Anatomical Considerations for the Use of the Popliteal Vein as a Potential Alternative for Central Venous Cannulation
Abstract
1. Introduction
2. Methods
2.1. Donor Population and Ethical Approval
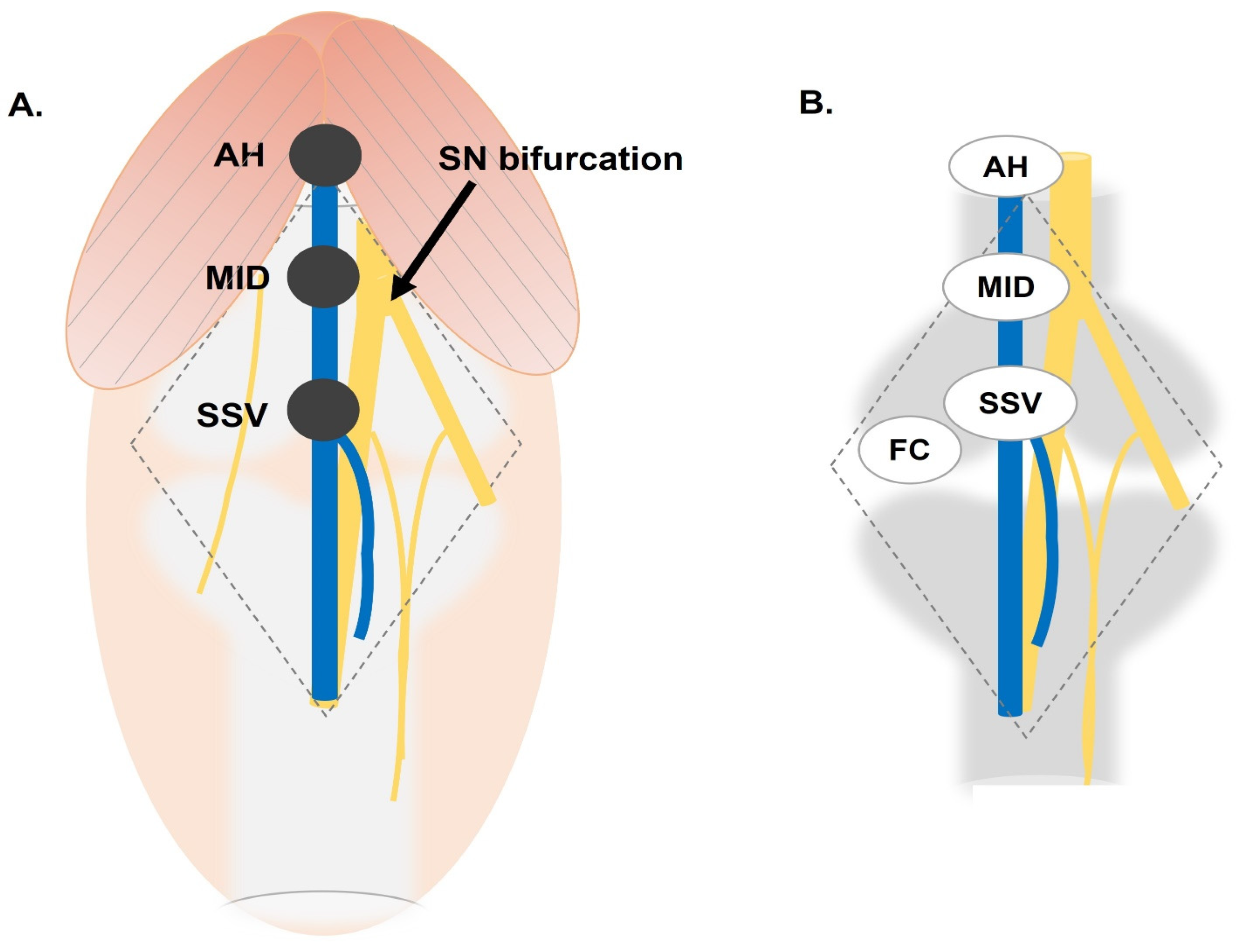
2.2. Dissection and Measurement of the Popliteal Vein
2.3. Statistical Analysis
3. Results
3.1. Descriptive Statistics of the Popliteal Vein
3.2. Laterality-Based Univariate Analysis
3.3. Sex-Based Univariate Analysis
3.4. Multivariate Analysis of Anatomical Sex and Laterality
4. Discussion
4.1. Evaluating the PV for Cannulation
4.2. Clinical Application of Popliteal Vein Cannulation
4.3. Contraindications of Popliteal Vein Cannulation
4.4. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Preventing Complications of Central Venous Catheterization|NEJM. Available online: https://www.nejm.org/doi/10.1056/NEJMra011883?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200www.ncbi.nlm.nih.gov (accessed on 26 March 2024).
