Abstract
Endodontic perforations are serious complications encountered in the dental setting. Early detection, diagnosis, and proper management of perforations are crucial for a favorable prognosis. However, there are a limited number of studies that provide an overview of perforations, emphasizing these three strategies: prevention, diagnostic challenges, and management. The objective of this narrative review is to highlight the multifaceted components of endodontic perforations while also identifying the most effective methods used in their detection, diagnosis, and management. An electronic literature search was conducted using various databases and applying keywords for articles published in English. Eligible papers were reviewed further to gather relevant information. The results of the literature search found that, although perforations are relatively uncommon occurrences in the clinical setting, they still need to be understood for the prevention and treatment of these iatrogenic complications. The combination of case complexity and limited operator experience often determines the likelihood of endodontic perforation occurrence. Accurate diagnosis and identification of perforations rely heavily on the combination of clinical examination and advanced imaging technologies. In recent times, new technologies have emerged and hope to contribute to a decreased occurrence of endodontic perforations and increased prognosis in cases that do arise.
1. Introduction
Endodontic perforations are characterized as “a communication between the root canal system and the external tooth surface [1].” In simple terms, perforations manifest as inadvertent holes extending from a tooth’s pulp to the outer surface of the root, which leads to the pulp’s interaction with the external environment of the adjacent tissues enclosing the tooth. Perforations are a major setback of root canal therapy, often manifesting as iatrogenic complications caused by a combination of case complexity and operator experience level. If left untreated, it can severely impact oral health [2]. Iatrogenic endodontic root perforations are different from pathologic root perforation caused by resorptive processes and inflammatory products of lesions as a sequelae of caries [2]. Endodontic perforations are often caused by malalignment of burs, files, or engine-driven endodontic instruments as the operator navigates the root canals. They can occur at any stage of root canal therapy, such as access cavity preparation, canal shaping, cleaning, and preparation. Consequences include secondary periodontal infections, abscess formation, fistula emergence, and an uncertain prognosis of the affected teeth, leading to potential tooth loss, ultimately negatively impacting the quality of life of the patient [2,3]. The incidence of perforation seen in the literature ranges from 0.6% to 17.6% in the clinical setting [4]. Endodontic perforations are the second highest cause of failed endodontically treated teeth, leading to 9.62% of all endodontic failures [3]. These statistics are high, and with the advent of advanced technologies such as the use of microscopes, ultrasonics, nickel titanium instruments, electronic apex locators, and CBCT, the expectation is for a reduction in the incidence of endodontic perforations. Some inherent factors that also contribute to endodontic perforations are the competency level of the operator, in the case of a dental school student versus an experienced endodontic specialist, or an altered pathological presentation of the tooth, such as caries or root resorption. Over the years, dental materials such as indium foil, super 2-ethoxybenzoic acid (super EBA), zinc oxide eugenol (ZOE), amalgam, Cavit, and composite resin have been used to repair perforations with varied success [5]. Bioactive materials such as calcium hydroxide, mineral trioxide aggregate, calcium silicate cements, and bioceramic nanotechnology have also been used with increased success [5]. We reviewed the literature to identify the key variables that lead to endodontic perforation, with a focus on the usefulness of CBCT in the prevention of perforations, diagnostic strategies to maximize their identification, and exploration of the current and future technologies used to optimize the prognosis and management of this endodontic complication.
2. Materials and Methods
This narrative review was conducted to synthesize contemporary knowledge surrounding endodontic perforations. A structured literature search was conducted across five major electronic databases to investigate relevant studies on endodontic perforation. Search criteria for PubMed, SCOPUS, EMBASE, Google Scholar, and Web of Science databases included keywords ‘endodontic perforation,’ ‘root canal perforation’ and ‘endodontic perforation CBCT.’ Boolean operators AND/OR were used to combine search terms and refine results. This search was limited to peer-reviewed journal articles published in English after the year of 2010. This timeframe limitation was implemented to capture research reflecting the most current knowledge, considering the growing clinical adoption of CBCT technology, advances in bioceramic materials, and contemporary treatment and prevention strategies currently being utilized in clinical practice. After title and abstract screening, 27 articles were included in the study. Each article was assessed for relevance, study design, and contribution to a clinical understanding of endodontic perforations. A detailed list of the included studies by type and focus area is presented in Table 1. This structured narrative approach allowed us to identify and integrate key themes and advancements in the fields, providing clinicians with a practical overview of diagnosis, management, and prevention of endodontic perforations.

