Sleep as a Priority: 24-Hour Movement Guidelines and Mental Health of Chinese College Students during the COVID-19 Pandemic
Abstract
1. Introduction
2. Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. Sociodemographic Factors
2.2.2. 24-Hour Movement Behaviors
2.2.3. Mental Health Problems
2.3. Data Analyses
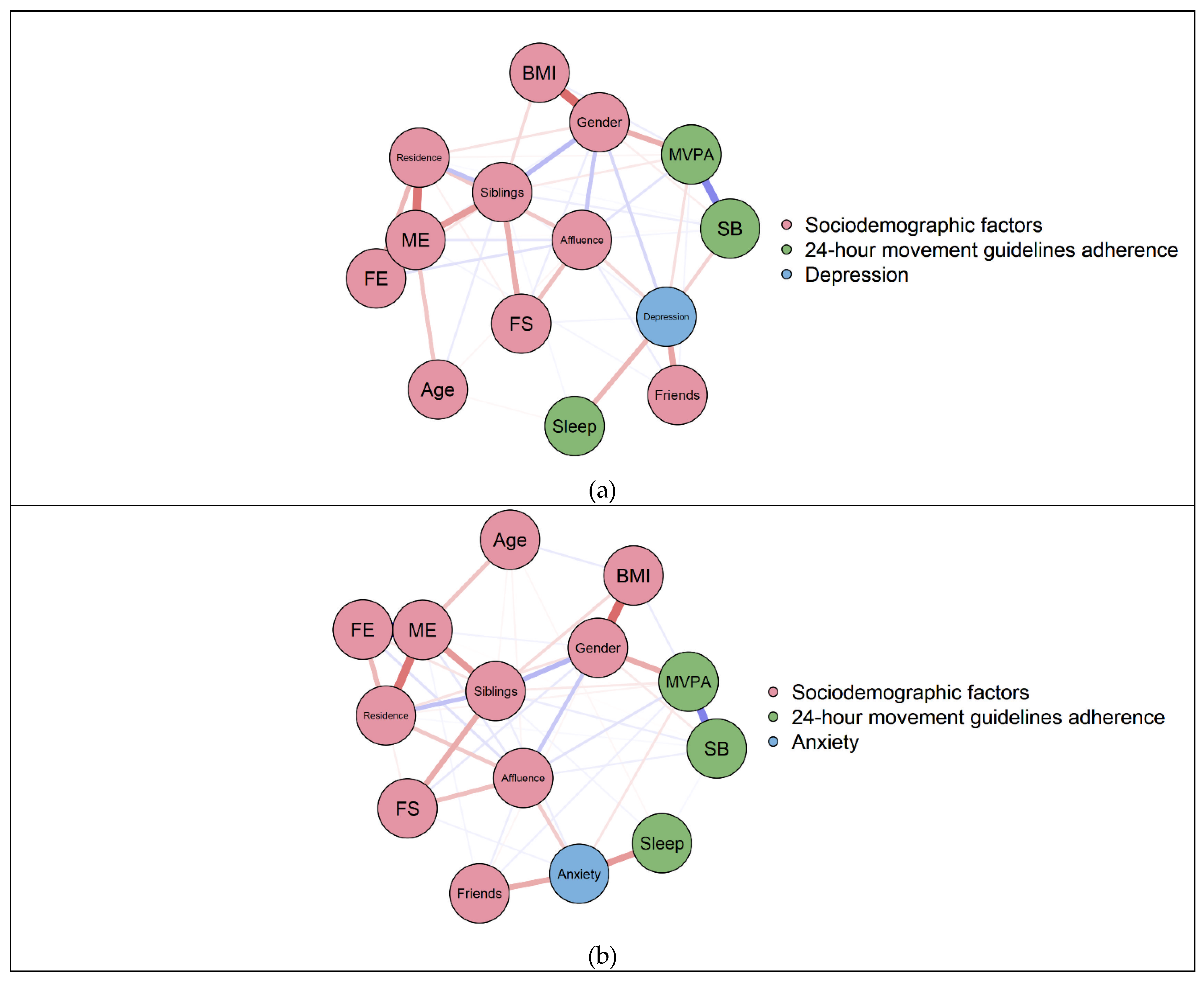
2.3.1. Network Analysis
2.3.2. Multivariate Analysis of Covariance (MANCOVA)
3. Results
3.1. Sample Characteristics
3.2. Individual Associations between Meeting 24-Hour Movement Guidelines with Depression and Anxiety
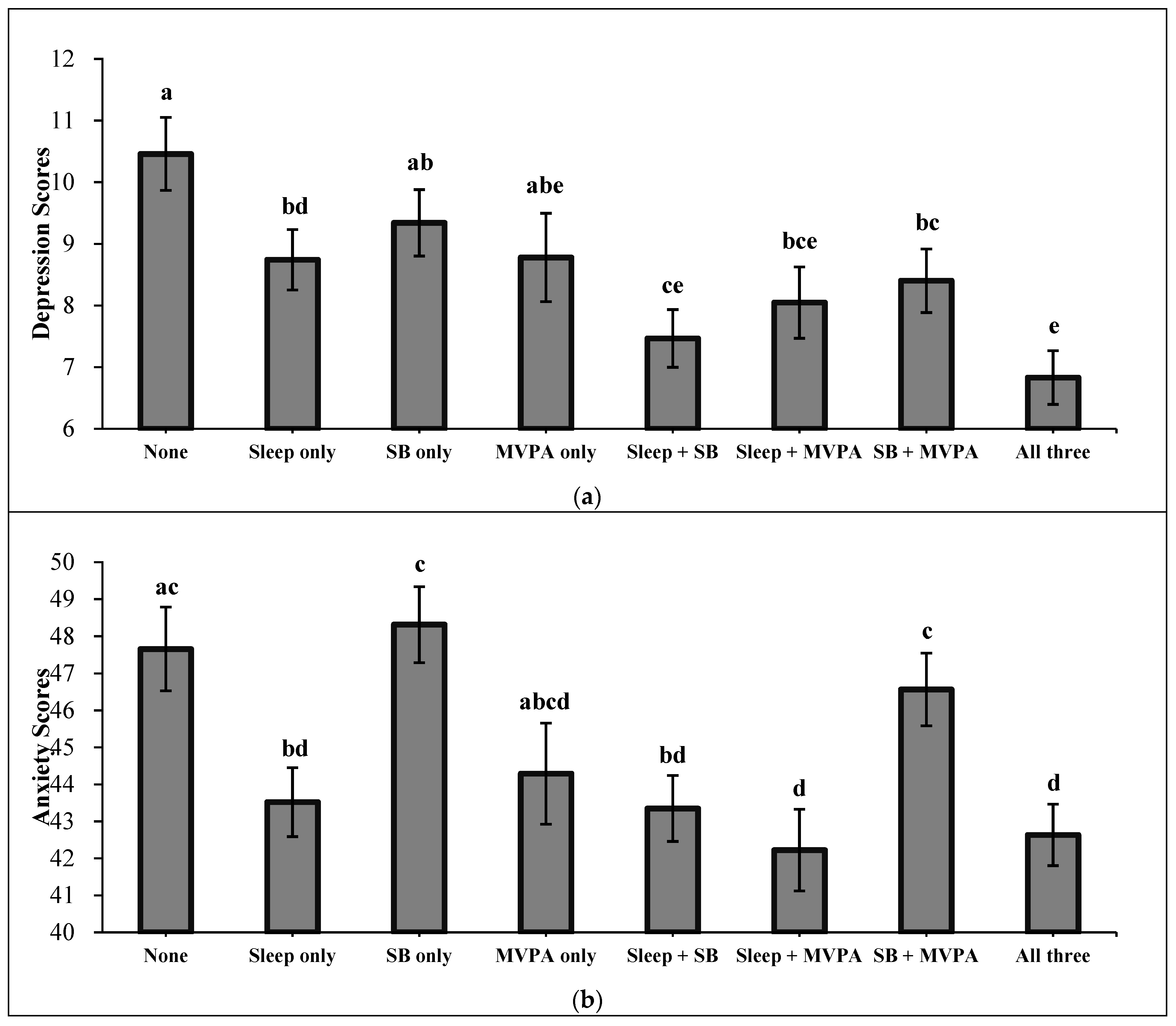
3.3. Combined Associations between Meeting 24-Hour Movement Guidelines with Depression and Anxiety
4. Discussion
4.1. Strengths and Practical Implications
4.2. Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hawes, M.T.; Szenczy, A.K.; Klein, D.N.; Hajcak, G.; Nelson, B.D. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol. Med. 2021, 1–9. [Google Scholar] [CrossRef]
- Fu, W.; Wang, C.; Zou, L.; Guo, Y.; Lu, Z.; Yan, S.; Mao, J. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Transl. Psychiatry 2020, 10, 225. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhao, J.; Ma, Z.; McReynolds, L.S.; Lin, D.; Chen, Z.; Wang, T.; Wang, D.; Zhang, Y.; Zhang, J.; et al. Mental Health Among College Students During the COVID-19 Pandemic in China: A 2-Wave Longitudinal Survey. J. Affect. Disord. 2021, 281, 597–604. [Google Scholar] [CrossRef]
- Browning, M.H.E.M.; Larson, L.R.; Sharaievska, I.; Rigolon, A.; McAnirlin, O.; Mullenbach, L.; Cloutier, S.; Vu, T.M.; Thomsen, J.; Reigner, N.; et al. Psychological impacts from COVID-19 among university students: Risk factors across seven states in the United States. PLoS ONE 2021, 16, e0245327. [Google Scholar] [CrossRef]
- Fu, W.; Yan, S.; Zong, Q.; Anderson-Luxford, D.; Song, X.; Lv, Z.; Lv, C. Mental health of college students during the COVID-19 epidemic in China. J. Affect. Disord. 2021, 280, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Tian, F.; Cui, Q.; Wu, H. Prevalence and its associated factors of depressive symptoms among Chinese college students during the COVID-19 pandemic. BMC Psychiatry 2021, 21, 1–8. [Google Scholar] [CrossRef]
- Trabelsi, K.; Ammar, A.; Masmoudi, L.; Boukhris, O.; Chtourou, H.; Bouaziz, B.; Brach, M.; Bentlage, E.; How, D.; Ahmed, M.; et al. Globally altered sleep patterns and physical activity levels by confinement in 5056 individuals: ECLB COVID-19 international online survey. Biol. Sport 2021, 38, 495–506. [Google Scholar] [CrossRef]
