Beaton and Anson Type A Classification of the Sciatic Nerve and Piriformis Complex: Clinical Considerations for Sex and Laterality
Abstract
1. Introduction
2. Material and Methods
2.1. Dissection of Cadaveric Donors
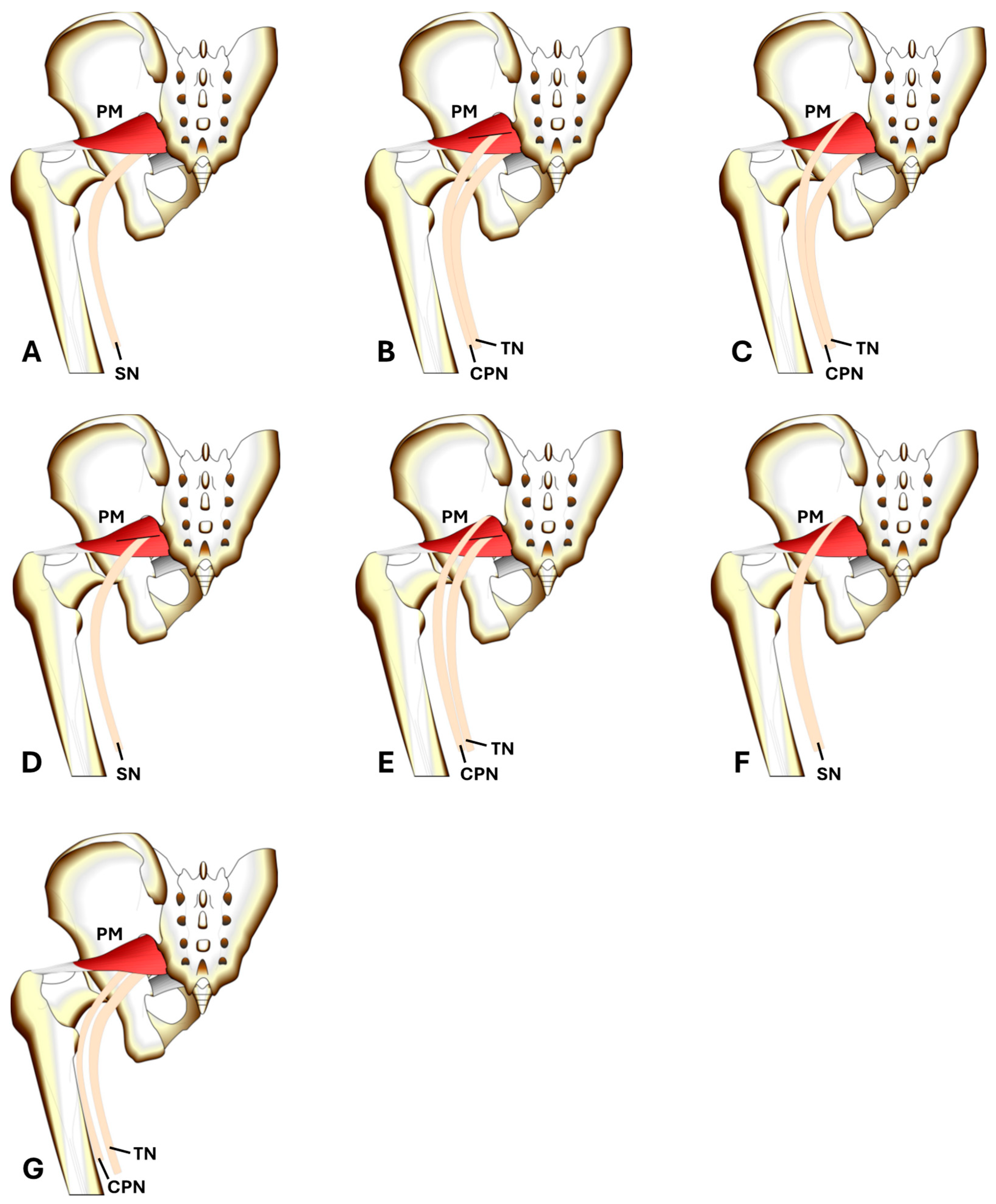
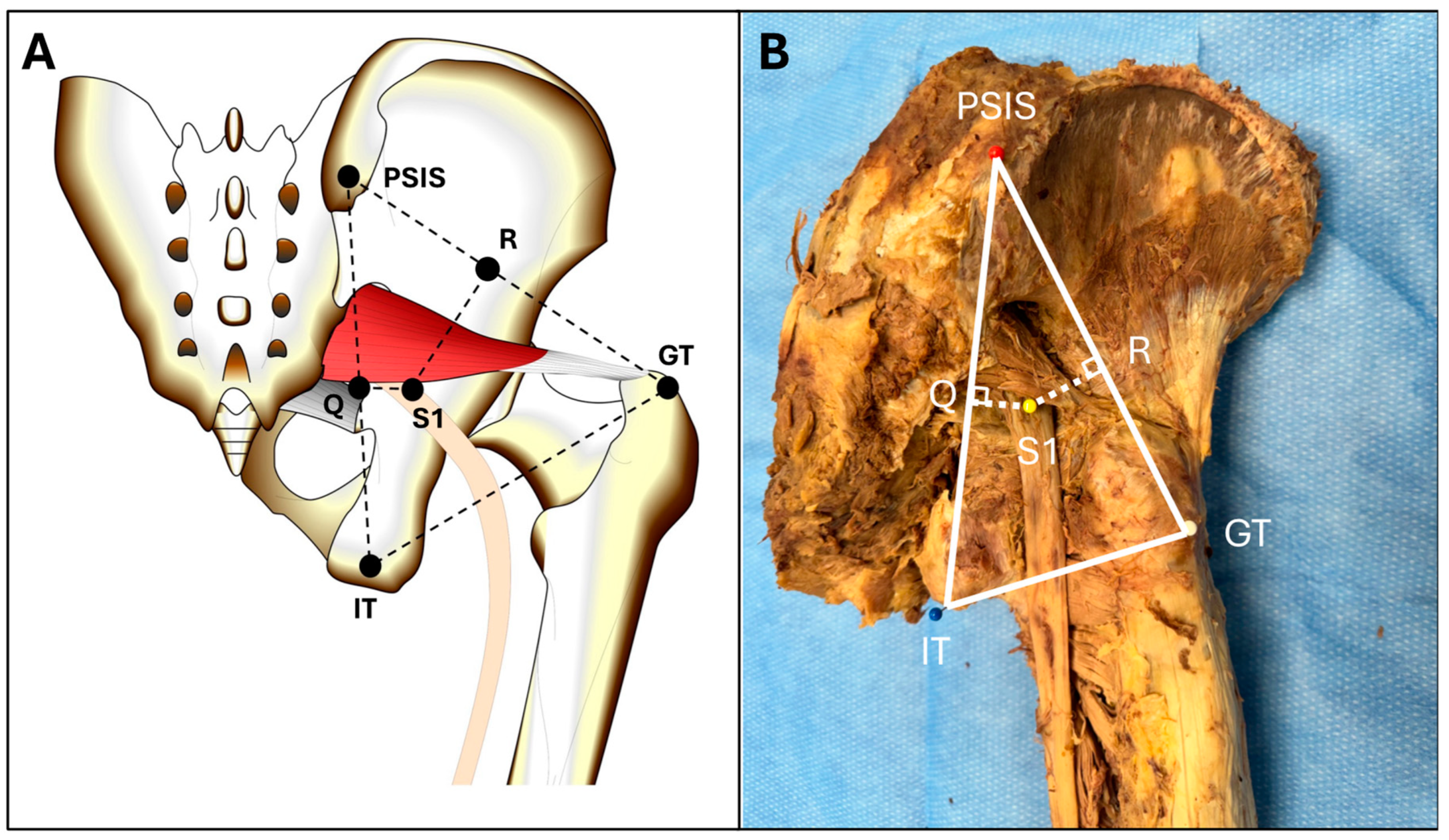
2.2. Evaluation of the Sciatic Nerve–Piriformis Relationship
2.3. Statistical Analysis
3. Results
3.1. Beaton and Anson Classification of Donors
3.2. Laterality Based Comparison of the SN-PM Region
3.3. Sex-Based Comparison of the SN-PM Region
4. Discussion
Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Berihu, B.A.; Debeb, Y.G. Anatomical variation in bifurcation and trifurcations of sciatic nerve and its clinical implications: In selected university in Ethiopia. BMC Res. Notes 2015, 8, 633. [Google Scholar] [CrossRef]
- Poutoglidou, F.; Piagkou, M.; Totlis, T.; Tzika, M.; Natsis, K. Sciatic Nerve Variants and the Piriformis Muscle: A Systematic Review and Meta-Analysis. Cureus 2020, 12, e11531. [Google Scholar] [CrossRef] [PubMed]
- Beaton, L.E.; Anson, B.J. The relation of the sciatic nerve and of its subdivisions to the piriformis muscle. Anat. Rec. 1937, 70, 1–5. [Google Scholar] [CrossRef]
- Wan-Ae-Loh, P.; Huanmanop, T.; Agthong, S.; Chentanez, V. Evaluation of the sciatic nerve location regarding its relationship to the piriformis muscle. Folia Morphol. 2020, 79, 681–689. [Google Scholar] [CrossRef]
- Jha, A.K.; Baral, P. Composite Anatomical Variations between the Sciatic Nerve and the Piriformis Muscle: A Nepalese Cadaveric Study. Case Rep. Neurol. Med. 2020, 2020, 7165818. [Google Scholar] [CrossRef] [PubMed]
