1. Introduction
Since the beginning of the current millennium, a variety of natural disasters have impacted the United States and many nations around the world [
1]. These disasters have highlighted the important roles veterinarians play following disasters as well as the importance of training veterinarians to assist with disaster planning and response in the support of public health [
1,
2]. In the case of the United States, despite the known and increasing threat of natural and human-made disasters, there are only two accredited veterinary schools in North America (North Carolina State University and Texas A&M University) where disaster planning, preparedness and response training are a requirement of the professional curriculum [
3,
4,
5].
As of 2007, veterinary students at the North Carolina State University College of Veterinary Medicine completed six hours of online training, six hours of classroom training, and two three-hour scenarios centered on the veterinarian’s role in disaster response. At the conclusion of this training, participants receive entry-level emergency response credentials which allow these students to support disaster response activities after graduation [
3].
A similar program was created at Texas A&M University College of Veterinary Medicine and Biomedical Sciences in 2012. There, senior veterinary students participate in a two-week clinical rotation (VMID 927—Veterinary Emergency Management) as part of their senior clinical curriculum. The rotation exposes students to community-level veterinary disaster planning and response as well as to the veterinarian’s role in disaster response. In the first week of the rotation, students receive experiential training in disaster preparedness through working with local jurisdictions (counties or communities) and entities including but not limited to animal shelters, zoos, and other animal-focused organizations in the development of emergency response plans.
During the second week, students shift their focus from disaster preparedness to response and the role of the veterinarian in a disaster. To achieve a better understanding of the veterinarian’s role in disaster response, students utilize a computer-based multi-user virtual learning environment (MUVE), Second Life
® (Linden Laboratories, San Francisco, CA, USA), to gain experience in disaster response as a veterinarian through an immersive, experiential learning opportunity [
6]. A more detailed review of the rotation’s Second Life
® experience will be provided later in this report. Lastly, after completing the rotation, students are eligible to receive the American Veterinary Medical Association’s (AVMA) Veterinary First Responder certificate [
1,
4]. A comparison of the two programs, their structures, and areas of focus is detailed in
Table 1. The reader will find an outline of a typical rotation at the end of this publication (
Appendix A).
The use of virtual reality (VR) and augmented reality (AR) in veterinary medical education has been proposed to support student learning, improve student wellbeing, and to ensure patient safety and animal welfare [
7,
8]. One such technology is Second Life
®, which can be classified as both a non-immerse VR and a three-dimensional multi-user virtual environment [
2,
9,
10]. Second Life
® was launched by Linden Labs in 2003 and is one of the most well-known and utilized virtual worlds today, particularly in health care education [
4,
9,
11,
12]. There are several successful examples of the use of Second Life
® to provide human health care professionals and emergency services personnel with emergency and disaster response training in a variety of settings and facing a variety of scenarios [
2,
13,
14,
15].
To the author’s knowledge, the Veterinary Emergency Management rotation at Texas A&M University is the only use of Second Life® in veterinary education aimed at preparing students for disaster response. The purpose of this communication is to outline how an MUVE is used to support veterinary disaster preparedness and response at Texas A&M University and demonstrate to others how effective and beneficial this tool can be in this type of training. Furthermore, we hope that this article not only spurs conversations amongst our colleagues on the importance of including disaster preparedness and response training in their veterinary curricula but that it also sparks their curiosity and stimulates their creativity as to using unconventional methods and modalities in their teaching.
2. The Simulation
When participating in the simulation portion of the rotation, students utilize a university-provided desktop computer with a standard mouse and keyboard. The computer is connected to the internet via a wireless internet connection. Students also are provided with a headset with a microphone. Students then communicate with faculty, actors, and other students via voice; however, they may use Second Life’s® text chat to directly message other participants. Students are placed in individual rooms with their computers and are isolated from one another, so all communication occurs within Second Life®.
Prior to beginning the scenario, students are provided with one hour of training on how to move, communicate, and interact with patients, avatars, and the virtual environment. Students create an individual account and are instructed to create a username devoid of any personally identifying information to include registered trademarks or registered brands as safeguards to protect their personal identity. Students are provided with two hours of training on a broad list of technical skill objectives that includes how to move their avatar within the virtual environment and how to perform avatar-specific functions such as visual focus and simulated manual manipulation of mechanical devices including cage doors or other common equipment encountered in the virtual environment. They are also instructed how to perform inter-avatar-specific tasks such as how to communicate with other avatar characters and peer veterinary student avatar team members, how to interact with patients, how to transcribe record entries of verbal orders and record dispensing of medications and dosages, how to document patient treatment instructions, and how to record second veterinarian confirmation of euthanasia decisions.
2.1. The Simulated Disaster Environment
The Second Life® environment used during the rotation is an exclusive island within Second Life® which is accessible only with permission from the course faculty. The environment was custom-made and developed for the course. It is modeled after actual disasters: Hurricane Ike (2008) and the Moore, OK, tornado (2013). These were chosen because there was ample animal case data (medical records and imagery) available from which to develop realistic simulated patients. This information was provided to contracted programmers who had experience working with Second Life®. The programmers were teamed with the faculty course instructors who together developed the virtual world using images of the areas affected by the disasters. The faculty obtained case histories and wound descriptions from private veterinary practitioners who responded to the Moore, OK, tornado including photographs of both small animals and large animals (horses, cattle, and goats). The case descriptions were based on actual traumatic injuries sustained by animals during or after the disasters or on conditions that would be expected following such events.
After compiling the imagery and case descriptions and obtaining faculty input, the programmers then constructed the visual simulation and designed the computer script code needed to articulate animal movement or action simulations needed to generate interactive realism between avatars or between avatars and animals, and to a small degree within an animal physiologically to show signs of stress or shock. Lastly, the programmers were also tasked to create character avatars for both the instructors as well as actors who would interact with the students during the simulation such as police officers, news reporters and camera operators, and pet owners [
4].
The environment is centered around a Base of Operations (BoO) that consists of two large tents and a large command vehicle. The two tents serve as the triage area and treatment facility for the small animal cases (
Figure 1). Various emergency and public works vehicles are also located both in the immediate vicinity of the BoO and elsewhere. Students do not have the ability to operate any of the vehicles located in the environment.
Beyond the core BoO, there are several large pastures that contain the large animal patients. Additionally, there are several hazards that the students may encounter such as down power lines. These hazards can cause injury to the avatars which results in them being suspended from play for approximately 30 s (
Figure 2). This is applied to highlight the importance of maintaining a high level of situational awareness when operating in a disaster area.
2.2. The Student’s Heads-Up Display
When a student is navigating the disaster scene in Second Life
®, they obtain information about the patients they encounter via a heads-up display (HUD). Consistent with many traditional videogames, Second Life
® features an HUD that provides the students with situational data and relevant details about the patients they encounter through imagery and text [
4,
16]. The HUD (
Figure 3) provides students with three main features: (1) the patient file, (2) the medical cache, and (3) the action bar, which allows individual and group chats, voice communication, the ability to change their visual perspective, and access to a map of the island.