- Tang, W.; Hu, T.; Hu, B.; Jin, C.; Wang, G.; Xie, C.; Chen, S.; Xu, J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020, 274, 1–7. [Google Scholar] [CrossRef]
- Diamond, R.; Byrd, E. Standing up for health—Improving mental wellbeing during COVID-19 isolation by reducing sedentary behaviour. J. Affect. Disord. 2020, 277, 232–234. [Google Scholar] [CrossRef]
- Pedišić, Ž.; Dumuid, D.; Olds, T.S. Integrating sleep, sedentary behaviour, and physical activity research in the emerging field of time-use epidemiology: Definitions, concepts, statistical methods, theoretical framework, and future directions. Kinesiology 2017, 2, 1–18. [Google Scholar]
- Tremblay, M.S.; Carson, V.; Chaput, J.; Connor Gorber, S.; Dinh, T.; Duggan, M.; Faulkner, G.; Gray, C.E.; Gruber, R.; Janson, K.; et al. Canadian 24-Hour Movement Guidelines for Children and Youth: An Integration of Physical Activity, Sedentary Behaviour, and Sleep. Appl. Physiol. Nutr. Metab. 2016, 41, S311–S327. [Google Scholar] [CrossRef]
- Ross, R.; Chaput, J.; Giangregorio, L.M.; Janssen, I.; Saunders, T.J.; Kho, M.E.; Poitras, V.J.; Tomasone, J.R.; El-Kotob, R.; McLaughlin, E.C.; et al. Canadian 24-Hour Movement Guidelines for Adults aged 18–64 years and Adults aged 65 years or older: An integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab. 2020, 45, S57–S102. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Chaput, J.; Adamo, K.B.; Aubert, S.; Barnes, J.D.; Choquette, L.; Duggan, M.; Faulkner, G.; Goldfield, G.S.; Gray, C.E.; et al. Canadian 24-Hour Movement Guidelines for the Early Years (0–4 years): An Integration of Physical Activity, Sedentary Behaviour, and Sleep. BMC Public Health 2017, 17, 1–32. [Google Scholar] [CrossRef]
- Janssen, I.; Roberts, K.C.; Thompson, W. Is adherence to the Canadian 24-Hour Movement Behaviour Guidelines for Children and Youth associated with improved indicators of physical, mental, and social health? Appl. Physiol. Nutr. Metab. 2017, 42, 725–731. [Google Scholar] [CrossRef]
- Rollo, S.; Antsygina, O.; Tremblay, M.S. The whole day matters: Understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J. Sport Health Sci. 2020, 9, 493–510. [Google Scholar] [CrossRef]
- Carson, V.; Chaput, J.; Janssen, I.; Tremblay, M.S. Health associations with meeting new 24-hour movement guidelines for Canadian children and youth. Prev. Med. 2017, 95, 7–13. [Google Scholar] [CrossRef]