Table 1.
The article type, article count, and study focus are presented in the table.
Inclusion Criteria:
- -
- Peer-reviewed articles published in English after the year 2010;
- -
- Clinical studies, review articles, and case series related to endodontic perforations;
- -
- Studies specifically addressing classification, diagnosis, prevention, or repair of endodontic perforations, including those evaluating CBCT applications.
Exclusion Criteria:
- -
- Articles published before 2010;
- -
- Non-English language publications without available translations;
- -
- Editorials, abstract-only publications, and studies not directly related to endodontic perforations.
3. Results
The data search identified a total of 27 relevant publications, which included 7 case reports, 4 official American Association of Endodontics (AAE) guideline standards, 2 comparative studies, 2 retrospective studies, 1 cross-sectional study, and 11 reviews (Table 1).
4. Discussion
4.1. Classifications
Endodontic perforations are commonly classified according to both the time of occurrence relative to the root canal treatment and the location of the perforation [2]. It is important to note that a perforation may occur at any phase during the process of endodontic treatment [3]. The three classifications based on the procedural stage of endodontic treatment include pre-operative, intra-operative, and post-operative perforations [2]. Pre-operative, or pathologic perforations, occur through extensive decay, trauma, and resorption of the root prior to root canal treatment [2,3,6]. Both intra-operative and post-operative perforations are complications that arise during dental treatment due to various factors, including case complexity, operator experience level, instrumentation techniques, and pathological considerations [7,8,9,10]. Intra-operative perforations are caused by access cavity preparation and canal instrumentation, whereas post-operative perforations occur when preparing and placing a post for the final restoration [2,6].
As noted, there are also many classifications of perforations based on the location of their occurrence. Coronal versus radicular perforation are the two broadest categories that distinguish the location based upon whether they occur in either the crown or root portions of the tooth [3]. One can further specify the perforation site by dividing the root of the tooth into its coronal, middle, and apical thirds [3]. Within these divisions, there are many subcategories, including furcal, strip, and crestal perforations, among others [2,11]. A furcal perforation occurs in the furcation area, which is where the roots of multi-rooted teeth diverge [11]. A strip perforation is commonly noted in the lateral wall of the root and is frequently associated with curved canals [1]. Crestal perforations occur near or at the level of epithelial attachment of the alveolar bone crest [11]. Understanding the various classifications of perforations provides insight into the potential challenges during root canal therapy (Figure 1). In addition, recognizing the factors that predispose a case to such mishaps is equally critical in preventing their occurrence.
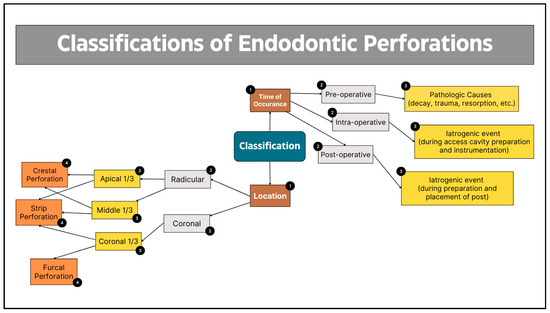
Figure 1.
Flowchart elucidating the different characterizations of endodontic perforations.
