The Vaccination Process against the COVID-19: Opportunities, Problems and mHealth Support
Abstract
:1. Introduction
1.1. Background
1.2. Purpose of the Study
1.3. Organization of the Study
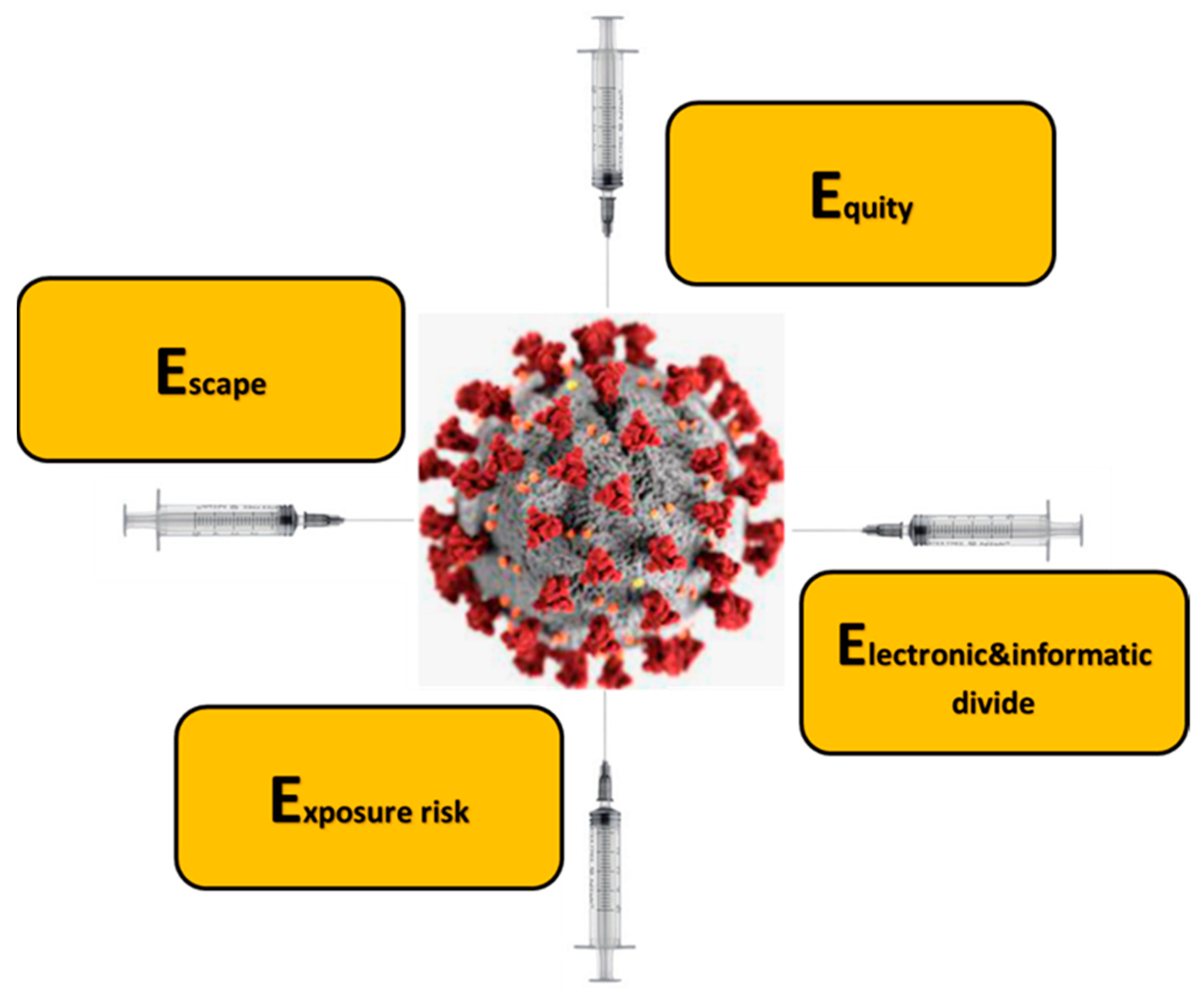
2. The Digital Divide, the Escape, the Exposure Risk, the Equity, and COVID-19
2.1. General Considerations
2.2. Electronic & Informatic Divide
2.3. Escape
2.4. Exposure Risk
2.5. Equity
3. The Role of Mobile Technology and mHealth to Fight the Problems Hampering the Process
3.1. General Considerations
3.2. Example of mTech Applications
3.3. The Usefulness of Dedicated Electronic Surveys Based on mTtech in the COVID-19 Era
3.3.1. Experiences and Considerations in the Vaccination Process
3.3.2. The Proposal and Test of an Electronic Survey
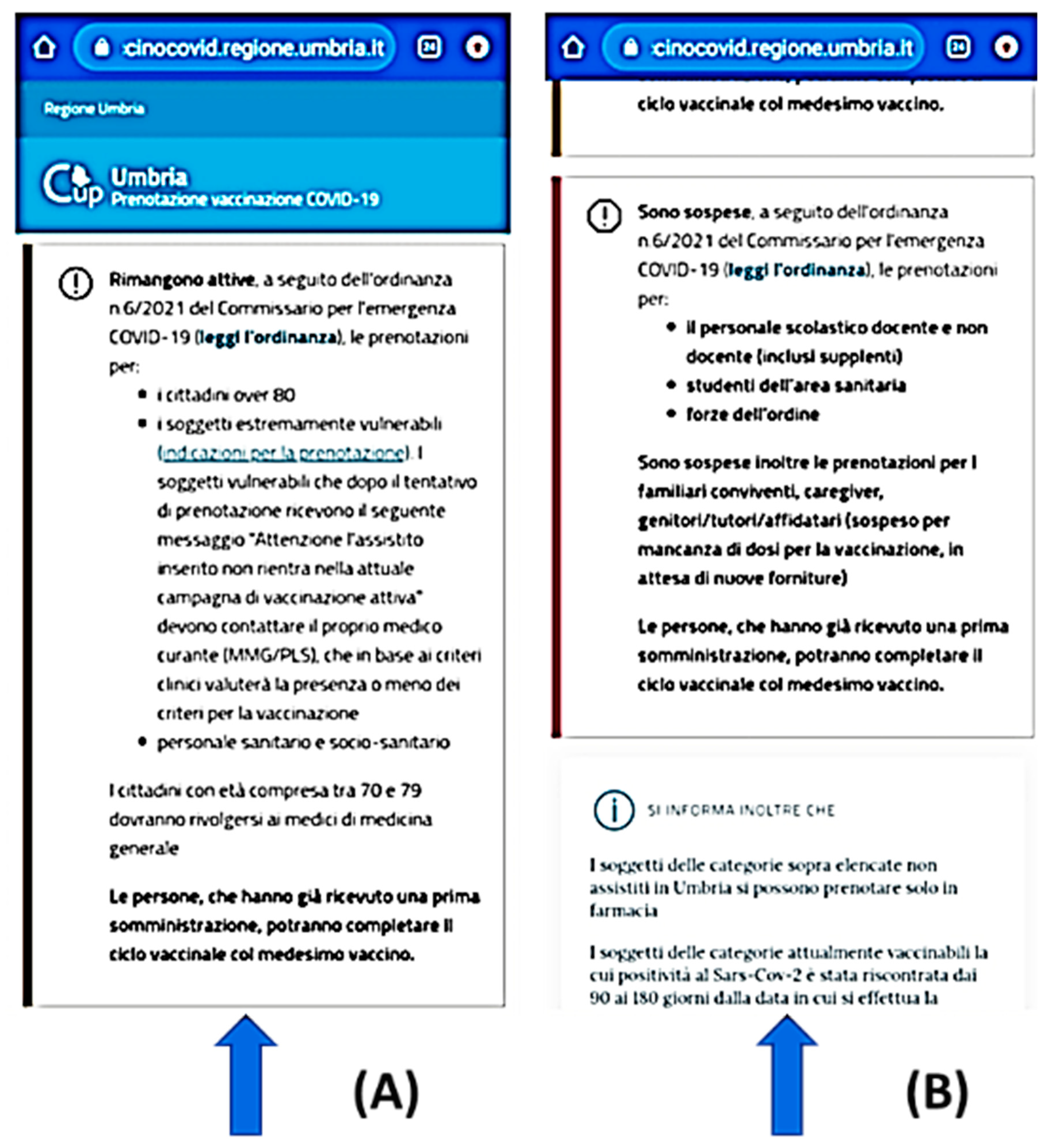
4. The mTech and the Usefulness to Optimize the Process: The Italian Example
4.1. General Considerations
4.2. An Example of the Italian Approach
5. Conclusions
5.1. Highlights
- New questions: vaccine intent. Vaccine status item enabled on 6 January 2021, 19 December 2020;
- Textual revisions to vaccine intent items 12 January 2021;
- New questions: Reasons for vaccine hesitancy, vaccine dosing Minor textual revisions 8 February 2021;
- New questions: Appointments for COVID vaccines, information about getting vac-cinated Textual revisions 2 March 2021;
5.2. Final Reflections
5.3. Final Thought
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. 2021. Available online: https://covid19.who.int/ (accessed on 18 August 2021).