- Kastelic, K.; Pedisic, Z.; Lipovac, D.; Kastelic, N.; Chen, S.T.; Sarabon, N. Associations of meeting 24-h movement guidelines with stress and self-rated health among adults: Is meeting more guidelines associated with greater benefits? BMC Public Health 2021, 21, 929. [Google Scholar] [CrossRef] [PubMed]
- Ayala, A.M.C.; Salmon, J.; Dunstan, D.W.; Arundell, L.; Timperio, A. Does light-intensity physical activity moderate the relationship between sitting time and adiposity markers in adolescents? J. Sport Health Sci. 2020, in press. [Google Scholar] [CrossRef]
- Lambiase, M.J.; Gabriel, K.P.; Kuller, L.H.; Matthews, K.A. Sleep and Executive Function in Older Women: The Moderating Effect of Physical Activity. J. Gerontol. Ser. A 2014, 69, 1170–1176. [Google Scholar] [CrossRef]
- Van Dyck, D.; Barnett, A.; Van Cauwenberg, J.; Zhang, C.J.P.; Sit, C.H.P.; Cerin, E. Main and interacting effects of physical activity and sedentary time on older adults’ BMI: The moderating roles of socio-demographic and environmental attributes. PLoS ONE 2020, 15, e0235833. [Google Scholar] [CrossRef] [PubMed]
- Epskamp, S.; Cramer, A.O.J.; Waldorp, L.J.; Schmittmann, V.D.; Borsboom, D. Network Visualizations of Relationships in Psychometric Data. J. Stat. Softw. 2012, 48, 1–18. [Google Scholar] [CrossRef]
- Lucena Martins, C.M.D.; Clark, C.C.T.; Ribeiro Bandeira, P.F.; Mota, J.; Duncan, M.J. Association between Compliance with the 24-Hour Movement Guidelines and Fundamental Movement Skills in Preschoolers: A Network Perspective. Int. J. Environ. Res. Public Health 2020, 17, 5443. [Google Scholar] [CrossRef] [PubMed]
- Cundiff, J.M.; Smith, T.W.; Uchino, B.N.; Berg, C.A. Subjective Social Status: Construct Validity and Associations with Psychosocial Vulnerability and Self-Rated Health. Int. J. Behav. Med. 2013, 20, 148–158. [Google Scholar] [CrossRef]
- Operario, D.; Adler, N.E.; Williams, D.R. Subjective social status: Reliability and predictive utility for global health. Psychol. Health 2004, 19, 237–246. [Google Scholar] [CrossRef]
- Macfarlane, D.J.; Lee, C.C.Y.; Ho, E.Y.K.; Chan, K.L.; Chan, D.T.S. Reliability and validity of the Chinese version of IPAQ (short, last 7 days). J. Sci. Med. Sport 2007, 10, 45–51. [Google Scholar] [CrossRef]
- Liu, X.; Tang, M.; Hu, L.; Wang, A.; Wu, H.; Zhao, G.; Gao, C.; Li, W. Reliability and validity of the Pittsburgh sleep quality index. Chin. J. Psychiatry 1996, 29, 103–107. [Google Scholar]
