Abstract
Laparoscopic urological surgery has become a cornerstone in the management of diverse urological pathologies, offering substantial advantages over traditional open approaches. These benefits include minimized incisions, reduced tissue trauma, decreased intraoperative blood loss, lower postoperative pain, shorter hospital stays, superior cosmesis, and accelerated recovery. Despite these advantages, laparoscopic surgery carries inherent risks, with major vascular injury (MVI) representing one of the most severe and potentially life-threatening complications. This review examines the incidence, etiologies, and management strategies for MVI in laparoscopic urological surgery, emphasizing the critical role of early recognition, standardized protocols, and surgical expertise in optimizing patient outcomes.
1. Introduction
Laparoscopic urological surgery has evolved significantly and is now the gold standard for treating a broad spectrum of urological conditions. Compared to open surgery, laparoscopic techniques reduce morbidity, postoperative pain, and hospitalization duration while improving cosmetic results. These benefits have driven widespread adoption among urologists and patients alike. However, this approach is not without risk; though rare, complications can be severe [1,2], with major vascular injury (MVI) being the most critical, often necessitating emergent intervention and conversion to open surgery [3,4,5].
Consistent with the prior literature, MVI is defined as an injury to major vessels such as the aorta, vena cava, iliac, and mesenteric vessels [6], excluding minor injuries (e.g., epigastric, omental, or abdominal wall vessels). This review explores the incidence, risk factors, and contemporary management strategies for MVI in laparoscopic urological surgery.
2. Evidence Acquisition
A non-systematic review of the literature was performed. Medline, PubMed, the Cochrane Database, and Embase were used as search engines for clinical trials, randomized controlled trials, review articles, and prospective and retrospective studies regarding the vascular management of uro-laparoscopy surgeries.
3. Incidence and Risk Factors
Vascular injuries account for approximately half of all laparoscopic complications [7]. Although MVI is rare (incidence: 0.01–0.64%) [8,9], it carries significant mortality risks, particularly when involving the abdominal aorta, inferior vena cava, or their major branches (e.g., iliac and mesenteric vessels) [10,11].
The overall incidence of major complications in laparoscopic surgery is low (~2%) [8,9,12,13], with vascular injuries occurring in 0.22–1.1% of cases [14]. However, these injuries contribute to 8–17% of perioperative deaths [15] and frequently require emergent conversion to open repair [16]. Additionally, MVI management often demands central vascular access, blood transfusion, vasopressor support, and adherence to advanced resuscitation protocols [17].
A study of 5347 laparoscopic urological procedures reported MVI in the abdominal aorta (two cases) and external iliac vein (one case), representing the 0.05% [6]. Similarly, Cheng et al. documented injuries to the renal artery, inferior mesenteric artery, external/common iliac arteries, superior mesenteric artery, and vena cava [18].
MVI most commonly occurs during initial laparoscopic access, particularly with Veress needle or primary trocar insertion [19], potentially leading to puncture-related hemorrhage or air embolism [20]. Other etiologies include excessive traction, ultrasonic scalpel misuse, Hem-o-lock clip failure, and Endo-GIA stapler malfunction.
4. Management Strategies
Cheng et al. advocate a systematic approach to MVI management [18]:
- Immediate Hemostasis: Identify and compress/clamp the bleeding site.
- Visual Optimization: Clear the surgical field to assess the injury.
- Resuscitation Preparedness: Mobilize resources for fluid/blood product administration.
- Pneumoperitoneum Adjustment: Temporarily increase pressure to reduce venous bleeding.
- Trocar Placement: Insert additional ports to facilitate repair.
- Vascular Exposure: Dissect and isolate the injured vessel.
- Definitive Repair: Suture or clamp the bleeding source.
- Temporary Occlusion: Apply bulldog clamps if needed.
- Conversion to Open Surgery: Proceed if laparoscopic repair is inadequate.
