Oral-Health-Related Quality of Life as Measured with the Child-OIDP Index and Oral Health Status in Spanish Adolescents
Abstract
1. Introduction
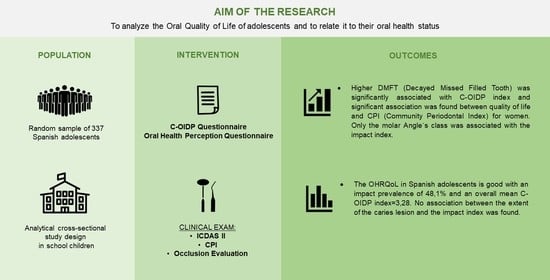
2. Materials and Methods
2.1. Study Design and Setting
2.2. Sample Selection
2.3. Survey Instruments
2.3.1. Oral Health Perception Questionnaire
2.3.2. Child-OIDP Questionnaire
2.4. Clinical Diagnostic Criteria
2.4.1. Dental Status
2.4.2. Periodontal Status
2.4.3. Occlusal Status
2.5. Field Work
2.6. Data Analysis
3. Results
3.1. Psychometric Properties of the Child-OIDP
3.2. Oral Health Perception
3.3. Impact of Oral Health Measured with Child-OIDP Index
3.4. Clinical Exam
3.5. Association between the C-OIDP Index and the Clinical Variables
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| C-OIDP | Child-Oral Impacts on Daily Performances |
| CPI | Community Periodontal Index |
| CS-C-OIDP | Condition Specific Child-Oral Impacts on Daily Performances |
| DMFT | Decayed Missed Filled Tooth |
| ICDAS II | International Caries Detection and Assessment System |
| OHRQoL | Oral-Health-Related Quality of Life |
| QoL | Quality of Life |
| OSS | Oral Satisfaction Scale |
| SESPO | Sociedad Española de Epidemiología y Salud Pública Oral |
| WHO | World Health Organization. |
References
- Kazeminia, M.; Abdi, A.; Shohaimi, S.; Jalali, R.; Vaisi-Raygani, A.; Salari, N.; Mohammadi, M. Dental caries in primary and permanent teeth in children’s worldwide, 1995 to 2019: A systematic review and meta-analysis. Head Face Med. 2020, 16, 22. [Google Scholar] [CrossRef]
- Blatz, M.B.; Chiche, G.; Bahat, O.; Roblee, R.; Coachman, C.; Heymann, H.O. Evolution of Aesthetic Dentistry. J. Dent. Res. 2019, 98, 1294–1304. [Google Scholar] [CrossRef]
- Hescot, P. The New Definition of Oral Health and Relationship between Oral Health and Quality of Life. Chin. J. Dent. Res. 2017, 20, 189–192. [Google Scholar]
- The World Health Organization Quality of Life assessment (WHOQOL): Position paper from the World Health Organization. Soc. Sci. Med. 1995, 41, 1403–1409. [CrossRef]
- Locker, D. Concepts of Oral Health, Disease and the Quality of Life. In Measuring Oral Health and Quality of Life; Slade, G.D., Ed.; University of North Carolina: Chapel Hill, NC, USA, 1997; pp. 11–23. [Google Scholar]
- Thomson, W.M.; Broder, H.L. Oral Health-Related Quality of Life in Children and Adolescents. Pediatr. Clin. North 2018, 65, 1073–1084. [Google Scholar] [CrossRef]
- Atchison, K.A.; Dolan, T.A. Development of the Geriatric Oral Health Assessment Index. J. Dent. Educ. 1990, 54, 680–687. [Google Scholar] [CrossRef]
- Slade, G.D.; Spencer, A.J. Development and evaluation of the Oral Health Impact Profile. Community Dent. Health 1994, 11, 3–11. [Google Scholar]
- Leão, A.; Sheiham, A. The development of a socio-dental measure of dental impacts on daily living. Community Dent. Health 1996, 13, 22–26. [Google Scholar]
- Adulyanon, S.; Sheiham, A. Oral Impacts on Daily Performances. In Measuring Oral Health and Quality of Life; Slade, G.D., Ed.; University of North Carolina: Chapel Hill, NC, USA, 1997; pp. 151–160. [Google Scholar]