4.2. Predisposition
Iatrogenic perforations and all endodontic mishaps are most likely to occur in a case categorized as ‘high difficulty,’ according to the AAE case difficulty form [7]. High-difficulty cases include those that involve the navigation of calcified canals, extensive decay, internal root resorption, tipped teeth, curved canals, dilacerated roots, and post-operative post placement [8,9,10]. Alongside the complexity of the case, a lack of experience on the part of the operator is another key factor that raises the risk of perforation [12]. In some cases, perforations and other iatrogenic complications occur due to the clinician’s lack of knowledge regarding the internal anatomy of the tooth and failure to account for the potential anatomical variations present in each individual case [3]. The combination of a difficult case and an inexperienced operator makes perforations particularly common in the pre-doctoral student clinic setting [7]. The prevalence of endodontic perforations, particularly in complex cases, emphasizes the critical need for meticulous procedural standards and, in some cases, endodontic specialist intervention. This is reflected in the AAE Treatment Standards, and prognosis for such perforations varies greatly depending on size, location, and time of treatment (Figure 2) [13].
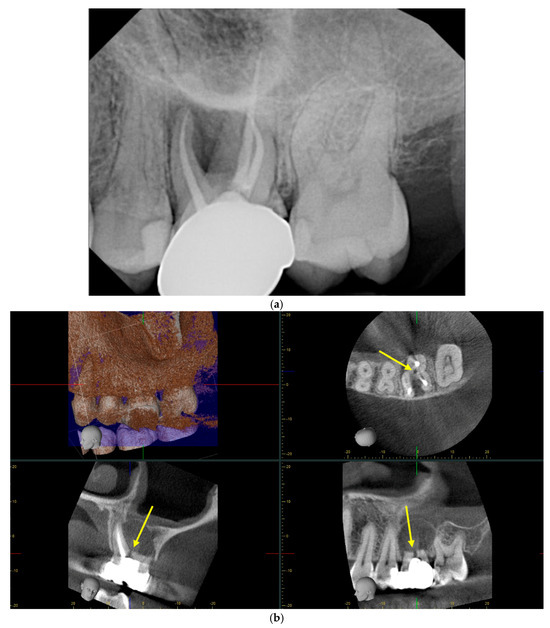
Figure 2.
Periapical radiograph versus CBCT illustrating the same furcal perforation on tooth #14: (a) in the periapical radiograph, the perforation is not well visualized due to the angulation of the image; (b) in this series of CBCT images, the perforation is much easier visualized (yellow arrows), attributed to the multiple planes of view.
4.3. Prognosis
The AAE Standard Practice and Treatment Options for the Compromised Tooth outlines the prognosis of perforated teeth. The best prognosis is a ‘small, apical perforation with no sulcular communication or osseous defect treated immediately’ [14,15]. The least favorable prognosis is a ‘large, apical, crestal, or furcal lesion communicating with the adjacent surrounding tissues and a probing defect with periodontal bone destruction that is not repaired’ [15]. Any diagnosis after seventy-two hours is less favorable, making efficient and accurate diagnosis critical to treatment prognosis [14]. Interestingly, endodontic perforations on the maxillary arch have a significantly greater prognosis when compared with their mandibular counterparts [2,10]. This may be due in part to the abundant vascular supply to the maxilla relative to the mandible [10]. These reports from the AAE and the literature show that there are many factors involved in the prognosis of this complication, and the AAE recommends that perforations are best treated by an endodontist, as it is not always possible to treat them non-surgically [13,14,15]. Understanding prognostic variability is essential in guiding treatment decisions and improving outcomes. On the opposite side of the spectrum, it is equally important to recognize the potential consequences of untreated or poorly managed perforations, which can have a significant impact on a patient’s oral health.
4.4. Consequences
Early detection of perforations is essential to minimize adverse effects. One poor outcome of perforations undetected during endodontic treatment is the extrusion of irrigants and materials into the surrounding tissue enclosing the tooth [13]. Siew et al. stated “The aim of repairing perforation is to regain and maintain healthy periodontium that is adjacent to the perforation site so that it is free from persistent inflammation” [10]. The consequences of perforations are complex. Due to the interaction between endodontic and periodontal tissues, these potential consequences include infection, pain, swelling, bone loss, and tooth loss [10,16]. The risk of endodontic failure is 10–12% greater in cases with perforations [12]. Hence, each clinical case must be carefully reviewed to determine the extent of perforation, presence or absence of infection, time of perforation occurrence, and periodontal status of the patient to form a personalized treatment plan.