Located on the left side of the HUD is the patient file (left side of
Figure 3). The patient file provides the students with information including signalment, vital parameters, history (if available), and a brief description of an illness or injury. The patient file also displays an image, either of the patient’s injury or some readily observable clinical signs or behaviors commonly associated with illness in veterinary species. The patient file is also the place where students document their assessment (medical record), any medications they administer, diagnostic tests they perform, or treatments they provide.
Opposite the patient file on the right side of the HUD is the medical cache. Here, students can view the treatment resources available to them including medications and supplies. The contents of the cache were developed by faculty veterinarians to reflect what a student may have available to them during an actual disaster. Students can withdraw volumes of medication or numbers of items from the cache that will be used during the treatment of a simulated patient. These are then automatically subtracted from the totals available; however, the students may request additional supplies if needed. The fulfillment of those requests is performed at the discretion of the faculty members.
To further simulate realism in the disaster response, the students are required to communicate via text messages to the Operations Officer to request resupply of drugs or other supplies contained in the cache. The students are also required to prepare Situation Reports (SITREPS) and transmit those to the Operations Officer in addition to receiving messages and reports from Operations giving new instructions or directing actions in response to evolving situations having an impact on the assigned mission.
2.3. Avatars
Prior to beginning the rotation, students create their unique avatar. The students are instructed to create a username which they will use during the simulation. The name they choose must be free of any identifying information that could allow others to discern the student’s identity after the simulation ends or after the end of the rotation. Although students can perform some customization of their avatar, the avatar is fitted with standard clothing (navy blue pants, a maroon Texas A&M VET shirt, hat, and mask) consistent with what actual VET veterinarians and members would wear during a real deployment. Students are also given introductory training on how to move their avatar in the environment, how to operate their HUD, and how to access case information and the available medical cache.
In addition to the faculty’s unique avatars, several other avatars were created and used during the simulation. These avatars are played by undergraduate students, hospital staff, and outside volunteers. The avatars interact with the veterinary students during the simulation and create addition challenges and add to the realism of the scenario. A script containing opening dialogue and the premise of their designated situational encounter was created for each avatar. This creates uniformity between students’ experiences, reduces the need for student and staff actors to create unique dialogue for each situation, and allows faculty members to more consistently evaluate student interactions.
Once the opening dialogue is initiated, the scripted avatar actor may then begin to improvise their interaction in response to the veterinary student’s conduct and verbal communication. All interactions become situationally based communications where a reply to a question will most likely generate a follow-up question seeking deeper understanding of what the veterinary student may have verbalized. The use of these character avatars adds an additional layer of realism and offers the faculty the ability to manipulate the situation based on student input. Furthermore, the avatars are based on individuals that a veterinarian operating in a disaster area may encounter. Below are some examples of the avatars the students may encounter during the simulation.
2.3.1. Journalists
The first avatars the students typically encounter are a journalist and camera operator. The pair are from a local television news organization and are navigating the area to report on the disaster. The journalist asks the students questions on their role in the area, the services they can provide, as well as the types of patients to which the students are able to provide care. This offers the students an opportunity to demonstrate their knowledge of disaster management and both the veterinarian’s individual roles and responsibilities in a disaster. It is also an opportunity for students to demonstrate their knowledge of the roles and functions of volunteer organizations, such as the VET, in veterinary disaster response.
2.3.2. Police Officer
Students next encounter a police officer. The officer approaches the students and states that they have been tasked with identifying and triaging livestock affected by the disaster. The officer asks questions about characteristics of a healthy animal, clinical signs associated with injury or disease, and the basics of animal handling, capture, movement, and restraint. This encounter offers students an opportunity to demonstrate their ability to communicate how to safely approach and move a large animal, as well as the nuances and complexities of basic animal behavior and welfare and veterinary triage.
2.3.3. Animal Owner
Some of the students also encounter the owner of a dog named Jojo. The dog is dropped off with one student with a mild epistaxis (nosebleed). Later, the owner interacts with a different student which occurs after Jojo has been treated and discharged to a nearby animal shelter. This transfer occurs without the owner being notified. Often, students overlook the importance of speaking with Jojo’s owner because the other cases they see arrive without an owner present. The owner informs the students that they face considerable financial hardships and are worried about the costs of Jojo’s care. The owner also exhibits considerable emotional distress because not only was Jojo transferred without their knowledge (the typical occurrence) but also because of Jojo’s condition and prognosis as well as the costs of possible referral-level care. This character is designed to sow confusion and to test the internal communication abilities of the students as well as their ability to stay calm under pressure.
2.4. Simulated Patients
Within the disaster environment, students can interact with 125 cases (57 companion animal species which are primarily dogs and cats, 26 horses, 28 cattle, 6 birds, and 8 small ruminants and camelids). Additionally, instructors have a detailed list of all patients to facilitate student learning and to ensure that there is uniformity in student experience. The key includes information available to the students including an image, case number, and a case description. The instructors are also able to see information regarding physical examinations and the results of commonly performed diagnostics testing. The key also contains information on the typical student approach to the case, the patient’s response to therapy, and the expected disposition of the case (shelter in place, refer to hospital, or euthanize).
