Abstract
Chronic exposure to the nephrotoxic metal pollutant, cadmium (Cd), has been associated with hypertension, but the mechanism by which it raises blood pressure is not understood. We hypothesize that exposure to Cd reduces the glomerular filtration rate (GFR), which in turn causes a rise in blood pressure. Data were collected from 447 Thai subjects with a mean age of 51.1 years, of which 48.8% had hypertension, 15.4% had diabetes, and 6.9% had an estimated GFR (eGFR) below 60 mL/min/1.73 m2 (low eGFR). More than half (58.8%) and 23.9% had moderate and severe tubular proteinuria, respectively. The mean blood and urinary Cd concentrations were 2.75 and 4.23 µg/L, respectively. Doubling of body burden of Cd increased the prevalence odds ratios (POR) for low eGFR and severe tubular proteinuria 41% and 48%, respectively. The POR for hypertension rose twofold in those with blood Cd levels of 0.61–1.69 µg/L or urinary Cd excretion levels ≥ 0.98 µg/g creatinine. In the hypertensive group, the eGFR was inversely associated with age (β = −0.517), the Cd excretion rate (β = −0.177), and diabetes (β = −0.175). By mediation analysis, an increase in SBP was attributable totally to the effect of Cd on GFR. Thus, blood pressure appeared to rise as GFR fell. This finding is consistent with the well-known role of the kidney in long-term blood pressure regulation, and explains a universally high prevalence of hypertension among patients with low eGFR.
1. Introduction
Hypertension, indicated by systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg, is a common risk factor for cardiovascular disease (CVD) and can be both a cause and a consequence of chronic kidney disease (CKD) [1,2,3]. Concerningly, mortality from CKD rose from the 13th leading cause of death in 2000 to the 7th in 2021, and it is projected to be the 5th leading cause of years of life lost by 2040 [4,5].
Because of its ubiquitous environmental presence, exposure to the nephrotoxic metal pollutant cadmium (Cd) is also a significant risk factor for CVD [6] and CKD [7]. A 75% increase in deaths from any cause among those with CKD was associated with Cd exposure even at low levels, reflected by urinary Cd levels ≥ 0.60 μg/g creatinine [8]. The risk of having CVD rose 2.58-fold and 2.79-fold at blood Cd level of 1 μg/L and urinary Cd excretion rate of 0.5 μg/g creatinine, respectively [6]. Notably, environmental Cd exposure appeared to adversely affect females and males differently [9,10,11,12].
In the U.S. general population, an overall mean urinary Cd excretion was 0.5 µg/g creatinine, and 2.5%, 7.1%, and 16% of non-smoking women (aged ≥ 20 years) had urinary Cd levels > 1, >0.7, and >0.5 μg/g creatinine, respectively [13]. In comparison, a study from Thailand reported a 22.5% prevalence of Cd excretion ≥ 1 µg/g creatinine in non-smoking women who had low body iron stores [14]. Thus, the proportions of at-risk subpopulations are concerning.
Effects of environmental exposure to Cd on blood pressure has been well documented in studies of the general populations of the U.S. [15,16,17], Canada [18], China [19,20,21], Korea [22,23], and Japan [24]. For non-occupationally exposed populations, diet is the main source of Cd exposure, other than through passive and active smoking [25,26,27,28]. The intestinal absorption rate of Cd can be as high as 45% [29,30] as Cd can be absorbed through several metal transporters for metal nutrients, iron, zinc, copper, and calcium (Fe, Zn, Cu and Ca) [31,32]. Furthermore, Cd complexed with metallothionein (MT) and phytochelatin (PC), as CdMT and CdPC, can be absorbed through transcytosis as well as receptor-mediated endocytosis [33,34,35]. Notably, however, there are no physiologic mechanisms for Cd elimination. Continued exposure will lead to its accumulation in tissues and organs throughout the body, notably in the kidneys, where it promoted the progression of kidney disease to kidney failure, especially in diabetics [36].
The kidneys play an indispensable role in long-term blood pressure regulation [2], and the principal site of Cd toxicity due to a preferential accumulation of Cd in the proximal tubular epithelium [37,38]. As these cells die, CdMT is released into tubular lumen and is excreted in urine [39]. Most or all excreted Cd originates from injured or dying kidney tubular epithelial cells, thus the excretion of Cd itself indicates the severity of the kidney injury at the present time [39]. A correlation between kidney accumulation and urinary Cd concentration also forms the basis for urinary Cd as an indicator of long-term exposure to Cd or its body burden [40].
The deleterious effects of Cd exposure on the kidneys have been investigated extensively in workplace and non-workplace exposure settings [41]. However, a few studies have explored the mechanism by which Cd raises blood pressure. The present study aimed to test the hypothesis that an increase in blood pressure is the result of kidney tubular cell damage by Cd. Because a reduction in the glomerular filtration rate (GFR) is a common sequela of ischemic acute tubular necrosis, and acute and chronic tubulointerstitial fibrosis, all of which create impediments to filtration [42,43], we quantified tubular cell damage, tubular proteinuria, systolic, and diastolic blood pressures (SBP and DBP) according to the estimated GFR (eGFR) and Cd exposure levels in those diagnosed with and without hypertension. Urinary excretion of Cd (ECd) and blood Cd concentrations ([Cd]b) were used as measures of exposure levels. Urinary excretion of β2-microglobulin (β2M) and N-acetyl-β-D-glucosaminidase (NAG) were used to assess tubular proteinuria and damage to the kidney tubular cells, respectively [41].
2. Results
2.1. Demographic and Biologic Characteristics of Participants
A total of 447 persons (333 women and 114 men) with a mean age of 51.1 years, were recruited to this study (Table 1).

Table 1.
Descriptive characteristics of study subjects according to cadmium burden tertiles.
Overall mean [Cd]u and [Cd]b values were 4.23 and 2.75 µg/L, respectively. Participants were grouped by the tertile of the Cd excretion rate [(ECd/Ccr) × 100]. Corresponding mean (ECd/Ccr) × 100 values in the low, middle, and high tertile groups were 0.38, 2.28 and 6.89 µg/L filtrate, equivalent to ECd/Ecr of 0.48, 3.07 and 8.48 µg/g creatinine. Mean blood Cd concentration [Cd]b values in the low, middle and high tertiles of Cd burden were 0.72, 2.37, and 5.14 µg/L, respectively.
[Cd]u and [Cd]b correlated strongly with each other in both women and men with respective Pearson’s correlation coefficients of 0.688 and 0.615. After controlling for age, [Cd]u and [Cd]b correlations remained with partial r values of 0.584 and 0.658 in women and men, respectively.
The percentages (%) of smoking in the top (42.7%) and middle (34.9%) ECd/Ccr tertile groups were higher than the low (16.2%) tertile group. The % hypertension were similar across ECd/Ccr tertiles, but diabetes was more prevalent in the low tertile (39.2%) compared with the middle (3.4%) and high (4.0%) tertile groups. In parallel, low eGFR was more prevalent in the low tertile (10.3%) than in the middle (1.3%) and top (8.7%) tertiles.