- Mo, P.K.H.; Luo, S.; Wang, S.; Zhao, J.; Zhang, G.; Li, L.; Li, L.; Xie, L.; Lau, J.T.F. Intention to receive the COVID-19 vaccination in China: Application of the diffusion of innovations theory and the moderating role of openness to experience. Vaccines 2021, 9, 129. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.B.; Bell, R.A. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine 2021, 39, 1080–1086. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.A.; McFadden, S.A.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef] [PubMed]
- Luo, C.; Ji, K.; Tang, Y.; Du, Z. Exploring the Expression Differences between Professionals and Laypeople toward the COVID-19 Vaccine: A Text Mining Approach. J. Med. Internet Res. 2021, 23, e30715. [Google Scholar] [CrossRef] [PubMed]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J. SAGE Working Group on Vaccine Hesitancy. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Truong, J.; Bakshi, S.; Wasim, A.; Ahmad, M.; Majid, U. What factors promote vaccine hesitancy or acceptance during pandemics? A systematic review and thematic analysis. Health Promot. Int. 2021, daab105. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, J.; Ryan, R.; Walsh, L.; Horey, D.; Leask, J.; Robinson, P.; Hill, S. Face-to-face interventions for informing or educating parents about early childhood vaccination. Cochrane Database Syst. Rev. 2018, 5, CD010038. [Google Scholar] [CrossRef]
- Giansanti, D. The Role of the mHealth in the Fight against the Covid-19: Successes and Failures. Healthcare 2021, 9, 58. [Google Scholar] [CrossRef]
- van Deursen, A.J.; van Dijk, J.A. The first-level digital divide shifts from inequalities in physical access to inequalities in material access. New Media Soc. 2019, 21, 354–375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neter, E.; Brainin, E.; Baron-Epel, O. Group differences in health literacy are ameliorated in ehealth literacy. Health Psychol. Behav. Med. 2021, 9, 480–497. [Google Scholar] [CrossRef] [PubMed]