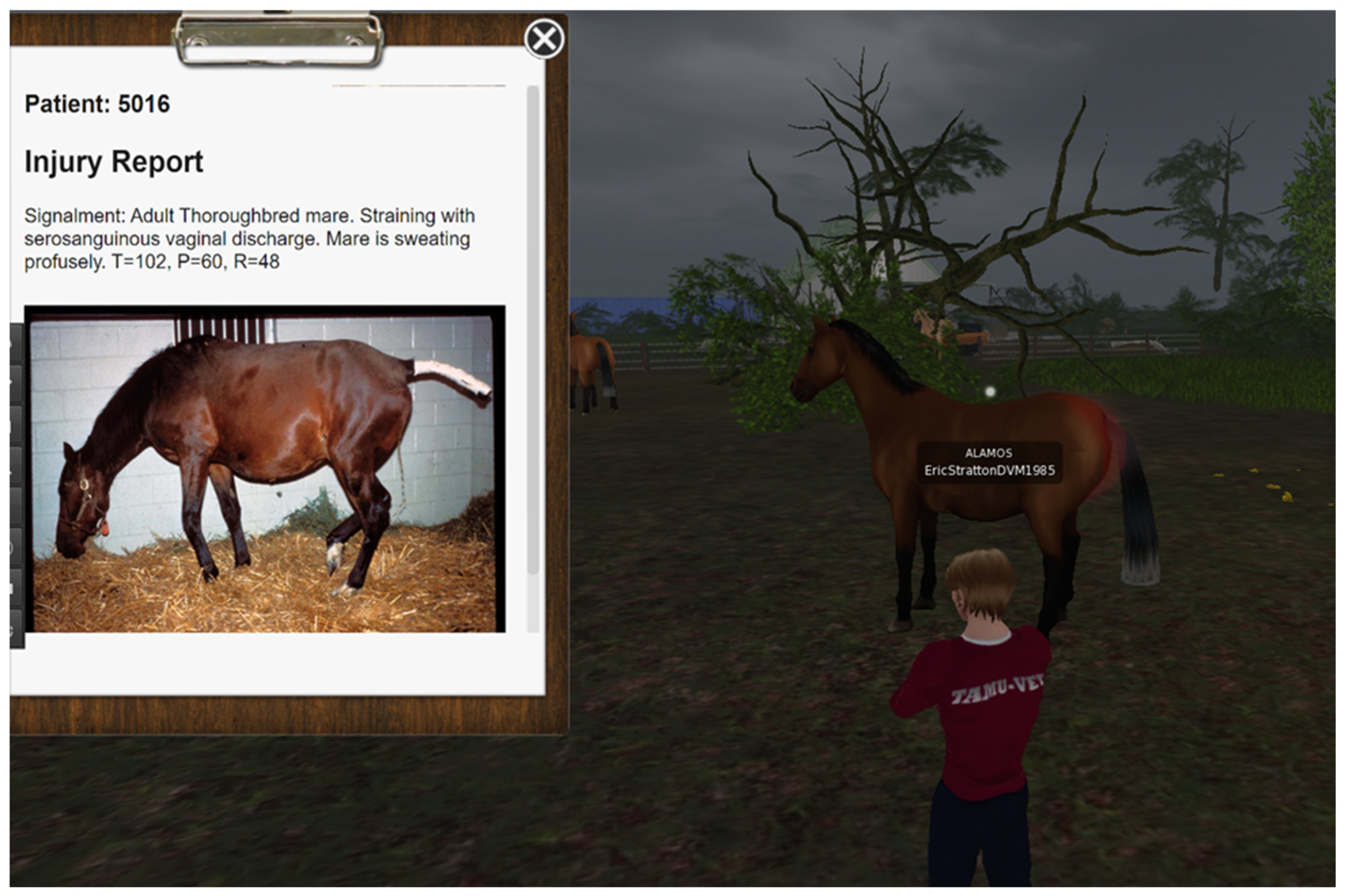
2.4.1. Equine Patient
Patient 5026 is an adult mare (female horse) that students encounter when participating in the large animal portion of the simulation. The patient is standing when the students find her in the field. The patient’s chart (
Figure 4) displays an image the students should quickly interpret to be of a mare in labor. Depending on validity, feasibility, and suitability of the students’ diagnostic and therapeutic plans, the faculty member may cause the mare to deliver (rez) a live or dead foal (neonatal horse). The delivery of a deceased foal indicates to the students that their diagnostic or therapeutic plans were either not suitable for the patient, were not feasible given the situation, or were not performed in a timely manner.
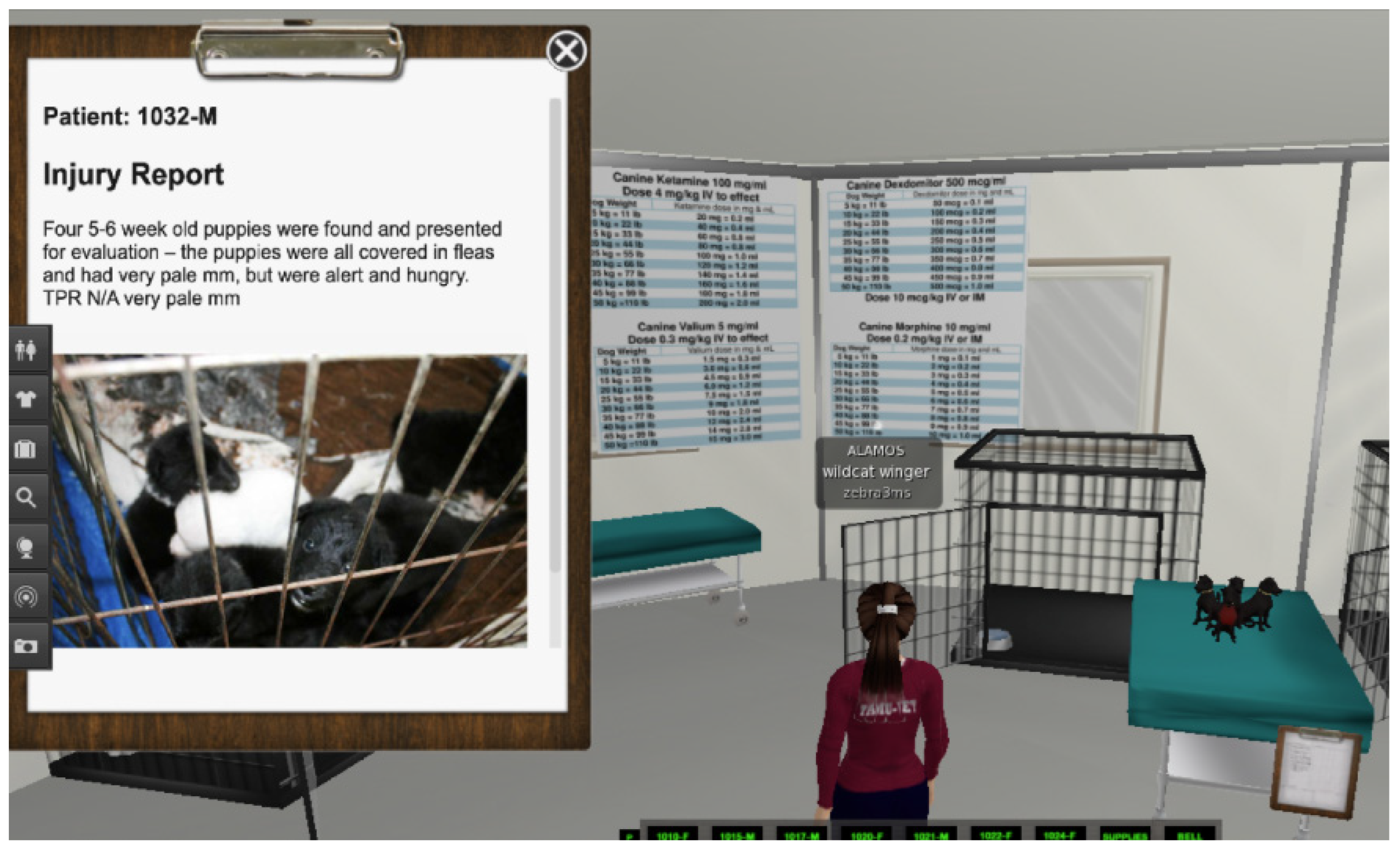
2.4.2. Canine Patient
Patient 1032-M is a litter of four 5–6-week-old puppies that is presented to the students when they are operating from the BoO, specifically the triage tent. When the students are presented with the patients, the puppies are alert and hungry but infested with fleas. The patients’ chart (
Figure 5) displays an image of several puppies in a dirty cage. As was the case with Patient 5026, the outcome of the puppies depends on validity, feasibility, and suitability of the students’ diagnostic and therapeutic plans. The timeliness of the students’ actions is also of paramount concern in this case. The faculty member can provide feedback to the puppies, including seizure activity. The students should recognize that the clinical signs being demonstrated by the puppy is likely due to hypoglycemia (low blood sugar) and providing a source of energy could result in resolution of the seizure signs. When presented with a neonate, the students must access a different bank of knowledge as these patients are very different from their adult counterparts. Timely intervention in these cases can be critical to their survival.
