Nanotherapeutics: A Way to Cure Cardiac Complications Associated with COVID-19 †
Abstract
1. Introduction
2. Viral Infection and Its Effect on the Human Body
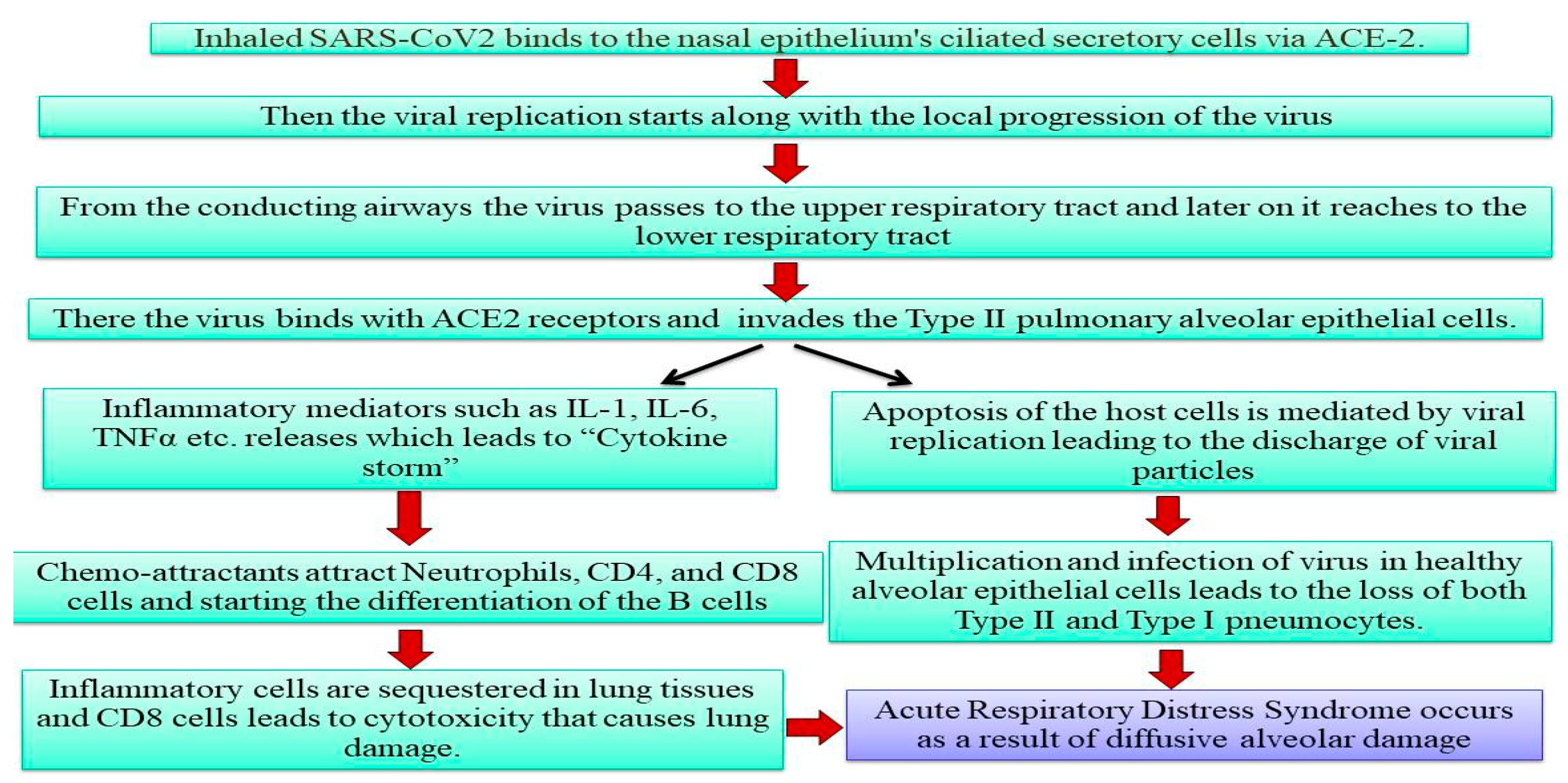
2.1. Pathophysiology of SARS-CoV-2
2.2. Effect on the Major Organs of the Body
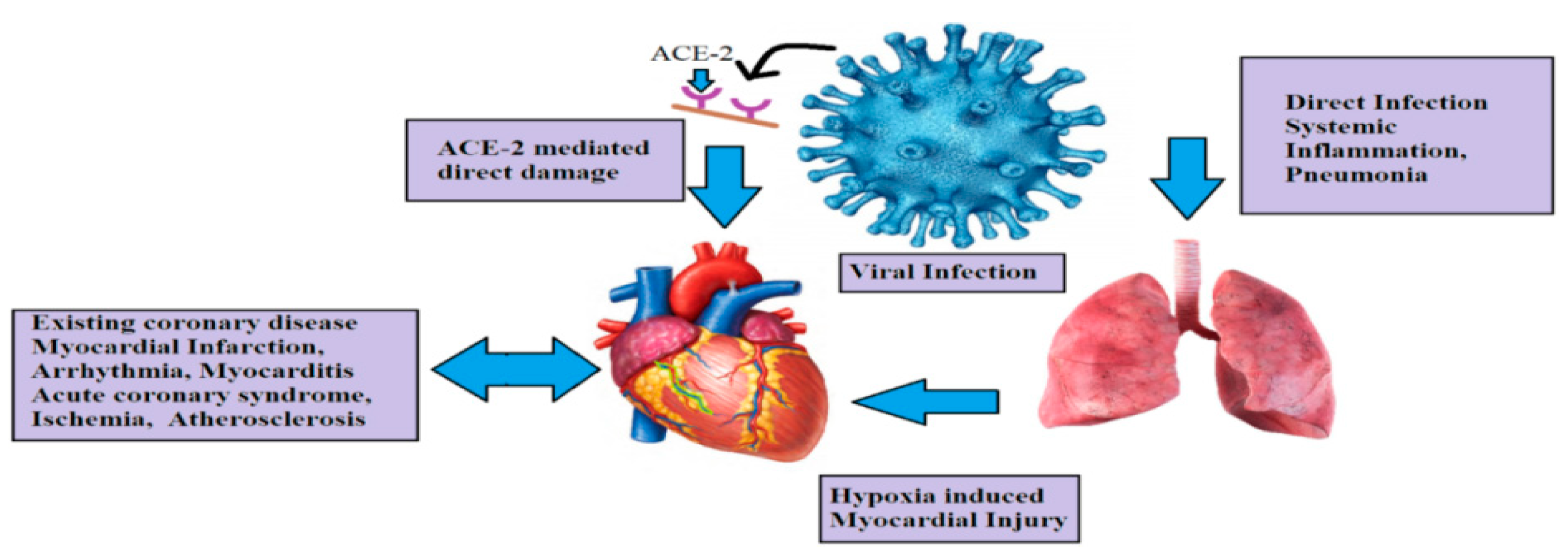
3. Cardiovascular Health and Related Complications Associated with COVID-19
4. Nanotherapeutics in COVID-19
5. Utilisation of Nanotherapeutics to Treat Cardiovascular Disorders
- Hypertension
- Hyperlipidemia
- Stroke
- Pulmonary Hypertension
- Myocardial Infarction
- Thrombosis
Role of Natural Products in the Treatment of Cardiovascular Disorders
6. Potential of Natural Product Derived Nanotherapeutics in Curing Cardiovascular Complications Associated with COVID-19
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yuki, K.; Fujiogi, M.; Koutsogiannaki, S. COVID-19 pathophysiology: A review. J. Clin. Immunol. 2020, 215, 108427. [Google Scholar] [CrossRef] [PubMed]
- Lotfi, M.; Hamblin, M.R.; Rezaei, N. COVID-19: Transmission, prevention, and potential therapeutic opportunities. Clin. Chim. Acta 2020, 508, 254–266. [Google Scholar] [CrossRef] [PubMed]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef]
- Malone, R.W.; Tisdall, P.; Fremont-Smith, P.; Liu, Y.; Huang, X.P.; White, K.M.; Miorin, L.; Moreno, E.; Alon, A.; Delaforge, E.; et al. COVID-19: Famotidine, histamine, mast cells, and mechanisms. Front. Pharmacol. 2021, 12, 633680. [Google Scholar] [CrossRef] [PubMed]
- Parasher, A. COVID-19: Current understanding of its pathophysiology, clinical presentation and treatment. Postgrad. Med. J. 2021, 97, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Jain, U. Effect of COVID-19 on the Organs. Cureus 2020, 12, e9540. [Google Scholar] [CrossRef] [PubMed]
- Nuzzo, D.; Picone, P. Potential neurological effects of severe COVID-19 infection. J. Neurosci. Res. 2020, 158, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Higgins, V.; Sohaei, D.; Diamandis, E.P.; Prassas, I. COVID-19: From an acute to chronic disease? Potential long-term health consequences. Crit. Rev. Clin. Lab. Sci. 2021, 58, 297–310. [Google Scholar] [CrossRef]
