Effect of Cognitive Distractors on Neonatal Endotracheal Intubation Performance: Insights from a Dual-Task Simulator
Abstract
1. Introduction
- Identify the limitations inherent in the current single-task ETI training paradigm, particularly its inadequacy in transferring skill from simulation to clinical settings.
- Develop the first dual-task mixed-reality (MR) simulator for neonatal endotracheal intubation. The simulator effectively captures expert-novice performance differences that traditional training paradigms fail to detect.
- Facilitate seamless transition between single-task and dual-task modes in future works using the MR simulator.
- Develop an automated skill evaluation strategy for trainee performance.
- Ground the efficacy of the multitask ETI training method in theoretical and empirical research from cognitive psychology, thereby paving the way for the evaluation of novel training regimens in future endeavors.
2. Related Work
3. Study Design
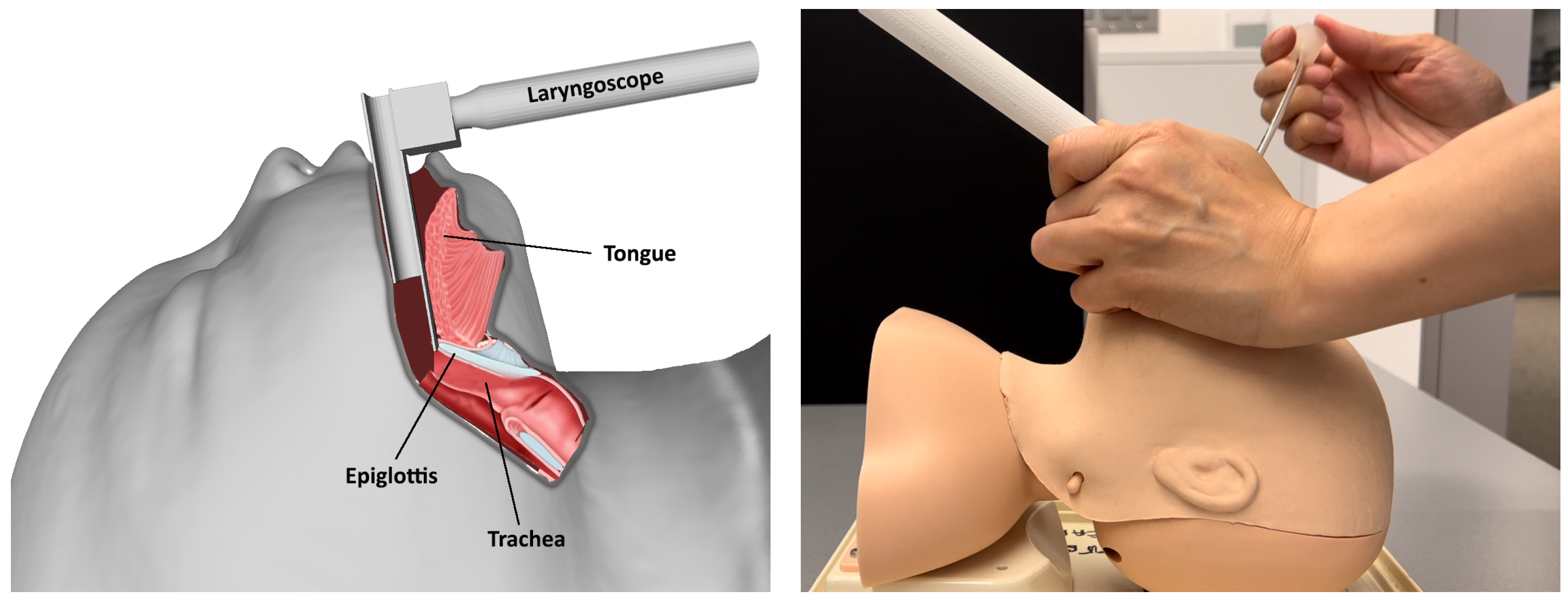
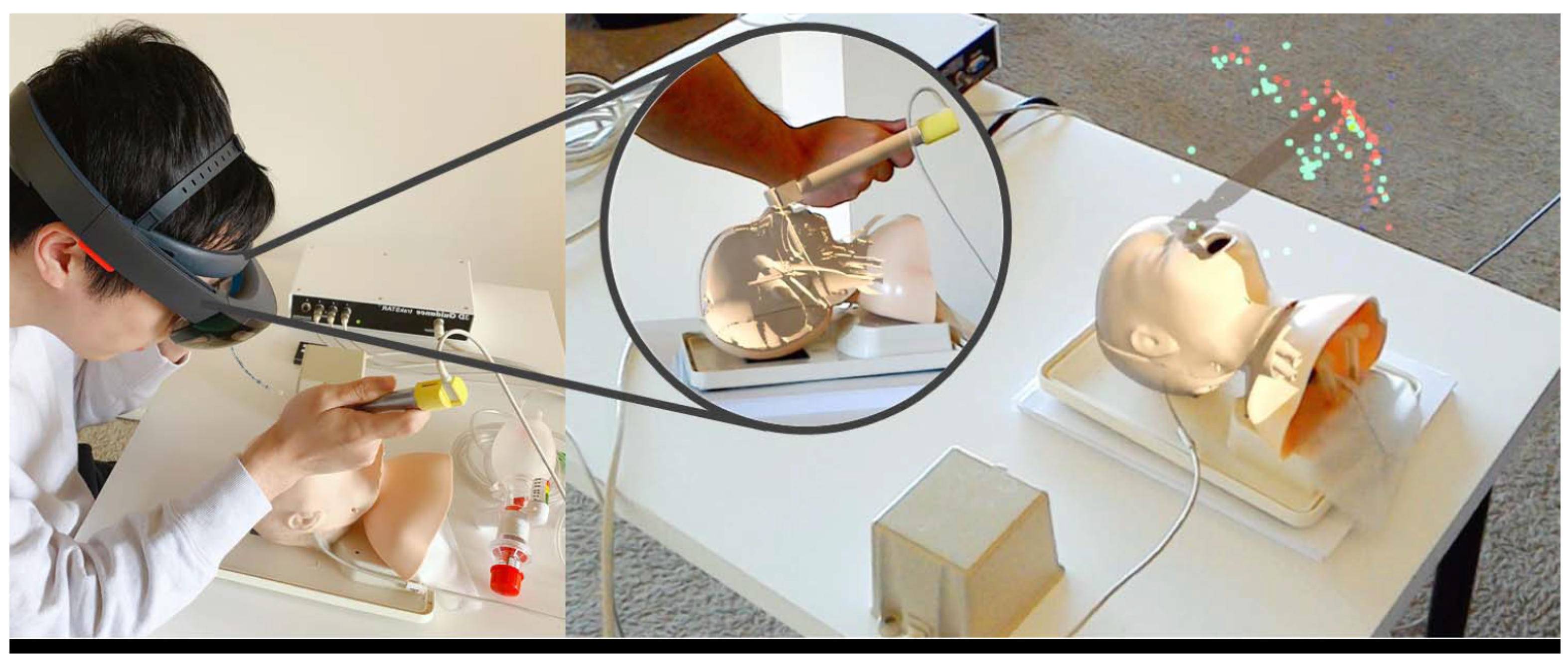
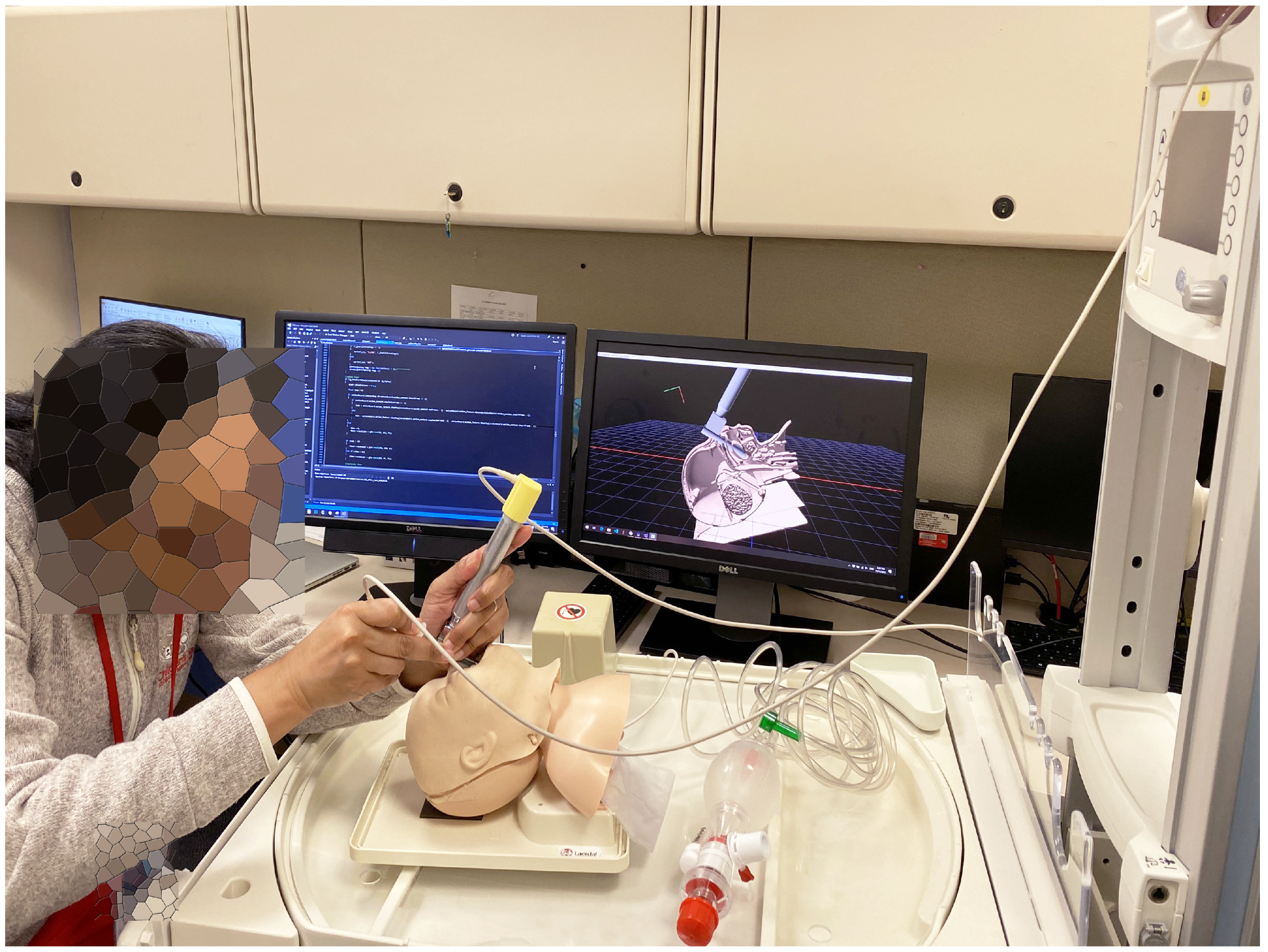
3.1. Simulator Design
- 1-back: Upon detecting a number’s immediate repetition, participants are instructed to activate the footswitch, enabling the MR simulator to capture the corresponding timestamp for a hit event recording. For example, a user will tap the footswitch upon hearing the second occurrence of the number 3 within the sequence {...6, 2, 3, 3, 5,...}. The number and order of the sequence are randomized for each trial.
- 2-back: Upon detecting a number’s recurrence after a different one, participants are instructed to activate the footswitch for a hit event recording. For example, a user will hit the footswitch when hearing the second occurrence of the number 8 within the sequence {...2, 7, 8, 5, 8,...}. The number and order of the sequence are randomized for each trial.
