The Effects of an Acute Exposure of Virtual vs. Real Slip and Trip Perturbations on Postural Control
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Equipment
2.3. Postural Control Assessment Battery
2.4. Experimental Procedures
2.5. Data Analysis
2.6. Statistical Analysis
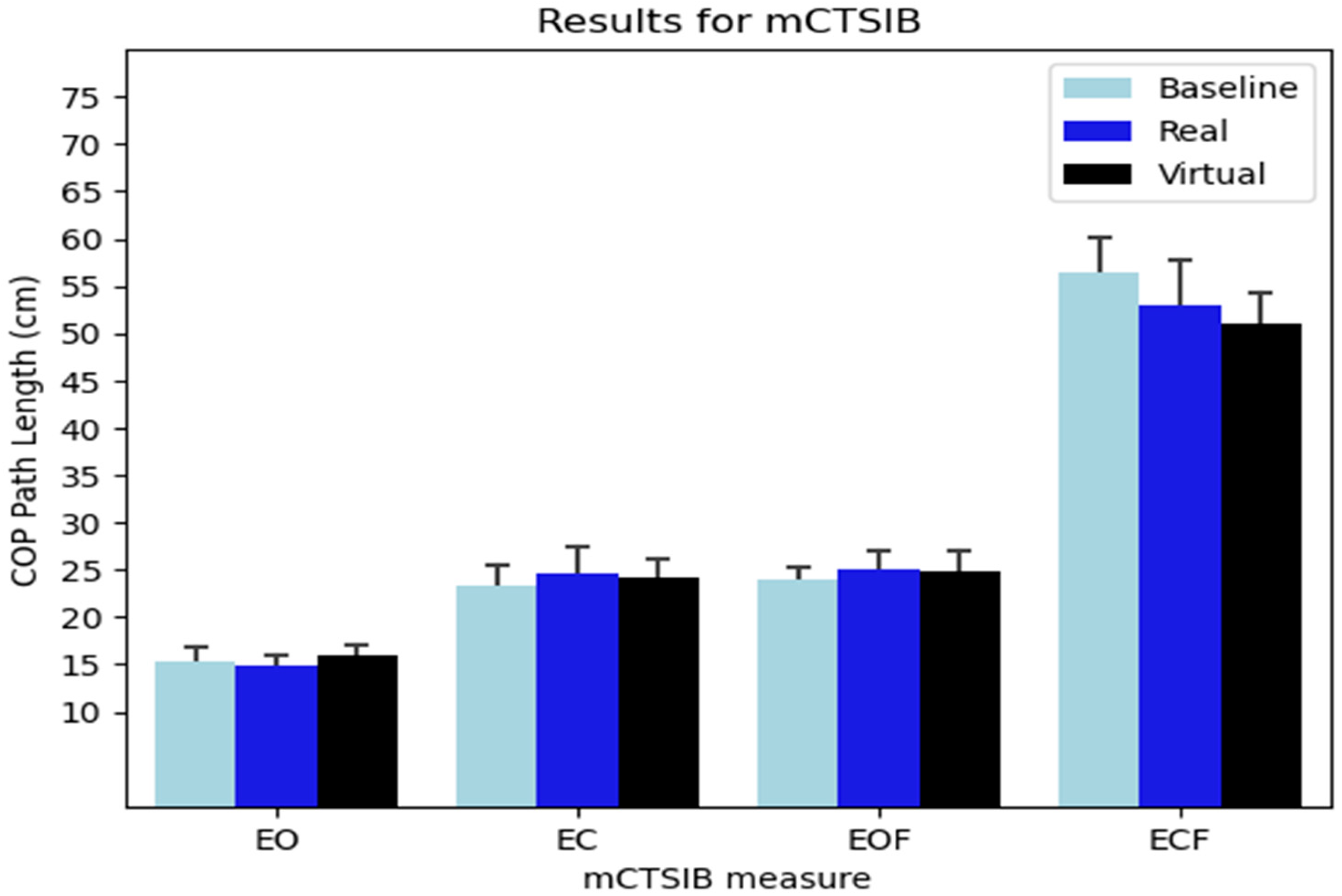
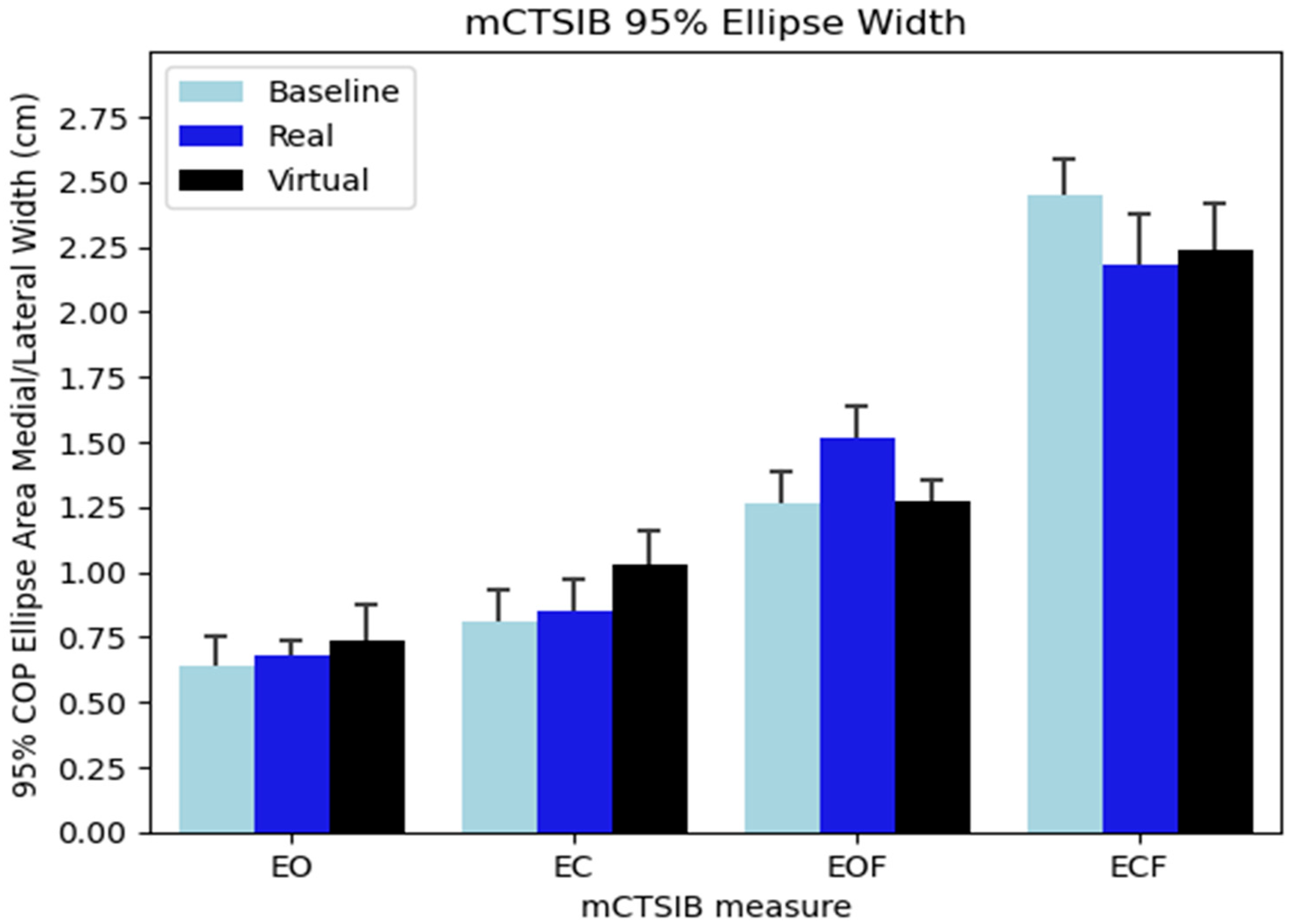
