Associations of Circadian Eating Pattern and Diet Quality with Substantial Postpartum Weight Retention
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Dietary Assessments
2.2.1. Assessment of Circadian Eating Patterns
2.2.2. Assessment of Diet Quality
2.3. Postpartum Weight Retention
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Maternal Characteristics
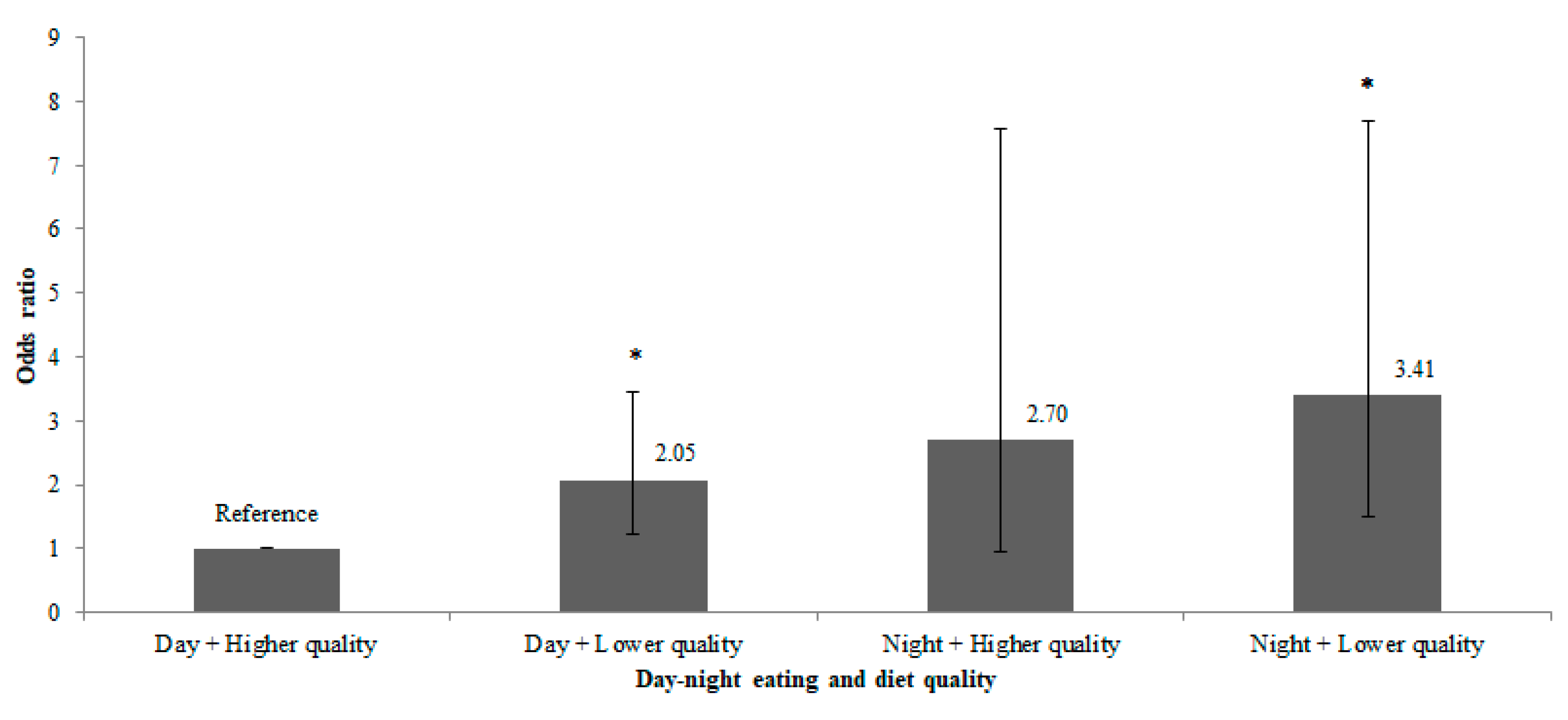
3.2. Associations Between Maternal Eating Patterns and Substantial PPWR
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- McKinley, M.C.; Allen-Walker, V.; McGirr, C.; Rooney, C.; Woodside, J.V. Weight loss after pregnancy: Challenges and opportunities. Nutr. Res. Rev. 2018, 31, 225–238. [Google Scholar] [CrossRef] [PubMed]
- Gunderson, E.P. Childbearing and obesity in women: Weight before, during, and after pregnancy. Obstet. Gynecol. Clin. N. Am. 2009, 36, 317–332. [Google Scholar] [CrossRef] [PubMed]
- Linné, Y.; Dye, L.; Barkeling, B.; Rössner, S. Long-term weight development in women: A 15-year follow-up of the effects of pregnancy. Obes. Res. 2004, 12, 1166–1178. [Google Scholar] [CrossRef] [PubMed]
- Gunderson, E.P.; Sternfeld, B.; Wellons, M.F.; Whitmer, R.A.; Chiang, V.; Quesenberry, C.P., Jr.; Lewis, C.E.; Sidney, S. Childbearing may increase visceral adipose tissue independent of overall increase in body fat. Obesity (Silver Spring) 2008, 16, 1078–1084. [Google Scholar] [CrossRef] [PubMed]
- Godfrey, K.M.; Reynolds, R.M.; Prescott, S.L.; Nyirenda, M.; Jaddoe, V.W.V.; Eriksson, J.G.; Broekman, B.F. Influence of maternal obesity on the long-term health of offspring. Lancet Diabetes Endocrinol. 2017, 5, 53–64. [Google Scholar] [CrossRef]
- Farpour-Lambert, N.J.; Ells, L.J.; Martinez de Tejada, B.; Scott, C. Obesity and Weight Gain in Pregnancy and Postpartum: An Evidence Review of Lifestyle Interventions to Inform Maternal and Child Health Policies. Front. Endocrinol. 2018, 9, 546. [Google Scholar] [CrossRef] [PubMed]
- Asher, G.; Sassone-Corsi, P. Time for food: The intimate interplay between nutrition, metabolism, and the circadian clock. Cell 2015, 161, 84–92. [Google Scholar] [CrossRef]
- Damiola, F.; Le Minh, N.; Preitner, N.; Kornmann, B.; Fleury-Olela, F.; Schibler, U. Restricted feeding uncouples circadian oscillators in peripheral tissues from the central pacemaker in the suprachiasmatic nucleus. Genes Dev. 2000, 14, 2950–2961. [Google Scholar] [CrossRef]
- Baron, K.G.; Reid, K.J.; Kern, A.S.; Zee, P.C. Role of sleep timing in caloric intake and BMI. Obesity (Silver Spring) 2011, 19, 1374–1381. [Google Scholar] [CrossRef]