- Culler, C.S.; Gunarajasingam, D.; Henshaw, M.M. Preschool oral health-related quality of life: A practical guide to measurement tools. J. Public Health Dent. 2021, 81, 29–41. [Google Scholar] [CrossRef]
- Hettiarachchi, R.M.; Kularatna, S.; Byrnes, J.; Scuffham, P.A. Pediatric Quality of Life Instruments in Oral Health Research: A Systematic Review. Value Health 2019, 22, 129–135. [Google Scholar] [CrossRef]
- Thomson, W.M. Subjective oral health measures for use with children: New Zealand´s contribution to a burgeoning field. J. R. Soc. N. Z. 2020, 50, 4–14. [Google Scholar] [CrossRef]
- Jokovic, A.; Locker, D.; Stephens, M.; Kenny, D.; Tompson, B.; Guyatt, G. Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J. Dent. Res. 2002, 81, 459–463. [Google Scholar] [CrossRef]
- Broder, H.L.; McGrath, C.; Cisneros, G.J. Questionnaire development: Face validity and item impact testing of the Child Oral Health Impact Profile. Community Dent. Oral Epidemiol. 2007, 1, 8–19. [Google Scholar] [CrossRef]
- Gherunpong, S.; Tsakos, G.; Sheiham, A. Developing and evaluating an oral health-related quality of life index for children; the CHILD-OIDP. Community Dent. Health 2004, 21, 161–169. [Google Scholar]
- Bernabé, E.; Krisdapong, S.; Sheiham, A.; Tsakos, G. Comparison of the discriminative ability of the generic and condition-specific forms of the Child-OIDP index: A study on children with different types of normative dental treatment needs. Community Dent. Oral Epidemiol. 2009, 37, 155–162. [Google Scholar] [CrossRef]
- Mbawalla, H.S.; Mtaya, M.; Masalu, J.R.; Brudvik, P.; Astrom, A.N. Discriminative ability of the generic and condition-specific Child-Oral Impacts on Daily Performances (Child-OIDP) by the Limpopo-Arusha School Health (LASH) project: A cross-sectional study. BMC Pediatr. 2011, 11, 45. [Google Scholar] [CrossRef]
- Patil, S.; Kahtani, A.A.; Baeshen, H.A.; Alamir, A.W.; Khan, S.; Bhandi, S.; Hosmani, J.; Raj, A.T.; Gadbail, A.; Gondivkar, S.; et al. Face Validity and Psychometric Evaluation of the Available Oral Health-related Quality of Life Instruments: A Systematic Review. Oral Health Prev. Dent. 2020, 18, 409–416. [Google Scholar]
- Pentapati, K.C.; Yeturu, S.K.; Siddiq, H. A reliability generalization meta-analysis of Child Oral Impacts on Daily Performances (C-OIDP) questionnaire. J. Oral Biol. Craniofac. Res. 2020, 10, 776–781. [Google Scholar] [CrossRef]
- Cortés-Martinicorena, F.J.; Rosel-Gallardo, E.; Artazcoz-Osés, J.; Bravo, M.; Tsakos, G. Adaptation and validation for Spain of the Child-Oral Impact on Daily Performance (C-OIDP) for use with adolescents. Med. Oral Patol. Oral Cir. Bucal 2010, 15, 106–111. [Google Scholar] [CrossRef]
- Montero, J.; Rosel, E.; Barrios, R.; López-Valverde, A.; Albaladejo, A.; Bravo, M. Oral health-related quality of life in 6- to 12-year-old schoolchildren in Spain. Int. J. Paediatr. Dent. 2016, 26, 220–230. [Google Scholar] [CrossRef]
- Bravo, M.; Cortés, F.J.; Casals, E.; Llena, C.; Almerich-Silla, J.M.; Cuenca, E. Basic oral health goals for Spain 2015/2020. Int. Dent. J. 2009, 59, 78–82. [Google Scholar]
