Abstract
One of the many consequences of climate change is an increase in the frequency, severity, and, thus, impact of wildfires across the globe. The destruction and loss of one’s home, belongings, and surrounding community, and the threat to personal safety and the safety of loved ones can have significant consequences on survivors’ mental health, which persist for years after. The objective of this scoping review was to identify primary studies examining the impact of wildfires on mental health and to summarize findings for PTSD, depression, anxiety, and substance use. Literature searches on Pubmed and Embase were conducted in February and April of 2021, respectively, with no date restrictions. A total of 254 studies were found in the two database searches, with 60 studies meeting the inclusion criteria. Three other studies were identified and included based on relevant in-text citations during data abstraction. The results show an increased rate of PTSD, depression, and generalized anxiety at several times of follow-up post-wildfire, from the subacute phase, to years after. An increased rate of mental health disorders post-wildfire has been found in both the adult and pediatric population, with a number of associated risk factors, the most significant being characteristics of the wildfire trauma itself. Several new terms have arisen in the literature secondary to an increased awareness and understanding of the impact of natural disasters on mental health, including ecological grief, solastalgia, and eco-anxiety. There are a number of patient factors and systemic changes that have been identified post-wildfire that can contribute to resilience and recovery.
1. Introduction
Warmer temperatures, longer summers, and blistering heat waves are all consequences of climate change and contributing factors to an increasing awareness and incidence of wildfires [1]. The three key ingredients necessary to start a fire are heat, oxygen, and fuel [2]. Consequences of climate change include warmer temperatures and changes in wind speed and rainfall patterns, the very factors necessary for wildfire ignition and propagation [3]. The World Health Organization (WHO) estimates that wildfires and volcanic activities impacted 6.2 million people globally from 1998 to 2017 [4]. Current statistics reveal an ongoing significant impact of wildfires across the globe. For example, in 2020, the United States reported that by October 2020 8 million acres of land had been burned by wildfires [5]. On average, Canada has spent 800 million dollars annually on wildfire related costs in recent years [6]. Similarly, Australia has reported an increase of 30.6 days in the annual number of average days with high-extreme fire danger from 2016 to 2019 [7]. Additionally, contributing to the greater human experience of and impact from wildfires are changes in human migration and expansion. The pattern of human expansion into areas previously dominated by wildlife and nature means more people now live close to, or in, wooded areas, which serve as the fuel and setting for wildfires [8]. Researchers calculate that global wildfires can produce between 1.75 and 13.5 billion metric tons of carbon annually which circulate in our atmosphere for months [9]. Thus, wildfires themselves contribute to the greenhouse effect, propagating further development of wildfires.
Wildfires exert various impacts and risks to public health including an acute risk of mortality and injury, and by wreaking havoc on the community and the ensuing response team. Wildfires destroy homes and workplaces, displace victims, and impact numerous medical conditions such as chronic obstructive pulmonary disease (COPD), asthma, and mental health [10,11,12]. Studies have found higher rates post-wildfire of hypertension, gastrointestinal disorders, diabetes, and COPD and asthma exacerbation, along with various psychiatric conditions, including mood and anxiety disorders [11,12,13,14,15]. The impact of wildfires on the survivors’ mental health has been found in both the adult and pediatric population, with children and adolescents also experiencing higher rates of mood and anxiety disorders post-wildfire [16,17]. Researchers studying the impact of wildfires on children and adolescents have utilized survey and scale measures administered to study participants in this demographic, as well as their parents and/or teachers, to gain an appreciation of mental health outcomes within a study population that may struggle with personally communicating mood symptoms secondary to their developmental level [16,18,19]. Behavioral changes post-wildfire in children can include increased irritability and changes in concentration, sleep, and academic performance [18,20]. The impact of wildfires on mental health cannot be ignored and should not be, as the World Health Organization (WHO) identified neuropsychiatric disorders as the leading cause of disability-adjusted life years in the U.S. in 2010 with mental and behavioural disorders contributing to 13.6% of the total [21]. The repercussions from wildfires can be widespread due to the ability of wildfire-created smoke to dissipate and persist, with the majority of follow-up studies being conducted within 1 to 2 years post-wildfire. However, there is evidence of ongoing mental health effects in more longitudinal studies made 10–20 years post-wildfire [22,23]. There are novel terms to describe emotional and mental health responses to natural disasters such as solastalgia, eco-anxiety, and ecological grief, which will likely become more prominent as such tragedies continue to occur [24,25,26].
This paper is a scoping review of the existing literature, investigating the research question of how wildfires impact mental health; specifically, post-traumatic stress disorder (PTSD), major depressive disorder/depression (MDD), generalized anxiety disorder (GAD), and substance use at various times of follow-up. Our objective was to summarize the existing information on the impact of wildfires on mental health, and contribute to the understanding of factors that contribute to and protect against psychopathology post-wildfire. This information may be utilized to determine evidence-based public health responses to mitigate adverse outcomes. To our knowledge, this is the first scoping review to specifically examine the mental health effects of wildfires.
Through our review, we hope to summarize specifically and comprehensively how wildfires impact mental health and discuss how this information may be utilized for future research, wildfire disaster response, and ultimately improving population health.
2. Materials and Methods
A literature search on 16 February 2021, was first conducted in Pubmed, with no date restrictions or language filters. Search terms included “post traumatic stress disorder”) OR PTSD OR psychosis OR schizophreni* OR depressi* OR anxiety OR “mental illness*” OR “psychiatric disorder*” OR “psychiatric illness*” OR “mental disorder*” OR “mental health” AND wildfire* or forestfire* or bushfire* OR wild n6 fire* OR bush n6 fire* OR forest n6 fire* OR vegetation n6 fire* OR landscape n6 fire*.
Then a literature search on 7 April 2021, was conducted on Embase/OVID in their 1974 to present database, with no language filters. Search terms included exp mental disease/, exp wildfire/, (post traumatic stress disorder or PTSD or psychosis or schizophreni* or depressi* or anxiety or mental illness* or psychiatric disorder* or psychiatric illness* or mental disorder* or mental health).mp., (wildfire* or forestfire* or bushfire* or brushfire*).mp., and ((wild or brush or bush or forest or vegetation or landscape or peat or peatland) adj3 fire*).mp. The final search included all these terms together.
2.1. Inclusion Criteria
This review contains primary articles and includes randomized controlled trials and observational studies, such as case-control or cross-sectional studies, which reported on PTSD, anxiety, depression, substance use, or resiliency measures as outcomes of interest following wildfire exposure. Participants in the studies came from a wide breadth of age categories, from primary school children to elderly adults in their 90′s.
2.2. Exclusion Criteria
- Reviews and subjective reports without any new objective primary data were excluded from this review.
- Studies focusing primarily on firefighters, emergency responders, or burn victims were excluded.
- Studies were excluded if the exposure was non-wildfire based or the primary outcome was not related to mental health.
- Studies with a primary outcome of schizophrenia and psychosis were excluded due to the limited number of total studies available.
2.3. Data Extraction
The primary author reviewed the articles to determine which studies met the inclusion criteria and then performed the data extraction based on outcome measures of interest.
3. Results
Our review appraised and synthesized evidence from the literature about the impact of wildfires on mental health, specifically with respect to PTSD, depression, anxiety, and substance use. We present the findings of our search strategy and then findings on our primary aim under the various clinical outcomes.
Outcome of Literature Search
Figure 1 is a flowchart summarizing our search process and outcomes. This review found 60 articles that met the inclusion criteria [13,14,16,17,19,20,22,23,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77]. Three other articles were obtained from review of relevant in-text citations during data abstraction [18,78,79].