- Bzeizi, K.; Abdulla, M.; Mohammed, N.; Alqamish, J.; Jamshidi, N.; Broering, D. Effect of COVID-19 on liver abnormalities: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 10599. [Google Scholar] [CrossRef]
- Kaafarani, H.M.; El Moheb, M.; Hwabejire, J.O.; Naar, L.; Christensen, M.A.; Breen, K.; Gaitanidis, A.; Alser, O.; Mashbari, H.; Bankhead-Kendall, B.; et al. Gastrointestinal complications in critically ill patients with COVID-19. Ann. Surg. 2020, 272, e61. [Google Scholar] [CrossRef]
- Merad, M.; Martin, J.C. Pathological inflammation in patients with COVID-19: A key role for monocytes and macrophages. Nat. Rev. Immunol. 2020, 20, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Tan, W.; Aboulhosn, J. The cardiovascular burden of coronavirus disease 2019 (COVID-19) with a focus on congenital heart disease. Int. J. Cardiol. 2020, 309, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Aghagoli, G.; Gallo Marin, B.; Soliman, L.B.; Sellke, F.W. Cardiac involvement in COVID-19 patients: Risk factors, predictors, and complications: A review. J. Card. Surg. 2020, 35, 1302–1305. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, S.; Narasimhan, A.K.; Gangodkar, D.; Dhanasekaran, S.; Jha, N.K.; Dua, K.; Thakur, V.K.; Gupta, P.K. Aptameric nanobiosensors for the diagnosis of COVID-19: An update. Mater. Lett. 2022, 308, 131237. [Google Scholar] [CrossRef] [PubMed]
- Dube, T.; Ghosh, A.; Mishra, J.; Kompella, U.B.; Panda, J.J. Repurposed drugs, molecular vaccines, immune-modulators, and nanotherapeutics to treat and prevent COVID-19 associated with SARS-CoV-2, a deadly nanovector. Adv. Ther. 2021, 4, 2000172. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Bakky, M.S.; Amin, E.; Ewees, M.G.; Mahmoud, N.I.; Mohammed, H.A.; Altowayan, W.M.; Abdellatif, A.A. Coagulation System Activation for Targeting of COVID-19: Insights into Anticoagulants, Vaccine-Loaded Nanoparticles, and Hypercoagulability in COVID-19 Vaccines. Viruses 2022, 14, 228. [Google Scholar] [CrossRef]
- Liu, L.; Ren, J.; He, Z.; Men, K.; Mao, Y.; Ye, T.; Chen, H.; Li, L.; Xu, B.; Wei, Y.; et al. Cholesterol-modified hydroxychloroquine-loaded nanocarriers in bleomycin-induced pulmonary fibrosis. Sci. Rep. 2017, 7, 10737. [Google Scholar] [CrossRef]