- Bravo Pérez, M.; Almerich Silla, J.M.; Canorea Díaz, E.; Casals Peidró, E.; Cortés Martinicorena, F.J.; Expósito Delgado, A.J.; Gómez Santos, G.; Hidalgo Olivares, G.; Lamas Oliveira, M.; Martínez Beneyto, Y.; et al. Encuesta de Salud Oral en España 2020. RCOE 2020, 25, 12–69. [Google Scholar]
- Petersen, P.E.; Baez, R.J.; World Health Organization. Oral Health Surveys: Basic Methods, 5th ed.; World Health Organization: Geneva, Switzerland, 2013; pp. 42–56. [Google Scholar]
- Álvarez-Azaustre, M.P.; Greco, R.; Llena, C. Oral Health-Related Quality of Life in Adolescents as Measured with the Child-OIDP Questionnaire: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 12995. [Google Scholar] [CrossRef]
- Almerich-Silla, J.M.; Boronat-Ferrer, T.; Montiel-Company, J.M.; Iranzo-Cortés, J.E. Caries prevalence in children from Valencia (Spain) using ICDAS II criteria, 2010. Med. Oral Patol Oral Cir. Bucal 2014, 19, 574–580. [Google Scholar] [CrossRef]
- Almerich-Torres, T.; Montiel-Company, J.M.; Bellot-Arcís, C.; Iranzo-Cortés, J.E.; Ortolá-Siscar, J.C.; Almerich-Silla, J.M. Caries Prevalence Evolution and Risk Factors among Schoolchildren and Adolescents from Valencia (Spain): Trends 1998–2018. Int. J. Environ. Res. Public Health 2020, 17, 6561. [Google Scholar] [CrossRef]
- Dikmen, B. Icdas II criteria (International Caries Detection and Assessment System). J. Istanb. Univ. Fac. Dent. 2015, 49, 63–72. [Google Scholar] [CrossRef]
- Ismail, A.I.; Sohn, W.; Tellez, M.; Amaya, A.; Sen, A.; Hasson, H.; Pitts, N.B. The International Caries Detection and Assessment System (ICDAS): An integrated system for measuring dental caries. Community Dent. Oral Epidemiol. 2007, 35, 170–178. [Google Scholar] [CrossRef]
- Pitts, N.B.; Carter, N.L.; Tsakos, G. The Brussels Statement on the Future Needs for Caries Epidemiology and Surveillance in Europe. Community Dent. Health 2018, 35, 66. [Google Scholar]
- Montero, J.; Bravo, M.; Albaladejo, A. Validation of two complementary oral-health related quality of life indicators (OIDP and OSS 0-10) in two qualitatively distinct samples of the Spanish population. Health Qual. Life Outcomes 2008, 6, 101. [Google Scholar] [CrossRef]
- ICCMS™ Caries Management. Available online: https://www.iccms-web.com (accessed on 11 August 2022).
- Proffit, W.R.; Fields, H.W., Jr.; Sarver, D.M.; Tello-Rodríguez, A.I. Contemporary Orthodontics, 6th ed.; Elsevier: Philadelphia, PA, USA, 2019. [Google Scholar]
- Bernabé, E.; Sheiham, A.; Tsakos, G. A comprehensive evaluation of the validity of Child-OIDP: Further evidence from Peru. Community Dent. Oral Epidemiol. 2008, 36, 317–325. [Google Scholar] [CrossRef]
- Castro, R.A.L.; Cortes, M.I.S.; Leão, A.T.; Portela, M.C.; Souza, I.P.R.; Tsakos, G.; Marcenes, W.; Sheiham, A. Child-OIDP index in Brazil: Cross-cultural adaptation and validation. Health Qual. Life Outcomes 2008, 6, 68. [Google Scholar] [CrossRef]
- Yusuf, H.; Gherunpong, S.; Tsakos, G.; Sheiham, A. Validation of an English version of Child-OIDP index, an oral health related quality of life measure for children. Health Qual. Life Outcomes 2006, 4, 38. [Google Scholar] [CrossRef]