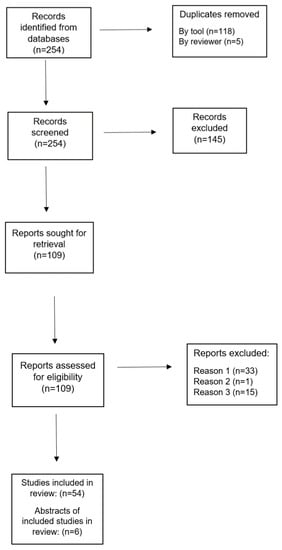
Figure 1.
Literature Search Flow Chart.
Table 1 details study characteristics. The earliest study was published in 1985 by Clayer et al. [13]. The vast majority (n = 57, 90%) were published from the year 2000 and onward. The results of the included studies are summarized in Table 2.

Table 1.
Characteristics of articles included in the study.

Table 2.
Results Table.
4. Discussion
This scoping review is specific to the impact of wildfires on mental health in both the adult and pediatric population. There are a number of narrative reports and letters discussing the impact of wildfire by experts in the field [5,80]. Our literature search identified one review specific to the impact of wildfire smoke exposure, which included a number of health outcomes including mental health [81]. In addition, there are several reviews that discussed the impact of wildfires on mental health within the broader context of natural disasters or climate change [12,25,82].
4.1. Post-Traumatic Stress Disorder
A post-natural disaster acute stress reaction is common and expected, but the rate at which an individual’s acute stress reaction may persist and develop into psychopathology is a common research objective [12]. Researchers have attempted to quantify the rates and severity of PTSD at various times post-wildfire in children, adolescents, and adults. This review suggests there are statistically and clinically significant increases in rates of PTSD in communities ravaged by wildfires. Among adults, higher rates of PTSD and associated symptoms were present shortly after a wildfire and up to 10 years post-wildfire [22,36]. In the adult population, the rate of probable PTSD based on a survey screening 3 months post-wildfire was found to be 24% and 60% in two separate studies [36,57]. At 6 months after a wildfire, the one month prevalence rate of PTSD in adults was 12.8%–26% [34,75]. At 18 months after the Fort McMurray wildfire, rates of likely PTSD continued to be higher than prior to the trauma, with studies finding similar rates, within 10.2%–13.6% [32,64,71]. Bryant et al. provided unique longitudinal information about the impact and prevalence of psychopathology post-wildfire [22,26,42]. From 3 to 10 years post-wildfire, the rate of fire-related PTSD in the high-impact group decreased from 15.6% to 7.6% [22,26,42].
Studies have looked at other outcomes or symptoms associated with PTSD post-wildfire including sleep disturbance and insomnia, anger, attachment style, interpersonal violence, and a term known as vicarious traumatization which is the development of PTSD symptoms from indirect trauma exposure [43,46,48,50,51,62,70,73].
A unique and recurring wildfire experience in South Asian countries is the seasonal haze created by bushfires from the intentional slash-and-burn technique used for clearing land for agricultural purposes [55]. Respondents who perceived lower Pollutants Standard Index values as dangerous were associated with higher IES-R scores [55]. In comparison, a study in British Columbia, Canada, on the impact of increased particulate matter (PM) and worsening air quality related to wildfires did not find an association with an increase in mental health related physician visits [63].
Rates of psychopathology post-wildfire exposure have also been studied in the pediatric population. In the sub-acute phase post-wildfire, the number of children with significant PTSD symptoms can be as high as 92% [16]. Studies that have assessed the rate of likely PTSD 6 months post-fire have found similar results with 9–12% of children and adolescents experiencing moderate to severe PTSD and as high as 29.4% in a study involving adolescents in Greece [19,58,65]. A year post-wildfire, the rate of PTSD in children and adolescents has been found to be between 27 and 37% [17,76]. The impact of a childhood exposure to a bushfire on one’s mental health as an adult was evaluated with a 20 year follow-up study conducted by Mcfarlane and Van Hooff [23]. They found no difference in the rate of lifetime or recent 1-month prevalence of PTSD in the wildfire exposed group versus controls [23].
Our literature search did not reveal a review specific to risk factors for developing PTSD post-bushfire, but such factors have been investigated by several primary studies. In adults, demographic factors such as female gender, widowed status, or fewer years of education, lower socioeconomic status, and non-caucasian ethnicity are associated risk factors, although gender was not always been found to be significant [26,32,69,73,78]. Trauma-related factors significant to increasing one’s risk of post-wildfire PTSD include personal witnessing of burning homes, having fear for one’s life or lives of loved ones, losing a loved one, significant property damage, or feeling a lack of support from family, friends, and/or the government [22,26,32,34,42,57,62,69]. The trauma related factors, including perceived threat to one’s life and subsequent reaction to the trauma, were found to be more contributory to the degree of PTSD symptoms than demographic or pre-trauma factors [69]. Finally, a contributing factor to the risk of developing PTSD post-bushfire is ongoing trauma and life stressors [22,23,26,42]. The risk factors for PTSD in children and adolescents were overall quite similar to adults, including demographic factors like female gender, younger age, and middle grades 7–9 [19,58,59,65,76]. For children, a greater predictor of increased emotional distress post-wildfire was the fear for their parents’ lives, even more than fear for their own life [19]. Combined with the identified risk factor in adults of a perceived lack of support from loved ones or the government, there is significant evidence to support the critical role a government and public health response has in mitigating mental health consequences after experiencing a bushfire [71]. A tangible government response may serve as validation that a traumatic experience has occurred, whilst providing avenues for recovery and moving forward. The impact and contribution ongoing adverse life events have on the risk of developing psychopathology post-wildfire is indicative of how cumulative stressors may deteriorate human resilience. As such, government aid should not be time sensitive post-wildfire, but rather be sustained in order to mitigate ongoing life stressors that can occur after a community is disrupted.
4.2. Depression
Second to PTSD, major depressive disorder (MDD) is one of the most common psychiatric illnesses studied and screened-for post-natural disasters [83]. Similar to rates of PTSD, there has also been shown to be higher rates of depression and associated symptoms post-wildfire in adults, which can persist up to 10 years [22,57]. In the adult population, studies have found rates of depression approximately 3 months post-bushfire, between 25.5 and 33% [36,57]. At 6 months post-wildfire, the estimated rates of MDD are between 10.4% and 17.1%, and between 18.3 and 24.8% at 18 months post-wildfire [32,33,64,71]. Finally, Bryant et al. studied a range of psychological outcomes over 10 years following the devastation of the Victorian Black Saturday bushfire including depression [22,26,42]. The rate of depression in the high-impact group was consistently around 10% at the three periods of follow-up [22,26,42].
Rates of depression post-wildfire have also been studied in children and adolescent populations. Mcdermott et al. were some of the first researchers to look at depression in children 6 months post-fire and found a rate of 4.7% [19]. However, a more recent study found a higher rate of depression 6 months post-wildfire at 20% [65]. Even at 18 months post-wildfire, one third of grade 7–12 students were found to meet criteria for depression compared to 17% in an age-matched control group [17,39].
The emotional response of solastalgia, which describes the mourning of changes in one’s natural environment, has been linked to levels of psychological distress post-wildfire [84]. Approximately one year after a wildfire, 35% of the participants had scores indicative of moderate-high risk for depression or anxiety on the Kessler Psychological Distress scale, and increased solastalgia was associated with greater odds of psychological distress [84].