- Wu, W.; Zhao, A.; Szeto, I.M.Y.; Wang, Y.; Meng, L.; Li, T.; Zhang, J.; Wang, M.; Tian, Z.; Zhang, Y. Diet quality, consumption of seafood and eggs are associated with sleep quality among Chinese urban adults: A cross-sectional study in eight cities of China. Food Sci. Nutr. 2019, 7, 2091–2102. [Google Scholar] [CrossRef]
- Chi, X.; Liang, K.; Chen, S.; Huang, Q.; Huang, L.; Yu, Q.; Jiao, C.; Guo, T.; Stubbs, B.; Hossain, M.M.; et al. Mental health problems among Chinese adolescents during the COVID-19: The importance of nutrition and physical activity. Int. J. Clin. Health Psychol. 2021, 21, 100218. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Shibata, A.; Muraoka, I. Relationship between meeting the recommendations for physical activity and health-related quality of life in adult Chinese Internet users. Open J. Prev. Med. 2011, 01, 94–100. [Google Scholar] [CrossRef][Green Version]
- Zhou, S.J.; Wang, L.L.; Yang, R.; Yang, X.J.; Zhang, L.G.; Guo, Z.C.; Chen, J.C.; Wang, J.Q.; Chen, J.X. Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med. 2020, 74, 39–47. [Google Scholar] [CrossRef]
- Wang, W.; Bian, Q.; Zhao, Y.; Li, X.; Wang, W.; Du, J.; Zhang, G.; Zhou, Q.; Zhao, M. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry 2014, 36, 539–544. [Google Scholar] [CrossRef]
- Zhang, Z. Behavioral Medicine Inventory Manual; The Chinese Medicine Electronic Audio and Video Publishing House: Beijing, China, 2005. [Google Scholar]
- Li, Y.; Li, G.; Yu, M.; Liu, C.; Qu, Y.; Wu, H. Association Between Anxiety Symptoms and Problematic Smartphone Use Among Chinese University Students: The Mediating/Moderating Role of Self-Efficacy. Front. Psychiatry 2021, 12. [Google Scholar] [CrossRef]
- Yu, Y.; Hu, M.; Liu, Z.; Liu, H.; Yang, J.P.; Zhou, L.; Xiao, S. Recognition of depression, anxiety, and alcohol abuse in a Chinese rural sample: A cross-sectional study. BMC Psychiatry 2016, 16, 1–9. [Google Scholar] [CrossRef]
- Xiang, M.; Tan, X.; Sun, J.; Yang, H.; Zhao, X.; Liu, L.; Hou, X.; Hu, M. Relationship of Physical Activity With Anxiety and Depression Symptoms in Chinese College Students During the COVID-19 Outbreak. Front. Psychol. 2020, 11. [Google Scholar] [CrossRef]
- Fruchterman, T.M.J.; Reingold, E.M. Graph drawing by force-directed placement. Softw. Pr. Exp. 1991, 21, 1129–1164. [Google Scholar] [CrossRef]
