Abstract
Sensory processing sensitivity, characterized by deeper cognitive, sensory and emotional information processing, has been previously related to several mental health problems. However, the studies are rare, and an integration of the obtained findings needs to be addressed. We conducted a systematic review of studies using scientific databases in order to integrate the available information about sensory processing sensitivity and its consequences in mental health. Thirteen studies were included and analyzed in the review. According to these studies, high levels of sensory processing sensitivity might be related to the appearance of several mental health disturbances, such as anxiety or depression.
1. Introduction
Sensory processing sensitivity (SPS) has been described from a vast variety of studies as an underlying phenotypic trait characterized by the ability to register and process environmental stimuli and its association to deeper cognitive, sensory and emotional information processing, probably due to a more sensitive central nervous system [1,2].
According to the assumptions developed within the framework of the theory of environmental sensitivity [3], humans are programmed to perceive, process, and react in a certain way to environmental stimuli. This way of processing the environment’s stimuli has a necessary function for survival, since it allows adaptation to context [2]. However, despite the fact that there is a neurobiological predisposition for the development of this adaptive function in human beings, significant differences have been observed in the way in which individuals react to environmental stimuli. Hence, it has been identified that some people exhibit a greater sensitivity to environmental stimuli [3]. In this sense, different studies have identified how some individuals process the cognitive, sensory and emotional information of the environment in a more intense and profound way, which leads to a greater emotional reactivity, a greater awareness of environmental subtleties and a greater propensity to over-stimulation [2,4].
Thus, these individual differences that may be found in this sensitivity trait could have an impact on mental health, affecting children through to adulthood [5]. Previous studies in this sense have shown how a high environmental sensitivity trait is associated with greater difficulties in different areas of people lives, such as family, school and personal and social lives, having been related to a significant deterioration of health and quality of life of them [5]. In this sense, highly sensitive people may experience an increase in mental health problems, including mainly anxiety and depression. In fact, according to recent studies, about 40% of highly sensitive people present mental health problems [5,6]. Therefore, the objective of this study was to analyze the association between sensory processing sensitivity and mental health implications.
2. Methodology and Quality Assessment
A systematic review study that applied the recommendations in the Preferred Reporting Items for Systematic reviews and Meta-Analysis declaration for these types of studies was carried out [7].
2.1. Data Sources
A systematic search was carried out in the PubMed, ScienceDirect and Scopus databases, using the keywords “sensory processing sensitivity” and “mental health” as MeSH descriptor.
2.2. Search Strategy
The Boolean indicator AND was used (sensory processing sensitivity AND mental health). The search for documents was limited to publications that appeared in scientific journals and books from January 2015 to January 2021.
2.3. Selection of Articles
Abstracts identified through the bibliographic search were independently evaluated by two authors to confirm the inclusion criteria. The quality of each study was independently evaluated by two authors, using the Crombie criteria adapted by Petticrew and Roberts [8]. Disagreements were resolved by a third author.
2.4. Inclusion and Exclusion Criteria
Inclusion criteria were: (1) articles that were available in full text and written in English or Spanish; (2) articles in which sensory processing sensitivity was reported with numerical values; (3) articles in which mental health implications were reported with numerical values.
The exclusion criteria were: (1) articles not related to sensory processing sensitivity; (2) articles that do not present mental health implications related to sensory processing sensitivity; (3) documents that were summaries for conferences; (4) articles that were reviews or meta-analyses.
2.5. Extracted Data
Data extraction was carried out by the lead author of the review, taking into account the year of publication (2015–2021), design and objective of the study, sample size, participants’ mean age, country of origin and relationship between sensory processing sensitivity and mental health implications.
3. Results
In total, 767 studies were identified. After the duplicates were removed (n = 12), the titles and summaries were read, and the other 742 were deleted according to the different exclusion criteria. Finally, 13 articles were included in this review (Figure 1).