There were fewer studies in the literature search investigating risk factors for depression post-bushfire in comparison to PTSD. However, some patient factors that have been identified in adults include female gender, age greater than 40 years old, a greater number of adverse experiences in childhood, a prior history of depressive disorder or anxiety disorder, and prior treatment with an antidepressant [14,33,64,71,73]. Other researchers did not find an association between demographic factors or gender and depression [57,78]. Trauma factors that increase risk of depression post-fire in adults are similar to PTSD: witnessing or experiencing property loss and fear for safety of loved ones [22,26,32,57,64]. Identified post-trauma risk factors include perceived lack of support from family, friends, or the government, ongoing life stressors, and having received counselling post-fire [22,26,32,33,42,64]. Similar risk factors for depression post-wildfire have also been identified in the pediatric population; although female gender has not been a consistent statistically significant risk factor, the trend is for higher symptom scores [58,59,65]. Finally, studies have commented on the association between PTSD and depression in children and adults, with a co-occurrence rate of 0.74 in adults [19,57].
Future research may utilize screening measures that combine specific depression related questions with associated behavioral changes that impact children’s functioning at home and school. Involving not only children and adolescent participants, but their parents, caregivers, and teachers in assessments would likely result in a more comprehensive screening for psychopathology post-wildfire.
4.3. Anxiety
There have been a number of studies investigating rates of anxiety disorders post-wildfire, although the quantity of evidence is smaller than that for PTSD and depression. Studies performed post-wildfire have shown higher rates of anxiety in both adult and the pediatric populations [17,19,31,36]. In adults surveyed 3 months post-wildfire, 27.0% met criteria for an anxiety disorder other than panic disorder and 17.4% had symptoms significant for panic disorder [36]. The one-month prevalence rate for generalized anxiety disorder symptoms 6 months post-wildfire was 19.8% [31]. At 18 months post-wildfire, the authors found similar rates of generalized anxiety disorder, between 15.7 and 18.7%, with self-reported pre-wildfire rates of anxiety estimated at 8.6–14.5% [32,64,71]. Finally, Bryant et al. followed a population of adults for up to 10 years after the Victorian Black Saturday bushfire, and over that time the rate of severe distress, as measured on the Kessler Psychological Distress Scale, decreased from 7.5% to 4.4% [22,26,42].
Anxiety in children and adolescents’ post-wildfire has also been studied, although to a lesser extent than adults. At 6 months post-wildfire, 14.1% of children had symptoms significant for high anxiety [19]. Looking later on, at 18 months after the Fort McMurray wildfire, 27% of grade 7–12 students had suspected anxiety, with another study finding no difference in the rate of anxiety disorders between wildfire exposed and control groups [17,39]. One unique study looked at childhood exposure to the Ash Wednesday wildfires of 1983 and followed up with participants 20 years later in adulthood [23]. Only the lifetime rate of any anxiety disorder other than PTSD was found to be significant, specifically with regards to environmental phobia [23].
A limitation in studies exploring anxiety is the reliance on scales to objectively measure anxiety such as the Global Health Questionnaire or the Kessler Psychological Distress Scale [22,60]. This may limit the ability to make specific mental health diagnoses, such as generalized anxiety disorder, without understanding the key criterion and degree of functional impact within each participant. One mechanism by which wildfires increase victims’ anxiety is the resulting emotion and mental turmoil of uncertainty after experiencing such devastating losses and damage to oneself, loved ones, property, belongings, and livelihood. The sensation of anxiety is not necessarily maladaptive, rather it may serve a functional purpose of helping create emotional motivation to respond and prepare for a perceived future threat [85,86]. Therefore, researchers and clinicians must distinguish between anxiety that serves as a normal and healthy response to a life stressor versus a debilitating anxiety disorder. Anxiety post-wildfire may help provide fuel for appropriate reactions, such as pursuing financial support, rebuilding one’s home, identifying available community resources, and cumulatively helping a victim heal from such trauma. However, functionally impairing anxiety describes an emotional response that no longer serves the individual, and therefore the distinction between the two is critical.
Similarly to the risk factors identified for PTSD and depression post-wildfire, the risk factors for anxiety can also be separated into patient factors, trauma factors, and post-trauma factors [31]. Patient factors include younger age or age ≤25 years old, lower socioeconomic status, a history of anxiety or depressive disorder, being on an antidepressant before the fire or prior adverse experiences in childhood [31,32,64,71,73]. Trauma related factors increasing the risk of anxiety include witnessing or experiencing property loss and experiencing or fearing the loss of loved ones [14,26,31,32,42,64]. Finally, factors that occur post-fire that may increase the risk of developing anxiety were similar to depression, including perceived lack of support and ongoing life stressors [14,26,31,32,42].
4.4. Substance Use
There is a paucity of evidence specific to substance use rates and disorders post-wildfire. In the resulting studies identified from the search terms, substance use post-wildfire was not explored as a primary independent outcome measure but always in combination with other psychological disorders [26,31,32,68]. It is estimated that at least 50% of individuals with a psychiatric illness will also have a comorbid substance use disorder at some point in their lives, and this number is significantly higher in certain populations or settings such as in-patient or treatment programs [87,88,89,90].
The existing studies indicate that there is an association between increased alcohol or drug use post-fire and psychiatric disorders [22,26,32,34,42,64]. For example, in adults 6 months post-wildfire, those with likely generalized anxiety disorder were three-times more likely to present with a drug related problem [31]. Studies have found the rate of alcohol use disorder or heavy alcohol use post-wildfire was 17% at 3 months post, 22% at 3 years post, and 18.6% at 10 years post, within the highly impacted community [22,36]. One study that evaluated substance use in college students 18 months after the Fort McMurray wildfire found a rate of 15.5% for high risk drinking, 13% for problematic drug use, and 4.4% for moderate-high nicotine dependence, with some gender differences in each category [71]. Some studies have found an association between drug related problems post-wildfire and mental illness but have not found the same relationship with high-risk drinking [32,34,64]. Other studies have found no difference in rates of substance or alcohol use in adults and adolescents exposed to a wildfire [14,23,39]. Thus, the exact relationship between mental illness and substance use and misuse is still unknown, but is likely reciprocal in nature due to a combination of genetic and environmental risk factors mutual to both; in addition, each disease may contribute to the development and persistence of the other through various factors such as the utilization of a substance as a coping mechanism for symptoms and the impact of substances on mood [87].
4.5. Resilience
Resilience is a common term found in the primary studies of this review as they investigated mental health outcomes such as PTSD, MDD, and GAD. It is a difficult concept to quantify objectively, as it represents such a complex sum of dynamic parts. Broadly, and within a psychological context, it refers to experiencing stressors and consequently negative emotional responses but adapting to such adversity with an absence of psychiatric conditions that by definition are functionally impairing [91,92]. Researchers have attempted to quantify resilience post-wildfire in patients or participants as the opposite of measures of psychopathology, i.e., low scores on psychological symptom scales or based on specific resiliency scales [22,26,42]. Although survey scales may be the best tool researchers have to quantify resiliency, they underestimate the fluidity and complexity of its constantly adapting components including patient characteristics and family and community supports. Individuals with high resilience scores after experiencing a wildfire had lower scores on screening measures for mental health disorders including PTSD, depression, and anxiety, and increased self-esteem and quality of life scores [17,73]. There is existing research on the relationship between resiliency factors such as coping strategies, group involvement, and psychotherapy with mental health outcomes post-wildfire [35,47,49,54]. Another focus of future research may be on appropriate tools and interventions from a broader public health perspective, to optimize patient resilience post-wildfire and prevent the development of psychopathology.