- Friedman, J.; Hastie, T.; Tibshirani, R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics 2008, 9, 432–441. [Google Scholar] [CrossRef]
- Foygel, R.; Drton, M. Extended Bayesian Information Criteria for Gaussian Graphical Models. Adv. Neural Inf. Process. Syst. 2010, 23, 604–612. [Google Scholar]
- Zhai, L.; Zhang, H.; Zhang, D. Sleep duration and depression among adults: A meta-analysis of prospective studies. Depress. Anxiety 2015, 32, 664–670. [Google Scholar] [CrossRef]
- Kim, S.Y.; Shin, Y.C.; Oh, K.S.; Shin, D.W.; Lim, W.J.; Kim, E.J.; Cho, S.J.; Jeon, S.W. The association of occupational stress and sleep duration with anxiety symptoms among healthy employees: A cohort study. Stress Health 2020, 36, 675–685. [Google Scholar] [CrossRef]
- Jiang, J.; Li, Y.; Mao, Z.; Wang, F.; Huo, W.; Liu, R.; Zhang, H.; Tian, Z.; Liu, X.; Zhang, X.; et al. Abnormal night sleep duration and poor sleep quality are independently and combinedly associated with elevated depressive symptoms in Chinese rural adults: Henan Rural Cohort. Sleep Med. 2020, 70, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Palmer, C.A.; Alfano, C.A. Sleep and emotion regulation: An organizing, integrative review. Sleep Med. Rev. 2017, 31, 6–16. [Google Scholar] [CrossRef]
- Blake, M.J.; Trinder, J.A.; Allen, N.B. Mechanisms underlying the association between insomnia, anxiety, and depression in adolescence: Implications for behavioral sleep interventions. Clin. Psychol. Rev. 2018, 63, 25–40. [Google Scholar] [CrossRef]
- Patte, K.A.; Faulkner, G.; Qian, W.; Duncan, M.; Leatherdale, S.T. Are one-year changes in adherence to the 24-hour movement guidelines associated with depressive symptoms among youth? BMC Public Health 2020, 20, 1–12. [Google Scholar] [CrossRef]
- Sampasa-Kanyinga, H.; Colman, I.; Goldfield, G.S.; Janssen, I.; Wang, J.; Podinic, I.; Tremblay, M.S.; Saunders, T.J.; Sampson, M.; Chaput, J. Combinations of physical activity, sedentary time, and sleep duration and their associations with depressive symptoms and other mental health problems in children and adolescents: A systematic review. Int. J. Behav. Nutr. Phys. 2020, 17, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Werneck, A.O.; Silva, D.R.; Malta, D.C.; Souza-Júnior, P.R.B.; Azevedo, L.O.; Barros, M.B.A.; Szwarcwald, C.L. Changes in the clustering of unhealthy movement behaviors during the COVID-19 quarantine and the association with mental health indicators among Brazilian adults. Transl. Behav. Med. 2021, 11, 323–331. [Google Scholar] [CrossRef]