4.5. Clinical Diagnosis
The clinical diagnosis of an endodontic perforation is challenging because there are no pathognomonic symptoms of this complication, making the signs of root canal perforation limited and nonspecific [17,18]. The first indication of root perforation is typically bleeding from the defect within the canal, especially seen if a perforation develops at the coronal aspect of a tooth [2,3]. However, this is not a reliable method of identification when cases involve open apices, internal resorption, and other systemic conditions, as they also are associated with excessive bleeding, potentially leading to a misdiagnosis [6]. For smaller perforations, evaluation using paper points may sometimes reveal bleeding if the hole arises further within the canal near the tissues and vasculature [2,6]. In root canal therapy cases where analgesic control is insufficient, patients may report unexpected discomfort immediately following a perforation [2,3]. With modern technology, we have additional clinical tools to assist in the identification and diagnosis of perforations, including apex locators and microscopes [6,17]. Microscopes have become quite useful in the identification of the location and size of perforations due to enhancing both the visualization and illumination of each case, resulting in an increased ability to diagnose and repair [2,3,14]. Another instrument used to assist in the diagnosis of perforations is the electronic apex locator. Although typically used to determine working length during endodontic treatment, an apex locator is an excellent tool to identify the presence of a perforation [2]. An apex locator functions by completing a circuit to alert the clinician when the file has reached tissue consistent with the periodontal ligament [3]. When the device reads zero and reaches the periodontal ligament at a depth much shorter than the estimated working length, it is likely a perforation [3]. The greatest limitation when using these methods is the timing, as these are only effective prior to obturation [17]. With the limitations of accurate clinical diagnosis, radiographic diagnosis is crucial when identifying endodontic perforations.
4.6. Radiographical Diagnosis
Radiographs play a critical role in the diagnosis of endodontic perforations, providing crucial imaging that guides clinical decision-making throughout the treatment process. Endodontic perforations are often clinically asymptomatic, making radiographical methods vital for accurate diagnosis [19]. Traditionally, periapical radiographs have been used as the primary imaging technique in the diagnosis, treatment, and post-operative follow-up of endodontic perforation [2,19]. However, periapical radiographs have limitations due to their two-dimensionality, making the determination of the location and severity of perforations challenging [2,3,19]. Additionally, it is sometimes impractical to use two-dimensional imaging, as perforations are often superimposed on intact root structure and filling materials, which creates artifacts, making them difficult to distinguish [2]. In recent times, cone-beam computed tomography (CBCT) imaging systems have become more popular in the diagnosis and treatment of endodontic perforations [2,19]. CBCT imaging allows providers to see in three dimensions, ultimately providing more conclusive information through fine detailing of root canal anatomy and any present lesions [6,19,20]. In general, imaging with a small FOV is preferred for the detection and treatment planning of perforations due to an increased image quality caused by the reduction in scatter [2]. In recent years, clinicians have debated whether CBCT imaging is a superior radiological diagnostic method or if traditional periapical radiographs should continue to be the primary radiographic diagnostic method.
4.7. CBCT versus Periapical Radiographs
Several studies have investigated the accuracy of the different radiographic methods used in the diagnosis of perforations. It is indicated by Shemesh et al. that a single periapical radiograph can only detect a perforation with 40% accuracy, but by obtaining two differently angled periapical radiographs, one increases the ability to detect the perforation to 63% [17]. In the same study, a CBCT was significantly more accurate than all combinations of periapical radiographs, with an 87% accuracy in correctly identifying perforations [17]. In another study, researchers report having found that cases involving periapical endodontic lesions show between a 57.1% and 63% improvement in the quality detection of said lesion using a CBCT when compared to the detection using a periapical radiograph (Figure 2) [20,21]. Obtaining a CBCT during treatment is also beneficial in identifying the exact location of perforation occurrence in order to ensure conservative treatment methods, as the multiplanar presentation of images using a CBCT contributes considerably to positive clinical outcomes [2,19,21]. CBCT imaging is certainly beneficial to the diagnosis and treatment of perforations, but there is additional radiation exposure to the patient and an increased cost associated with a CBCT relative to a traditional periapical radiograph; hence, the use of a CBCT should be justified based on the ‘as low as reasonably achieved’ (ALARA) principle [17,20]. Alshamrani et al. suggested that the use of CBCT should only be considered if there is a possibility to alter the clinical course [3]. Additionally, CBCT imaging still has some of the classic radiographic limitations, including cases with the presence of radiopaque filling and gutta-percha, as they both may create beam hardening artifacts that mimic perforation [2,17,18]. Advances in radiography are certainly helpful in diagnosis, but it is important not to rely solely on any one diagnostic method and instead use a combination to ensure a higher chance of proper diagnosis.