4.6. Environmentally Related Distress
Destructive natural disasters such as wildfires damage man-made structures but also the surrounding natural environment. The ensuing mourning and emotional response from the loss of nature has been termed ecological grief [24,93]. Closely related to ecological grief, and even called a sub-concept, is the term solastalgia; which is described as the feeling of homesickness whilst still at home [24]. The Aboriginal population residing in the Northwest Territories have been studied qualitatively in regards to their response to experiencing a wildfire, and a common theme was mourning their natural home and way of life [94]. The emotions linked to solastalgia also include anxiety, as it describes an emotional response that can include worry about potential environmental changes [24]. Eco-anxiety is worry or distress regarding the negative consequences of environmental changes [24,85,95,96]. The terms ecological grief, solastalgia, and eco-anxiety embody the psychological distress and reactions that can occur after a natural disaster or from climate change, and have started to appear in the literature on how wildfires impact mental health. Such terms reflect the role by which coping strategies that utilize the connection to one’s surrounding ecosystem may mitigate feelings of loss, mourning, and stress [97,98]. Qualitative evidence indicates that individuals may find a benefit in personal recovery through interactions and participation in environmental recovery [98]. This may reflect the protective factor a strong environmental connection provides by motivating the individual to participate in rebuilding processes that help their personal recovery.
4.7. Future Research
The existing studies show that wildfires do increase the rates of both medical and mental illness post-exposure; therefore, another area for future research may be a focus on the connection between the two, as well as the impact on less-studied outcomes such as psychosis [13]. McFarlane and Van Hooff identified limitations within the current disaster research, describing how the majority of studies are focused on follow-up within 1–2 years rather than greater longitudinal monitoring [99]. More long-term follow-up can provide key information on risk factors for persistence of psychiatric complications and information for interventions. Finally, with social media the dissemination of information is more rapid and uncontrollable than ever before. The public perception of facts and news is as important as the facts themselves, and future research could be into effective post-disaster communication, dissemination of information, and the impact on the individual. A novel method of population mental health support, which has been explored most recently throughout the COVID-19 pandemic, has been the utilization of supportive text messages [100]. Studies have found a significant reduction in anxiety, depression, and stress symptoms based on survey scores, as well as in prior randomized controlled clinical trials [100,101,102,103,104,105,106]. High user satisfaction has also been reported with supportive text message interventions [107,108,109,110]. From our literature search, text messaging as an intervention and public health response has not yet been explored in a wildfire impacted population and could serve as a novel area for research.
4.8. Limitations of the Study
Several of the limitations of this review were due to the constraints of time. Pubmed and Embase/OVID were chosen as the databases for the literature search, due to their accessibility and the availability of primary studies. However, including more databases in our literature search would add to the breadth of results and available data. Another limitation was that substance use was not one of our core search terms, and it was not until after the database search that we realized the volume of evidence available on rates of substance use post-wildfire and decided to include information from the included studies in this review. Other limitations included a single author performing the data extraction, an additional author would have added to the consistency of result data extracted. Moreover, not all included articles were peer reviewed, which may influence the quality of these studies.
5. Conclusions
With populations continuing to live closer to nature or once forested areas, wildfires will continue to exist and pose a threat to individual wellbeing and public health. In understanding the consequences of wildfires on both medical conditions and mental disorders, there is a need for a public health response that is comprehensive, sustained, and as adaptive as the people it serves. There is a strong body of literature to support the impact of wildfires on mental health, but more information is needed on the effective public health measures and rebuilding strategies that can optimize patient resilience post-wildfire.
Author Contributions
This paper is a result of the work of P.T., E.E. and V.I.O.A. P.T. is the primary author. All authors have read and agreed to the published version of the manuscript.
Funding
Funding for this review and its publishing was provided through an unrestricted grant from the Department of Psychiatry at the University of Alberta.
Institutional Review Board Statement
Ethical review was not applicable to this study as it is a review.
Informed Consent Statement
Informed consent is not applicable.
Data Availability Statement
All data used in this review article are in public domain as described in the methods section.
Acknowledgments
A sincere thank you to Laura Hamonic, a librarian with the University of Alberta, who provided much needed guidance and assistance with the technical aspects of writing a scoping review.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Krawisz, B. Health Effects of Climate Destabilization: Understanding the Problem. WMJ Off. Publ. State Med. Soc. Wis. 2020, 119, 132–138. [Google Scholar]
- The Combustion Process. Available online: http://www.auburn.edu/academic/forestry_wildlife/fire/combustion.htm (accessed on 7 March 2021).
- Xu, R.; Yu, P.; Abramson, M.J.; Johnston, F.H.; Samet, J.M.; Bell, M.L.; Haines, A.; Ebi, K.L.; Li, S.; Guo, Y. Wildfires, Global Climate Change, and Human Health. N. Engl. J. Med. 2020, 383, 2173–2181. [Google Scholar] [CrossRef]
- Wildfires. Available online: https://www.who.int/westernpacific/health-topics/wildfires (accessed on 4 March 2021).
- Nelson, R. US Wildfires and Mental Illness Stress Health Systems. Lancet 2020, 396, 1546–1547. [Google Scholar] [CrossRef]
- B.J. Stocks Wildfire Investigations Ltd. Evaluating Past, Current and Future Forest Fire Load Trends in Canada. 2013. Available online: https://www.ccfm.org/wp-content/uploads/2013/08/2-Fire-Load-Trends.pdf (accessed on 3 January 2021).
- Zhang, Y.; Beggs, P.J.; McGushin, A.; Bambrick, H.; Trueck, S.; Hanigan, I.C.; Morgan, G.G.; Berry, H.L.; Linnenluecke, M.K.; Johnston, F.H.; et al. The 2020 Special Report of the MJA-Lancet Countdown on Health and Climate Change: Lessons Learnt from Australia’s “Black Summer”. Med. J. Aust. 2020, 213, 490–492.e10. [Google Scholar] [CrossRef] [PubMed]
- A Cohesive Strategy is Needed to Address Catastrophic Wildfire Threats. Available online: https://www.govinfo.gov/content/pkg/CHRG-106hhrg59491/html/CHRG-106hhrg59491.htm (accessed on 4 March 2021).