- Van Deursen, A.J.; Helsper, E.J. Collateral benefits of Internet use: Explaining the diverse outcomes of engaging with the Internet. New Media Soc. 2018, 20, 2333–2351. [Google Scholar] [CrossRef] [Green Version]
- Giansanti, D.; Veltro, G. The Digital Divide in the Era of COVID-19: An Investigation into an Important Obstacle to the Access to the mHealth by the Citizen. Healthcare 2021, 9, 371. [Google Scholar] [CrossRef] [PubMed]
- Gabbiadini, A.; Baldissarri, C.; Durante, F.; Valtorta, R.R.; De Rosa, M.; Gallucci, M. Together Apart: The Mitigating Role of Digital Communication Technologies on Negative Affect during the COVID-19 Outbreak in Italy. Front. Psychol. 2020, 11, 554678. [Google Scholar] [CrossRef]
- Shah, S.G.S.; Nogueras, D.; Van Woerden, H.C.; Kiparoglou, V. The COVID-19 Pandemic—A pandemic of lockdown loneliness and the role of digital technology: A viewpoint (Preprint). J. Med. Internet Res. 2020, 22, e22287. [Google Scholar] [CrossRef] [PubMed]
- Kondylakis, H.; Katehakis, D.G.; Kouroubali, A.; Logothetidis, F.; Triantafyllidis, A.; Kalamaras, I.; Votis, K.; Tzovaras, D. COVID-19 Mobile Apps: A Systematic Review of the Literature. J. Med. Internet Res. 2020, 22, e23170. [Google Scholar] [CrossRef]
- Lai, J.; Widmar, N.O. Revisiting the Digital Divide in the COVID-19 Era. Appl. Econ. Perspect. Policy 2020, 43, 458–464. [Google Scholar] [CrossRef]
- Shek, D.T.L. COVID-19 and Quality of Life: Twelve Reflections. Appl. Res. Qual. Life 2021, 16, 1–11. [Google Scholar] [CrossRef]
- L’app dei Servizi Pubblici. Available online: https://io.italia.it/ (accessed on 18 August 2021).