- Fahy, B.; Sockrider, M. Central Venous Catheter. Am. J. Respir. Crit. Care Med. 2019, 199, P21–P22. [Google Scholar] [CrossRef] [PubMed]
- Cannulation of the Popliteal Vein as an Intraoperative Emergency Access in Prone Position: A Case Report—Tobias Kammerer, Tobias Brezina. 2022. Available online: https://journals.sagepub.com/doi/abs/10.1177/11297298211008091 (accessed on 26 March 2024).
- Yang, M.X.; Ng, P.K. Central Venous Catheter Insertion in the Prone Position-A Last Resort in Critically Ill COVID-19 Patients. J. Intensive Care Med. 2021, 36, 373–375. [Google Scholar] [CrossRef]
- Rabi Andaloussi, M.; Touab, R.; Samali, E.M.; Balkhi, H. The larger the better: Tourniquet-facilitated popliteal vein cannulation for vascular access in prone position. Anaesth. Crit. Care Pain. Med. 2021, 40, 100913. [Google Scholar] [CrossRef]
- Hadaya, J.; Benharash, P. Prone Positioning for Acute Respiratory Distress Syndrome (ARDS). JAMA 2020, 324, 1361. [Google Scholar] [CrossRef] [PubMed]
- Chua, E.X.; Zahir, S.M.I.S.M.; Ng, K.T.; Teoh, W.Y.; Hasan, M.S.; Ruslan, S.R.B.; Abosamak, M.F. Effect of prone versus supine position in COVID-19 patients: A systematic review and meta-analysis. J. Clin. Anesth. 2021, 74, 110406. [Google Scholar] [CrossRef]
- Guérin, C.; Albert, R.K.; Beitler, J.; Gattinoni, L.; Jaber, S.; Marini, J.J.; Munshi, L.; Papazian, L.; Pesenti, A.; Vieillard-Baron, A.; et al. Prone position in ARDS patients: Why, when, how and for whom. Intensive Care Med. 2020, 46, 2385–2396. [Google Scholar] [CrossRef]
- Parhar, K.K.S.; Zuege, D.J.; Shariff, K.; Knight, G.; Bagshaw, S.M. Prone positioning for ARDS patients-tips for preparation and use during the COVID-19 pandemic. Can. J. Anaesth. 2021, 68, 541–545. [Google Scholar] [CrossRef] [PubMed]
- Chua, E.X.; Wong, Z.Z.; Hasan, M.S.; Atan, R.; Yunos, N.A.M.; Yip, H.W.; Teoh, W.Y.; Ramli, M.A.S.; Ng, K.T. Prone ventilation in intubated COVID-19 patients: A systematic review and meta-analysis. Braz. J. Anesthesiol. 2022, 72, 780–789. [Google Scholar] [CrossRef]
- Kharat, A.; Simon, M.; Guérin, C. Prone position in COVID 19-associated acute respiratory failure. Curr. Opin. Crit. Care 2022, 28, 57–65. [Google Scholar] [CrossRef]
- Langer, T.; Brioni, M.; Guzzardella, A.; Carlesso, E.; Cabrini, L.; Castelli, G.; Dalla Corte, F.; De Robertis, E.; Favarato, M.; Forastieri, A.; et al. Prone position in intubated, mechanically ventilated patients with COVID-19: A multi-centric study of more than 1000 patients. Crit. Care 2021, 25, 128. [Google Scholar] [CrossRef]
- Ehrmann, S.; Li, J.; Ibarra-Estrada, M.; Perez, Y.; Pavlov, I.; McNicholas, B.; Roca, O.; Mirza, S.; Vines, D.; Garcia-Salcido, R.; et al. Awake prone positioning for COVID-19 acute hypoxaemic respiratory failure: A randomised, controlled, multinational, open-label meta-trial. Lancet Respir. Med. 2021, 9, 1387–1395. [Google Scholar] [CrossRef] [PubMed]
- Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: A prospective cohort study. Intensive Care Med. 2021, 47, 60–73. [CrossRef]
- Andrea, R.; Garcia-Alvarez, A.; Miró, J.; Poch Lopez de Briñas, E.J.; Martinez-Pastor, J.C.; Martinez-Palli, G.; Torres, A.; Guasch Casany, E.; Soy, D.; Urra, X.; et al. Clinical features, ventilatory management, and outcome of ARDS caused by COVID-19 are similar to other causes of ARDS. Intensive Care Med. 2020, 46, 2200–2211. [Google Scholar] [CrossRef]
