1. Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HCT) is a potentially curative treatment option for several malignant and non-malignant hematologic diseases. Increasing availability of donors and procedural improvements, including immunosuppression, prophylaxis, and treatment of infections, have contributed to the improved outcome of this treatment modality over the last few decades [
1,
2,
3,
4].
The introduction of reduced-intensity conditioning (RIC) and non-myeloablative conditioning regimens have made transplantation of older, frail, and more severely ill patients feasible [
5,
6,
7,
8]. While allo-HCT reduces the risk of relapse of underlying malignancy compared with other conventional therapies, it is associated with a significant risk of toxicity and non-relapse mortality (NRM), which may outweigh the benefits [
9]. Therefore, the decision whether to recommend HCT or not requires careful consideration of those factors. Relapse risk is mainly driven by disease biology and remission status at transplant, while NRM is strongly driven by patient fitness and comorbidities [
10,
11]. Over the past few decades, several scores have been developed for the prediction of NRM risk taking into account patient-related, disease-related, or combined parameters [
12,
13,
14,
15,
16,
17,
18], the HCT Comorbidity Index (HCT-CI) being the most commonly used [
13].
The HCT-CI, which builds on the Charlson Comorbidity Index (CCI), further defines transplant-specific risks that can be partially objectified, with the goal of predicting two-year NRM. Three risk groups were identified by the HCT-CI score: 0 points, low risk; 1–2 points, intermediate risk; and 3 points, high risk. The corresponding two-year NRM rates are 14%, 21%, and 41%, respectively [
13]. The HCT-CI has been repeatedly adjusted by adding parameters such as age with a cut-off at 40 years (HCT-CI/age), ferritin, albumin, and platelets (augmented HCT-CI) or combinations of augmented HCT-CI, age risk groups, as well as cytogenetic and molecular risk groups (AML composite model, AML-CM) [
19,
20,
21]. Although being well established in clinical practice, the HCT-CI is limited by subjective user interpretation and the need for a detailed, sometimes patient-reported, medical history. Furthermore, the 40 years cut-off of the HCT-CI/age is not representative of current transplant practice, where the median patient age became much higher [
22,
23]. Other widely used scores do not focus on comorbidities: the EBMT score includes patient and donor factors, the endothelial activation and stress index (EASIX) uses a formula reflecting endothelial dysfunction, while the Dana–Farber Cancer Institute (DFCI) score focuses on disease risk factors [
14,
15,
17].
This study set out to identify objectifiable patient-related, comorbidity-associated parameters that impact the risk of NRM and use them to create a concise tool for the prediction of patient outcome after allo-HCT.
3. Results
In the training cohort, 119 patients experienced the event of NRM, while 167 patients had relapse of underlying malignancy. The median survival time for the entire cohort was 1673 days. Death occurred in 234 patients, and the median survival time among the patients who died was 154 days.
3.1. Patient-Specific Risk Score
The univariate analysis included more than 20 patient-related parameters (
Supplementary Table S1). Factors with
p < 0.1 in univariate analysis were then entered into the multivariate model and weighted according to the associated hazard ratios, as described in the methods section (
Table 1 and
Table 2). Factors that did not impact NRM risk were removed through stepwise backward elimination. This was the case for the factors NT-proBNP and CMV-status. Accordingly, serum albumin < 20 g/L was assigned a weighted score of 3. Serum creatinine > 1.5xULN and age above 70 years were assigned a score of 2. A score of 1 was assigned to serum albumin < LLN–20 g/L, serum creatinine > ULN–1.5xULN, left ventricular ejection fraction (LVEF) ≤ 50%, forced expiratory volume (FEV1) < 60%, vital capacity (VC) < 75%, C-reactive protein (CRP) ≥ 6 mg/L, and age 60–69 years.
The sum of the weighted scores assigned to each patient in the training cohort ranged from 0 to 9 points, with rising scores indicating a higher NRM risk. Patients with a score of 0 or 1 points had the lowest two-year (2yr) NRM rates at 12% and 7%, respectively. Forty percent of the patients in the training set could be assigned to score 0 or 1. Patients who achieved two and three points had 2yr NRM rates of 22% and 19%, respectively. They accounted for 25% and 18% of the patients in the training set, respectively. Nine percent of patients from the training cohort had four points or at least five points. With four points, a two-year NRM of 28% was seen, whereas five or more points was associated with the highest NRM of 46% (
Supplementary Table S2).
