Abstract
Individualized, serial production of innovative implants is a major area of application for additive manufacturing in the field of medicine. Individualized healthcare requires faster delivery of the implant to the clinic or hospital facility. The total manufacturing process, including data generation using 3D drawings, imaging techniques, 3D printing and post-processing, usually takes up to a week, especially implants from risk class III, which requires qualified equipment and a validated process. In this study, we describe how to develop a new biomechanical model for dental implants from its conception for the patent to the final product which is ready to be manufactured using additive manufacturing. The benefits and limitations of titanium metal printing for dental implant prototypes are presented by the authors.
1. Introduction
Developing a new biomedical device, especially osseointegrated bone screws and/or implants for dentistry, orthopedics, neurosurgery, and all kinds of protheses fixed by bone implants, is a challenge that involves different professionals with different areas of expertise. The development of new concepts for biomedical devices can usually be performed by surgeons specialized in the field of innovation. The next steps involve a designer, engineer, and different technicians who will help to apply computational simulations, laboratory experiments, animal testing, and clinical trials where they are mandatory.
The aim of this study is to describe the whole process of developing a new biomechanism for bone screws for the application of dental implants, from concept creation by the author, initial patent design, and further needs, which will make individualized production possible using commercially pure titanium, or titanium alloy (Ti6Al4V), and where each component is fabricated by additive manufacturing (3D printing). This process can be applied to the research of innovative technologies, for companies and individuals, becoming a promising way to prototype new biomedical devices with all the advantages that 3D printing technology aggregates, including its quality and validated process.
The present and future of biomedical devices is in three-dimensional (3D) printing [1]. These technologies are having a remarkable impact on all aspects in the field of medicine, enhancing the possibilities to make precise, complex geometrical forms, from the initial concept and digital data, and in a variety of materials. It has been praised as a disruptive technology which will change manufacturing [2].
Three-dimensional printing by Selective Laser Sintering (SLS) has been available since 1986 [3]. Surgical applications using this method emerged later with improved technologies, making it possible for straightforward individualized or batch production of bone implants for surgeries in orthopedics, dentistry, neurosurgeries, and cranioplasties in both oral and maxillofacial surgery [3,4,5].
Direct metal laser sintering (DMLS) is the most widely used metal 3D printing technology. DMLS and SLM (selective laser melting) are used by technicians interchangeably, but they are also slightly different. Although the process is the same, DMLS is preferable when alloys are being created for metal parts, whereas SLM is used to create single element metals (Titanium CP) [6,7].
The additive manufacturing technology can also effectively integrate diverse types of living cells within a three-dimensional scaffold made up of conventional micro or nanoscale biomaterials to create an artificial bone graft capable of regenerating the damaged tissues [8,9,10,11,12,13].
In this work, we describe how to rapidly prototype a new biomechanical model for bone screws as a dental implant in 3D, improving the designs, optimizing the 3D printing process, and correlating desired functional aspects, and within the limitations of the additive manufacturing process. The purpose of this work is to describe how to prototype an innovative biomedical device by 3D printing.
2. Materials and Methods
The bioactive kinetic screw (BKS), as seen in Figure 1, was created by the first author, and intended to reutilize the bone removed and discarded during the drilling for a dental implant’s insertion into the bone. The original design was made by the first author on a sheet of paper. The goal at that point was to describe the new biomechanical concept and the possibility of applying for a patent request. A specialized company in Brazil, Modal Marcas e Patentes, for patent deposit, developed the first 3D design in Solidworks®. After six modifications by the author, finally the concept was ready to fill the patent request which was subsequently successfully completed.
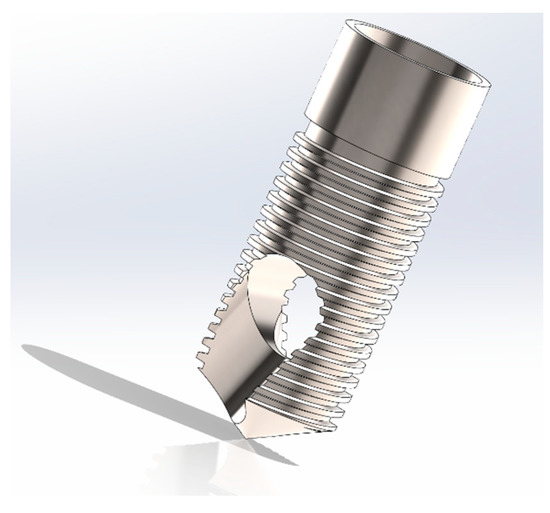
Figure 1.