- Schuch, F.B.; Bulzing, R.A.; Meyer, J.; Vancampfort, D.; Firth, J.; Stubbs, B.; Grabovac, I.; Willeit, P.; Tavares, V.D.O.; Calegaro, V.C.; et al. Associations of moderate to vigorous physical activity and sedentary behavior with depressive and anxiety symptoms in self-isolating people during the COVID-19 pandemic: A cross-sectional survey in Brazil. Psychiatry Res. 2020, 292, 113339. [Google Scholar] [CrossRef]
- Sampasa-Kanyinga, H.; Colman, I.; Goldfield, G.S.; Janssen, I.; Wang, J.; Tremblay, M.S.; Barnes, J.D.; Walsh, J.J.; Chaput, J. 24-Hour Movement Behaviors and Internalizing and Externalizing Behaviors Among Youth. J. Adolesc. Health 2021, 68, 969–977. [Google Scholar] [CrossRef] [PubMed]
- Wolf, S.; Seiffer, B.; Zeibig, J.; Welkerling, J.; Brokmeier, L.; Atrott, B.; Ehring, T.; Schuch, F.B. Is Physical Activity Associated with Less Depression and Anxiety During the COVID-19 Pandemic? A Rapid Systematic Review. Sports Med. 2021, 1–13. [Google Scholar] [CrossRef]
- Richardson, D.L.; Clarke, N.D.; Broom, D.R.; Tallis, J.; Duncan, M.J. Life after lockdown: The role of sport, exercise and physical activity in ameliorating the mental health implications of COVID-19 restrictions. J. Sports Sci. 2021, 1–3. [Google Scholar] [CrossRef]
- Wright, K.P.; Linton, S.K.; Withrow, D.; Casiraghi, L.; Lanza, S.M.; Iglesia, H.D.L.; Vetter, C.; Depner, C.M. Sleep in university students prior to and during COVID-19 Stay-at-Home orders. Curr. Biol. 2020, 30, R797–R798. [Google Scholar] [CrossRef]
- Hisler, G.C.; Twenge, J.M. Sleep characteristics of U.S. adults before and during the COVID-19 pandemic. Soc. Sci. Med. 2021, 276, 113849. [Google Scholar] [CrossRef] [PubMed]
- Altena, E.; Baglioni, C.; Espie, C.A.; Ellis, J.; Gavriloff, D.; Holzinger, B.; Schlarb, A.; Frase, L.; Jernelöv, S.; Riemann, D. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of the European CBT-I Academy. J. Sleep Res. 2020, 29, e13052. [Google Scholar] [CrossRef]
- Morin, C.M.; Carrier, J.; Bastien, C.; Godbout, R. Sleep and circadian rhythm in response to the COVID-19 pandemic. Can. J. Public Health 2020, 111, 654–657. [Google Scholar] [CrossRef]
- Mello, M.T.D.; Silva, A.; Guerreiro, R.D.C.; Da-Silva, F.R.; Esteves, A.M.; Poyares, D.; Piovezan, R.; Treptow, E.; Starling, M.; Rosa, D.S.; et al. Sleep and COVID-19: Considerations about immunity, pathophysiology, and treatment. Sleep Sci. 2020, 13, 199–209. [Google Scholar] [CrossRef]