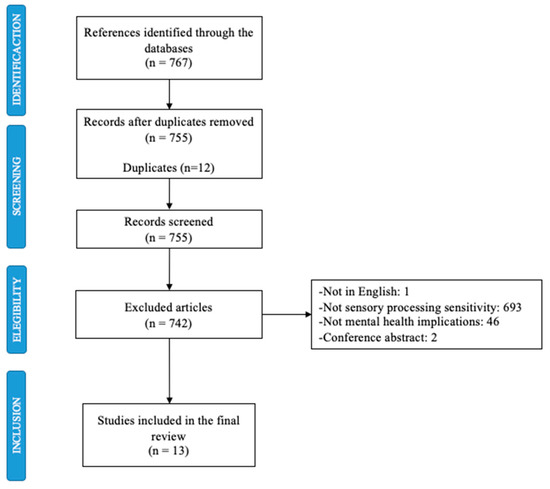
Figure 1.
Selection of the studies.
3.1. Description Data and Types of Studies
Table 1 shows the characteristics of the studies included. Of the participants, 54.57% were women and the remaining 45.43% were men, with a mean participant age of about 35.95 years.

Table 1.
Description of the studies included in the review.
As for the country of origin, three of the studies were conducted in Japan [10,12,17], two in the United States [9,15], and the other two in the United Kingdom [14,19]. One article was carried out in each of the following countries: Malaysia, Sweden, Denmark, Iran, Israel and China [11,13,16,18,20,21].
Table 1, which also presents the design of the studies, shows that 11 of the 13 of them were cross-sectional studies [10,11,12,13,14,15,17,18,19,20,21]. One was a cohort study [9] and another one was a longitudinal and seasonally counterbalanced study [16].
3.2. Relationship between SPS and Mental Health
Table 1 indicates the relationship between sensory processing sensitivity and mental health implications in each of the studies included. A positive association between SPS and mental health problems is observed in every study [9,10,11,12,13,14,15,16,17,18,19,20,21]. Specifically, five articles point out adaptative disorders (anxiety and depression) as a result of high levels of SPS [9,10,11,12,16,17]. Four of these studies indicate that high levels of SPS is related to stress [13,14,20,21]. Two of them mention the influence of SPS in obsessive thoughts and compulsive behaviors [15,18].
4. Conclusions
Sensory processing sensitivity seems to be a personality trait that facilitates the appearance of mental health problems, such as anxiety, depression, sleep disturbances or stress. More and more current studies are demonstrating the mental health consequences of presenting high levels of SPS. However, research on this issue should continue, since more knowledge of this trait is needed in order to understand its functioning and its health implications in order to create assessment and intervention protocols to improve the quality of life of the highly sensitive population.
Author Contributions
Conceptualization R.F.-C., N.R.-R., B.C.-L.; methodology, N.R.-R. and B.C.-L.; investigation, R.F.-C., N.R.-R. and B.C.-L.; resources, R.F.-C. and B.C.-L.; writing—original draft preparation, R.F.-C., N.R.-R. and B.C.-L.; writing—review and editing, N.A.-B. and M.S.-S.; supervision, R.F.-C., N.R.-R. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the European Commission (project no: 2018-1-PL01-KA201-051033).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Aron, E.N.; Aron, A. Sensory-processing sensitivity and its relation to introversion and emotionality. J. Pers. Soc. Psychol. 1997, 73, 345–368. [Google Scholar] [CrossRef] [PubMed]
- Greven, C.U.; Lionetti, F.; Booth, C.; Aron, E.N.; Fox, E.; Schendan, H.E.; Pluess, M.; Bruining, H.; Acevedo, B.; Bijttebier, P.; et al. Sensory Processing Sensitivity in the context of Environmental Sensitivity: A critical review and development of research agenda. Neurosci. Biobehav. Rev. 2019, 98, 287–305. [Google Scholar] [CrossRef] [PubMed]
- Pluess, M.; Assary, E.; Lionetti, F.; Lester, K.J.; Krapohl, E.; Aron, E.N.; Aron, A. Environmental sensitivity in children: Development of the Highly Sensitive Child Scale and identification of sensitivity groups. Dev. Psychol. 2018, 54, 51–70. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, A.; Scharf, M. How do highly sensitive persons parent their adolescent children? The role of sensory processing sensitivity in parenting practices. J. Soc. Pers. Relationships 2020, 37, 1825–1842. [Google Scholar] [CrossRef]