Prototype of BKS ready to be 3D printed.
An extensive literature review [14,15,16,17] was conducted after that to determine all the engineering and biological concepts to be applied in BKS, and given the possible sizes of the screw, flutes, through hole, threads, pitch, prothesis connections, angle of cut, angle of threads, every detail should be designed with the purpose of obtaining primary stability (mechanical) in the bone and secondary stability (biological) for as long a period as possible. Based on the literature review, these choices are made in relation to the purpose of the biomedical device and the characteristics desired by the author. The screw can be produced in any size according to the required bone specifications. In this study, we applied the size of 10 mm length and 4 mm diameter.
The next step was to evaluate by finite element analysis (FEA) the thermo-mechanical behavior of the BKS into the bone. At that point, modifications can be made by the authors, to achieve desired goals about the strain–stress levels which are required in order for the new prototype to be developed [14,15,16,17].
Once the computer simulations are finished, printing prototypes are mandatory to check if the desired outcomes observed in the project are fulfilled by the 3D printing process, and that they have an accuracy of 0.1 mm [2,5]. Prototypes can also be 3D printed in composites before the 3D metal printing; a filament extrusion system can be used because of the feasibility and similarity in the results of the printed device. The final concept design will be ready to metal 3D print by specialized additive manufacturing factories that have a validated process as seen in Figure 2.
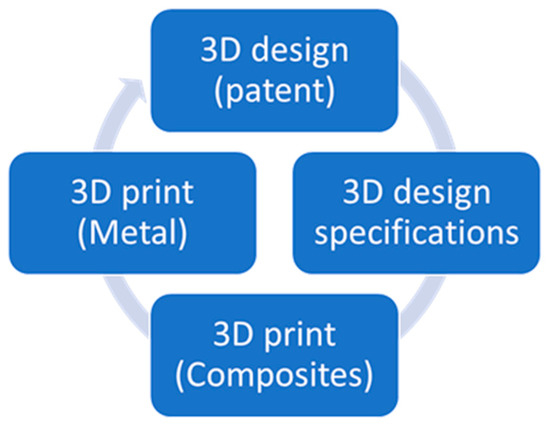
Figure 2.
Methodology applied to develop a 3D-printed prototype of a dental implant.
Approved factories for biomedical devices manufacturing can deliver the final product ready to use, depending on the regulations applied for specific biomedical device [18,19]. Class III devices (biomedical devices) are subjected to higher regulatory scrutiny. However, the guidance lacks information on point-of-care manufacturing, which may be a significant gap as hospitals have rapidly invested in 3D printers over the past few years. Under the medical devices category, the FDA has also cleared software programs specifically intended to generate 3D models of a patient’s anatomy. The FDA leaves it up to the medical facility to use the software correctly and within the scope of its intended use [18].
Within the European Union (EU), medical devices are regulated by European Council Directives 93/42/EEC (for medical devices, known as the MDD). The majority of 3D printed medical devices to date have been under MDD regulation and these are considered “custom-made”, which is defined as being specifically made in accordance with a written prescription of any person authorized by national law by virtue of that person’s professional qualifications. This allows for, under their responsibility, specific design characteristics and is intended for the sole use of a particular patient to exclusively meet their individual conditions and needs [19,20].
3. Results
Since its first conceptualization for the patent, the BKS design was modified in Solidworks®, as seen in Figure 3, and printed in composites and metal for a visual analysis and for the efficacy of 3D printing in relation to the final desired outcome.
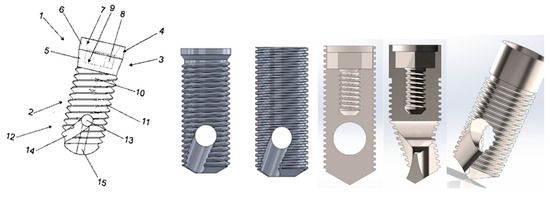
Figure 3.