- Hassanzadeh, P. Nanotheranostics against COVID-19: From multivalent to immune-targeted materials. J. Control. Release 2020, 328, 112–126. [Google Scholar] [CrossRef]
- Cavalcanti, A.; Rosen, L.; Kretly, L.C.; Rosenfeld, M.; Einav, S. Nanorobotic challenges in biomedical applications, design and control. In Proceedings of the 2004 11th IEEE International Conference on Electronics, Circuits and Systems, Tel Aviv, Israel, 13–15 December 2004; IEEE: Piscataway, NJ, USA; pp. 447–450. [Google Scholar] [CrossRef]
- Sahoo, S.K.; Parveen, S.; Panda, J.J. The present and future of nanotechnology in human health care. Nanomedicine. 2007, 3, 20–31. [Google Scholar] [CrossRef]
- Martín Giménez, V.M.; Kassuha, D.E.; Manucha, W. Nanomedicine applied to cardiovascular diseases: Latest developments. Ther. Adv. Cardiovasc. Dis. 2017, 11, 133–142. [Google Scholar] [CrossRef]
- Korin, N.; Kanapathipillai, M.; Matthews, B.D.; Crescente, M.; Brill, A.; Mammoto, T.; Ghosh, K.; Jurek, S.; Bencherif, S.A.; Bhatta, D.; et al. Shear-activated nanotherapeutics for drug targeting to obstructed blood vessels. Science 2012, 337, 738–742. [Google Scholar] [CrossRef] [PubMed]
- Khan, J.; Deb, P.K.; Priya, S.; Medina, K.D.; Devi, R.; Walode, S.G.; Rudrapal, M. Dietary flavonoids: Cardioprotective potential with antioxidant effects and their pharmacokinetic, toxicological and therapeutic concerns. Molecules 2021, 26, 4021. [Google Scholar] [CrossRef] [PubMed]
- Arbeláez, L.F.; Pardo, A.C.; Fantinelli, J.C.; Schinella, G.R.; Mosca, S.M.; Ríos, J.L. Cardioprotection and natural polyphenols: An update of clinical and experimental studies. Food Funct. 2018, 9, 6129–6145. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.A.; Kim, J.H. Possibility as role of ginseng and ginsenosides on inhibiting the heart disease of COVID-19: A systematic review. J. Ginseng Res. 2022, 46, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, A.; Raish, M.; Alkharfy, K.M. The potential role of thymoquinone in preventing the cardiovascular complications of COVID-19. Curr. Vasc. Pharmacol. 2021, 141, 106899. [Google Scholar] [CrossRef]