3.2. Dataset Collection
4. Methods
4.1. Primary ETI Task Metrics
4.2. Secondary Task Metrics
4.3. Statistic Metrics
- There is no performance difference between experts and novices for each task setting.
- There is no performance difference under different task settings for the same group (expert or novice).
- There is no difference between experts and novices on how the dual-task impacts their performance.
- There is no difference in ETI performance under intensive training.
5. Results and Discussion
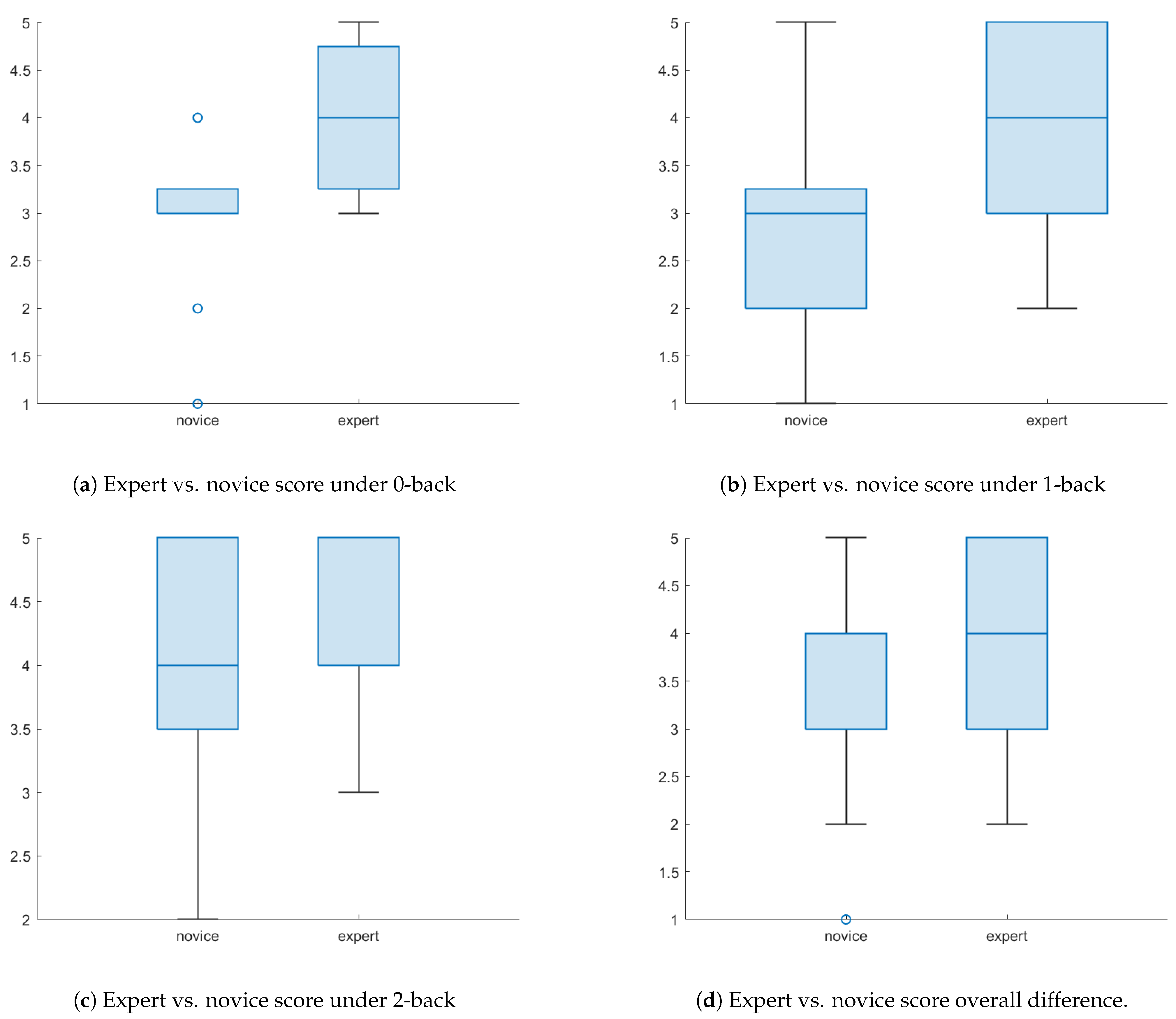
5.1. Expert vs. Novice
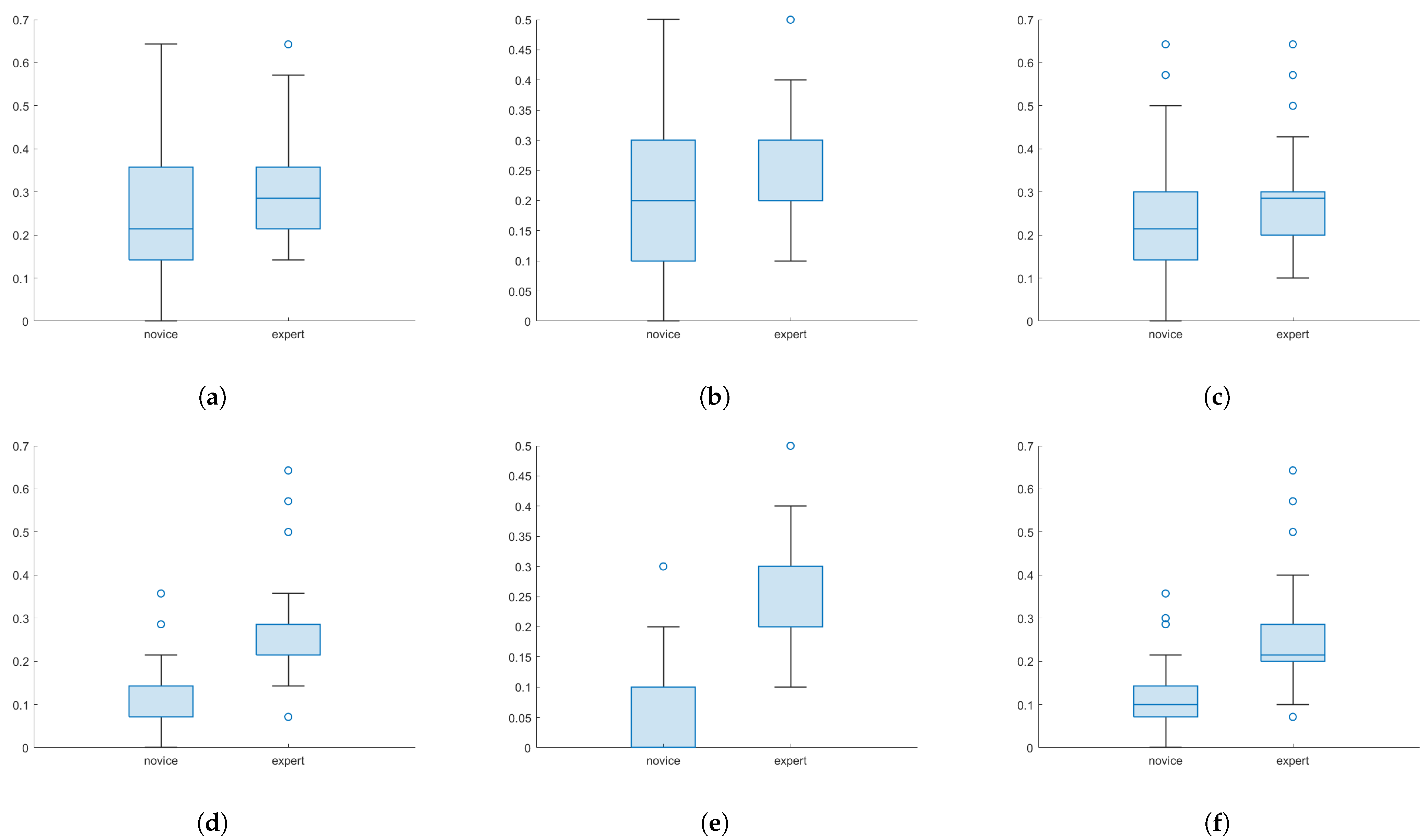
5.1.1. Primary Task Performance Comparison
5.1.2. Secondary Task Performance Comparison
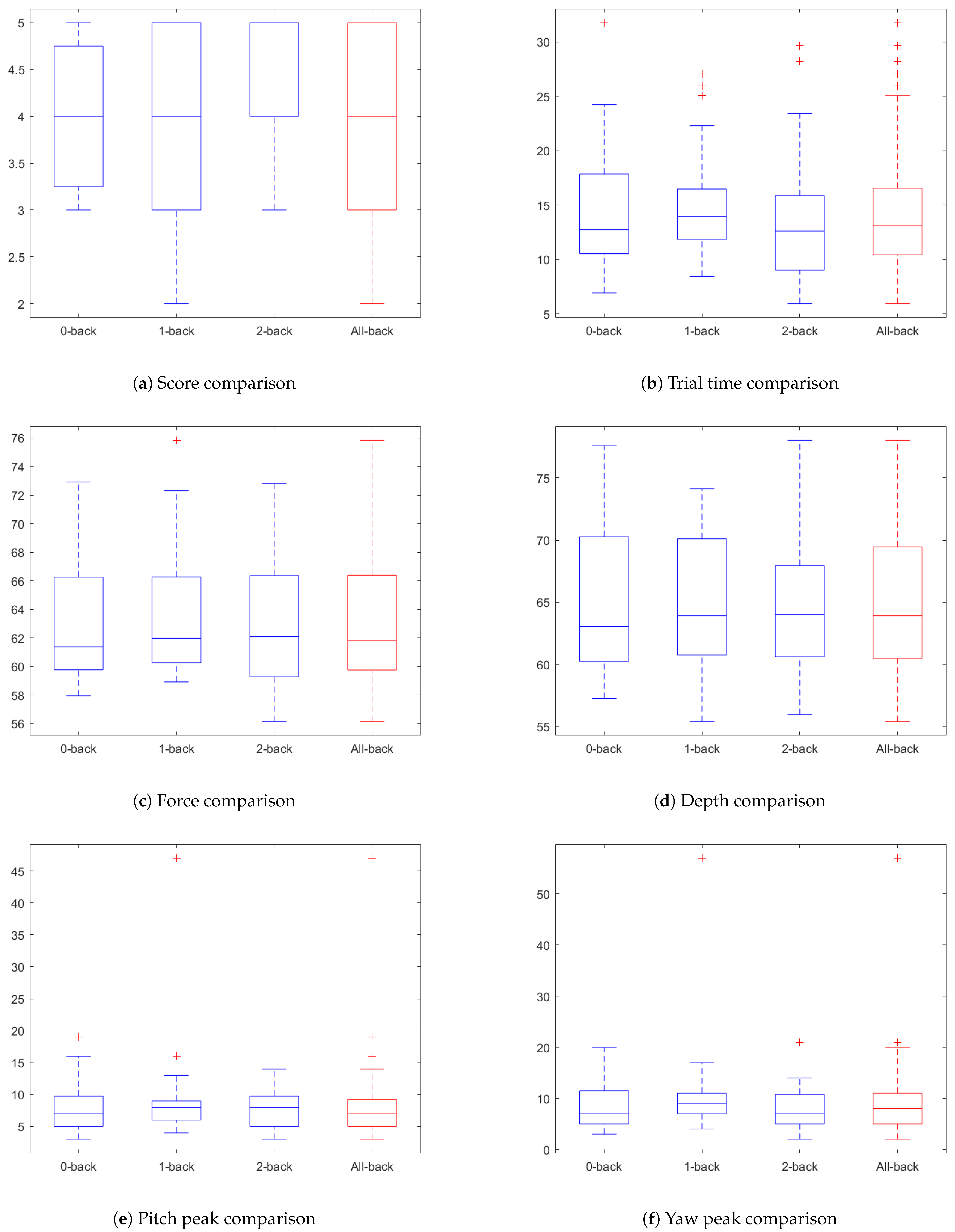
5.2. Dual-Task Interference Effects on Expert
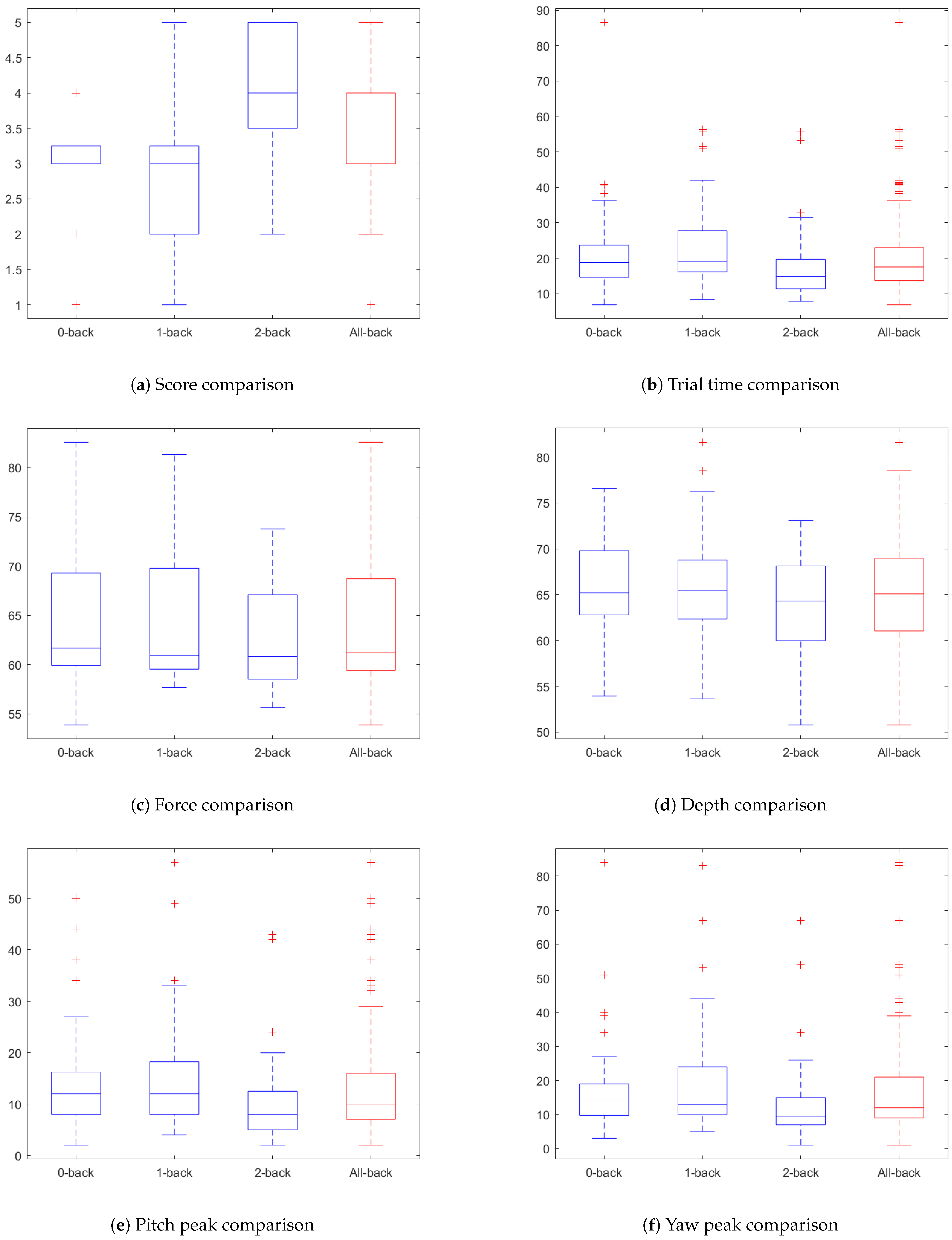
5.3. Dual-Task Interference Effects on Novice
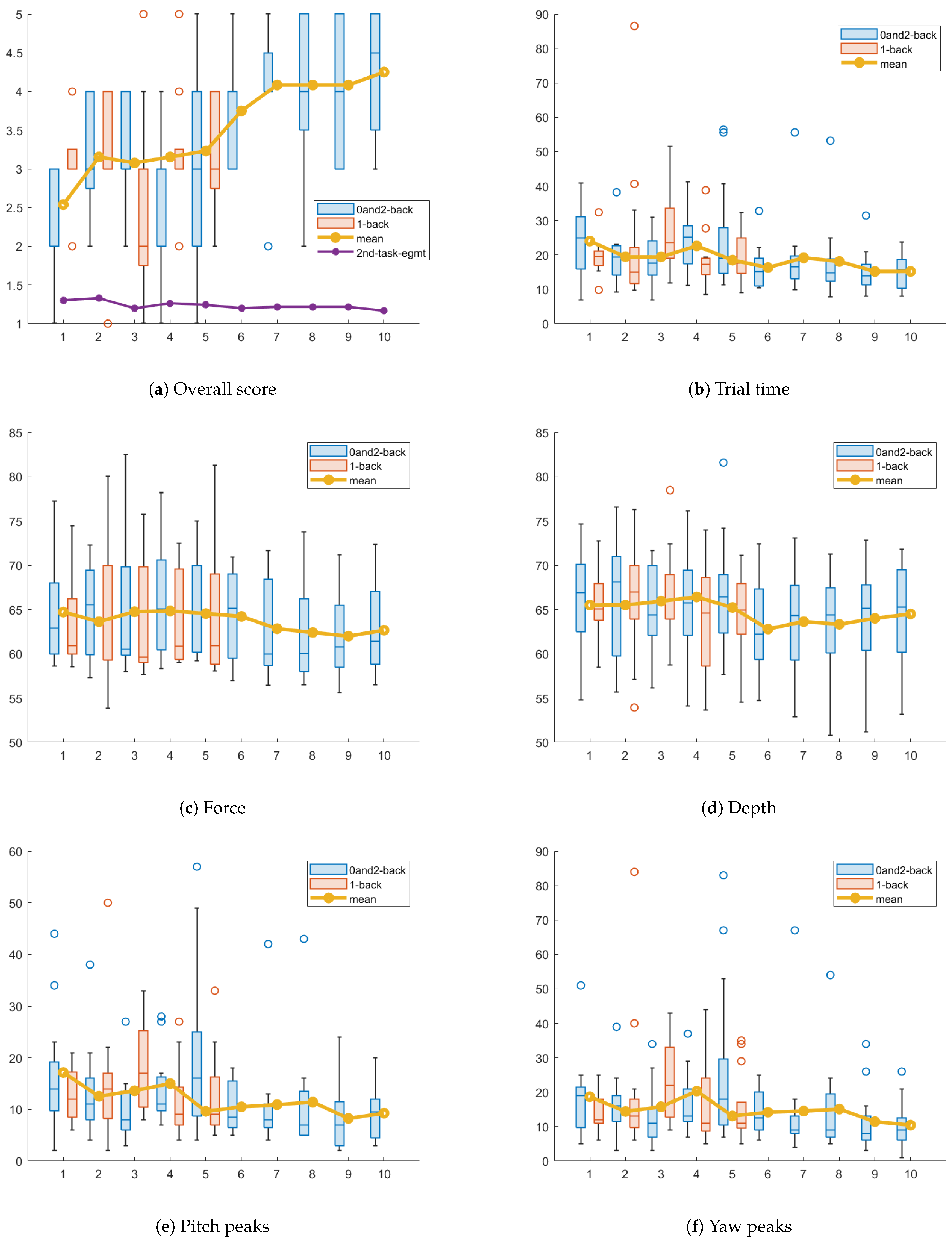
5.4. ETI Performance Variation over Trials
5.4.1. Expert Performance Change over Trials
5.4.2. Novice Performance Change over Trials
5.5. Discussion
- Single-task performance measurements are insufficient to evaluate practitioner’s readiness for clinical practice.
- Individuals with different levels of expertise exhibit distinct responses when subjected to dual-task conditions.
- Experts exhibit greater resilience to the adverse effects of elevated cognitive load, as compared to novices.
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ETI | Neonatal endotracheal intubation |
| ICUs | Intensive care units |
| ANOVA | Analysis of variance |
| MR | Mixed reality |
| AR | Augmented reality |
References
- Weiner, G.M.; Zaichkin, J. (Eds.) Textbook of Neonatal Resuscitation, 8th ed.; American Academy of Pediatrics and American Heart Association: Washington, DC, USA, 2021. [Google Scholar]
- DeMeo, S.D.; Katakam, L.; Goldberg, R.N.; Tanaka, D. Predicting neonatal intubation competency in trainees. Pediatrics 2015, 135, e1229–e1236. [Google Scholar] [CrossRef] [PubMed]
- Evans, P.; Shults, J.; Weinberg, D.D.; Napolitano, N.; Ades, A.; Johnston, L.; Levit, O.; Brei, B.; Krick, J.; Sawyer, T.; et al. Intubation competence during neonatal fellowship training. Pediatrics 2021, 148, e2020036145. [Google Scholar] [CrossRef]