Evolution of the 3D design in Solidworks®. Characterized by a main body (1) that describes a cylindrical trunk (2), whose upper section (3) projects a head (4) with lower tapered section (5) from which extends a cylindrical trunk (6) that internally describes an oblique wall (7) that ends in an internal hexagon (8) whose bottom (9) projects centrally and longitudinally blind hole (10), cylindrical trunk (2) provided with a superb thread (11), whose lower section (12) has a through hole (13) that projects conductive grooves transversely (14), cylindrical trunk (2) is liable to receive a longitudinal hole (15) which communicates with the through-hole (13).
3.1. BKS 3D Printing
Three-dimensional printing in composites during the development process was a fundamental task before the metal printing. It is a feasible and faster way to evaluate the quality and features through a visual analysis and assess the connections for the prothesis and, at same time, the executability for the final titanium metal printing, as seen in Figure 4.

Figure 4.
Testing connections in the BKS 3D printed in composite (Nylon).
During the metallic printing tests, as seen in Figure 5, we found unfavorable results with the initial 3D designs. This pointed out improvements to be completed in the final model. These changes helped not only for making possible the fabrication of the biomedical device BKS by additive manufacturing, but also improved the function for the primary stability insertion torque in the bone.
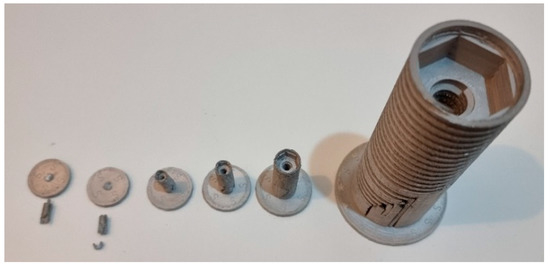
Figure 5.
BKS printed in metal with varied sizes before the final printing process.
After all adjustments and tests, the final prototype is ready to be 3D printed by a specialized additive manufacturing factory that has a validated process for biomedical devices with all certifications required for class III devices.
All these procedures optimize the result and make it feasible for developing new prototypes for healthcare, especially because the inventor will be able to make and analyze the 3D concept in a printed device before sending for a more expensive way of production in titanium.
3.2. BKS FEM Model
In this work, a 3D numerical and structural linear model was developed by the authors, using ANSYS 2020 R2®–Workbench 2020 R2, with the new BKS biomechanism in Ti6Al4V (Grade 5) compared with a regular screw with the same size and threads of BKS. The mechanical properties of the material are shown in Table 1 [21].

Table 1.
Mechanical properties [21].
The application of the finite element modelling (FEM) aims to simulate the BKS biomechanism and evaluate the distribution of mechanical stresses and strains in the screw with or without the new biomechanism. The 3D model was built by the authors, using Solidworks® and ANSYS 2020 R2®–Workbench 2020 R2 software, as shown in Figure 6. Accordingly, the mesh adopted to use in our simulations consists of a total of 23,215 tetrahedron elements in BKS screw and 47,722 elements in the regular screw without biomechanism. The same element size was adopted equal to 0.3 mm.
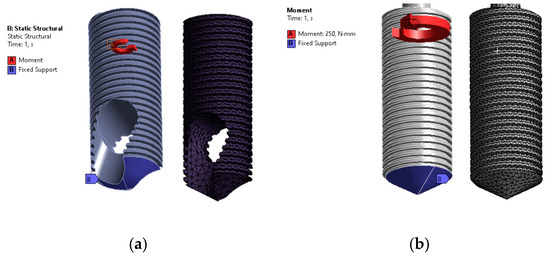
Figure 6.
Static structural analysis. Boundary conditions and mesh. (a) BKS screw. (b) Regular screw without biomechanism.
Based on the geometrical model, volumetric finite element meshes were generated using SOLID187 element. SOLID187 element is a higher order, defined by 10 nodes having three degrees of freedom at each node (translations in the nodal x, y, and z directions). This tetrahedron element has a quadratic displacement behaviour with four-point integration and is suitable for modelling irregular meshes, such as those produced from CAD/CAM systems.