- Marinac, C.R.; Nelson, S.H.; Breen, C.I.; Hartman, S.J.; Natarajan, L.; Pierce, J.P.; Flatt, S.W.; Sears, D.D.; Patterson, R.E. Prolonged Nightly Fasting and Breast Cancer Prognosis. JAMA Oncol. 2016, 2, 1049–1055. [Google Scholar] [CrossRef]
- McHill, A.W.; Phillips, A.J.; Czeisler, C.A.; Keating, L.; Yee, K.; Barger, L.K.; Garaulet, M.; Scheer, F.A.; Klerman, E.B. Later circadian timing of food intake is associated with increased body fat. Am. J. Clin. Nutr. 2017, 106, 1213–1219. [Google Scholar] [CrossRef] [PubMed]
- Jakubowicz, D.; Barnea, M.; Wainstein, J.; Froy, O. High caloric intake at breakfast vs. dinner differentially influences weight loss of overweight and obese women. Obesity (Silver Spring) 2013, 21, 2504–2512. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Hollis, J.H. Associations between eating frequency and energy intake, energy density, diet quality and body weight status in adults from the USA. Br. J. Nutr. 2016, 115, 2138–2144. [Google Scholar] [CrossRef]
- Von Ruesten, A.; Brantsæter, A.L.; Haugen, M.; Meltzer, H.M.; Mehlig, K.; Winkvist, A.; Lissner, L. Adherence of pregnant women to Nordic dietary guidelines in relation to postpartum weight retention: Results from the Norwegian Mother and Child Cohort Study. BMC Public Health 2014, 14, 75. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.L.; Sotres-Alvarez, D.; Siega-Riz, A.M. Maternal dietary patterns during the second trimester are associated with preterm birth. J. Nutr. 2015, 145, 1857–1864. [Google Scholar] [CrossRef] [PubMed]
- Hillesund, E.R.; Bere, E.; Haugen, M.; Øverby, N.C. Development of a New Nordic Diet score and its association with gestational weight gain and fetal growth—A study performed in the Norwegian Mother and Child Cohort Study (MoBa). Public Health Nutr. 2014, 17, 1909–1918. [Google Scholar] [CrossRef] [PubMed]
- Saunders, L.; Guldner, L.; Costet, N.; Kadhel, P.; Rouget, F.; Monfort, C.; Thomé, J.P.; Multigner, L.; Cordier, S. Effect of a Mediterranean diet during pregnancy on fetal growth and preterm delivery: Results from a French Caribbean mother–child cohort study (TIMOUN). Paediatr. Perinat. Epidemiol. 2014, 28, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Dietary Guidelines Advisory Committee. Scientific Report of the 2015 Dietary Guidelines Advisory Committee; US Department of Health and Human Services: Washington, DC, USA; USDA: Washington, DC, USA, 2015.