- Guerin, C.; Beuret, P.; Constantin, J.M.; Bellani, G.; Garcia-Olivares, P.; Roca, O.; Meertens, J.H.; Maia, P.A.; Becher, T.; Peterson, J.; et al. A prospective international observational prevalence study on prone positioning of ARDS patients: The APRONET (ARDS Prone Position Network) study. Intensive Care Med. 2018, 44, 22–37. [Google Scholar] [CrossRef]
- Bellani, G.; Laffey, J.G.; Pham, T.; Fan, E.; Brochard, L.; Esteban, A.; Gattinoni, L.; Van Haren, F.; Larsson, A.; McAuley, D.F.; et al. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 2016, 315, 788–800. [Google Scholar] [CrossRef] [PubMed]
- Koksoy, C.; Cetinkaya, O.A. Popliteal Access in the Supine Position for Endovenous Management of Deep Vein Thrombosis. EJVES Short Rep. 2019, 46, 5–8. [Google Scholar] [CrossRef]
- Hale, D.F.; Cannon, J.W.; Batchinsky, A.I.; Cancio, L.C.; Aden, J.K.; White, C.E.; Renz, E.M.; Blackbourne, L.H.; Chung, K.K. Prone positioning improves oxygenation in adult burn patients with severe acute respiratory distress syndrome. J. Trauma Acute Care Surg. 2012, 72, 1634–1639. [Google Scholar] [CrossRef] [PubMed]
- Oto, B.; Orosco, R.I.; Panter, E.; Velamuri, R.; Kar, A.R.; Caffrey, J. Prone Positioning of the Burn Patient With Acute Respiratory Distress Syndrome: A Review of the Evidence and Practical Considerations. J. Burn. Care Res. 2018, 39, 471–475. [Google Scholar] [CrossRef]
- Voggenreiter, G.; Neudeck, F.; Aufmkolk, M.; Fabinder, J.; Hirche, H.; Obertacke, U.; Schmit-Neuerburg, K.P. Intermittent prone positioning in the treatment of severe and moderate posttraumatic lung injury. Crit. Care Med. 1999, 27, 2375–2382. [Google Scholar] [CrossRef]
- Shi, L.; Chen, Q.; Yang, R.; Liao, L.; Zhang, J.; Liu, Y. Challenges of PICC placement via the popliteal vein under ultrasound guidance in a patient with severe burns: A case report. J. Vasc. Access, 2024; 11297298241245066, epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Balakrishnan, N.; Beaini, H.; Carter, S.; Araj, F.G. Bedside popliteal vein cannulation for simultaneous plasmapheresis and renal replacement therapy in the prone position. J. Invasive Cardiol. 2024, 3. [Google Scholar] [CrossRef] [PubMed]
- Hamed, M.O.; Abdelmagid, M.; Ahmed, M. Popliteal venous access for renal replacement therapy in a critically ill patient with central access failure. BMJ Case Rep. 2024, 17, e258796. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.T.; Kim, H.S.; Lim, Y.J.; Bahk, J.H.; Lee, K.H.; Kim, C.S.; Kim, S.D.; Jeon, Y. The influence of passive leg elevation on the cross-sectional area of the internal jugular vein and the subclavian vein in awake adults. Anaesth. Intensive Care 2008, 36, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Clenaghan, S.; McLaughlin, R.E.; Martyn, C.; McGovern, S.; Bowra, J. Relationship between Trendelenburg tilt and internal jugular vein diameter. Emerg. Med. J. 2005, 22, 867–868. [Google Scholar] [CrossRef] [PubMed]