- Abubakar, M.B.; Usman, D.; Batiha, G.E.; Cruz-Martins, N.; Malami, I.; Ibrahim, K.G.; Abubakar, B.; Bello, M.B.; Muhammad, A.; Gan, S.H.; et al. Natural products modulating Angiotensin Converting Enzyme 2 (ACE2) as potential COVID-19 therapies. Front. Pharmacol. 2021, 12, 1–19. [Google Scholar] [CrossRef]
- Pechanova, O.; Dayar, E.; Cebova, M. Therapeutic potential of polyphenols-loaded polymeric nanoparticles in cardiovascular system. Molecules 2020, 25, 3322. [Google Scholar] [CrossRef]
- Tan, M.E.; He, C.H.; Jiang, W.; Zeng, C.; Yu, N.; Huang, W.; Gao, Z.G.; Xing, J.G. Development of solid lipid nanoparticles containing total flavonoid extract from Dracocephalum moldavica L. and their therapeutic effect against myocardial ischemia–reperfusion injury in rats. Int. J. Nanomed. 2017, 12, 3253. [Google Scholar] [CrossRef]
- Hesari, M.; Mohammadi, P.; Khademi, F.; Shackebaei, D.; Momtaz, S.; Moasefi, N.; Farzaei, M.H.; Abdollahi, M. Current Advances in the use of nanophytomedicine therapies for human cardiovascular diseases. Int. J. Nanomed. 2021, 16, 3293–3315. [Google Scholar] [CrossRef]
- Zhang, L.; Zhu, K.; Zeng, H.; Zhang, J.; Pu, Y.; Wang, Z.; Zhang, T.; Wang, B. Resveratrol solid lipid nanoparticles to trigger credible inhibition of doxorubicin cardiotoxicity. Int. J. Nanomed. 2019, 14, 6061–6071. [Google Scholar] [CrossRef]
- Xiong, F.; Wang, H.; Geng, K.K.; Gu, N.; Zhu, J.B. Optimized preparation, characterization and biodistribution in heart of breviscapine lipid emulsion. Chem. Pharm. Bull. 2010, 58, 1455–1460. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Atale, N.; Saxena, S.; Nirmala, J.G.; Narendhirakannan, R.T.; Mohanty, S.; Rani, V. Synthesis and characterization of Sygyzium cumini nanoparticles for its protective potential in high glucose-induced cardiac stress: A green approach. App. Biochem. Biotechnol. 2017, 181, 1140–1154. [Google Scholar] [CrossRef] [PubMed]
| Name of the Natural Product | Source | Nanoformulations | Mechanism of Action | Reference |
|---|---|---|---|---|
| Total flavonoid extract (tilianin, luteolin, and rosmarinic acid) | Dracocephalum moldavica L. | Solid lipid nanoparticle | Improves the integrity of myocardial membrane; reduces the level of IL-1β & TNF-α | [29] |