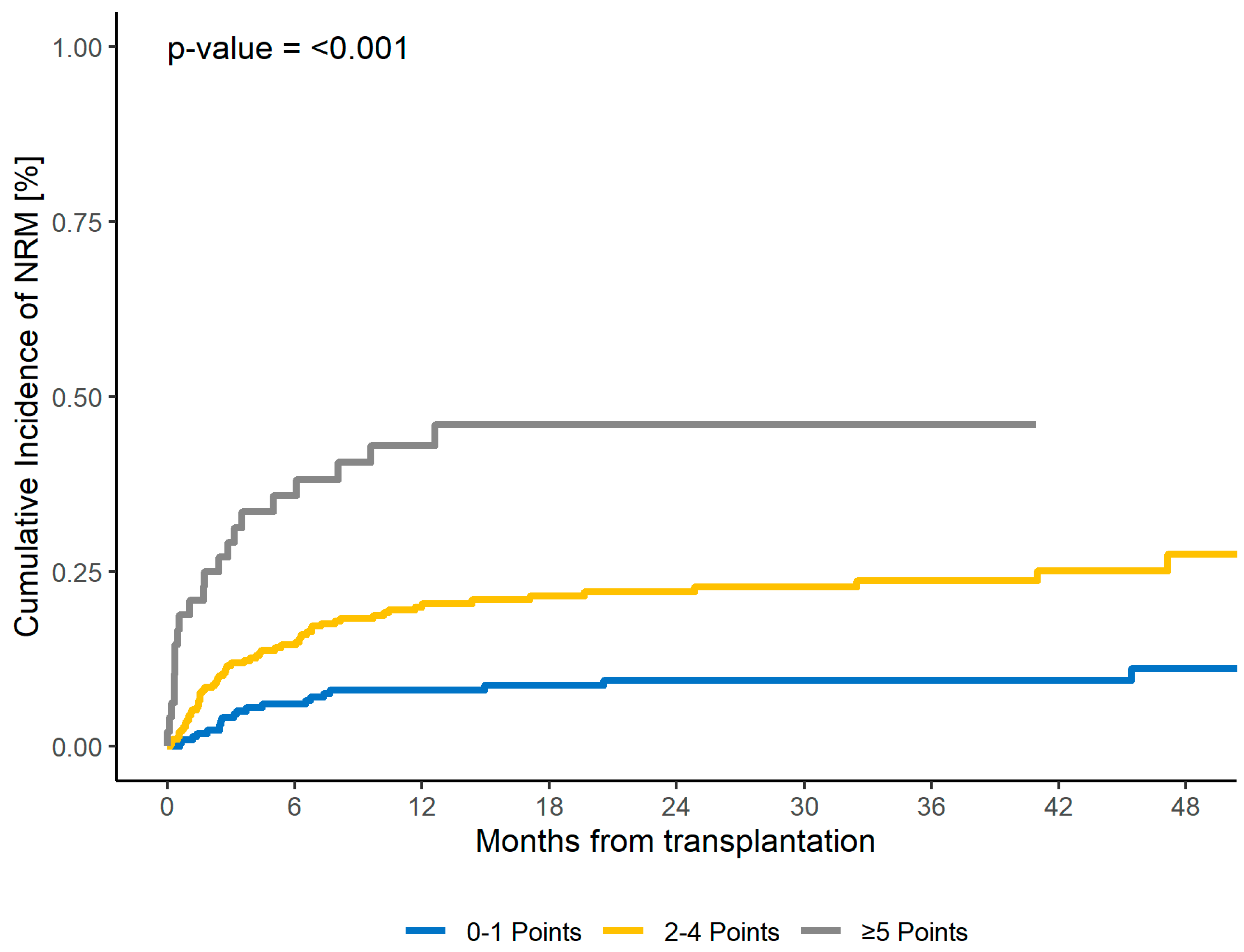
Three risk groups were identified based on the sum of points, suggesting a possible three-point risk score (CORE HCT) that differentiates the risk groups as follows: low risk with zero or one point, intermediate risk with two, three, or four points, and high risk with at least five points. The corresponding NRM rates were 9% for the low-risk group, 22% for the intermediate-risk group, and 46% for the high-risk group. The CORE HCT risk score was predictive for 2yr NRM both in the training cohort (
p < 0.001) and in the first validation cohort (
p < 0.001) (
Table 3 and
Table 4,
Figure 1,
Supplementary Figure S1). Subsequently, the c-statistics for NRM were evaluated for the first validation cohort, revealing a value of 0.63 (SE 0.04,
p = 0.003).