More than half (58.8%) of participants had moderate proteinuria, and 23.9% had severe proteinuria. The % severe tubular proteinuria rose to 31.3% in the top ECd/Ccr tertile, compared with 14.8% in the middle tertile group.
Mean age (56.6 years), mean BMI (25.5 kg/m2), mean SBP (134 mmHg), and mean DBP (83 mmHg) in the low tertile group were all statistically higher than the middle and top ECd/Ccr tertile groups. The mean eGFR of 84 mL/min/1.73 m2 in the low tertile was 7–12 mL/min/1.73 m2 below the mean eGFR values in the middle and top tertiles.
2.2. Cadmium, Hypertension, Low eGFR and Tubular Proteinuria
We used logistic regression to evaluate associations of age, BMI, gender, smoking, diabetes, and Cd burden with prevalence odds ratios (POR) for hypertension (Table 2).

Table 2.
Effects of cadmium burden on prevalence odds ratios for hypertension.
The prevalence odds ratio (POR) for hypertension rose with BMI (POR 1.082, 95% CI: 1.027–1.140) and Cd burden at a medium level (POR 2.114, 95% CI: 1.049–4.260). An increase in POR for hypertension was statistically insignificantly in the heavy Cd burden group (p = 0.092).
Results of an analogous analysis with [Cd]b can be found in Table 3.

Table 3.
Prevalence odds ratios for hypertension in relation to blood cadmium quartiles.
Per every 1 kg/m2 increase in BMI, the POR for hypertension rose 8.3% (95% CI: 2.9–14.0). Compared with [Cd]b < 0.60 µg/L, the POR for hypertension increased to 2.113 (95% CI: 1.191–3.749) and 1.833 (95% CI: 1.000–3.360) in those with [Cd]b of 0.61–1.69, and 1.70–3.38 µg/L, respectively. An increment of the POR for hypertension in the top [Cd]b quartile ([Cd]b > 6.92 µg/L) was statistically insignificant (p = 0.082).
To evaluate the effects of Cd on the prevalence of low eGFR and tubular proteinuria, three more logistic regression models were conducted (Table 4).

Table 4.
Prevalence odds ratios for low eGFR and tubular proteinuria in relation to cadmium body burden and other independent variables.
For every one-year older, the POR for low eGFR, moderate, and severe tubular proteinuria rose 14.6%, 3.7%, and 6.4%, while doubling of body burden of Cd was associated with 41%, 23%, and 48% increases in the POR for low eGFR, moderate, and severe tubular proteinuria, respectively. Among diabetics, there were 4.3-fold, 5.5-fold, and 13.4-fold increases in the POR for low eGFR, moderate, and severe tubular proteinuria, respectively.
2.3. Comparing Effects of Cadmium on eGFR in Women and Men
Scatterplots that related eGFR to the Cd excretion rates Cd in women and men are presented in Figure 1.
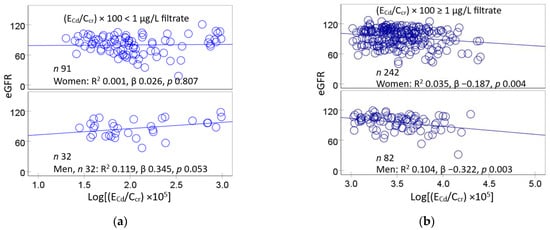
Figure 1.
Comparing cadmium effects on GFR in women and men. Scatterplots relate eGFR to log[(ECd/Ccr) × 105] in women and men with (ECd/Ccr) × 100 < 1 µg/L filtrate (a) and ECd/Ccr) × 100 ≥ 1 µg/L filtrate (b). Coefficients of determination (R2) and standardized β-coefficients for all scatterplots, numbers of subjects in subgroups, and p-values are provided.
2.4. Comparing Effects of Cadmium on eGFR in the Normotensive and Hypertensive Groups
Scatterplots that related eGFR to the excretion rate of Cd in the normotensive and hypertensive groups are presented in Figure 2.
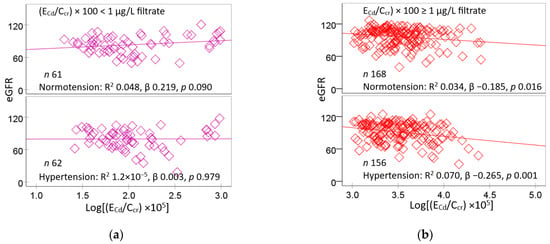
Figure 2.
Comparing the effects of cadmium on GFR in the normotensive and hypertensive groups. Scatterplots relate eGFR to log[(ECd/Ccr) × 105] in normotensive and hypertensive with (ECd/Ccr) × 100 < 1 µg/L filtrate (a) and ECd/Ccr) × 100 ≥ 1 µg/L filtrate (b). Coefficients of determination (R2) and standardized β-coefficients for all scatterplots, numbers of subjects in subgroups, and p-values are provided.
Lower eGFR values were associated with higher ECd/Ccr values in both normotensive (β = −0.034) and hypertensive groups (β = −0.070) who had medium plus heavy Cd burdens (Figure 2b). In comparison, eGFR and ECd/Ccr were not corelated with each other in the groups with a mild Cd burden, regardless of blood pressure status (Figure 2a).
In a multiple regression of eGFR, age, BMI, log2[(ECd/Ccr) × 105], gender, hypertension, smoking, and diabetes contributed, respectively, to 27.9%, 24.8%, 31.8%, and 24.2% of the variation in eGFR in women and men, and in the normotensive and hypertensive groups (Table 5).

Table 5.
Comparing inverse associations of eGFR with the cadmium excretion rate in subjects grouped by gender and blood pressure status.
In women, lower eGFR values were associated with older age (β = −0.528) higher ECd/Ccr (β = −0.121), and diabetes (β = −0.133). In men, lower eGFR values were associated with older age (β = −0.505) and hypertension (β = −0.203). In the normotensive group, eGFR was inversely associated with age (β = −0.559) while showing a positive association with smoking. In the hypertensive group, eGFR was inversely associated with age (β = −0.517), ECd/Ccr (β = −0.177), and diabetes (β = −0.175).
2.5. Inverse Relationships between Blood Pressure and eGFR
Scatterplots relating blood pressure levels to eGFR can be found in Figure 3.
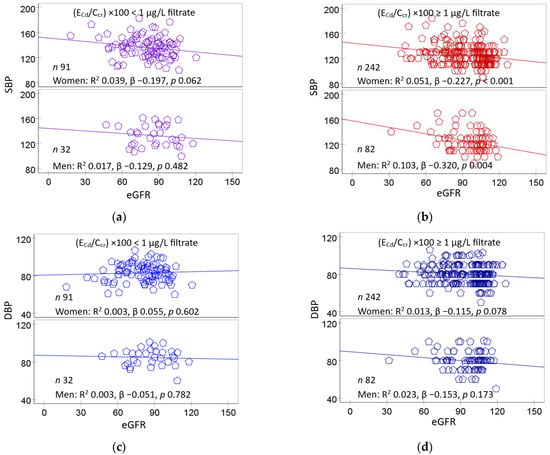
Figure 3.