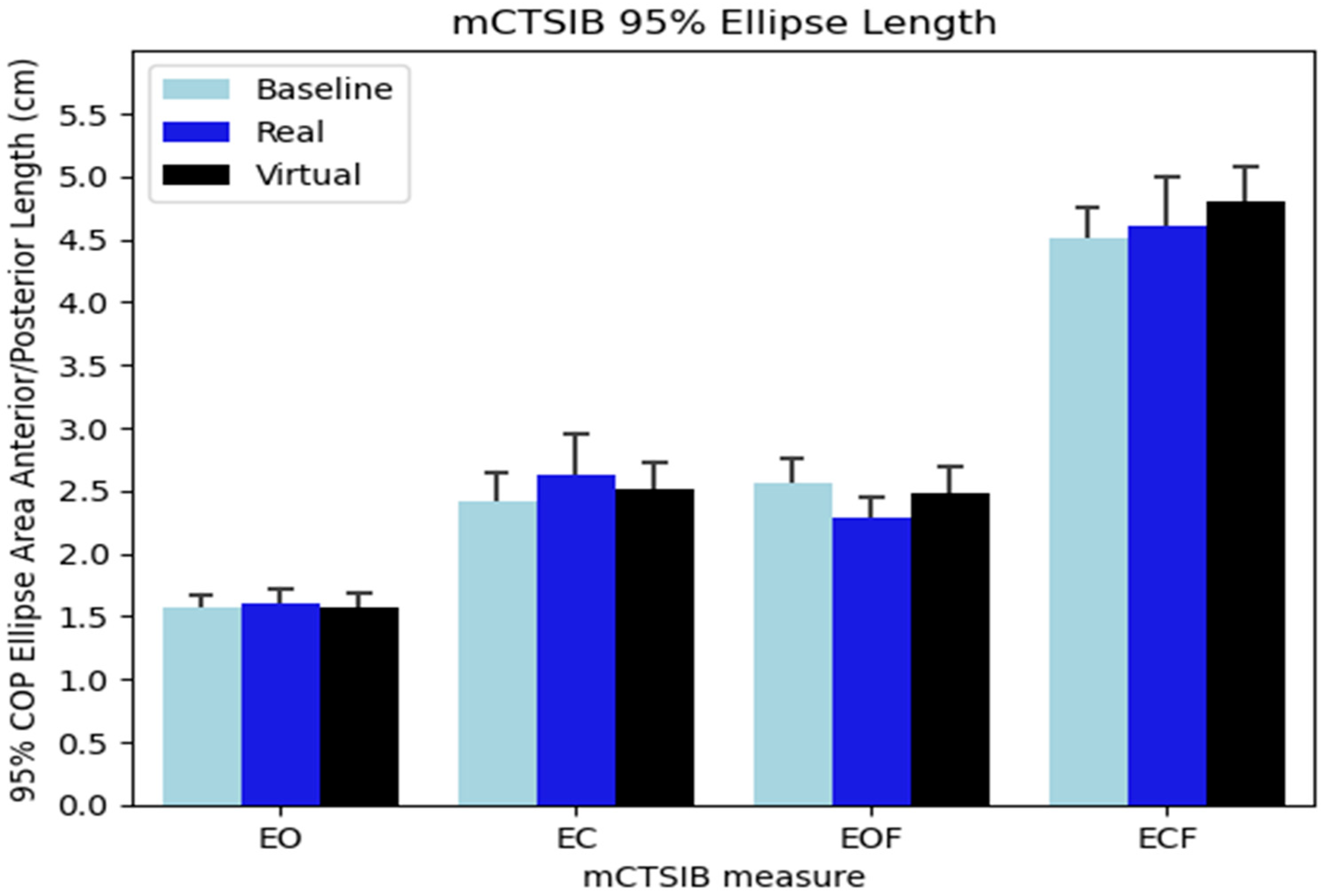
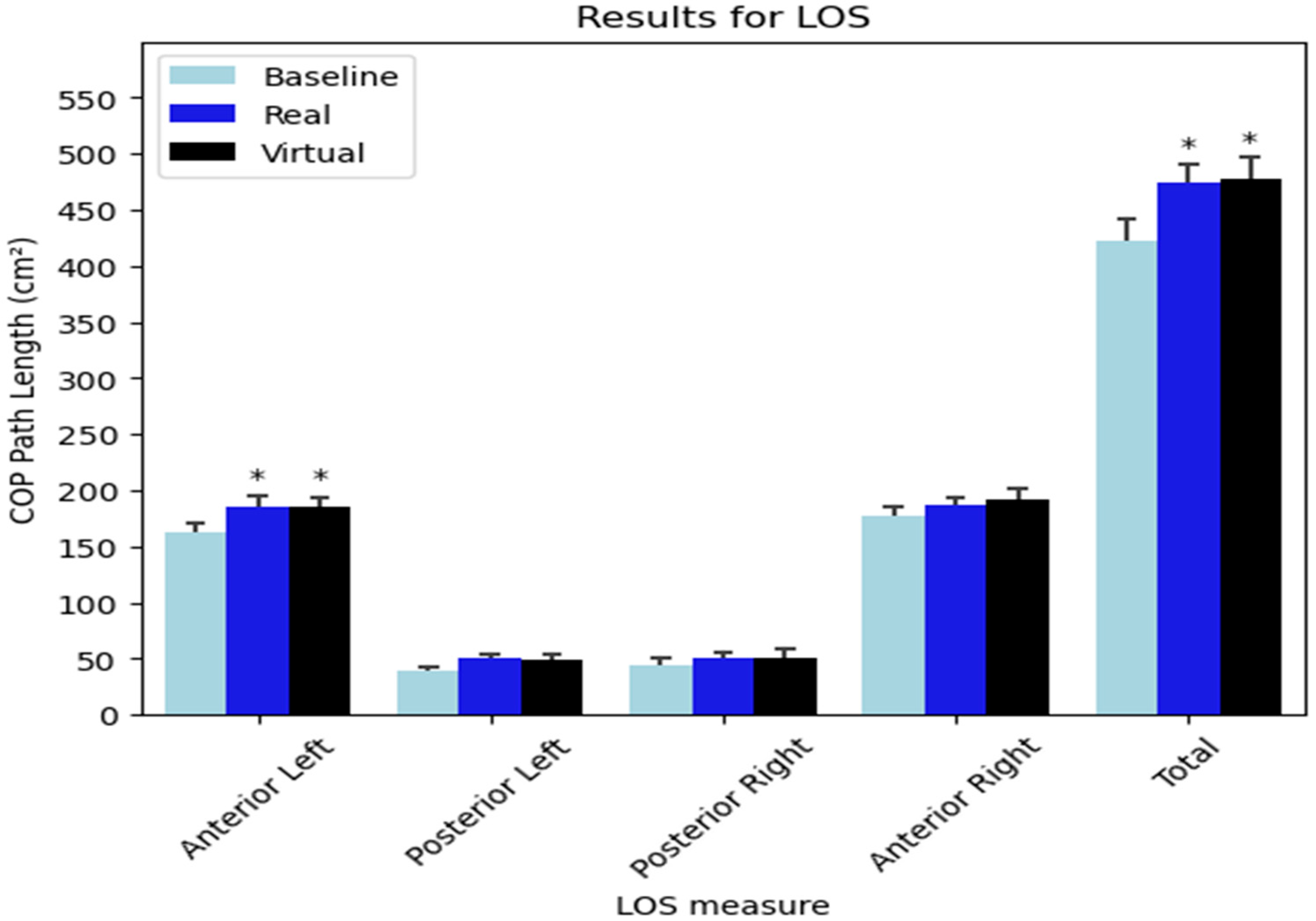
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Talbot, L.A.; Musiol, R.J.; Witham, E.K.; Metter, E.J. Falls in Young, Middle-Aged and Older Community Dwelling Adults: Perceived Cause, Environmental Factors and Injury. BMC Public Health 2005, 5, 86. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-H. Tools for Assessing Fall Risk in the Elderly: A Systematic Review and Meta-Analysis. Aging Clin. Exp. Res. 2018, 30, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.D.; Guo, L.; Kim, J.; Xiong, S. Comparison of Fatal Occupational Injuries in Construction Industry in the United States, South Korea, and China. Int. J. Ind. Ergon. 2019, 71, 64–74. [Google Scholar] [CrossRef]
- Jackson, S.A.; Loomis, D. Fatal Occupational Injuries in the North Carolina Construction Industry, 1978–1994. Appl. Occup. Environ. Hyg. 2002, 17, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Center for Disease Control and Prevention Deaths from Older Adult Falls. Available online: https://www.cdc.gov/falls/data/fall-deaths.html (accessed on 5 September 2022).