3.2. Survival and Relapse
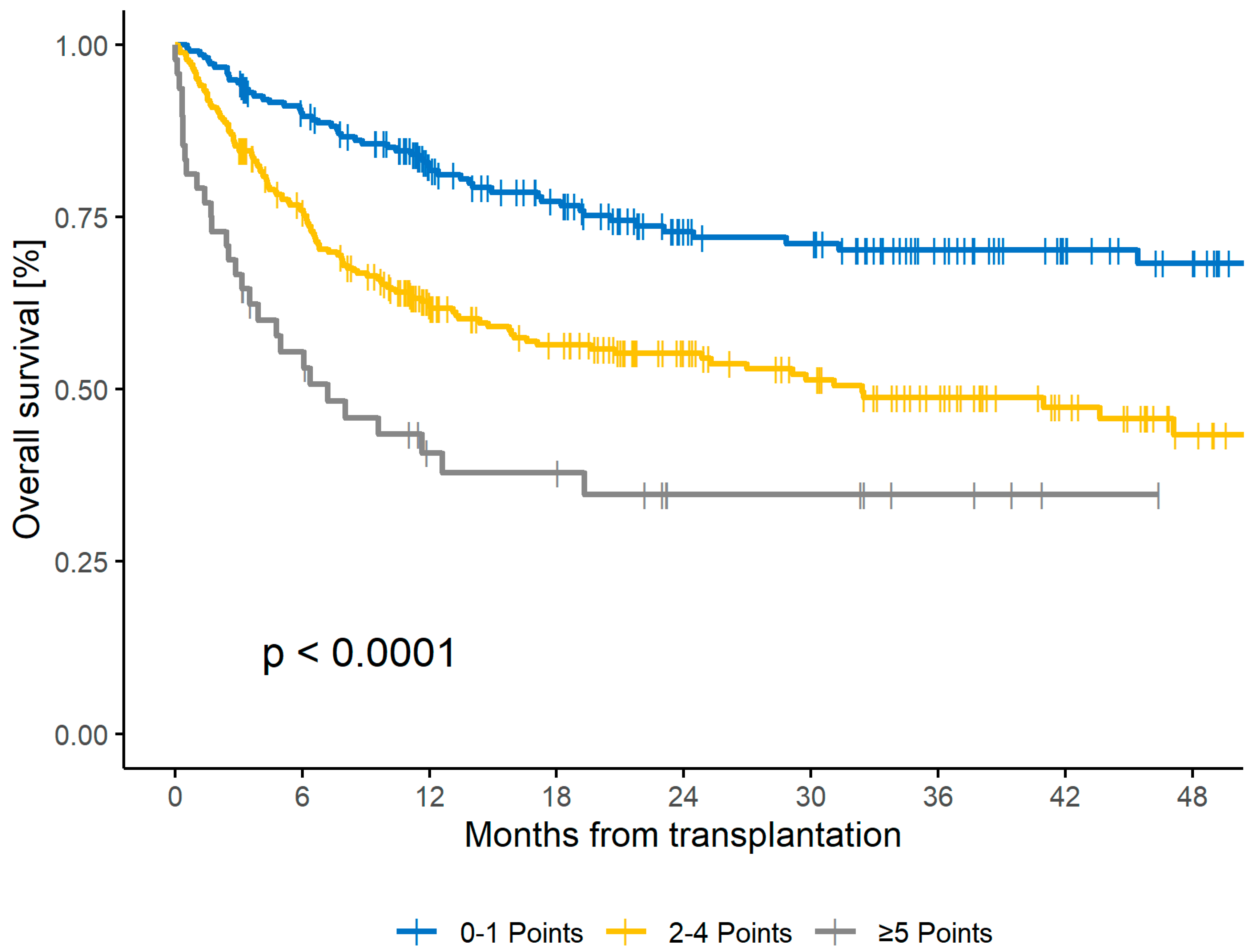
Accordingly, the CORE HCT score was also predictive for OS. The corresponding 2yr OS rates for low-, intermediate-, and high-risk scores were 73%, 55%, and 35%, respectively (
p < 0.001), in the training set and 73%, 47%, and 18%, respectively (
p < 0.001), in the first validation set (
Figure 2 and
Supplementary Figure S2). The C-statistics for OS in the first validation cohort were 0.659 (SE 0.03,
p < 0.001). Regarding relapse rates, no significant influence (
p = 0.243) was seen in the training cohort. For the low-, intermediate-, and high-risk groups, the two-year relapse incidences were 27%, 31%, and 16%, respectively.