2.5. Student Participation and Assessment
The prototype of this virtual simulation exercise was introduced in the first year of the clinical rotation (2012). That year, the senior class size at Texas A&M numbered 129 students who were fractioned into 24 two-week clinical rotations. The number of students assigned for each clinical rotation ranged between six and seven. Over the years, Texas A&M expanded its resident student class size and also began accepting contract program students from Ross University and St. George’s University in the Caribbean. These students come to Texas A&M to complete their fourth-year clinical studies. The senior class size during the 2024–25 academic year at Texas A&M now numbers 162 plus an additional 39 students coming from Ross University and St. George’s University (Professional Programs Office, CVM-BS, Texas A&M). The swelling of the senior class has increased the number of students of the rotation to 11-to-12. Since its inception, more than 1800 students have enrolled in the rotation and participated in the simulation [
4].
The virtual simulation environment has proven to be an effective and reliable assessment tool enabling real-time evaluation of student learning outcome objectives in two domains, those being (1) critical thinking and problem solving leading to medical decisions that extend across the full range of outcomes, including decisions ending in euthanasia, and (2) human interactions and communications as integral components of the client–practitioner relationship that become disrupted or interfered with by disaster conditions.
The customized design functions include but are not limited to video recording capability and script/text documentation of medical care provided to each patient treated in the virtual environment. With each interaction between a student and an animal, a medical record must be generated. The record is automatically saved and available for review and critique following the completion of the simulation. Saved information normally contains a range of variables including the assignment of a triage level (green, yellow, red or black), a diagnosis, disposition, medications dispensed, and treatments administered.
A post-simulation review is conducted in a clinical-round style which allows the faculty and students to revisit the disaster scene. This is also an opportunity to reexamine the situation and signalment of the animals that were treated. Students then discuss the case with the faculty clinician centered on the medical decisions that determined the disposition of the case. Experienced faculty offer their clinical advice and provide real-world experience with similar situations through clinical narratives. The intent of the review is to allow students to discuss their findings and diagnostic and therapeutic approaches. This encourages individual reflection and promotes skill development.
Evaluation and assessment of the students’ interaction and communication with each other and with the actors is also included as part of the review. Student communication and expression of empathy, compassion, and sympathy with the animal owners and other character actors who play victims or officials of the local jurisdiction in the disaster serve as key indicators of the veterinary student’s professional competency proficiency. The human interaction and communication evaluation and assessment is conducted in real time, listening to verbal communication between character actor avatars engaged in conversation with veterinary student avatars who are deployed to provide for the medical treatment of animals. The veterinary students in the simulation are assessed using a rubric (
Appendix A) that was created to aid faculty in maintaining inter-rater reliability as evaluators and to assist with establishing performance factors that measure the student’s professional competency strength [
4]. Professional competency performance indicators include participation (the student’s individual effort); critical thinking/problem solving; team work (interaction and cooperation); communication (written and verbal); and leadership [
4]. The reader can review an example of the rubric, which has been included at the end of this publication (
Appendix B).
3. Limitations and Challenges
The limitations associated with using Second Life
® to conduct veterinary disaster preparedness training can be placed into two main categories: those challenges that are specific to the program itself and those that are imposed by external forces or circumstances. Both the program-specific limitations and external circumstances can detrimentally impact student learning and the overall student experience. Using Second Life
® to conduct veterinary disaster response training can be accompanied by several of the same limitations that are seen when the program is used to conduct disaster response training with human medical providers and first responders [
14]. Despite these shared limitations, the authors have identified others that are unique to the current application of Second Life
®.
First, the information available in a patient’s charts is static and does not change following medical intervention or medication administration. It should be noted that this is not a specific limitation of Second Life
®. Instead, this is a result of the limited funding dedicated to the program. In fact, there are documented examples of dynamic vital signs and additional diagnostic imaging and laboratory reports available in Second Life
® and other similar MUVE scenarios specifically designed to train human medical providers [
12,
17,
18]. There is ample room for improvement in Second Life
® and, with additional funding, these changes could be made to offer more real-time feedback. It is also prudent to note that the goal of the rotation is not to assess the clinical abilities of these students, but instead it is an opportunity to engage in problem-solving exercises centered on the disaster environment. Regardless, the authors still believe that adding dynamic patient characteristics would support student learning.
Another significant limitation of Second Life in this application is its inability to relay sensory information via touch or smell. In certain instances, tactile sensory information can be provided to a user via haptic feedback. The value of haptic feedback in medical education, specifically on training surgical skills, has been evaluated by several studies, with mixed results [
19,
20,
21,
22,
23,
24]. The addition of haptic feedback to a simulator also requires additional equipment and comes with an added cost [
20,
25].
The authors believe that although the inability of Second Life® to provide haptic feedback is a limitation, its absence does not impact student learning. Furthermore, without an entirely immersive experience, haptic feedback alone serves little purpose in this scenario. The limitation has been overcome by the construction of case-specific supplemental information contained outside of the simulation that can be provided to the students upon their request. The supplemental information provides the student with physical results that would have been obtained if the patient animal could have been palpated or if odors could have been detected by smell.
Students are informed of these technological limitations when they receive their orientation and initial training for the simulation. The students are informed that they may request additional information about a patient outside what is present in the medical chart. During the initial training, students are also provided with example cases that demonstrate some of the limitations of Second Life® pertaining to diagnostics and treatment. For example, when presented with a patient they suspect may be pregnant, they are unable to perform palpation to determine pregnancy. Instead, they must first inform the instructor in real time that they want to perform a palpation and must describe their technique as well as any supplies that are needed. The quality and detail of information the students provide to the faculty member will determine the feedback they receive.
Another reported issue associated with the use of MUVEs in medical education is that users may experience cognitive overload [
6,
13,
26]. During the simulation, students are expected to communicate with faculty, peers, and actors via both voice and chat. They are also expected to make medical decisions for their patients and must maintain situational awareness to ensure the safety of their avatars and that of the colleagues. The sum of these activities could cause some students to experience cognitive overload.