- Health Promotion Board Singapore. Pregnancy and Diet. Ministry of Health: Singapore, 2013. Available online: http://www.hpb.gov.sg/HOPPortal/health-article/3826 (accessed on 23 August 2013).
- Soh, S.E.; Tint, M.T.; Gluckman, P.D.; Godfrey, K.M.; Rifkin-Graboi, A.; Chan, Y.H.; Stünkel, W.; Holbrook, J.D.; Kwek, K.; Chong, Y.S.; et al. Cohort profile: Growing Up in Singapore Towards healthy Outcomes (GUSTO) birth cohort study. Int. J. Epidemiol. 2014, 43, 1401–1409. [Google Scholar] [CrossRef]
- Conway, J.M.; Ingwersen, L.A.; Vinyard, B.T.; Moshfegh, A.J. Effectiveness of the US Department of Agriculture 5-step multiple-pass method in assessing food intake in obese and nonobese women. Am. J. Clin. Nutr. 2003, 77, 1171–1178. [Google Scholar] [CrossRef]
- Han, C.Y.; Colega, M.; Quah, E.P.L.; Chan, Y.H.; Godfrey, K.M.; Kwek, K.; Saw, S.M.; Gluckman, P.D.; Chong, Y.S.; Chong, M.F.F.; et al. A healthy eating index to measure diet quality in pregnant women in Singapore: A crosssectional study. BMC Nutr. 2015, 1, 39. [Google Scholar] [CrossRef]
- Loy, S.L.; Chan, J.K.; Wee, P.H.; Colega, M.T.; Cheung, Y.B.; Godfrey, K.M.; Kwek, K.; Saw, S.M.; Chong, Y.S.; Natarajan, P.; et al. Maternal Circadian Eating Time and Frequency Are Associated with Blood Glucose Concentrations during Pregnancy. J. Nutr. 2017, 147, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Loy, S.L.; Cheng, T.S.; Colega, M.T.; Cheung, Y.B.; Godfrey, K.M.; Gluckman, P.D.; Kwek, K.; Saw, S.M.; Chong, Y.S.; Padmapriya, N.; et al. Predominantly night-time feeding and maternal glycaemic levels during pregnancy. Br. J. Nutr. 2016, 115, 1563–1570. [Google Scholar] [CrossRef] [PubMed]
- Chia, A.; Tint, M.A.; Han, C.Y.; Chen, L.W.; Colega, M.T.; Aris, I.M.; Chua, M.C.; Tan, K.H.; Yap, F.; Shek, L.P.; et al. Adherence to a healthy eating index for pregnant women is associated with lower neonatal adiposity in a multiethnic Asian cohort: The Growing Up in Singapore Towards healthy Outcomes (GUSTO) study. Am. J. Clin. Nutr. 2018, 107, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Gibney, M.J.; Wolever, T.M. Periodicity of eating and human health: Present perspective and future directions. Br. J. Nutr. 1997, 77, S3–S5. [Google Scholar] [CrossRef] [PubMed]
- Loy, S.L.; Ng, M.J.H.; Cheung, Y.B.; Godfrey, K.M.; Calder, P.C.; Lek, N.; Yap, F.; Müller-Riemenschneider, F.; Natarajan, P.; Chong, Y.S.; et al. Plasma omega-3 fatty acids in pregnancy are inversely associated with postpartum weight retention in a multi-ethnic Asian cohort. Am. J. Clin. Nutr. 2017, 105, 1158–1165. [Google Scholar] [CrossRef]
- Padmapriya, N.; Shen, L.; Soh, S.E.; Shen, Z.; Kwek, K.; Godfrey, K.M.; Gluckman, P.D.; Chong, Y.S.; Saw, S.M.; Müller-Riemenschneider, F. Physical activity and sedentary behavior patterns before and during pregnancy in a multi-ethnic sample of Asian Women in Singapore. Matern. Child Health J. 2015, 19, 2523–2535. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Gibson, J.; McKenzie-McHarg, K.; Shakespeare, J.; Price, J.; Gray, R. A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr. Scand. 2009, 119, 350–364. [Google Scholar] [CrossRef]