- Konrad, C.; Schupfer, G.; Wietlisbach, M.; Gerber, H. Learning manual skills in anesthesiology: Is there a recommended number of cases for anesthetic procedures? Anesth. Analg. 1998, 86, 635–639. [Google Scholar] [CrossRef]
- Xiao, X.; Zhao, S.; Meng, Y.; Soghier, L.; Zhang, X.; Hahn, J. A physics-based virtual reality simulation framework for neonatal endotracheal intubation. In Proceedings of the 2020 IEEE Conference on Virtual Reality and 3D User Interfaces (VR), Atlanta, GA, USA, 22–26 March 2020; pp. 557–565. [Google Scholar]
- Meng, Y.; Hahn, J.K. An Automatic Grading System for Neonatal Endotracheal Intubation with Multi-Task Convolutional Neural Network. In Proceedings of the 2023 IEEE EMBS International Conference on Biomedical and Health Informatics (BHI), Pittsburgh, PA, USA, 15–18 October 2023; pp. 1–4. [Google Scholar]
- Haubner, L.Y.; Barry, J.S.; Johnston, L.C.; Soghier, L.; Tatum, P.M.; Kessler, D.; Downes, K.; Auerbach, M. Neonatal intubation performance: Room for improvement in tertiary neonatal intensive care units. Resuscitation 2013, 84, 1359–1364. [Google Scholar] [CrossRef]
- Schneider, W.; Shiffrin, R.M. Controlled and automatic human information processing: I. Detection, search, and attention. Psychol. Rev. 1977, 84, 1. [Google Scholar] [CrossRef]
- Sweller, J. Cognitive load during problem solving: Effects on learning. Cogn. Sci. 1988, 12, 257–285. [Google Scholar] [CrossRef]
- Logan, G.D. Automaticity, resources, and memory: Theoretical controversies and practical implications. Hum. Factors 1988, 30, 583–598. [Google Scholar] [CrossRef]
- Wickens, C.D. Processing resources and attention. In Multiple Task Performance; CRC Press: Boca Raton, FL, USA, 2020; pp. 3–34. [Google Scholar]
- Stefanidis, D.; Scerbo, M.W.; Korndorffer, J.R., Jr.; Scott, D.J. Redefining simulator proficiency using automaticity theory. Am. J. Surg. 2007, 193, 502–506. [Google Scholar] [CrossRef]
- Szafranski, C.; Kahol, K.; Ghaemmaghami, V.; Smith, M.; Ferrara, J.J. Distractions and surgical proficiency: An educational perspective. Am. J. Surg. 2009, 198, 804–810. [Google Scholar] [CrossRef]
- Haji, F.A.; Khan, R.; Regehr, G.; Drake, J.; de Ribaupierre, S.; Dubrowski, A. Measuring cognitive load during simulation-based psychomotor skills training: Sensitivity of secondary-task performance and subjective ratings. Adv. Health Sci. Educ. 2015, 20, 1237–1253. [Google Scholar] [CrossRef]