- Jagiellowicz, J.; Zarinafsar, S.; Acevedo, B.P. Health and social outcomes in highly sensitive persons. In The Highly Sensitive Brain; Elsevier BV: Amsterdam, The Netherlands, 2020; pp. 75–107. [Google Scholar]
- Acevedo, B.P. The basics of sensory processing sensitivity. In The Highly Sensitive Brain; Elsevier BV: Amsterdam, The Netherlands, 2020; pp. 1–15. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petticrew, M.; Roberts, H. Systematic Reviews in the Social Sciences: A Practical Guide; John Wiley & Sons: Hoboken, NJ, USA, 2006. [Google Scholar]
- Stern, B.; Strober, L.B.; Goverover, Y. Relationship between sensory processing patterns, trait anxiety, and health-related quality of life in multiple sclerosis. J. Health Psychol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Kibe, C.; Suzuki, M.; Hirano, M.; Boniwell, I. Sensory processing sensitivity and culturally modified resilience education: Dif-ferential susceptibility in Japanese adolescents. PLoS ONE 2020, 15, e0239002. [Google Scholar] [CrossRef] [PubMed]
- Khodabakhsh, S.; Loh, S.C.; Rosli, N.A. Relationship Between Neurological Threshold in Sensory Profile, Depression, and Anxiety among Adults. Pertanika J. Soc. Sci. Humanit. 2020, 28, 605–615. [Google Scholar]
- Yano, K.; Kase, T.; Oishi, K. The effects of sensory-processing sensitivity and sense of coherence on depressive symptoms in university students. Health Psychol. Open 2019, 6, 6. [Google Scholar] [CrossRef] [PubMed]
- Andersson, H.; Sutton, D.; Bejerholm, U.; Argentzell, E. Experiences of sensory input in daily occupations for people with serious mental illness. Scand. J. Occup. Ther. 2021, 28, 446–456. [Google Scholar] [CrossRef] [PubMed]
- Carr, M.; Matthews, E.; Williams, J.; Blagrove, M. Testing the theory of Differential Susceptibility to nightmares: The interaction of Sensory Processing Sensitivity with the relationship of low mental wellbeing to nightmare frequency and nightmare distress. J. Sleep Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Harrison, L.A.; Kats, A.; Williams, M.E.; Aziz-Zadeh, L. The Importance of Sensory Processing in Mental Health: A Proposed Addition to the Research Domain Criteria (RDoC) and Suggestions for RDoC 2.0. Front. Psychol. 2019, 10, 103. [Google Scholar] [CrossRef] [PubMed]
- Hjordt, L.V.; Stenbæk, D.S. Sensory processing sensitivity and its association with seasonal affective disorder. Psychiatry Res. 2019, 272, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Kawashima, I.; Nitta, Y.; Kumano, H. Dispositional Mindfulness Mediates the Relationship Between Sensory-Processing Sensitivity and Trait Anxiety, Well-Being, and Psychosomatic Symptoms. Psychol. Rep. 2020, 123, 1083–1098. [Google Scholar] [CrossRef] [PubMed]
- Khosravani, V.; Ganji, Z.; Bastan, F.S.; Ardestani, S.M.S.; Amirinezhad, A. Psychometric properties of the highly sensitive person scale and its relation to symptom dimensions in patients with obsessive-compulsive disorder. Curr. Psychol. 2021, 40, 2725–2734. [Google Scholar] [CrossRef]
- Panagiotidi, M.; Overton, P.G.; Stafford, T. The relationship between sensory processing sensitivity and attention deficit hyperactivity disorder traits: A spectrum approach. Psychiatry Res. 2020, 293, 113477. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Zhang, R.; Li, X.; Feng, T.; Yan, N. The moderating role of sensory processing sensitivity in the link between stress and depression: A VBM study. Neuropsychol. 2021, 150, 107704. [Google Scholar] [CrossRef] [PubMed]
- Meyerson, J.; Gelkopf, M.; Eli, I.; Uziel, N. Burnout and professional quality of life among Israeli dentists: The role of sensory processing sensitivity. Int. Dent. J. 2020, 70, 29–37. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).