- Alberti, K.G.; Zimmet, P.Z. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet. Med. 1998, 15, 539–553. [Google Scholar] [CrossRef]
- De Onis, M.; Garza, C.; Victora, C.G.; Onyango, A.W.; Frongillo, E.A.; Martines, J. The WHO Multicentre Growth Reference Study: Planning, study design, and methodology. Food Nutr. Bull. 2004, 25, S15–S26. [Google Scholar] [CrossRef]
- Cheung, Y.B. Analysis of repeated measurements and clustered data. In Statistical Analysis of Human Growth and Development; CRC Press: Boca Raton, FL, USA, 2014; pp. 152–153. [Google Scholar]
- Royston, P. Multiple imputation of missing values. Stata J. 2004, 4, 227–241. [Google Scholar] [CrossRef]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; John Wiley & Sons: New York, NY, USA, 2004. [Google Scholar]
- Martins, A.P.; Benicio, M.H. Influence of dietary intake during gestation on postpartum weight retention. Rev. Saude. Publica 2011, 45, 870–877. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Davis, J.N.; Shearrer, G.E.; Tao, W.; Hurston, S.R.; Gunderson, E.P. Dietary variables associated with substantial postpartum weight retention at 1-year among women with GDM pregnancy. BMC Obes. 2017, 4, 31. [Google Scholar] [CrossRef] [PubMed]
- Sofer, S.; Stark, A.H.; Madar, Z. Nutrition targeting by food timing: Time-related dietary approaches to combat obesity and metabolic syndrome. Adv. Nutr. 2015, 6, 214–223. [Google Scholar] [CrossRef]
- Hatori, M.; Vollmers, C.; Zarrinpar, A.; DiTacchio, L.; Bushong, E.A.; Gill, S.; Leblanc, M.; Chaix, A.; Joens, M.; Fitzpatrick, J.A.; et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab. 2012, 15, 848–860. [Google Scholar] [CrossRef]
- Garaulet, M.; Gómez-Abellán, P. Timing of food intake and obesity: A novel association. Physiol. Behav. 2014, 134, 44–50. [Google Scholar] [CrossRef]
- Hsieh, S.D.; Muto, T.; Murase, T.; Tsuji, H.; Arase, Y. Association of short sleep duration with obesity, diabetes, fatty liver and behavioral factors in Japanese men. Intern. Med. 2011, 50, 2499–2502. [Google Scholar] [CrossRef][Green Version]
- Cipolla-Neto, J.; Amaral, F.G.; Afeche, S.C.; Tan, D.X.; Reiter, R.J. Melatonin, energy metabolism, and obesity: A review. J. Pineal Res. 2014, 56, 371–381. [Google Scholar] [CrossRef]
- Bo, S.; Fadda, M.; Castiglione, A.; Ciccone, G.; De Francesco, A.; Fedele, D.; Guggino, A.; Parasiliti Caprino, M.; Ferrara, S.; Vezio Boggio, M.; et al. Is the timing of caloric intake associated with variation in diet-induced thermogenesis and in the metabolic pattern? A randomized cross-over study. Int. J. Obes. 2015, 39, 1689–1695. [Google Scholar] [CrossRef]
- Shim, J.S.; Oh, K.; Kim, H.C. Dietary assessment methods in epidemiologic studies. Epidemiol. Health 2014, 36, e2014009. [Google Scholar] [CrossRef]
- Moran, L.J.; Sui, Z.; Cramp, C.S.; Dodd, J.M. A decrease in diet quality occurs during pregnancy in overweight and obese women which is maintained post-partum. Int. J. Obes. 2013, 37, 704–711. [Google Scholar] [CrossRef] [PubMed]