- Zirkle, M.; Roberson, D.W.; Leuwer, R.; Dubrowski, A. Using a virtual reality temporal bone simulator to assess otolaryngology trainees. Laryngoscope 2007, 117, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Bailey, J.; Ioannou, I.; Wijewickrema, S.; O’Leary, S.; Kennedy, G. Pattern-based real-time feedback for a temporal bone simulator. In Proceedings of the 19th ACM Symposium on Virtual Reality Software and Technology, Singapore, 6–8 October 2013; pp. 7–16. [Google Scholar]
- Pratt, P.; Ives, M.; Lawton, G.; Simmons, J.; Radev, N.; Spyropoulou, L.; Amiras, D. Through the HoloLens™ looking glass: Augmented reality for extremity reconstruction surgery using 3D vascular models with perforating vessels. Eur. Radiol. Exp. 2018, 2, 2. [Google Scholar] [CrossRef] [PubMed]
- Hamza-Lup, F.G.; Rolland, J.P.; Hughes, C. A distributed augmented reality system for medical training and simulation. arXiv 2018, arXiv:1811.12815. [Google Scholar]
- Alismail, A.; Thomas, J.; Daher, N.S.; Cohen, A.; Almutairi, W.; Terry, M.H.; Huang, C.; Tan, L.D. Augmented reality glasses improve adherence to evidence-based intubation practice. Adv. Med. Educ. Pract. 2019, 10, 279–286. [Google Scholar] [CrossRef]
- Desselle, M.R.; Brown, R.A.; James, A.R.; Midwinter, M.J.; Powell, S.K.; Woodruff, M.A. Augmented and virtual reality in surgery. Comput. Sci. Eng. 2020, 22, 18–26. [Google Scholar] [CrossRef]
- Dwivedi, S.; Hayes, J.; Pedron, I.; Kang, J.; Brenner, L.J.; Barnes, C.; Bailly, A.; Tanous, K.; Nelson, C.; Moats, J.; et al. Comparing the efficacy of AR-based training with video-based training. In Proceedings of the Human Factors and Ergonomics Society Annual Meeting, Atlanta, GA, USA, 10–14 October 2022; Volume 66, pp. 1862–1866. [Google Scholar]
- Foglia, E.E.; Ades, A.; Napolitano, N.; Leffelman, J.; Nadkarni, V.; Nishisaki, A. Factors associated with adverse events during tracheal intubation in the NICU. Neonatology 2015, 108, 23–29. [Google Scholar] [CrossRef]
- Hatch, L.D.; Grubb, P.H.; Lea, A.S.; Walsh, W.F.; Markham, M.H.; Whitney, G.M.; Slaughter, J.C.; Stark, A.R.; Ely, E.W. Endotracheal intubation in neonates: A prospective study of adverse safety events in 162 infants. J. Pediatr. 2016, 168, 62–66. [Google Scholar] [CrossRef]