3.3. Second Validation
Patients in the 2013–2018 cohort were randomly assigned to a training cohort to construct the score and a first validation cohort to check for consistency. For further validation, a more recently treated cohort of 205 patients who underwent allo-HCT between 2019 and 2020 was analyzed. In this group, NRM was seen in 33 cases, while 52 patients experienced disease relapse. The cohort had a median survival time of 904 days. There were 71 cases of mortality, with the median survival time for individuals who experienced death being 174 days. The CORE HCT score was also predictive for two-year NRM and two-year OS in this second validation cohort, with
p = 0.002 and
p < 0.001, respectively (
Table 5,
Supplementary Table S3, and Supplementary Figures S3 and S4). The c-statistics in this cohort for NRM and OS were 0.666 (SE 0.05,
p = 0.001) and 0.675 (SE 0.039,
p < 0.001), respectively.
Next, for comparison, the impact of HCT-CI on NRM was analyzed in this patient cohort. The distribution of risk groups indicated that 13% of patients were classified as low risk, 26% as intermediate risk, and 61% as high risk. The corresponding two-year NRM rates for these groups were 30%, 16%, and 16%, respectively (p = 0.249), and the two-year OS rates were 64%, 73%, and 60%, respectively (p = 0.29). The C-statistics for NRM and OS were 0.431 (SE 0.057, p = 0.223) and 0.535 (SE 0.042, p = 0.411), respectively.
3.4. CORE Score Subgroup Analysis
After demonstrating the ability of the CORE HCT score to predict NRM and OS outcome in all three cohorts, analysis of the subgroups was performed. For this, patients with complete data sets from the training and the two validation cohorts were included (
n = 1025). The CORE HCT score predicted NRM in patients who received myeloablative conditioning (MAC,
n = 583,
p < 0.001), reduced-intensity conditioning (RIC,
n = 442,
p < 0.001), had received ATG (
n = 828,
p < 0.001), had conditioning without ATG (
n = 197,
p < 0.001), with underlying disease AML (
n = 397,
p < 0.001), MDS (
n = 150,
p = 0.027), myelofibrosis (
n= 133,
p = 0.003), had transplants from matched related donors, MRD (
n = 205,
p < 0.001), unrelated donors (
n = 793,
p < 0.001), and haploidentical related donors (
n = 27,
p = 0.046). The results of subgroup analysis are summarized in
Supplementary Table S4 and Supplementary Figures S5–S8.
3.5. Multivariate Analysis for NRM including Donor- and Transplant-Related Factors
We next studied the impact of the CORE HCT score in a multivariate analysis model including donor- and transplant-related factors and all patients with available data from the entire cohort (
n = 931). The CORE HCT score maintained high significance, with HR of 2.06 (95% CI: 1.4–3.1,
p < 0.001) and 5.09 (95% CI: 2.9–8.9,
p < 0.001) for intermediate and high risk compared with low risk, respectively. Interestingly, Eastern Cooperative Oncology Group (ECOG) 3–4 was independently associated with a higher risk of NRM compared with ECOG 1–2 (HR: 2.05; 95% CI: 1.4–3.1;
p < 0.001). Other borderline significant parameters included the absence ATG in conditioning (HR: 1.52; 95% CI: 1–2.3;
p = 0.049), patient CMV seropositive status (HR: 1.41; 95% CI: 1–2;
p = 0.041), and HLA-mismatched unrelated donor transplant (HR: 1.68; 95% CI: 1–2.8;
p = 0.044) (
Supplementary Tables S5 and S6, Supplementary Figure S9). The C-statistic for the combined score of CORE HCT score and ECOG was 0.675 (SE 0.024,
p < 0.001). In comparison, the CORE HCT score for all three cohorts showed a similar c-statistic of 0.648 (SE 0.022,
p < 0.001).