- Tubert-Jeannin, S.; Pegon-Machat, E.; Gremeau-Richard, C.; Lecuyer, M.M.; Tsakos, G. Validation of a French version of Child-OIDP index. Eur. J. Oral Sci. 2005, 113, 355–362. [Google Scholar] [CrossRef]
- Rosel, E.; Tsakos, G.; Bernabé, E.; Sheiham, A.; Bravo, M. Assessing the level of agreement between the self- and interview-administered Child-OIDP. Community Dent. Oral Epidemiol. 2010, 38, 340–347. [Google Scholar] [CrossRef]
- Pitts, N.B.; Banerjee, A.; Mazevet, M.E.; Goffin, G.; Martignon, S. From ‘ICDAS’ to ‘Caries Care International’: The 20-year journey building international consensus to take caries evidence into clinical practice. Br. Dent. J. 2021, 231, 769–774. [Google Scholar] [CrossRef]
- Bianco, A.; Fortunato, L.; Nobile, C.G.A.; Pavia, M. Prevalence and determinants of oral impacts on daily performance: Results from a survey among school children in Italy. Eur. J. Public Health 2010, 20, 595–600. [Google Scholar] [CrossRef]
- Pavithran, V.K.; Murali, R.; Krishna, M.; Shamala, A.; Yalamalli, M.; Kumar, A.V.; Raina, R. Impact of oral diseases on daily activities among 12- to 15-year-old institutionalized orphan and non-orphan children in Bengaluru city: A cross-sectional analytical study. Indian J. Dent. Res. 2020, 31, 396–402. [Google Scholar] [CrossRef]
- Alzahrani, A.A.H.; Alhassan, E.M.; Albanghali, M.A. Association between oral diseases and impact on daily performance among male Saudi schoolchildren. Clin. Exp. Dent. Res. 2019, 5, 655–664. [Google Scholar] [CrossRef]
- Dumitrache, M.A.; Comes, C.; Teodorescu, E.; Dumitrascu, L.; Cuculescu, M.; Ionescu, E. Life quality related to oral health of schoolchildren from Bucharest. Rev. Romana Bioet. 2009, 7, 169–178. [Google Scholar]
- Hamamci, N.; Başaran, G.; Uysal, E. Dental Aesthetic Index scores and perception of personal dental appearance among Turkish university students. Eur. J. Orthod. 2009, 31, 168–173. [Google Scholar] [CrossRef]
- Bakhtiar, M.; Mohammadi, T.M.; Hajizamani, A.; Vossoughi, M. Association of Oral Health Indicators with Quality-of-Life Related to Oral Health among Iranian Adolescent. J. Int. Oral Health 2014, 6, 5–9. [Google Scholar]
- Basavaraj, P.; Sunil, M.K.; Nagarajappa, R.; Ashish, S.; Ramesh, G. Correlation between oral health and Child-OIDP Index in 12-and 15-year-old children from Modinagar, India. Asia Pac. J. Public Health 2014, 26, 390–400. [Google Scholar] [CrossRef]
- Alrashed, M.; Alqerban, A. The relationship between malocclusion and oral health-related quality of life among adolescents: A systematic literature review and meta-analysis. Eur. J. Orthod. 2021, 43, 173–183. [Google Scholar] [CrossRef]
- Cronbach, L. Coefficient alpha and the internal structure of tests. Psychometrica 2006, 16, 297–333. [Google Scholar] [CrossRef]
- Athira, S.; Jayakumar, H.L.; Chandra, M.; Gupta, T.; Dithi, C.; Anand, P.J.S. Oral Health-Related Quality of Life of School Children Aged 12–17 Years According to the Child-Oral Impacts on Daily Performances Index and the Impact of Oral Health Status on Index Scores. Int. J. Prev. Public Health Sci. 2015, 1, 25–30. [Google Scholar]