- Han, S.K.; Kim, Y.S.; Kim, T.H.; Kang, S.H. Surgical Treatment of Piriformis Syndrome. Clin. Orthop. Surg. 2017, 9, 136. [Google Scholar] [CrossRef]
- Pećina, M. Contribution to the etiological explanation of the piriformis syndrome. Acta Anat. 1979, 105, 181–187. [Google Scholar] [PubMed]
- Fishman, L.M.; Dombi, G.W.; Michaelsen, C.; Ringel, S.; Rozbruch, J.; Rosner, B.; Weber, C. Piriformis syndrome: Diagnosis, treatment, and outcome—A 10-year study. Arch. Phys. Med. Rehabil. 2002, 83, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Benzon, H.T.; Katz, J.A.; Benzon, H.A.; Iqbal, M.S. Piriformis Syndrome: Anatomic Considerations, a New Injection Technique, and a Review of the Literature. Anesthesiology 2003, 98, 1442–1448. [Google Scholar] [CrossRef]
- Moretti, V.M.; Post, Z.D. Surgical Approaches for Total Hip Arthroplasty. Indian J. Orthop. 2017, 51, 368–376. [Google Scholar] [CrossRef]
- Navarro, R.A.; Schmalzried, T.P.; Amstutz, H.C.; Dorey, F.J. Surgical approach and nerve palsy in total hip arthroplasty. J. Arthroplast. 1995, 10, 1–5. [Google Scholar] [CrossRef]
- Kim, H.J.; Park, S.H. Sciatic nerve injection injury. J. Int. Med. Res. 2014, 42, 887–897. [Google Scholar] [CrossRef]
- Kline, D.G.; Kim, D.; Midha, R.; Harsh, C.; Tiel, R. Management and results of sciatic nerve injuries: A 24-year experience. J. Neurosurg. 1998, 89, 13–23. [Google Scholar] [CrossRef]
- Güvençer, M.; Akyer, P.; Iyem, C.; Tetik, S.; Naderi, S. Anatomic considerations and the relationship between the piriformis muscle and the sciatic nerve. Surg. Radiol. Anat. 2008, 30, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Haładaj, R.; Pingot, M.; Polguj, M.; Wysiadecki, G.; Topol, M. Anthropometric Study of the Piriformis Muscle and Sciatic Nerve: A Morphological Analysis in a Polish Population. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2015, 21, 3760–3768. [Google Scholar] [CrossRef]