In the present study, an electric motor EM-12L with a maximum power of 59 W was selected, and angular speeds between 100 and 40,000 rpm [22]. The new BKS tool, intended for use in ongoing research, will work with different angular speeds depending on the material with which it is made, and with a constant feed rate of 0.5 mm/s vertically downwards. In this study, only the mechanical load due to the cutting torque was considered in the model and the thermal effect produced by the BKS was not considered in this simulation. The relation between the torque ( in Nm), the maximum electrical power during drilling (P in W) and the speed of rotation (n in rpm) is determined according by Equation (1).
Boundary conditions, which represent typical drilling phenomena, are established on the lower surface of the BKS as fixed, and on the upper surface with the application of torque equal to 250 Nm, according to the rotational speed of 2250 rpm, using Equation (1).
The obtained results from equivalent stress and equivalent elastic strain are shown in Figure 7 and Figure 8.
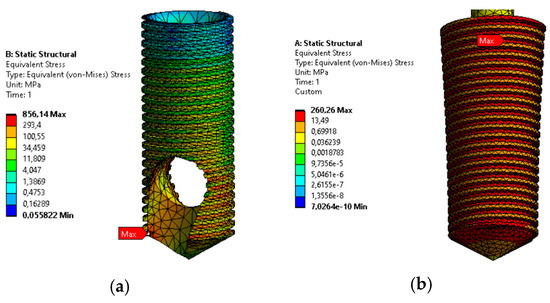
Figure 7.
Equivalent stress in BKS screw (a) and regular screw without biomechanism (b).
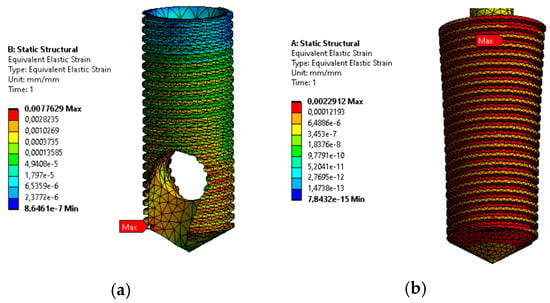
Figure 8.
Equivalent elastic strain in BKS screw (a) and Regular screw without biomechanism (b).
Numerical results show that stress and strain levels increase 3.3 and 3.4 times more (respectively) in the BKS screw when compared with regular screw without the new biomechanism.
At the tip of the screw, the BKS presents higher stress and strain. The equivalent elastic stress determines the level of stress in the BKS that can be transmitted in the drilling process to the bone material.
The calculated stresses and strains vary along the entire length of the BKS, and this can be justified by the inertia of its cross section, with free space existing in the BKS mechanism. The inertia cross section at the bottom decreases, hence the strain increases. The strain level follows the same behavior.
The use of the geometry with the new biomechanics induces greater stresses and strains, but always within the ultimate admissible limit.
4. Discussion
Additive manufacturing or 3D printing is a disruptive technology, and it impacts multiples disciplines, including tissue engineering and biomedical engineering. Biomaterials are natural, synthetic, or combined materials used to improve the healing process of damaged body parts while cooperating with living systems [20]. Since the improvements obtained with osseointegration after Branemark’s work, metallic, ceramic, and polymeric biomaterials have stablished unique innovations to biomedical devices, improving the quality of human life.
Biocompatibility is recognized by the literature as the primary goal for the biological assessment of a biomaterial. The elastic modulus is observed in an equal manner for mechanical performance. Metals are mostly bioinert, whereas ceramics, glasses and polymers can be bioinert or bioactive [23,24].
Metals and their alloys are applied in all biomedical devices, such as commercially pure titanium and its alloy (Ti6Al4V), for orthopedic, maxillofacial surgeries and load-bearing hip and knee implants, respectively. Stainless steel 316L is used for fracture treatment, and CoCr alloys for mobility surfaces [8,20,24].
It is crucial to invent new biomaterials with individual properties and mandatory to settle proved manufacturing standards to build distinct biomedical devices. Three-dimensional printing has updated biomedical device manufacturing, especially for porous scaffolds and patient-matched implants, increasing the design possibilities of biomedical devices [25,26].