- Thomas, E.; Battaglia, G.; Patti, A.; Brusa, J.; Leonardi, V.; Palma, A.; Bellafiore, M. Physical Activity Programs for Balance and Fall Prevention in Elderly. Medicine 2019, 98, e16218. [Google Scholar] [CrossRef] [PubMed]
- Meyns, P.; Pans, L.; Plasmans, K.; Heyrman, L.; Desloovere, K.; Molenaers, G. The Effect of Additional Virtual Reality Training on Balance in Children with Cerebral Palsy after Lower Limb Surgery: A Feasibility Study. Games Health J. 2017, 6, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Park, D.-S.; Lee, D.-G.; Lee, K.; Lee, G. Effects of Virtual Reality Training Using Xbox Kinect on Motor Function in Stroke Survivors: A Preliminary Study. J. Stroke Cerebrovasc. Dis. 2017, 26, 2313–2319. [Google Scholar] [CrossRef] [PubMed]
- Prasertsakul, T.; Kaimuk, P.; Chinjenpradit, W.; Limroongreungrat, W.; Charoensuk, W. The Effect of Virtual Reality-Based Balance Training on Motor Learning and Postural Control in Healthy Adults: A Randomized Preliminary Study. Biomed. Eng. Online 2018, 17, 124. [Google Scholar] [CrossRef] [PubMed]
- Mirelman, A.; Rochester, L.; Maidan, I.; Del Din, S.; Alcock, L.; Nieuwhof, F.; Rikkert, M.O.; Bloem, B.R.; Pelosin, E.; Avanzino, L.; et al. Addition of a Non-Immersive Virtual Reality Component to Treadmill Training to Reduce Fall Risk in Older Adults (V-TIME): A Randomised Controlled Trial. Lancet 2016, 388, 1170–1182. [Google Scholar] [CrossRef] [PubMed]
- Juras, G.; Brachman, A.; Michalska, J.; Kamieniarz, A.; Pawłowski, M.; Hadamus, A.; Białoszewski, D.; Błaszczyk, J.; Słomka, K.J. Standards of Virtual Reality Application in Balance Training Programs in Clinical Practice: A Systematic Review. Games Health J. 2019, 8, 101–111. [Google Scholar] [CrossRef] [PubMed]
- Huygelier, H.; Schraepen, B.; van Ee, R.; Abeele, V.V.; Gillebert, C.R. Acceptance of Immersive Head-Mounted Virtual Reality in Older Adults. Sci. Rep. 2019, 9, 4519. [Google Scholar] [CrossRef] [PubMed]
- Szpak, A.; Michalski, S.C.; Saredakis, D.; Chen, C.S.; Loetscher, T. Beyond Feeling Sick: The Visual and Cognitive Aftereffects of Virtual Reality. IEEE Access 2019, 7, 130883–130892. [Google Scholar] [CrossRef]
- Dużmańska, N.; Strojny, P.; Strojny, A. Can Simulator Sickness Be Avoided? A Review on Temporal Aspects of Simulator Sickness. Front. Psychol. 2018, 9, 2132. [Google Scholar] [CrossRef] [PubMed]
- Lo, W.T.; So, R.H.Y. Cybersickness in the Presence of Scene Rotational Movements along Different Axes. Appl. Ergon. 2001, 32, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Chander, H.; Shojaei, A.; Deb, S.; Arachchige, S.N.K.K.; Hudson, C.; Knight, A.C.; Carruth, D.W. Impact of Virtual Reality–Generated Construction Environments at Different Heights on Postural Stability and Fall Risk. Work Health Saf. 2021, 69, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, A.S.; Feiner, S.K. Combating VR Sickness through Subtle Dynamic Field-of-View Modification. In Proceedings of the 2016 IEEE Symposium on 3D User Interfaces (3DUI), Greenville, SC, USA, 19–20 March 2016; pp. 201–210. [Google Scholar]
- Akizuki, H.; Uno, A.; Arai, K.; Morioka, S.; Ohyama, S.; Nishiike, S.; Tamura, K.; Takeda, N. Effects of Immersion in Virtual Reality on Postural Control. Neurosci. Lett. 2005, 379, 23–26. [Google Scholar] [CrossRef] [PubMed]
- Conner, N.O.; Freeman, H.R.; Jones, J.A.; Luczak, T.; Carruth, D.; Knight, A.C.; Chander, H. Virtual Reality Induced Symptoms and Effects: Concerns, Causes, Assessment & Mitigation. Virtual Worlds 2022, 1, 130–146. [Google Scholar] [CrossRef]
- Elias, Z.M.; Batumalai, U.M.; Azmi, A.N.H. Virtual Reality Games on Accommodation and Convergence. Appl. Ergon. 2019, 81, 102879. [Google Scholar] [CrossRef] [PubMed]