- Tomaszewski, K.A.; Graves, M.J.; Henry, B.M.; Popieluszko, P.; Roy, J.; Pękala, P.A.; Hsieh, W.C.; Vikse, J.; Walocha, J.A. Surgical anatomy of the sciatic nerve: A meta-analysis. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2016, 34, 1820–1827. [Google Scholar] [CrossRef]
- Gänsslen, A.; Grechenig, S.; Nerlich, M.; Müller, M. Standard Approaches to the Acetabulum Part 1: Kocher-Langenbeck Approach. Acta Chir. Orthop. Traumatol. Cech. 2016, 83, 141–146. [Google Scholar]
- Goldsmith, A.J.; Liteplo, A.; Hayes, B.D.; Duggan, N.; Huang, C.; Shokoohi, H. Ultrasound-guided transgluteal sciatic nerve analgesia for refractory back pain in the ED. Am. J. Emerg. Med. 2020, 38, 1792–1795. [Google Scholar] [CrossRef]
- Selame, L.A.; McFadden, K.; Duggan, N.M.; Goldsmith, A.J.; Shokoohi, H. Ultrasound-Guided Transgluteal Sciatic Nerve Block for Gluteal Procedural Analgesia. J. Emerg. Med. 2021, 60, 512–516. [Google Scholar] [CrossRef] [PubMed]
- Okutomi, Y.; Konishi, Y.; Kakinuma, A.; Sawamura, S. Preoperative Femoral Nerve Block and Postoperative Sciatic Nerve Block at the Subgluteal Space after Total Knee Arthroplasty: A Retrospective Cohort Study. Cureus 2023, 15, e50882. [Google Scholar] [CrossRef]
- Wiederhold, B.D.; Garmon, E.H.; Peterson, E.; Stevens, J.B.; O’Rourke, M.C. Nerve Block Anesthesia. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: http://www.ncbi.nlm.nih.gov/books/NBK431109/ (accessed on 7 May 2024).