- Xie, S.; Yu, Q.; Li, T.; Xu, M.; Wu, J.; Li, Y. Comparison of the effect of different degrees of passive leg raising on the internal jugular vein cross-sectional area in patients before thoracic surgery. BMC Anesthesiol. 2019, 19, 78. [Google Scholar] [CrossRef]
- Sharp, R.; Cummings, M.; Childs, J.; Fielder, A.; Mikocka-Walus, A.; Grech, C.; Esterman, A. Measurement of Vein Diameter for Peripherally Inserted Central Catheter (PICC) Insertion: An Observational Study. J. Infus. Nurs. 2015, 38, 351–357. [Google Scholar] [CrossRef]
- Lake-Bakaar, G.; Ahmed, M.; Evenson, A.; Bonder, A.; Faintuch, S.; Sundaram, V. Hagen-Poiseuille’s law: The link between cirrhosis, liver stiffness, portal hypertension and hepatic decompensation. World J. Hepatol. 2015, 7, 28–32. [Google Scholar] [CrossRef]
- Berman, D.J.; Schiavi, A.; Frank, S.M.; Duarte, S.; Schwengel, D.A.; Miller, C.R. Factors that influence flow through intravascular catheters: The clinical relevance of Poiseuille’s law. Transfusion 2020, 60, 1410–1417. [Google Scholar] [CrossRef]
- Jayanthi, N.V.G.; Dabke, H.V. The effect of IV cannula length on the rate of infusion. Injury 2006, 37, 41–45. [Google Scholar] [CrossRef]
- Ilonzo, N.; Rao, A.; Soundararajan, K.; Vouyouka, A.; Han, D.; Tadros, R.; Kim, S.Y.; Love, B.; Ting, W.; Marin, M.; et al. The importance of a centralized line service during the COVID-19 pandemic. J. Vasc. Surg. 2020, 72, 403–404. [Google Scholar] [CrossRef]
- Verhoeff, K.; Saybel, R.; Mathura, P.; Tsang, B.; Fawcett, V.; Widder, S. Ensuring adequate vascular access in patients with major trauma: A quality improvement initiative. BMJ Open Qual. 2018, 7, e000090. [Google Scholar] [CrossRef]
- Citla Sridhar, D.; Abou-Ismail, M.Y.; Ahuja, S.P. Central venous catheter-related thrombosis in children and adults. Thromb. Res. 2020, 187, 103–112. [Google Scholar] [CrossRef]
- Gunawansa, N.; Sudusinghe, D.H.; Wijayaratne, D.R. Hemodialysis Catheter-Related Central Venous Thrombosis: Clinical Approach to Evaluation and Management. Ann. Vasc. Surg. 2018, 51, 298–305. [Google Scholar] [CrossRef]
- Verso, M.; Agnelli, G. Venous thromboembolism associated with long-term use of central venous catheters in cancer patients. J. Clin. Oncol. 2003, 21, 3665–3675. [Google Scholar] [CrossRef]
- Kamphuisen, P.W.; Lee, A.Y.Y. Catheter-related thrombosis: Lifeline or a pain in the neck? Hematol. Am. Soc. Hematol. Educ. Program 2012, 2012, 638–644. [Google Scholar] [CrossRef]
- Parienti, J.J.; Mongardon, N.; Mégarbane, B.; Mira, J.P.; Kalfon, P.; Gros, A.; Marqué, S.; Thuong, M.; Pottier, V.; Ramakers, M.; et al. Intravascular Complications of Central Venous Catheterization by Insertion Site. N. Engl. J. Med. 2015, 373, 1220–1229. [Google Scholar] [CrossRef] [PubMed]
- Wall, C.; Moore, J.; Thachil, J. Catheter-related thrombosis: A practical approach. J. Intensive Care Soc. 2016, 17, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Gahlot, R.; Nigam, C.; Kumar, V.; Yadav, G.; Anupurba, S. Catheter-related bloodstream infections. Int. J. Crit. Illn. Inj. Sci. 2014, 4, 162–167. [Google Scholar] [CrossRef]
- The Risk of Bloodstream Infection in Adults with Different Intravascular Devices: A Systematic Review of 200 Published Prospective Studies. Available online: https://pubmed.ncbi.nlm.nih.gov/16970212/ (accessed on 26 March 2024).