- Sanders, R.C., Jr.; Giuliano, J.S., Jr.; Sullivan, J.E.; Brown, C.A., III; Walls, R.M.; Nadkarni, V.; Nishisaki, A. National Emergency Airway Registry for Children Investigators and Pediatric Acute Lung Injury and Sepsis Investigators Network. Level of trainee and tracheal intubation outcomes. Pediatrics 2013, 131, e821–e828. [Google Scholar] [CrossRef]
- Russo, S.G.; Bollinger, M.; Strack, M.; Crozier, T.A.; Bauer, M.; Heuer, J. Transfer of airway skills from manikin training to patient: Success of ventilation with facemask or LMA-SupremeTM by medical students. Anaesthesia 2013, 68, 1124–1131. [Google Scholar] [CrossRef]
- Prabhu, A.; Smith, W.; Yurko, Y.; Acker, C.; Stefanidis, D. Increased stress levels may explain the incomplete transfer of simulator-acquired skill to the operating room. Surgery 2010, 147, 640–645. [Google Scholar] [CrossRef]
- Mayrose, J.; Kesavadas, T.; Chugh, K.; Joshi, D.; Ellis, D.G. Utilization of virtual reality for endotracheal intubation training. Resuscitation 2003, 59, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Demirel, D.; Alexander, Y.; Halic, T.; Sankaranarayanan, G.; Ryason, A.; Spindler, D.; Butler, K.L.; Caroline, C.; Petrusa, E.; Molina, M.; et al. Virtual airway skills trainer (VAST) simulator. Stud. Health Technol. Inform. 2016, 220, 91. [Google Scholar] [PubMed]
- Mayrose, J.; Myers, J.W. Endotracheal intubation: Application of virtual reality to emergency medical services education. Simul. Healthc. 2007, 2, 231–234. [Google Scholar] [CrossRef]
- Rodrigues, M.A.F.; Gillies, D.; Charters, P. A biomechanical model of the upper airways for simulating laryngoscopy. Comput. Methods Biomech. Biomed. Eng. 2001, 4, 127–148. [Google Scholar] [CrossRef]
- Meng, Y. VR Enhanced Interactive Intubation Simulation. In Proceedings of the International Conference on Modeling, Simulation and Visualization Methods (MSV). The Steering Committee of The World Congress in Computer Science, Computer Engineering and Applied Computing (WorldComp), Las Vegas, NV, USA, 1–5 August 2018; pp. 81–87. [Google Scholar]
- Schumacher, E.H.; Seymour, T.L.; Glass, J.M.; Fencsik, D.E.; Lauber, E.J.; Kieras, D.E.; Meyer, D.E. Virtually perfect time sharing in dual-task performance: Uncorking the central cognitive bottleneck. Psychol. Sci. 2001, 12, 101–108. [Google Scholar] [CrossRef]