- Shloim, N.; Rudolf, M.; Feltbower, R.G.; Blundell-Birtill, P.; Hetherington, M.M. Israeli and British women’s wellbeing and eating behaviours in pregnancy and postpartum. J. Reprod. Infant Psychol. 2019, 37, 123–138. [Google Scholar] [CrossRef] [PubMed]

| Variable | Total (n = 687) | Non-Substantial PPWR <5 kg (n = 577) | Substantial PPWR ≥5 kg (n = 110) | pa |
|---|---|---|---|---|
| PPWR, kg | 1.1 ± 4.1 | −0.2 ± 2.9 | 7.7 ± 2.9 | <0.001 |
| Maternal age, years | 31.3 ± 5.2 | 31.6 ± 5.1 | 29.5 ± 5.1 | <0.001 |
| Ethnicity, n (%) | <0.001 | |||
| Chinese | 392 (57.1) | 349 (60.5) | 43 (39.1) | |
| Malay | 172 (25.0) | 132 (22.9) | 40 (36.4) | |
| Indian | 123 (17.9) | 96 (16.6) | 27 (24.5) | |
| Education, n (%) | 0.433 | |||
| None/Primary/Secondary | 243 (35.4) | 199 (34.5) | 44 (40.0) | |
| Post-secondary | 216 (31.4) | 186 (32.2) | 30 (27.3) | |
| Tertiary | 228 (33.2) | 192 (33.3) | 36 (32.7) | |
| Parity, n (%) | <0.001 | |||
| 0 | 246 (35.8) | 180 (31.2) | 66 (60.0) | |
| ≥1 | 441 (64.2) | 397 (68.8) | 44 (40.0) | |
| Employment status, n (%) | 0.825 | |||
| Unemployed | 227 (33.0) | 192 (33.3) | 35 (31.8) | |
| Employed | 460 (67.0) | 385 (66.7) | 75 (68.2) | |
| Night shift, n (%) | >0.950 | |||
| No | 656 (95.5) | 551 (95.5) | 105 (95.5) | |
| Yes | 31 (4.5) | 26 (4.5) | 5 (4.5) | |
| Physical activity, n (%) | 0.837 | |||
| <600 MET-min/week | 223 (32.5) | 187 (32.4) | 36 (32.7) | |
| 600 to <3000 MET-min/week | 343 (49.9) | 286 (49.6) | 57 (51.8) | |
| ≥3000 MET-min/week | 121 (17.6) | 104 (18.0) | 17 (15.5) | |
| BMI at ≤14 weeks’ gestation, kg/m2 | 23.6 ± 4.5 | 23.4 ± 4.3 | 24.8 ± 4.9 | 0.002 |
| Gestational weight gain, kg/week | 0.47 ± 0.13 | 0.46 ± 0.14 | 0.52 ± 0.13 | <0.001 |
| Total EPDS score | 7.4 ± 4.5 | 7.4 ± 4.4 | 7.3 ± 4.8 | 0.815 |
| Sleep duration, hours | 7.2 ± 1.8 | 7.1 ± 1.8 | 7.3 ± 1.8 | 0.494 |
| Bedtime, 24-h clock | 2312 ± 0105 | 2308 ± 0131 | 2331 ± 0341 | 0.120 |
| Gestational diabetes, n (%) | <0.001 | |||
| No | 557 (81.1) | 453 (78.5) | 104 (94.5) | |
| Yes | 130 (18.9) | 124 (21.5) | 6 (5.5) | |
| Mode of feeding, n (%) | 0.454 | |||
| Breastfeeding | 62 (9.0) | 53 (9.2) | 9 (8.2) | |
| Mixed feeding | 456 (66.4) | 387 (67.1) | 69 (62.7) | |
| Formula feeding | 169 (24.6) | 137 (23.7) | 32 (29.1) |
| Variable | Total (n = 687) | Non-Substantial PPWR <5 kg (n = 577) | Substantial PPWR ≥5 kg (n = 110) | pa |
|---|---|---|---|---|
| Day–night eating, n (%) | 0.170 | |||
| Day eating | 596 (86.8) | 505 (87.5) | 91 (82.7) | |
| Night eating | 91 (13.2) | 72 (12.5) | 19 (17.3) | |
| Night fasting intervals (hours), n (%) | 0.889 | |||
| <9 h | 184 (26.8) | 154 (26.7) | 30 (27.3) | |
| 9–10 h | 264 (38.4) | 224 (38.8) | 40 (36.4) | |
| 11–12 h | 239 (34.8) | 199 (34.5) | 40 (36.4) | |
| Eating episodes per day, n (%) | 0.794 | |||
| 1–3 times | 215 (31.3) | 180 (31.2) | 35 (31.8) | |
| 4 times | 218 (31.7) | 185 (32.1) | 33 (30.0) | |