- Kourtesis, P.; Collina, S.; Doumas, L.A.A.; MacPherson, S.E. Technological Competence Is a Pre-Condition for Effective Implementation of Virtual Reality Head Mounted Displays in Human Neuroscience: A Technological Review and Meta-Analysis. Front. Hum. Neurosci. 2019, 13, 342. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, N.; Takagi, H. Virtual Reality Environment Design of Managing Both Presence and Virtual Reality Sickness. J. Physiol. Anthropol. Appl. Hum. Sci. 2004, 23, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Cho, G.H.; Hwangbo, G.; Shin, H.S. The Effects of Virtual Reality-Based Balance Training on Balance of the Elderly. J. Phys. Ther. Sci. 2014, 26, 615–617. [Google Scholar] [CrossRef] [PubMed]
- Goble, D.J.; Cone, B.L.; Fling, B.W. Using the Wii Fit as a Tool for Balance Assessment and Neurorehabilitation: The First Half Decade of “Wii-Search”. J. Neuroeng. Rehabil. 2014, 11, 12. [Google Scholar] [CrossRef] [PubMed]
- Phu, S.; Vogrin, S.; Al Saedi, A.; Duque, G. Balance Training Using Virtual Reality Improves Balance and Physical Performance in Older Adults at High Risk of Falls. Clin. Interv. Aging 2019, 14, 1567–1577. [Google Scholar] [CrossRef] [PubMed]
- Sinitski, E.H.; Thompson, A.A.; Godsell, P.; Honey, J.; Besemann, M. Postural Stability and Simulator Sickness after Walking on a Treadmill in a Virtual Environment with a Curved Display. Displays 2018, 52, 1–7. [Google Scholar] [CrossRef]
- Jung, J.; Yu, J.; Kang, H. Effects of Virtual Reality Treadmill Training on Balance and Balance Self-Efficacy in Stroke Patients with a History of Falling. J. Phys. Ther. Sci. 2012, 24, 1133–1136. [Google Scholar] [CrossRef]
- Parijat, P.; Lockhart, T.E. Effects of Moveable Platform Training in Preventing Slip-Induced Falls in Older Adults. Ann. Biomed. Eng. 2012, 40, 1111–1121. [Google Scholar] [CrossRef] [PubMed]
- Benedict, S.E.; Hinshaw, J.W.; Byron-Fields, R.; Baweja, H.S.; Goble, D.J. Effects of Fatigue on the BTrackS Balance Test for Concussion Management. Int. J. Athl. Ther. Train. 2017, 22, 23–28. [Google Scholar] [CrossRef]
- Nolff, M.R.; Conner, N.O.; Haworth, J.L.; Goble, D.J. Lower Limb Asymmetry Evaluation Using the Balance Tracking System (BTrackS) Single Leg Stance Protocol. J. Mot. Behav. 2022, 55, 493–498. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, S.M.; Baweja, H.S.; Goble, D.J. Validating the BTrackS Balance Plate as a Low Cost Alternative for the Measurement of Sway-Induced Center of Pressure. J. Biomech. 2016, 49, 4142–4145. [Google Scholar] [CrossRef] [PubMed]
- Goble, D.J.; Brar, H.; Brown, E.C.; Marks, C.R.; Baweja, H.S. Normative Data for the Balance Tracking System Modified Clinical Test of Sensory Integration and Balance Protocol. Med. Devices Évid. Res. 2019, 12, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Haworth, J.; Goble, D.; Pile, M.; Kendall, B. BTrackS Limits of Stability Test Is a Reliable Assessment of Volitional Dynamic Postural Control. Gait Posture 2020, 80, 298–301. [Google Scholar] [CrossRef] [PubMed]
- Szczerbik, E.; Kalinowska, M.; Święcicka, A.; Graff, K.; Syczewska, M. The Impact of Two Weeks of Traditional Therapy Supplemented with Virtual Reality on Balance Control in Neurologically-Impaired Children and Adolescents. J. Bodyw. Mov. Ther. 2021, 28, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Ghafar, M.A.A.; Abdelraouf, O.R.; Harraz, E.M.; Seyam, M.K.; Morsy, W.E.; Amin, W.M.; Abd-Elfattah, H.M. Virtual Reality Rehabilitation Helps to Improve Postural Balance in Children with Autism Spectrum Disorder: A Randomized Control Trial. Phys. Occup. Ther. Pediatr. 2025, 45, 423–436. [Google Scholar] [CrossRef] [PubMed]