- Paas, F.G.; Van Merriënboer, J.J. Instructional control of cognitive load in the training of complex cognitive tasks. Educ. Psychol. Rev. 1994, 6, 351–371. [Google Scholar] [CrossRef]
- Sweller, J. Cognitive load theory. In Psychology of Learning and Motivation; Elsevier: Amsterdam, The Netherlands, 2011; Volume 55, pp. 37–76. [Google Scholar]
- Cook, D.A.; Hamstra, S.J.; Brydges, R.; Zendejas, B.; Szostek, J.H.; Wang, A.T.; Erwin, P.J.; Hatala, R. Comparative effectiveness of instructional design features in simulation-based education: Systematic review and meta-analysis. Med. Teach. 2013, 35, e867–e898. [Google Scholar] [CrossRef]
- Ward, M.D.; Helton, W.S. Dual-task interference while receiving information on a head mounted display and manual tracking with and without auditory warnings. Appl. Ergon. 2022, 101, 103713. [Google Scholar] [CrossRef]
- Neter, J.; Kutner, M.H.; Nachtsheim, C.J.; Wasserman, W. Applied Linear Statistical Models; McGraw-Hill/Irwin: New York, NY, USA, 1996. [Google Scholar]
- Ralston, A.; Wilf, H.S. (Eds.) Mathematical Methods for Digital Computers; Wiley: New York, NY, USA, 1960. [Google Scholar]




| Metrics | Descriptions |
|---|---|
| Overall score | The performance is evaluated by experts based on the entire procedure. |
| Trial time | Time used to complete an ETI procedure. The shorter the better. |
| Duration of glottis visibility | The duration of glottis being in the line of sight of the laryngoscope. The longer the better. |
| Force | The force exerted by the laryngoscope on the upper gum. The smaller the better. |
| Penetration depth | The penetration depth of the laryngoscope into the tongue plane. It has to be the right amount to view glottis, but not too deep to damage the tongue. |
| Pitch peaks | The pitch angle peaks of the laryngoscope to measure the smoothness of motion. |
| Yaw peaks | The yaw angle peaks of the laryngoscope to measure the smoothness of motion. |
| Test | 0-Back | 1-Back | 2-Back | Overall |
|---|---|---|---|---|
| Expert score | ||||
| Novice score | ||||
| t-value | ||||
| F-value | = 40.32 | |||
| p-value |
| Test | 1-Back | 2-Back | Overall |
|---|---|---|---|
| Expert engagement | |||
| Novice engagement | |||
| Engagement t-value | |||
| Engagement F-value | |||
| Engagement p-value | |||