Cognitive load, however, is commonly reported in emergency departments and disaster scenes [
27,
28,
29]. Although not measured directly, the authors can anecdotally attest to the effect of increased cognitive load on student performance as demonstrated by errors in medical math, lapses in both voice and text communication, and in their failure to recognize critical elements of their patient’s health status. There is also evidence that training under cognitive load improves the ability to perform critical tasks such as surgical procedures and the driving abilities of emergency responders [
30,
31].
Anecdotally, the authors have noted that some students become distracted by either the environment or by some of the features of their avatars such as the ability to fly. These perceived distractions may reduce what the students learn during the training period, which could result in reduced efficiency as a result of being unfamiliar with either the task (s), HUD, or other critical skills during the simulation. Similar findings were reported elsewhere [
6].
Perhaps the most serious limitation that affects the quality of this simulation and one that is not directly linked to Second Life® is lack of a permanent standing pool of avatar character actors as part of the instructional team. This results in a reliance on volunteer actors playing the various avatar roles in the scenario. The authors would prefer to use professional or trained actors to fill these roles but that would likely require considerable compensation for their services. Currently, undergraduate students from the university fill these roles and do so for one credit of independent study. Other actors come from a small pool of non-students who are associated with the rotation, and they willingly volunteer their time to assist with support of the simulation. Although actors are recruited on a continuous basis throughout the year, there is still often a shortage of qualified actors.
The actors provide the interpersonal interactions that are essential to developing and evaluating the students’ communication skills. The actors bring added human emotion to the scenario. Anecdotally, the more times the students play their roles in the simulation, the more conversations appear more comfortable and natural, and their emotions appear more genuine. They also stimulate the students to examine the ethical, moral, and legal liabilities that a veterinarian remains accountable for in an emergency response. The actors, through their avatar character, can introduce the personal loss that is suffered by those that experience disaster. This creates a path for examining whether compassion is present as part of the human interaction.
Table 2 summarizes the limitations of Second Life
® as well as the external limitations.
4. Advantages
As discussed in the analysis of immersive training in medical education, there are many benefits to conducting high-stakes, low-frequency disaster response training in a virtual, immersive environment [
32,
33]. First, there is essentially zero safety risk to students and patients. Next, the training can be repeated ad infinitum allowing for repeated attempts; however, that is not part of the current curriculum. Instead, it offers a consistent and homogenous experience amongst the student body which results in a more uniform experience and promotes a more consistent skill set in each graduating class. Although the initial costs and investments needed to develop this virtual environment were high, the operating costs for each rotation are essentially zero. Periodically, investments are made to improve the virtual environment, and ultimately the students’ experience, but these costs have no impact on the regular conduction of the rotation.
5. Future Directions
Future directions for the use of Second Life
® in the rotation are centered on improving the student experience and facilitating more thorough assessment of student performance. First, to add additional realism and to make the patients more interactive, the authors are collaborating with the contract designers to integrate patient vital parameters (similar to a health bar or health status indicator in other video games) that serve as a visual representation of the patient’s health represented through heart rate, respiratory rate, and temperature. That information could then be manipulated (increased or decreased) by a faculty member in response to student actions (treatment or lack of treatment). The use of a health bar is common in many popular video games and is generally positively received by players [
34]. Given the demographics of the rotation, it is likely that the use of a health bar on simulated patients would be both familiar and well received by students participating in the simulation.
There has also been discussion about creating a second virtual environment. Instead of a tornado event, this virtual environment would be modeled after a large, catastrophic hurricane. Given Texas A&M University’s proximity to the Gulf of Mexico coupled with the impacts of climate change on the Atlantic hurricane season, this is a situation that many of the rotation’s graduates may face during their professional career. Although many of the injuries seen following a hurricane would be similar to those that would be seen in the wake of a tornado, there are other injuries, primarily those associated with prolonged submersion in water, that would be beneficial for students to see.
To further improve the student experience, the authors are interested in advancing to fully immersive VR by incorporating stereoscopic 3D headsets such as Meta Quest (Reality Labs, San Francisco, CA) or a similar device that is compatible with Second Life
® [
7]. Several studies have been published that have demonstrated the efficacy of this technology in medical education [
35,
36,
37]. The use of this technology is not without consequence or complication as some users reported experiencing nausea and others reported technical issues with the equipment [
36,
37]. Unfortunately, this type of improvement will require considerable financial investment.
6. Summary
The use of Second Life® in the Veterinary Emergency Management rotation to train veterinary students to respond to disasters is the first of its kind. More than 1800 senior veterinary students as well as students from other veterinary schools in the United States, Caribbean, and Europe have taken part in the simulation. Those students who have completed the rotation carry with them into their clinical practice a set of disaster preparedness response skills that enhance the capacity of their individual animal hospital as well as their local community that could prove invaluable in the wake of a disaster. The use of the MUVE, Second Life®, provides those students with an invaluable experiential learning opportunity that could not be achieved without the use of this technology.
Used in this context, Second Life®, allows students to demonstrate their critical thinking and problem-solving abilities in a safe and controlled environment. The students are also able to practice communicating with their peers and with external actors in stressful but controlled situations. Regardless of their involvement in disaster response after graduation, the development of critical thinking, problem-solving, and communication skills will benefit them in their professional careers. Moreover, it allows for the assessment of the students’ abilities in these domains.
The authors hope that this publication serves as an effective demonstration of the value of using Second Life® in veterinary disaster preparedness and response training. We hope too that the information provided here serves as not only a reference for the development of a disaster-specific clinical rotation but that it inspires other institutions, educators, and community and industry stakeholders to invest in such a program. Doing so can build veterinary disaster preparedness response capacities at local and state levels, which could prove invaluable before, during and after future disasters. We also believe that the use of Second Life® could be employed in other nations to promote the capacity to respond to natural disasters and epizootics. The online nature of Second Life® could easily facilitate the global distribution of knowledge and skill development through experiential learning lead by experts in their fields.
Author Contributions
Conceptualization, K.J., N.E. and D.Z.; original draft preparation, K.J., N.E. and D.Z.; writing—review and editing, K.J., N.E. and D.Z.; visualization, K.J. and D.Z.; supervision, D.Z.; project administration, N.E. and D.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study.
Acknowledgments
The authors would like to recognize the contract software programmers using their avatar names, Xandi Mars and Random Cole. Without their years of dedication, expertise, and support, the disaster simulation would not be what it is today and the more than 1 veterinary students who participated in the rotation would not have the knowledge and skills to better assist their patients, clients, and communities in time of need.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
Table A1.
An outline of a typical rotation.
Table A1.