Cadmium and eGFR as predictors of blood pressure increases. Scatterplots relate SBP (a,b) and DBP (c,d) to eGFR in women and men with (ECd/Ccr) × 100 of <1 and ≥ 1 µg/L filtrate. Coefficients of determination (R2) and standardized β-coefficients for all scatterplots, numbers of participants in subgroups, and p-values are provided.
A significant inverse dose–response relationship was evident between SBP and eGFR in women (β = −0.227) and men (β = −0.320) of the medium plus heavy Cd burden group (Figure 3b), but not a mild Cd burden group (Figure 3a). In comparison, DBP did not significantly correlate with eGFR in women or men at any Cd burden (Figure 3c,d).
2.6. Regression Model Analysis of SBP and DBP
Results of an evaluation of the independent effect of GFR and diabetes on SBP and DBP are presented in Table 6.

Table 6.
Multiple linear regression analysis to evaluate association of systolic and diastolic blood pressures with cadmium, eGFR, and other variables.
Age, BMI, log2[(ECd/Ccr) × 105], eGFR, gender, hypertension, smoking, and diabetes together contributed, respectively, to 19.9%, 15.7%, and 15.0% of the variation in SBP in all subjects, the mild Cd burden, and medium plus heavy Cd burden groups. The fractional DBP variation explained by these independent variables in the mild Cd burden, and medium plus heavy Cd burden groups, were 4.6%, 0%, and 5.8%, respectively.
In an inclusive analysis, higher SBP values were associated with older age (β = 0.243), higher BMI (β = 0.113), lower eGFR (β = −0.106), and diabetes (β = 0.216). In the mild Cd burden group, SBP showed positive associations with BMI (β = 0.395) and diabetes (β = 0.202). In the medium plus high Cd burden group, SBP showed a significant association with diabetes (β = 0.265), while showing an inverse association with eGFR (β = −0.176).
In an equivalent inclusive analysis, higher DBP values were associated only with higher BMI values (β = 0.123). In the medium plus high Cd burden group only, higher DBP values were associated with higher BMI (β = 0.123), lower eGFR (β = −0.130), and diabetes (β = 0.193).
2.7. Mediation Analysis
We employed a simple mediation model analysis to explore whether Cd increased blood pressure through its effect on GFR. In this analysis, eGFR was a single mediator, while ECd/Ccr was an independent variable, and SBP or DBP was a dependent variable). Results for those with (ECd/Ccr) ×100 ≥ 1 µg/L filtrate (the high Cd-group, n = 322) can be found in Figure 4.
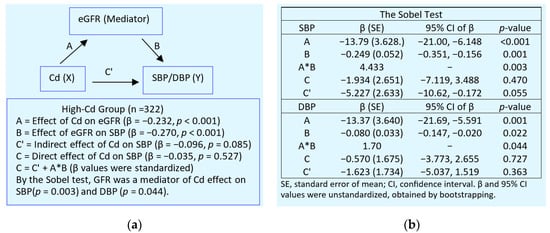
Figure 4.
Mediation analysis of the effect of cadmium on blood pressure in the high-exposure group. (a) A model depicts eGFR as a mediator of the effect of Cd on blood pressure increases and standardized β values (b) The Sobel test of unstandardized β coefficients describing relationships of Cd with eGFR (A), eGFR with blood pressure (B), and Cd with blood pressure (C′).
In the high-Cd group, Cd did not affect SBP or DBP directly, but through its effect on GFR. GFR was a full mediator of the increment of both SBP and DBP in Cd exposed persons with (ECd/Ccr) ×100 ≥ 1 µg/L filtrate.
An equivalent mediation analysis was undertaken for those with (ECd/Ccr) ×100 < 1 µg/L filtrate (the low-Cd burden group, n = 123), and results are provided in Figure 5.
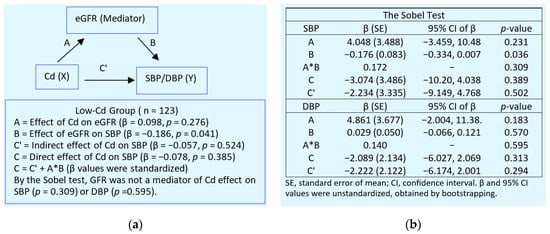
Figure 5.
Mediation analysis of the effect of cadmium on blood pressure in the low-exposure group. (a) A model depicts eGFR as a mediator of the effect of Cd on blood pressure increases and standardized β values. (b) The Sobel test of unstandardized β coefficients describing relationships of Cd with eGFR (A), eGFR with blood pressure (B), and Cd with blood pressure (C′).
In the low-Cd group (Figure 5), an effect of eGFR on SBP was statistically significant (standardized β = −0.186, p = 0.041). However, the Sobel test result (A*B) indicated that eGFR was not a mediator of the effect of Cd on SBP (p = 0.309) or DBP (p = 0.595).
3. Discussion
In this Thai cohort of 447 adults, the overall mean Cd excretion rate was 0.003 µg/L filtrate, corresponding to 4.03 µg/g creatinine. The mean blood and urinary Cd concentrations were 2.75 and 4.23 µg/L, respectively. Nearly half (48.8%) of the cohort’s participants had hypertension, while 15.4% and 6.9% had diabetes and low eGFR, respectively. Similarly, a study from Bangladesh reported that half of those aged ≥ 60 years had hypertension [46]. The prevalence of low eGFR in our study was in line with the figure of 6.3% found in the Taiwanese general population [47]. However, the % of hypertension and diabetes in the present study were higher than those recorded in studies from the U.S., where hypertension and diabetes were 39% and 10.3–13%, respectively [48,49].
The high prevalence of hypertension in this cohort was its strength as it meant that even a modest sample size (n < 1000) could offer a sufficient number of cases from which a reliable conclusion could be drawn. Previously, an effect of smoking on the risk of CVD had been found to be partially mediated by Cd [50,51]. An inclusion of smokers and diabetics was an additional strength as they enabled an adjustment for their effects in realistic population situations. Another strength was that Cd exposure was assessed with blood and urinary Cd levels.
The limitations of the study are acknowledged. They include a one-time-only assessment of Cd exposure and its effects, and the heterogeneity in the hormonal status of women; both menopausal and post-menopausal women were included [52,53,54,55,56], and there was a small number of men (n = 114) in the study cohort; this meant that definitive conclusions about gender disparity in the prevalence, severity, and adverse outcomes of Cd-induced hypertension could not be made [53,54,55,56].
3.1. A Rise in Blood Pressure at Low Levels of Cadmium Exposure
An increased risk of hypertension was associated with both urinary and blood Cd levels (Table 2 and Table 3). POR for hypertension rose two-fold in the medium burden group and in those with the blood Cd quartiles 2 and 3. However, the increases in POR for hypertension in those with a heavy burden of Cd (POR 1.66) and those with the top blood Cd quartile (POR 1.80) were not statistically significant. Thus, Cd effects on blood pressure appeared to be particularly strong in low-dose exposure conditions as detailed below.