- Sabiston, C.M.; O’Loughlin, E.; Brunet, J.; Chaiton, M.; Low, N.C.; Barnett, T.; O’Loughlin, J. Linking depression symptom trajectories in adolescence to physical activity and team sports participation in young adults. Prev. Med. 2013, 56, 95–98. [Google Scholar] [CrossRef]
- Owens, J.; Adolescent, S.W.G.; Committee, O.A. Insufficient sleep in adolescents and young adults: An update on causes and consequences. Pediatrics 2014, 134, e921. [Google Scholar] [CrossRef]
- Sun, Y.; Shi, L.; Bao, Y.; Sun, Y.; Shi, J.; Lu, L. The bidirectional relationship between sleep duration and depression in community-dwelling middle-aged and elderly individuals: Evidence from a longitudinal study. Sleep Med. 2018, 52, 221–229. [Google Scholar] [CrossRef]
- Zink, J.; Ebrahimian, S.; Belcher, B.R.; Leventhal, A.M. Reciprocal associations between depression and screen-based sedentary behaviors in adolescents differ by depressive symptom dimension and screen-type. J. Affect. Disord. 2020, 263, 39–46. [Google Scholar] [CrossRef]
- Goldstein, C. Current and Future Roles of Consumer Sleep Technologies in Sleep Medicine. Sleep Med. Clin. 2020, 15, 391–408. [Google Scholar] [CrossRef]
- Kandola, A.; Lewis, G.; Osborn, D.P.J.; Stubbs, B.; Hayes, J.F. Depressive symptoms and objectively measured physical activity and sedentary behaviour throughout adolescence: A prospective cohort study. Lancet Psychiatry 2020, 7, 262–271. [Google Scholar] [CrossRef]
- Opie, R.S.; Itsiopoulos, C.; Parletta, N.; Sanchez-Villegas, A.; Akbaraly, T.N.; Ruusunen, A.; Jacka, F.N. Dietary recommendations for the prevention of depression. Nutr. Neurosci. 2016, 20, 161–171. [Google Scholar] [CrossRef] [PubMed]
| Variables | Category | n | % | Variables | Category/Range | N/M | %/SD |
|---|---|---|---|---|---|---|---|
| Gender | Male | 665 | 36.0 | Meeting the MVPA guideline | No | 950 | 51.5 |
| Female | 1181 | 64.0 | Yes | 896 | 48.5 | ||
| Family structure | Full | 1664 | 90.1 | Combinations of guidelines met | None | 119 | 6.4 |
| Divorced | 117 | 6.3 | Sleep only | 260 | 14.1 | ||
| Other | 65 | 3.5 | SB only | 168 | 9.1 | ||
| Father’s education | Middle school or below | 891 | 48.3 | MVPA only | 67 | 3.6 | |
| High school | 636 | 34.5 | Sleep + SB | 403 | 21.8 | ||
| College or university | 254 | 13.8 | Sleep + MVPA | 129 | 7.0 | ||
| Master or above | 65 | 3.5 | Sleep + MVPA | 201 | 10.9 | ||