- Esculier, J.-F.; Vaudrin, J.; Bériault, P.; Gagnon, K.; Tremblay, L.E. Home-Based Balance Training Programme Using Wii Fit with Balance Board for Parkinsons’s Disease: A Pilot Study. J. Rehabil. Med. 2012, 44, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Vogt, S.; Skjæret-Maroni, N.; Neuhaus, D.; Baumeister, J. Virtual Reality Interventions for Balance Prevention and Rehabilitation after Musculoskeletal Lower Limb Impairments in Young up to Middle-Aged Adults: A Comprehensive Review on Used Technology, Balance Outcome Measures and Observed Effects. Int. J. Med. Inform. 2019, 126, 46–58. [Google Scholar] [CrossRef] [PubMed]
- Barbanchon, C.; Mouraux, D.; Baudry, S. Repeated Exposure to Virtual Reality Decreases Reliance on Visual Inputs for Balance Control in Healthy Adults. Hum. Mov. Sci. 2024, 96, 103236. [Google Scholar] [CrossRef] [PubMed]
- Pineda, R.C.; Krampe, R.T.; Vanlandewijck, Y.; Biesen, D.V. Reliability of Center of Pressure Excursion as a Measure of Postural Control in Bipedal Stance of Individuals with Intellectual Disability: A Pilot Study. PLoS ONE 2020, 15, e0240702. [Google Scholar] [CrossRef] [PubMed]
- Reutimann, S.; Hill-Strathy, M.; Krewer, C.; Bergmann, J.; Müller, F.; Jahn, K.; Rauen, K. Influence of Footwear on Postural Sway: A Systematic Review and Meta-Analysis on Barefoot and Shod Bipedal Static Posturography in Patients and Healthy Subjects. Gait Posture 2022, 92, 302–314. [Google Scholar] [CrossRef] [PubMed]
- Ruhe, A.; Fejer, R.; Walker, B. The Test–Retest Reliability of Centre of Pressure Measures in Bipedal Static Task Conditions—A Systematic Review of the Literature. Gait Posture 2010, 32, 436–445. [Google Scholar] [CrossRef] [PubMed]
- Quijoux, F.; Vienne-Jumeau, A.; Bertin-Hugault, F.; Zawieja, P.; Lefèvre, M.; Vidal, P.-P.; Ricard, D. Center of Pressure Displacement Characteristics Differentiate Fall Risk in Older People: A Systematic Review with Meta-Analysis. Ageing Res. Rev. 2020, 62, 101117. [Google Scholar] [CrossRef] [PubMed]
- Mehdizadeh, S.; Van Ooteghem, K.; Gulka, H.; Nabavi, H.; Faieghi, M.; Taati, B.; Iaboni, A. A Systematic Review of Center of Pressure Measures to Quantify Gait Changes in Older Adults. Exp. Gerontol. 2021, 143, 111170. [Google Scholar] [CrossRef] [PubMed]



| Variable | Mean | STD |
|---|---|---|
| Age (years) | 23.46 | 3.31 |
| Height (cm) | 173.85 | 8.46 |
| Weight (N) | 806 | 111.89 |
| Shoe Size (U.S. men’s) | 9.03 | 2.71 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Conner, N.O.; Chander, H.; Derby, H.; Pannell, W.C.; Daniels, J.B.; Knight, A.C. The Effects of an Acute Exposure of Virtual vs. Real Slip and Trip Perturbations on Postural Control. Virtual Worlds 2025, 4, 34. https://doi.org/10.3390/virtualworlds4030034
Conner NO, Chander H, Derby H, Pannell WC, Daniels JB, Knight AC. The Effects of an Acute Exposure of Virtual vs. Real Slip and Trip Perturbations on Postural Control. Virtual Worlds. 2025; 4(3):34. https://doi.org/10.3390/virtualworlds4030034
Chicago/Turabian StyleConner, Nathan O., Harish Chander, Hunter Derby, William C. Pannell, Jacob B. Daniels, and Adam C. Knight. 2025. "The Effects of an Acute Exposure of Virtual vs. Real Slip and Trip Perturbations on Postural Control" Virtual Worlds 4, no. 3: 34. https://doi.org/10.3390/virtualworlds4030034
APA StyleConner, N. O., Chander, H., Derby, H., Pannell, W. C., Daniels, J. B., & Knight, A. C. (2025). The Effects of an Acute Exposure of Virtual vs. Real Slip and Trip Perturbations on Postural Control. Virtual Worlds, 4(3), 34. https://doi.org/10.3390/virtualworlds4030034