- Dhawan, P.; Singh, A.; Agarwal, A.; Aeran, H. Psychometric properties of Hindi version of child oral impact on daily performances (C-OIDP) index amongst school children in North India. J. Oral Biol. Craniofac. Res. 2019, 9, 10–13. [Google Scholar] [CrossRef]
- Simangwa, L.D.; Johansson, A.K.; Johansson, A.; Minja, I.K.; Åstrøm, A.N. Oral impacts on daily performances and its socio-demographic and clinical distribution: A cross-sectional study of adolescents living in Maasai population areas, Tanzania. Health Qual. Life Outcomes 2020, 18, 181. [Google Scholar] [CrossRef]
- Reinoso-Vintimilla, N.; del Castillo-López, C. Calidad de vida relacionada a la salud bucal en escolares de Sayausí, Cuenca Ecuador. Quality of life related to the oral health in school from Sayausí, Cuenca Ecuador. Rev. Estomatol. Hered. 2017, 27, 227–234. [Google Scholar] [CrossRef]
- Kumar, S.; Kumar, A.; Badiyani, B.; Kumar, A.; Basak, D.; Ismail, L.M.B. Oral health impact, dental caries experience, and associated factors in 12–15-year-old school children in India. Int. J. Adolesc. Med. Health 2017, 29, 2. [Google Scholar] [CrossRef]
- Paredes-Martínez, E.R.; Díaz-Pizán, M.E. Impact of oral conditions on the quality of life in schoolchildren in San Juan de Miraflores. Lima, Perú. Rev. Estomatol. Hered. 2014, 24, 171–177. [Google Scholar] [CrossRef]
- Naidoo, S.; Sheiham, A.; Tsakos, G. The relation between oral impacts on daily performances and perceived clinical oral conditions in primary school children in the Ugu District, Kwazulu Natal, South Africa. SADJ 2013, 68, 214–218. [Google Scholar]
- Nordin, E.A.B.; Shoaib, L.A.; Yusof, Z.Y.M.; Manan, N.M.; Othman, S.A. Oral health-related quality of life among 11–12 years old indigenous children in Malaysia. BMC Oral Health 2019, 19, 152. [Google Scholar]
- Bernabé, E.; Tsakos, G.; Sheiham, A. Intensity and extent of oral impacts on daily performances by type of self-perceived oral problems. Eur. J. Oral Sci. 2007, 115, 111–116. [Google Scholar] [CrossRef]
- Marcelo-Ingunza, J.; del Castillo-López, C.; Evangelista-Alva, A.; Sánchez-Borjas, P. Oral Health Related Quality of Life in school children of urban-marginal area. Rev. Estomatol. Hered. 2015, 25, 194–204. [Google Scholar]
- Moreno-Ruiz, X.; Vera-Abara, C.; Cartes-Velásquez, R. Oral health impact on the quality of life of 11 to 14 years-old schoolchildren, Licantén, 2013. Rev. Clin. Periodoncia Implantol. Rehabil. Oral 2014, 7, 142–148. [Google Scholar]
- Arumrahayu, W.; Maharani, D.A.; Adiatman, M. An Indonesian version of child oral impact on daily performances (C-OIDP): Assessing validity and reliability. J. Int. Dent. Med. Res. 2018, 11, 1049–1052. [Google Scholar]
- Vera, C.; Moreno, X.; Rivera, D.C. Adaptation and validation of Child Oral Impact on Daily Performance index in 11-14-year-old Chilean school children. J. Oral Res. 2013, 2, 119–124. [Google Scholar] [CrossRef][Green Version]
- Peker, K.; Eden, E.; Ak, A.S.; Uysal, Ö.; Bermek, G. Psychometric evaluation of the child oral impacts on daily performances (C-OIDP) for use in Turkish primary school children: A cross sectional validation study. BMC Oral Health 2020, 20, 173. [Google Scholar] [CrossRef]