An outline of a typical rotation.
| Week | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday and Sunday |
|---|
Week 1
Disaster Preparedness | | | | | | |
Week 2
Disaster Response | | Individual resiliency and mental health in disasters Field euthanasia techniques Risk and disaster communication Developing a medical cache Principles of emergency sheltering
| | | | |
Appendix B
This appendix contains five rubrics used to evaluate student performance during the simulation. The rubrics are used to assess five New Graduate Outcomes (NGOs) which include (
Table A2) NGO 6: emergency and intensive care case management; (
Table A3) NGO 8: communication, ethical conduct, and professional behavior; (
Table A4) NGO 10: team collaboration, leadership, and practice management; (
Table A5) NGO 12: multicultural awareness and self-management; and (
Table A6) NGO 13: animal welfare. Other NGOs are assessed during the rotation; however, these NGOs pertain to the county assessment and plan development, shelter planning, and other emergency preparedness functions. These rubrics were adapted from a previous publication [
4] (pp. 40–45).
Table A2.
Rubric used to evaluate New Graduate Outcome (NGO) 6: emergency and intensive care case management.
Table A2.
Rubric used to evaluate New Graduate Outcome (NGO) 6: emergency and intensive care case management.
| Score | % of Grade | Rating | Suggested Comments | Dimension Comments |
|---|
| | 15 | Excellent | | Excellent:Can perform rapid, efficient examination and triage for an emergency patient in a disaster setting without assistance or guidance. Confidently recognizes patients requiring immediate vs. delayed care. Can accurately and independently create and implement an appropriate therapeutic plan for a patient in a disaster setting.
|
| | | Satisfactory | | Satisfactory:Can perform an examination or triage an emergent patient but may require faculty assistance in a disaster setting and lacks confidence to perform without assistance. Can complete a treatment plan for an emergent patient in a disaster setting without faculty support in most cases. Can recognize patients requiring immediate vs. delayed care in a disaster setting in most cases.
|
| | | Needs Improvement | | Needs Improvement:Requires faculty assistance to triage a patient in a disaster setting or needs improvement in completing an examination on an emergent patient in a disaster setting. Needs improvement in recognizing patients requiring immediate or delayed care in a disaster setting. Inconsistently demonstrates knowledge of basic medical therapy and requires faculty support or encouragement to create a therapeutic plan for a patient in a disaster setting.
|
| | | Unsatisfactory | | Unsatisfactory:Is unable to properly examine or triage an emergent patient in a disaster setting even with faculty guidance. Is unable to recognize or provide care for a patient in a disaster setting requiring immediate vs. delayed care. Lacks the knowledge to discuss basic principles of medical therapy or to create a basic therapeutic plan for an emergency patient in a disaster setting.
|
Table A3.
Rubric used to evaluate NGO 8: communication, ethical conduct, and professional behavior.
Table A3.
Rubric used to evaluate NGO 8: communication, ethical conduct, and professional behavior.
| Score | % of Grade | Rating | Suggested Comments | Dimension Comments |
|---|
| | 20 | Excellent | | Excellent:Is an articulate, succinct, and confident communicator. Demonstrates a high level of professional confidence and the ability to self-reflect to improve professional performance. Is highly effective through verbal communication. Clearly possesses empathy, which is easily demonstrated in interactions with clients or others. Demonstrates extraordinary collegiality and willingness to assist colleagues with patient care Displays professional demeanor, punctuality, and attire at all times.
|
| | | Satisfactory | | Satisfactory:Demonstrates acceptable communication skills but will benefit from experience. Clearly demonstrates growing professional confidence and the ability to self-reflect to improve professional success. Demonstrates good verbal communication skills. Demonstrates empathy for clients in most situations. Is collegial and volunteers to assist colleagues with patient care on some occasions. Demonstrates acceptable professional demeanor, punctuality, and/or attire in most situations
|
| | | Needs Improvement | | Needs Improvement:Needs improvement in communication skills and additional experience to become a more effective communicator. Inconsistently demonstrates an appropriate level of professional confidence and needs improvement in the ability to self-reflect to improve performance. Needs improvement in verbal communication skills to become an effective communicator. Fails to consistently demonstrate appropriate empathy for clients or others. Fails to demonstrate collegiality and will assist colleagues only when asked. Lacks consistent demonstration of professional demeanor, punctuality, or attire.
|
| | | Unsatisfactory | | Unsatisfactory:Demonstrates an unacceptable level of client communication skills and will require considerable experience to improve skills to an appropriate level. Lacks professional confidence and is unable to self-reflect to improve personal performance. Demonstrates unacceptable verbal communication skills. Lacks the ability to demonstrate empathy for patients. Refuses to provide collegial support or assist colleagues. Routinely fails to demonstrate professional demeanor, punctuality, and/or attire.
|
Table A4.
Rubric used to evaluate NGO 10: team collaboration, leadership, and practice management.
Table A4.
Rubric used to evaluate NGO 10: team collaboration, leadership, and practice management.
| Score | % of Grade | Rating | Suggested Comments | Dimension Comments |
|---|
| | 20 | Excellent | | Excellent:Interacts in an enthusiastic and highly effective manner with all members of the health care team. Seeks opportunities for leadership and acts as a role model for colleagues through strong leadership skills 3. Works extremely well under pressure, maintains work ethic, and manages stressful situations with ease. Willingly works autonomously and clearly accepts personal responsibility. Demonstrates strong understanding of practice management principles and works with others to share this knowledge.
|
| | | Satisfactory | | Satisfactory:Interacts in a positive manner with most members of the health care team. Can perform as a leader and willingly accepts the leadership role if it arises. Can maintain work ethic under pressure with minimal personal stress. Can work autonomously when necessary and can accept personal responsibility. Demonstrates an appropriate understanding of practice management principles.
|
| | | Needs Improvement | | Needs Improvement:Fails to consistently interact in a positive manner with members of the health care team. Lacks strong leadership skills and will assume a leadership role only when prompted by clinician. Fails to consistently maintain work ethic under the pressure of basic case management and is easily stressed when in intense situations. Is uncomfortable working autonomously and fails to consistently accept personal responsibility. Needs improvement in understanding basic practice management principles.
|
| | | Unsatisfactory | | UnsatisfactoryIs unable to positively interact with members of the health care team. Demonstrates poor leadership skills, avoids leadership opportunities, and appears uncomfortable assuming a leadership role. Fails to maintain work ethic under pressure and displays negative behaviors and clear signs of stress under the pressure of basic case management. Is unable to work autonomously or accept personal responsibility. Demonstrates poor understanding of practice management principles.
|
Table A5.
Rubric used to evaluate NGO 12: multicultural awareness and self-management.
Table A5.