4.8. Management
As stated previously, Siew et al. indicated that “The goal of repairing root perforation is to reestablish healthy periodontium adjacent to the perforation, freeing the site from inflammation, infection, and subsequent attachment loss” [10]. The effective management of perforations requires the clinician to seal the defect, usually with a biocompatible material, eliminating the connection between the pulp and external environment [3]. Perforations can be treated in one of two ways: surgically or non-surgically [2,10]. Management of these lesions depends on several factors, including time, extent, and location of the perforation [6,14,15]. Recent research suggests that these factors are no longer as indicative of prognosis since the introduction of the treatment material MTA, highlighting the great advancement in the management of this complication [2,12]. Perforations that are sealed immediately after identification typically have the best prognosis [3]. The overall success of perforation repair is about 72.5%; however, a meta-analysis performed by Siew et al. found an overall repair success rate with MTA of 80.9% [10]. Siew also mentioned that some studies indicate that the success of a root canal-treated tooth can be as high as 90% after perforation repair [10]. These are notable percentages, as the success of uncomplicated primary root canal therapy is also about 90%, highlighting the importance of thoroughly reviewing each case and considering perforation repair before extracting the tooth [10].
4.9. Repair Materials
Various materials have been used to repair endodontic perforations in the past. These include zinc oxide eugenol cement, gutta-percha, glass ionomer cement, and calcium hydroxide, among many others [2,10,12,22]. However, none of these materials provides the environment necessary for the re-establishment of healthy tissue, resulting in far from ideal perforation success rates [2]. In recent decades, biocompatible materials have been introduced and are quickly becoming popular options when repairing root perforations. The bioactive material MTA has been the material of choice in perforation repair for years, as it has had great success in the repair of perforation when compared to previous materials and allows for the re-establishment of healthy tissue [10,22]. Claduer and others stated that this is partly due to the bond strength of most dental materials being significantly reduced in the presence of moisture contamination, whereas MTA requires moisture for proper setting [2,10,22]. The major disadvantages of MTA are the potential discoloration of tooth structure and an extremely long setup time of approximately three hours [2,23,24]. In recent years, additional bioceramic materials such as Bio-C repair and biodentine have been introduced as a new subset of viable material options in the treatment of perforations (Figure 3). Research indicates that bioceramics have high compressive strength, good sealing ability, and quick setting time in an aqueous medium, and they have the potential to be the primary treatment material as the field continues to advance [6,11]. One of the advantages of Bio-C repair is that it is supplied in a ready-to-use form of putty, unlike its MTA counterpart [24,25]. Biodentine also has its advantages when compared to MTA, as it has been seen to be more effective in preventing dye leakage [23,24,25]. Although studies show that new bioceramics have certain advantages over MTA, historical evidence suggests that MTA still has great success in treating endodontic perforations and will continue to be a good treatment option, as more ongoing high-quality studies assess the newer bioceramic materials as the field continues to progress [25].