- Chaudhary, F.A.; Iqbal, A.; Khalid, M.D.; Noor, N.; Syed, J.; Baig, M.N.; Khattak, O.; Din, S.U. Validation and Reliability Testing of the Child Oral Impacts on Daily Performances (C-OIDP): Cross-Cultural Adaptation and Psychometric Properties in Pakistani School-Going Children. Children 2022, 9, 631. [Google Scholar] [CrossRef]
- Nasia, A.A.; Arumrahayu, W.; Rosalien, R.; Maharani, A.; Adiatman, M. Child-oral impacts on daily performances index in indonesia: Cross-cultural adaptation and initial validation. Malays. J. Public Health Med. 2019, 2, 68–77. [Google Scholar] [CrossRef]
- Alade, O.; Ajoloko, E.; Dedeke, A.; Uti, O.; Sofola, O. Self-reported halitosis and oral health related quality of life in adolescent students from a suburban community in Nigeria. Afr. Health Sci. 2020, 20, 2044–2049. [Google Scholar] [CrossRef]
- Kragt, L.; Dhamo, B.; Wolvius, E.B.; Ongkosuwito, E.M. The impact of malocclusions on oral health-related quality of life in children-a systematic review and meta-analysis. Clin. Oral Investig. 2016, 20, 1881–1894. [Google Scholar] [CrossRef]

| ICDAS II | |||
|---|---|---|---|
| Restoration Code | Criteria | Caries Code | Criteria |
| 0 | No restoration or sealant | 0 | Healthy |
| 1 | Sealant in poor condition | 1 | Visual change in enamel after drying |
| 2 | Sealant in good condition | 2 | Visual change in enamel with wet tooth |
| 3 | Tooth-coloured filling | 3 | Localized enamel break |
| 4 | Amalgam | 4 | Underlying dark shade in dentine |
| 5 | Steel crown | 5 | Cavity with exposed dentine |
| 6 | Porcelain restoration | 6 | Extensive cavity |
| 7 | Lost or fractured filling | ||
| 8 | Temporary restoration | ||
| C-OIDP | Eating | Speaking | Brushing | Sleeping | Emotion | Schoolwork | Smiling | Playing |
|---|---|---|---|---|---|---|---|---|
| Eating | 1.00 | |||||||
| Speaking | 0.28 | 1.00 | ||||||
| Brushing | 0.16 | 0.47 | 1.00 | |||||
| Sleeping | 0.23 | 0.41 | 0.15 | 1.00 | ||||
| Emotion | 0.39 | 0.48 | 0.43 | 0.41 | 1.00 | |||
| Schoolwork | 0.32 | 0.41 | 0.42 | 0.06 | 0.34 | 1.00 | ||
| Smiling | 0.09 | 0.08 | 0.05 | 0.06 | 0.16 | 0.00 | 1.00 | |
| Playing | 0.15 | 0.13 | 0.09 | 0.08 | 0.07 | 0.07 | 0.00 | 1.000 |
| Corrected Item-Total Correlation | Cronbach’s Alpha If Item is Deleted | |
|---|---|---|
| Eating | 0.38 | 0.59 |
| Speaking | 0.57 | 0.56 |
| Brushing | 0.40 | 0.59 |
| Spleeping | 0.36 | 0.60 |
| Emotion | 0.61 | 0.50 |
| Schoolwork | 0.39 | 0.62 |
| Smiling | 0.13 | 0.70 |
| Playing | 0.13 | 0.65 |
| ICDAS 1–3 | ICDAS 4–6 | ||||
|---|---|---|---|---|---|
| N° of Teeth | n | % | N° of Teeth | n | % |
| 0 | 221 | 65.6 | 0 | 296 | 87.8 |
| 1 | 62 | 18.4 | 1 | 25 | 7.4 |
| 2 | 29 | 8.6 | 2 | 10 | 3 |
| 3 | 12 | 3.6 | 3 | 4 | 1.2 |
| 4 | 8 | 2.4 | 4 | 1 | 0.3 |
| 5 | 3 | 0.9 | 10 | 1 | 0.3 |
| 6 | 1 | 0.3 | |||
| 8 | 1 | 0.3 | |||
| Total | 337 | 100 | Total | 337 | 100 |
| CPI = 0 (Healthy) | CPI = 1 (Bleeding) | CPI = 2 (Calculus) | |
|---|---|---|---|
| Index Teeth | % Participants | ||
| 1.6 | 49.6 | 40.7 | 9.8 |
| 1.1 | 60.5 | 35.3 | 4.2 |
| 2.6 | 37.4 | 50.4 | 12.2 |