Three-dimensionally printed metallic implants in the initial stages of development were intended to create porous structures to reduce the natural stiffness of the material and the methods for biological integration [27].
The new BKS presented all of the following desired factors combined in one biomedical device: the possibility to be 3D printed in commercially pure titanium and its alloy (Ti6Al4V); the presence of grooves and a hole making it porous decreasing the stiffness of the device; and can be a patient-matched implant.
One of the greatest benefits added on this new BKS prototype is the innovation for patient-matched dental implants and can be performed in a straightforward manner through a validated and certified company, after biomechanical tests, and following international regulatory rules [13,14].
Three-dimensionally printed patient-matched implants are being increasingly and continually developed and applied in the last years. Over 100,000 mass-produced metallic implants for human use are being additive manufactured every year only in the United States and used regularly in hospitals worldwide. Regulatory approval for 3D-printed devices can be slow if the operations are significantly different from traditional approaches [18,19,20].
Metal powders are the raw materials for additive manufacturing technologies. It is still questionable how long these powders can be reused, and what proper techniques should be applied to guarantee the robustness of the process [3,4].
With improved design flexibility and materials options in additive manufacturing, diversified innovative biomedical devices will be available to benefit long-established challenges in human care.
Creativity and imagination are needed to solve problems, and healthcare innovations in biomedical devices are a reality and will become the primary founders of disruptive technologies, both aggregating and increasing economic value. Three-dimensional printing is described to be the fourth industrial revolution and it is changing the traditional manufacturing process, being sustainable for the environment, economy, and society [28,29].
The final design of BKS was reinforced in the crest module diameter (top of the dental implants, as seen in Figure 1) after failures in metal 3D printing, while improving the prosthesis connection surface, decreasing stress within the bone where higher stresses occur. The gain in crest module diameter enhances the prosthesis adaptation with lesser stresses during loading [30]. We realized that techniques to minimize the part volume and using additive manufacturing technologies that do not require support structures can help keep costs as low as possible. Metal filament for 3D printers is not suited for industrial metal 3D printing, both from a throughput and from a quality perspective.
The best solution for biomedical devices is DMLS (direct metal laser sintering). SLM (selective laser melting) uses a combination of heat and pressure to make particles stick together. Melting (DMLS) uses high enough temperatures to cause the particles to fully melt and join. Sintered parts have high porosity and require heat treatments to be strengthened, though they will never be as strong as forged metal parts; melted parts are fully solid and do not require heat treatments.
Macro design in implants focuses on the relationship between osseointegration and mechanical features of implant design engineering and helps to understand which implant to select depending on different clinical conditions. Micro design features include the study of the biological aspect of implant design and focuses on the host response patterns and implant survival. It influences cell behavior on the surface such as adhesion, proliferation, and differentiation of cells as well as the mineralization of the extracellular matrix at the implant’s surfaces [14,17,24].
BKS, the new biomechanism presented in this work, aims to bring biomechanical benefits to all types of screws and their designs in which bone integration is necessary in the short and long term. The disadvantage is when a temporary fixation of the screw is needed. In this case, the BKS is contra-indicated.
5. Conclusions
The creation, development, and prototyping of innovative biomedical devices has seen a huge improvement with the recent technologies and software, especially related to 3D printing and 3D drawings, respectively. DMLS (direct metal laser sintering) additive manufacturing offers a better quality and faster process of developing a complete prototype to be used for experiments or human application, following international regulatory rules.
The numerical results obtained by FEM showed that the BKS has structural strength for its proposed biomechanics and pointed out that the region on the top of the screw (crest module), where bone-implant contact occurs and the prosthesis is fixed in a dental implant, was designed to be most reinforced area of the screw.
Future studies will describe the results of the BKS prototype in vivo. These results can be used to add novel changes in the 3D model, applying the same method described in this work.
6. Patents
Carlos Aurelio Andreucci, C.A.A. (2022). Disposição construtiva aplicada em parafuso para implante ósseo (Brasil/Internacional Patent No. WO2022036425A1). WIPO (PCT). URL WO2022036425A1–Disposição construtiva aplicada em parafuso para implante ósseo–Google Patents.