MVI represents an indication for conversion to open surgery [16]. However, when laparoscopic management of the complication is feasible, the initial surgical maneuver should focus on achieving rapid hemorrhage control through direct compression, followed by meticulous field exposure to identify the vascular defect and attempt its repair [21,22]. In the case of an MVI, consultation with a vascular surgeon is recommended, even if the complication is managed through a minimally invasive approach.
5. Prevention
Anatomic mastery remains fundamental to preventing vascular complications, particularly in complex minimally invasive procedures [23]. Given the technical demands of surgeries involving major vessels (e.g., retroperitoneal dissections or large renal masses [24], such cases should be reserved for experienced surgeons. Trainees should undergo rigorous simulation-based education (e.g., artificial models, virtual reality, and supervised hands-on experience) to prepare for high-risk scenarios [25].
The advent of precision surgery in urology emphasizes tailored approaches based on patient-specific anatomy and disease characteristics. Three-dimensional (3D) laparoscopy has demonstrated superior outcomes over conventional 2D systems by enhancing depth perception and spatial accuracy, particularly in complex procedures [26].
Three-dimensional printing technology enables the creation of patient-specific anatomical models for surgical preoperative planning, postoperative evaluation, and the development of training devices [27,28,29]. Its greatest strength lies in the production of highly complex structures, even in limited quantities or as single copies. These 3D-printed models provide an unparalleled level of personalization, as they are reconstructed directly from patient medical imaging, resulting in an exact 1:1 scale replica of the relevant anatomy.
A key advantage of 3D-printed anatomical models is their ability to enhance spatial understanding and mitigate surgical risks, particularly in vascular anatomy (Figure 1). By transforming medical imaging data into a tangible and intuitive format, these models allow surgeons to meticulously examine anatomical structures, identify variations or anomalies, and anticipate potential complications. They provide a physical representation of critical structures and spatial relationships, facilitating precise preoperative planning. Furthermore, surgeons can use these models to test and select optimal surgical instruments, thereby reducing intraoperative uncertainties and improving procedural safety [30].
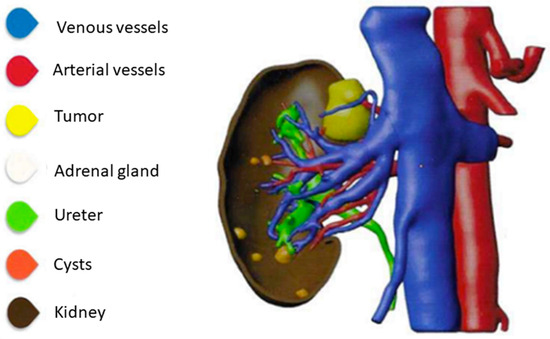
Figure 1.
Three-dimensional modeling of a renal tumor.
Hyde et al. examined the impact of interactive 3D virtual models on preoperative surgical decision-making. Their findings revealed that in 19% of cases, surgeons modified their planned approach after evaluating the 3D model. Additionally, surgeon confidence in decision-making improved significantly, with the 3D virtual model being consulted in four out of five patient datasets [31].
Porpiglia et al. assessed the utility of Hyper-Accuracy 3D models (HA3D™) in improving the visualization of renal arterial vasculature for perioperative planning during robotic partial nephrectomy for complex renal masses. The study demonstrated that the HA3D™ group had a significantly lower rate of global ischemia compared to the 2D group (23.8% vs. 80.6%, p < 0.01). Notably, 43% of patients in the HA3D™ group underwent selective clamping of secondary-order arterial branches of the renal artery. Furthermore, in 90.5% of HA3D™ cases, the intraoperative management of the renal pedicle matched the preoperative plan, underscoring the model’s precision in surgical planning [32].
In vascular surgery, where precision is paramount, 3D models offer a significant advantage by improving the visualization of intricate vessel networks and minimizing the risk of iatrogenic injury. This technology not only optimizes surgical outcomes but also serves as a valuable educational tool for training and interdisciplinary collaboration [33,34].
6. Recommendations for Training
To mitigate MVI risks, surgical curricula should integrate the following:
- -
- Three-dimensional simulation for preoperative rehearsal.