In a Chinese case-control study, a 1.33-fold increase in the risk of hypertension was associated with urinary Cd levels > 1.07 μg/L [20]. In the present study, a two-fold rise in POR for hypertension was observed in the medium burden group with urinary Cd levels > 0.57 µg/L (Table 2). A 2.6-fold increase in risk of hypertension was seen in white and Mexican-American women who had blood Cd levels ≥ 0.4 µg/L [15]. In the present study, an increase in POR for hypertension was found in those who had blood Cd of 0.61–3.38 µg/L (Table 3).
In a study from Korea, increases in prevalence of pre-hypertension and hypertension were associated with doubling blood Cd from 0.62 to 1.33 µg/L in men, and from 0.73 to 1.57 µg/L in women [22]. In a study of residents in a Cd-polluted area of China, increased risk of hypertension was associated with blood Cd of 1–1.7 µg/L [19].
In a Canadian study, SBP and DBP were positively associated with blood Cd, but the risk of hypertension fell 52% in women who were current smokers and had a very high blood Cd level [18]. In the Canadian health measure survey, the mean values for blood and urinary excretion of Cd in current smokers were 1.64 µg/L and 0.58 µg/g creatinine, respectively [57]. A similar observation was made in a U.S. population study, where associations between blood pressure measurements and blood Cd were particularly strong in non-smokers, moderate in former smokers, and weak or negligible in current smokers [15].
3.2. Different Susceptibility to Cadmium-Induced Hypertension
The urinary and blood Cd levels found to be associated with a significant increase in risk of hypertension varied among populations. This may be due to different susceptibility to hypertension or some protective factors. For instance, white and Mexican-American women were found to be more susceptible to Cd-induced blood pressure increases than black women; an increased risk of hypertension was seen in Caucasian (OR 1.54) and Mexican-American women (OR 2.38) who had blood Cd as little as 0.4 µg/L, but not in black women or white, black, or Mexican-American men [16].
Male–female differences were evident from a regression model analysis (Table 5), where an inverse association of eGFR and Cd burden was found only in women (β = −0.121, p = 0.051). In comparison, male eGFR did not show a significant association with Cd burden (β = −0.077, p = 0.463). In a Taiwanese study, an association of urinary Cd and a tubular damage marker (urinary NAG) was found in women only [58]. In a Thai population study, the risk of hypertension rose 20% in Cd-exposed subjects with kidney tubular damage, assessed with urinary NAG excretion [59].
People with diabetes were more susceptible to adverse kidney effects of Cd than their non-diabetic counterparts. In a Dutch cross-sectional study, including 231 patients with type 2 diabetes, Cd exposure increased the risk of diabetic kidney disease [60]. In a six-year median follow-up of these diabetic patients, a progressive reduction of eGFR was attributable to Cd exposure [36].
In a prospective cohort study, a 49% increase in all-cause mortality among the diabetics was associated with urinary Cd levels > 0.60 μg/L [61]. In the present study, the risk of having low eGFR, moderate, and severe tubular proteinuria among diabetics rose 4.3-fold, 5.5-fold, and 13.4-fold, respectively (Table 4). Both SBP (β = 0.265) and DBP (β = 0.193) rose significantly among diabetics with (ECd/Ccr) × 100 ≥ 1 µg/L filtrate (Table 6). This Cd-induced SBP and DBP increment may promote kidney disease development in Cd-exposed diabetics given that hypertension is a strong independent risk factor for the development and progression of CKD [3,62]. A 1.76-fold increase in death from CVD among U.S. citizens with hypertension was associated with elevated Cd exposure, indicated by blood Cd levels ≥ 0.80 μg/L [63]. At the same Cd exposure level, the risk of death from CVD rose 2.12-fold among non-smokers who had hypertension [63].
3.3. A Rise of Blood Pressure Due to Tubular Damage and GFR Loss
To the best of our knowledge, the present study has provided, for the first time, evidence linking Cd-induced eGFR reduction to a rise in blood pressure (Figure 3). SBP was inversely associated with eGFR in women (β = −0.227) and men (β = −0.320) who had medium plus heavy Cd burdens, (ECd/Ccr) × 100 ≥ 1 µg/L filtrate. DBP showed a weak inverse association with eGFR (Figure 3a,b vs. Figure 3c,d). By multiple regression analysis (Table 6), an independent effect of eGFR reduction on a rise of SBP was found in the medium plus heavy Cd burden group (β = −0.176). Using the mediation analysis, GFR reduction was a full mediator of Cd effect on blood pressure increases in the high-exposure group (Figure 4). Our observation that blood pressure rises as GFR falls helps to explain why patients with CKD have hypertension almost universally.
The doubling of the body burden of Cd was associated, respectively, with increases of 41%, 23%, and 48% in the POR values for low eGFR, moderate, and severe tubular proteinuria, evident from increased β2M excretion levels (Table 4). In Japanese population studies, increased β2M excretion levels were associated with enhanced risks of hypertension and a large decline in eGFR (10 mL/min/1.73 m2) over a five-year observation period [64,65]. Thus, an increased risk of hypertension among study subjects could be attributed to Cd-induced tubular damage and GFR loss.
In summary, we have shown that increases in blood pressure may be a consequence of a decrease in GFR induced by Cd. The indispensable role of the kidneys in long-term blood pressure regulation is well established [2]. As their function declines (indicated by low eGFR), the kidneys eliminate less water and sodium, which may increase blood pressure. Rats with Cd-induced hypertension showed increased sodium retention and reduced sodium excretion [66,67,68]. Thus, increased tubular avidity for filtered sodium appeared to be a possible mechanism by which lifelong, low-dose Cd intake caused hypertension.
CKD has now reached epidemic proportions and is predicted to become an even greater health problem in years to come as its major risk factors—obesity, diabetes, hypertension, and non-alcoholic fatty liver—continue to rise. Given the immense financial and community burden, developing strategies to reduce its progression to kidney failure is of vital importance. Cd excretion corresponding to a discernible GFR decline at ECd/Ccr of 0.01 µg/L filtrate is extremely low.
4. Materials and Methods
4.1. Participants
This study was conducted following the principles outlined in the Declaration of Helsinki. Participants were recruited from Nakhon Si Thammarat Province in the south and Mae Sot District in the northwest of Thailand [69,70]. Previous studies suggest female preponderance effects Cd exposure [9,12]. Thus, more women were recruited to maximize the likelihood of finding an effect of Cd in a modest sample size (n = 447).
All participants gave informed consent prior to participation. They had been living at their current addresses for at least 30 years. Exclusion criteria were pregnancy, breast-feeding, a history of metal work, and a hospital record or physician’s diagnosis of an advanced chronic disease. All subjects were provided with details of study objectives, study procedures, benefits, and potential risks, and they all provided their written informed consent prior to participation.
The Office of the Human Research Ethics Committee of Walailak University approved the study protocol for the Nakhon Si Thammarat group (Approval number WUEC-20-132-01, 28 May 2020) [69]. The study protocol for the Mae Sot group was approved by the Institutional Ethical Committees of Chiang Mai University and the Mae Sot Hospital (Approval No. 142/2544, 5 October 2001) [70].