- Soufir, L.; Timsit, J.F.; Mahe, C.; Carlet, J.; Regnier, B.; Chevret, S. Attributable morbidity and mortality of catheter-related septicemia in critically ill patients: A matched, risk-adjusted, cohort study. Infect. Control Hosp. Epidemiol. 1999, 20, 396–401. [Google Scholar] [CrossRef] [PubMed]
- The Risk of Catheter-Related Bloodstream Infection with Femoral Venous Catheters as Compared to Subclavian and Internal Jugular Venous Catheters: A Systematic Review of the Literature and Meta-Analysis. Available online: https://pubmed.ncbi.nlm.nih.gov/22809915/ (accessed on 26 March 2024).
- Woo, K.; Rigberg, D.; Lawrence, P.F. Safe Central Venous Access in an Overburdened Health System. JAMA 2021, 325, 299–300. [Google Scholar] [CrossRef]


| Landmark | Measurement | Mean (SD) (95% CI) |
|---|---|---|
| AH | Diameter | 7.69 (1.37) (7.27–8.11) |
| MID | 7.69 (1.73) (7.17–8.21) | |
| SSV | 7.28 (1.76) (6.75–7.81) | |
| AH-SSV | Length | 115.20 (35.39) (104.59–125.86) |
| AH-FCs | 145.99 (16.99) (140.83–151.15) | |
| MID-SSV | 57.61 (17.70) (52.30–62.93) | |
| SSV-FC | 32.41 (30.61) (23.21–41.60) |
| Landmark | Measurement | Left (SD) (95% CI) | Right (SD) (95% CI) | Test | p Value |
|---|---|---|---|---|---|
| AH | Diameter | 7.56 (1.35) (6.96–8.16) | 7.83 (1.40) (7.19–8.47) | Student’s t | 0.53 |
| MID | 7.59 (1.73) (6.82–8.35) | 7.79 (1.76) (7.03–8.56) | Student’s t | 0.69 | |
| SSV | 7.27 (1.82) (6.46–8.07) | 7.30 (1.74) (6.55–8.05) | Student’s t | 0.95 | |
| AH-SSV | Length | 120.84 (32.80) (106.30–135.38) | 109.85 (37.64) (93.58–126.13) | Student’s t | 0.30 |
| AH-FCs | 146.56 (18.80) (138.22–154.89) | 145.45 (15.88) (138.58–152.32) | Student’s t | 0.83 | |
| MID-SSV | 60.42 (16.40) (53.15–67.69) | 54.93 (18.82) (46.79–63.06) | Student’s t | 0.30 | |
| SSV-FCs | 28.10 (21.40) (18.62–37.59) | 36.52 (37.42) (20.34–52.70) | Mann–Whitney U | 0.56 |
| Landmark | Measurement | Males (SD) (95% CI) | Females (SD) (95% CI) | Test | p Value |
|---|---|---|---|---|---|
| AH | Diameter | 8.16 (1.33) (7.65–8.66) | 6.73 (0.87) (6.23–7.23) | Student’s t | <0.05 |
| MID | 8.28 (1.60) (7.67–8.88) | 6.64 (1.46) (5.86–7.42) | Student’s t | <0.05 | |
| SSV | 7.94 (1.73) (7.29–8.60) | 6.09 (1.07) (5.52–6.65) | MWU | <0.05 | |
| AH-SSV | Length | 107.91 (40.84) (92.38–123.45) | 128.48 (16.45) (119.71–137.24) | MWU | 0.11 |
| AH-FCs | 142.33 (18.10) (135.45–149.22) | 152.61 (13.47) (145.43–159.79) | Student’s t | 0.05 | |
| MID-SSV | 53.96 (20.42) (46.19–61.72) | 64.24 (8.22) (59.86–68.62) | MWU | 0.11 | |