4. Discussion
This study identified patient-related, comorbidity-associated factors that are associated with an increased risk of NRM. The factors reflect and quantify the functions of the key organs of the lungs, heart, and kidneys, as well as inflammation and patient age, which can all be easily identified by objectifiable laboratory or functional tests. Both VC and FEV1 were independently significantly associated with worse outcomes, emphasizing a central role of lung function in overall patient fitness. Our study demonstrates that a score consisting of the seven factors serum albumin, serum creatinine, CRP, LVEF, VC, FEV1, and age can predict the NRM and OS of patients undergoing allo-HCT. The score can be calculated in a straightforward manner in clinical routine and relies on concise objectifiable parameters that are well-documented during transplant procedures and thus also available for retrospective analysis.
Although biological fitness, rather than patient age alone, is crucial for treatment decisions, age is still a major influence factor on outcome after allo-HCT [
24,
25,
26,
27]. To take into account the increasing age of transplant patients, cut-offs at 60 and 70 years were used in our study, differing from the 40 years cut-off in the HCT-CI score [
19,
22].
With the proposed three CORE HCT risk groups, most patients can be assigned to the low- (39%) and intermediate- (52%) risk groups, showing distinct NRM rates with 11–13% absolute difference in the training, first, and second validation cohorts. This may present a further advantage compared with the HCT-CI score, in which only a 7% absolute difference (14% vs. 21%) was seen between the low- and intermediate-risk groups [
13]. The CORE HCT high-risk group accounted for only 9% of the entire population and identified a small, but further distinct risk population. This reflects current transplant practice, whereby only a small fraction of patients with very high risk of NRM undergo the procedure.
The HCT-CI assigns patients to the high-risk group (28% of patients in the initial cohort) if they have three or more points, which is the case when patients, for example, have a single factor, such as a prior solid tumor requiring therapy or corrected diffusing capacity for carbon monoxide (DLCOc) < 66% [
13]. The treatment practice and outcome of solid tumors have evolved since 2005, including less aggressive strategies. Consequently, due to the assumed high risk of NRM, patients or treating physicians could reject allo-HCT as treatment option.
In our analysis of the most recently treated patient cohort, we observed no significant correlation between HCT-CI risk groups and NRM or OS. The HCT-CI high-risk group included a rather high proportion of patients (61%) and exhibited a relatively low 2yr NRM rate (16%). The primary factor contributing to the high-risk category was severe pulmonary impairment, particularly a decline in DLCOc, which was prevalent in 73% of high-risk patients in our cohort. Other studies have identified severe pulmonary impairments as the main factor contributing to high-risk HCT-CI scores [
13,
28,
29,
30]. The CORE score also includes two lung function parameters (FEV1 and VC), highlighting the importance of pulmonary fitness. However, DLCO and DLCOc did not show a significant impact on NRM in our cohort (
Supplementary Table S7). These findings suggest that either HCT-CI places excessive emphasis on DLCO and/or that DLCO is not the most suitable measure for evaluating pulmonary comorbidity in our patient population.
The multivariate analysis including the CORE HCT score and donor and transplant characteristics showed that ECOG and CORE are independent factors impacting outcome. Other significant factors included absent ATG in conditioning, patient CMV seropositive status, and HLA-mismatched unrelated donor transplants. Owing to its subjective character, we chose not to include ECOG in the CORE score, but consider it complementary. The combination of CORE HCT score and ECOG (
Table 6 and
Supplementary Figure S9) did not improve discrimination, as evidenced by the similar c-statistics of 0.675 vs. 0.648 for CORE and ECOG vs. CORE alone, respectively.
Our study is limited by weaknesses inherent to its retrospective character. The parameters included in the CORE HCT score are, however, precise, objectifiable, and well-documented in patient files. Another constraint in our study lies in the exclusive reliance on data from a singular transplantation center, with both validation cohorts originating from the same center, although the second validation cohort is enriched with the most recent data. Ongoing efforts are dedicated to external validation with comparison of the CORE HCT score and other well-established risk scores.
Though the c-statistics yielded moderate results (0.648), probably due to the complex interplay of numerous (also patient-independent) parameters influencing the outcomes of NRM and OS, these results are comparable to those of the initial publication of the HCT-CI score (0.661) and perform better than the HCT-CI in the second validation cohort [
13].