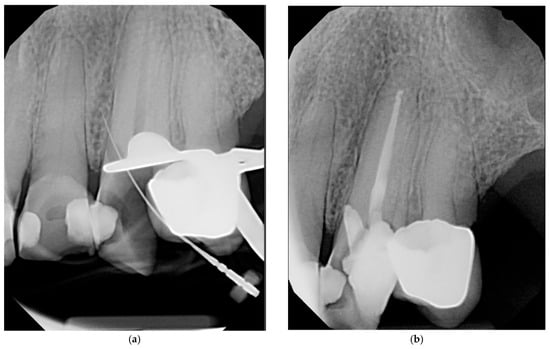
Figure 3.
Periapical radiographs illustrating the same crestal perforation on tooth #11: (a) periapical radiograph illustrating perforation intra-operatively; (b) periapical radiograph illustrating perforation immediately after repair using Bio-C repair putty.
4.10. Advanced Therapy
The field of endodontics is constantly evolving, and many new technologies have been developed to aid in advancements in treatment options. The use of 3D printing technology for guided endodontic access is a new method of treatment that can help avoid perforations during root canal therapy [26]. This method combines the technologies of CBCT and computer-aided design and computer-aided manufacturing (CAD/CAM) in order to prevent endodontic mishaps by increasing the predictability of root canal therapy [26]. This technology is extremely useful in cases of pulp canal obliteration and cases with difficult negotiation of canals [26]. The future direction of the field of endodontic therapy may rely more heavily on guided endodontics, as it has the potential to decrease the number of endodontic mishaps, including perforations. Additionally, other modern technologies have emerged to assist with the treatment of existing endodontic lesions. Regenerative endodontic treatment uses tissue engineering strategies as an alternative for treating endodontic lesions [27]. A handful of studies have shown successful attempts at managing endodontic lesions through regenerative endodontic procedures [28]. Given the recent advancements in endodontics, these two methods show promising results and may be efficacious alternatives in the management of challenging endodontic lesions in the near future, potentially leading to the revolutionization of the field of endodontics.
5. Conclusions
Endodontic perforations are serious complications that impact a patient’s oral health, reduce the prognosis of root canal therapy, and ultimately impact quality of life. Though endodontic perforations can be iatrogenic or pathological, it is of utmost importance for the practitioner to know the limitations of experience and expertise and make appropriate referrals to endodontists in endodontic cases beyond their comfort level. Accurate clinical and radiographic diagnoses are important, as well as elapsed time before treatment, perforation location, and size. Treatment with bioactive material such as MTA has been shown to be an effective biological sealing technique with good outcomes28. The continued innovation of current and new technologies focused on both the prevention and treatment of perforations will help continue reducing the risk of endodontic perforations in the clinical setting while increasing prognosis in cases that do arise.
5.1. Study Limitations
Despite the broad nature of this narrative review, several limitations should be acknowledged. First, this review is inherently constrained by the availability of studies published in English after the year 2010, which may exclude relevant findings from earlier research or studies in other languages. The search focuses on CBCT and its usefulness in the prevention of endodontic complications, which limits the articles included. Additionally, the review relies on a limited number of comparative and retrospective studies, which may impact the generalizability of the findings. The lack of standardized reporting in studies on perforations also makes it difficult to establish definitive guidelines. However, the synthesis of vital information on perforations presented in this paper serves as a quick reference for general dentists and endodontists.
5.2. Future Prospects
Future research should focus on several key areas to enhance the understanding of the prevention, diagnosis, and management of endodontic perforations. First, there is a need for well-designed studies comparing the imaging modalities of CBCT versus periapical radiographs. This will help establish more definitive guidelines on when advanced imaging techniques should be utilized. Prospective studies and clinical trials should also examine the long-term efficacy of various perforation repair materials, particularly the newer bioceramic materials such as Bio-C repair and biodentine. Another promising area for research is the application of artificial intelligence in endodontic diagnostics, which could help in the early detection and classification of perforations. Lastly, future studies should further explore the potential of regenerative endodontic procedures in managing perforations, particularly in cases where traditional treatments may not be an option. Advancements in these areas will be critical in improving evidence-based treatment outcomes and prevention methods for endodontic perforations.