Levels of various contaminants, including arsenic, chromium, lead, and Cd in samples of soils and food crops in Nakhon Si Thammarat were within permissible ranges [68], and no association was found between water arsenic concentration and the risk of diabetes [71,72]. In comparison, the Cd concentration of the paddy soil samples from the Mae Sot district exceeded the standard of 0.15 mg/kg, and the rice samples collected from household storage contained four times the amount of the permissible Cd level of 0.1 mg/kg [73]. In a health survey of residents of the Mae Sot District (n = 5273), urinary Cd excretion levels correlated with hypertension and diabetes [74].
4.2. Blood Pressure and Cadmium Exposure Ascertainment
Our study design was population-based and recruited participants from their communities. This precluded a 24 h measurement, and more visits to communities for a second measurement. The one-time measurement of SBP/DBP was the average of 3 repeated measurements. The diagnosis of hypertension relied primarily on the assessment made by the presiding physician and the recorded use of anti-hypertensive medication. Of 233 subjects included as hypertensive cases in our study, 220 (94.4%) were being treated and 13 hypertensive cases were identified during our visit.
Cd exposure was based on urinary Cd excretion (ECd) and blood Cd concentration ([Cd]b). Simultaneous urine and whole blood sampling were undertaken after an overnight fast. Aliquots of blood and urine samples were stored at −80 °C for later analysis. Atomic absorption spectrophotometry was used to determine urinary and blood levels of [Cd]u and [Cd]b using multi-element standards (Merck KGaA, Darmstadt, Germany) for instrument calibration. For quality control and assurance purposes, blood and urine samples from subjects, blood control samples (ClinChek, Munich, Germany), and the reference urine metal controls (Lyphocheck, Bio-Rad, Hercules, CA, USA) were simultaneously analyzed.
The limit of detection (LOD) for Cd in blood or urine was 0.3 µg/L for [Cd]b and 0.1 µg/L for [Cd]u. The Cd concentration assigned to a sample that contained Cd below its LOD was assigned a value of the LOD divided by the square root of 2 [75].
4.3. Normalization of Cadmium Excretion Rate
ECd was normalized to creatinine clearance (Ccr) as ECd/Ccr = [Cd]u[cr]p/[cr]u, where [Cd]u = urine concentration of Cd (mass/volume); [cr]p = plasma creatinine concentration (mg/dL); and [cr]u = urine creatinine concentration (mg/dL). ECd/Ccr was expressed as an amount of Cd excreted per volume of the glomerular filtrate. Ccr-normalization corrects for urine dilution and number of functioning nephrons [45].
ECd was normalized to Ecr as [Cd]u/[cr]u, where [Cd]u = urine concentration of Cd (mass/volume) and [cr]u = urine creatinine concentration (mg/dL). ECd/Ecr was expressed in μg/g creatinine. Ecr-normalization corrects for urine dilution, but it is influenced by muscle mass. The effect of Cd exposure on GFR was obscure, when ECd was normalized to Ecr [76].
4.4. Estimated Glomerular Filtration Rate (eGFR)
We used the GFR estimating equations, established by the chronic kidney disease epidemiology collaboration (CKD–EPI) to compute the estimated GFR (eGFR) [44]. The CKD–EPI equations have been validated with inulin clearance [77].
Male eGFR = 141 × [cr]p/0.9Y × 0.993age, where Y = −0.411 if [cr]p ≤ 0.9 mg/dL and Y = −1.209 if [cr]p > 0.9 mg/dL.
Female eGFR = 144 × [cr]p/0.7Y × 0.993age, where Y = −0.329 if [cr]p ≤ 0.7 mg/dL and Y = −1.209 if [cr]p > 0.7 mg/dL.
4.5. Statistical Analysis
Data were analyzed with IBM SPSS Statistics 21 (IBM Inc., New York, NY, USA). The Kruskal-Wallis test was used to assess differences in means across tertiles of Cd burden, and the Pearson chi-squared test was used to assess differences in percentages. Distribution of continuous variables was assessed by the one-sample Kolmogorov–Smirnov test. A logarithmic transformation was applied to variables that showed rightward skewing. A simple mediation model with a single mediator was used in the mediation analysis [78,79]
Prevalence Odds Ratio (POR) for hypertension, which was defined as SBP ≥ 140 mmHg or DBP ≥ 90 mmHg [1], was determined by logistic regression. Multiple linear regression was used to identify variables affecting eGFR, SBP, and DBP. For all tests, p-values ≤ 0.05 were considered as statistically significant.
5. Conclusions
By mediation analysis, an increase in SBP was attributable totally to Cd-induced GFR loss. Cd appeared to influence SBP more markedly than DBP. A two-fold increased risk of hypertension was associated with urinary Cd excretion of 0.98 µg/g creatinine and a blood Cd level of 0.61 µg/L. As these are levels that are reported widely in studies of non-occupationally exposed populations from across the world, it is imperative that authorities monitor the environmental levels of Cd closely, especially in staple foods.
Author Contributions
Conceptualization, S.S., D.A.V. and A.B.Đ.; methodology, S.Y., T.K. and P.P.; formal analysis, S.S. and A.B.Đ.; investigation, S.S., S.Y., T.K. and P.P.; resources, D.A.V., S.Y. and A.B.Đ.; data curation, S.S. and S.Y.; writing—original draft preparation, S.S.; writing—review and editing, S.S., D.A.V. and A.B.Đ.; project administration, S.S. and S.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This is not applicable for the present study, which used archived data [69,70].
Informed Consent Statement
Written informed consent was obtained from study subjects.
Data Availability Statement
All data are contained within this article.