- Robertson, E.; Reeve, K.S.; Niedzwiedz, C.L.; Moore, J.; Blake, M.; Green, M.; Katikireddi, S.V.; Benzeval, M.J. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav. Immun. 2021, 94, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, R.G.; Hagen, L.; Walker, K.; O’Leary, H.; Lengacher, C. The COVID-19 vaccine social media infodemic: Healthcare providers’ missed dose in addressing misinformation and vaccine hesitancy. Hum. Vaccines Immunother. 2021, 23, 1–3. [Google Scholar] [CrossRef]
- Buckner, J.H.; Chowell, G.; Springborn, M.R. Dynamic prioritization of COVID-19 vaccines when social distancing is limited for essential workers. Proc. Natl. Acad. Sci. USA 2021, 118, e2025786118. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.T.; Kahn, J.; Kachalia, A. Who Goes First? Government Leaders and of SARS-CoV-2 Vaccines. N. Engl. J. Med. 2021, 384, e15. [Google Scholar] [CrossRef] [PubMed]
- Buckner, J.H.; Chowell, G.; Springborn, M.R. Optimal Dynamic Prioritization of COVID-19 Vaccines. medRxiv 2020. [Google Scholar] [CrossRef]
- June, Y.C.; Hwichang, J.; Philippe, B.; Norio, O.; Yongdai, K. View ORCID ProfileShinya Tsuzuki COVID-19 Vaccine Prioritisation in Japan and South Korea. medRxiv 2021. [Google Scholar] [CrossRef]
- Joint Action Health Equity Europe. Available online: https://jahee.iss.it/ (accessed on 18 August 2021).
- Centers for Disease Control and Prevention. Health Equity—Promoting Fair Access to Health. Available online: https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/index.html (accessed on 18 August 2021).
- Centers for Disease Control and Prevention. CDC COVID-19 Response Health Equity Strategy: Accelerating Progress Towards Reducing COVID-19 Disparities and Achieving Health Equity. Available online: https://www.cdc.gov/coronavirus/2019-ncov/downloads/community/CDC-Strategy.pdf (accessed on 18 August 2021).