Rubric used to evaluate NGO 12: multicultural awareness and self-management.
| Score | % of Grade | Rating | Suggested Comments | Dimension Comments |
|---|
| | 15 | Excellent | | Excellent:Explores and embraces the diversity and cultural differences of fellow students, instructors, and the community. Demonstrates a high level of cultural competence and communicates with exceptional cultural sensitivity. Is highly organized and demonstrates effective management of personal time, resources, and work assignments.
|
| | | Satisfactory | | Satisfactory:Demonstrates acceptance of the diversity and cultural differences of fellow students, instructors, and community. Demonstrates cultural competence and communicates with acceptable cultural sensitivity. Demonstrates acceptable organizational skills and management of personal time, resources, and work assignments.
|
| | | Needs Improvement | | Needs Improvement:Requires prompting but can acknowledge diversity and cultural differences of fellow students, instructors, and community Requires encouragement to demonstrate cultural competence and to communicate cultural sensitivity. Needs improvement in both organizational and personal management skills.
|
| | | Unsatisfactory | | UnsatisfactoryDemonstrates a lack of acceptance of the diversity or cultural differences of fellow students, instructors, or community. Lacks understanding of cultural competence and fails to communicate with cultural sensitivity despite instructor encouragement. Demonstrates poor organizational skills and lacks appropriate management of personal time, resources, or assignments.
|
Table A6.
Rubric used to evaluate NGO 13: animal welfare.
Table A6.
Rubric used to evaluate NGO 13: animal welfare.
| Score | % of Grade | Rating | Suggested Comments | Dimension Comments |
|---|
| | 15 | Excellent | | Excellent:Effectively and consistently applies knowledge of animal behavior to improve safety of the patient and health care team. Clearly recognizes when euthanasia is an appropriate option for a patient and can clearly discuss principles of euthanasia. Effectively addresses client grief regarding euthanasia without clinician prompting.
|
| | | Satisfactory | | Satisfactory:Demonstrates knowledge of animal behavior to improve safety of the patient and team in most situations. Recognizes when euthanasia is an appropriate option for most patients. Can manage client grief but may require clinician prompting to initiate
|
| | | Needs Improvement | | Needs Improvement:Demonstrates inconsistent knowledge of animal behavior and needs improvement in selection of appropriate restraint methods. Fails to recognize euthanasia as an appropriate option for a patient but may be able to discuss the principles of euthanasia. Fails to demonstrate appropriate mechanisms for mediating client grief unless prompted by clinician.
|
| | | Unsatisfactory | | UnsatisfactoryDemonstrates inappropriate knowledge of animal behavior or consistently makes poor selections for appropriate restraint Is unable to recognize when euthanasia is an appropriate option for a patient and is unable to discuss the principles of euthanasia. Fails to provide or initiate management of client grief even with clinician prompting.
|
References
- Bissett, W.T.; Zoran, D.L.; Clendenin, A.; Espitia, N.F.; Moyer, W.; Rogers, K.S. How a Disaster Preparedness Rotation Helps Teach the Seven NAVMEC Professional Competencies: The Texas A&M University Experience. J. Vet. Med. Educ. 2013, 40, 378–388. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Sun, N.; Cao, C.; Hou, S.; Gong, Y. Review on Visualization Technology in Simulation Training System for Major Natural Disasters. Nat. Hazards 2022, 112, 1851–1882. [Google Scholar] [CrossRef]
- Dunning, D.; Martin, M.P.; Tickel, J.L.; Gentry, W.B.; Cowen, P.; Slenning, B.D. Preparedness and Disaster Response Training for Veterinary Students: Literature Review and Description of the North Carolina State University Credentialed Veterinary Responder Program. J. Vet. Med. Educ. 2009, 36, 317–330. [Google Scholar] [CrossRef]
- Espitia, N.F.; Zoran, D.L.; Clendenin, A.; Crosby, S.M.; Dominguez, B.; Ellis, C.L.; Hilburn, A.; Moyer, W.; Bissett, W.T. Direct Measurement of Veterinary Student Learning Outcomes for the NAVMEC Professional Competencies in a Multi-User Virtual Learning Environment. J. Vet. Med. Educ. 2021, 48, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Garcia, L.N.; Stefanou, C.; Huston, C.L.; Bell, S.A. Assessing Veterinary Practice and Practitioner Preparedness for Natural and Man-Made Disasters, Including COVID-19. J. Vet. Med. Educ. 2021, 49, e20210066. [Google Scholar] [CrossRef] [PubMed]
- Traphagan, T.W.; Chiang, Y.V.; Chang, H.M.; Wattanawaha, B.; Lee, H.; Mayrath, M.C.; Woo, J.; Yoon, H.-J.; Jee, M.J.; Resta, P.E. Cognitive, Social and Teaching Presence in a Virtual World and a Text Chat. Comput. Educ. 2010, 55, 923–936. [Google Scholar] [CrossRef]
- Aghapour, M.; Bockstahler, B. State of the Art and Future Prospects of Virtual and Augmented Reality in Veterinary Medicine: A Systematic Review. Animals 2022, 12, 3517. [Google Scholar] [CrossRef]
- Petrov, P.; Atanasova, T. Digital Twins with Application of AR and VR in Livestock Instructions. Probl. Eng. Cybern. Robot. 2021, 77, 39–50. [Google Scholar] [CrossRef]
- Mauldin Pereira, M.; Artemiou, E.; McGonigle, D.; Conan, A.; Sithole, F.; Yvorchuk-St. Jean, K. Using the Virtual World of Second Life in Veterinary Medicine: Student and Faculty Perceptions. J. Vet. Med. Educ. 2018, 45, 148–155. [Google Scholar] [CrossRef]
- Salmon, G. The Future for (Second) Life and Learning. Br. J. Educ. Technol. 2009, 40, 526–538. [Google Scholar] [CrossRef]
- Wiecha, J.; Heyden, R.; Sternthal, E.; Merialdi, M. Learning in a Virtual World: Experience with Using Second Life for Medical Education. J. Med. Internet Res. 2010, 12, e1. [Google Scholar] [CrossRef] [PubMed]
- Neubacher, M.; Siebers, P.; Wittek, A.; Recker, F. How to Play a Game Properly—Enhancing Obstetrics and Gynecology Education through Gamification: A Scoping Review. Geburtshilfe Frauenheilkd. 2024, 84, 1126–1134. [Google Scholar] [CrossRef]