- Teo, I.; Thompson, J.; Neo, Y.N.; Lundie, S.; Munnoch, D.A. Lower limb dominance and volume in healthy individuals. Lymphology 2017, 50, 197–202. [Google Scholar] [PubMed]
- Neogi, T.; Zhang, Y. Epidemiology of OA. Rheum. Dis. Clin. N. Am. 2013, 39, 1–19. [Google Scholar] [CrossRef]
- Stavrakis, A.I.; SooHoo, N.F.; Lieberman, J.R. Bilateral Total Hip Arthroplasty has Similar Complication Rates to Unilateral Total Hip Arthroplasty. J. Arthroplast. 2015, 30, 1211–1214. [Google Scholar] [CrossRef]
- Fu, M.; Zhou, H.; Li, Y.; Jin, H.; Liu, X. Global, regional, and national burdens of hip osteoarthritis from 1990 to 2019: Estimates from the 2019 Global Burden of Disease Study. Arthritis Res. Ther. 2022, 24, 8. [Google Scholar] [CrossRef] [PubMed]
- Bal, B.S.; Vallurupalli, S. Minimally invasive total hip arthroplasty with the anterior approach. Indian J. Orthop. 2008, 42, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Prakash, S.; Rai, A.; Manhas, V.; Malhotra, R. Sciatic nerve palsy after direct anterior approach for total hip replacement. BMJ Case Rep. 2023, 16, e252818. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.Y.; Sharma, I.; Sabbagh, R.S.; Narendran, N.B.; Everhart, J.S.; Slaven, J.E.; Archdeacon, M.T.; Sagi, H.C.; Mullis, B.H.; Natoli, R.M. Risk of Postoperative Sciatic Nerve Palsy after Posterior Acetabular Fracture Fixation: Does Patient Position Matter? J. Orthop. Trauma. 2023, 37, 64. [Google Scholar] [CrossRef]
- Stone, A.V.; Howse, E.A.; Mannava, S.; Miller, B.A.; Botros, D.; Stubbs, A.J. Basic Hip Arthroscopy: Diagnostic Hip Arthroscopy. Arthrosc. Tech. 2017, 6, e699–e704. [Google Scholar] [CrossRef]
- Martin, S. Portal Placement for Hip Arthroscopy. J. Med. Insight 2024, 30. [Google Scholar] [CrossRef]
- Kern, M.J.; Murray, R.S.; Sherman, T.I.; Postma, W.F. Incidence of Nerve Injury after Hip Arthroscopy. J. Am. Acad. Orthop. Surg. 2018, 26, 773. [Google Scholar] [CrossRef]
- Yektaş, A.; Balkan, B. Comparison of sciatic nerve block quality achieved using the anterior and posterior approaches: A randomised trial. BMC Anesthesiol. 2019, 19, 225. [Google Scholar] [CrossRef]
- Ota, J.; Sakura, S.; Hara, K.; Saito, Y. Ultrasound-Guided Anterior Approach to Sciatic Nerve Block: A Comparison with the Posterior Approach. Anesth. Analg. 2009, 108, 660. [Google Scholar] [CrossRef] [PubMed]
| B&A Classification | Prevalence | Total Limbs | Male Limbs | Female Limbs | Donor Symmetry * |
|---|---|---|---|---|---|
| A | 90.3% | 56 | 24 | 32 | 25/31 (AA) |
| B | 1.6% | 1 | 1 | 0 | 0/31 (BB) |
| C | 1.6% | 1 | 1 | 0 | 0/31 (CC) |