- Osama, T.; Razai, M.S.; Majeed, A. Covid-19 vaccine passports: Access, equity, and ethics. BMJ 2021, 373, n861. [Google Scholar] [CrossRef] [PubMed]
- Martin, E.G.; Birkhead, G.S.; Holtgrave, D.R. Maintaining a Focus on Health Equity during the COVID-19 Vaccine Rollout. J. Public Health Manag. Pract. 2021, 27, 226–228. [Google Scholar] [CrossRef] [PubMed]
- So, A.D.; Woo, J. Achieving path-dependent equity for global COVID-19 vaccine allocation. Med 2021, 2, 373–377. [Google Scholar] [CrossRef]
- Goldstein, A. Failure to achieve global vaccine equity will have dire consequences. BMJ 2021, 372, n712. [Google Scholar] [CrossRef] [PubMed]
- Tarzian, A.J.; Geppert, C.M.A. The Veterans Health Administration Approach to COVID-19 Vaccine Allocation-Balancing Utility and Equity. Fed. Pract. 2021, 38, 52–54. [Google Scholar] [CrossRef]
- Franco-Paredes, C.; Suarez, J.A.; Henao-Martínez, A.F. Global COVID-19 vaccine equity should precede requiring travelers proof of vaccination. Int. J. Infect. Dis. 2021, 105, 243–244. [Google Scholar] [CrossRef]
- Pepperrell, T.; Rodgers, F.; Tandon, P.; Sarsfield, K.; Pugh-Jones, M.; Rashid, T.; Keestra, S. Making a COVID-19 vaccine that works for everyone: Ensuring equity and inclusivity in clinical trials. Glob. Health Action. 2021, 14, 1892309. [Google Scholar] [CrossRef] [PubMed]
- Bell, K.J.L.; Glasziou, P.; Stanaway, F.; Bossuyt, P.; Irwig, L. Equity and evidence during vaccine rollout: Stepped wedge cluster randomised trials could help. BMJ 2021, 372, n435. [Google Scholar] [CrossRef] [PubMed]
- Jean-Jacques, M.; Bauchner, H. Vaccine Distribution-Equity Left Behind? JAMA 2021, 325, 829–830. [Google Scholar] [CrossRef] [PubMed]
- Modi, N.; Ayres-de-Campos, D.; Bancalari, E.; Benders, M.; Briana, D.; Di Renzo, G.C.; Fonseca, E.B.; Hod, M.; Poon, L.; Cortes, M.S.; et al. Equity in coronavirus disease 2019 vaccine development and deployment. Am. J. Obs. Gynecol. 2021, 224, 423–427. [Google Scholar] [CrossRef]
- Todd, A.; Bambra, C. Learning from past mistakes? The COVID-19 vaccine and the inverse equity hypothesis. Eur. J. Public Health 2021, 31, 2. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H. SARS-CoV-2 vaccine development, access, and equity. J. Exp. Med. 2020, 217, e20201288. [Google Scholar] [CrossRef]
- Kupferschmidt, K. Global plan seeks to promote vaccine equity, spread risks. Science 2020, 369, 489–490. [Google Scholar] [CrossRef]
- Kobayashi, T.; Nishina, Y.; Tomoi, H.; Harada, K.; Tanaka, K.; Matsumoto, E.; Horimukai, K.; Ishihara, J.; Sasaki, S.; Inaba, K.; et al. Corowa-kun: Impact of a COVID-19 vaccine information1 chatbot on vaccine hesitancy, Japan 2021. medRxiv 2021. [Google Scholar] [CrossRef]
- Pandey, R.; Gautam, V.; Pal, R.; Bandhey, H.; Dhingra, L.S.; Sharma, H.; Jain, C.; Bhagat, K.; Arushi; Patel, L.; et al. A Machine Learning Application for Raising WASH Awareness in the Times of COVID-19 Pandemic. arXiv 2020, arXiv:2003.07074. [Google Scholar]
- Ansa IT Economia. Available online: https://www.ansa.it/bannernews/notizie/breaking_news_eco/2020/12/18/-manovra-un-cellulare-per-1-anno-con-isee-sotto-20mila-euro-_14e1c456-f1f4-4630-9cc5-ff8ab26d596c.html (accessed on 18 August 2021).