- Conradi, E.; Kavia, S.; Burden, D.; Rice, A.; Woodham, L.; Beaumont, C.; Savin-Baden, M.; Poulton, T. Virtual Patients in a Virtual World: Training Paramedic Students for Practice. Med. Teach. 2009, 31, 713–720. [Google Scholar] [CrossRef]
- Gout, L.; Hart, A.; Houze-Cerfon, C.-H.; Sarin, R.; Ciottone, G.R.; Bounes, V. Creating a Novel Disaster Medicine Virtual Reality Training Environment. Prehospital Disaster Med. 2020, 35, 225–228. [Google Scholar] [CrossRef]
- Monahan, C.; Ullberg, L.; Harvey, K. Virtual Emergency Preparedness Planning Using Second Life. In Proceedings of the 2009 IEEE/INFORMS International Conference on Service Operations, Logistics and Informatics, Chicago, IL, USA, 22–24 July 2009; IEEE: Chicago, IL, USA, 2009; pp. 306–310. [Google Scholar] [CrossRef]
- Caroux, L.; Isbister, K. Influence of Head-up Displays’ Characteristics on User Experience in Video Games. Int. J. Hum.-Comput. Stud. 2016, 87, 65–79. [Google Scholar] [CrossRef]
- Zackoff, M.W.; Cruse, B.; Sahay, R.D.; Zhang, B.; Sosa, T.; Schwartz, J.; Depinet, H.; Schumacher, D.; Geis, G.L. Multiuser Immersive Virtual Reality Simulation for Interprofessional Sepsis Recognition and Management. J. Hosp. Med. 2024, 19, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Lerner, D.; Mohr, S.; Schild, J.; Göring, M.; Luiz, T. An Immersive Multi-User Virtual Reality for Emergency Simulation Training: Usability Study. JMIR Serious Games 2020, 8, e18822. [Google Scholar] [CrossRef] [PubMed]
- Fairhurst, K.; Strickland, A.; Maddern, G. The LapSim Virtual Reality Simulator: Promising but Not yet Proven. Surg. Endosc. 2011, 25, 343–355. [Google Scholar] [CrossRef]
- Van Der Meijden, O.A.J.; Schijven, M.P. The Value of Haptic Feedback in Conventional and Robot-Assisted Minimal Invasive Surgery and Virtual Reality Training: A Current Review. Surg. Endosc. 2009, 23, 1180–1190. [Google Scholar] [CrossRef]
- Westebring-Van Der Putten, E.P.; Goossens, R.H.M.; Jakimowicz, J.J.; Dankelman, J. Haptics in Minimally Invasive Surgery—A Review. Minim. Invasive Ther. Allied Technol. 2008, 17, 3–16. [Google Scholar] [CrossRef]
- Tholey, G.; Desai, J.P.; Castellanos, A.E. Force Feedback Plays a Significant Role in Minimally Invasive Surgery: Results and Analysis. Ann. Surg. 2005, 241, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Gurusamy, K.; Aggarwal, R.; Palanivelu, L.; Davidson, B.R. Systematic Review of Randomized Controlled Trials on the Effectiveness of Virtual Reality Training for Laparoscopic Surgery. Br. J. Surg. 2008, 95, 1088–1097. [Google Scholar] [CrossRef] [PubMed]
- Våpenstad, C.; Hofstad, E.F.; Bø, L.E.; Kuhry, E.; Johnsen, G.; Mårvik, R.; Langø, T.; Hernes, T.N. Lack of Transfer of Skills after Virtual Reality Simulator Training with Haptic Feedback. Minim. Invasive Ther. Allied Technol. 2017, 26, 346–354. [Google Scholar] [CrossRef]
- Kneebone, R. Simulation in Surgical Training: Educational Issues and Practical Implications. Med. Educ. 2003, 37, 267–277. [Google Scholar] [CrossRef]
- Rudolphi-Solero, T.; Lorenzo-Álvarez, R.; Domínguez-Pinos, D.; Ruiz-Gómez, M.J.; Sendra-Portero, F. An Interuniversity Competition for Medical Students to Learn Radiology in the Second Life Metaverse. J. Am. Coll. Radiol. 2024, 21, 812–821. [Google Scholar] [CrossRef] [PubMed]
- Appelboom, Y.; Groenen, Y.; Notten, D.; Bruin, A.D.; Buijs, J.; Haak, H.R.; Broggreve, H.F.; Lambriks, L.; Stassen, P.M. Experienced Cognitive Load in the Emergency Department. A Prospective Study. PLoS ONE 2025, 20, e0314052. [Google Scholar] [CrossRef]
- Dworkis, D.A.; Jain, A.; Wolfe, M.; Sanko, S.; Arora, S. Cognitive Load during Training for Out-of-Department Emergency Responses. AEM Educ. Train. 2022, 6, e10742. [Google Scholar] [CrossRef]
- Gutiérrez, Á.; Blanco, P.; Ruiz, V.; Chatzigeorgiou, C.; Oregui, X.; Álvarez, M.; Navarro, S.; Feidakis, M.; Azpiroz, I.; Izquierdo, G.; et al. Biosignals Monitoring of First Responders for Cognitive Load Estimation in Real-Time Operation. Appl. Sci. 2023, 13, 7368. [Google Scholar] [CrossRef]
- Sankaranarayanan, G.; Odlozil, C.A.; Wells, K.O.; Leeds, S.G.; Chauhan, S.; Fleshman, J.W.; Jones, D.B.; De, S. Training with Cognitive Load Improves Performance under Similar Conditions in a Real Surgical Task. Am. J. Surg. 2020, 220, 620–629. [Google Scholar] [CrossRef]
- Hembroff, C.C.; Arbuthnott, K.D.; Krätzig, G.P. Emergency Response Driver Training: Dual-Task Decrements of Dispatch Communication. Transp. Res. Part F Traffic Psychol. Behav. 2018, 59, 222–235. [Google Scholar] [CrossRef]
- Lateef, F. Simulation-Based Learning: Just like the Real Thing. J. Emerg. Trauma Shock 2010, 3, 348. [Google Scholar] [CrossRef] [PubMed]
- Pottle, J. Virtual Reality and the Transformation of Medical Education. Future Healthc. J. 2019, 6, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Gittens, C.L.; Gloumeau, P.C. Does a Segmented Health Bar Affect a Player’s Preference for a Game? A Pilot Study. In Proceedings of the 2015 IEEE Games Entertainment Media Conference (GEM), Toronto, ON, Canada, 14–16 October 2015; pp. 1–8. [Google Scholar] [CrossRef]
- Moro, C.; Štromberga, Z.; Stirling, A. Virtualisation Devices for Student Learning: Comparison between Desktop-Based (Oculus Rift) and Mobile-Based (Gear VR) Virtual Reality in Medical and Health Science Education. Australas. J. Educ. Technol. 2017, 33, 1–10. [Google Scholar] [CrossRef]
- Zackoff, M.W.; Real, F.J.; Sahay, R.D.; Fei, L.; Guiot, A.; Lehmann, C.; Tegtmeyer, K.; Klein, M. Impact of an Immersive Virtual Reality Curriculum on Medical Students’ Clinical Assessment of Infants With Respiratory Distress. Pediatr. Crit. Care Med. 2020, 21, 477–485. [Google Scholar] [CrossRef]
- O’Connor, M.; Stowe, J.; Potocnik, J.; Giannotti, N.; Murphy, S.; Rainford, L. 3D Virtual Reality Simulation in Radiography Education: The Students’ Experience. Radiography 2021, 27, 208–214. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).