| SSV-FC | 36.02 (36.79) (22.02–50.01) | 25.86 (12.25) (19.33–32.39) | MWU | 0.72 |
| ANOVA | |||||||
|---|---|---|---|---|---|---|---|
| Laterality vs. Sex | Mean Difference | SE | df | t | p | ||
| Diameter of PV at AH | Male Left | Male Right | −0.167 | 0.458 | 39.0 | −0.364 | 0.718 |
| Female Left | 1.403 | 0.546 | 39.0 | 2.571 | 0.014 | ||
| Female Right | 1.258 | 0.601 | 39.0 | 2.094 | 0.043 | ||
| Male Right | Female Left | 1.569 | 0.539 | 39.0 | 2.911 | 0.006 | |
| Female Right | 1.425 | 0.595 | 39.0 | 2.396 | 0.021 | ||
| Female Left | Female Right | −0.145 | 0.665 | 39.0 | −0.217 | 0.829 | |
| Diameter at MID | Male Left | Male Right | −0.0520 | 0.588 | 41.0 | −0.0885 | 0.930 |
| Female Left | 1.8205 | 0.701 | 41.0 | 2.5957 | 0.012 | ||
| Female Right | 1.4043 | 0.701 | 41.0 | 2.0022 | 0.052 | ||
| Male Right | Female Left | 1.8726 | 0.693 | 41.0 | 2.7029 | 0.010 | |
| Female Right | 1.4563 | 0.693 | 41.0 | 2.1021 | 0.042 | ||
| Female Left | Female Right | −0.4163 | 0.791 | 41.0 | −0.5261 | 0.602 | |
| Diameter of PV at SSV | Male Left | Male Right | 0.104 | 0.581 | 41.0 | 0.178 | 0.859 |
| Female Left | 2.009 | 0.693 | 41.0 | 2.899 | 0.006 | ||
| Female Right | 1.808 | 0.693 | 41.0 | 2.609 | 0.013 | ||
| Male Right | Female Left | 1.906 | 0.685 | 41.0 | 2.783 | 0.008 | |
| Female Right | 1.704 | 0.685 | 41.0 | 2.489 | 0.017 | ||
| Female Left | Female Right | −0.201 | 0.782 | 41.0 | −0.257 | 0.798 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Graves, A.L.; Marchese, C.R.; Creamer, B.A.; Dennis, J.F. Anatomical Considerations for the Use of the Popliteal Vein as a Potential Alternative for Central Venous Cannulation. Anatomia 2024, 3, 192-201. https://doi.org/10.3390/anatomia3030015
Graves AL, Marchese CR, Creamer BA, Dennis JF. Anatomical Considerations for the Use of the Popliteal Vein as a Potential Alternative for Central Venous Cannulation. Anatomia. 2024; 3(3):192-201. https://doi.org/10.3390/anatomia3030015
Chicago/Turabian StyleGraves, Aaron L., Charles R. Marchese, Bradley A. Creamer, and Jennifer F. Dennis. 2024. "Anatomical Considerations for the Use of the Popliteal Vein as a Potential Alternative for Central Venous Cannulation" Anatomia 3, no. 3: 192-201. https://doi.org/10.3390/anatomia3030015
APA StyleGraves, A. L., Marchese, C. R., Creamer, B. A., & Dennis, J. F. (2024). Anatomical Considerations for the Use of the Popliteal Vein as a Potential Alternative for Central Venous Cannulation. Anatomia, 3(3), 192-201. https://doi.org/10.3390/anatomia3030015