| 4.6 | 53.7 | 43.3 | 3 |
| 3.1 | 46.3 | 16 | 37.7 |
| 3.6 | 49.3 | 47.8 | 3 |
| C-OIDP | ||||||
|---|---|---|---|---|---|---|
| Variables | n | Mean ± SD | 95%CI | Median | Interq. Range | p |
| DMF-T Index = 0 | 234 | 3.16 ± 7.07 | 2.25–4.08 | 0 | 2.78 | 0.03 |
| DMF-T Index > 0 | 103 | 3.53 ± 5.21 | 2.51–4.55 | 1.38 | 5.56 | |
| ICDAS 1–3 = 0 | 221 | 3.45 ± 7.34 | 2.47–4.42 | 0 | 3.47 | 0.69 |
| ICDAS 1–3 > 0 | 116 | 2.95 ± 4.71 | 2.09–3.82 | 1.38 | 4.17 | |
| ICDAS 4–6 = 0 | 296 | 3.27 ± 6.74 | 2.50–4.04 | 0 | 2.78 | 0.89 |
| ICDAS 4–6 > 0 | 41 | 3.31 ± 5.10 | 1.70–4.93 | 0 | 5.56 | |
| CPI Index = 0 | 52 | 1.73 ± 2.47 | 1.04–2.42 | 0 | 2.78 | 0.36 |
| CPI Index > 0 | 285 | 3.56 ± 7.01 | 2.74–4.38 | 0 | 4.17 | |
| Malocclusion | 86 | 3.1 ± 7.5 | 1.5–4.7 | 0 | 4.5 | 0.37 |
| No malocclusion | 251 | 3.3 ± 6.1 | 2.5–4.1 | 0 | 4.1 | |
| No incisor crowding | 249 | 3.37 ± 6.98 | 2.50–4.24 | 0 | 4.17 | 0.90 |
| Incisor crowding | 88 | 3.01 ± 5.17 | 1.91–4.11 | 0 | 2.78 | |
| No incisor diastema | 278 | 3.39 ± 6.89 | 2.58–4.21 | 0 | 4.17 | 0.88 |
| Incisor diastema | 59 | 2.73 ± 4.67 | 1.51–3.94 | 0 | 2.78 | |
| No increased overbite | 226 | 3.52 ± 7.30 | 2.57–4.48 | 0 | 4.17 | 0.68 |
| Increased overbite | 111 | 2.77 ± 4.66 | 1.89–3.65 | 0 | 4.17 | |
| No increased overjet | 219 | 3.19 ± 6.49 | 2.33–4.06 | 0 | 4.17 | 0.56 |
| Increased overjet | 118 | 3.43 ± 6.69 | 2.21–4.66 | 0 | 2.78 | |
| No anterior open bite | 315 | 3.21 ± 6.65 | 2.47–3.95 | 0 | 2.78 | 0.12 |
| Anterior open bite | 22 | 4.22 ± 4.93 | 2.04–6.41 | 0 | 8.33 | |
| No posterior crossbite | 310 | 3.19 ± 6.41 | 2.47–3.91 | 0 | 2.78 | 0.33 |
| Posterior crossbite | 27 | 4.28 ± 8.10 | 1.06–7.47 | 0 | 4.17 | |
| Angle’s Class I | 111 | 2.6 ± 5.1 | 1.6–3.6 | 0 | 2.7 | 0.04 |
| Angle’s Class II | 121 | 3.6 ± 5.2 | 2.7–4.6 | 1.3 | 5.5 | |
| Angle’s Class III | 105 | 3.4 ± 8.8 | 1.7–5.1 | 0 | 2.7 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alvarez-Azaustre, M.P.; Greco, R.; Llena, C. Oral-Health-Related Quality of Life as Measured with the Child-OIDP Index and Oral Health Status in Spanish Adolescents. Int. J. Environ. Res. Public Health 2022, 19, 12450. https://doi.org/10.3390/ijerph191912450
Alvarez-Azaustre MP, Greco R, Llena C. Oral-Health-Related Quality of Life as Measured with the Child-OIDP Index and Oral Health Status in Spanish Adolescents. International Journal of Environmental Research and Public Health. 2022; 19(19):12450. https://doi.org/10.3390/ijerph191912450
Chicago/Turabian StyleAlvarez-Azaustre, María Paloma, Rossana Greco, and Carmen Llena. 2022. "Oral-Health-Related Quality of Life as Measured with the Child-OIDP Index and Oral Health Status in Spanish Adolescents" International Journal of Environmental Research and Public Health 19, no. 19: 12450. https://doi.org/10.3390/ijerph191912450
APA StyleAlvarez-Azaustre, M. P., Greco, R., & Llena, C. (2022). Oral-Health-Related Quality of Life as Measured with the Child-OIDP Index and Oral Health Status in Spanish Adolescents. International Journal of Environmental Research and Public Health, 19(19), 12450. https://doi.org/10.3390/ijerph191912450