Author Contributions
Conceptualization, T.M.D., N.L.P., and A.F.D.; methodology, T.M.D., N.L.P., and A.F.D.; investigation, T.M.D. and N.L.P.; writing—original draft preparation, T.M.D. and N.L.P.; writing—review and editing, T.M.D., N.L.P., and A.F.D.; supervision, A.F.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not Applicable.
Informed Consent Statement
Not Applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AAE | American Association of Endodontics |
| CBCT | Cone-beam computed tomography |
| FOV | Field of view |
| MTA | Mineral trioxide aggregate |
References
- American Association of Endodontists. Glossary of Endodontic Terms 2016; American Association of Endodontists: Chicago, IL, USA, 2015; Volume 9, Available online: https://www.aae.org/specialty/clinical-resources/glossary-endodontic-terms/ (accessed on 3 July 2025).
- Cauder, T. Present status and future directions-Managing perforations. Int. Endod. J. 2022, 55, 872–891. [Google Scholar] [CrossRef]
- Alshamrani, A.S.; Almusharraf, A.Y.; Alshammari, K.A.; Ali, E.J.; Almutairi, H.H.; Farrash, F.A.; Alghamdi, H.S.; Alqahtani, A.A.; Alosaimi, A.A. Causes, diagnosis, treatment and prognosis of root perforations. Int. J. Community. Med. Public Health 2023, 10, 351–356. [Google Scholar] [CrossRef]
- Sarao, S.K.; Berlin-Broner, Y.; Levin, L. Occurrence and Risk Factors of Dental Root Perforations: A Systematic Review. Int. Dent. J. 2020, 71, 96–105. [Google Scholar] [CrossRef]
- Asthana, G.; Bhargava, S. Bioactive Materials: A Comprehensive Review. Sch. J. App. Med. Sci. 2014, 2, 3231–3237. [Google Scholar]
- Estrela, C.; Decurcio, D.D.A.; Rossi-Fedele, G.; Silva, J.A.; Guedes, O.A.; Borges, Á.H. Root perforations: A review of diagnosis, prognosis and materials. Braz. Oral Res. 2018, 32, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Haug, S.R.; Solfjeld, A.F.; Ranheim, L.E.; Bårdsen, A. Impact of Case Difficulty on Endodontic Mishaps in an Undergraduate Student Clinic. J. Endod. 2018, 44, 1088–1095. [Google Scholar] [CrossRef] [PubMed]
- Casadei, B.D.A.; Lara-Mendes, S.T.D.O.; Barbosa, C.D.F.M.; Araújo, C.V.; de Freitas, C.A.; Machado, V.C.; Santa-Rosa, C.C. Access to original canal trajectory after deviation and perforation with guided endodontic assistance. Aust. Endod. J. 2020, 46, 101–106. [Google Scholar] [CrossRef]
- Alquthami, H.; Almalik, A.M.; Alzahrani, F.F.; Badawi, L. Successful management of teeth with different types of endodontic-periodontal lesions. Case Rep. Dent. 2018, 2018, 7084245. [Google Scholar] [CrossRef]
- Siew, K.; Lee, A.H.C.; Cheung, G.S.P. Treatment outcome of repaired root perforation: A systematic review and meta-analysis. J. Endod. 2015, 41, 1795–1804. [Google Scholar] [CrossRef]
- Kakani, A.M.; Veeramachaneni, C.; Majeti, C.; Tummala, M.; Khiyani, L. A Review on Perforation Repair Materials. J. Clin. Diagn. Res. 2015, 9, 9–13. [Google Scholar] [CrossRef]
- Giovarruscio, M.; Tonini, R.; Zavattini, A.; Foschi, F. Reparative procedures for endodontic perforations: Towards a standardised approach. Endod. EPT 2020, 14, 217–228. [Google Scholar]
- American Association of Endodontists. Treatment Standards Whitepaper; American Association of Endodontists: Chicago, IL, USA, 2020; Available online: https://www.aae.org/specialty/wp-content/uploads/sites/2/2018/04/TreatmentStandards_Whitepaper.pdf (accessed on 22 March 2024).