- -
- Structured mentorship in high-risk procedures.
- -
- Competency-based assessments prior to independent practice [27].
7. Conclusions
Although rare, MVI in laparoscopic urological surgery poses significant challenges due to its potential for catastrophic outcomes. Early recognition, protocol-driven management, and surgeon experience are pivotal to improving survival. Continued advancements in imaging, simulation, and technique standardization—coupled with enhanced training—will further reduce MVI incidence. By prioritizing proactive prevention and systematic intervention, urologists can ensure safer laparoscopic procedures with optimal patient outcomes.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study.
Acknowledgments
We extend our gratitude to Ignacio Castillón Vela for his generous and selfless contribution in providing images of 3D models used in his case studies.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Lin, Y.-H.; Chung, H.-J.; Lin, A.T.; Chang, Y.-H.; Huang, W.J.; Hsu, Y.-S.; Chang, S.-C.; Chen, K.-K. Complications of Pure Transperitoneal Laparoscopic Surgery in Urology: The Taipei Veterans General Hospital Experience. J. Chin. Med. Assoc. 2007, 70, 481. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Guo, J.; Zeng, Z.; Cao, R.; Hu, J. Intraoperative serious complications of laparoscopic urological surgeries: A single institute experience of 4,380 procedures. Int. Braz. J. Urol. 2019, 45, 739–746. [Google Scholar] [CrossRef] [PubMed]
- Furriel, F.T.G.; Laguna, M.P.; Figueiredo, A.J.C.; Nunes, P.T.C.; Rassweiler, J.J. Training of European urology residents in laparoscopy: Results of a pan-European survey. BJU Int. 2013, 112, 1223–1228. [Google Scholar] [CrossRef] [PubMed]
- Guillonneau, B.; Abbou, C.C.; Doublet, J.D.; Gaston, R.; Janetschek, G.; Mandressi, A.; Rassweiler, J.J.; Vallancien, G. Proposal for a ‘European Scoring System for Laparoscopic Operations in Urology’. Eur. Urol. 2001, 40, 2–6; discussion 7. [Google Scholar] [CrossRef]
- Ghavamian, R. Complications of Laparoscopic and Robotic Urologic Surgery; Springer Science & Business Media: New York, NY, USA, 2010. [Google Scholar]
- Simforoosh, N.; Basiri, A.; Ziaee, S.-A.; Tabibi, A.; Nouralizadeh, A.; Radfar, M.H.; Sarhangnejad, R.; Mirsadeghi, A. Major vascular injury in laparoscopic urology. JSLS J. Soc. Laparoendosc. Surg. 2014, 18, e2014-00283. [Google Scholar] [CrossRef]
- Gaur, D.D. Retroperitoneal and pelvic extraperitoneal laparoscopy: An international perspective. Urology 1998, 52, 566–571. [Google Scholar] [CrossRef]
- Makai, G.; Isaacson, K. Complications of Gynecologic Laparoscopy. Clin. Obstet. Gynecol. 2009, 52, 401. [Google Scholar] [CrossRef]
- Saidi, M.H.; Vancaillie, T.G.; White, A.J.; Sadler, R.K.; Akright, B.D.; Farhart, S.A. Complications of major operative laparoscopy. A review of 452 cases. J. Reprod. Med. 1996, 41, 471–476. [Google Scholar]
- McDonald, P.T.; Rich, N.M.; Collins, G.J.; Andersen, C.A.; Kozloff, L. Vascular trauma secondary to diagnostic and therapeutic procedures: Laparoscopy. Am. J. Surg. 1978, 135, 651–655. [Google Scholar] [CrossRef]