Author Contributions
Conceptualization, C.A.A.; methodology, C.A.A.; software, E.M.M.F.; validation, C.A.A., E.M.M.F. and R.N.J.; formal analysis, R.N.J.; investigation, C.A.A.; resources, C.A.A.; data curation, C.A.A.; writing—original draft preparation, C.A.A.; writing—review and editing, E.M.M.F.; visualization, R.N.J.; supervision, E.M.M.F.; project administration, R.N.J.; funding acquisition, C.A.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Coriaty, N.; Pettibone, K.; Todd, N.; Rush, S.; Carter, R.; Zdenek, C. Titanium Scaffolding: An Innovative Modality for Salvage of Failed First Ray Procedures. J. Foot Ankle Surg. 2018, 57, 593–599. [Google Scholar] [CrossRef] [PubMed]
- Dawood, A.; Marti, B.M.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Deckard, C. Method and Apparatus for Producing Parts by Selective Sintering. U.S. Patent US4863538A, 5 September 1989. [Google Scholar]
- Melchels, F.P.W.; Feijen, J.; Grijpma, D.W. A review on stereolithography and its applications in biomedical engineering. Biomaterials 2010, 31, 6121–6130. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Yang, Y.; Bharech, S.; Lin, B.; Schröder, J.; Xu, B. 3D-multilayer simulation of microstructure and mechanical properties of porous materials by selective sintering. GAMM-Mitteilungen 2021, 44, e202100017. [Google Scholar] [CrossRef]
- Cerea, M.; Dolcini, G.A. Custom-Made Direct Metal Laser Sintering Titanium Subperiosteal Implants: A Retrospective Clinical Study on 70 Patients. BioMed Res. Int. 2018, 2018, 5420391. [Google Scholar] [CrossRef]
- Jaivignesh, M.; Babu, A.S.; Arumaikkannu, G. In-vitro Analysis of Titanium Cellular Structures Fabricated by Direct Metal Laser Sintering. Mater. Today Proc. 2020, 22, 2372–2377. [Google Scholar] [CrossRef]
- Cheng, L.; Shoma, K.; Suresh, S.; He, H.; Rajput, R.S.; Feng, Q.; Ramesh, S.; Wang, Y.; Krishnan, S.; Ostrovidov, S.; et al. 3D Printing of Micro- and Nanoscale Bone Substitutes: A Review on Technical and Translational Perspectives. Int. J. Nanomed. 2021, 16, 4289–4319. [Google Scholar] [CrossRef]
- Cox, S.C.; Thornby, J.A.; Gibbons, G.J.; Williams, M.A.; Mallick, K.K. 3D printing of porous hydroxyapatite scaffolds intended for use in bone tissue engineering applications. Mater. Sci. Eng. C 2015, 47, 237–247. [Google Scholar] [CrossRef]
- Kim, J.I.; Kim, D.Y.; Kwon, D.Y.; Kang, H.J.; Min, B.H.; Kim, M.S. An injectable biodegradable temperature-responsive gel with an adjustable persistence window. Biomaterials 2012, 33, 2823–2834. [Google Scholar] [CrossRef]
- Kantaros, A.; Piromalis, D. Fabricating Lattice Structures via 3D Printing: The Case of Porous Bio-Engineered Scaffolds. Appl. Mech. 2021, 2, 18. [Google Scholar] [CrossRef]
- Inzana, J.A.; Olvera, D.; Fuller, S.M.; Kelly, J.P.; Graeve, O.A.; Schwarz, E.M.; Kates, S.L.; Awad, H.A. 3D printing of composite calcium phosphate and collagen scaffolds for bone regeneration. Biomaterials 2014, 35, 4026–4034. [Google Scholar] [CrossRef]
- Kantaros, A.; Chatzidai, N.; Karalekas, D. 3D printing-assisted design of scaffold structures. Int. J. Adv. Manuf. Technol. 2015, 82, 559–571. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Fonseca, E.M.M.; Jorge, R.N. Advances and Current Trends in Biomechanics, 1st ed.; Taylor & Francis: London, UK, 2021; pp. 1–4. [Google Scholar]
- Fernandes, M.G.; Fonseca, E.M.; Natal, R.M. Three-dimensional dynamic finite element and experimental models for drilling processes. Proc. Inst. Mech. Eng. Part L J. Mater. Des. Appl. 2015, 232, 35–43. [Google Scholar] [CrossRef]
- Fernandes, M.G.; Fonseca, E.M.; Jorge, R.N. Thermo-mechanical stresses distribution on bone drilling: Numerical and experimental procedures. Proc. Inst. Mech. Eng. Part L J. Mater. Des. Appl. 2019, 233, 637–646. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Alshaya, A.; Fonseca, E.M.M.; Jorge, R.N. Proposal for a New Bioactive Kinetic Screw in an Implant, Using a Numerical Model. Appl. Sci. 2022, 12, 779. [Google Scholar] [CrossRef]
- Available online: https://www.fda.gov/medical-devices/3d-printing-medical-devices/3d-printing-medical-devices-point-care-discussion-paper (accessed on 28 October 2022).