- Istituto Superiore di Sanità. Available online: https://www.iss.it/covid19-fake-news (accessed on 18 August 2021).
- Hengchen, D.; Saccardo, S.; Han, M.; Roh, L.; Raja, N.; Vangala, S.; Modi, H.; Pandya, S.; Sloyan, M.; Croymans, D.M. Behavioral nudges increase COVID-19 vaccinations: Two randomized controlled trials. Nature 2021. [Google Scholar] [CrossRef]
- Reddick, C.G.; Enriquez, R.; Harris, R.J.; Sharma, B. Determinants of broadband access and affordability: An analysis of a community survey on the digital divide. Cities 2020, 106, 102904. [Google Scholar] [CrossRef] [PubMed]
- Fatmi, Z.; Mahmood, S.; Hameed, W.; Qazi, I.; Siddiqui, M.; Dhanwani, A.; Siddiqi, S. Knowledge, attitudes and practices towards COVID-19 among Pakistani residents: Information access and low literacy vulnerabilities. East. Mediterr. Health J. 2020, 26, 1446–1455. [Google Scholar] [CrossRef]
- Bonal, X.; González, S. The impact of lockdown on the learning gap: Family and school divisions in times of crisis. Int. Rev. Educ. 2020, 66, 635–655. [Google Scholar] [CrossRef]
- Campos-Castillo, C.; Laestadius, L.I. Racial and Ethnic Digital Divides in Posting COVID-19 Content on Social Media among US Adults: Secondary Survey Analysis. J. Med. Internet Res. 2020, 22, e20472. [Google Scholar] [CrossRef]
- Campos-Castillo, C.; Anthony, D. Racial and ethnic differences in self-reported telehealth use during the COVID-19 pandemic: A secondary analysis of a US survey of internet users from late March. J. Am. Med. Inform. Assoc. 2021, 28, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Salomon, J.A.; Reinhart, A.; Bilinski, A.; Chua, E.J.; La Motte-Kerr, W.; Rönn, M.; Reitsma, M.; Morris, K.A.; LaRocca, S.; Farag, T.; et al. The U.S. COVID-19 Trends and Impact Survey, 2020–2021: Continuous real-time measurement of COVID-19 symptoms, risks, protective behaviors, testing and vaccination. MedRxiv 2021. [Google Scholar] [CrossRef]
- A Survey on Your Opinion on the Vaccination Process. Available online: https://forms.office.com/Pages/ResponsePage.aspx?id=_ccwzxZmYkutg7V0sn1ZEvPNtNci4kVMpoVUounzQ3tURURYQ0lCVlc3TVlHSjlXVEFBRVEwM0ZFNS4u (accessed on 18 August 2021).
- Partecipa al Cashback con L’app IO. Available online: https://io.italia.it/cashback/ (accessed on 18 August 2021).