Acknowledgments
This work was supported by resources from the Centre for Kidney Disease Research, Translational Research Institute, the Department of Kidney and Transplant Services, Princess Alexandra Hospital, the Department of Toxicology, Faculty of Pharmacy, University of Belgrade, Serbia.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Bloch, M.J.; Basile, J.N. Review of recent literature in hypertension: Updated clinical practice guidelines for chronic kidney disease now include albuminuria in the classification system. J. Clin. Hypertens. 2013, 15, 865–867. [Google Scholar] [CrossRef] [PubMed]
- Crowley, S.D.; Coffman, T.M. The inextricable role of the kidney in hypertension. J. Clin. Investig. 2014, 124, 2341–2347. [Google Scholar]
- Kalantar-Zadeh, K.; Jafar, T.H.; Nitsch, D.; Neuen, B.L.; Perkovic, V. Chronic kidney disease. Lancet 2021, 398, 786–802. [Google Scholar] [CrossRef] [PubMed]
- Foreman, K.J.; Marquez, N.; Dolgert, A.; Fukutaki, K.; Fullman, N.; McGaughey, M.; Pletcher, M.A.; Smith, A.E.; Tang, K.; Yuan, C.W.; et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: Reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet 2018, 392, 2052–2090. [Google Scholar] [CrossRef] [PubMed]
- GBD 2021 Forecasting Collaborators. Burden of disease scenarios for 204 countries and territories, 2022–2050: A forecasting analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 2204–2256. [Google Scholar] [CrossRef]
- Verzelloni, P.; Urbano, T.; Wise, L.A.; Vinceti, M.; Filippini, T. Cadmium exposure and cardiovascular disease risk: A systematic review and dose-response meta-analysis. Environ. Pollut. 2024, 345, 123462. [Google Scholar] [CrossRef] [PubMed]
- Doccioli, C.; Sera, F.; Francavilla, A.; Cupisti, A.; Biggeri, A. Association of cadmium environmental exposure with chronic kidney disease: A systematic review and meta-analysis. Sci. Total Environ. 2024, 906, 167165. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wang, X.; Ma, Z.; Dang, Y.; Yang, Y.; Cao, S.; Ouyang, C.; Shi, X.; Pan, J.; Hu, X. Associations of urinary and blood cadmium concentrations with all-cause mortality in US adults with chronic kidney disease: A prospective cohort study. Environ. Sci. Pollut. Res. Int. 2023, 30, 61659–61671. [Google Scholar] [CrossRef]
- Nishijo, M.; Satarug, S.; Honda, R.; Tsuritani, I.; Aoshima, K. The gender differences in health effects of environmental cadmium exposure and potential mechanisms. Mol. Cell. Biochem. 2004, 255, 87–92. [Google Scholar] [CrossRef]
- Trzcinka-Ochocka, M.; Jakubowski, M.; Szymczak, W.; Janasik, B.; Brodzka, R. The effects of low environmental cadmium exposure on bone density. Environ. Res. 2010, 110, 286–293. [Google Scholar] [CrossRef]
- Nishijo, M.; Nambunmee, K.; Suvagandha, D.; Swaddiwudhipong, W.; Ruangyuttikarn, W.; Nishino, Y. Gender-specific impact of cadmium exposure on bone metabolism in older people living in a cadmium-polluted area in Thailand. Int. J. Environ. Res. Public Health 2017, 14, 401. [Google Scholar] [CrossRef] [PubMed]
- Madrigal, J.M.; Ricardo, A.C.; Persky, V.; Turyk, M. Associations between blood cadmium concentration and kidney function in the U.S. population: Impact of sex, diabetes and hypertension. Environ. Res. 2018, 169, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Mortensen, M.E.; Wong, L.Y.; Osterloh, J.D. Smoking status and urine cadmium above levels associated with subclinical renal effects in U.S. adults without chronic kidney disease. Int. J. Hyg. Environ. Health 2011, 214, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Satarug, S.; Ujjin, P.; Vanavanitkun, Y.; Baker, J.R.; Moore, M.R. Influence of body iron store status and cigarette smoking on cadmium body burden of healthy Thai women and men. Toxicol. Lett. 2004, 148, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Tellez-Plaza, M.; Navas-Acien, A.; Crainiceanu, C.M.; Guallar, E. Cadmium exposure and hypertension in the 1999–2004 National Health and Nutrition Examination Survey (NHANES). Environ. Health Perspect. 2008, 116, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Scinicariello, F.; Abadin, H.G.; Murray, H.E. Association of low-level blood lead and blood pressure in NHANES 1999–2006. Environ. Res. 2011, 111, 1249–1257. [Google Scholar] [CrossRef]
- Oliver-Williams, C.; Howard, A.G.; Navas-Acien, A.; Howard, B.V.; Tellez-Plaza, M.; Franceschini, N. Cadmium body burden, hypertension, and changes in blood pressure over time: Results from a prospective cohort study in American Indians. J. Am. Soc. Hypertens. 2018, 12, 426–437.e9. [Google Scholar] [CrossRef]
- Garner, R.E.; Levallois, P. Associations between cadmium levels in blood and urine, blood pressure and hypertension among Canadian adults. Environ. Res. 2017, 155, 64–72. [Google Scholar] [CrossRef]
- Chen, X.; Wang, Z.; Zhu, G.; Liang, Y.; Jin, T. Benchmark dose estimation of cadmium reference level for hypertension in a Chinese population. Environ. Toxicol. Pharmacol. 2015, 39, 208–212. [Google Scholar] [CrossRef]
- Wu, W.; Liu, D.; Jiang, S.; Zhang, K.; Zhou, H.; Lu, Q. Polymorphisms in gene MMP-2 modify the association of cadmium exposure with hypertension risk. Environ. Int. 2019, 124, 441–447. [Google Scholar] [CrossRef]
- Zhong, Q.; Wu, H.B.; Niu, Q.S.; Jia, P.P.; Qin, Q.R.; Wang, X.D.; He, J.L.; Yang, W.J.; Huang, F. Exposure to multiple metals and the risk of hypertension in adults: A prospective cohort study in a local area on the Yangtze River, China. Environ. Int. 2021, 153, 106538. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.K.; Kim, Y. Association of blood cadmium with hypertension in the Korean general population: Analysis of the 2008–2010 Korean National Health and Nutrition Examination Survey data. Am. J. Ind. Med. 2012, 55, 1060–1067. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.A.; Park, E.; Kim, S.; Kim, B. Influence of serum ferritin combined with blood cadmium concentrations on blood pressure and hypertension: From the Korean National Health and Nutrition Examination Survey. Chemosphere 2022, 288, 132469. [Google Scholar] [CrossRef] [PubMed]
- Kaneda, M.; Wai, K.M.; Kanda, A.; Ando, M.; Murashita, K.; Nakaji, S.; Ihara, K. Low level of serum cadmium in relation to blood pressures among Japanese general population. Biol. Trace Element Res. 2021, 200, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, T.; Kataoka, Y.; Hayashi, K.; Matsuda, R.; Uneyama, C. Dietary exposure of the Japanese general population to elements: Total diet study 2013–2018. Food Saf. 2022, 10, 83–101. [Google Scholar] [CrossRef]