- Available online: https://www.ema.europa.eu/en/human-regulatory/overview/medical-devices (accessed on 28 October 2022).
- Bandyopadhyay, A.; Ghosh, S.; Boccaccini, A.R.; Bose, S. 3D printing of biomedical materials and devices. J. Mater. Res. 2021, 36, 3713–3724. [Google Scholar] [CrossRef]
- Shah, F.A.; Trobos, M.; Thomsen, P.; Palmquist, A. Commercially pure titanium (cp-Ti) versus titanium alloy (Ti6Al4V) materials as bone anchored implants—Is one truly better than the other? Mater. Sci. Eng. C 2016, 62, 960–966. [Google Scholar] [CrossRef]
- Available online: https://www.wh.com/en_global/dental-products/restoration-prosthetics/electric-motor/em-12l/ (accessed on 22 November 2022).
- Ashtiani, R.E.; Alam, M.; Tavakolizadeh, S.; Abbasi, K. The Role of Biomaterials and Biocompatible Materials in Implant-Supported Dental Prosthesis. Evidence-Based Complement. Altern. Med. 2021, 2021, 3349433. [Google Scholar] [CrossRef]
- Albrektsson, T.; Johansson, C. Osteoinduction, osteoconduction and osseointegration. Eur. Spine J. 2001, 10 (Suppl. S2), S96–S101. [Google Scholar]
- Bose, S.; Ke, D.; Sahasrabudhe, H.; Bandyopadhyay, A. Additive manufacturing of biomaterials. Prog. Mater. Sci. 2018, 93, 45–111. [Google Scholar] [CrossRef]
- Bandyopadhyay, A.; Mitra, I.; Bose, S. 3D Printing for Bone Regeneration. Curr. Osteoporos. Rep. 2020, 18, 505–514. [Google Scholar] [CrossRef]
- Dumas, M.; Terriault, P.; Brailovski, V. Modelling and characterization of a porosity graded lattice structure for additively manufactured biomaterials. Mater. Des. 2017, 121, 383–392. [Google Scholar] [CrossRef]
- Liu, Z.; Jiang, Q.; Zhang, Y.; Li, T.; Zhang, H. Sustainability of 3D Printing: A Critical Review and Recommendations. In Proceedings of the ASME 2016 11th International Manufacturing Science and Engineering Conference, Blacksburg, VA, USA, 27 June–1 July 2016; Volume 2, p. 4. [Google Scholar] [CrossRef]
- Jiang, Q.; Liu, Z.; Li, T.; Cong, W.; Zhang, H.-C. Emergy-based life-cycle assessment (Em-LCA) for sustainability assessment: A case study of laser additive manufacturing versus CNC machining. Int. J. Adv. Manuf. Technol. 2019, 102, 4109–4120. [Google Scholar] [CrossRef]
- Shetty, P.; Yadav, P.; Tahir, M.; Saini, V.; Prajapati, D.; Mahesh, L. Implant Design and Stress Distribution. Int. J. Oral Implant. Clin. Res. 2016, 7, 34–39. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).