| Curcumin | Curcumin longa | Curcumin nanoemulsion | Increases 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibition showing antihypercholestrolemic activity | [30] |
| Quercetin | Prunus avium | Quercetin-loaded PLGA | Reduces the production of the inflammatory cytokines | [30] |
| Ginsenoside R3 | Panax ginseng | R3 loaded in Pluronic F127 micelles | Reduces myocardial levels of LDH, CK-MB, and CK. Maintains integrity of myocytes and reduces apoptosis | [30] |
| Resveratrol | - | Liposomal encapsulations containing berberine | In myocardial infraction, it preserves left ventricular ejection and reduces adverse cardiac remodeling | [30] |
| Resveratrol | - | Polycaprolactone encapsulated resveratrol nanocapsule | Reduces systolic and diastolic blood pressure | [30] |
| Solid lipid nanoparticle loaded with Resveratrol | Protects heart from Doxorubicin-induced toxicity; increases heart rate, ejection fraction, and fractional shortening | [31] | ||
| Breviscapine | Erigeron breviscapus | Lipid emulsion | Removes blood stasis and promotes blood circulation | [30,32] |
| Methanolic extract | Syzygium cumini | Silver nanoparticle | Reduces oxidative damage and maintains the integrity of high glucose stressed cardiac cells | [33] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pal, S.; Saha, R.; Jha, S.; Sarkar, B. Nanotherapeutics: A Way to Cure Cardiac Complications Associated with COVID-19. Med. Sci. Forum 2022, 10, 10. https://doi.org/10.3390/IECH2022-12301
Pal S, Saha R, Jha S, Sarkar B. Nanotherapeutics: A Way to Cure Cardiac Complications Associated with COVID-19. Medical Sciences Forum. 2022; 10(1):10. https://doi.org/10.3390/IECH2022-12301
Chicago/Turabian StylePal, Shreyashi, Rajdeep Saha, Shivesh Jha, and Biswatrish Sarkar. 2022. "Nanotherapeutics: A Way to Cure Cardiac Complications Associated with COVID-19" Medical Sciences Forum 10, no. 1: 10. https://doi.org/10.3390/IECH2022-12301
APA StylePal, S., Saha, R., Jha, S., & Sarkar, B. (2022). Nanotherapeutics: A Way to Cure Cardiac Complications Associated with COVID-19. Medical Sciences Forum, 10(1), 10. https://doi.org/10.3390/IECH2022-12301