- Almerud, P.; Zamaratskaia, G.; Lindroos, A.K.; Bjermo, H.; Andersson, E.M.; Lundh, T.; Ankarberg, E.H.; Lignell, S. Cadmium, total mercury, and lead in blood and associations with diet, sociodemographic factors, and smoking in Swedish adolescents. Environ. Res. 2021, 197, 110991. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Song, H.; Lee, J.; Kim, Y.J.; Chung, H.S.; Yu, J.M.; Jang, G.; Park, R.; Chung, W.; Oh, C.M.; et al. Smoking and passive smoking increases mortality through mediation effect of cadmium exposure in the United States. Sci. Rep. 2023, 13, 3878. [Google Scholar] [CrossRef]
- Hill, D.T.; Jandev, V.; Petroni, M.; Atallah-Yunes, N.; Bendinskas, K.; Brann, L.S.; Heffernan, K.; Larsen, D.A.; MacKenzie, J.A.; Palmer, C.D.; et al. Airborne levels of cadmium are correlated with urinary cadmium concentrations among young children living in the New York state city of Syracuse, USA. Environ. Res. 2023, 223, 115450. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, Y.; Nomiyama, T.; Kumagai, N.; Dekio, F.; Uemura, T.; Takebayashi, T.; Nishiwaki, Y.; Matsumoto, Y.; Sano, Y.; Hosoda, K.; et al. Uptake of cadmium in meals from the digestive tract of young non-smoking Japanese female volunteers. J. Occup. Health 2003, 45, 43–52. [Google Scholar] [CrossRef]
- Horiguchi, H.; Oguma, E.; Sasaki, S.; Miyamoto, K.; Ikeda, Y.; Machida, M.; Kayama, F. Comprehensive study of the effects of age, iron deficiency, diabetes mellitus, and cadmium burden on dietary cadmium absorption in cadmium-exposed female Japanese farmers. Toxicol. Appl. Pharmacol. 2004, 196, 114–123. [Google Scholar] [CrossRef]
- Satarug, S.; Phelps, K.R. Chapter 14: Cadmium Exposure and Toxicity. In Metal Toxicology Handbook; Bagchi, D., Bagchi, M., Eds.; CRC Press: Boca Raton, FL, USA, 2021; pp. 219–274. [Google Scholar]
- Satarug, S.; Vesey, D.A.; Gobe, G.C.; Phelps, K.R. Estimation of health risks associated with dietary cadmium exposure. Arch. Toxicol. 2023, 97, 329–358. [Google Scholar] [CrossRef] [PubMed]
- Fujita, Y.; el Belbasi, H.I.; Min, K.S.; Onosaka, S.; Okada, Y.; Matsumoto, Y.; Mutoh, N.; Tanaka, K. Fate of cadmium bound to phytochelatin in rats. Res. Commun. Chem. Pathol. Pharmacol. 1993, 82, 357–365. [Google Scholar] [PubMed]
- Langelueddecke, C.; Roussa, E.; Fenton, R.A.; Thévenod, F. Expression and function of the lipocalin-2 (24p3/NGAL) receptor in rodent and human intestinal epithelia. PLoS ONE 2013, 8, e71586. [Google Scholar] [CrossRef] [PubMed]
- Langelueddecke, C.; Lee, W.K.; Thévenod, F. Differential transcytosis and toxicity of the hNGAL receptor ligands cadmium-metallothionein and cadmium-phytochelatin in colon-like Caco-2 cells: Implications for in vivo cadmium toxicity. Toxicol. Lett. 2014, 226, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Oosterwijk, M.M.; Hagedoorn, I.J.M.; Maatman, R.G.H.J.; Bakker, S.J.L.; Navis, G.; Laverman, G.D. Cadmium, active smoking and renal function deterioration in patients with type 2 diabetes. Nephrol. Dial. Transplant. 2023, 38, 876–883. [Google Scholar] [CrossRef] [PubMed]
- Satarug, S.; Baker, J.R.; Reilly, P.E.; Moore, M.R.; Williams, D.J. Cadmium levels in the lung, liver, kidney cortex, and urine samples from Australians without occupational exposure to metals. Arch. Environ. Health 2002, 57, 69–77. [Google Scholar] [CrossRef]
- Barregard, L.; Sallsten, G.; Lundh, T.; Mölne, J. Low-level exposure to lead, cadmium and mercury, and histopathological findings in kidney biopsies. Environ. Res. 2022, 211, 113119. [Google Scholar] [CrossRef]
- Satarug, S.; Vesey, D.A.; Ruangyuttikarn, W.; Nishijo, M.; Gobe, G.C.; Phelps, K.R. The source and pathophysiologic significance of excreted cadmium. Toxics 2019, 7, 55. [Google Scholar] [CrossRef] [PubMed]
- Akerstrom, M.; Barregard, L.; Lundh, T.; Sallsten, G. The relationship between cadmium in kidney and cadmium in urine and blood in an environmentally exposed population. Toxicol. Appl. Pharmacol. 2013, 268, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Johri, N.; Jacquillet, G.; Unwin, R. Heavy metal poisoning: The effects of cadmium on the kidney. Biometals 2010, 23, 783–792. [Google Scholar] [CrossRef]
- Satarug, S.; Gobe, G.C.; Vesey, D.A.; Phelps, K.R. Cadmium and lead exposure, nephrotoxicity, and mortality. Toxics 2020, 8, 86. [Google Scholar] [CrossRef] [PubMed]
- Lang, S.M.; Schiffl, H. Smoking status, cadmium, and chronic kidney disease. Ren. Replace Ther. 2024, 10, 17. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Scmid, C.H.; Zhang, Y.; Castro, A.F., III; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Phelps, K.R.; Gosmanova, E.O. A generic method for analysis of plasma concentrations. Clin. Nephrol. 2020, 94, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Hanif, A.A.M.; Shamim, A.A.; Hossain, M.M.; Hasan, M.; Khan, M.S.A.; Hossaine, M.; Ullah, M.A.; Sarker, S.K.; Rahman, S.M.M.; Mitra, D.K.; et al. Gender-specific prevalence and associated factors of hypertension among elderly Bangladeshi people: Findings from a nationally representative cross-sectional survey. BMJ Open 2021, 11, e038326. [Google Scholar] [CrossRef] [PubMed]
- Tsai, H.J.; Hung, C.H.; Wang, C.W.; Tu, H.P.; Li, C.H.; Tsai, C.C.; Lin, W.Y.; Chen, S.C.; Kuo, C.H. Associations among heavy metals and proteinuria and chronic kidney disease. Diagnostics 2021, 11, 282. [Google Scholar] [CrossRef] [PubMed]
- Shi, P.; Yan, H.; Fan, X.; Xi, S. A benchmark dose analysis for urinary cadmium and type 2 diabetes mellitus. Environ. Pollut. 2021, 273, 116519. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Oh, S.; Kang, H.; Kim, S.; Lee, G.; Li, L.; Kim, C.T.; An, J.N.; Oh, Y.K.; Lim, C.S.; et al. Environment-wide association study of CKD. Clin. J. Am. Soc. Nephrol. 2020, 15, 766–775. [Google Scholar] [CrossRef]
- Li, H.; Fagerberg, B.; Sallsten, G.; Borné, Y.; Hedblad, B.; Engström, G.; Barregard, L.; Andersson, E.M. Smoking-induced risk of future cardiovascular disease is partly mediated by cadmium in tobacco: Malmö Diet and Cancer Cohort Study. Environ. Health 2019, 18, 56. [Google Scholar] [CrossRef]
- Hecht, E.M.; Landy, D.C.; Ahn, S.; Hlaing, W.M.; Hennekens, C.H. Hypothesis: Cadmium explains, in part, why smoking increases the risk of cardiovascular disease. J. Cardiovasc. Pharmacol. Ther. 2013, 18, 550–554. [Google Scholar] [CrossRef]