| 5 times | 143 (20.8) | 122 (21.1) | 21 (19.1) | |
| 6–10 times | 111 (16.2) | 90 (15.6) | 21 (19.1) | |
| HEI-SGP score | 53.0 ± 13.9 | 53.6 ± 14.0 | 49.4 ± 12.7 | 0.003 |
| Diet Quality, n (%) | 0.004 | |||
| Higher | 344 (50.1) | 303 (52.5) | 41 (37.3) | |
| Lower | 343 (49.9) | 274 (47.5) | 69 (62.7) | |
| Total energy intake, kJ/day (1 kcal = 4.186 kJ) | 7890 ± 2358 | 7886 ± 2320 | 7914 ± 2561 | 0.908 |
| Substantial PPWR ≥5 kg | |||||
|---|---|---|---|---|---|
| Eating Patterns | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Day-night eating | |||||
| Day eating | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Night eating | 1.95 (1.05, 3.62) | 1.82 (0.96, 3.43) | 2.04 (1.07, 3.91) | 2.02 (1.05, 3.89) | 2.04 (1.06, 3.94) |
| Night fasting intervals | |||||
| <9 h | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 9–10 h | 0.81 (0.46, 1.43) | 0.88 (0.49, 1.58) | 0.87 (0.48, 1.58) | 0.85 (0.46, 1.54) | 0.87 (0.47, 1.59) |
| 11–12 h | 1.19 (0.65, 2.20) | 1.32 (0.70, 2.50) | 1.34 (0.71, 2.54) | 1.26 (0.66, 2.40) | 1.29 (0.67, 2.48) |
| Eating episodes per day | |||||
| ≤3 times | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 4 times | 1.12 (0.61, 2.05) | 1.16 (0.63, 2.14) | 1.14 (0.61, 2.11) | 1.17 (0.63, 2.20) | 1.21 (0.64, 2.27) |
| 5 times | 1.22 (0.59, 2.50) | 1.27 (0.61, 2.62) | 1.30 (0.62, 2.71) | 1.25 (0.60, 2.62) | 1.97 (0.61, 2.71) |
| ≥6 times | 1.93 (0.85, 4.37) | 1.96 (0.86, 4.49) | 2.14 (0.92, 4.97) | 2.15 (0.92, 5.03) | 2.20 (0.94, 5.17) |
| Diet quality | |||||
| Higher | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Lower | 1.91 (1.17, 3.10) | 1.94 (1.19, 3.17) | 1.81 (1.10, 2.97) | 1.84 (1.11, 3.03) | 1.82 (1.10, 3.01) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Loy, S.L.; Cheung, Y.B.; Colega, M.T.; Chia, A.; Han, C.Y.; Godfrey, K.M.; Chong, Y.-S.; Shek, L.P.-C.; Tan, K.H.; Lek, N.; et al. Associations of Circadian Eating Pattern and Diet Quality with Substantial Postpartum Weight Retention. Nutrients 2019, 11, 2686. https://doi.org/10.3390/nu11112686
Loy SL, Cheung YB, Colega MT, Chia A, Han CY, Godfrey KM, Chong Y-S, Shek LP-C, Tan KH, Lek N, et al. Associations of Circadian Eating Pattern and Diet Quality with Substantial Postpartum Weight Retention. Nutrients. 2019; 11(11):2686. https://doi.org/10.3390/nu11112686
Chicago/Turabian StyleLoy, See Ling, Yin Bun Cheung, Marjorelee T. Colega, Airu Chia, Chad Yixian Han, Keith M. Godfrey, Yap-Seng Chong, Lynette Pei-Chi Shek, Kok Hian Tan, Ngee Lek, and et al. 2019. "Associations of Circadian Eating Pattern and Diet Quality with Substantial Postpartum Weight Retention" Nutrients 11, no. 11: 2686. https://doi.org/10.3390/nu11112686
APA StyleLoy, S. L., Cheung, Y. B., Colega, M. T., Chia, A., Han, C. Y., Godfrey, K. M., Chong, Y.-S., Shek, L. P.-C., Tan, K. H., Lek, N., Chan, J. K. Y., Chong, M. F.-F., & Yap, F. (2019). Associations of Circadian Eating Pattern and Diet Quality with Substantial Postpartum Weight Retention. Nutrients, 11(11), 2686. https://doi.org/10.3390/nu11112686