- Johns, C. Wildfires, Greenhouse Gas Emissions and Climate Change; Future Directions International: Nedlands, Australia, 2020. [Google Scholar]
- Doerr, S.H.; Santín, C. Global Trends in Wildfire and Its Impacts: Perceptions versus Realities in a Changing World. Philos. Trans. R. Soc. B Biol. Sci. 2016, 371, 20150345. [Google Scholar] [CrossRef] [PubMed]
- Weilnhammer, V.; Schmid, J.; Mittermeier, I.; Schreiber, F.; Jiang, L.; Pastuhovic, V.; Herr, C.; Heinze, S. Extreme Weather Events in Europe and Their Health Consequences—A Systematic Review. Int. J. Hyg. Environ. Health 2021, 233, 113688. [Google Scholar] [CrossRef]
- Hrabok, M.; Delorme, A.; Agyapong, V.I.O. Threats to Mental Health and Well-Being Associated with Climate Change. J. Anxiety Disord. 2020, 76, 102295. [Google Scholar] [CrossRef] [PubMed]
- Clayer, J.R.; Bookless-Pratz, C.; Harris, R.I. Some Health Consequences of a Natural Disaster. Med. J. Aust. 1985, 143, 182–184. [Google Scholar] [CrossRef]
- Cherry, N.; Haynes, W. Effects of the Fort McMurray Wildfires on the Health of Evacuated Workers: Follow-up of 2 Cohorts. CMAJ Open 2017, 5, E638–E645. [Google Scholar] [CrossRef] [Green Version]
- Howard, C.; Rose, C.; Dodd, W.; Kohle, K.; Scott, C.; Scott, P.; Cunsolo, A.; Orbinski, J. SOS! Summer of Smoke: A Retrospective Cohort Study Examining the Cardiorespiratory Impacts of a Severe and Prolonged Wildfire Season in Canada’s High Subarctic. BMJ Open 2021, 11, e037029. [Google Scholar] [CrossRef]
- Jones, R.T.; Ribbe, D.P.; Cunningham, P.B.; Weddle, J.D.; Langley, A.K. Psychological Impact of Fire Disaster on Children and Their Parents. Behav. Modif. 2002, 26, 163–186. [Google Scholar] [CrossRef] [Green Version]
- Brown, M.R.G.; Agyapong, V.; Greenshaw, A.J.; Cribben, I.; Brett-MacLean, P.; Drolet, J.; McDonald-Harker, C.; Omeje, J.; Mankowsi, M.; Noble, S.; et al. Significant PTSD and Other Mental Health Effects Present 18 Months After the Fort Mcmurray Wildfire: Findings From 3070 Grades 7–12 Students. Front. Psychiatry 2019, 10, 623. [Google Scholar] [CrossRef] [Green Version]
- McFarlane, A.C.; Policansky, S.K.; Irwin, C. A Longitudinal Study of the Psychological Morbidity in Children Due to a Natural Disaster. Psychol. Med. 1987, 17, 727–738. [Google Scholar] [CrossRef]
- McDermott, B.M.C.; Palmer, L.J. Post-Disaster Service Provision Following Proactive Identification of Children with Emotional Distress and Depression. Aust. N. Z. J. Psychiatry 1999, 33, 855–863. [Google Scholar] [CrossRef] [PubMed]
- Kirsch, K.R.; Feldt, B.A.; Zane, D.F.; Haywood, T.; Jones, R.W.; Horney, J.A. Longitudinal Community Assessment for Public Health Emergency Response to Wildfire, Bastrop County, Texas. Health Secur. 2016, 14, 93–104. [Google Scholar] [CrossRef]
- NIMH. U.S. Leading Categories of Diseases/Disorders. Available online: https://www.nimh.nih.gov/health/statistics/disability/us-leading-categories-of-diseases-disorders.shtml (accessed on 4 March 2021).
- Bryant, R.A.; Gibbs, L.; Colin Gallagher, H.; Pattison, P.; Lusher, D.; MacDougall, C.; Harms, L.; Block, K.; Ireton, G.; Richardson, J.; et al. The Dynamic Course of Psychological Outcomes Following the Victorian Black Saturday Bushfires. Aust. N. Z. J. Psychiatry 2020, 55, 666–677. [Google Scholar] [CrossRef] [PubMed]
- McFarlane, A.C.; Van Hooff, M. Impact of Childhood Exposure to a Natural Disaster on Adult Mental Health: 20-Year Longitudinal Follow-up Study. Br. J. Psychiatry 2009, 195, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Comtesse, H.; Ertl, V.; Hengst, S.M.C.; Rosner, R.; Smid, G.E. Ecological Grief as a Response to Environmental Change: A Mental Health Risk or Functional Response? Int. J. Environ. Res. Public Health 2021, 18, 734. [Google Scholar] [CrossRef] [PubMed]
- Palinkas, L.A.; Wong, M. Global Climate Change and Mental Health. Curr. Opin. Psychol. 2020, 32, 12–16. [Google Scholar] [CrossRef]
- Bryant, R.A.; Waters, E.; Gibbs, L.; Gallagher, H.C.; Pattison, P.; Lusher, D.; MacDougall, C.; Harms, L.; Block, K.; Snowdon, E.; et al. Psychological Outcomes Following the Victorian Black Saturday Bushfires. Aust. N. Z. J. Psychiatry 2014, 48, 634–643. [Google Scholar] [CrossRef] [Green Version]
- Adamis, D.; Papanikolaou, V.; Mellon, R.C.; Prodromitis, G.; Tyrovola, K.; Kyriopoulos, J. P-1035—Long-Term Psychological Effects of a Wildfire Disaster in Greece. Eur. Psychiatry 2012, 27, 1. [Google Scholar] [CrossRef]
- Adamis, D.; Papanikolaou, V.; Kyriopoulos, J. P-581—Quality of Life after a Wildfire Disaster in a Rural Area of Greece. Eur. Psychiatry 2012, 27, 1. [Google Scholar] [CrossRef]
- Adamis, D.; Papanikolaou, V.; Mellon, R.C.; Prodromitis, G. The Impact of Wildfires on Mental Health of Residents in a Rural Area of Greece. A Case Control Population Based Study. Eur. Psychiatry 2011, 26, 1188. [Google Scholar] [CrossRef]
- Afifi, W.A.; Felix, E.D.; Afifi, T.D. The Impact of Uncertainty and Communal Coping on Mental Health Following Natural Disasters. Anxiety Stress Coping 2012, 25, 329–347. [Google Scholar] [CrossRef]
- Agyapong, V.I.O.; Hrabok, M.; Juhas, M.; Omeje, J.; Denga, E.; Nwaka, B.; Akinjise, I.; Corbett, S.E.; Moosavi, S.; Brown, M.; et al. Prevalence Rates and Predictors of Generalized Anxiety Disorder Symptoms in Residents of Fort McMurray Six Months After a Wildfire. Front. Psychiatry 2018, 9, 345. [Google Scholar] [CrossRef] [Green Version]
- Agyapong, V.I.O.; Ritchie, A.; Brown, M.R.G.; Noble, S.; Mankowsi, M.; Denga, E.; Nwaka, B.; Akinjise, I.; Corbett, S.E.; Moosavi, S.; et al. Long-Term Mental Health Effects of a Devastating Wildfire Are Amplified by Socio-Demographic and Clinical Antecedents in Elementary and High School Staff. Front. Psychiatry 2020, 11, 448. [Google Scholar] [CrossRef]
- Oral Communications. Eur. Psychiatry 2018, 48, S72–S140. [CrossRef]
- Agyapong, V.I.O.; Juhas, M.; Omege, J.; Denga, E.; Nwaka, B.; Akinjise, I.; Corbett, S.E.; Brown, M.; Chue, P.; Li, X.-M.; et al. Prevalence Rates and Correlates of Likely Post-Traumatic Stress Disorder in Residents of Fort McMurray 6 Months After a Wildfire. Int. J. Ment. Health Addict. 2019, 19. [Google Scholar] [CrossRef]
- Belleville, G.; Lebel, J.; Ouellet, M.-C.; Békés, V.; Morin, C.M.; Bergeron, N.; Campbell, T.; Ghosh, S.; Bouchard, S.; Guay, S.; et al. Resilient—An Online Multidimensional Treatment to Promote Resilience and Better Sleep: A Randomized Controlled Trial. Sleep Med. 2019, 64, S214–S215. [Google Scholar] [CrossRef]
- Belleville, G.; Ouellet, M.-C.; Morin, C.M. Post-Traumatic Stress among Evacuees from the 2016 Fort McMurray Wildfires: Exploration of Psychological and Sleep Symptoms Three Months after the Evacuation. Int. J. Environ. Res. Public Health 2019, 16, 1604. [Google Scholar] [CrossRef] [Green Version]