| D | 0 | 0 | 0 | 0 | 0/31 (DD) |
| E | 0 | 0 | 0 | 0 | 0/31 (EE) |
| F | 0 | 0 | 0 | 0 | 0/31 (FF) |
| G | 6.5% | 4 | 2 | 2 | 0/31 (GG) |
| Measurement | Left, Mean (SD) | Right, Mean (SD) | Two-Tailed p-Value |
|---|---|---|---|
| PSIS-IT | 174.79 (12.22) | 175.57 (10.59) | 0.81 |
| IT-GT | 104.62 (15.13) | 108.36 (12.74) | 0.35 |
| GT-PSIS | 176.23 (11.30) | 169.87 (12.54) | 0.07 |
| S1-PSIS | 89.90 (8.54) | 92.26 (7.63) | 0.32 |
| S1-IT | 88.49 (9.18) | 89.56 (7.61) | 0.66 |
| S1-GT | 97.78 (11.80) | 92.13 (12.27) | 0.11 |
| S1-R | 31.33 (8.55) | 33.66 (6.59) | 0.29 |
| S1-Q | 23.22 (5.89) | 24.26 (5.62) | 0.53 |
| Measurement | Combined, Mean (SD) | Male, Mean (SD) | Female, Mean (SD) | Two-Tailed p-Value | One-Tailed p-Value |
|---|---|---|---|---|---|
| PSIS-IT | 175.17 (11.34) | 183.86 (6.91) | 168.09 (9.10) | <0.01 | <0.01 |
| IT-GT | 106.45 (14.00) | 116.08 (10.36) | 98.60 (11.51) | <0.01 | <0.01 |
| GT-PSIS | 173.12 (12.23) | 180.80 (9.67) | 166.86 (10.48) | <0.01 | <0.01 |
| S1-PSIS | 91.06 (8.11) | 95.45 (8.31) | 87.47 (6.01) | <0.01 | <0.01 |
| S1-IT | 89.01 (8.38) | 94.54 (5.13) | 84.50 (7.83) | <0.01 | <0.01 |
| S1-GT | 95.01 (12.24) | 101.09 (10.28) | 90.07 (11.60) | <0.01 | <0.01 |
| S1-R | 32.47 (7.66) | 36.98 (6.41) | 28.79 (6.63) | <0.01 | <0.01 |
| S1-Q | 23.73 (5.72) | 25.36 (6.22) | 22.41 (5.01) | 0.07 | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marchese, C.R.; Graves, A.L.; Pautler, B.J.; Dye, D.; Creamer, B.A.; Dennis, J.F. Beaton and Anson Type A Classification of the Sciatic Nerve and Piriformis Complex: Clinical Considerations for Sex and Laterality. Anatomia 2024, 3, 182-191. https://doi.org/10.3390/anatomia3030014
Marchese CR, Graves AL, Pautler BJ, Dye D, Creamer BA, Dennis JF. Beaton and Anson Type A Classification of the Sciatic Nerve and Piriformis Complex: Clinical Considerations for Sex and Laterality. Anatomia. 2024; 3(3):182-191. https://doi.org/10.3390/anatomia3030014
Chicago/Turabian StyleMarchese, Charles R., Aaron L. Graves, Benjamin J. Pautler, David Dye, Bradley A. Creamer, and Jennifer F. Dennis. 2024. "Beaton and Anson Type A Classification of the Sciatic Nerve and Piriformis Complex: Clinical Considerations for Sex and Laterality" Anatomia 3, no. 3: 182-191. https://doi.org/10.3390/anatomia3030014
APA StyleMarchese, C. R., Graves, A. L., Pautler, B. J., Dye, D., Creamer, B. A., & Dennis, J. F. (2024). Beaton and Anson Type A Classification of the Sciatic Nerve and Piriformis Complex: Clinical Considerations for Sex and Laterality. Anatomia, 3(3), 182-191. https://doi.org/10.3390/anatomia3030014