- American Association of Endodontists. The Standard Practice in Contemporary Endodontics. In Endodontics Colleagues for Excellence; American Association of Endodontists: Chicago, IL, USA, 2014; pp. 2–9. [Google Scholar]
- American Association of Endodontists. Treatment Options for the Compromised Tooth: A Decision Guide; American Association of Endodontists: Chicago, IL, USA, 2017; Available online: https://www.aae.org/treatmentoptions (accessed on 22 March 2024).
- Olcay, K.; Ataoglu, H.; Belli, S. Evaluation of Related Factors in the Failure of Endodontically Treated Teeth: A Cross-sectional Study. J. Endod. 2018, 44, 38–45. [Google Scholar] [CrossRef]
- Shemesh, H.; Cristescu, R.C.; Wesselink, P.R.; Wu, M.K. The use of cone-beam computed tomography and digital periapical radiographs to diagnose root perforations. J. Endod. 2011, 37, 513–516. [Google Scholar] [CrossRef]
- Shokri, A.; Eskandarloo, A.; Noruzi-Gangachin, M.; Khajeh, S. Detection of root perforations using conventional and digital intraoral radiography, multidetector computed tomography and cone beam computed tomography. Restor. Dent. Endod. 2015, 40, 58–67. [Google Scholar] [CrossRef]
- Ball, R.L.; Barbizam, J.V.; Cohenca, N. Intraoperative endodontic applications of cone-beam computed tomography. J. Endod. 2013, 39, 548–557. [Google Scholar] [CrossRef] [PubMed]
- Venskutonis, T.; Plotino, G.; Juodzbalys, G.; Mickevičiene, L. The importance of cone-beam computed tomography in the management of endodontic problems: A review of the literature. J. Endod. 2014, 40, 1895–1901. [Google Scholar] [CrossRef] [PubMed]
- Guidice, R.; Nicita, F.; Puleio, F.; Alibrandi, A.; Cervino, G.; Lizio, A.S.; Pantaleo, G. Acuracy of Periapical Radiography and CBCT in Endodontic Evaluation. Int. J. Dent. Vol. 2018, 2018, 2514243. [Google Scholar] [CrossRef]
- Mente, J.; Hage, N.; Pfefferle, T.; Kock, M.J.; Geletneky, B.; Dreyhaupt, J.; Martin, N.; Staehle, H.J. Treatment Outcome of Mineral Trioxide Aggregate: Repair of Root Perforations. J. Endod. 2010, 36, 208–213. [Google Scholar] [CrossRef]
- Evans, M.D. A contemporary treatment of an iatrogenic root perforation; a case report. J. Endod. 2021, 47, 520–525. [Google Scholar] [CrossRef]
- Soares de Toubes, K.; Tonelli, S.Q.; Girelli, C.F.; Azevedo, C.G.; Thompson, A.C.; Nunes, E.; Silveira, F.F. Bio-C Repair-A New Bioceramic Material for Root Perforation Management Two Case Reports. Braz. Dent. J. 2021, 32, 104–110. [Google Scholar] [CrossRef]
- Dong, X.; Xu, X. Bioceramics in Endodontics: Updates and Future Perspectives. MDPI Bioeng. J. 2023, 10, 354. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.; Wealleans, J.; Ray, J. Endodontic applications of 3D printing. Int. Endod. J. 2018, 51, 1005–1018. [Google Scholar] [CrossRef] [PubMed]
- Scelza, P.; Goncalves, F.; Caldas, I.; Nunes, F.; Lourenco, E.S.; Tavares, S.; Magno, M.; Pintor, A.; Mourao, C.F.; Alves, G.; et al. Prognosis of Regenerative Endodontic Procedures in Mature Teeth: A Systematic Review and Meta-Analysis of Clinial and Radiographic Parameters. MDPI Mater. J. 2021, 14, 4418. [Google Scholar] [CrossRef]
- Briuzela, C.; Meza, G.; Khoury, M. Revolutionizing Endodontics: Innovative Approaches for Treating Mature Teeth With Closed Apices and Apical Lesions: A Report of Two Cases. J. Endod. 2024, 50, 596–601. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).