- Binet, É.; Ouellet, M.-C.; Lebel, J.; Békés, V.; Morin, C.M.; Bergeron, N.; Campbell, T.; Ghosh, S.; Bouchard, S.; Guay, S.; et al. A Portrait of Mental Health Services Utilization and Perceived Barriers to Care in Men and Women Evacuated During the 2016 Fort McMurray Wildfires. Adm. Policy Ment. Health Ment. Health Serv. Res. 2021, 1–13. [Google Scholar] [CrossRef]
- Block, K.; Molyneaux, R.; Gibbs, L.; Alkemade, N.; Baker, E.; MacDougall, C.; Ireton, G.; Forbes, D. The Role of the Natural Environment in Disaster Recovery: “We Live Here Because We Love the Bush”. Health Place 2019, 57, 61–69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, M.R.G.; Agyapong, V.; Greenshaw, A.J.; Cribben, I.; Brett-MacLean, P.; Drolet, J.; McDonald-Harker, C.; Omeje, J.; Mankowsi, M.; Noble, S.; et al. After the Fort McMurray Wildfire There Are Significant Increases in Mental Health Symptoms in Grade 7–12 Students Compared to Controls. BMC Psychiatry 2019, 19, 18. [Google Scholar] [CrossRef] [Green Version]
- Bryant, R.A.; Creamer, M.; O’Donnell, M.; Forbes, D.; Felmingham, K.L.; Silove, D.; Malhi, G.; van Hoof, M.; McFarlane, A.C.; Nickerson, A. Separation from Parents during Childhood Trauma Predicts Adult Attachment Security and Post-Traumatic Stress Disorder. Psychol. Med. 2017, 47, 2028–2035. [Google Scholar] [CrossRef] [PubMed]
- Bryant, R.A.; Gallagher, H.C.; Gibbs, L.; Pattison, P.; MacDougall, C.; Harms, L.; Block, K.; Baker, E.; Sinnott, V.; Ireton, G.; et al. Mental Health and Social Networks After Disaster. Am. J. Psychiatry 2017, 174, 277–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bryant, R.A.; Gibbs, L.; Gallagher, H.C.; Pattison, P.; Lusher, D.; MacDougall, C.; Harms, L.; Block, K.; Sinnott, V.; Ireton, G.; et al. Longitudinal Study of Changing Psychological Outcomes Following the Victorian Black Saturday Bushfires. Aust. N. Z. J. Psychiatry 2018, 52, 542–551. [Google Scholar] [CrossRef] [Green Version]
- Byrne, M.K.; Lerias, D.; Sullivan, N.L. Predicting Vicarious Traumatization in Those Indirectly Exposed to Bushfires. Stress Health 2006, 22, 167–177. [Google Scholar] [CrossRef]
- Caamano-Isorna, F.; Figueiras, A.; Sastre, I.; Montes-Martínez, A.; Taracido, M.; Piñeiro-Lamas, M. Respiratory and Mental Health Effects of Wildfires: An Ecological Study in Galician Municipalities (North-West Spain). Environ. Health 2011, 10, 48. [Google Scholar] [CrossRef] [Green Version]
- Camilleri, P.; Healy, C.; Macdonald, E.; Nicholls, S.; Sykes, J.; Winkworth, G.; Woodward, M. Recovery from Bushfires: The Experience of the 2003 Canberra Bushfires Three Years After. Australas. J. Paramed. 2010, 8. [Google Scholar] [CrossRef] [Green Version]
- Cowlishaw, S.; Metcalf, O.; Varker, T.; Stone, C.; Molyneaux, R.; Gibbs, L.; Block, K.; Harms, L.; MacDougall, C.; Gallagher, H.C.; et al. Anger Dimensions and Mental Health Following a Disaster: Distribution and Implications After a Major Bushfire. J. Trauma. Stress 2021, 34, 46–55. [Google Scholar] [CrossRef]
- Felix, E.; Afifi, T.; Kia-Keating, M.; Brown, L.; Afifi, W.; Reyes, G. Family Functioning and Posttraumatic Growth among Parents and Youth Following Wildfire Disasters. Am. J. Orthopsychiatry 2015, 85, 191–200. [Google Scholar] [CrossRef]
- Forbes, D.; Alkemade, N.; Waters, E.; Gibbs, L.; Gallagher, C.; Pattison, P.; Lusher, D.; MacDougall, C.; Harms, L.; Block, K.; et al. The Role of Anger and Ongoing Stressors in Mental Health Following a Natural Disaster. Aust. N. Z. J. Psychiatry 2015, 49, 706–713. [Google Scholar] [CrossRef]
- Gallagher, H.C.; Block, K.; Gibbs, L.; Forbes, D.; Lusher, D.; Molyneaux, R.; Richardson, J.; Pattison, P.; MacDougall, C.; Bryant, R.A. The Effect of Group Involvement on Post-Disaster Mental Health: A Longitudinal Multilevel Analysis. Soc. Sci. Med. 2019, 220, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, H.C.; Lusher, D.; Gibbs, L.; Pattison, P.; Forbes, D.; Block, K.; Harms, L.; MacDougall, C.; Kellett, C.; Ireton, G.; et al. Dyadic Effects of Attachment on Mental Health: Couples in a Postdisaster Context. J. Fam. Psychol. 2017, 31, 192–202. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, H.C.; Richardson, J.; Forbes, D.; Harms, L.; Gibbs, L.; Alkemade, N.; MacDougall, C.; Waters, E.; Block, K.; Lusher, D.; et al. Mental Health Following Separation in a Disaster: The Role of Attachment: Disaster-Related Separation and Attachment. J. Trauma. Stress 2016, 29, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Hashoul-Andary, R.; Assayag-Nitzan, Y.; Yuval, K.; Aderka, I.M.; Litz, B.; Bernstein, A. A Longitudinal Study of Emotional Distress Intolerance and Psychopathology Following Exposure to a Potentially Traumatic Event in a Community Sample. Cogn. Ther. Res. 2016, 40, 1–13. [Google Scholar] [CrossRef]
- Hertz-Picciotto, I. 43.3 Mental Health in Children and Adolescents Exposed to the 2017 and/or 2018 Wildfires in Northern California. J. Am. Acad. Child. Adolesc. Psychiatry 2020, 59, S66. [Google Scholar] [CrossRef]
- Hooper, J.; Magor-Blatch, L.; Bhullar, N. Life after Bushfire: Post-Traumatic Stress, Coping, Post-Traumatic Growth. Australas. J. Paramed. 2018, 15. [Google Scholar] [CrossRef] [Green Version]
- Ho, R.C.; Zhang, M.W.; Ho, C.S.; Pan, F.; Lu, Y.; Sharma, V.K. Impact of 2013 South Asian Haze Crisis: Study of Physical and Psychological Symptoms and Perceived Dangerousness of Pollution Level. BMC Psychiatry 2014, 14, 81. [Google Scholar] [CrossRef] [Green Version]
- Jones, R.T.; Ribbe, D.P.; Cunningham, P. Psychosocial Correlates of Fire Disaster among Children and Adolescents. J. Trauma. Stress 1994, 7, 117–122. [Google Scholar] [CrossRef]
- Marshall, G.N.; Schell, T.L.; Elliott, M.N.; Rayburn, N.R.; Jaycox, L.H. Psychiatric Disorders Among Adults Seeking Emergency Disaster Assistance After a Wildland-Urban Interface Fire. Psychiatr. Serv. 2007, 58, 509–514. [Google Scholar] [CrossRef]
- McDermott, B.M.; Lee, E.M.; Judd, M.; Gibbon, P. Posttraumatic Stress Disorder and General Psychopathology in Children and Adolescents Following a Wildfire Disaster. Can. J. Psychiatry 2005, 50, 137–143. [Google Scholar] [CrossRef] [Green Version]
- Mcdermott, B.M.; Palmer, L.J. Postdisaster Emotional Distress, Depression and Event-Related Variables: Findings Across Child and Adolescent Developmental Stages. Aust. N. Z. J. Psychiatry 2002, 36, 754–761. [Google Scholar] [CrossRef]