- Nordestgaard, A.G.; Bodily, K.C.; Osborne, R.W., Jr.; Buttorff, J.D. Major vascular injuries during laparoscopic procedures. Am. J. Surg. 1995, 169, 543–545. [Google Scholar] [CrossRef]
- Vilos, G.; Ternamian, A.; Dempster, J.; Lefebvre, G.; Allaire, C.; Arneja, J.; Birch, C.; Dempsey, T.; Laberge, P.Y.; Leduc, D.; et al. Laparoscopic Entry: A Review of Techniques, Technologies, and Complications. J. Obstet. Gynaecol. Can. 2007, 29, 433–447. [Google Scholar] [CrossRef]
- Azevedo, J.L.M.C.; Azevedo, O.C.; Miyahira, S.A.; Miguel, G.P.; Becker, O.M., Jr.; Hypólito, O.H.M.; Machado, A.C.C.G.; Cardia, W.; Yamaguchi, G.A.; Godinho, L.; et al. Injuries caused by Veress needle insertion for creation of pneumoperitoneum: A systematic literature review. Surg. Endosc. 2009, 23, 1428–1432. [Google Scholar] [CrossRef]
- Castillo, O.A.; Peacock, L.; Vitagliano, G.; Pinto, I.; Portalier, P. Laparoscopic repair of an iliac artery injury during radical cystoprostatectomy. Surg. Laparosc. Endosc. Percutan Tech. 2008, 18, 315–318. [Google Scholar] [CrossRef] [PubMed]
- Roviaro, G.C.; Varoli, F.; Saguatti, L.; Vergani, C.; Maciocco, M.; Scarduelli, A. Major vascular injuries in laparoscopic surgery. Surg. Endosc. Other Interv. Tech. 2002, 16, 1192–1196. [Google Scholar] [CrossRef] [PubMed]
- Sandadi, S.; Johannigman, J.A.; Wong, V.L.; Blebea, J.; Altose, M.D.; Hurd, W.W. Recognition and management of major vessel injury during laparoscopy. J. Minim. Invasive Gynecol. 2010, 17, 692–702. [Google Scholar] [CrossRef] [PubMed]
- Asfour, V.; Smythe, E.; Attia, R. Vascular injury at laparoscopy: A guide to management. J. Obstet. Gynaecol. 2018, 38, 598–606. [Google Scholar] [CrossRef]
- Cheng, S.; Zheng, Q.; Xu, L.; Zhao, W.; Li, G.; Ding, G. Management of major vascular injury in laparoscopic urology. Laparosc. Endosc. Robot. Surg. 2020, 3, 107–110. [Google Scholar] [CrossRef]
- Dunne, N.; Booth, M.I.; Dehn, T.C.B. Establishing pneumoperitoneum: Verres or Hasson? The debate continues. Ann. R. Coll. Surg. Engl. 2011, 93, 22–24. [Google Scholar] [CrossRef]
- Lafullarde, T.; Van Hee, R.; Gys, T. A safe and simple method for routine open access in laparoscopic procedures. Surg. Endosc. 1999, 13, 769–772. [Google Scholar] [CrossRef]
- Jafari, M.D.; Pigazzi, A. Techniques for laparoscopic repair of major intraoperative vascular injury: Case reports and review of literature. Surg. Endosc. 2013, 27, 3021–3027. [Google Scholar] [CrossRef]
- Li, P.; Mao, D.; Zhou, J.; Sun, H. Management of inferior vena cava injury and secondary thrombosis after percutaneous nephrolithotomy: A case report. J. Int. Med. Res. 2021, 49, 3000605211058868. [Google Scholar] [CrossRef]
- Rogers, C.G.; Singh, A.; Blatt, A.M.; Linehan, W.M.; Pinto, P.A. Robotic partial nephrectomy for complex renal tumors: Surgical technique. Eur. Urol. 2008, 53, 514–521. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gill, I.S.; Kavoussi, L.R.; Lane, B.R.; Blute, M.L.; Babineau, D.; Colombo, J.R.; Frank, I.; Permpongkosol, S.; Weight, C.J.; Kaouk, J.H.; et al. Comparison of 1,800 laparoscopic and open partial nephrectomies for single renal tumors. J. Urol. 2007, 178, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Simhan, J.; Smaldone, M.C.; Tsai, K.J.; Li, T.; Reyes, J.M.; Canter, D.; Kutikov, A.; Chen, D.Y.; Greenberg, R.E.; Uzzo, R.G.; et al. Perioperative outcomes of robotic and open partial nephrectomy for moderately and highly complex renal lesions. J. Urol. 2012, 187, 2000–2004. [Google Scholar] [CrossRef] [PubMed]