- Vahter, M.; Berglund, M.; Akesson, A. Toxic metals and the menopause. J. Br. Menopause Soc. 2004, 10, 60–64. [Google Scholar] [CrossRef] [PubMed]
- Reckelhoff, J.F. Gender differences in the regulation of blood pressure. Hypertension 2001, 37, 1199–1208. [Google Scholar] [CrossRef] [PubMed]
- Reckelhoff, J.F. Mechanisms of sex and gender differences in hypertension. J. Hum. Hypertens. 2023, 37, 596–601. [Google Scholar] [CrossRef] [PubMed]
- Connelly, P.J.; Currie, G.; Delles, C. Sex differences in the prevalence, outcomes and management of hypertension. Curr. Hypertens. Rep. 2022, 24, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.M.; Kim, H.C.; Kang, D.R. Sex differences in hypertension prevalence and control: Analysis of the 2010–2014 Korea National Health and Nutrition Examination Survey. PLoS ONE 2017, 12, e0178334. [Google Scholar] [CrossRef] [PubMed]
- Garner, R.; Levallois, P. Cadmium levels and sources of exposure among Canadian adults. Health Reports 2016, 27, 10–18. [Google Scholar] [PubMed]
- Liao, K.W.; Chien, L.C.; Chen, Y.C.; Kao, H.C. Sex-specific differences in early renal impairment associated with arsenic, lead, and cadmium exposure among young adults in Taiwan. Environ. Sci. Pollut. Res. Int. 2022, 29, 52655–52664. [Google Scholar] [CrossRef] [PubMed]
- Satarug, S.; Nishijo, M.; Ujjin, P.; Vanavanitkun, Y.; Moore, M.R. Cadmium-induced nephropathy in the development of high blood pressure. Toxicol. Lett. 2005, 157, 57–68. [Google Scholar] [CrossRef] [PubMed]
- Hagedoorn, I.J.M.; Gant, C.M.; Huizen, S.V.; Maatman, R.G.H.J.; Navis, G.; Bakker, S.J.L.; Laverman, G.D. Lifestyle-related exposure to cadmium and lead is associated with diabetic kidney disease. J. Clin. Med. 2020, 9, 2432. [Google Scholar] [CrossRef]
- Liu, Y.; Yang, D.; Shi, F.; Wang, F.; Liu, X.; Wen, H.; Mubarik, S.; Yu, C. Association of serum 25(OH)D, cadmium, CRP with all-cause, cause-specific mortality: A prospective cohort study. Front. Nutr. 2022, 9, 803985. [Google Scholar] [CrossRef]
- Mayne, K.J.; Sullivan, M.K.; Lees, J.S. Sex and gender differences in the management of chronic kidney disease and hypertension. J. Hum. Hypertens. 2023, 37, 649–653. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Shen, R.; Shen, J.; Lyu, L.; Wei, T. Association of blood cadmium with all-cause and cause-specific mortality in patients with hypertension. Front. Public Health 2023, 11, 1106732. [Google Scholar] [CrossRef] [PubMed]
- Mashima, Y.; Konta, T.; Kudo, K.; Takasaki, S.; Ichikawa, K.; Suzuki, K.; Shibata, Y.; Watanabe, T.; Kato, T.; Kawata, S.; et al. Increases in urinary albumin and beta2-microglobulin are independently associated with blood pressure in the Japanese general population: The Takahata Study. Hypertens. Res. 2011, 34, 831–835. [Google Scholar] [CrossRef] [PubMed]
- Kudo, K.; Konta, T.; Mashima, Y.; Ichikawa, K.; Takasaki, S.; Ikeda, A.; Hoshikawa, M.; Suzuki, K.; Shibata, Y.; Watanabe, T.; et al. The association between renal tubular damage and rapid renal deterioration in the Japanese population: The Takahata study. Clin. Exp. Nephrol. 2011, 15, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Perry, H.M.; Erlanger, M.; Perry, E.F. Increase in the systolic pressure of rats chronically fed cadmium. Environ. Health Perspect. 1979, 28, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Perry, H.M., Jr.; Erlanger, M.W. Sodium retention in rats with cadmium-induced hypertension. Sci. Total Environ. 1981, 22, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Peña, A.; Iturri, S.J. Cadmium as hypertensive agent. Effect on ion excretion in rats. Comp. Biochem. Physiol. C Comp. Pharmacol. Toxicol. 1993, 106, 315–319. [Google Scholar] [CrossRef]
- Yimthiang, S.; Pouyfung, P.; Khamphaya, T.; Kuraeiad, S.; Wongrith, P.; Vesey, D.A.; Gobe, G.C.; Satarug, S. Effects of environmental exposure to cadmium and lead on the risks of diabetes and kidney dysfunction. Int. J. Environ. Res. Public Health 2022, 19, 2259. [Google Scholar] [CrossRef] [PubMed]
- Satarug, S.; Swaddiwudhipong, W.; Ruangyuttikarn, W.; Nishijo, M.; Ruiz, P. Modeling cadmium exposures in low- and high-exposure areas in Thailand. Environ. Health Perspect. 2013, 121, 531–536. [Google Scholar] [CrossRef]
- Zarcinas, B.A.; Pongsakul, P.; McLaughlin, M.J.; Cozens, G. Heavy metals in soils and crops in Southeast Asia. 2. Thailand. Environ. Geochem. Health 2004, 26, 359–371. [Google Scholar] [CrossRef]
- Sripaoraya, K.; Siriwong, W.; Pavittranon, S.; Chapman, R.S. Environmental arsenic exposure and risk of diabetes type 2 in Ron Phibun subdistrict, Nakhon Si Thammarat Province, Thailand: Unmatched and matched case-control studies. Risk Manag Healthc. Policy 2017, 10, 41–48. [Google Scholar] [CrossRef]
- Suwatvitayakorn, P.; Ko, M.S.; Kim, K.W.; Chanpiwat, P. Human health risk assessment of cadmium exposure through rice consumption in cadmium-contaminated areas of the Mae Tao sub-district, Tak, Thailand. Environ. Geochem. Health 2020, 42, 2331–2344. [Google Scholar] [CrossRef] [PubMed]
- Swaddiwudhipong, W.; Mahasakpan, P.; Limpatanachote, P.; Krintratun, S. Correlations of urinary cadmium with hypertension and diabetes in persons living in cadmium-contaminated villages in northwestern Thailand: A population study. Environ. Res. 2010, 110, 612–616. [Google Scholar] [CrossRef] [PubMed]
- Hornung, R.W.; Reed, L.D. Estimation of average concentration in the presence of nondetectable values. Appl. Occup. Environ. Hyg. 1990, 5, 46–51. [Google Scholar] [CrossRef]
- Satarug, S.; Vesey, D.A.; Nishijo, M.; Ruangyuttikarn, W.; Gobe, G.C.; Phelps, K.R. The effect of cadmium on GFR is clarified by normalization of excretion rates to creatinine clearance. Int. J. Mol. Sci. 2021, 22, 1762. [Google Scholar] [CrossRef] [PubMed]
- White, C.A.; Allen, C.M.; Akbari, A.; Collier, C.P.; Holland, D.C.; Day, A.G.; Knoll, G.A. Comparison of the new and traditional CKD-EPI GFR estimation equations with urinary inulin clearance: A study of equation performance. Clin. Chim. Acta 2019, 488, 189–195. [Google Scholar] [CrossRef] [PubMed]
- MacKinnon, D.P.; Warsi, G.; Dwyer, J.H. A simulation study of mediated effect measures. Multiv. Behav. Res. 1995, 30, 41–62. [Google Scholar] [CrossRef] [PubMed]
- Preacher, K.J.; Hayes, A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Meth. Instrum. Comput. 2004, 36, 717–731. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).