- McFarlane, A.C.; Clayer, J.R.; Bookless, C.L. Psychiatric Morbidity Following a Natural Disaster: An Australian Bushfire. Soc. Psychiatry Psychiatr. Epidemiol. 1997, 32, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Mellon, R.C.; Papanikolau, V.; Prodromitis, G. Locus of Control and Psychopathology in Relation to Levels of Trauma and Loss: Self-Reports of Peloponnesian Wildfire Survivors: Locus of Control and Psychopathology in Relation to Levels of Trauma and Loss. J. Trauma. Stress 2009, 22, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Molyneaux, R.; Gibbs, L.; Bryant, R.A.; Humphreys, C.; Hegarty, K.; Kellett, C.; Gallagher, H.C.; Block, K.; Harms, L.; Richardson, J.F.; et al. Interpersonal Violence and Mental Health Outcomes Following Disaster. BJPsych Open 2020, 6, e1. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.; Copes, R.; Fisk, R.; Joy, R.; Chan, K.; Brauer, M. Population Health Effects of Air Quality Changes Due to Forest Fires in British Columbia in 2003: Estimates from Physician-Visit Billing Data. Can. J. Public Health 2006, 97, 105–108. [Google Scholar] [CrossRef]
- Moosavi, S.; Nwaka, B.; Akinjise, I.; Corbett, S.E.; Chue, P.; Greenshaw, A.J.; Silverstone, P.H.; Li, X.-M.; Agyapong, V.I.O. Mental Health Effects in Primary Care Patients 18 Months After a Major Wildfire in Fort McMurray: Risk Increased by Social Demographic Issues, Clinical Antecedents, and Degree of Fire Exposure. Front. Psychiatry 2019, 10, 683. [Google Scholar] [CrossRef]
- Papadatou, D.; Giannopoulou, I.; Bitsakou, P.; Bellali, T.; Talias, M.A.; Tselepi, K. Adolescents’ Reactions after a Wildfire Disaster in Greece. J. Trauma. Stress 2012, 25, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Papanikolaou, V.; Adamis, D.; Mellon, R.C.; Prodromitis, G. Psychological Distress Following Wildfires Disaster in a Rural Part of Greece: A Case-Control Population-Based Study. Int. J. Emerg. Ment. Health 2011, 13, 11–26. [Google Scholar]
- Papanikolaou, V.; Leon, G.R.; Kyriopoulos, J.; Levett, J.; Pallis, E. Surveying the Ashes: Experience from the 2007 Peloponnese Wildfires Six Months after the Disaster. Prehosp. Disaster Med. 2011, 26, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Parslow, R.A.; Jorm, A.F. Tobacco Use after Experiencing a Major Natural Disaster: Analysis of a Longitudinal Study of 2063 Young Adults. Addiction 2006, 101, 1044–1050. [Google Scholar] [CrossRef]
- Parslow, R.A.; Jorm, A.F.; Christensen, H. Associations of Pre-Trauma Attributes and Trauma Exposure with Screening Positive for PTSD: Analysis of a Community-Based Study of 2085 Young Adults. Psychol. Med. 2006, 36, 387–395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Psarros, C.; Theleritis, C.; Economou, M.; Tzavara, C.; Kioulos, K.T.; Mantonakis, L.; Soldatos, C.R.; Bergiannaki, J.-D. Insomnia and PTSD One Month after Wildfires: Evidence for an Independent Role of the “Fear of Imminent Death”. Int. J. Psychiatry Clin. Pract. 2017, 21, 137–141. [Google Scholar] [CrossRef]
- Ritchie, A.; Sautner, B.; Omege, J.; Denga, E.; Nwaka, B.; Akinjise, I.; Corbett, S.E.; Moosavi, S.; Greenshaw, A.; Chue, P.; et al. Long-Term Mental Health Effects of a Devastating Wildfire Are Amplified by Sociodemographic and Clinical Antecedents in College Students. Disaster Med. Public Health Prep. 2020, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Scher, C.D.; Ellwanger, J. Fire-Related Cognitions Moderate the Impact of Risk Factors on Adjustment Following Wildfire Disaster. J. Anxiety Disord. 2009, 23, 891–896. [Google Scholar] [CrossRef]
- Silveira, S.; Kornbluh, M.; Withers, M.C.; Grennan, G.; Ramanathan, V.; Mishra, J. Chronic Mental Health Sequelae of Climate Change Extremes: A Case Study of the Deadliest Californian Wildfire. Int. J. Environ. Res. Public Health 2021, 18, 1487. [Google Scholar] [CrossRef]
- Tally, S.; Levack, A.; Sarkin, A.J.; Gilmer, T.; Groessl, E.J. The Impact of the San Diego Wildfires on a General Mental Health Population Residing in Evacuation Areas. Adm. Policy Ment. Health Ment. Health Serv. Res. 2013, 40, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Verstraeten, B.S.E.; Elgbeili, G.; Hyde, A.; King, S.; Olson, D.M. Maternal Mental Health after a Wildfire: Effects of Social Support in the Fort McMurray Wood Buffalo Study. Can. J. Psychiatry 2020, 070674372097085. [Google Scholar] [CrossRef]
- Yelland, C.; Robinson, P.; Lock, C.; La Greca, A.M.; Kokegei, B.; Ridgway, V.; Lai, B. Bushfire Impact on Youth. J. Trauma. Stress 2010. [Google Scholar] [CrossRef]
- Zeller, M.; Yuval, K.; Nitzan-Assayag, Y.; Bernstein, A. Self-Compassion in Recovery Following Potentially Traumatic Stress: Longitudinal Study of At-Risk Youth. J. Abnorm. Child Psychol. 2015, 43, 645–653. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.T.; Ribbe, D.P.; Cunningham, P.; Weddle, J.D. Psychosocial Correlates of a Wildfire Disaster: Post Disaster Adult Reactions. Fire Technol. 2003, 39, 103–117. [Google Scholar] [CrossRef]
- McFarlane, A.C. Posttraumatic Phenomena in a Longitudinal Study of Children Following a Natural Disaster. J. Am. Acad. Child Adolesc. Psychiatry 1987, 26, 764–769. [Google Scholar] [CrossRef]
- The Lancet Australia on Fire. Lancet 2020, 395, 165. [CrossRef] [Green Version]
- Reid, C.E.; Brauer, M.; Johnston, F.H.; Jerrett, M.; Balmes, J.R.; Elliott, C.T. Critical Review of Health Impacts of Wildfire Smoke Exposure. Environ. Health Perspect. 2016, 124, 1334–1343. [Google Scholar] [CrossRef] [Green Version]
- Cianconi, P.; Betrò, S.; Janiri, L. The Impact of Climate Change on Mental Health: A Systematic Descriptive Review. Front. Psychiatry 2020, 11, 74. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.R.; Adams, Z.W.; Menon, S.V.; Youngstrom, E.A.; Bunnell, B.E.; Acierno, R.; Ruggiero, K.J.; Danielson, C.K. How Should We Screen for Depression Following a Natural Disaster? An ROC Approach to Post-Disaster Screening in Adolescents and Adults. J. Affect. Disord. 2016, 202, 102–109. [Google Scholar] [CrossRef] [Green Version]
- Eisenman, D.; McCaffrey, S.; Donatello, I.; Marshal, G. An Ecosystems and Vulnerable Populations Perspective on Solastalgia and Psychological Distress After a Wildfire. EcoHealth 2015, 12, 602–610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clayton, S. Climate Anxiety: Psychological Responses to Climate Change. J. Anxiety Disord. 2020, 74, 102263. [Google Scholar] [CrossRef]
- Barlow, D.H.; Durand, V.M.; Hofmann, S.G. Abnormal Psychology: An Integrative Approach, 8th ed.; Cengage Learning: Boston, MA, USA, 2017. [Google Scholar]
- Ross, S.; Peselow, E. Co-Occurring Psychotic and Addictive Disorders: Neurobiology and Diagnosis. Clin. Neuropharmacol. 2012, 35, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Kelly, T.M.; Daley, D.C. Integrated Treatment of Substance Use and Psychiatric Disorders. Soc. Work Public Health 2013, 28, 388–406. [Google Scholar] [CrossRef]
- Shantna, K.; Chaudhury, S.; Verma, A.; Singh, A. Comorbid Psychiatric Disorders in Substance Dependence Patients: A Control Study. Ind. Psychiatry J. 2009, 18, 84. [Google Scholar] [CrossRef]
- Comorbidity of Substance Use and Mental Health Disorders in Europe (Perspectives on Drugs). Available online: https://www.emcdda.europa.eu/publications/pods/comorbidity-substance-use-mental-health (accessed on 5 March 2021).