- Najib, I.D.; Wang, Q.; Wang, S. Two-Dimensional Versus Three-Dimensional Laparoscopic Systems in Urology: A Systematic Review and Meta-Analysis. J. Endourol. 2018, 32, 781–790. [Google Scholar] [CrossRef]
- Piramide, F.; Kowalewski, K.-F.; Cacciamani, G.; Belenchon, I.R.; Taratkin, M.; Carbonara, U.; Marchioni, M.; De Groote, R.; Knipper, S.; Pecoraro, A.; et al. Three-dimensional Model-assisted Minimally Invasive Partial Nephrectomy: A Systematic Review with Meta-analysis of Comparative Studies. Eur. Urol. Oncol. 2022, 5, 640–650. [Google Scholar] [CrossRef]
- Checcucci, E.; Amparore, D.; Fiori, C.; Manfredi, M.; Ivano, M.; Di Dio, M.; Niculescu, G.; Piramide, F.; Cattaneo, G.; Piazzolla, P.; et al. 3D imaging applications for robotic urologic surgery: An ESUT YAUWP review. World J. Urol. 2020, 38, 869–881. [Google Scholar] [CrossRef]
- Cacciamani, G.E.; Okhunov, Z.; Meneses, A.D.; Rodriguez-Socarras, M.E.; Rivas, J.G.; Porpiglia, F.; Liatsikos, E.; Veneziano, D. Impact of Three-dimensional Printing in Urology: State of the Art and Future Perspectives. A Systematic Review by ESUT-YAUWP Group. Eur. Urol. 2019, 76, 209–221. [Google Scholar] [CrossRef]
- Marconi, S.; Negrello, E.; Mauri, V.; Pugliese, L.; Peri, A.; Argenti, F.; Auricchio, F.; Pietrabissa, A. Toward the improvement of 3D-printed vessels’ anatomical models for robotic surgery training. Int. J. Artif. Organs 2019, 42, 558–565. [Google Scholar] [CrossRef]
- Hyde, E.R.; Berger, L.U.; Ramachandran, N.; Hughes-Hallett, A.; Pavithran, N.P.; Tran, M.G.B.; Ourselin, S.; Bex, A.; Mumtaz, F.H. Interactive virtual 3D models of renal cancer patient anatomies alter partial nephrectomy surgical planning decisions and increase surgeon confidence compared to volume-rendered images. Int. J. Comput. Assist. Radiol. Surg. 2019, 14, 723–732. [Google Scholar] [CrossRef]
- Porpiglia, F.; Fiori, C.; Checcucci, E.; Amparore, D.; Bertolo, R. Hyperaccuracy Three-dimensional Reconstruction Is Able to Maximize the Efficacy of Selective Clamping During Robot-assisted Partial Nephrectomy for Complex Renal Masses. Eur. Urol. 2018, 74, 651–660. [Google Scholar] [CrossRef]
- Kang, S.K.; Zhang, A.; Pandharipande, P.V.; Chandarana, H.; Braithwaite, R.S.; Littenberg, B. DWI for Renal Mass Characterization: Systematic Review and Meta-Analysis of Diagnostic Test Performance. AJR Am. J. Roentgenol. 2015, 205, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Sighinolfi, M.C.; Menezes, A.D.; Patel, V.; Moschovas, M.; Assumma, S.; Calcagnile, T.; Panio, E.; Sangalli, M.; Turri, F.; Sarchi, L.; et al. Three-Dimensional Customized Imaging Reconstruction for Urological Surgery: Diffusion and Role in Real-Life Practice from an International Survey. J. Pers. Med. 2023, 13, 1435. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).