- Bonato, P. Wearable sensors/systems and their impact on biomedical engineering. IEEE Eng. Med. Boil. Mag. 2003, 22, 18–20. [Google Scholar] [CrossRef]
- Moss, R.J.; Süle, A.; Kohl, S. eHealth and mHealth. Eur. J. Hosp. Pharm. 2019, 26, 57–58. [Google Scholar] [CrossRef] [Green Version]
- Bashshur, R.; Doarn, C.R.; Frenk, J.M.; Kvedar, J.C.; Woolliscroft, J.O. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed. e-Health 2020, 26, 571–573. [Google Scholar] [CrossRef] [Green Version]
- Pollmann, T.R.; Schönert, S.; Müller, J.; Pollmann, J.; Resconi, E.; Wiesinger, C.; Haack, C.; Shtembari, L.; Turcati, A.; Neumair, B.; et al. The impact of digital contact tracing on the SARS-CoV-2 pandemic-a comprehensive modelling study. EPJ Data Sci. 2021, 10, 37. [Google Scholar] [CrossRef] [PubMed]
- Yousuf, H.; van der Linden, S.; Bredius, L.; Ted van Essen, G.A.; Sweep, G.; Preminger, Z.; van Gorp, E.; Scherder, E.; Narula, J.; Hofstra, L. A media intervention applying debunking versus non-debunking content to combat vaccine misinformation in elderly in the Netherlands: A digital randomised trial. EClinicalMedicine. 2021, 35, 100881. [Google Scholar] [CrossRef] [PubMed]
- Duch, R.M.; Barnett, A.; Filipek, M.; Roope, L.; Violato, M.; Clarke, P. Cash versus Lotteries: COVID-19 Vaccine Incentives Experiment. medRxiv 2021. [Google Scholar] [CrossRef]
- Walker, K.K.; Head, K.J.; Owens, H.; Zimet, G.D. A qualitative study exploring the relationship between mothers’ vaccine hesitancy and health beliefs with COVID-19 vaccination intention and prevention during the early pandemic months. Hum. Vaccines Immunother. 2021, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Auslander, B.A.; Meers, J.M.; Short, M.B.; Zimet, G.D.; Rosenthal, S.L. A qualitative analysis of the vaccine intention-behaviour relationship: Parents’ descriptions of their intentions, decision-making behaviour and planning processes towards HPV vaccination. Psychol. Health 2019, 34, 271–288. [Google Scholar] [CrossRef]
- Mollema, L.; Staal, J.M.; van Steenbergen, J.E.; Paulussen, T.G.; de Melker, H.E. An exploratory qualitative assessment of factors influencing childhood vaccine providers’ intention to recommend immunization in the Netherlands. BMC Public Health 2012, 12, 128. [Google Scholar] [CrossRef] [Green Version]
- Ajovalasit, S.; Dorgali, V.M.; Mazza, A.; d’Onofrio, A.; Manfredi, P. Evidence of disorientation towards immunization on online social media after contrasting political communication on vaccines. Results from an analysis of Twitter data in Italy. PLoS ONE 2021, 16, e0253569. [Google Scholar] [CrossRef]


| Opinion on: | Averaged Grade |
|---|---|
| The survey is capable to face aspects of equity, exposure risk, electronic and informatic divide, escape. | 5.1 |
| The survey is user-friendly. | 4.9 |
| The survey is clear. | 4.8 |
| The survey is fast in the operations. | 4.9 |
| The survey runs well | 4.9 |
| The survey is useful for the government | 5.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simeoni, R.; Maccioni, G.; Giansanti, D. The Vaccination Process against the COVID-19: Opportunities, Problems and mHealth Support. Healthcare 2021, 9, 1165. https://doi.org/10.3390/healthcare9091165
Simeoni R, Maccioni G, Giansanti D. The Vaccination Process against the COVID-19: Opportunities, Problems and mHealth Support. Healthcare. 2021; 9(9):1165. https://doi.org/10.3390/healthcare9091165
Chicago/Turabian StyleSimeoni, Rossella, Giovanni Maccioni, and Daniele Giansanti. 2021. "The Vaccination Process against the COVID-19: Opportunities, Problems and mHealth Support" Healthcare 9, no. 9: 1165. https://doi.org/10.3390/healthcare9091165
APA StyleSimeoni, R., Maccioni, G., & Giansanti, D. (2021). The Vaccination Process against the COVID-19: Opportunities, Problems and mHealth Support. Healthcare, 9(9), 1165. https://doi.org/10.3390/healthcare9091165