| Expert accuracy | |||
| Novice accuracy | |||
| Accuracy t-value | |||
| Accuracy F-value | |||
| Accuracy p-value |
| Feature | 0 vs. 1-Back (p) | 0 vs. 2-Back (p) | 1 vs. 2-Back (p) | (p) |
|---|---|---|---|---|
| Overall Score | ||||
| Trial time | ||||
| Glottis view | ||||
| Force | ||||
| Depth | ||||
| Pitch Peaks | ||||
| Yaw peaks |
| Feature | 0 vs. 1-Back (p) | 0 vs. 2-Back (p) | 1 vs. 2-Back (p) | (p) |
|---|---|---|---|---|
| Overall Score | ||||
| Trial time | ||||
| Glottis view | ||||
| Force | ||||
| Depth | ||||
| Pitch Peaks | ||||
| Yaw peaks |
| Feature | Trial 5 vs. 1 (p) | Trial 11 vs. 1 (p) | Trial 15 vs. 1 (p) | (p) |
|---|---|---|---|---|
| Overall Score | ||||
| Trial time | ||||
| Glottis view | ||||
| Force | ||||
| Depth | ||||
| Pitch Peaks | ||||
| Yaw peaks |
| Feature | Trial 5 vs. 1 (p) | Trial 11 vs. 1 (p) | Trial 15 vs. 1 (p) | (p) |
|---|---|---|---|---|
| Overall Score | ||||
| Trial time | ||||
| Glottis view | ||||
| Force | ||||
| Depth | ||||
| Pitch Peaks | ||||
| Yaw peaks |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meng, Y.; Zhao, S.; Zhang, X.; Philbeck, J.; Mahableshwarkar, P.; Feng, B.; Soghier, L.; Hahn, J. Effect of Cognitive Distractors on Neonatal Endotracheal Intubation Performance: Insights from a Dual-Task Simulator. Virtual Worlds 2025, 4, 20. https://doi.org/10.3390/virtualworlds4020020
Meng Y, Zhao S, Zhang X, Philbeck J, Mahableshwarkar P, Feng B, Soghier L, Hahn J. Effect of Cognitive Distractors on Neonatal Endotracheal Intubation Performance: Insights from a Dual-Task Simulator. Virtual Worlds. 2025; 4(2):20. https://doi.org/10.3390/virtualworlds4020020
Chicago/Turabian StyleMeng, Yan, Shang Zhao, Xiaoke Zhang, John Philbeck, Prachi Mahableshwarkar, Boyuan Feng, Lamia Soghier, and James Hahn. 2025. "Effect of Cognitive Distractors on Neonatal Endotracheal Intubation Performance: Insights from a Dual-Task Simulator" Virtual Worlds 4, no. 2: 20. https://doi.org/10.3390/virtualworlds4020020
APA StyleMeng, Y., Zhao, S., Zhang, X., Philbeck, J., Mahableshwarkar, P., Feng, B., Soghier, L., & Hahn, J. (2025). Effect of Cognitive Distractors on Neonatal Endotracheal Intubation Performance: Insights from a Dual-Task Simulator. Virtual Worlds, 4(2), 20. https://doi.org/10.3390/virtualworlds4020020