- Friedberg, A.; Malefakis, D. Resilience, Trauma, and Coping. Psychodyn. Psychiatry 2018, 46, 81–113. [Google Scholar] [CrossRef] [Green Version]
- Windle, G. What Is Resilience? A Review and Concept Analysis. Rev. Clin. Gerontol. 2011, 21, 152–169. [Google Scholar] [CrossRef]
- Cunsolo, A.; Ellis, N.R. Ecological Grief as a Mental Health Response to Climate Change-Related Loss. Nat. Clim. Chang. 2018, 8, 275–281. [Google Scholar] [CrossRef]
- Dodd, W.; Scott, P.; Howard, C.; Scott, C.; Rose, C.; Cunsolo, A.; Orbinski, J. Lived Experience of a Record Wildfire Season in the Northwest Territories, Canada. Can. J. Public Health 2018, 109, 327–337. [Google Scholar] [CrossRef]
- Clayton, S.; Karazsia, B.T. Development and Validation of a Measure of Climate Change Anxiety. J. Environ. Psychol. 2020, 69, 101434. [Google Scholar] [CrossRef]
- Usher, K.; Durkin, J.; Bhullar, N. Eco-anxiety: How Thinking about Climate Change-related Environmental Decline Is Affecting Our Mental Health. Int. J. Ment. Health Nurs. 2019, 28, 1233–1234. [Google Scholar] [CrossRef] [PubMed]
- Parker, C.L.; Wellbery, C.E.; Mueller, M. The Changing Climate: Managing Health Impacts. Am. Fam. Physician 2019, 100, 618–626. [Google Scholar]
- Husk, K.; Lovell, R.; Cooper, C.; Stahl-Timmins, W.; Garside, R. Participation in Environmental Enhancement and Conservation Activities for Health and Well-Being in Adults: A Review of Quantitative and Qualitative Evidence. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef] [Green Version]
- McFarlane, A.C.; Van Hooff, M. Learning for the Future: The Challenge of Disaster Research. Aust. N. Z. J. Psychiatry 2014, 48, 600–602. [Google Scholar] [CrossRef] [PubMed]
- Agyapong, V.I.O.; Hrabok, M.; Shalaby, R.; Vuong, W.; Noble, J.M.; Gusnowski, A.; Mrklas, K.; Li, D.; Urichuck, L.; Snaterse, M.; et al. Text4Hope: Receiving Daily Supportive Text Messages for 3 Months During the COVID-19 Pandemic Reduces Stress, Anxiety, and Depression. Disaster Med. Public Health Prep. 2021, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Agyapong, V.I.O. Coronavirus Disease 2019 Pandemic: Health System and Community Response to a Text Message (Text4Hope) Program Supporting Mental Health in Alberta. Disaster Med. Public Health Prep. 2020, 14, e5–e6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agyapong, V.I.O.; Hrabok, M.; Vuong, W.; Gusnowski, A.; Shalaby, R.; Mrklas, K.; Li, D.; Urichuk, L.; Snaterse, M.; Surood, S.; et al. Closing the Psychological Treatment Gap During the COVID-19 Pandemic with a Supportive Text Messaging Program: Protocol for Implementation and Evaluation. JMIR Res. Protoc. 2020, 9, e19292. [Google Scholar] [CrossRef]
- Agyapong, V.I.O.; Shalaby, R.; Hrabok, M.; Vuong, W.; Noble, J.M.; Gusnowski, A.; Mrklas, K.; Li, D.; Snaterse, M.; Surood, S.; et al. Mental Health Outreach via Supportive Text Messages during the COVID-19 Pandemic: Improved Mental Health and Reduced Suicidal Ideation after Six Weeks in Subscribers of Text4Hope Compared to a Control Population. Int. J. Environ. Res. Public Health 2021, 18, 2157. [Google Scholar] [CrossRef] [PubMed]
- Agyapong, V.I.O.; Hrabok, M.; Vuong, W.; Shalaby, R.; Noble, J.M.; Gusnowski, A.; Mrklas, K.J.; Li, D.; Urichuk, L.; Snaterse, M.; et al. Changes in Stress, Anxiety, and Depression Levels of Subscribers to a Daily Supportive Text Message Program (Text4Hope) During the COVID-19 Pandemic: Cross-Sectional Survey Study. JMIR Ment. Health 2020, 7, e22423. [Google Scholar] [CrossRef] [PubMed]
- Agyapong, V.I.O.; Mrklas, K.; Suen, V.Y.M.; Rose, M.S.; Jahn, M.; Gladue, I.; Kozak, J.; Leslie, M.; Dursun, S.; Ohinmaa, A.; et al. Supportive Text Messages to Reduce Mood Symptoms and Problem Drinking in Patients with Primary Depression or Alcohol Use Disorder: Protocol for an Implementation Research Study. JMIR Res. Protoc. 2015, 4, e55. [Google Scholar] [CrossRef]
- Agyapong, V.I.O.; McLoughlin, D.M.; Farren, C.K. Six-Months Outcomes of a Randomised Trial of Supportive Text Messaging for Depression and Comorbid Alcohol Use Disorder. J. Affect. Disord. 2013, 151, 100–104. [Google Scholar] [CrossRef]
- Agyapong, V.I.O.; Ahern, S.; McLoughlin, D.M.; Farren, C.K. Supportive Text Messaging for Depression and Comorbid Alcohol Use Disorder: Single-Blind Randomised Trial. J. Affect. Disord. 2012, 141, 168–176. [Google Scholar] [CrossRef]
- Agyapong, V.I.O.; Mrklas, K.; Juhás, M.; Omeje, J.; Ohinmaa, A.; Dursun, S.M.; Greenshaw, A.J. Cross-Sectional Survey Evaluating Text4Mood: Mobile Health Program to Reduce Psychological Treatment Gap in Mental Healthcare in Alberta through Daily Supportive Text Messages. BMC Psychiatry 2016, 16, 378. [Google Scholar] [CrossRef] [Green Version]
- Agyapong, V.I.O.; Milnes, J.; McLoughlin, D.M.; Farren, C.K. Perception of Patients with Alcohol Use Disorder and Comorbid Depression about the Usefulness of Supportive Text Messages. Technol. Health Care 2013, 21, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Shalaby, R.; Vuong, W.; Hrabok, M.; Gusnowski, A.; Mrklas, K.; Li, D.; Snaterse, M.; Surood, S.; Cao, B.; Li, X.-M.; et al. Gender Differences in Satisfaction with a Text Messaging Program (Text4Hope) and Anticipated Receptivity to Technology-Based Health Support During the COVID-19 Pandemic: Cross-Sectional Survey Study. JMIR MHealth UHealth 2021, 9, e24184. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).