| Mother’s education | Middle school or below | 1086 | 58.8 | Sleep + SB + MVPA | 499 | 27.0 | |
| High school | 560 | 30.3 | Depression symptoms | Minimal | 673 | 36.5 | |
| College or university | 158 | 8.6 | Mild | 738 | 40.0 | ||
| Master or above | 42 | 2.3 | Moderate | 279 | 15.1 | ||
| Number of siblings | None | 639 | 34.6 | Moderately severe | 108 | 5.9 | |
| One or more | 1207 | 65.4 | Severe | 48 | 2.6 | ||
| Number of friends | None | 29 | 1.6 | Anxiety symptoms | Minimal | 1462 | 79.2 |
| One to two | 608 | 32.9 | Mild | 277 | 15.0 | ||
| Three to five | 964 | 52.2 | Moderate | 89 | 4.8 | ||
| Six or more | 245 | 13.3 | Severe | 18 | 1.0 | ||
| Residence | Urban | 1278 | 69.2 | Variables | Range | M | SD |
| Rural | 568 | 30.8 | Age (years) | 18–26 | 20.67 | 1.61 | |
| Meeting the sleep guideline | No | 555 | 30.1 | BMI (kg/m2) | 10–44 | 20.27 | 2.88 |
| Yes | 1291 | 69.9 | Perceived family affluence | 1–10 | 5.71 | 1.64 | |
| Meeting the SB guideline | No | 575 | 31.1 | Depression symptoms | 0–27 | 6.83 | 5.19 |
| Yes | 1271 | 68.9 | Anxiety symptoms | 25–85 | 41.79 | 9.82 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liang, K.; de Lucena Martins, C.M.; Chen, S.-T.; Clark, C.C.T.; Duncan, M.J.; Bu, H.; Huang, L.; Chi, X. Sleep as a Priority: 24-Hour Movement Guidelines and Mental Health of Chinese College Students during the COVID-19 Pandemic. Healthcare 2021, 9, 1166. https://doi.org/10.3390/healthcare9091166
Liang K, de Lucena Martins CM, Chen S-T, Clark CCT, Duncan MJ, Bu H, Huang L, Chi X. Sleep as a Priority: 24-Hour Movement Guidelines and Mental Health of Chinese College Students during the COVID-19 Pandemic. Healthcare. 2021; 9(9):1166. https://doi.org/10.3390/healthcare9091166
Chicago/Turabian StyleLiang, Kaixin, Clarice Maria de Lucena Martins, Si-Tong Chen, Cain Craig Truman Clark, Michael Joseph Duncan, He Bu, Liuyue Huang, and Xinli Chi. 2021. "Sleep as a Priority: 24-Hour Movement Guidelines and Mental Health of Chinese College Students during the COVID-19 Pandemic" Healthcare 9, no. 9: 1166. https://doi.org/10.3390/healthcare9091166
APA StyleLiang, K., de Lucena Martins, C. M., Chen, S.-T., Clark, C. C. T., Duncan, M. J., Bu, H., Huang, L., & Chi, X. (2021). Sleep as a Priority: 24-Hour Movement Guidelines and Mental Health of Chinese College Students during the COVID-19 Pandemic. Healthcare, 9(9), 1166. https://doi.org/10.3390/healthcare9091166








