5.05) | 0.15 | <0.001 |
| Obesity (BMI ≥ 30 kg/m2) | 5.94 (4.68 to 7.21) | 0.29 | <0.001 |
| Prediabetes (HbA1c 5.7 to 6.4%) | 1.87 (0. 61 to 3.14) | 0.82 | 0.004 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sánchez, E.; Sapiña-Beltrán, E.; Gavaldà, R.; Barbé, F.; Torres, G.; Sauret, A.; Dalmases, M.; López-Cano, C.; Gutiérrez-Carrasquilla, L.; Bermúdez-López, M.; et al. Prediabetes Is Associated with Increased Prevalence of Sleep-Disordered Breathing. J. Clin. Med. 2022, 11, 1413. https://doi.org/10.3390/jcm11051413
Sánchez E, Sapiña-Beltrán E, Gavaldà R, Barbé F, Torres G, Sauret A, Dalmases M, López-Cano C, Gutiérrez-Carrasquilla L, Bermúdez-López M, et al. Prediabetes Is Associated with Increased Prevalence of Sleep-Disordered Breathing. Journal of Clinical Medicine. 2022; 11(5):1413. https://doi.org/10.3390/jcm11051413
Chicago/Turabian StyleSánchez, Enric, Esther Sapiña-Beltrán, Ricard Gavaldà, Ferran Barbé, Gerard Torres, Ariadna Sauret, Mireia Dalmases, Carolina López-Cano, Liliana Gutiérrez-Carrasquilla, Marcelino Bermúdez-López, and et al. 2022. "Prediabetes Is Associated with Increased Prevalence of Sleep-Disordered Breathing" Journal of Clinical Medicine 11, no. 5: 1413. https://doi.org/10.3390/jcm11051413






